Abstract
Imidazole and benzimidazole rings are the most important nitrogen-containing heterocycles, which are widely explored and utilized by the pharmaceutical industry for drug discovery. Due to their special structural features and electron-rich environment, imidazole- and benzimidazole-containing drugs bind to a variety of therapeutic targets, thereby exhibiting a broad spectrum of bioactivities. Numerous imidazole- and benzimidazole-based drugs have been extensively used in the clinic to treat various types of diseases with high therapeutic potential. Due to their enormous medicinal value, the research and development of imidazole- and benzimidazole-containing drugs is an increasingly active and attractive topic of medicinal chemistry. This review enlightens the landscape of the discovery and development of imidazole- and benzimidazole-based drugs with an emphasis on structure activity relationship features (SAR), medicinal chemistry, and their mechanism of action. Furthermore, the present review also provides the recent advances in the development of imidazole- and benzimidazole-based drugs along with new perspectives. We hope that this paper will open up new opportunities for researchers to design future generation novel and potent imidazole- and benzimidazole-containing drugs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heterocyclic compounds occupy a central position in medicinal chemistry and are of particular interest and significant importance in the search for new bioactive molecules in the pharmaceutical industry (Gaba et al., 2014). The nitrogen-containing heterocycles, in particular, exhibit diverse range of biological activities due in part to their similarities with many natural and synthetic molecules with known biological activities (DeSimone et al., 2004). The imidazole and benzimidazole rings have been commonly used as privileged scaffolds for the development of therapeutic molecules of pharmaceutical or biological interest. Imidazole is a five-membered aromatic heterocycle widely present in the important biological building blocks, such as amino acid histidine (a normal constituent of most proteins), histamine, purines, and biotin (Fei and Zhou, 2013), whereas benzimidazole is a six-membered bicyclic heteroaromatic compound in which benzene ring is fused to the 4- and 5-positions of imidazole ring. In 1872, Hoebrecker reported the first benzimidazole synthesis of 2,5- and 2,6-dimethylbenzimidazole by ring-closure reaction of benzene-1,2-diamine derivatives (Wright, 1951) and more interest in the area of benzimidazole-based chemistry was developed in the 1950s, when 5,6-dimethyl-1-(α-D-ribofuranosyl)benzimidazole was found as an integral part of the structure of vitamin B12 (Barker et al., 1960). Moreover in 1882, Radziszewski reported the first synthesis of highly substituted imidazoles by condensing 1,2-diketones with different aldehydes in the presence of ammonia (Radziszewski, 1882). Afterward, the related research and drug discovery in this class of compounds are rapidly developing and have achieved great progress.
Both, imidazole and benzimidazole rings contain two nitrogen atoms with amphoteric nature, i.e., possessing both acidic and basic characteristics. These rings exist in two equivalent tautomeric forms, in which the hydrogen atom can be located on either of the two nitrogen atoms (Fig. 1). Furthermore, the electron-rich nitrogen heterocycles could not only readily accept or donate protons, but also form diverse weak interactions easily. These special structural features of imidazole and benzimidazole rings with desirable electron-rich characteristic is beneficial for imidazole and benzimidazole derivatives to readily bind with a variety of therapeutic targets, thereby exhibiting broad pharmacological activities (Wright, 1951; Bhatnagar et al., 2011; Ingle and Magar, 2011; Gaba et al., 2010; Fig. 2). From the last decade, a diverse range of biological activities based on imidazole and benzimidazole derivatives has been reviewed by several authors (Narasimhan et al., 2011; Yadav and Ganguly, 2015; Gaba et al., 2015). Their ubiquitous properties and important role in different diseases has attracted special interest in imidazole- and benzimidazole-based medicinal chemistry. The work embodied in this article relates to the clinically useful imidazole as well as benzimidazole-containing drugs with their discovery and development. Moreover, the mechanism of action, SAR points as well as some opinions have been presented to help medicinal chemist and chemical biologist in designing invaluable novel drugs with imidazole and benzimidazole cores for the treatment of different disorders. It is anticipated that this review will be helpful for new thoughts in the quest for rational design of more active and potent drugs in future research.
Imidazole- and benzimidazole-based drugs in the service of humankind
The imidazole and benzimidazole scaffolds are extremely versatile and have featured a number of clinically used drugs such as antihistaminic, antiulcer, antihypertensive, antibacterial, antifungal, antiparasitic, antiemetic, anticancer, antiviral, and other therapeutic agents with high therapeutic potency and market value. Therefore, it is worthwhile to get insight into the discovery and development of imidazole- and benzimidazole-containing drugs along with their mechanism of action and SAR features for future endeavors.
Antihistaminic drugs
Histamine is an important chemical mediator and neurotransmitter that influences a variety of physiological and pathophysiological processes in the body via stimulation of a class of G protein-coupled histamine receptor subtypes, i.e., H1, H2, H3, and H4 (Hough, 2001). The biogenic amine, histamine, is known to participate in allergic and inflammatory reactions, gastric acid secretion, and immunomodulation, as well as in neurotransmission. Antihistaminic drugs or histamine receptor antagonists that were the first to be introduced are ones that bind at H1-receptor sites and block the action of histamine. They are therefore designated as H1-receptor antagonists and are used for the treatment of allergic conditions (Parsons and Ganellin, 2006). The benzimidazole-containing drugs, i.e., bilastine, astemizole, mizolastine, emedastine, and clemizole, are playing a vital role as H1-receptor antagonists (Fig. 3). Bilastine was developed by FAES Farma as a selective and potent antagonist at H1 receptor sites for the treatment of allergic rhinoconjunctivitis and urticaria (Corcostegui et al., 2005). Astemizole, a second-generation H1-receptor antagonist, was discovered in 1977 by Janssen Pharmaceutica. It was developed from a series of diphenylbutylpiperidine antihistamines in an effort to extend the duration of action. The piperidino-aminobenzimidazole moiety appears to be required for H1-receptor affinity and contributes significantly for persistent receptor binding that result in prolonged action. But it has been withdrawn from the market because of side effects like QT interval prolongation and arrhythmias (Zhou et al., 1999). Mizolastine, structurally resembling astemizole, is fast-acting non-sedating antihistaminic drug. It does not prevent the actual release of histamine from mast cells, just prevents it binding to receptors. It has not been shown to increase the QT interval and considered as an effective antihistaminic in the management of allergic rhinitis and chronic idiopathic urticarial (Prakash and Lamb, 1998). Emedastine is also a second-generation H1-receptor antagonist with high affinity and specificity for H1-receptors. It is used in the form of eye drops to treat allergic conjunctivitis (Bielory et al., 2005), whereas clemizole is first-generation antihistamine used to treat itching and allergic reactions.
Histamine has a physiological role in regulating the secretion of acid in the stomach, where it stimulates the parietal cells to produce hydrochloric acid. In the 1970s a new class of drugs was invented that blocked the action of histamine at its H2-receptors so-called as H2-receptor antagonists. These drugs were shown to be extremely effective in antagonizing the action of histamine on parietal cells (specifically H2-receptors) in the stomach and decrease the production of acid by these cells. The discovery of first H2-receptor antagonist, i.e., cimetidine is strongly associated with Sir James Black and coworkers. The scientists at GlaxoSmithKline initiated a program of systematic research of H2-receptor antagonists starting from the structure of histamine. The first breakthrough was the N α-guanylhistamine that possessed weak antagonistic activity against the gastric secretion induced by histamine. The lengthening of the side chain of this compound increased the H2-receptor antagonistic activity, but a residual agonist effect remained. Therefore, the basic guanidino group was replaced by a neutral thiourea that eventually led to the development of burimamide, a specific competitive antagonist of H2-receptor 100-times more potent than N α-guanylhistamine, proved the existence of the H2-receptor. But it was not suitable for progression to clinical trials because its antagonist activity was too low for oral administration. Further, modification of the structure of burimamide was done by inserting an electronegative atom, i.e., sulfur instead of the methylene group into the side chain and a methyl group at five-position on imidazole ring that obtained metiamide with enhanced H2-receptor antagonistic activity as compared to burimamide. Metiamide was an effective agent; however, it was associated with unacceptable nephrotoxicity and agranulocytosis. The toxicity was proposed to arise from the thiourea group, so further structure modification was carried out by replacing the thiourea group in metiamide with an N-cyanoguanidine group that led to the ultimate discovery of cimetidine with potent antagonistic activity (Scheinfeld, 2003; Fig. 4). Cimetidine is a prototypical H2-receptor antagonist, developed at GlaxoSmithKline by Black and coworkers, and has established new vistas for the effective treatment of gastric ulcers, heartburn, and gastritis (Black et al., 1972). It reached the clinic at the end of 1976, as the pioneer drug which revolutionized the medical treatment of peptic ulcer disease. Indeed, in many countries, it became the best-selling prescription medicine and was the first of the ‘‘blockbuster’’ products (billion dollar annual sales; Freston, 1982).
H3- and H4-receptors agonists/antagonists
In recent years, significant attention has been focused on the potential therapeutic use of drugs acting on H3- and H4-receptors (Bhatt et al., 2010; Geyer and Buschauer, 2011; Tiligada et al., 2009). The H3-receptor is mainly located on neurons, predominantly in the central nervous system (Leurs et al., 2005). At H3-receptor, histamine itself is a highly active agonist. Methylation of the α-carbon atom of histamine’s ethylamine side chain leads to R-α-methylhistamine, with a highly reduced activity at both the H1- and H2-receptors and potent agonist activity at the H3-receptor, whereas the addition of a methyl group to the aliphatic amine nitrogen of histamine resulted in non-selective H3-receptor agonist such as N-α-methylhistamine (Fig. 5). For potent H3-receptor agonism, the amine function of histamine can be incorporated in ring structure, e.g., immepip. Immepip and R-α-methylhistamine have been used as reference ligands to study the H3-receptor, both of them also have considerable activity for H4-receptor. Therefore, new potent and selective agonists have been developed, i.e., methimepip (N-methyl analog of immepip-containing piperidine), immethridine (pyridine congener of immepip), and imetit (isothiourea derivative) all retaining the imidazole ring of histamine (Arrang et al., 1988; Kitbunnadaj et al., 2004). Nevertheless, H3-receptor antagonists have received a major boost for the treatment of dementia, Alzheimer’s disease, narcolepsy, hyperactivity disorder or allergic rhinitis, and many more compounds from different companies have been under clinical investigation (Sander et al., 2008). Early potent H3-receptor antagonists, like cipralisant, thioperamide (analog of immepip), and clobenpropit (analog of imetit), iodophenpropit (Singh and Jadhav, 2013; Jansen et al., 1994; 2000), proxifan (Clapp and Luckman, 2012), and ciproxifan (Motawaj and Arrang, 2011) have been reported (Fig. 5). The recently described H4-receptor is mainly expressed in various cells of the immune system like eosinophils, T-lymphocytes, dendritic cells, mast cells, and basophils (Igel et al., 2010). Therefore, H4-receptor antagonists appear to have immunomodulatory role and are also being investigated as anti-inflammatory and analgesic drugs (Stark, 2003). Recently, 2,5-disubstituted benzimidazole derivative, i.e., JNJ 10191584 as a potent and selective H4-receptor antagonist has been reported as an anti-inflammatory analgesic agent (Coruzzi et al., 2007). Due to the structural similarity of H3- and H4-receptors, the H3-receptor- targeting drugs have also significant affinity for H4-receptor which is discussed in Fig. 5.
From SAR features, it is found that for histamine receptor antagonists, the imidazole, and benzimidazole rings are considered as essential elements required for receptor affinity (Yu et al., 2010). For H1-receptor antagonistic activity different substitutions are required on 1-, 2-position of benzimidazole scaffold. The 1-position should contain halogen substituted benzyl ring or alkyl ethers, whereas the 2-position should comprise aromatic rings and a basic nitrogen atom. The imidazole ring substituted with a C5 methyl group affords H2-receptor selectivity; a four-atom side chain, which includes one sulfur atom (the sulfur atom increases potency compared to carbon congeners); and a terminal polar nonbasic unit, i.e., an N-cyanoguanidine substituents is required for potent H2-receptor antagonistic activity. Guanidines substituted with electron-withdrawing groups, i.e., cyano group, have significantly decreased basicity compared to guanidine, and they are neutral or nonprotonated at physiological pH, thereby preserving the activity of the drug in a physiological environment that does not cause agranulocytosis (Fig. 4). Modulation at 5-position of the imidazole ring leads to histamine selective agonist action, whereas N-guanylhistamine as weak antagonists. It is also observed that various modifications have been done at 5-position of the imidazole ring to develop H3 as well as H4 receptor agonists as well as antagonists.
Antiulcer drugs
Gastric acid has been known to be a key factor in normal upper gastrointestinal functions, including protein digestion, iron or calcium absorption as well as provide some protection against bacterial infection. However, inappropriate level of acid underlies several pathological conditions, including gastroesophageal reflux disease (GERD), heartburn, and peptic ulcers (Olbe et al., 2003). Gastric damage or gastrointestinal toxicity represents an important medical and socioeconomic problem, which can be treated by blocking acid secretion through proton pump inhibitors (PPIs). These drugs have emerged as the treatment of choice for acid-related diseases, which act irreversibly by blocking the H+-K+-ATPase of the gastric parietal cells and thereby reducing the gastric acid secretion (Zajac et al., 2013).
The vast majority of these drugs are benzimidazole derivatives and their discovery as PPIs may be traced back to the 1968 when George Sachs and his collaborators described an H+-K+-ATPase as the proton pump that moves acid across the gastric mucosa and gastric parietal cells (Sachs et al., 1968; Blum et al., 1971; Chang et al., 1977; Sachs and Wallmark, 1989). Further, it was discovered that H+-K+-ATPase is the final step of gastric acid secretion, and blockade of this enzyme could lead to potent inhibitors of acid secretion irrespective of external or endogenous signals. This biochemical work was coincided with synthetic work by focusing on gastric acid inhibition. In the mid-1970s, the search for drugs that might to control acid secretion began by the Astra Pharmaceuticals. From the literature it is found that the 2-(pyridin-2-yl)ethanethioamide developed by the Servier exhibited antisecretory activity; this compound, however, showed toxicity due to thioamide group, and further research into this compound was cancelled (Fig. 6; Lindberg and Carlsson, 2006). In 1973, the work of James Black and colleagues suggested that substituted imidazole (e.g., cimetidine) is important to control acid by acting on H2-receptors (Brimblecombe et al., 1978). Therefore, based on the structure of cimetidine, a benzimidazole ring was added to 2-(pyridin-2-yl)ethanethioamide by the Astra group along with modification of the sulfide (2-(pyridin-2-ylmethylthio)-benzimidazole) to a sulfoxide that led to the introduction of 2-(2-pyridinylmethylsulfinyl)-benzimidazole (timoprazole) with a surprisingly high level of antisecretory activity (Fig. 6; Olbe et al., 2003; Shin et al., 2008). Later on, studies on timoprazole revealed an enlargement of the thyroid gland due to inhibition of iodine uptake as well as atrophy of the thymus gland, so it could not be used in humans. Moreover, it was found that some substituted mercapto-benzimidazoles have no effect on iodine uptake and the introduction of such substituents into timoprazole resulted in elimination of the toxic effects, without reducing the antisecretory effects (Lindberg and Carlsson, 2006). A variety of analogs of timoprazole were synthesized, and picoprazole was found to have antisecretory action without iodine blockage activity. SAR studies on analogs of picoprazole showed that electron-donating groups on the pyridine ring, which increased the pK a of the pyridine ring, also increased the potency as an inhibitor of H+-K+-ATPase (Fig. 7). As a result the best analog was omeprazole that is substituted with two methoxy groups, one at 6-position of the benzimidazole, other at 4-position of the pyridine, and two methyl groups at 3 and 5-positions of pyridine. It is the first PPI discovered by AstraZeneca in 1978 that controlled the acid secretion in the stomach also clinically superior than H2-receptor antagonists (Shin et al., 2008; Fellenius et al., 1981; Munson et al., 2005). In 1996, omeprazole became the world’s biggest ever selling pharmaceutical, and by 2004 over 800 million patients had been treated with this drug worldwide. After that a number of analogs of omeprazole were studied by pharmaceutical companies with different substitutions on benzimidazole as well as pyridine ring which led to the discovery of lansoprazole, pantoprazole, esomeprazole (i.e., S-enantiomer of omeprazole) and rabeprazole all claiming to share a flourishing market, after their development (Fig. 6; Shin et al., 2008; Sachs et al., 2007). Esomeprazole was discovered in 1987 by AstraZeneca having faster onset of antisecretory action and higher bioavailability than the R-enantiomer, i.e., omeprazole. It is used to treat peptic ulcers and GERD, which became one of the most widely prescribed drugs, with sales of about $5 billion in 2009 (Sachs et al., 2007). Lansoprazole was the second PPI discovered in 1984 by Takeda and reached in the market in 1991. It has no substitutions at the benzimidazole ring, but two substituents are present on the pyridine ring, i.e., a methyl group at 3-position and a trifluoroethoxy group at 4-position. Dexlansoprazole (R-enantiomer of lansoprazole) was launched as a follow up of lansoprazole in 2009. Moreover, both enantiomers have similar effects on the proton pump (Emerson and Marzella, 2010), whereas rabeprazole was discovered by Eisai Co. and it is similar to lansoprazole in having no substituents on its benzimidazole part, whereas a methyl group is present at 3-position of pyridine, and the only difference is the methoxypropoxy substitution at 4-position instead of the trifluoroethoxy group on lansoprazole. Pantoprazole was the third PPI introduced into the German market in 1994 that was discovered by Byk-Gulden. It has a difluoroalkoxy side group on the benzimidazole ring and two methoxy groups in 3- and 4-positions on the pyridine ring (Senn-Bilfinger and Sturm, 2006). Ilaprazole, a pyrrole-substituted benzimidazole, was synthesized at IL-Yang Pharmaceutical. Its antisecretory activity is proved to be two to three times higher and its half-life two to three times longer than that of omeprazole (Scarpignato and Hunt, 2008), whereas tenatoprazole, consisting of one imidazopyridine ring connected to a pyridine ring by a sulfinylmethyl chain, represents a new chemical entity developed by Mitsubishi Pharma in Japan and is now under active development by Sidem (France). The inhibitory activity of this novel compound on gastric H+-K+-ATPase has been thoroughly characterized (Fig. 6; Shin et al., 2008). Like other PPIs, tenatoprazole is a prodrug (pK a = 4.04), which is converted to the active sulfenamide or sulfenic acid in the acidic secretory canaliculus of the stimulated parietal cell.
Mechanism of action and chemistry behind PPIs
PPIs are mainly lipophilic prodrugs, which readily crosses the cell membrane into the parietal cells within the acidic environment. In an acid environment, the inactive drug is protonated and rearranges into its active form which covalently or irreversibly binds to the ATPase enzyme via disulfide bond, thereby inhibiting the gastric proton pump and prevents further release of H+ ions. One sulfur atom in the disulfide bond comes from a cysteine residue on ATPase enzyme, and another comes from the PPIs (Herling and Weidmann, 1994; Fig. 8). The PPIs currently on the market all contain the same 2-pyridylmethylsulfinyl benzimidazole as pharmacophore and differ only in the nature of substituents placed on both benzimidazole and pyridine rings. The sulfinyl moiety in the parent PPIs is not sufficiently reactive to form essential disulfide bond, so it must first be activated through protonation reaction in the highly acidic parietal cell followed by rearrangement to form active sulfenamide or sulfenic acid derivative.
The only two nitrogen atoms, i.e., the pyridine nitrogen and double-bonded benzimidazole nitrogen (N3) are capable of accepting proton. The tissue selectivity of PPIs is based on both their pH-dependent accumulation, as weak bases in the acidic compartment of the parietal cell, and acid-induced rearrangement of the parent compound to the pharmacologically active compounds (Kromer, 1995). The pK a of the pyridine nitrogen (pK a1) runs between 3.83 (lansoprazole and pantoprazole) and 4.53 (rabeprazole). Omeprazole (and its S-isomer esomeprazole) has a pK a1 of 4.06. These pK a1 values ensure that the pyridine nitrogen of all PPIs will be cationic at low pH (1.3) of the parietal cells. The highly cationic nature of the pyridine nitrogen is helpful in trapping the PPIs in the parietal cells. The pK a value of benzimidazole N3 (designated as pK a2) is much lower than that of pyridine nitrogen and ranges from 0.11 (pantoprazole) to 0.79 (omeprazole and esomeprazole). Lansoprazole and rabeprazole have identical pK a2 values as 0.62. These lower pK a values mean that the benzimidazole ring protonates after the pyridine ring, and the extent of protonation will be significantly lower.
Once the benzimidazole N3 is protonated, equilibrium is established between the dication and the two monocations (Fig. 8). After that, the lone pair electrons of the unionized pyridine nitrogen attacks at the C2 of the benzimidazole ring via intramolecular nucleophilic attack. When the pyridine attacks, a new bond is formed between the benzimidazole carbon and the pyridine nitrogen, i.e., a five-member ring as an intermediate so-called spiro compound. The spiro carbon is highly electron-deficient, and to satisfy this demand, electrons from the N3-hydrogen bond are donated to this carbon, thereby regenerating the benzimidazole double bond and releasing the N3-hydrogen as proton. When this double bond forms, it forces the bond between the benzimidazole and the sulfinyl sulfur atom to break. The oxygen atom of the sulfinyl group willingly takes the released proton, converting the sulfinyl to sulfenic acid (–S–OH). The sulfenic acid moiety can form a disulfide bond with the sulfhydryl (SH) group of proton pump cystine residues, releasing a molecule of water. Further, the lone pair of electrons on the nitrogen of benzimidazole ring attacks the electron-deficient sulfur atom of the sulfenic acid to generate a cyclic structure known as a sulfenamide and again releasing a molecule of water (Fig. 8). The sulfenamide sulfur atom is capable of forming a disulfide bond with -SH group of the proton pump cystine residues. The disulfide bond between the proton pump and the PPIs is extremely stable, and the bond cannot break to regenerate the free SH group on the proton pump cystine residues. The inhibition is therefore irreversible and the H+-K+-ATPase will no longer secrete acid (Shin and Sachs, 2009).
Salient features of PPIs
-
1.
Substituted benzimidazole moiety, substituted pyridine ring, and methyl sulfinyl chain connecting these two rings are the most important parts for the antisecretory activity.
-
2.
For proton pump inhibition activity, it is found that the 1-, 4-, 6- and 7-positions of benzimidazole ring should be unsubstituted, whereas 5-position should bear electron-donating substituents. The 2-position should be substituted with pyridinmethylsulfinyl moiety, and this pyridine ring should further contain electron-donating groups at 3-, 4-, and 5-positions (Fig. 7).
-
3.
It is eventually realized that the weakly basic nature of the benzimidazoles might contribute to drug effectiveness by permitting their accumulation in acidic environments. Indeed, substituted benzimidazoles with pK a values around 4.0 accumulate about 1000-fold in low-pH spaces and thus result in great organ selectivity.
-
4.
Biological activity and chemical stability are largely dependent on the type of substituents (i.e., electron-withdrawing or electron-donating groups) on both benzimidazole and pyridine rings. The electron-donating substituents have a significant impact on chemical reactivity and antisecretory action. Electron-donating substituents on the pyridine ring as well as on the C5 position of the benzimidazole ring increase the percentage existing in cationic form in gastric pH and also enhance the rate of formation of the active sulfenic acid/sulfenamide products, whereas electron-withdrawing substituents will have the opposite effect.
Angiotensin II type 1 (AT1) receptor antagonists
High blood pressure is one of the most common health problems worldwide, which can lead to heart attack, heart failure, and peripheral arterial disease. Thus, there is a continuing need for the development of potent antihypertensive drugs with higher curative effects and lower side effects. Several imidazole- as well as benzimidazole-based compounds have been well explored as antihypertensive drugs acting by interrupting an important hormone pathway, i.e., renin–angiotensin system, which plays a pivotal role in the regulation of blood pressure and fluid and electrolyte homeostasis.
Angiotensinogen, a polypeptide, is cleaved by renin to produce a decapeptide, Angiotensin I (Ang I), which is further acted upon by angiotensin-converting enzyme (ACE) to generate Angiotensin II (Ang II) an octapeptide which acts on G protein-coupled AT1 receptors resulting in vasoconstriction, sodium retention, and aldosterone release to cause hypertensive action. The various strategies to control these actions of Ang II include blocking the production of Ang II through the use of renin and ACE inhibitors or blocking the binding of Ang II to AT1 receptors. The major breakthrough in the understanding of the renin–angiotensin system was triggered by the development of ACE inhibitors. However, the inhibition of ACE produces an increase in the plasma bradykinin level and contributes to the side effects of ACE inhibitors, e.g., angioedema. To overcome several of the deficiencies of ACE inhibitors, the specific Ang II receptor antagonists were discovered and developed (Naik et al., 2010; Burnier, 2001). The concept of treating hypertension by a specific blockade of the renin–angiotensin system was first established with the use of saralasin, a nonselective antagonist of Ang II receptors. Although, saralasin reduced the arterial pressure in hypertensive patients with high circulating plasma renin activity, its therapeutic potential remained limited, since due to its peptidic nature, it has a very short plasma half-life, is not orally bioavailable, and also possesses significant Ang II-like agonistic properties.
The origin of potent nonpeptide Ang II receptor antagonists with high AT1 selectivity can be traced back to the Takeda series of 1-benzylimidazol-5-acetic acid derivatives. In 1982, Furukawa and colleagues of Takeda Chemical Industries at Osaka in Japan discovered weak nonpeptide Ang II receptor antagonists, i.e., S-8307 and S-8308 from a group of 1-benzylimidazole-5-acetic acid derivatives. The S-8307 and S-8308 have moderate potency, short duration of action, and limited oral bioavailability; however, they are selective and competitive AT1 receptor antagonists without partial agonist activity. On the other hand, a group at DuPont postulated that both Ang II and the Takeda leads were bound at the same receptor site. These two molecules served as lead compounds for further optimization of AT1 receptor blockers. Using nuclear magnetic resonance studies on the spatial structure of Ang II, scientists at DuPont discovered that the Takeda structures should be enlarged at a particular position to resemble more closely with the much larger peptide Ang II. Computer modeling was used to compare S-8308 and S-8307 with Ang II, and it was seen that Ang II contains two acidic residues near the NH2 terminus. These groups were not mimicked by the Takeda leads, and therefore, it was hypothesized that acidic functional groups would have to be added to the compounds (Fig. 9). The 4-carboxy-derivative, EXP-6155, had a binding activity which was tenfold greater than that of S-8308 which further strengthened this hypothesis. By replacing the 4-carboxy-group with a 2-carboxy-benzamido moiety, the compound EXP-6803 was synthesized (Fig. 10). It had highly increased binding affinity, but was only active when administered intravenously. Replacing the 2-carboxy-benzamido group with a 2-carboxy-phenyl group created the lipophilic biphenyl-containing EXP-7711, which exhibited oral activity. Then the polar carboxyl group was replaced with a more lipophilic tetrazole group in order to increase oral bioavailability and duration of action that led to the invention of losartan. This discovery took place in 1986, and losartan became the first successful competitive Ang II receptor antagonist approved in the USA in 1995.
In 1992, using a different lead optimization from S-8308, eprosartan was developed by SmithKline Beecham researchers, from Takeda series of benzylimidazoles (Fig. 10). Eprosartan does not have biphenyl-methyl structure, and to enhance its binding affinity, chain extension at 5-position of imidazole was done by a trans-5-acrylic acid group followed by the addition of a 2-thienylmethyl moiety. Further, replacement of the 2-chlorobenzyl group with a 4-carboxylbenzyl group resulted in eprosartan as a nonbiphenyl-, nontetrazole-based selective, potent, and competitive AT1 receptor antagonist with high affinity (Wexler et al., 1996). After the successful development of losartan and eprosartan, many pharmaceutical companies initiated studies in the development of more effective AT1 receptor antagonists. The goal was to discover potent compounds with long-lasting effect suitable for once-a-day dosing. Therefore, much effort was made to search lead compounds by synthesizing different heterocyclic compounds bearing various types of substituents on heterocyclic ring. To achieve the goal, the first screening of the synthesized compounds was done by an in vivo method out of which the lead compound A, having the hydroxymethyl and carboxyl groups at the 4- and 5-positions in the imidazole ring, respectively, showed potent activity over losartan. In 1991, DuPont researchers reported that large lipophilic or electron-withdrawing substituents at 4-position of imidazole were preferred to develop potent AT1 receptor antagonists (Carini et al., 1991). The hydrophilic hydroxylmethyl group in compound A seemed to have an important role in potent antagonist activity. Therefore, the lead compound A was further optimized by the introduction of a hydrophilic group at 4-position in the imidazole ring instead of hydrophobic one that led to the birth of olmesartan (Fig. 10). Olmesartan medoxomil is an imidazole-containing ester prodrug developed by Sankyo Pharma as AT1 receptor antagonist that was launched onto the market in 2002. In vivo, the prodrug is completely and rapidly hydrolyzed into the active acid form, olmesartan. The hydroxylisopropyl group connected to the imidazole ring in addition to the 5-carboxyl group contributes its strong antagonistic activity (Yanagisawa et al., 2012).
Further, potent AT1 receptor antagonists have also been obtained by replacing the imidazole ring with fused heterocyclic moiety, i.e., benzimidazole. Candesartan cilexetil is a benzimidazole ester carbonate prodrug, which was developed by Takeda. In vivo, it is rapidly converted to the much more potent corresponding 7-carboxylic acid, candesartan. The carboxyl group of the benzimidazole ring in candesartan plays an important role in binding with AT1 receptors. Candesartan and its prodrug have a stronger blood pressure lowering effect than losartan. Telmisartan is also an orally active potent AT1-selective antagonist that was discovered and developed in 1991 by Boehringer Ingelheim. It is unusual in that it contains benzimidazole with a second benzimidazole attached at 6-position signifying a bulky lipophilic group and a carboxylic acid at the 2-position of the biphenyl-methyl group which is more potent than the tetrazole analog (Fig. 10; Burnier and Brunner, 2000). Among all AT1 receptor antagonists, it is the most lipophilic compound and showed excellent oral absorption and tissue penetration. Both, candesartan and telmisartan are successfully prescribed for lowering of blood pressure. Azilsartan, developed as a result of the medicinal chemistry effort by Takeda group, is the most recently announced benzimidazole-containing AT1 receptor antagonist for the treatment of hypertension. It is the eighth AT1 receptor antagonist in clinical use worldwide, which was discovered by modification of the tetrazole ring in candesartan, and has a unique moiety, 5-oxo-1,2,4-oxadiazole, instead of tetrazole ring. The biphenyl-5-oxo-1,2,4-oxadiazole moiety may increase the lipophilicity and bioavailability compared with candesartan (Kohara et al., 1996). Azilsartan medoxomil, a prodrug of azilsartan, was approved in the USA by the FDA in 2011 for the treatment of hypertension. Azilsartan medoxomil and azilsartan both have shown greater antihypertensive effects than other AT1 receptor antagonists (Miura et al., 2013).
In general, it has been found that the imidazole and benzimidazole rings are the important pharmacophore for bioactivity of AT1 receptor antagonists. The potency and receptor affinity is largely dependent on the type of substituents present on these rings. For AT1 receptor antagonist activity the 1-, 2-, 4- and 5-positions of imidazole ring should be substituted, whereas 3-position should be unsubstituted (Fig. 11). The 1-position should bear biphenyl-methyl group along with acidic residues, i.e., tetrazole or carboxylate groups. The tetrazole and carboxylate groups of the biphenyl-methyl must be in the ortho position for optimal activity. These acidic groups bind to a basic position in the receptor that is required for potent antagonistic activity (Yanagiasawa et al., 1996). It is also found that the tetrazole group is superior in terms of metabolic stability, lipophilicity, and oral bioavailability. Lipophilic substitutes like the linear alkyl group, e.g., n-butyl group at 2-position of imidazole ring together with biphenyl-methyl group provides hydrophobic binding as these are associated with hydrophobic pockets of the receptor. It has also been reported that hydroxy group in the 4-position on the imidazole ring (e.g., losartan) plays an important role in the binding affinity and compensates for the disadvantage of lipophilicity of the bulky alkyl group. Imidazoles (e.g., olmesartan) that have hydroxy methyl and carboxy groups at 4- and 5-positions possessed potent antagonistic activity, because of hydrogen bonding and hydrophilicity of the hydroxymethyl group (Yanagiasawa et al., 1996).
The structure of eprosartan is the one that differs most from the other AT1 receptor antagonists, and the usual biphenyl-methyl group has been replaced by a carboxybenzyl group, and this change resulted in a stronger binding to the receptor; however, the biochemical and physiological effects are not significantly improved (Aulakh et al., 2007). The p-carboxylic group on the N-benzyl ring resulted in nanomolar affinity for AT1 receptor and good oral activity, while the presence of a thienyl ring (sulfur-containing heterocycle) together with two acid groups is important to achieve potency (Unger and Scholkens, 2004).
For benzimidazole-based AT1 receptor antagonism, the 1-position should also contain biphenyl-methyl group along with acidic groups. Incorporation of acidic groups like tetrazole or COOH produced orally active antagonists. The 2-position should be substituted with alkyl or alkoxy chain. The 3- and 5-positions should be unsubstituted, whereas 4- and 6-positions remain unsubstituted or should bear alkyl or bulky lipophilic groups, respectively. A carboxyl group at 7-position of benzimidazole provides potent compounds (Fig. 11). Esterification of the acidic function (ester prodrugs e.g., candesartan cilexetil and olmesartan medoxomil) improves the oral bioavailability.
Antifungal drugs
Fungal infections pose a continuing and serious threat to human health and life. These infections are estimated to occur in billions of people each year, and recent evidence suggests the rate is increasing (http://www.lef.org/protocols/infections/fungal_infections_candida_01.htm). As a result, serious attention has been directed toward the discovery and development of antifungal drugs. Among antifungal agents, azoles compounds such as imidazoles are the first class of synthetic antifungal agents which are widely used for the treatment of both superficial and systemic fungal infections. This chemical group has well represented with numerous clinically useful drugs that act by inhibiting cytochrome P-450-dependent 14α-lanosteroldemethylase enzyme which is required for fungal ergosterol biosynthesis (Rezaei et al., 2011). The first report of antifungal activity of an azole compound, benzimidazole, was described in 1944 by Woolley, who was studying biotin deficiency in animals and microbes (Woolley, 1944). At that time, mycotic diseases were of minimal interest so Woolley’s initial discovery was largely ignored. Thirty years later, Vanden Bossche observed that phenethylimidazole, another azole moiety with antifungal activity, inhibited the uptake of purines in yeast form Candida species by interference at the cell membrane (Vanden Bossche, 1974). In, Jerchel et al., 1952 revived Woolley’s work and reported that certain substituted benzimidazole compounds had significant antifungal activity (Jerchel et al., 1952). This publication encouraged other investigators to screen this group of chemicals in search of clinically useful antifungal agents. The breakthrough came in 1958 to 1959 when chlormidazole, a chlorobenzyl imidazole, was developed and studied as an antifungal drug (Sheehan et al., 1999). The introduction of chlormidazole heralded the beginning of the modern era of antifungal therapy. The three azoles compounds from two different laboratories were introduced into the market, i.e., clotrimazole, the first imidazole antifungal drug developed by chemists at Bayer AG, and miconazole and econazole, developed by Janssen Pharmaceutica, have represented the antifungal armamentarium in the late 1960s (Fromtling, 1988). The in vitro activity of clotrimazole against dermatophytes, yeasts, and dimorphic as well as filamentous fungi, is well established (Shadomy, 1971). However, unacceptable side effects following oral administration (Tettenborn, 1974) and unpredictable pharmacokinetics have limited the use of clotrimazole for topical treatment of dermatophytic infections and superficial Candida infections, including oral thrush and vaginal candidiasis (Burgess and Bodey, 1972). Miconazole, a phenethyl imidazole derivative synthesized in 1969, was the first azole available for parenteral administration. The drug has a limited spectrum of activity including dermatophytes, Candida species, dimorphic fungi, and Pseudallescheria boydii. The agent has proven to be topically an effective antifungal agent, but toxicity associated with the vehicle used for intravenous administration has limited its parenteral use (Heel et al., 1980). However, it has been used successfully in the treatment of systemic Candida infections, pseudallescheriasis, and some refractory cases of cryptococcal meningitis (Bennett, 1981; Lutwick et al., 1979). Econazole, structurally identical to miconazole with the absence of one chlorine atom on one benzene ring, was also developed by Janssen Pharmaceutica in 1974. Topically, this drug possessed broad-spectrum activity against dermatophytes, Candida, and other infections (Godefroi et al. 1969). During this decade, attempts to develop systemic formulations of clotrimazole and miconazole were made, but with limited success (Burgess and Bodey, 1972; Heel et al., 1980; Sawyer et al. 1975; Fainstein and Bodey, 1980). The introduction of ketoconazole in 1981 by Janssen Pharmaceutica represented the nadir in the search for new safe and effective agents. For nearly a decade, it was the only oral agent available for the treatment of systemic fungal infections and considered to be the ‘‘gold standard’’ (Heeres et al., 1979). Over the years, a number of clinically relevant shortcomings of this compound appeared like dose-related gastrointestinal side effects, unpredictable drug interactions (e.g., cyclosporine), largely fungistatic, proved to be less effective in immunocompromised patients, and intravenous formulation is not available. Thus, the poor response rates and frequent recurrences of major fungal infections, as well as the toxicity associated with ketoconazole therapy, led to the search for more potent antifungal drugs. Much effort has been made by different pharmaceutical companies toward antifungal therapy that resulted in various drugs containing imidazole such as flutrimazole (Alomar et al., 1995), bifonazole (Bayer AG; Plempel et al., 1983), butoconazole, an outlier having a 1-(phenylbutyl)-imidazole scaffold (Syntex Research Laboratories; Fromtling, 1986), croconazole (Shionogi Research Laboratories; Ogata et al., 1983), fenticonazole (Recordati SpA; Tajana et al., 1981), isoconazole (Janssen Pharmaceutica; Hernandez Molina et al., 1992), oxiconazole (F. Hoffmann-LaRoche and Siegfried AG; Polak, 1982), sulconazole (Syntex Research; Yoshida et al., 1984), tioconazole (Pfizer; Jevons et al., 1979), luliconazole (Nihon Nohyaku Co., Ltd.; Uchida et al., 2004), omoconazole (Siegfried AG; Thiele et al., 1987, Fromtling, 1988), sertaconazole (Ortiz, 1992; Palacin et al., 2001), neticonazole (Nimura et al., 2001), and eberconazole (designed and investigated by the Wassermann investigation center; Fernandez-Torres et al., 2003) (Fig. 12).
Moreover, benzimidazole-containing systemic fungicide, e.g., benomyl was introduced in 1968 by DuPont, and carbendazim, metabolite of benomyl, was developed in 1973 by BASF, Hoeschst (now part of Bayer) and DuPont (Fig. 12). Due to toxicity as well as prevalence of resistance of parasitic fungi, these drugs are withdrawn from the market (Stringer and Wright, 1976).
Development of imidazole-containing antifungal drugs by structural modification of miconazole
-
1.
A number of clinically approved conazoles have been developed by extensive exploration or structural modification on the miconazole (a phenethyl imidazole derivative) molecule.
-
2.
Removal of one chlorine atom on one benzene ring gave econazole which is effective for topical antifungal therapy.
-
3.
Further, replacement of the oxygen by a sulfur (thioether formation) in the econazole structure led to the discovery of sulconazole, another broad-spectrum antimycotic agent developed for topical application.
-
4.
Structural modification of the econazole molecule by substitution of a large phenylthio group for the 4-chloro in the benzylether moiety led to the synthesis of fenticonazole, a compound with broad-spectrum activity.
-
5.
Replacement of the 2,4-dichlorobenzyl group in the miconazole structure with a 2-(3-chlorothienyl)-methyl moiety gave tioconazole, a new broad-spectrum antifungal agent.
-
6.
Insertion of an oxime moiety into the miconazole structure gave oxiconazole, a new broad-spectrum antifungal. The chemical structure contains an oxime-ether fragment, which exhibited E and Z geometric isomers, of which the Z-form clearly demonstrated superior antifungal activity compared to the E-isomer.
-
7.
Substitution of the 2,4-dichlorobenzyl moiety in miconazole with a 3-(7-chlorobenzothiophene)-methyl group gave sertaconazole, another imidazole derivative with broad-spectrum antifungal activity. The benzothiophene group makes the compound lipophilic, which enhances the penetration of drug through the horny layer of the skin where some pathogenic fungi thrives, but avoids systemic absorption.
-
8.
All the aforementioned imidazole derivatives are 1-(arylethyl)-imidazoles, and elongation of the distance between the aryl and the imidazole rings gave rise to the discovery of the 1-(arylbutyl)-imidazole derivative, i.e., butoconazole.
-
9.
Incorporation of the dioxolane ring led to the discovery of new miconazole analogue, i.e., ketoconazole, the first orally active broad-spectrum antifungal agent.
-
10.
From SAR insight, it is found that the halogenated aryl derivatives are required for broad-spectrum antifungal activity.
Antiparasitic drugs
Parasites are microorganisms that live on or inside another organism (the host) and produce harmful effects by growing, reproducing, or giving off toxins to the host that result in parasitic infection. Such organisms may include helminths (nematodes, cestodes, and trematodes etc.) or protozoa, (ameba). Parasitic infections can spread through contaminated water, waste, fecal matter, blood, or through food and constitute one of the most widespread human health problems, mainly in tropical and subtropical regions. Since parasites are eukaryotic, they share many common features with their mammalian host; therefore, the development of effective and selective drugs against parasites is a challenging task (http://www.healthline.com/health/parasitic-infections#Overview1). Antiparasitics are a class of drugs which are indicated for the treatment of parasitic infections. Among heterocycles, the imidazole- and benzimidazole-based drugs have played a major role to combat such infections. The nitroimidazole-based drugs, i.e., metronidazole, ornidazole, secnidazole, nimorazole, and tinidazole are well-established drugs in widespread clinical use to treat diseases caused by protozoa and anaerobic bacteria. Particularly, structurally simple metronidazole is an effective synthetic compound introduced in 1960 and possesses strong inhibitory efficacies against anaerobic bacteria such as Helicobacter pylori and protozoa such as Giardia, Lamblia, and Entamoeba histolytica (Khabnadideh et al. 2007). Although metronidazole is a product of synthetic chemistry, its origin goes back to the discovery of azomycin (2-nitroimidazole) in 1953, by Nakamura at the prolific laboratory of Hamao Umezawa in Tokyo, and its structure was solved in 1955 (Nakamura 1955). Azomycin, produced from the extract of soil Streptomyces cultures, was the first 2-nitroimidazole to exhibit activity against several protozoans, specifically Trichomonas. Azomycin itself turned out to be too toxic to be used clinically, but it inspired the synthesis of a series of analogs by the French team that led to the emergence of metronidazole, an important drug for treating protozoal and trichomonas infections (Cosar and Julou, 1959). Serendipitously, it was found to be active against ulcerative gingivitis, bacterial infection of gums, and this led to the realization of its broader antibacterial activity. It is especially active against anaerobic bacteria such as Bacteroides fragilis and is approved for a number of indications which involve this pathogen (Shinn, 1962). Azomycin became the chemical lead in extensive synthetic development of over hundred compounds. Benzindazole is another 2-nitroimidazole-based drug and find its therapeutic use in Chagas disease due to trypanosomiasis infection.
However, 5-nitroimidazoles constitute the largest group of nitroimidazoles with antiprotozoal and antibacterial activities. Metronidazole is the prototype more active drug available for treatment of trichomoniasis, amebiasis, giardiasis, and active against anaerobic bacteria. Despite the availability of metronidazole since the late 1950s, the mechanism of action of the drug is still unknown. It is generally agreed that the nitroaryl compounds (nitroimidazoles) are reduced to nitro radical anions, which in turn react with oxygen to regenerate the nitroaryl and the superoxide radical anion. Further reduction of superoxide radical anion leads to hydrogen peroxide, and homolytic cleavage of the latter leads to hydroxyl radical formation. Superoxide radical anion, hydrogen peroxide, and hydroxyl radicals are reactive oxygen species that cause destructive effects on cell components, i.e., DNA, proteins, and membranes (DoCampo, 1990; Fig. 13). In order to improve bioavailability of metronidazole, extensive chemical modifications were carried out. As 1-(2-hydroxyethyl) side chain at 1-position of metronidazole is readily oxidized metabolically, replacement of side chain resulted in the development of other clinically useful antibacterial and antiprotozoal drugs, like tinidazole, panidazole, ornidazole, secnidazole, carnidazole, nimorazole, dimetridazole, ipronidazole, ronidazole, azanidazole, fexinidazole, sulphimidazole, and propenidazole (Kapoor et al., 2003; Fig. 14).
Anthelmintics
The therapeutic potential of benzimidazole in parasite chemotherapy was recognized after the introduction of phenzidole as a sheep anthelmintic by Imperial Chemical Industry in the early sixties (McFarland, 1972). In 1961, Brown and his team at Merck Sharp & Dohme Laboratories discovered thiabendazole as a broad-spectrum anthelmintic (Brown et al., 1961). The introduction of thiabendazole against parasite infections of both humans and domestic animals provided a major breakthrough that opened up a new era to design further potent anthelmintics. Thiabendazole is the first benzimidazole to be marketed over 50 years ago to combat helminthic infections. Although, it shows broad-spectrum activity against different helminths, it suffers from the limitation of being readily metabolized into inactive 5-hydroxythiabendazole, with very short half-life (Fisher, 1986). To prevent enzymatic hydroxylation of thiabendazole at 5-position, Merk scientists synthesized a variety of 5-substituted thiabendazoles, of which cambendazole showed promising activity with a longer half-life (Hoff et al., 1970; Hoff, 1982). Another milestone in the SAR of benzimidazoles was achieved at SmithKline Laboratory, where replacement of the thiazole ring of thiabendazole by thiocarbamate led to the discovery of parbendazole with high anthelmintic activity (Actor et al., 1967). The discovery of parbendazole stimulated a vigorous search for better benzimidazole anthelmintics in different pharmaceutical companies of the world. A number of benzimidazole-based broad-spectrum anthelmintics as derivatives of carbendazim came into the market that act by inhibiting the microtubule formation, such as mebendazole, flubendazole, cyclobendazole, fenbendazole, oxfendazole (or fenbendazole sulfoxide), oxibendazole, nocodazole, albendazole, ricobendazole, (albendazole sulfoxide), and luxabendazole (Townsendand and Wise, 1990; Martin, 1997; Fig. 15). Albendazole, fenbendazole, and oxfendazole are the first benzimidazoles to be successfully used for the treatment of all growth stages of gastrointestinal nematodes. These drugs may also be used in the treatment of lungworms, tapeworms, and adult stages of liver fluke. The noncarbamate benzimidazole, triclabendazole, was later introduced as antihelmenthic agents for treatment of all stages of liver fluke, but it is ineffective against nematodes. Luxabendazole is a benzimidazole sulfide used in the treatment of food-producing animal. The low solubility of benzimidazole sulfides and sulfoxides leads to their low absorption from gut, resulting in low bioavailability. Therefore, netobimin and febantel, which are the prodrugs of albendazole and fenbendazole, respectively, have greater water solubility resulting in improved absorption and increased bioavailability, whereas other pro-benzimidazoles such as benomyl and thiophanate, have found widespread use as fungicidal agents, which are precursors of carbendazim (Ozkay et al., 2010).
It is found that various benzimidazole-based drugs for parasitic chemotherapy have been developed by carrying out structure modifications at 2, 5(6)-positions of the benzimidazole nucleus. The presence of hydrogen atom at 1-position of benzimidazole is essential for anthelmintic activity, as all 1-substituted benzimidazoles led to lowering or loss of activity except for benomyl (prodrug). The presence of substituents on 2- and 5(6)-positions of benzimidazole plays a significant role in determining the anthelmintic profile, whereas the 1-, 4- and 7-positions should be unsubstituted. Although, benzimidazole-2-carbamates possess broad-spectrum activity against different gastrointestinal helminths, virtually all of them suffer from the limitation of being highly insoluble, due to which these have poor and inconsistent gastrointestinal drug absorption making them weakly active and ineffective. In an attempt to improve the solubility of benzimidazole-2-carbamates, a large number of 2-alkyl/aryl carbonylaminobenzimidazoles and 2-benzimidazolylureas have been synthesized. Further, to improve biological response a variety of 5-alkylthio and 5-arylthiobenzimidazole-2-carbamates have been prepared. The corresponding sulfoxide and sulfones have also been synthesized. In general, 5-alkylthio/arylthiobenzimidazole-2-carbamates and their sulfoxides offer a wider spectrum of activities and improve efficacy. Of these fenbendazole, oxfendazole, albendazole, and ricobendazole have possessed broad-spectrum anthelmintic activity. Replacement of sulfur in 5-alkylthio/arylthiobenzimidazole-2-carbamates by oxygen gives 5-alkoxy/aryloxybenzimidazole-2-carbamates, i.e., oxibendazole and luxabendazole, which exhibit high activity against different helminth parasites in domestic animals. However, 5-amino benzimidazoles like cambendazole showed poor anthelmintic activity. From the foregoing discussion on SAR, it can be concluded that it is possible to achieve high anthelmintic activity by benzimidazole having a hydrogen atom at 1-position, a methoxycarbonylamino function at 2-position and an alkyl, aryl, aralkyl, or heteroaryl groups attached to 5-position through a CO, CHOH, CONH, S, SO, or O bridge (Sharma, 1990). The demonstration of higher-order anthelmintic activity by thiabendazole and cambendazole possessing a 4-thiazolyl group at 2-position of benzimidazole may be explained by electronic and structural congruence of the thiazolyl pharmacophore with the methoxycarbonylamino function (McCracken and Lipkowitz, 1990; Fig. 16).
Adrenergic receptor agonists/antagonists
The endogenous catecholamines, adrenaline (epinephrine), and noradrenaline (norepinephrine) act through adrenergic receptors. The adrenergic receptors (or adrenoceptors) are divided into two major types, i.e., α-receptors (α1 and α2 subtypes) and β-receptors (β1, β2 and β3 subtypes). All these are G protein-coupled receptors, widely located in various organs and tissues, and mediate pharmacological action like smooth muscle contraction, lowering of blood pressure, increased heart rate, and bronchodilation (Insel, 1996). A number of adrenergic receptor agonists as well as antagonists containing imidazole scaffold have been developed and successfully used clinically. Tolazoline and phentolamine are imidazole derivatives act as α1-adrenergic receptor antagonists that have antihypertensive activity, although these drugs have been replaced in general clinical use by far better agents because of their side effects. Tolazoline has structural similarities to the imidazoline α1-agonists, such as naphazoline and xylometazoline, but does not have the lipophilic substituents required for agonist activity. Oxymetazoline, a topical decongestant, was developed from xylometazoline in 1961 at Merck by Fruhstorfer. It acts as a selective α1-agonist and partial α2-agonist, works by constricting the blood vessels in the nose. The decongestant effect is due to constriction of large veins in the nose, which swell up during the inflammation of any infection or allergy of the nose (Griffith, 2003).
The α2-adrenoceptor is considered as an attractive therapeutic target for the treatment of hypertension. Many imidazole-based drugs have the ability to interact with α 2-adrenoceptor and are potent vasodilators. Clonidine, an imidazoline compound, is a centrally acting prototype of selective α2-adrenergic receptor agonist. At the beginning of the 1960s, scientists at Boehringer Ingelheim started working with an aim to synthesize peripherally active adrenergic compounds for nasal decongestion as simple nasal drops. The research investigators observed that most of the decongestive agents are derived from the imidazoline structure. Additionally, this portion is connected to an aromatic nucleus by a methylene (–CH2–) bridge. Therefore, the first fundamental alteration was done by replacing the –CH2– bridge by –NH– group. However, this replacement of the –CH2– bridge by –NH– group had not been achieved chemically in compounds substituted at both 2- and 6-positions of the phenyl ring. The problem was solved by introducing chlorine atoms as substituents in the 2- and 6-positions of the phenyl ring that led to the discovery of clonidine which exists in imino and amino tautomeric forms (Fig. 17). Clonidine was subsequently developed for its blood-lowering effect and introduced into clinical practice in the 1966 as a centrally acting antihypertensive agent. It acts by stimulating the pre-synaptic α 2-adrenoceptor, thereby decreasing the noradrenaline release from both central and peripheral sympathetic nerve terminals. Besides its therapeutic value, clonidine has proved to be an essential pharmacological tool and has provided valuable insight into the importance of central α2-adrenoceptors (Stahle, 2000). Lofexidine (Fig. 17) is structurally analogous to clonidine, another α2-adrenergic receptor agonist used for the treatment of opioid withdrawal symptoms. It also contains an imidazole ring and a 2,6-dichlorinated phenyl ring. Administration of lofexidine in heroin addicts has been shown to be more effective for a longer duration, with fewer withdrawal symptoms than clonidine even after 1 day (Gerra et al., 2001). Moxonidine is an imidazoline-containing selective agonist of I1-imidazoline receptors in the central nervous system used to reduce blood pressure. The novel mechanism of action of moxonidine claimed fewer adverse effects than the older centrally acting agents such as clonidine. It was developed by Solvay Pharmaceuticals and represents a new-generation centrally acting antihypertensive which by virtue of its selectivity for the imidazoline receptor is expected to have fewer α2-related adverse effects (sedation and dry mouth) (Morris and Reid, 1997). Idazoxan, efaroxan atipamezole, and fipamezole are also imidazole-based drugs acting as selective α2-adrenergic receptor antagonists (Clarke and Harris, 2002). Atipamezole is indicated for the reversal of sedative and analgesic effects of dexmedetomidine and medetomidine in dogs. It has also been researched in humans as a potential antiparkinson drug (Pertovaara et al., 2005). Fipamezole is an innovative, highly selective α2-adrenergic receptor antagonist indicated for the treatment of levodopa-induced dyskinesia in parkinson disease. It enhances the signalling of neurotransmitters in the brain, including dopamine, serotonin, and noradrenaline (Fig. 17) (Savola et al., 2003).
5-Hydroxytryptamine (5-HT3, serotonin) receptor antagonists
The 5-HT3 receptor is a subtype of serotonin receptors belongs to the superfamily of ligand-gated ion channels, which are found in the central nervous system in the area postrema (chemoreceptor trigger zone), vomiting center, and gastrointestinal tract. Serotonin blockers or 5-HT3 receptor antagonists are a class of drugs which are used to control nausea and vomiting by acting on 5-HT3 receptors. These drugs have ability to block the action of serotonin from activating nerves that bring about the vomiting reflex. The 5-HT3 receptor antagonists were originally discovered in the 1990s and are one of the newest types of antivomiting drugs on the market. The effectiveness of these drugs has revolutionized the management of nausea and vomiting produced by cancer chemotherapy or radiotherapy and is considered as the gold standard for this purpose. These drugs inhibit the action of serotonin on nerves that transmit vomiting impulses from the intestines to the brain.
The history of the 5-HT3 receptor antagonists began, when Gaddum and Picarelli (Gaddum and Picarelli, 1957) proposed the existence of two serotonin receptor subtypes, i.e., the M and D receptors (thus named because their function could be blocked by morphine and dibenzyline, respectively), in a landmark paper (Gaddum and Picarelli, 1957). The M receptor was later renamed as the 5-HT3 receptor (Barnes et al., 2009). A variety of indole analogues as 5-HT antagonists were developed in the late 1970s, but none of them selectively blocked the 5-HT3 receptor. The first-generation 5-HT3 receptor antagonist, i.e., ondansetron was developed from the lead compound, i.e., indolylpropanone, in around 1984 by the scientists working at Glaxo Laboratories. Initially a promising series of imidazoles were explored, but proved to be inactive by mouth, so the decision was taken to limit the flexibility of the indolylpropanone side chain by linking it to an adjacent position in the indole ring, thus forming a third ring to give a tetrahydrocarbazolone. When this gave encouraging results, the corresponding analog of the most promising of the earlier imidazoles was synthesized. It was proved active by mouth and in 1990 became the first 5-HT3 receptor antagonist to be introduced into the clinic, with the approved name of ondansetron. It is prescribed as an antiemetic agent to control vomiting induced when chemotherapy releases serotonin from enterochromaffin cells in the upper gastrointestinal tract. The released serotonin then acts on both local 5-HT3 receptors as well as on those in the chemoreceptor trigger zone of the brain to stimulate the vagus nerve and so cause vomiting (Butler et al., 1988) (Fig. 18). A related group of antagonists that possess an imidazole or related heterocyclic terminal amine include alosetron, ramosetron, fabesetron, and cilansetron (Fig. 19). Alosetron is also a carbazole derivative, structurally analogous to ondansetron, act on 5-HT3 receptors in the gastrointestinal tract. It is the first compound of this type to be developed for irritable bowel syndrome (Elizabeth et al., 2000). Ramosetron is a selective 5-HT3 receptor antagonist with an affinity higher than ondansetron. It also contains an indole aromatic ring along with benzimidazole moiety as a basic center both associated with carbonyl linkage. It is more efficacious than other setrons against nausea and vomiting induced by chemotherapy or surgical interventions and also indicated for a treatment of diarrhea-predominant irritable bowel syndrome in males (Rabasseda, 2002; Nakata-Fukuda et al., 2014). Cilansetron, a novel 1,7-annelated indole, is a second selective and competitive 5-HT3 receptor antagonist. Cilansetron and alosetron are structurally similar to ondansetron; however, cilansetron is reported to be 10 times more potent than ondansetron. It is specifically designed and developed by Solvay Pharmaceuticals for treatment of irritable bowel syndrome with diarrhea predominance that is effective in men as well as women (Chey and Cash, 2005).
From the above discussed data, it is identified that 5-HT3 receptor antagonists share a common pharmacophoric features. A composite pharmacophore model for 5-HT3 receptor antagonists is shown in Fig. 20. An aromatic moiety (preferably indole) important for binding affinity which is associated with hydrophobic binding regions, a linking acyl group capable of hydrogen bonding interactions, and a basic amine (imidazole or benzimidazole) can be regarded as the key pharmacophoric elements of the known 5-HT3 receptor antagonists.
Anticancer drugs
Cancer is one of the most serious threats to human health, which has drawn unusual attention all over the world. Extensive research has been devoted toward the development of effective anticancer therapeutics, involving radiation therapy and chemotherapy (Grasso et al., 2012). Imidazole-based anticancer drugs possess considerable potentiality because of their ability to interfere with DNA synthesis and then halt the cell growth and division. So far, many imidazole-containing anticancer drugs dacarbazine, zoledronic acid, azathioprine, misonidazole, pimonidazole, nilotinib, tipifarnib, fadrozole, indimitecan, and bendamustine have been developed, playing an important role in the clinic (Fig. 21). Dacarbazine is a member of the class of alkylating agents, which destroy cancer cells by adding an alkyl group to DNA. It is a structural analogue of imidazole carboxamide, a purine precursor, and used for the treatment of metastatic malignant melanoma, Hodgkin lymphoma, sarcoma, and islet cell carcinoma of the pancreas (Pectasides et al., 1989). Zoledronic acid, a bisphosphonate, is an inhibitor of osteoclast-mediated bone resorption and is used in the management of patients with cancer. It slows down bone resorption, allowing the bone-forming cells time to rebuild normal bone and allowing bone remodeling (Li and Davis, 2003). Moreover, nitroimidazole-based drugs have also been developed with great value, i.e., azathioprine, having 4-nitroimidazole-5yl-moiety attached to purine through sulfur has shown cytotoxic as well as immunosuppressive action. It acts as a prodrug for mercaptopurine and used for the treatment of childhood acute lymphoblastic leukemia (Hawwa et al., 2008), Whereas misonidazole, etanidazole, and pimonidazole are 2-nitroimidazoles, acting as radiosensitizer of hypoxic tumor cells (Josephy et al., 1981). Pimonidazole is reduced in hypoxic environments, as in tumor cells; thereby it can be used as a hypoxia marker. In hypoxic cells, reduced pimonidazole binds to -SH-containing molecules such as glutathione and proteins, and the resulting complexes accumulated in tissues, thereby sensitizing cells to be more susceptible for radiation treatment (Varia et al., 1998). Etanidazole also possess potential applications in cancer chemotherapy by depleting glutathione concentration and inhibits glutathione transferase. This enhances the cytotoxicity of ionizing radiation (Yang et al., 2012). Nilotinib (Fig. 21) is a novel and selective small molecule Bcr-Abl.
Tyrosine kinase inhibitor was approved for the treatment of imatinib-resistant chronic myelogenous leukemia and acts by interacting with the ATP-binding site of BCR–ABL with a high affinity (DeRemer et al., 2011). Tipifarnib (Fig. 21) is a potent farnesyl transferase inhibitor developed by Johnson & Johnson Pharmaceutical for the treatment of acute myeloid leukemia. It is a nonpeptidomimetic quinolone analog of imidazole-containing heterocycle that competitively inhibits the enzyme. The imidazole group is the central pharmacophore, and it may interact with the coordination structure of the zinc catalytic site (Thomas and Elhamri, 2007). Azole-based selective aromatase inhibitors such as fadrozole is of great interest to medicinal chemists. It has been recommended as first-line drugs in the therapy of breast cancer (Raats et al., 1992). On the other hand, indimitecan has been demonstrated to inhibit topoisomerase-I enzyme by intercalating between the DNA base pairs and to stabilize a ternary complex. Additionally, they produce a unique pattern of DNA cleavage sites relative to camptothecins and therefore may target genes differently, which could result in a different spectrum of anticancer activities (Beck et al., 2014), whereas bendamustine (Fig. 21) is also a bifunctional alkylating agent, synthesized in the 1960s by Ozegowski and Krebs in East Germany with the aim of combining the alkylating properties of 2-chloroethylamine and the antimetabolite properties of a benzimidazole ring (Tageja and Nagi, 2010). It is believed to act as an alkylating agent that induces interstrand DNA cross-linking and is used in the treatment of chronic lymphocytic leukemia and lymphomas (Hartmann and Zimmer, 1972; Kath et al., 2001). It has a nitrogen mustard moiety, a benzimidazole ring, and an alkane carboxylic acid side chain, which all may be responsible for its cytotoxic activity. The benzimidazole ring may be responsible for the purine analog activity of bendamustine (Weide, 2008).
Antiviral drugs
Viral infections are common obligate parasites, which severely threaten the health of human beings. Much research has been carried out toward the development of imidazole- and benzimidazole-based drugs against human cytomegalovirus (HCMV), human herpes simplex virus, human immunodeficiency virus, and hepatitis B and C virus. Nucleoside analogs are currently in clinical use for the treatment of such infections act by inhibiting viral replication. In the late 1980, Leroy B. Townsend and John C. Drach at the University of Michigan discovered antiviral activity in a series of benzimidazole derivatives. The two compounds, TCRB and 2-bromo analog (BDCRB), were found to be potent and selective inhibitors of HCMV replication. The most exciting aspect of this new chemical series was the mode of action that involves the inhibition of viral DNA synthesis and viral egress. Unfortunately, their clinical development potential was limited because of rapid metabolic cleavage of the sugar from the heterocycle. Through a collaborative partnership with Burroughs Wellcome, they conducted SAR studies on benzimidazole series that led to the emergence of two clinical candidates, i.e., the pyranoside of BDCRB and maribavir, each novel but with distinct modes of action. Maribavir is a selective, orally bioavailable ribosyl benzimidazole, which is introduced for the prevention and treatment of HCMV disease in hematopoietic stem cell/bone marrow transplant patients (Biron et al., 2002). A ribosyl moiety at 1-position proved to be very important for the activity (Chodosh et al., 1989; Fig. 22). However, nucleoside analogs are associated with solubility problems, so extensive work has been done in exploring non-nucleoside compounds as antiviral agents. This led to the discovery of enviroxime and enviradine which are the non-nucleoside analogs and came into clinical use in the early 1980s as potent broad-spectrum inhibitors of RNA viruses. Enviroxime and related compounds inhibit the replication of rhinoviruses and enteroviruses (Heinz and Vance, 1995). Another imidazole-based non-nucleoside analog capravirine was developed by Pfizer as a reverse-transcriptase inhibitor that act by forming an extensive hydrogen bond network with the enzyme. But in early July 2005, it was discontinued after the results of two Phase IIb studies that failed to show a statistically-significant difference between standard triple-drug HIV therapies and the same therapy combined with capravirine (Gewurz et al., 2004; Ren et al., 2000).
Miscellaneous
In addition to the above discussed therapeutic areas, imidazole as well as benzimidazole-based drugs have also been approved for clinical use such as anticonvulsants, antithyroids, antidiabetics, sedative and hypnotics, anesthetics, immunosuppressants, anticoagulants, retinoic acid metabolism blockers, thromboxane synthetase inhibitors, and analgesics which are discussed in Table 1.
Future directions
The imidazole- and benzimidazole-based drug discovery and development is an attractive topic and draws more and more researchers to engage in this research area. An increasing number of imidazole and benzimidazole derivatives have been explored and related research is ongoing with infinite potentiality. As it can be seen in Table 2, there are currently adequate numbers of drug candidates in different stages of clinical trials which are discovered by various pharmaceutical companies.
In future research, novel as well as potent chemical entities can be explored by combining both imidazole and benimidazole scaffolds with enormous potentiality for the treatment of diverse diseases. This may revolutionize the world of medicine in the next century. Due to the problems like resistance, toxicity, or poor bioavailability, there is a need for modification of existing agents that will bring about a big change for improvement of activity or change in activity. Prodrug concept can also be utilized to improve bioavailability of existing drugs. Benzimidazole derivatives have attracted considerable attention in recent years. Combination of the modifications at positions 1, 2 and 5 of the molecule has provided the most active drugs. However, the 4-, 6-, and 7-positions of benzimidazole need to be explored further for novel entities with exciting biological activities.
As discussed above acid-related diseases, such as peptic ulcers and GERD are an extremely common set of human ailments and PPIs are mainstay of therapy. Improvements in PPIs can be made by altering the mechanism of activation of PPIs. What may be amenable to future research is to generate PPIs with a much longer residence time in the blood so that more pumps can be inhibited and also bedtime dosing can be achieved. Moreover, novel PPIs can be designed in future with improved pharmacological profile by use of imidazole ring in place of benzimidazole in PPIs.
Stereochemistry can have a profound effect on both the pharmacokinetic and pharmacodynamic properties of a drug, and it is very important to study the stereochemical features of the compounds. Furthermore, related isomers of existing clinically approved drugs need to explore and studied. Because living systems (proteins and other biological targets) are themselves chiral, so in a chiral environment, one enantiomer may display different chemical and pharmacological behavior than the other enantiomer.
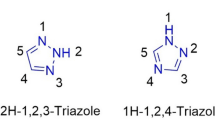
The main problem in the treatment of fungal infections is the increasing prevalence of drug resistance due to the increased use of antibiotics and immunosuppressive drugs. Thus, the pursuit of structurally novel imidazoles with more effective, less toxic, and less resistances remains to be a highly challenging task and has aroused great interest in discovery and development of new antifungal drugs. Further structural modifications on clinical azole drugs are required to increase the antifungal potency and selectivity as well as to improve the bioavailability. Due to resistance to imidazole-based antifungal therapy, benzimidazole nucleus can be optimized to generate new, safer, and more effective drugs that satisfy the increasing need of patients afflicted with fungal infections. In recent years much effort has been devoted toward triazole-based antifungal drugs as these possess superior antifungal activity. Therefore, in our opinion novel drugs can be discovered by combining imidazole–trizole- or benzimidazole–trizole-based heterocycles. This concept can represent the next major step forward in the development of broad-spectrum, more potent, and less toxic antifungal drugs. We are hopeful that these perspectives could provide the impetus to investigate novel and more efficacious drugs in future.
Conclusion
The structurally simple bioactive heterocycles, i.e., imidazole and benzimidazole have played an imperative role in drug discovery and development. A large amount of effort has been invested toward imidazole- and benzimidazole-based medicinal chemistry with outstanding achievements that resulted in various drugs for the treatment of many diseases with great therapeutic utility. Imidazole- and benzimidazole-based medicinal chemistry as well as designing of drugs will continue to be an overwhelmingly attractive topic in quite a long time. There is no comprehensive report on the discovery and development of imidazole- and benzimidazole-based drugs along with their mechanism and SAR features available in the literature till date. This review is an endeavor to highlight for the first time more than 160 drugs containing imidazole and benzimidazole bioactive heterocycles along with their development and therapeutic uses. The successful strategies as well new perspectives have been discussed to discover novel drugs in the future. We hope this paper will form a comprehensive foundation and reference source that will open up new opportunities for researchers interested in imidazole- and benzimidazole-based medicinal chemistry and drug designing.
References
Actor P, Anderson EL, DiCuollo CJ, Ferlanto RJ, Hoover JRE, Pagano JF, Ravin LR, Scheidy SF, Stedman RJ, Theodorides VJ (1967) New broad spectrum anthelmintic, methyl 5(6)-butyl-2-benzimidazolecarbamate. Nature 215:321–322
Alomar A, Videla S, Delgadillo J, Gich I, Izquierdo I, Forn J (1995) Flutrimazole 1 % dermal cream in the treatment of dermatomycoses: a multicenter, double-blind, randomized, comparative clinical trial with bifonazole 1 % cream. Efficacy of flutrimazole 1 % dermal cream in dermatomycoses. Catalan flutrimazole study group. Dermatology 190:295–300
Arrang JM, Garbarg M, Lancelot JC, Lecomte JM, Pollard H, Robba M, Schunack W, Schwartz JC (1988) Highly potent and selective ligands for a new class H3 of histamine receptor. Invest Radiol 23:S130–S132
Aulakh GK, Sodhi RK, Singh M (2007) An update on non-peptide angiotensin receptor antagonists and related RAAS modulators. Life Sci 81:615–639
Barker HA, Smyth RD, Weissbach H, Toohey JI, Ladd JN, Volcani BE (1960) Isolation and properties of crystalline cobamide coenzymes containing benzimidazole or 5,6 dimethylbenzimidazole. J Biol Chem 235:480–488
Barnes NM, Hales TG, Lummis SCR, Peters JA (2009) The 5-HT3 receptor-the relationship between structure and function. Neuropharmacology 56:273–284
Beck DE, Agama K, Marchand C, Chergui A, Pommier Y, Cushman M (2014) Synthesis and biological evaluation of new carbohydrate-substituted indenoisoquinoline topoisomerase I inhibitors and improved syntheses of the experimental anticancer agents Indotecan (LMP400) and Indimitecan (LMP776). J Med Chem 57:1495–1512
Belch JJ, Cormie J, Newman P, McLaren M, Barbenel J, Capell H, Leiberman P, Forbes CD, Prentice CR (1983) Dazoxiben, a thromboxane synthetase inhibitor, in the treatment of Raynaud’s syndrome: a double-blind trial. Br J Clin Pharmacol 15:113S–116S
Bennett JE (1981) Miconazole in cryptococcosis and systemic candidiasis: a word of caution. Ann Intern Med 94:708–709
Bhatnagar A, Sharma PK, Kumar N (2011) A review on “Imidazoles”: their chemistry and pharmacological potentials. Int J PharmTech Res 3:268–282
Bhatt HG, Agrawal YK, Raval HG, Manna K, Desai PR (2010) Histamine H4 receptor: a novel therapeutic target for immune and allergic responses. Mini Rev Med Chem 10:1293–1308
Bielory L, Lien KW, Bigelsen S (2005) Efficacy and tolerability of newer antihistamines in the treatment of allergic conjunctivitis. Drugs 65:215–228
Biron KK, Harvey RJ, Chamberlain SC, Good SS, Smith AA III, Davis MG, Talarico CL, Miller WH, Ferris R, Dornsife RE, Stanat SC, Drach JC, Townsend LB, Koszalka GW (2002) Potent and selective inhibition of human cytomegalovirus replication by 1263W94: a benzimidazole L-riboside with a unique mode of action. Antimicrob Agents Chemother 46:2365–2372
Black JW, Duncan WAM, Durant CJ, Ganellin CR, Parsons EM (1972) Definition and antagonism of histamine H2-receptors. Nature 236:385–390
Blum AL, Shah G, St Pierre T, Helander HF, Sung CP, Wiebelhaus VD, Sachs G (1971) Properties of soluble ATPase of gastric mucosa. Biochim Biophys Acta 249:101–111
Brimblecombe RW, Duncan WA, Durant GJ, Emmett JC, Ganellin CR, Leslie GB, Parsons ME (1978) Characterization and development of cimetidine as a histamine H2-receptor antagonist. Gastroenterology 74:339–347
Brown HD, Matzuk AR, Ilves IR, Peterson LH, Harris SA, Sarett LH, Egerton JR, Yakstis JJ, Campbell WC, Cuckler AC (1961) Antiparasitic drugs. IV. 2-(4'-Thiazolyl)-benzimidazole, a new anthelmintic. J Am Chem Soc 83:1764–1765
Burgess MA, Bodey GP (1972) Clotrimazole (Bay b 5097): in vitro and clinical pharmacological studies. Antimicrob Agents Chemother 2:423–426
Burnier M (2001) Angiotensin II type 1 receptor blockers. Circulation 103:904–912
Burnier M, Brunner HR (2000) Angiotensin II receptor antagonists. Lancet 355:637–645
Butler A, Hill JM, Ireland SJ, Jordan CC, Tyers MB (1988) Pharmacological properties of GR38032F, a novel antagonist at 5-HT3 receptors. Br J Pharmacol 94:397–412
Carini DJ, Duncia JV, Aldrich PE, Chiu AT, Johnson AL, Pierce ME, Price WA, Santella JB III, Wells GJ, Wexler RR, Wong PC, Yoo S, Timmermans PBMWM (1991) Nonpeptide angiotensin II receptor antagonists: the discovery of a series of N-(biphenylylmethyl)imidazoles as potent, orally active antihypertensives. J Med Chem 34:2525–2547
Chang H, Saccomani G, Rabon E, Schackmann R, Sachs G (1977) Proton transport by gastric membrane vesicles. Biochim Biophys Acta 464:313–327
Chey WD, Cash BD (2005) Cilansetron: a new serotonergic agent for the irritable bowel syndrome with diarrhea. Expert Opin Investig Drugs 14:185–193
Chodosh LA, Fire A, Samuels M, Sharp PA (1989) 5,6-Dichloro-1-beta-D- ribofuranosylbenzimidazole inhibits transcription elongation by RNA polymerase II in vitro. J Biol Chem 264:2250–2257
Clapp RH, Luckman SM (2012) Proxyfan acts as a neutral antagonist of histamine H3 receptors in the feeding-related hypothalamic ventromedial nucleus. Br J Pharmacol 167:1099–1110
Clarke RW, Harris J (2002) RX 821002 as a tool for physiological investigation of alpha(2)- adrenoceptors. CNS Drug Rev 8:177–192
Cooper DS (1984) Antithyroid drugs. N Engl J Med 311:1353–1362
Corcostegui R, Labeaga L, Innerarity A, Berisa A, Orjales A (2005) Preclinical pharmacology of bilastine, a new selective histamine H1 receptor antagonist: receptor selectivity and in vitro antihistaminic activity. Drugs RD 6:371–384
Coruzzi G, Adami M, Guaita E, De Esch IJ, Leurs R (2007) Anti-inflammatory and antinociceptive effects of the selective histamine H4-receptor antagonists JNJ7777120 and VUF6002 in a rat model of carrageenan-induced acute inflammation. Eur J Pharmacol 563:240–244
Cosar C, Julou L (1959) The activity of 1-(2-hydroxyethyl)-2-methyl-5-nitroimidazole (R.P. 8823) against experimental Trichomonas vaginalis infections. Ann Inst Pasteur 96:238–241
DeRemer DL, Katsanevas K, Ustun C (2011) Critical appraisal of nilotinib in frontline treatment of chronic myeloid leukemia. Cancer Manag Res 3:65–78
DeSimone RW, Currie KS, Mitchell SA, Darrow JW, Pippin DA (2004) Privileged structures: applications in drug discovery. Comb Chem High T Scr 7:473–494
Diacon AH, Dawson R, Groote-Bidlingmaier F, Symons G, Venter A, Donald PR, Niekerk C, Everitt D, Hutchings J, Burger DA, Schall R, Mendel CM (2015) Bactericidal activity of pyrazinamide and clofazimine alone and in combinations with pretomanid and bedaquiline. Am J Respir Crit Care Med 191:943–953
DoCampo R (1990) Sensitivity of parasites to free radical damage by antiparasitic drugs. Chem Biol Interact 73:1–27
Elizabeth B, Lurie P, Wolfe SM (2000) Alosetron for irritable bowel syndrome. Lancet 356:2009
Emerson CR, Marzella N (2010) Dexlansoprazole: a proton pump inhibitor with a dual delayed- release system. Clin Ther 32:1578–1596
Fainstein V, Bodey GP (1980) Cardiorespiratory toxicity due to miconazole. Ann Intern Med 93:432–433
Fei F, Zhou Z (2013) New substituted benzimidazole derivatives: a patent review (2010–2012). Expert Opin Ther Pat 23:1157–1179
Fellenius E, Berglindh T, Sachs G, Olbe L, Elander B, Sjostrand S, Wallmark B (1981) Substituted benzimidazoles inhibit gastric acid secretion by blocking (H++K+) ATPase. Nature 290:159–161
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, Parkin DM, Forman D, Bray F (2015) Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer 136:E359–E386
Fernandez-Torres B, Inza I, Guarro J (2003) In vitro activities of the new antifungal drug eberconazole and three other topical agents against 200 strains of dermatophytes. J Clin Microbiol 41:5209–5211
Fisher MH (1986) Chemistry of antinematodal agents. In: Campbell WC, Rew RS (eds) Chemotherapy of parasitic diseases. Plenum Press, New York, pp 239–266
Freston JW (1982) Cimetidine. I. developments, pharmacology, and efficacy. Ann Intern Med 97:573–580
Fromtling RA (1986) Butoconazole: a new antifungal agent. Rev Recent Work. Drugs Today 22:261–263
Fromtling RA (1988) Overview of medically important antifungal azole derivatives. Clin Microbiol Rev 1:187–217
Gaba M, Singh D, Singh S, Sharma V, Gaba P (2010) Synthesis and pharmacological evaluation of novel 5-substituted-1-(phenylsulphonyl)-2-methylbenzimidazole derivatives as anti- inflammatory and analgesic Agents. Eur J Med Chem 45:2245–2249
Gaba M, Singh S, Mohan C (2014) Benzimidazole: an emerging scaffold for analgesic and anti- inflammatory agents. Eur J Med Chem 76:494–505
Gaba M, Gaba P, Uppal D, Dhingra N, Bahia MS, Silakari O, Mohan C (2015) Benzimidazole derivatives: search for GI-friendly anti-inflammatory analgesic agents. Acta Pharm Sin B 5:337–342
Gaddum JH, Picarelli ZP (1957) Two kinds of tryptamine receptor. Br J Pharmacol Chemother 12:323–328
Gerra G, Zaimovic A, Giusti F, Gennaro CD, Zambelli U, Gardini S, Delsignore R (2001) Lofexidine versus clonidine in rapid opiate detoxification. J Subst Abuse Treat 21:11–17
Gewurz BE, Jacobs M, Proper JA, Dahl TA, Fujiwara T, Dezube BJ (2004) Capravirine, a nonnucleoside reverse-transcriptase inhibitor in patients infected with HIV-1: a phase 1 study. J Infect Dis 190:1957–1961
Geyer R, Buschauer A (2011) Synthesis and histamine H3 and H4 receptor activity of conformationally restricted cyanoguanidines related to UR-PI376. Arch Pharm 344:775–785
Giese JL, Stanley TH (1983) Etomidate: a new intravenous anesthetic induction agent. Pharmacotherapy 3:251–258
Godefroi EF, Heeres J, Van Cutsem J, Janssen PA (1969) The preparation and antimycotic properties of derivatives of 1-phenethylimidazole. J Med Chem 12:784–791
Gordon SG, Miller MW, Saunders AB (2006) Pimobendan in heart failure therapy-a silver bullet. J Am Anim Hosp Assoc 42:90–93
Grasso CS, Wu YM, Robinson DR, Cao X, Dhanasekaran SM, Khan AP, Quist MJ, Jing XJ, Lonigro RJ, Brenner JC, Asangani IA, Ateeq B, Chun SY, Siddiqui J, Sam L, Anstett M, Mehra R, Prensner JR, Palanisamy N, Ryslik GA, Vandin F, Raphael BJ, Lakshmi PK, Rhodes DR, Pienta KJ, Chinnaiyan AM, Tomlins SA (2012) The mutational landscape of lethal castration-resistant prostate cancer. Nature 487:239–243
Griffith RK (2003) Adrenergics and adrenergic-blocking agents. In: Abraham DJ (ed) Burger’s medicinal chemistry and drug discovery. Wiley, Hoboken, pp 1–37
Hartmann M, Zimmer CH (1972) Investigation of cross-link formation in DNA by the alkylating cytostatica IMET 3106, 3393 and 3943. Biochim Biophys Acta 287:386–389
Hauel NH, Nar H, Priepke H, Ries U, Stassen JM, Wienen W (2002) Structure-based design of novel potent nonpeptide thrombin inhibitors. J Med Chem 45:1757–1766
Hawwa AF, Millership JS, Collier PS, Vandenbroeck K, McCarthy A, Dempsey S, Cairns C, Collins J, Rodgers C, McElnay JC (2008) Pharmacogenomic studies of the anticancer and immunosuppressive thiopurines mercaptopurine and azathioprine. Br J Clin Pharmacol 66:517–528
Heel RC, Brogden RN, Parke GE, Speight TM, Avery GS (1980) Miconazole: a preliminary review of its therapeutic efficacy in systemic fungal infections. Drugs 19:7–30
Heeres J, Backx LJ, Mostmans JH, Van Cutsem J (1979) Antimycotic imidazoles. Part 4. Synthesis and antifungal activity of ketoconazole, a new potent orally active broad- spectrum antifungal agent. J Med Chem 22:1003–1005
Heinz BA, Vance LM (1995) The antiviral compound enviroxime targets the 3A coding region of rhinovirus and poliovirus. J Virol 69:74189–74197
Herling AW, Weidmann K (1994) Progress in medicinal chemistry. In: Ellis GP, Luscombe DK (ed) Gastric H+/K+ATPase inhibitors. Elsevier Science BV, pp 233–264
Hernandez Molina JM, Llosa J, Martinez Brocal A, Ventosa A (1992) In vitro activity of cloconazole, sulconazole, butoconazole, isoconazole, fenticonazole, and five other antifungal agents against clinical isolates of Candida albicans and Candida spp. Mycopathalogia 118:15–21
Hoff DR (1982) In: Bindra JS, Lednicer D (eds) Chronicles of drug discovery. Wiley, New York, pp 239–256
Hoff DR, Fisher MH, Bochis RJ, Lusi RJ, Waksmunski A, Egerton RJ, Yastis JJ, Cuckler AC, Campbell WC (1970) A new broad spectrum anthelmintic: 2-(4-thiazolyl)-iso- propoxycarbonyl aminobenzimidazole. Experientia 26:550–552
Hough LB (2001) Genomics meets histamine receptors: new subtypes, new receptors. Mol Pharmacol 59:415–419
http://www.healthline.com/health/parasitic-infections#Overview1
http://www.lef.org/protocols/infections/fungal_infections_candida_01.htm
http://www.dddmag.com/news/2012/08/ferrer-files-arasertaconazole-ind
Igel P, Dove S, Buschauer A (2010) Histamine H4 receptor agonists. Bioorg Med Chem Lett 20:7191–7199
Ingle RG, Magar DD (2011) Heterocyclic chemistry of benzimidazoles and potential activities of derivatives. Int J Drug Res Tech 1:26–32
Insel PA (1996) Adrenergic receptors-evolving concepts and clinical implications. N Engl J Med 334:580–585
Ishikawa H (1999) Mizoribine and mycophenolate mofetil. Curr Med Chem 6:575–597
Jansen FP, Wu TS, Voss HP, Steinbusch HW, Vollinga RC, Rademaker B, Bast A, Timmerman H (1994) Characterization of the binding of the first selective radiolabelled histamine H3-receptor antagonist, 125I-iodophenpropit, to rat brain. Br J Pharmcol 113:355–362
Jansen FP, Mochizuki T, Maeyama K, Leurs R, Timmerman H (2000) Characterization of histamine H3 receptors in mouse brain using the H3 antagonist 125Iiodophenpropit. Naunyn-Schmiedeberg Arch Pharmacol 362:60–67
Janssen PA, Niemegeers CJ, Schellekens KH, Marsboom RH, Herin VV, Amery WK, Admiraal PV, Bosker JT, Crul JF, Pearce C, Zegveld C (1971) Bezitramide (R 4845), a new potent and orally long-acting analgesic compound. Arzneim Forsch 21:862–867
Jarrad AM, Karoli T, Blaskovich MAT, Lyras D, Coope MA (2015) Clostridium difficile drug pipeline: challenges in discovery and development of new agents. J Med Chem 58:5164–5185
Jerchel D, Fischer H, Fracht M (1952) Zur Darstellung der benzimidazole. Liebigs Ann Chem 575:162–173
Jevons S, Gymer GE, Brammer KW, Cox DA, Leeming MRG (1979) Antifungal activity of tioconazole (UK-20, 349), a new imidazole derivative. Antimicrob Agents Chemother 15:597–602
Johns TG, Piper DC, James GW (1979) The pharmacological profile of a potential hypnotic compound RU 31158. Arch Int Pharmacodyn Ther 240:53–65
Jones CD, Andrews DM, Barker AJ, Blades K, Daunt P, East S, Geh C, Graham MA, Johnson KM, Loddick SA, McFarland HM, McGregor A, Moss L, Rudge DA, Simpson PB, Swain ML, Tam KY, Tucker JA, Walker M (2008) The discovery of AZD5597, a potent imidazole pyrimidine amide CDK inhibitor suitable for intravenous dosing. Bioorg Med Chem Lett 18:6369–6373
Josephy PD, Palcic B, Skarsgard LD (1981) In vitro metabolism of misonidazole. Br J Cancer 43:443–450
Kapetanovic IM, Kupferberg HJ (1984) Nafimidone, an imidazole anticonvulsant, and its metabolite as potent inhibitors of microsomal metabolism of phenytoin and carbamazepine. Drug Metab Dispos 12:560–564
Kapoor VK, Chadha R, Venisetty PK, Prasanth S (2003) Medicinal significance of nitroimidazoles: some recent advances. J Sci Ind Res 62:659–665
Kath R, Blumenstengel K, Fricke HJ, Hoffken K (2001) Bendamustine monotherapy in advanced and refractory chronic lymphocytic leukemia. J Cancer Res Clin Oncol 127:48–54
Kemp KM, Henderlight L, Neville M (2008) Pre-cedex: is it the future of cooperative sedation? Crit Care Insider 38:50–55
Khabnadideh S, Rezaei Z, Khalafi NA, Motazedian MH, Eskandari M (2007) Synthesis of metronidazole derivatives as antigiardiasis agents. DARU J Pharm Sci 15:17–20
Kitbunnadaj R, Zuiderveld OP, Christophe B, Hulscher S, Menge WM, Gelens E, Snip E, Bakker RA, Celanire S, Gillard M, Talaga P, Timmerman H, Leurs R (2004) Identification of 4-(1H-imidazol-4(5)-ylmethyl)pyridine (immethridine) as a novel, potent, and highly selective histamine H(3) receptor agonist. J Med Chem 47:2414–2417
Kohara Y, Kubo K, Imamiya E, Wada T, Inada Y, Naka T (1996) Synthesis and angiotensin II receptor antagonistic activities of benzimidazole derivatives bearing acidic heterocycles as novel tetrazole bioisosteres. J Med Chem 39:5228–5235
Kromer W (1995) Similarities and differences in the properties of substituted benzimidazoles: a comparison between pantoprazole and related compounds. Digestion 56:443–454
Kupietzky A, Houpt MI (1993) Midazolam: a review of its use for conscious sedation of children. Pediatr Dent 15:237–241
Leurs R, Bakker RA, Timmerman H, de Esch IJ (2005) The histamine H3 receptor: from gene cloning to H3 receptor drugs. Nat Rev Drug Discov 4:107–120
Li EC, Davis LE (2003) Zoledronic acid: a new parenteral bisphosphonate. Clin Ther 25:2669–2708
Lindberg P, Carlsson E (2006) Analogue-based drug discovery. In: Fischer J, Ganellin CR (eds) Esomeprazole in the framework of proton-pump inhibitor development. Wiley-VCH Verlag, Weinheim, pp 81–113
Lutwick L, Rytel MW, Yanez JP, Galgiani JN, Stevens DA (1979) Deep infections from Petriellidium boydii treated with miconazole. J Am Med Assoc 241:271–272
Martin RJ (1997) Modes of action of anthelmintic drugs. Vet J 154:11–34
McCracken RO, Lipkowitz KB (1990) Structure-activity relationships of benzothiazole and benzimidazole anthelmintics: a molecular modeling approach to in vivo drug efficacy. J Parasitol 76:853–864
McFarland JW (1972) The chemotherapy of intestinal nematodes. Prog Drug Res 16:157–193
Miura S, Okabe A, Matsuo Y, Karnik SS, Saku K (2013) Unique binding behavior of the recently approved angiotensin II receptor blocker azilsartan compared with that of condensation. Hypertens Res 36:134–139
Morris STW, Reid JL (1997) Moxonidine: a review. J Hum Hypertens 11:629–635
Motawaj M, Arrang JM (2011) Ciproxifan, a histamine H3-receptor antagonist / inverse agonist, modulates methamphetamine-induced sensitization in mice. Eur J Neurosci 33:1197–1204
Munson K, Garcia R, Sachs G (2005) Inhibitor and ion binding sites on the gastric H, K- ATPase. Biochemistry 44:5267–5284
Naik P, Murumkar P, Giridhar R, Yadav MR (2010) Angiotensin II receptor type 1 (AT1) selective nonpeptidic antagonists-a perspective. Bioorg Med Chem 18:8418–8456
Nakamura S (1955) Structure of azomycin, a new antibiotic. Pharm Bull 3:379–383
Nakata-Fukuda M, Hirata T, Keto Y, Yamano M, Yokoyama T, Uchiyama Y (2014) Inhibitory effect of the selective serotonin 5-HT3 receptor antagonist ramosetron on duodenal acidification-induced gastric hypersensitivity in rats. Eur J Pharmacol 15:88–92
Narasimhan B, Sharma D, Kumar P (2011) Biological importance of imidazole nucleus in the new millennium. Med Chem Res 20:1119–1140
Nimura K, Niwano Y, Ishiduka S, Fukumoto R (2001) Comparison of in vitro antifungal activities of topical antimycotics launched in 1990s in Japan. Int J Antimicrob Agents 18:173–178
Njar VC, Brodie AM (2015) Discovery and development of Galeterone (TOK-001 or VN/124-1) for the treatment of all stages of prostate cancer. J Med Chem 58:2077–2087
Ogata M, Matsumoto H, Hamada Y, Takehara M, Tawara K (1983) 1-[1-[2-[(3-chlorobenzyl) oxy] phenyl] vinyl]-1H-imidazole hydrochloride, a new potent antifungal agent. J Med Chem 26:768–770
Olbe L, Carlsson E, Lindberg P (2003) A proton-pump inhibitor expedition: the case histories of omeprazole and esomeprazole. Nat Rev Drug Discov 2:132–139
Ortiz JA (1992) Sertaconazole (FI-7045). A new antifungal agent. Arzneim Forsch 42:689–690
Ozkay Y, Tunali Y, Karaca H, Isikdag I (2010) Antimicrobial activity and a SAR study of some novel benzimidazole derivatives bearing hydrazone moiety. Eur J Med Chem 45:3293–3298
Palacin C, Tarrago C, Agut J, Guglietta A (2001) In vitro activity of sertaconazole, ketoconazole, fenticonazole, clotrimazole and itraconazole against pathogenic vaginal yeast infections. Methods Find Exp Clin Pharmacol 23:61–64
Parsons ME, Ganellin CR (2006) Histamine and its receptors. Br J Pharmacol 147:S127–S135
Pectasides D, Yianniotis H, Alevizakos N, Bafaloukos D, Barbounis V, Varthalitis J, Dimitriadis M, Athanassiou A (1989) Treatment of metastatic malignant melanoma with dacarbazine, vindesine and cisplatin. Br J Cancer 60:627–629
Penning TD, Zhu GD, Gandhi VB, Gong J, Liu X, Shi Y, Klinghofer V, Johnson EF, Donawho CK, Frost DJ, Bontcheva-Diaz V, Bouska JJ, Osterling DJ, Olson AM, Marsh KC, Luo Y, Giranda VL (2009) Discovery of the Poly(ADP-ribose) polymerase (PARP) inhibitor 2-[(R)- 2-methylpyrrolidin-2-yl]-1H-benzimidazole-4-carboxamide (ABT-888) for the treatment of cancer. J Med Chem 52:514–523
Pertovaara A, Haapalinna A, Sirvio J, Virtanen R (2005) Pharmacological properties, central nervous system effects, and potential therapeutic applications of atipamezole, a selective alpha2-adrenoceptor antagonist. CNS Drug Rev 11:273–288
Plempel M, Regel E, Buchel KH (1983) Antimycotic efficacy of bifonazole in vitro and in vivo. Arzneimittelforschung 33:517–524
Polak A (1982) Oxiconazole, a new imidazole derivative. Evaluation of antifungal activity in vitro and in vivo. Arzneimittelforschung 32:17–24
Prakash A, Lamb HM (1998) Mizolastine: a review of its use in allergic rhinitis and chronic idiopathic urticaria. BioDrugs 10:41–63
Raats JI, Falkson G, Falkson HC (1992) A study of fadrozole, a new aromatase inhibitor, in postmenopausal women with advanced metastatic breast cancer. J Clin Oncol 10:111–116
Rabasseda X (2002) Ramosetron, a 5-HT3 receptor antagonist for the control of nausea and vomiting. Drugs Today 38:75–89
Radziszewski B (1882) Ueber die Constitution des Lophins und verwandter Verbindungen. Chem Ber 15:1493–1496
Ren J, Nichols C, Bird LE, Fujiwara T, Sugimoto H, Stuart DI, Stammers DK (2000) Binding of the second generation nonnucleoside inhibitor S-1153 to HIV-1 reverse transcriptase involves extensive main chain hydrogen bonding. J Biol Chem 275:14316–14320
Rezaei Z, Khabnadideh S, Zomorodian K, Pakshir K, Kashi G, Sanagoei N, Gholami S (2011) Design, synthesis and antifungal activity of some new imidazole and triazole derivatives. Arch Pharm Chem Life Sci 344:658–665
Sachs G, Wallmark B (1989) The gastric H+, K+-ATPase: the site of action of omeprazole. Scand J Gatroenterol 66:3–11
Sachs G, Collier RH, Schoemaker RL, Hirschowitz BI (1968) The energy source of gastric acid secretion. Biochim Biophys Acta 162:210–219
Sachs G, Shin JM, Vagin O, Lambrecht N, Yakubov I, Munson K (2007) The gastric H, K ATPase as a drug target. J Clin Gastroenterol 41:S226–S242
Sander K, Kottke T, Stark H (2008) Histamine H3 receptor antagonists go to clinics. Biol Pharm Bull 31:2163–2181
Savic I, Widen L, Stone-Elander S (1991) Feasibility of reversing benzodiazepine tolerance with flumazenil. Lancet 337:133–137
Savola JM, Hill M, Engstrom M, Merivuori H, Wurster S, McGuire SG, Fox SH, Crossman AR, Brotchie JM (2003) Fipamezole (JP-1730) is a potent alpha2 adrenergic receptor antagonist that reduces levodopa-induced dyskinesia in the MPTP-lesioned primate model of parkinson’s disease. Mov Disord 18:872–883
Sawyer PR, Brogden RN, Pinder RM, Speight TM, Avery (1975) Clotrimazole: a review of its antifungal activity and therapeutic efficacy. Drugs 9:424–447
Scarpignato C, Hunt RH (2008) Proton pump inhibitors: the beginning of the end or the end of the beginning? Curr Opin Pharmacol 8:677–684
Scheinfeld N (2003) Cimetidine: a review of the recent developments and reports in cutaneous medicine. Dermatol Online J 9:4
Schimke K, Davis TM (2007) Drug evaluation: rivoglitazone, a new oral therapy for the treatment of type 2 diabetes. Curr Opin Investig Drugs 8:338–344
Senn-Bilfinger J, Sturm E (2006) Analogue-based drug discovery. In: Fischer J, Ganellin CR (eds) The development of a new proton-pump inhibitor: The case history of pantoprazole. Wiley-VCH Verlag, Weinheim, pp 115–136
Shadomy S (1971) In vitro antifungal activity of clotrimazole (Bay b 5097). Infect Immun 4:143–148
Sharma S (1990) Vector-borne diseases. Prog Drug Res 35:365–485
Sheehan DJ, Hitchcock CA, Sibley CM (1999) Current and emerging azole antifungal agents. Clin Microbiol Rev 12:40–79
Shin JM, Sachs G (2009) Long lasting inhibitors of the gastric H, K-ATPase. Expert Rev Clin Pharmacol 2:461–468
Shin JM, Munson K, Vagin O, Sachs G (2008) The gastric H+-K-ATPase: structure, function, and inhibition. Pflug Arch Eur J Phy 457:609–622
Shinn DLS (1962) Metronidazole in acute ulcerative gingivitis. Lancet 279:1191
Singh M, Jadhav HR (2013) Histamine H3 receptor function and ligands: recent developments. Mini Rev Med Chem 13:47–57
Spasov AA, Yozhitsa IN, Bugaeva LI, Anisimova VA (1999) Benzimidazole derivatives: spectrum of pharmacological activity and toxicological properties. Pharm Chem J 33:232–243
Stahle H (2000) A historical perspective: development of clonidine. Baillieres Clin Anaesthesiol 14:237–246
Stark H (2003) Recent advances in histamine H3/H4 receptor ligands. Expert Opin Ther Pat 13:851–865
Stringer A, Wright MA (1976) The toxicity of benomyl and some related 2-substituted benzimidazoles to the earthworm Lumbricus terrestris. Pest Sci 7:459–464
Sun L, Li D, Dong X, Yu H, Dong JT, Zhang C, Lu X, Zhou J (2008) Small-molecule inhibition of Aurora kinases triggers spindle checkpoint-independent apoptosis in cancer cells. Biochem Pharmacol 75:1027–1034
Tageja N, Nagi J (2010) Bendamustine: something old, something new. Cancer Chemother Pharmacol 66:413–423
Tajana A, Sibilia C, Cappelletti R, Cova A, Nardi D (1981) Physico-chemical, structural and analytical studies on fenticonazole, a new drug with antimycotic properties. Arzneim Forsch 31:2127–2133
Tarral A, Blesson S, Mordt OV, Torreele E, Sassella D, Bray MA, Hovsepian L, Evene E, Gualano V, Felices M, Strub-Wourgaft N (2014) Determination of an optimal dosing regimen for fexinidazole, a novel oral drug for the treatment of human African trypanosomiasis: first-in-human studies. Clin Pharmacokinet 53:565–580
Tettenborn D (1974) Toxicity of clotrimazole. Postgrad Med J 50:17–20
Thiele K, Zirngibl L, Pfenniger MH, Egli M, Dobler M (1987) Antimycotic imidazolyl-alkenes Synthesis and X-ray crystal structure of omoconazole. Helv Chim Acta 70:441–444
Thomas X, Elhamri M (2007) Tipifarnib in the treatment of acute myeloid leukemia. Biologics 1:415–424
Tiligada E, Zampeli E, Sander K, Stark H (2009) Histamine H3 and H4 receptors as novel drug targets. Expert Opin Invest Drugs 18:1519–1531
Townsendand LB, Wise DS (1990) The synthesis and chemistry of certain anthelmintic benzimidazoles. Parasitol Today 6:107–112
Uchida K, Nishiyama Y, Yamaguchi H (2004) In vitro antifungal activity of luliconazole (NND-502), a novel imidazole antifungal agent. J Infect Chemother 10:216–219
Unger T, Scholkens BA (ed), Angiotensin Vol. II, Maillard M, Burnier M, Clinical pharmacology of angiotensin II receptor antagonists, Springer:Berlin. (2004) pp 454–476
Upton AM, Cho S, Yang TJ, Kim Y, Wang Y, Lu Y, Wang B, Xu J, Mdluli K, Ma Z, Franzblau SG (2015) In vitro and in vivo activities of the nitroimidazole TBA-354 against Mycobacterium tuberculosis. Antimicrob Agents Chemother 59:136–144
Vahlquist A, Blockhuys S, Steijlen P, Van Rossem K, Didona B, Blanco D, Traupe H (2014) Oral liarozole in the treatment of patients with moderate/severe lamellar ichthyosis: results of a randomized, double-blind, multinational, placebo-controlled phase II/III trial. Br J Dermatol 170:173–181
Vanden Bossche H (1974) Biochemical effects of miconazole on fungi. Biochem Pharmacol 23:887–899
Varia MA, Calkins-Adams DP, Rinker LH, Kennedy AS, Novotny DB Jr, Fowler WC, Raleigh JA (1998) Pimonidazole: a novel hypoxia marker for complementary study of tumor hypoxia and cell proliferation in cervical carcinoma. Gynecol Oncol 71:270–277
Weide R (2008) Bendamustine HCL for the treatment of relapsed indolent non-Hodgkin’s lymphoma. Ther Clin Risk Manag 4:727–732
Wexler RR, Greenlee WJ, Irvin JD, Goldberg MR, Prendergast K, Smith RD, Timmermans PB (1996) Nonpeptide angiotensin II receptor antagonists: the next generation in antihypertensive therapy. J Med Chem 39:625–656
Woolley DW (1944) Some biological effects produced by benzimidazole and their reversal by purines. J Biol Chem 152:225–232
Wright JB (1951) The chemistry of the benzimidazoles. Chem Rev 48:397–541
Xavier AS, Lakshmanan M (2014) Delamanid: a new armor in combating drug-resistant tuberculosis. J Pharmacol Pharmacother 5:222–224
Yadav G, Ganguly S (2015) Structure activity relationship (SAR) study of benzimidazole scaffold for different biological activities: a mini-review. Eur J Med Chem 97:419–443
Yanagiasawa H, Amemiya Y, Kanazaki T, Shimoji Y, Fujimoto K, Kitahara Y, Sada T, Mizuno M, Ikeda M, Miyamoto S, Furukawa Y, Koike H (1996) Nonpeptide angiotensin II receptor antagonists: synthesis, biological activities, and structure-activity relationships of imidazole-5-carboxylic acids bearing alkyl, alkenyl, and hydroxyalkyl substituents at the 4-position and their related compounds. J Med Chem 39:323–338
Yanagisawa H, Koike H, Miura S (2012) Case studies in modern drug discovery and development. In: Huang X, Aslanian RG (eds) Olmesartan medoxomil: an angiotensin II receptor blocker. Wiley, USA, pp 46–64
Yang Y, Jin C, Li H, He Y, Liu Z, Bai L, Dou K (2012) Improved radiosensitizing effect of the combination of etanidazole and paclitaxel for hepatocellular carcinoma in vivo. Exp Ther Med 3:299–303
Yoshida H, Kasuga O, Yamaguchi T (1984) Studies on antifungal activities of sulconazole. Chemotherapy 32:477–484
Yu F, Bonaventure P, Thurmond RL (2010) Histamine in inflammation. In: Thurmond RL (ed) The future antihistamines: histamine H3 and H4 receptor ligands. Landes Bioscience. Springer, Berlin, pp 125–140
Zajac P, Holbrook A, Super ME, Vogt M (2013) An overview: current clinical guidelines for the evaluation, diagnosis, treatment, and management of dyspepsia. Osteopath Fam Physician 5:79–85
Zhou Z, Vorperian VR, Gong Q, Zhang S, January CT (1999) Block of HERG potassium channels by the antihistamine astemizole and its metabolites desmethyl astemizole and nor astemizole. J Cardiovasc Electrophysiol 10:836–843
Acknowledgments
The author(s) would like to acknowledge Punjab Technical University, Kapurthala, Punjab, India, and ASBASJSM College of Pharmacy, Bela, for providing an institutional research platform and necessary facilities. The authors would like to thank Mr. Sarbjot Singh, Senior Research Scientist at Panacea Biotec Ltd., for proof reading the manuscript and his constant support.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gaba, M., Mohan, C. Development of drugs based on imidazole and benzimidazole bioactive heterocycles: recent advances and future directions. Med Chem Res 25, 173–210 (2016). https://doi.org/10.1007/s00044-015-1495-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00044-015-1495-5