Abstract
Purpose
To evaluate the impact of a novel computer-fabricated lingual nitinol retainer compared to a conventional lingual flexible spiral wire twistflex retainer on oral health.
Methods
The study was based on a retrospective controlled clinical study with pilot character, an in vitro investigation of material-dependent biofilm formation and an analysis of biofilm formation after intraoral incubation. Sixty-one patients with completed fixed orthodontic treatment and retention phase for at least 6 months with twistflex retainers (group 1, n = 31) or computer-aided design/computer-aided manufacturing (CAD/CAM) nitinol retainers (group 2, n = 30) were included and examined regarding plaque index (PI), gingival index (GI), probing depths, bleeding on probing (BOP) and marginal recessions (MR). Material-dependent biofilm formation of twistflex, untreated nitinol and electropolished nitinol wire samples were assessed (1) in vitro: using optical density (OD) measurement of 10 samples of each and (2) in vivo: using histomorphometric analysis of 18 samples of each.
Results
Patients treated with nitinol retainers had significant better oral health indices (PI1 = 1.29 ± 0.06, PI2 = 0.94 ± 0.06; GI1 = 0.71 ± 0.05, GI2 = 0.56 ± 0.04; BOP1 = 0.11 ± 0.01, BOP2 = 0.08 ± 0.01; PD1 = 1.79 ± 0.03 mm, PD2 = 1.59 ± 0.04 mm) except for MR (0.08 ± 0.03 mm versus 0.08 ± 0.02 mm) compared to twistflex retainers. After 24 h intraoral incubation nitinol retainers demonstrated significant less biofilm formation compared to twistflex retainers. In the in vitro investigation the temporary significant differences between the groups were compensated in the end.
Conclusions
Based on the results it can be assumed that nitinol-made CAD/CAM developed lingual retainers have a positive effect on oral health.
Zusammenfassung
Ziel
Beurteilung des Einflusses lingualer konventioneller Twist-Flex-Retainer und innovativer CAD/CAM(„computer-aided design/computer-aided manufacturing“)-Nitinol-Retainer auf die orale Gesundheit.
Methoden
Die Studie basiert auf einer als Pilotstudie konzipierten retrospektiven kontrollierten klinischen Studie, einer In-vitro-Untersuchung der materialabhängigen Biofilmbildung und einer Analyse der Biofilmbildung nach intraoraler Inkubation. Einundsechzig Patienten mit abgeschlossener festsitzender kieferorthopädischer Behandlung und einer Retentionsphase von mindestens 6 Monaten mit Twist-Flex-Retainern (Gruppe 1, n = 31) oder CAD/CAM-Nitinol-Retainern (Gruppe 2, n = 30) wurden hinsichtlich Plaqueindex (PI), Zahnfleischindex (GI), Sondierungstiefen, Blutungen bei Sondierung (BOP) und marginalen Rezessionen (MR) untersucht. Die materialabhängige Biofilmbildung bei Twist-Flex-, unbehandelten Nitinol- und elektropolierten Nitinol-Drahtproben wurde erstens in vitro beurteilt, unter Verwendung der optischen Dichte (OD) und Messung von jeweils 10 Proben, zweitens in vivo, unter Verwendung einer histomorphometrischen Analyse von jeweils 18 Proben.
Ergebnisse
Patienten, die mit Nitinol-Retainern behandelt wurden, hatten signifikant bessere Mundgesundheitsindizes (PI1 = 1,29 ± 0,06, PI2 = 0,94 ± 0,06; GI1 = 0,71 ± 0,05, GI2 = 0,56 ± 0,04; BOP1 = 0,11 ± 0,01, BOP2 = 0,08 ± 0,01; PD1 = 1,79 ± 0,03 mm, PD2 = 1,59 ± 0,04 mm) mit Ausnahme von MR (0,08 ± 0,03 vs. 0,08 ± 0,02 mm) im Vergleich zu mit Twist-Flex-Retainern behandelten. Nach 24 h intraoraler Inkubation zeigten Nitinol-Retainer im Vergleich zu Twist-Flex-Retainern eine deutlich geringere Biofilmbildung. In der In-vitro-Untersuchung wurden die vorübergehenden signifikanten Unterschiede zwischen den Gruppen am Ende kompensiert.
Schlussfolgerungen
Auf Grundlage der Ergebnisse kann davon ausgegangen werden, dass linguale CAD/CAM-Nitinol-Retainer einen positiven Effekt auf die Mundgesundheit haben.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
After orthodontic treatment removable or fixed retention appliances are commonly used to stabilise the treatment result [1, 2]. Over time, various retention systems have been developed and are commercially available for short-term and long-term use [1, 3,4,5,6]. Since Zacchrisson fixed flexible spiral wire lingual retainers are considered the gold standard (method of first choice) in the post orthodontic retention phase [7,8,9].
Irrespective of the anticipated benefits regarding tooth stabilization, aesthetic appearance and independency from patient’s compliance fixed lingual retainers can cause side effects, for instance caries and periodontal reactions due to the limited oral hygiene [10,11,12,13,14,15,16,17,18]. Animal and in vivo studies have shown that fixed lingual retainers can have a negative impact on periodontal health and lead to an increased incidence of gingival recessions, increased plaque accumulation, and increased bleeding [11, 18, 19]. In recent years, however, unexpected complications like tooth movement, torque changes and inclinations have also been described during orthodontic retention with fixed lingual retainers [7, 8, 20,21,22,23,24].
Altogether, there are only a limited number of studies examining the effect of different retainer regimes, particularly fixed lingual retainers on oral health and the quality of evidence is very low [1, 25].
Against the background of permanent retention and increasing requirements regarding biocompatibility, function, aesthetics and oral health, digitally designed nitinol-made lingual retainers using CAD/CAM technology seem to be a promising and innovative approach [7, 26, 27]. They show a high precision and positioning accuracy, a fact that might reduce unwanted tooth movements [27]. In addition, they have an electropolished surface which could minimise bacterial adhesion and plaque formation.
To date, there has been no study investigating the effects of a nitinol-made computer-aided design/computer-aided manufacturing (CAD/CAM) developed lingual retainer on oral health. Therefore, the first aim of this study was to compare the impact of fixed CAD/CAM nitinol retainers on oral health parameters with patients treated by conventional flexible spiral wire twistflex retainers. The second aim was the investigation if there were retainer material-dependent differences regarding the amount of biofilm formation. The working hypothesis was that using a nitinol-made CAD/CAM developed lingual retainer has a positive effect on oral health with less biofilm formation.
Materials and methods
Trial design
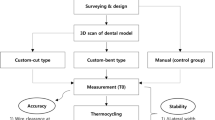
This study consisted of three parts: The first part was a retrospective controlled clinical study which was intended to function as a pilot study; the second part an in vitro investigation of the possible retainer material-dependent biofilm formation and the last part included an analysis of the intraoral biofilm formation after 24 h in vivo incubation.
The Ethics Committee of University of Aachen approved this study. The study was conducted with informed consent of all patients and in full accordance with the ethical requirements of the World Medical Association Declaration of Helsinki (2008).
Retrospective controlled clinical study—participants
All patients attending the Department of Orthodontics at University Aachen in Germany for routine orthodontic examinations between September 2014 and June 2015 were assessed for eligibility. Since this study was designed as a retrospective pilot investigation no sample size calculation was performed. The inclusion criteria were provision of written consent, completed fixed orthodontic treatment with 0.022 × 0.028 inch edgewise appliance, current wearing of a six-point fixed lingual retainer (flexible spiral wire 0.0175 inch stainless steel twistflex or 0.14 × 0.14 inch CAD/CAM nitinol wire, Fig. 1) for at least 6 months and treatment by the same orthodontist. Exclusion criteria were lack of written consent; retention phase below 6 months, broken or damaged retainers and retainers with broken bonding pads, as well as the use of another treatment or retainer protocol.
Six-point fixed lingual retainers: a flexible spiral wire 0.0175 inch stainless steel twistflex wire, b 0.014 × 0.014 inch computer-aided design/computer-aided manufacturing (CAD/CAM)-fabricated nitinol wire
Festsitzende Lingualretainer: a Twist-Flex-Retainer, gefertigt aus einem runden verseilten Stahldraht (0,0175 ’’), b CAD/CAM(„computer-aided design/computer-aided manufacturing“)-gefertigter Retainer aus einem Vierkant-Nitinol-Draht (0,014 × 0,014 ’’)
Sixty one patients aged 22 to 56 years met the inclusion criteria. They were assigned to two groups: group 1 (n = 31) treated with twistflex retainers served as control and group 2 (n = 30) used the novel CAD/CAM electropolished nitinol retainers. No incentives were offered.
Clinical examinations and oral health parameters
Examinations were conducted using a dental light, mirror and a pressure-calibrated periodontal probe (Dentsply Ash Instruments, UK). No radiographs were taken. All measurements were rechecked for accuracy.
The following oral health parameters were recorded:
-
1.
Plaque index (PI), as developed by Löe [28] and described by Pandis et al. [29]. Plaque accumulation was scored on the mesial, distal, buccal and lingual surfaces for each mandibular incisor and canine and categorised (0: absence of plaque, 1: plaque on the probe, 2: visible plaque, 3: abundant plaque). The results of the PI were averaged for each tooth and a mean value was estimated resulting in three categories: 0.1–1: slight plaque accumulation; 1.1–2: moderate plaque accumulation and 2.1–3: severe plaque accumulation.
-
2.
Gingival index (GI), as developed by Löe [28] and described by Al-Nimri et al. [14]: Gingival inflammation was scored on the mesial, distal, buccal and lingual surfaces for each mandibular incisor and canine and categorised (0: absence of inflammation, 1: mild inflammation (slight change in colour and texture, no bleeding on probing), 2: moderate inflammation (glazing, redness, oedema, hypertrophy, bleeding on probing), 3: severe inflammation (marked redness, hypertrophy, tendency toward spontaneous bleeding)). The results of the GI were averaged for each tooth and a mean value was estimated resulting in three categories: 0.1–1: mild inflammation; 1.1–2: moderate inflammation and 2.1–3: severe inflammation of the gingiva.
-
3.
Bleeding on probing (BOP), was scored according to Ainamo and Bay [30] with a pressure-calibrated probe (Dentsply Ash Instruments, UK) on six sides of each mandibular incisor and canine (mesio-lingual, mesio-buccal, lingual, buccal, disto-lingual, disto-buccal) and categorised in Code 1, if bleeding occurred and Code 0, in the absence of bleeding.
-
4.
Probing depth (PD) was measured in millimetres with a pressure-calibrated probe (Dentsply Ash Instruments, UK) on six sides of each mandibular incisor and canine (mesio-lingual, mesio-buccal, lingual, buccal, disto-lingual, disto-buccal) as distance from the gingival margin to the most apical part of the sulcus. The results of the PD were averaged for each tooth and a mean value was estimated.
-
5.
Marginal recessions (MR) were measured in millimetres on two sides of each mandibular incisor and canine (lingual, buccal) using a periodontal probe as distance from the dental-enamel junction to the gingival margin. The results of the MR were averaged for each tooth and a mean value was estimated.
Patients were examined by one orthodontist who had received special calibration training following WHO guidelines [31]. The examiner first practiced the examination on a group of 10 subjects. Afterwards, the orthodontist examined a group of 20 preselected subjects to assess the consistency. All measurements were rechecked for accuracy. The intraclass correlation coefficients for intraobserver agreement regarding the measurements of PI, GI, BOP, PD and MR were 0.83–0.89.
In vitro biofilm formation
An in vitro approach was used to determine the possible retainer material-dependent differences in biofilm formation. For this purpose, 10 samples of each of a twistflex, an untreated nitinol and an electropolished nitinol wire (length 1.5 cm) were incubated in 1 ml of human saliva at 37 °C for 24 h. Afterwards, each sample was transferred under sterile conditions into test tubes containing 5 ml broth (Brain Heart Infusion, Oxoid Ltd., UK) and further incubated at 37 °C in a shaking water bath to simulate the oral environment. Brain Heart Infusion Nutrient Broth (BHI) was used as negative control.
After 0 h (T0), 1 h (T1), 2 h (T2), 3 (T3), 4 (T4), 5 (T5), 6 (T6), 7 (T7), 8 (T8), 10 (T9) and 24 h (T10) the optical density (OD) was measured in a photometer (Biowave WPA CO8000, Biochrom, UK) at a wavelength of 600 nm. The results of the OD were averaged for each measurement time and each sample and mean values were estimated. The determination of the OD allowed an evaluation of the material-dependent biofilm formation. More biofilm formation was associated with a higher density.
Analysis of biofilm formation after intraoral incubation
For the last part of the study nine subjects were selected from a larger pool of patients treated at the Department of Orthodontics at University Aachen in Germany, using the following inclusion criteria: provision of written consent, at the present time no dental treatment need and performance of good oral hygiene.
For the analysis of the retainer-dependent intraoral biofilm formation individual removable maxillary appliances with integrated samples of a twistflex, an untreated nitinol and an electropolished nitinol wire (length 1.8 cm, two of each per subject, 54 samples in total) were produced (Fig. 2). Participants were instructed to wear the appliances for a period of 24 h without the performance of any oral hygiene measure.
Individual removable maxillary appliance with integrated samples of a twistflex, an untreated nitinol and an electropolished nitinol wire (length 1.8 cm, two of each per subject)
Individualisierte herausnehmbare Oberkieferapparatur mit integrierten Proben von Twist-Flex-, unbehandelten und elektropolierten Nitinol-Drähten (Länge je 1,8 cm, je 2 Drähte jeder Sorte)
Subsequently, the test wires were removed, applied to BHI agar plates (Brain Heart Infusion Agar, Oxoid Ltd., UK) and incubated at 37 °C. After 0 h (T0), 2 h (T1), 4 (T2), 6 (T3), 8 (T4), 10 (T5), 12 (T6), 16 (T7) and 24 h (T8) digital photos (Nikon, model D5200, Japan) with a constant focus-object distance of 40 cm were taken. Image procession was conducted using the software Photoshop 7.0 (Adobe Inc., San Jose, CA, USA).
For the digital evaluation of biofilm formation each individual wire sample was digitally cut out of the image area to a uniform size of 4.00 cm × 2.00 cm and a histomorphometric analysis of the bacterial colonised areas along the material samples was assessed with the microscope software AxioVision Release 4.8.2 (Zeiss, Germany). Based on the pixel-brightness ratio bacterial colonization was visualised with a red colour for assessment of bacterial amount in percent.
Statistical analysis
Data was statistically analysed in GraphPad Prism 7 (San Diego, CA, USA). Comparisons of the different variables between the groups were conducted using the unpaired t‑test (Figs. 3 and 5) and 2‑way analysis of variance (ANOVA; Fig. 4). A p-value ≤0.05 was used to indicate statistically significant differences.
Oral health parameters a plaque index (PI) and gingival index (GI), b bleeding on probing index (BOP), c probing depth (PD) and marginal recession (MR) of the twistflex retainer group (1) and CAD/CAM nitinol retainer group (2). ***p ≤ 0.001; *p ≤ 0.05
Mundgesundheitsbezogene Parameter a Plaque- (PI) und Gingivaindex (GI), b Blutung auf Sondierung (BOP), c Sondierungstiefe (PD) und Rezessionen (MR) der Twist-Flex- (1) und der CAD/CAM-Nitinol-Gruppe (2). Statistische Signifikanzen markiert *** p ≤ 0,001; * p ≤ 0,05
Optical density of a twistflex, an untreated nitinol and an electropolished nitinol wire after 0 h (T0), 1 h (T1), 2 h (T2), 3 (T3), 4 (T4), 5 (T5), 6 (T6), 7 (T7), 8 (T8), 10 (T9) and 24 h (T10). Statistically significant differences are marked with * twistflex versus untreated nitinol, # untreated nitinol versus electropolished nitinol. p ≤ 0.05
Optische Dichte (OD) gemessen an Proben eines Twist-Flex-, eines unbehandelten und eines elektropolierten Nitinol-Drahtes nach 0 h (T0), 1 h (T1), 2 h (T2), 3 h (T3), 4 h (T4), 5 h (T5), 6 h (T6), 7 h (T7), 8 h (T8), 10 h (T9) and 24 h (T10). Statistische Signifikanzen markiert mit * Twist-Flex- vs. unbehandelter Nitinol-Draht, # unbehandelter vs. elektropolierter Nitinol-Draht, p ≤ 0,05
Histomorphometric analysis of biofilm formation of a twistflex, an untreated nitinol and an electropolished nitinol wire after 0 h (T0), 2 h (T1), 4 (T2), 6 (T3), 8 (T4), 10 (T5), 12 (T6), 16 (T7) and 24 h (T8). Statistically significant differences are marked with * twistflex versus untreated nitinol, ÷ twistflex versus electropolished nitinol. p ≤ 0.05
Histomorphometrische Analyse der Biofilmformation auf Proben eines Twist-Flex-, eines unbehandelten und eines elektropolierten Nitinol-Drahtes nach 0 h (T0), 2 h (T1), 4 (T2), 6 (T3), 8 (T4), 10 (T5), 12 (T6), 16 (T7) und 24 h (T8). Statistische Signifikanzen markiert mit * Twist-Flex- vs. unbehandelter Nitinol-Draht, ÷ Twist-Flex- vs. elektropolierter Nitinol-Draht, p ≤ 0.05
Results
Clinical examinations and oral health parameters
For the first part of the study a total of 61 patients aged 22 to 56 years with an average retainer wearing time of 7.2 ± 0.8 months were assigned to two groups: 31 subjects in group 1 (twistflex retainer) and 30 in group 2 (CAD/CAM nitinol retainer). Fig. 3 illustrates the results regarding the oral health parameters plaque index (PI), gingival index (GI), bleeding on probing (BOP), probing depth (PD) and marginal recession (MR). Group 1 showed higher values compared to group 2 regarding mean PI (1.29 ± 0.06. versus 0.94 ± 0.06), mean GI (0.71 ± 0.05 versus 0.56 ± 0.04), mean BOP (0.11 ± 0.01 versus 0.08 ± 0.01) and mean PD (1.79 ± 0.03 mm versus 1.59 ± 0.04 mm). These differences were statistically significant (p ≤ 0.05). The difference between the two groups regarding mean MR was not statistically significant (MR 0.08 ± 0.03 mm versus 0.08 ± 0.02 mm; p > 0.05).
In vitro biofilm formation
To determine the possible retainer material-dependent differences in biofilm formation the optical density (OD) of a total of 30 samples of each of a twistflex, an untreated nitinol and an electropolished nitinol wire was assessed. Fig. 4 presents a comparison of the OD between all three groups at all measuring times (T0–T10). With increasing measuring time a higher bacterial growth could be investigated in all groups. Statistically significant differences were observed at the time point T8 between twistflex and untreated as well as untreated and electropolished nitinol wire samples in favour of the electropolished wire. Due to the bacterial growths there were no significant differences regarding OD in the first days of observation. After day 8 bacteria entered the stationary phase that is why no significant differences were detected either.
Analysis of biofilm formation after intraoral incubation
For the determination of the retainer-dependent intraoral biofilm formation a total of 54 samples of a twistflex, an untreated nitinol and an electropolished nitinol wire were examined. Fig. 5 presents the histomorphometric analysis of the biofilm area of all wire samples. With increasing measuring time a higher biofilm formation could be investigated in all groups, with a statistically significant increase in the twistflex group after 24 h (T8). The differences regarding bacterial colonization between the twistflex group and the untreated and electropolished nitinol wire group at time point T8 were statistically significant (twistflex 5.92 ± 3.93%; untreated nitinol 3.20 ± 2.07% and electropolished nitinol 3.07 ± 1.76%; p ≤ 0.05) in favour of the electropolished wire.
Discussion
This study evaluated the impact of a novel computer-fabricated lingual nitinol retainer compared to a conventional lingual flexible spiral wire on oral health. Patients treated with nitinol retainers had significant better oral health indices (plaque index, gingival index, bleeding on probing, probing depth) except for marginal recession compared to twistflex retainers. In addition, the twistflex retainer results revealed that there were material-dependent differences regarding the amount of biofilm formation. After 24 h intraoral incubation nitinol retainers demonstrated significant less biofilm formation compared to twistflex retainers. In the in vitro investigation the temporary significant differences between the groups were compensated in the end, indicating that in vitro results cannot be transferred in full to in vivo outcomes. Although a tendency to an increased bacterial adhesion and growth on the retainer material was foreseeable.
Fixed lingual retainers are associated with increased plaque accumulation, gingival inflammatory signs and gingival recession, even though the quality of evidence is low with partly contradictory studies [1, 13, 16, 18, 19, 29, 32,33,34]. In the present study all patients treated with lingual retainers showed impairments of their oral health parameters—though less in the nitinol retainer group than in the twistflex group. Clinical parameters were increased indicating that retainers can cause gingival inflammation. Probing depth increase and bleeding tendency are signs of tissue irritation and are associated with the development of periodontal disease and attachment loss [35,36,37]. In case of gingival recessions, only a very low incidence and amount could be detected in the present study with no significant differences between the groups. The development of marginal recessions is a multifactorial process that can occur during and after orthodontic treatment [29, 38]. Gingival biotype, plaque accumulation, inflammatory signs and orthodontic treatment and retention time can be predisposing factors [29, 39]. The present study included patients wearing fixed lingual retainers for at least 6 months, maybe the retention period was too short to cause gingival recessions. All things considered, the in vivo results clearly indicated that patients wearing CAD/CAM nitinol retainers had significant lower plaque, gingiva and inflammatory indices and showed less biofilm formation than patients with twistflex retainers. Although the measured differences were small they were of significant amount. The values are comparable to a recent review analyzing the effects of fixed appliances on periodontal health [40]. The clinical relevance of these differences needs to be addressed in further studies.
For the differences between the groups several factors can be responsible, for instance the influence of material characteristics, surface properties, attachment and wire stranding [14, 17, 18, 41, 42]. The present study suggests that multistranded wires promote biofilm formation and confirms the results of another study [14]. Smooth and polished surfaces seem to complicate the bacterial adhesion process [18, 42]. In our study electropolished nitinol retainers showed less biofilm formation compared to the flexible spiral wire stainless steel twistflex retainer in both in vivo investigations. It can be assumed that the material and design of the CAD/CAM fabricated nitinol retainer were responsible for the differences.
Nitinol is a nickel-titanium alloy, which includes the advantages of the material titanium regarding formation of a stable passive layer, absence of corrosion and no potentially toxic and allergenic stimuli [43,44,45]. The 3D modeling software during the manufacturing process allows a high precision and positioning accuracy of the lingual retainer with less plaque retention sites [27]. Electropolishing, a surface refinement, results in an additional improvement of the material properties [46]. Highly polished surfaces and custom-made bonding pads are recommended to avoid plaque and calculus accumulation [10, 18, 47].
To our knowledge, this was the first study investigating the impact of a nitinol-made CAD/CAM developed lingual retainer on oral health. The study results were based on a retrospective case-control study, an in vitro investigation of material-dependent biofilm formation and an analysis of biofilm formation after intraoral incubation. All patients treated with lingual retainers showed impairments of their oral health parameters—though less in the nitinol retainer group than in the twistflex group. Patients wearing CAD/CAM nitinol retainers had significant lower plaque and gingiva indices than patients with twistflex retainers. In addition, the results revealed that there were material-dependent differences regarding the amount of biofilm formation. Despite complexity of the study the findings of this investigation should be interpreted with caution. Outcomes are based on patients wearing fixed lingual retainers for at least 6 months due to the recent development of this CAD/CAM nitinol retainer and can be regarded as short-term retention findings.
Since the study was designed as a retrospective controlled clinical study with pilot character, no sample size calculation was performed. Nevertheless, the results of this study can serve as a basis for further prospective research in order to enable reliable assessments about the impact of fixed lingual retainers on oral health of patients with long-term retention.
Conclusion
This study evaluated the impact of a novel computer-fabricated lingual nitinol retainer compared to a conventional lingual flexible spiral wire twistflex retainer on oral health. Based on the results it can be assumed that nitinol-made CAD/CAM developed lingual retainers have a positive effect on oral health. Further clinical studies are needed to assess the long-term effects of lingual nitinol retainers and for generalizability of the study results.
References
Littlewood SJ, Millett DT, Doubleday B et al (2016) Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst Rev 1:CD2283. https://doi.org/10.1002/14651858.CD002283.pub4
Padmos JAD, Fudalej PS, Renkema AM (2018) Epidemiologic study of orthodontic retention procedures. Am J Orthod Dentofacial Orthop 153:496–504. https://doi.org/10.1016/j.ajodo.2017.08.013
Wu HM, Zhang JJ, Pan J, Chen D (2014) Clinical evaluation of glass fiber-reinforced composites for fixed orthodontic lingual retainers. Shanghai Kou Qiang Yi Xue 23:80–82
Xu XC, Li RM, Tang GH (2011) Clinical evaluation of lingual fixed retainer combined with Hawley retainer and vacuum-formed retainer. Shanghai Kou Qiang Yi Xue 20(6):623–626
Uzdil F, Kayalioglu M, Kendi E, Toroglu MS (2010) A new type of modified Essix retainer for anterior open bite retention. Prog Orthod 11:45–52
Amundsen OC, Wisth PJ (2005) Clinical pearl: LingLockTM—the flossable fixed retainer. J Orthod 32:241–243. https://doi.org/10.1179/146531205225021195
Renkema AM, Renkema A, Bronkhorst E, Katsaros C (2011) Long-term effectiveness of canine-to-canine bonded flexible spiral wire lingual retainers. Am J Orthod Dentofacial Orthop 139:614–621. https://doi.org/10.1016/j.ajodo.2009.06.041
Katsaros C, Livas C, Renkema AM (2007) Unexpected complications of bonded mandibular lingual retainers. Am J Orthod Dentofacial Orthop 132:838–841. https://doi.org/10.1016/j.ajodo.2007.07.011
Zachrisson BU (1977) Clinical experience with direct-bonded orthodontic retainers. Am J Orthod Dentofacial Orthop 71:440–448
Corbett AI, Leggitt VL, Angelov N et al (2015) Periodontal health of anterior teeth with two types of fixed retainers. Angle Orthod 85:699–705. https://doi.org/10.2319/060314-398.1
Torkan S, Oshagh M, Khojastepour L et al (2014) Clinical and radiographic comparison of the effects of two types of fixed retainers on periodontium—a randomized clinical trial. Prog Orthod 15:1–7. https://doi.org/10.1186/s40510-014-0047-8
Lukiantchuki MA, Hayacibara RM, Ramos AL (2011) Comparison of periodontal parameters after the use of orthodontic multi-stranded wire retainers and modified retainers. Dental Press J Orthod 16:44.e1–44.e7. https://doi.org/10.1590/S1415-54192007000100007
César Neto JB, Simoés Regio MR, Martos J et al (2010) Analysis of the periodontal status of patients with mandibular-bonded retainers. Rev Odonto Ciênc 25(2):132–136. https://doi.org/10.1590/S1980-65232010000200005
Al-Nimri K, Al Habashneh R, Obeidat M (2009) Gingival health and relapse tendency: A prospective study of two types of lower fixed retainers. Aust Orthod J 25:142–146
Shirasu BK, Hayacibara RM, Ramos AL (2007) Comparação de parâmetros periodontais após utilização de contenção convencional 3x3 plana e contenção modificada. Rev Dent Press Ortodon Ortop Facial 12(1):41–47. https://doi.org/10.1590/S1415-54192007000100007
Heier EE, De Smit AA, Wijgaerts IA, Adriaens PA (1997) Periodontal implications of bonded versus removable retainers. Am J Orthod Dentofacial Orthop 112:607–616. https://doi.org/10.1016/S0889-5406(97)70225-7
Artun J, Spadafora AT, Shapiro PA et al (1987) Hygiene status associated with different types of bonded, orthodontic canine-to-canine retainers: A clinical trial. J Clin Periodontol 14:89–94. https://doi.org/10.1111/j.1600-051X.1987.tb00948.x
Artun J (1984) Caries and peridontal reactions associated with long-term use of different types of lingual retainers. Am J Orthod Dentofacial Orthop 86:112–118
Levin L, Samorodnitzky-Naveh GR, Machtei EE (2008) The association of orthodontic treatment and fixed retainers with gingival health. J Periodontol 79:2087–2092. https://doi.org/10.1902/jop.2008.080128
Kučera J, Marek I (2016) Unexpected complications associated with mandibular fixed retainers: A retrospective study. Am J Orthod Dentofacial Orthop 149:202–211. https://doi.org/10.1016/j.ajodo.2015.07.035
Pazera P, Fudalej P, Katsaros C (2012) Severe complication of a bonded mandibular lingual retainer. Am J Orthod Dentofacial Orthop 142:406–409. https://doi.org/10.1016/j.ajodo.2012.01.019
Yitschaky O, Yitschaky M, Sagi HK (2012) Orthodontic fixed retainer: Fix or not fix? That is the question. Refuat Hapeh Vehashinayim 29:29–36
Sifakakis I, Pandis N, Eliades T et al (2011) In-vitro assessment of the forces generated by lingual fixed retainers. Am J Orthod Dentofacial Orthop 139:44–48. https://doi.org/10.1016/j.ajodo.2010.02.029
Dahl EH, Zachrisson BU (1991) Long-term experience with direct-bonded lingual retainers. J Clin Orthod 25:728–737
Westerlund A, Daxberg E‑L, Liljegren A et al (2014) Stability and side effects of orthodontic retainers—A systematic review. Dentistry 4:1–17. https://doi.org/10.4172/2161-1122.1000258
Kravitz ND, Grauer D, Schumacher P, Jo Y (2017) Memotain: A CAD/CAM nickel-titanium lingual retainer. Am J Orthod Dentofacial Orthop 151:812–815. https://doi.org/10.1016/j.ajodo.2016.11.021
Wolf M, Schumacher P, Jäger F et al (2015) Novel lingual retainer created using CAD/CAM technology: Evaluation of its positioning accuracy. J Orofac Orthop 76:164–174. https://doi.org/10.1007/s00056-014-0279-8
Löe H (1967) The Gingival Index, the Plaque Index and the Retention Index Systems. J Periodontol 38:610–616. https://doi.org/10.1902/jop.1967.38.6.610
Pandis N, Vlahopoulos K, Madianos P, Eliades T (2007) Long-term periodontal status of patients with mandibular lingual fixed retention. Eur J Orthod 29:471–476. https://doi.org/10.1093/ejo/cjm042
Ainamo J, Bay I (1975) Problems and proposals for recording gingivitis and plaque. Int Dent J 25:229–235
World Health Organization (2013) Oral health surveys: Basic methods, 5th edn. WHO, Genf
Dietrich P, Patcas R, Pandis N, Eliades T (2015) Long-term follow-up of maxillary fixed retention: Survival rate and periodontal health. Eur J Orthod 37:37–42. https://doi.org/10.1093/ejo/cju001
Rody WJ, Akhlaghi H, Akyalcin S et al (2011) Impact of orthodontic retainers on periodontal health status assessed by biomarkers in gingival crevicular fluid. Angle Orthod 81:1083–1089. https://doi.org/10.2319/011011-15.1
Störmann I, Ehmer U (2002) A prospective randomized study of different retainer types. J Orofac Orthop 63:42–50. https://doi.org/10.1007/s00056-002-0040-6
Chapple ILC, Mealey BL, Van Dyke TE et al (2018) Periodontal health and gingival diseases and conditions on an intact and a reduced periodontium: Consensus report of workgroup 1 of the 2017 World Workshop on the Classification of Periodontal and Peri-Implant Diseases and Conditions. J Periodontol 89:S74–S84. https://doi.org/10.1111/jcpe.12957
Lang NP, Adler R, Joss A, Nyman S (1990) Absence of bleeding on probing. An indicator of periodontal stability. J Clin Periodontol 17:714–721. https://doi.org/10.1111/j.1600-051X.1990.tb01059.x
Lang NP, Joss A, Orsanic T et al (1986) Bleeding on probing. A predictor for the progression of periodontal disease? J Clin Periodontol 13:590–596. https://doi.org/10.1111/j.1600-051X.1986.tb00852.x
Kassab MM, Cohen RE (2003) The etiology and prevalence of gingival recession. J Am Dent Assoc 134:220–225. https://doi.org/10.14219/jada.archive.2003.0137
Melsen B, Allais D (2005) Factors of importance for the development of dehiscences during labial movement of mandibular incisors: A retrospective study of adult orthodontic patients. Am J Orthod Dentofacial Orthop 127:552–561. https://doi.org/10.1016/j.ajodo.2003.12.026
Cerroni S, Pasquantonio G, Condò R, Cerroni L (2018) Orthodontic fixed appliance and periodontal status: An updated systematic review. Open Dent J 12:614–622. https://doi.org/10.2174/1745017901814010614
Artun J, Spadafora AT, Shapiro PA (1997) A 3‑year follow-up study of various types of orthodontic canine-to-canine retainers. Eur J Orthod 19:501–509. https://doi.org/10.1093/ejo/19.5.501
Drescher D, Bourauel C, Schumacher HA (1989) Frictional forces between bracket and arch wire. Am J Orthod Dentofacial Orthop 96:397–404. https://doi.org/10.1016/0889-5406(89)90324-7
Pérez LM, Gracia-Villa L, Puértolas JA et al (2009) Effect of nitinol surface treatments on its physico-chemical properties. J Biomed Mater Res Part B Appl Biomater 91:337–347. https://doi.org/10.1002/jbm.b.31407
Clinard K, Von Fraunhofer JA, Kuftinec MM (1981) The corrosion susceptibility of modern orthodontic spring wires. J Dent Res 60A:1277
Edie JW, Andreasen GF, Zaytoun MP (1981) Surface corrosion of nickel and stainless steel under clinical conditions. Angle Orthod 51:319–324
Anderson ME, Price JWH, Parashos P (2007) Fracture resistance of electropolished rotary nickel–titanium endodontic instruments. J Endod 33:1212–1216
Gorelick L, Geiger AM, John A (1982) Incidence of white spot formation after bonding and banding. Am J Orthod Dentofacial Orthop 81:93–98
Acknowledgements
The authors thank the German Association of Orthodontics (DGKFO) for financial support. The authors thank Pascal Schumacher for CAD/CAM material support. The authors also thank C. Kirschneck and P. Proff (University of Regensburg, Department of Orthodontics) for improving data presentation and interpretation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
I. Knaup, Y. Wagner, J. Wego, U. Fritz, A. Jäger and M. Wolf declare that they have no competing interests.
Ethical standards
The Ethics Committee of University of Aachen approved this study. All procedures performed in the study involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments. Informed consent was obtained from all individual participants included in the study.
Additional information
I. Knaup and Y. Wagner contributed equally to this manuscript.
Rights and permissions
About this article
Cite this article
Knaup, I., Wagner, Y., Wego, J. et al. Potential impact of lingual retainers on oral health: comparison between conventional twistflex retainers and CAD/CAM fabricated nitinol retainers. J Orofac Orthop 80, 88–96 (2019). https://doi.org/10.1007/s00056-019-00169-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00056-019-00169-7