Abstract
Objectives
The objective is to determine association of age, gender, BMI, body image (body satisfaction, body appearance), depression, unhealthy weight control behaviors with smoking among Serbian adolescents and specifically association of these variables with smoking for weight control among adolescent smokers.
Methods
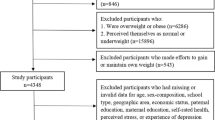
This is a secondary analysis of data collected from 2763 students aged 13–15 years old (49.9% boys; 50.1% girls) obtained through cross-sectional Health Behavior in School-aged Children Survey conducted in Serbia in 2018 and analyzed using multivariable logistic regression.
Results
In Serbia, 12.9% adolescents 13–15 years old smoke and 6.6% smoke for weight control, while this practice was present among 48.8% of the smokers. Higher odds of smoking were found among adolescents who perceive themselves thin and good looking, while these two factors didn’t play role for the smoking for weight control among smokers. Depression and unhealthy weight control behavior other than smoking significantly predicted smoking and smoking for weight control. Gender was not associated with smoking in adolescents, but among adolescent smokers, boys had two times higher chance compared to girls to report smoking for weight control.
Conclusions
Findings call for incorporating and strengthening interventions for adolescents’ weight control management and mental health as part of smoking prevention and cessation programs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adolescence is a period when many risk behaviors are established including smoking (National Center for Chronic Disease Prevention and Health Promotion 2012) and unhealthy dietary practices (Hazzard et al. 2017). Worldwide more than 340 million (18%) children and adolescents between 5 and 19 years of age are either overweight or obese (NCD Risk Factor Collaboration 2017) and approximately 10% of 13–15 years old adolescents smoke with significant differences between counties (Arrazola et al. 2017). High prevalence of these unhealthy behaviors represents a serious public health challenge and underline the necessity for continuous implementation of evidence-based interventions.
Co-occurrence of various risk factors which is repeatedly found in many studies (Charrier et al. 2019; Ellickson et al. 2001) is additional burden to adolescents’ health (Neumark-Sztainer et al. 1998). Tobacco use can be the first indication of adolescent problem behavior (Zullig et al. 2001) and smoking and unhealthy diet are also found to cluster which multiplies their negative effects (Larson et al. 2007; Strauss and Mir 2001; Forrest and Forrest 2008; Seo and Jiang 2009). Adolescent smokers more frequently tend to practice unhealthy diet compared to non-smokers (Krowchuk et al. 1998; Sim et al. 2017) with gender differences and other psychosocial factors mediating this association (Brown et al. 2015).
In recent decades, increase in different weight loss practices among adolescents has been noticed, not only due to increase in obesity prevalence, but also because adolescent’s tendency to look like their skinny idols (Daee et al. 2002).Instead of applying recommended professional advice aimed at losing weight, certain proportion of adolescents tend to practice unhealthy weight control measures including fasting, vomiting and laxative and diet pills use (Forrest and Forrest 2008) that are also associated with different psychological and physiological negative effects (Daee et al. 2002). In previous research gender (Croll et al. 2002) and poor body image (Boutelle et al. 2002) were found to correlate with unhealthy dieting behaviors.
One of the unhealthy practices for losing weight is smoking which is noticed among both genders (Fulkerson and French 2003). While association between belief of smoking as a weight-control strategy and smoking is well documented (Camp et al. 1993; Cavallo et al. 2006), less is known about other characteristics of adolescents using smoking as weight control behavior. Available studies that provide insight into association between smoking and dieting originate mostly from Americas (Forrest and Forrest 2008) and Asia (Sim et al. 2017) and to lesser extent from Europe (Penzes et al. 2012), but there is lack of such studies in the Western Balkans and more specifically in Serbia which is one of the most populated countries in this region. With almost every fifth adolescent 15 years old being smoker, Serbia is above average current smoker prevalence of other 2017/2018 HBSC participating countries (Inchley et al. 2020). Given the high prevalence of smoking in Serbia it is of importance to identify all correlates that contribute to the burden of smoking, especially its co-occurrence with other risk behaviors.
More specifically, aim of the study was to determine prevalence of smoking for weight control among adolescents and separately among adolescent smokers and to explore the association of age, gender, BMI, body image (body satisfaction, body appearance), depression, unhealthy weight control behavior with smoking as well as association of these variables with smoking for weight control.
Methods
Sample and procedures
Data for this study were obtained from the 2017/2018 Health Behavior in School-aged Children Survey (HBSC) in Serbia that was conducted by the Institute of Public Health of Serbia “Dr Milan Jovanovic Batut”. HBSC is a collaborative cross-sectional study, conducted every 4 years in Europe and North America. The study population included nationally representative sample of 11, 13- and 15-years old primary and secondary school students (henceforth referred to as adolescents). A stratified, multistage sampling approach was used for the sample selection. Independent samples were selected for each of the age groups. Data were collected using anonymous, self-administered questionnaires based on standardized HBSC methodology which is described elsewhere (Roberts et al. 2009; Inchley 2018). Data collection was performed after the permissions from the schools and informed consent of the parents and adolescents. Survey included 4028 adolescents from 101 schools in Serbia. The response rate was 86.3% for schools and 86.1% for adolescents, respectively. In this secondary analysis we used data collected from adolescents of the national seventh grade of primary school and first grade of secondary school (13- and 15-years old students) as only they were asked about weight control behavior. In total, in this analysis we included 2763 adolescents (49.9% boys and 50.1% girls) aged 13–15 years (mean ± standard deviation 14.8 ± 1.0 age). Approval for the HBSC study in Serbia was obtained from the Ethical Review Board of the Institute of Public Health of Serbia.
Measures
Our main outcome variables were smoking status among adolescents and smoking more for weight control among adolescent smokers. We defined smokers as adolescents who smoked at least once in the past 30 days.
We analyzed the association of age, gender, BMI, body image (body satisfaction, body appearance), depression, unhealthy weight control behavior with smoking (smoking at least once in the past 30 day vs not smoking) in whole sample as well as association of these variables with smoking for weight control (smoking for weigh control vs. smoking without this intention) among smokers.
Our independents variables were gender, grade, socio-economic status, body mass Index (BMI) body image (physical appearance and perceived body weight), depression and unhealthy weight control behavior.
Since adolescents in one grade can be of different age and they are socializing with their peers from the class, grade was chosen as demographic variable over the age.
Socio-economic status was assessed based on the family affluence scale. Responses related to car ownership, computer ownership, having an own bedroom, number of bathrooms, having dishwasher, and number of family travels outside the country per year were scored and summed to form a Family Affluence Scale summary score (FAS) (Currie et al. 2008). The outcome categories used in our analyses were: (1) low affluence; (2) medium affluence and (3) high affluence.
Body mass index (BMI = kg/m2) was calculated based on self-reported weight (kg) and height (m) then compared against the age- and gender-distribution of BMI in adolescence using IOTF cut-offs (Cole and Lobstein 2012). Adolescents were classified in three categorical variables as underweight, normal weight and overweight (including obese).
Self-perceived body dissatisfaction included the following answers on the question “Do you think your body is……..? with following answer categories: much too thin, a bit too thin, about the right size, a bit too fat and much too fat that were collapsed into three categorical variables: underweight (much too thin, a bit too thin); (2) normal weight (about the right size) and (3) overweight/obese (a bit too fat and much too fat).
Self-perceived physical appearance included the following answer categories: very good looking, quite good looking, about average, not very good looking and not at all good looking for the question” Do you think you are…? “that were grouped into three categories: (1) Very/quite good looking; (2) Average good looking and (3) Not very/not at all good looking.
Depression was estimated based on score obtained with the Short Depression Scale (Center for Epidemiologic Studies Short Depression Scale (CES-D-R 10) (Bradley et al. 2010) for assessing symptoms of depression. Adolescents indicated if they had felt in a specific way during the past week ((1) were bothered by things that usually don't bother them; (2) had trouble keeping their mind on what he/she was doing; (3) felt depressed; (4) felt that everything he/she did was an effort; (5) felt hopeful about the future; (6) felt fearful; (7) had restless sleep; (8) were happy; (9) felt lonely; (10) could not “get going”). Answer categories were: Rarely or none of the time (less than 1 day) coded as 0; Some or a little of the time (1–2 days) coded as 1; Occasionally or a moderate amount of time (3–4 days) coded as 2; All of the time (5–7 days) coded 3. Exemption for coding was made for questions 5 and 8 that were coded in opposite direction (i.e. rarely or none of the time/less than 1 day was coded as 3, while all of the time was coded as 0). The total score was calculated by summing up the 10 items. A score of 10 or higher out of 30 was the cut-off for clinically significant depressive symptoms. In analysis we used categorical variable: depressed and not depressed.
Weight control behaviour were assessed by question “Which of the following things did you do to control your weight during the last 12 months?” which is included in the HBSC protocol and is recommended for 13 and 15-years-olds only. Item provides a list of techniques used to reduce body weight, namely exercising, skipping meals, fasting (i.e. to go without eating for 24 h or more), eating less sweets, eating less fat, drinking fewer soft drinks, eating less (i.e. smaller amounts of food), eating more fruit and/or vegetables, drinking more water, restricting diet to one or more food groups, vomiting, use diet pills or laxatives, smoking more, dieting under the supervision of a professional. We selected unhealthy weight control behaviors (UWCB)(skipping meals, fasting, restricting diet to one or more food groups, laxative and diet pill use and vomiting after meals and smoking more). These UWCB were further grouped into the less extreme unhealthy weight control measures (including restricting diet to one or more food groups, skipping meals and fasting) and extreme weight control measures (including vomiting, using laxative/diet pills and smoking). In logistic regressions we used variable which included extreme weight control measures other than smoking (vomiting and laxative/diet pills).
Statistical analysis
We used descriptive statistics for presenting prevalence of all explored variables in total sample, among smokers and among those smoking for weight control.
We performed bi-variable analyses to calculate unadjusted odds ratios for each independent variable (gender, grade, FAS, BMI, depression, perceived body weight, perceived physical appearance, unhealthy weight control behaviors) for smoking as outcome variable and separately only for smokers with smoking for weight control as outcome.
For calculating Adjusted Odds Ratio (OR) we built multivariable regression models using Enter method.
As we did not confirm any significant interaction of gender with independent variables, we omitted it from further analysis. Variables were entered into three steps. All models were controlled for gender, grade and FAS. As a core model we used one with the Body Mass Index, Self-perceived body weight, self perceived physical appearance, depression, less extreme and extreme weight control behaviours. The models were evaluated for goodness of fit with the Hosmer–Lemeshow test and likelihood -ratio chi square. We assumed as statistically significant findings with a p value < 0.05. All statistical analyses were performed using SPSS version 22.0 software (SPSS Inc., Chicago, IL, USA).
Results
Total sample included 2763 adolescents from the seventh grade of primary school (42.2%, mean age ± standard deviation 13.7 ± 0.3) and the first grade of secondary school (57.5%%, mean age ± standard deviation 15.7 ± 0.3 age). In total sample there were 12.9% smokers. Majority of adolescents had normal weight (71.3%), perceived themselves as average looking (73.0%), but on the other majority (58.3%) thought they are much or a bit too thin. More than one fifth of adolescents (21.4%) were screened as depressed and 37.7% practiced at least one unhealthy weight control behavior. Almost same percentage of adolescent reported fasting (6.6%), vomiting (6.4%) and smoking (6.6%) for weight control. More than half smokers (50.9%) smoked more for weight control. Among smokers, more than half (58.8%) of those who suffer from depression smoke for weight control.
Results of multivariable logistic regression with smoking as dependent variable show that being older (OR/95% CI 7.40/ 4.99–10.99), perceive an own body weight as much or a bit too thin (OR/95% CI 1.57/ 1.17–2.10), perceive own physical appearance as very or quite good looking (OR/95% CI 1.74/1.15–2.63), being depressed (OR/95% CI 1.98/ 11.48–2.66), and reporting less extreme (OR/95% CI 1.89/1.44–2.49) or extremely unhealthy weight control (OR/95% CI 2.68/1.81–3.98) increased the chance to smoke at least once in past 30 days among adolescents. We did not prove a significant association of gender or family affluence with smoking status. Moreover, being overweight or obese was significantly associated with smoking status only in crude model, and the significant association of reporting self-perceived physical appearance as not very or not at all good looking with smoking status disappeared after adding weight control variables into the model.
Multivariable logistic regression of factors associated with smoking for weight control among smokers showed that being a girl reduced (OR/95% CI 0.49/0.28–0.85), while being older (OR/95% CI 5.63/2.12–14.98), being depressed (OR/95% CI 1.93/1.11–3.36), and reporting less extreme (OR/95% CI 2.86/1.67–4.91), or extremely unhealthy weight control other than smoking (OR/95% CI 2.95/1.38–6.30), increased the chance to smoke for weight control among smoking adolescents. The association of gender with smoking for weight control was significant only after adding depression into the model. We did not prove a significant association of family affluence, and self-perceived body weight with smoking for weight control. Moreover, being overweight or obese and perceiving own physical appearance as not very or not at all good looking significantly increased the chance for smoking for weight control only in crude models.
Discussion
The aim of our study was to determine prevalence of smoking for weight control among total sample of Serbian adolescents and specifically among smokers. We also explored association of body image, depression and unhealthy weight control behavior with smoking and specifically with smoking for weight reduction among Serbian adolescents.
Among 13–15 years old adolescents, 12.9% smoke, 6.6% practice smoking as weight control behavior while this practice was present among more than half of the smokers.
Being older, reporting depression and unhealthy weight control behaviours was associated with smoking in adolescents as well as with smoking for weight control in smoking adolescents, but neither family affluence, nor BMI were associated with higher odds for smoking or smoking for weight control. Body image was associated with smoking, but not with smoking for weight control. Adolescents reporting being thin or good looking have higher odds for smoking in comparison to those who reported to have perceived their weight as about right and their physical appearance as about average.
Gender was not associated with smoking in adolescents but was associated with smoking for weight control in smoking adolescents, e.g. among smokers, boys has two times higher chance in comparison to girls to report smoking for weight control.
These findings confirm there are no gender differences in smoking status among Serbian adolescents which was also found in other school-based surveys in Serbia (Kilibarda et al. 2019). However, unlike other research (Sim et al. 2017) boys but not girls had twice higher chance to smoke for weight control once they were already smoking and similarly to research on association of body image and gender, this calls for additional interventions targeted to boys (Kopcakova et al. 2014). As expected, grade predicted both smoking status and practice of smoking for weight control. Prevalence among the first grade adolescents was 15 percent-point higher compared to 13 year old from primary school (19.6% compared to 3.8%) indicating that transition from primary to secondary school is critical time for additional interventions.
Whereas some studies showed association of gender with smoking status and smoking as weight control behavior (Fulkerson and French 2003) our results differ as we didn’t find such association. One explanation might be increase in the WCB among boys in many countries (Dzielska et al. 2020) but as this is the first HBSC study in Serbia we cannot confirm changes in patterns of weight control behaviors among adolescents by gender.
Our findings that more than one third of adolescents (37.7%) practiced unhealthy weight control measures and 6.6% smoked for weight control are especially worrying given the association of these behaviors with smoking. Even so we focused on cigarettes, it can be expected that unhealthy weight control behaviour correlation was not specifically limited to cigarettes, but existed also to other tobacco products as it was previously found in other countries (Sutter et al. 2016).While some studies showed association between overweight/obesity and smoking (Jacobs 2019) we were not able to observe this association in multivariable regression model. In line with research of Lee et al. (2015) we found that students that perceived themselves as underweight had higher odds to smoke as well as those who perceived their physical appearance as very/quite good looking. This indicates that adolescents might smoke as they think it would look more attractive but due to the cross- sectional nature of our study we cannot explore direction of this association.
Depression was associated with smoking status as adolescents with depressive symptoms had twice higher odds of being smokers compared to those not depressed and this finding is also in line with previously published (Upadhyaya et al. 2002). We found that depression plays role also in engaging in smoking for weight control, but design of this study doesn’t allow us to elaborate on the direction of association between smoking and depression which can be either one or bi-directional (Fluharty et al. 2017). This finding should be interpreted also in light of evidence that body dissatisfaction is associated with depressive symptoms (Felton et al. 2010).
Apart from exploring association of smoking status and unhealthy weight control practices in our study, we additionally focused on prevalence and characteristics of smokers that smoke more to control weight. We found that slightly more than half of the smokers (50.9%) reported this unhealthy weight control behavior. Such high percentage can partly be explained by belief that smoking can help in control of body weight, similarly as in the study in the USA in which 40% of 13- year old students expressed such beliefs (Klesges et al. 1997).
The statistically significant differences between smokers who smoke more for weight control and those who did not were found by grade, symptoms of depression and engaging in other unhealthy weight control practices. Correlation of risky weight control behaviors and smoking was also confirmed in other studies (Forrest and Forrest 2008).
Some studies show that extreme weight-control behaviors were positively associated to overweight and body image dissatisfaction (de Santana et al. 2016) while others found that body weight had higher influence on weight control (Sim et al. 2017) and as well as extreme weight behaviours (Silva et al. 2018). We found that neither BMI nor body image predicted smoking for weight control. Previous research found some difference in correlates by gender with no significant relationship between BMI and smoking to control weight for females and positive relationship for overweight males who were more likely to report smoking for weight control (Cavallo et al. 2006).
Our finding that depression was associated with smoking status and smoking for weight control stresses the importance of interventions aimed to improve the mental health of adolescents. Necessity of mental health intervention is also backed up with findings on importance of emotional regulation processes for pursuing life goals and values (Ferreira and Trindade 2015) and association of body image perception and depression (Hong and Hong 2019).
Higher odds of practicing extreme weight control behaviours among smokers and also among those who already smoke more for weight control, confirm findings from growing body of evidence on clustering risk behaviors and importance of tackling psychosocial aspects in interventions aimed at health behavior change (Thomas et al. 2020). These findings stress the importance of identification of specifically vulnerable groups and carefully designed multi component interventions rather than separate interventions for substance use prevention or promotion of healthy diet.
Limitations
Limitation of this study are related to the cross-sectional design of the survey and the data collection in terms of recall bias, social desirability and faking bad phenomenon in students’ responses (Groth and Kleka 2018).In addition, results cannot be generalized to all adolescents of the explored age group, as some of them are not in the educational system, However, data are collected in line with well elaborated HBSC methodology (Roberts et al. 2009; Inchley 2018) which provides solid ground for high quality data. Nationally representative sample allows generalization of findings for Serbian students 13- and 15- years old, but not for all adolescents in these age groups as not all of them are in the school system as secondary school is not obligatory. However, representativeness of the sample, international comparable data and standardized methodology indicate that results of our study could be useful for the other countries of Western Balkan and other central and eastern European countries with similarities in prevalence and characteristics of risk behaviors in adolescents.
Conclusion
Results of our study indicate that body image is better predictor of smoking status than actual BMI. Depression and other unhealthy weight control behavior were found to be significantly associated both with smoking in general and with smoking as weight control strategy. Findings point out clustering of risk behavior and call for incorporating and strengthening interventions for adolescents’ weight control management and mental health as part of smoking prevention and cessation programs. Apart from clustering of risk behaviors, these programs shall take into account possible presence of mental health problems such as depression. Sharp increase in smoking prevalence and in smoking for weight control in the transition period between primary and secondary school underlines the need for additional interventions among 13- and 15-years old adolescents.
References
Arrazola RA, Ahluwalia IB, Pun E et al (2017) Current tobacco smoking and desire to quit smoking among students aged 13–15 years - global youth tobacco survey, 61 countries, 2012–2015. MMWR Morb Mortal Wkly Rep 66(20):533–537. https://doi.org/10.15585/mmwr.mm6620a3
Boutelle K, Neumark-Sztainer D, Story M, Resnick M (2002) Weight control behaviors among obese, overweight, and nonoverweight adolescents. J Pediatr Psychol 27(6):531–540. https://doi.org/10.1093/jpepsy/27.6.531
Bradley KL, Bagnell AL, Brannen CL (2010) Factorial validity of the center for epidemiological studies depression 10 in adolescents. Issues Mental Health Nursing 31(6):408–412. https://doi.org/10.3109/01612840903484105
Brown CS, Kola-Palmer S, Dhingra K (2015) Gender differences and correlates of extreme dieting behaviours in US adolescents. J Health Psychol 20(5):569–579. https://doi.org/10.1177/1359105315573441
Camp DE, Klesges RC, Relyea G (1993) The relationship between body weight concerns and adolescent smoking. Health Psychol 12(1):24–32. https://doi.org/10.1037//0278-6133.12.1.24
Cavallo DA, Duhig AM, McKee S, Krishnan-Sarin S (2006) Gender and weight concerns in adolescent smokers. Addict Behav 31(11):2140–2146. https://doi.org/10.1016/j.addbeh.2006.02.021
Charrier L, Berchialla P, Dalmasso P, Borraccino A, Lemma P, Cavallo F (2019) Cigarette smoking and multiple health risk behaviors: a latent class regression model to identify a profile of young adolescents. Risk Anal 39(8):1771–1782. https://doi.org/10.1111/risa.13297
Cole TJ, Lobstein T (2012) Extended international (IOTF) body mass index cut-offs for thinness, overweight and obesity. Pediatric Obesity 7(4):284–294. https://doi.org/10.1111/j.2047-6310.2012.00064.x
Croll J, Neumark-Sztainer D, Story M, Ireland M (2002) Prevalence and risk and protective factors related to disordered eating behaviors among adolescents: relationship to gender and ethnicity. J Adolesc Health 31(2):166–175. https://doi.org/10.1016/s1054-139x(02)00368-3
Currie C, Molcho M, Boyce W, Holstein B, Torsheim T, Richter M (2008) Researching health inequalities in adolescents: the development of the health behaviour in school-aged children (HBSC) family affluence scale. Soc Sci Med 66(6):1429–1436. https://doi.org/10.1016/j.socscimed.2007.11.024
Daee A, Robinson P, Lawson M, Turpin JA, Gregory B, Tobias JD (2002) Psychologic and physiologic effects of dieting in adolescents. South Med J 95(9):1032–1041
de Santana ML et al (2016) Risk factors for adopting extreme weight-control behaviors among public school adolescents in Salvador, Brazil: a case-control study. J Am Coll Nutr 35(2):113–117. https://doi.org/10.1080/07315724.2014.951903
Dzielska A, Kelly C, Ojala K et al (2020) Weight reduction behaviors among european adolescents-changes from 2001/2002 to 2017/2018. J Adolesc Health 66(6S):S70–S80. https://doi.org/10.1016/j.jadohealth.2020.03.008
Ellickson PL, Tucker JS, Klein DJ (2001) High-risk behaviors associated with early smoking: results from a 5-year follow-up. J Adolesc Health 28(6):465–473. https://doi.org/10.1016/s1054-139x(00)00202-0
Felton J, Cole DA, Tilghman-Osborne C, Maxwell MA (2010) The relation of weight change to depressive symptoms in adolescence. Dev Psychopathol 22(1):205–216. https://doi.org/10.1017/S0954579409990356
Ferreira C, Trindade IA (2015) Body image-related cognitive fusion as a main mediational process between body-related experiences and women's quality of life. Eating Weight Disorders EWD 20(1):91–97. https://doi.org/10.1007/s40519-014-0155-y
Fluharty M, Taylor AE, Grabski M, Munafò MR (2017) The association of cigarette smoking with depression and anxiety: a systematic review. Nicotine Tobacco Res 19(1):3–13. https://doi.org/10.1093/ntr/ntw140
Forrest KY, Forrest AG (2008) Correlates of risky weight-contrl behaviors in adolescents. Am J Health Studies 23(1):16
Fulkerson JA, French SA (2003) Cigarette smoking for weight loss or control among adolescents: gender and racial/ethnic differences. J Adolesc Health 32(4):306–313. https://doi.org/10.1016/s1054-139x(02)00566-9
Groth J, Kleka P (2018) Patterns of intentional faking in questionnaire-based study of psychopathy. Current Issues Personal Psychol 6(4):305–317
Hazzard VM, Hahn SL, Sonneville KR (2017) Weight misperception and disordered weight control behaviors among U.S. high school students with overweight and obesity: associations and trends, 1999–2013. Eat Behav 26:189–195. https://doi.org/10.1016/j.eatbeh.2017.07.001
Hong GW, Hong SM (2019) Relationships among body mass index, body image, and depression in Korean adults: Korea national health and nutrition examination survey 2014 and 2016. J Obesity Metabolic Syndrome 28(1):61–68. https://doi.org/10.7570/jomes.2019.28.1.61
Inchley J CD, Cosma A Samdal O (2018) Health behaviour in school-aged children (HBSC) study protocol: background, methodology and mandatory items for the 2017/18 survey.
Inchley J, Currie D, Budisavljevic S, Torsheim T, Jåstad A, Cosma A et al (eds) (2020) Spotlight on adolescent health and well-being. Findings from the 2017/2018 Health Behaviour in School-aged Children (HBSC) survey in Europe and Canada. International report, vol 2. Key data. WHO Regional Office for Europe, Copenhagen. Licence: CC BY-NC-SA 3.0 IGO
Jacobs M (2019) Adolescent smoking: the relationship between cigarette consumption and BMI. Addict Behav Rep 9:100153. https://doi.org/10.1016/j.abrep.2018.100153
Kilibarda B, Vukovic D, Krstev S (2019) Prevalence and correlates of concurrent use of cigarettes, electronic cigarettes, and waterpipes among Serbian youth. Tobacco Induced Diseases 17:66. https://doi.org/10.18332/tid/111357
Klesges RC, Elliott VE, Robinson LA (1997) Chronic dieting and the belief that smoking controls body weight in a biracial, population-based adolescent sample. Tob Control 6(2):89–94. https://doi.org/10.1136/tc.6.2.89
Kopcakova J, Dankulincova VZ, Madarasova GA, van Dijk JP, Reijneveld SA (2014) Is being a boy and feeling fat a barrier for physical activity? The association between body image, gender and physical activity among adolescents. J Environ Res Public Health 11(11):11167–11176
Krowchuk DP, Kreiter SR, Woods CR, Sinal SH, DuRant RH (1998) Problem dieting behaviors among young adolescents. Arch Pediatr Adolesc Med 152(9):884–888. https://doi.org/10.1001/archpedi.152.9.884
Larson NI, Story M, Perry CL, Neumark-Sztainer D, Hannan PJ (2007) Are diet and physical activity patterns related to cigarette smoking in adolescents? Findings from project EAT. Preventing Chronic Disease 4(3):A51
Lee WT et al (2015) Relationships between body image, body mass index, and smoking in Korean adolescents: results of a nationwide Korea youth risk behavior web-based survey. Asian Pac J Cancer Prev 16(15):6273–6278
National Center for Chronic Disease Prevention and Health Promotion (US) Office on Smoking and Health (2012). Prevention tobacco use among youth and young adults: a report of the surgeon general. Centers for Disease Control and Prevention (US), Atlanta
NCD Risk Facor Collaboration (2017) Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 12.89 million children, adolescents, and adults. Lancet (London, England) 390(10113):2627–2642. https://doi.org/10.1016/s0140-6736(17)32129-3
Neumark-Sztainer D, Story M, Dixon LB, Murray DM (1998) Adolescents engaging in unhealthy weight control behaviors: are they at risk for other health-compromising behaviors? Am J Public Health 88(6):952–955. https://doi.org/10.2105/ajph.88.6.952
Penzes M, Czegledi E, Balazs P, Foley KL (2012) Factors associated with tobacco smoking and the belief about weight control effect of smoking among Hungarian adolescents. Cent Eur J Public Health 20(1):11–17
Roberts C et al (2009) The Health Behaviour in School-aged Children (HBSC) study: methodological developments and current tensions. Int J Public Health 54(Suppl 2):140–150. https://doi.org/10.1007/s00038-009-5405-9
Scardera S, Sacco S, Di Sante J, Booij L (2020) Body image-related cognitive fusion and disordered eating: the role of self-compassion and sad mood. Eating Weight Disorders Studies Anorexia Bulimia Obesity. https://doi.org/10.1007/s40519-020-00868-w
Seo DC, Jiang N (2009) Associations between smoking and extreme dieting among adolescents. J Youth Adolesc 38(10):1364–1373. https://doi.org/10.1007/s10964-009-9421-0
Silva SUD, Barufaldi LA, Andrade S, Santos MAS, Claro RM (2018) Nutritional status, body image, and their association with extreme weight control behaviors among Brazilian adolescents, National Adolescent Student Health Survey 2015. Braz J Epidemiol 21(11):e180011. https://doi.org/10.1590/1980-549720180011.supl.1
Sim WY et al (2017) The relationship between smoking and unhealthy weight control behaviors among Korean adolescents: the tenth Korea youth risk behavior web-based survey, 2014. Korean J Family Med 38(1):28–33. https://doi.org/10.4082/kjfm.2017.38.1.28
Strauss RS, Mir HM (2001) Smoking and weight loss attempts in overweight and normal-weight adolescents. Int J Obesity Related Metabolic Disorders J Int Assoc Study Obesity 25(9):1381–1385. https://doi.org/10.1038/sj.ijo.0801683
Sutter ME, Nasim A, Veldheer S, Cobb CO (2016) Associations between unhealthy dieting behaviors and tobacco use among adolescents. J Eat Disord 4:39–39. https://doi.org/10.1186/s40337-016-0126-y
Szamreta EA, Qin B, Ohman-Strickland PA et al (2017) Associations of anthropometric, behavioral, and social factors on level of body esteem in peripubertal girls. J Dev Behav Pediatr 38(1):58–64. https://doi.org/10.1097/DBP.0000000000000360
Thomas K, Nilsson E, Festin K et al (2020) Associations of psychosocial factors with multiple health behaviors: a population-based study of middle-aged men and women. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17041239
Upadhyaya HP, Deas D, Brady KT, Kruesi M (2002) Cigarette smoking and psychiatric comorbidity in children and adolescents. J Am Acad Child Adolesc Psychiatry 41(11):1294–1305. https://doi.org/10.1097/00004583-200211000-00010
Zullig KJ, Valois RF, Huebner ES, Oeltmann JE, Drane JW (2001) Relationship between perceived life satisfaction and adolescents' substance abuse. J Adoles Health 29(4):279–288. https://doi.org/10.1016/s1054-139x(01)00269-5
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no Conflict of interest.
Ethical statement
De-identified data used for this analysis were obtained from the Health Behaviour in School-aged Children Study 2017/2918 conducted in Serbia. Data collection procedures and questionnaires were in line with the international Health Behaviour in School-aged Children Study research protocol and were implemented after obtaining approval from the Ethical Committee of the Institute of Public Health of Serbia. Participation in the study was voluntary and anonymous.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the special issue "Adolescent health in Central and Eastern Europe".
Rights and permissions
About this article
Cite this article
Kilibarda, B., Gudelj Rakic, J., Mitov Scekic, S. et al. Smoking as a weight control strategy of Serbian adolescents. Int J Public Health 65, 1319–1329 (2020). https://doi.org/10.1007/s00038-020-01469-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-020-01469-1