Abstract
Objectives
Our study aims to describe French general practitioners’ (GPs’) practices toward pregnant patients regarding alcohol consumption and smoking and to highlight factors associated with specific practices.
Methods
In 2015, a representative sample of 1414 French GPs completed a telephone survey based on a stratified random sampling.
Results
61% of GPs declared screening for alcohol use and 82% for smoking at least once with each pregnant patient; quitting was not systematically advised either for alcohol or for smoking. GPs’ practices were significantly better among those who had more recent ongoing training. GPs who drank regularly were less likely to screen for alcohol use and GPs’ drinking frequency was inversely related to recommending quitting. Current and former smokers were less likely to recommend quitting to pregnant patients smoking over five cigarettes per day.
Conclusions
Screening and counselling practices for substance use during pregnancy are heterogeneous among French GPs and are notably related to their personal consumption. GP’s role in preventing substance use during pregnancy could be strengthened by actions regarding their own consumption and by modifications in their initial and ongoing training.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Alcohol use and tobacco smoking during pregnancy induce serious health risks for both the mother and the baby. Alcohol use can cause low birth weight, preterm birth or miscarriage (Feodor Nilsson et al. 2014; Miyake et al. 2014; Valero De Bernabe et al. 2004) and can also induce a range of physical and cognitive disorders known as foetal alcohol spectrum disorders (FASD) (BMA 2016). Smoking during pregnancy is associated with pregnancy complications, such as ectopic pregnancy, preterm premature rupture of the membrane, miscarriage, preterm birth, and is also linked to health problems of the new born such as low birthweight, sudden infant death syndrome, delay in foetal growth and neuro-development (Castles et al. 1999; Herrmann et al. 2008; Malloy et al. 1992; U.S. Department of Health and Human Services 2014). As a result, in France, official recommendations are no consumption of either alcohol or tobacco during pregnancy (Santé Publique France 2018a, b). Yet, in 2010, in France, 23% of pregnant women stated that they had drunk alcohol at least once while they were pregnant, among them 3% did before knowing they were pregnant (Saurel-Cubizolles et al. 2013). It has been estimated that FASD prevalence in France in 2009 was about 0.5 for 1000 births, this figure is probably underestimated due to difficulties of diagnosis and data reporting (Bloch et al. 2008). Meanwhile, 17% of pregnant women smoked tobacco during the 3rd trimester of pregnancy (Blondel et al. 2012). Even though since 2003 a reduction of smoking among pregnant women is seen in France, this prevalence is still relatively high compared to many other European countries, for instance Sweden (5%) or Norway (7%) (Euro-Peristat 2013).
GPs have an important position regarding prevention of substance use during pregnancy (WHO 2014). However, latest data showed that, in 2009, only 63% of French GPs reported screening for smoking at least once with all of their patients while only 23% did for alcohol use (Beck et al. 2011). GPs are not the main medical interlocutor during pregnancy, yet in 2010, they filled 22% of pregnancy certifications (official form mandatory for the health insurance fund) in France and 24% of pregnant women stated that they have had at least one antenatal visit with a GP (Blondel et al. 2012). Thus, GPs are a medical contact for many pregnant women and they can play a decisive role for the prevention of foetal harm. It is important to monitor their professional practice and factors associated with specific attitudes as disparities among French GPs have been shown regarding prevention (Beck et al. 2011; Collange et al. 2016; Gelly et al. 2014; Verger et al. 2015). Both sex and age are common factors associated with types of practices among GPs but other characteristics also appear to be significant, such as self confidence in addressing a given subject with patients and workload for instance (Collange et al. 2016; Verger et al. 2015). Important regional disparities are also seen in pregnancy monitoring implication by French GPs, which can be partly explained by differences in GPs density between regions (Buyck 2016). Besides, several studies pointed out the fact that GPs’ alcohol and tobacco consumption and representations could be related to their professional practices (Ketterer et al. 2014; Tam et al. 2013; Underner et al. 2006).
Overall, few quantitative studies focus on the specific subject of how GPs address with substance use during pregnancy. This is true in France but more generally, recent data covering this field are hard to find. Hence, our study brings an up-to-date research on this topic.
Using a representative sample of French GPs, our objectives were:
-
To investigate alcohol and tobacco screening, and counselling by GPs among their pregnant patients.
-
To highlight factors associated with GPs’ specific professional practices.
Methods
Data collection
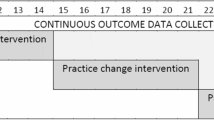
At the end of 2013, a representative panel of French GPs was set up to measure their beliefs, attitudes and patient management around various general public health themes (vaccination, pregnancy, cancer, multiple chronic conditions management and social precariousness). The survey is set to last 3 years organized in five survey waves each centred on one particular subject. The sample includes one nationally representative sample complemented with three regional oversamples.
A stratified random sampling design based on several sociodemographic and administrative data was used for GPs’ inclusion: sex, age (stratified in terciles of the sampling base: < 50, 50–58, > 58 years old), density of GPs in the municipality of practice (Barlet et al. 2012), GP’s workload (number of medical acts between November 2011 and December 2012). Both the density of GPs and the workload were summarized in variables with three levels whose thresholds correspond to the first and third quartiles. GPs characteristics are presented in Table 1. A dedicated publication is available for a full presentation of the survey methodology (Le Maréchal et al. 2015).
Of the 5151 GPs contacted during the inclusion wave, 1706 were both eligible and willing to participate in the survey. Of these, 1582 actually completed the first wave and 1414 the second wave. The survey was conducted by phone but GPs unwilling to do it over the phone could fill the questionnaire online: 1351 phones interviews were completed and 63 were done online.
The present study focuses on the results from the national sample of the second wave which took place between December 2014 and April 2015, and deals with gynaecologic and pregnancy follow-up. Among many other indicators (Buyck 2016), this survey wave included questions about the way in which GPs address alcohol and tobacco consumptions with their pregnant patients. In addition, GPs’ personal alcohol and tobacco consumptions were also monitored.
Measures
Professional practice
Professional practice was measured through two dimensions: screening for substance use and counselling.
Screening was measured by asking GPs how often they raise the issue alcohol and tobacco consumption with their pregnant patients: systematically (with the interviewer’s specification: “systematically meaning at least once with every patient”), often, sometimes or never. All four possible answers were read by the interviewer before the GPs chose one.
Regarding counselling, GPs were asked “what advice do you offer to pregnant women drinking alcohol occasionally?” with four possible answers: no drinking, no more than one glass per occasion, other advice and no advice at all. Two scenarios were proposed for smoking: “what advice do you offer to pregnant women smoking (a) more than five cigarettes a day? (b) less than five cigarettes a day?” Possible answers were: no smoking, reduced consumption and no advice at all. Answers were summarized in three binary variables (alcohol and both smoking scenarios): recommendation to stop the consumption versus any other advice. For each substance, the case of GPs giving no advice at all was too rare to be considered separately and yet possibly too different to be grouped with others, thus was excluded from analyses (12 GPs were excluded from the alcohol analysis and 13 were from the tobacco analysis). The five cigarettes per day cut-off comes from a qualitative work among French health professionals (GPs, gynaecologists, obstetricians and midwives) (Ifop and Santé publique France 2013), which showed that some of them tolerate a tobacco consumption up to five cigarettes per day with their pregnant patients; as for them, up to this point the risk is limited enough.
Five dependent binary variables were studied:
-
Screening for alcohol use once with every pregnant patient, versus any other response.
-
Screening for smoking once with every pregnant patient, versus any other response.
-
Giving the recommendation to quit alcohol use, versus any other response (GPs giving no advice at all excluded).
-
Giving the recommendation to quit smoking (two variables for smoking based on the level of consumption) versus any other response (GPs giving no advice at all excluded).
Personal consumption
GPs’ alcohol use was ascertained by asking respondents on how many days during the previous week they had drunk alcohol: every day, on 3–6 days, on 1 or 2 days or never. This question was asked four times corresponding to four types of alcohol: wine, beer, strong liquor and any other alcoholic beverage. That information was summarized by dividing GPs in three groups: regular alcohol drinkers (reporting drinking 3 days a week or more for at least one type of alcohol), occasional drinkers (reporting drinking 1 or 2 days a week for at least one type of alcohol but never more than that for each type) and non-drinkers.
GPs’ smoking status was ascertained by asking respondents if they currently smoked, even occasionally and non-smokers were asked if they had smoked in their life. GPs were divided in three groups: current smokers, former smokers and never smokers.
Other variables
GPs were asked how frequently, during the year before the survey, they had received a female patient as part of the official mandatory pregnancy monitoring programme and a binary variable was created to indicate if they did so at least once every 3 months.
GP’s ongoing training was assessed by the reported number of medical training half-days the GP attended during the year before the survey, no matter the topic of the training which could include prevention-related topics but not necessarily.
Self-efficacy in dealing with alcohol or tobacco consumption of their pregnant patients was evaluated through two questions: “Personally, do you think that the advices you give your female patients regarding their (a) alcohol (b) tobacco consumption are… very effective/quite effective/quite ineffective/very ineffective”.
All measures are presented in Tables 1 and 2.
Statistical analyses
When estimating percentages, data were weighted according to the stratification variables (sex, age, workload and density of GPs in the municipality) to cope with possible selection bias and thus obtain population representative estimates. The correlates of both practice indicators were identified using unweighted multivariate logistic regressions, separately for alcohol and tobacco-related indicators (weighted percentages, adjusted odds ratios and 95% confidence intervals are presented). In each regression, all stratification variables were included in addition to GPs’ recent training, quarterly pregnancy monitoring binary variable, GPs’ alcohol consumption and self-efficacy for alcohol counselling in alcohol-related analyses and GPs’ tobacco consumption and self-efficacy for tobacco-related analyses. We ran the regressions without the weights as we were looking for correlates at the individual level but we performed weighted regression for sensitivity analyses. All covariates were included into a single model for each outcome. All statistical analyses were conducted using Stata/SE (v.13.1).
Results
Alcohol screening and counselling
Alcohol screening once with every pregnant patient was done by 61% of GPs, while quitting recommendation for occasional drinking was given by 77% of them (Table 2).
Multivariate analyses did not reveal any significant link between both indicators and GPs’ sex (Table 3). Age was not related to systematic screening and no clear relationship was found regarding recommending quitting though younger GPs were more often doing so. GPs’ workload was not associated with screening for alcohol use but busiest GPs were more likely to recommend quitting. Practicing in a municipality with a low GP density was not related to systematic screening but to a lower probability of recommending quitting. No significant relationship was found between GPs’ recent training and systematic screening but most recently trained GPs were more likely to counsel quitting. Doing a pregnancy monitoring at least once a trimester was positively associated with systematic screening for alcohol but not associated with counselling quitting. GPs who felt confident in the effectiveness of their counselling were more likely to screen for drinking but no significant link was found with recommending quitting.
Among GPs, 24% reported alcohol consumption on at least 3 days in the past week, 48% on 1 or 2 days and 28% never. GPs’ personal consumption also turned out to be significantly related to professional practice. Regular alcohol consumers (on the week before the survey) were less likely to screen for alcohol use. Moreover, we observed a clear gradient in GPs’ inclination to recommending quitting: the frequency of alcohol use was inversely related to recommending quitting.
Tobacco screening and counselling
Screening for smoking once with every pregnant patient was done by 82% of GPs. Quitting recommendation was given by 92% of GPs for smokers under five cigarettes per day and by 88% of them for smokers over five cigarettes per day (Table 2).
As opposed to alcohol drinking, very few relationships were found for all smoking-related dependent variables (Table 4). GPs’ sex, age, workload, self-efficacy in coping with smoking as well as the local GP density were not significantly related to either systematic screening for smoking or quitting recommendation (aside from age and counselling smokers over five cigarettes per day). None of the covariates turned out to be significantly related to recommending quitting to pregnant patient smoking less than five cigarettes per day.
GPs who had more than 8 half-days of recent training were more likely to screen for smoking with all their pregnant patients and to counsel quitting to smokers over five cigarettes per day. Doing a pregnancy monitoring at least once a trimester was associated with systematic screening for smoking but no significant link was found regarding counselling.
Among GPs, 16% were smokers at the time of the survey, 33% were former smokers while 50% had never smoked. Smoker and former smoker GPs were less likely to counsel quitting to a pregnant patient smoking more than five cigarettes per day but GPs’ smoking status was not related with both screening and counselling smokers under five cigarettes per day.
For both alcohol- and smoking-related analyses, the weighted regression estimates led to the same conclusions.
Discussion
Main findings
In the research field of GPs’ practices, data and studies regarding the specific topic of substance use during pregnancy are scarce, and quantitative analyses are even scarcer. Our study highlighted disparities of practice among GPs thus emphasizing the need for more monitoring in this field. Screening once with every pregnant patient for alcohol consumption and tobacco smoking was not performed by all French GPs in 2015 and the “zero consumption” guideline was not the systematic answer to consumption. In 2009, one national representative French study highlighted that GPs performed systematic screening with their patients considerably more frequently regarding smoking (63%) than alcohol consumption (23%) (Beck et al. 2011). Our study confirms that it is still the case in 2015, although to a lesser extent.
In our study, professional behaviour was linked to GPs’ personal substance use. Regular drinkers were less prone to screen for alcohol use at least once with every pregnant patient compared to occasional drinkers or abstinent GPs and the frequency of alcohol use was inversely related to recommending quitting. Pregnant patients smoking over five cigarettes a day received more frequently recommendations to decrease the number of cigarettes, as opposed to quitting, from current and former smoker compared to never smoker GPs. It could thus be hypothesized that a more moderate use of alcohol and smoking cessation among GPs, not only would benefit on their own health, but could also benefit their pregnant patients.
Two similar French studies were done at a local scale. In one, the authors concluded that no differences were found between smoker and non-smoker GPs regarding screening for smoking among all categories of patients (yet a difference was found for the overall frequency of screening) and inquiring about the patient’s intentions to quit (De Col et al. 2010). The other study, however, concluded that smoking was inversely correlated with screening for smoking and inquiring about quitting intentions (Underner et al. 2006). To our knowledge, no quantitative study focuses on the relationship between GPs’ alcohol use and their practices with pregnant patients but some qualitative studies also suggested that personal attitudes regarding alcohol use may affect GPs’ practice (Ketterer et al. 2014; Tam et al. 2013).
Regarding GPs’ consumptions, our study shows that alcohol use was less frequent in 2015 than what it used to be: regular consumption (at least 3 days per week the week before the survey) decreased from 30% in 2003 (last available nationally representative estimate in France) to 24% in 2015 while abstinence increased from 19 to 28% (Gautier 2005). The decrease of regular consumption is seen among men (from 34 to 28%) but the overall drop also comes from an increase of the proportion of women among GPs who are less often regular drinkers (16%, stable between 2003 and 2015). In comparison with the national representative surveys among the French population, the rate of French adults drinking at least twice a week remained stable between 2005 and 2014 (Richard and Beck 2016). GPs’ smoking rate has decreased from 29% in 2003 (Gautier 2005) to 16% in 2015—the decrease being observed for both sexes—as opposed to the stability observed in the French population, in which the smoking rate was 35% both in 2000 (McNeill et al. 2015) and in 2015 (Andler et al. 2016).
Finally, in our study, GPs’ clinical practice with pregnant patients regarding alcohol use and smoking was found to be associated with their recent training: more trained GPs were more prone to screen for smoking and to recommend quitting smoking and alcohol consumption. We also found that systematic screening for alcohol use was related to a higher self-efficacy in dealing with alcohol-related issues. A prior study has shown that French GPs were more likely to screen for alcohol or smoking at least once with every patient if they felt that GPs had a role to play in that field (Gautier 2011). Initial and ongoing training could thus be updated and promoted to emphasize the role of GPs in preventing foetal harm due to the mother’s alcohol and smoking habits.
Attitudes of GPs toward alcohol and tobacco prevention
In 2010, GPs issued about one quarter of all pregnancy certifications in France, making them significant actors in relaying prevention messages related to addictive behaviours. As opposed to the rather well-known dangerousness of smoking and heavy drinking, scientific evidence is still lacking to settle the question of the potential harm of moderate alcohol use. In France, health authorities choose to follow the precautionary principle of no consumption at all during pregnancy. Yet, the scientific uncertainty contributes to an overall confusion in individuals’ perceptions (Cogordan et al. 2016). Healthcare professionals are no exception and there is still a strong uncertainty regarding what official guidelines they should refer to and what practical message they should deliver (Geirsson et al. 2005; Kesmodel 2016). Similarly, in other fields of prevention such as vaccination, French GPs exhibit different behaviours depending on their overall level of trust in official institutions and guidelines (Raude et al. 2016).
In addition to the lack of scientific consensus, alcohol use can be a particularly sensitive subject due to sociocultural beliefs and attitudes—France remains one of the highest wine producing and consuming countries—and thereby there remain obstacles in communication between GPs and patients (Crawford-Williams et al. 2015; Tam et al. 2013). Besides, several studies have highlighted social disparities among patients regarding tobacco or alcohol screening and counselling (Brown et al. 2016; Engdahl and Nilsen 2011). Our data do not suggest any inferences on this point but the complex situation of alcohol might explain why, in our study, GPs’ practices regarding smoking among their pregnant patients appear to be somehow more homogeneous than their practices regarding alcohol use. A qualitative study also highlighted the fact that, for some GPs, smoking is an “easier” subject to assess than alcohol use (Ampt et al. 2009).
Smoking cessation is a difficult issue as most attempts to quit fail (Hughes et al. 2004). Some GPs may thus believe that recommending a decrease is more likely to be followed than recommending quitting. In France in 2012, pregnant women who smoked were more worried about the impact on their unborn child of the potential stress caused by smoking cessation than about the impact of moderate smoking (Dumas 2015). However, this belief is not scientifically supported (Chamberlain et al. 2017), and overall the potential stress caused by smoking cessation is largely outweighed by the proven benefits of quitting for both the mother and the infant.
Limitations and further research
The main limitation of our study is that most of the data we used were self-reported and the memory and desirability biases cannot, therefore, be ruled out. Several variables (GP’s age and workload, local GP density) used for the sampling design were stratified prior to the survey and the analyses and cut-offs could not be changed afterwards. Moreover, the limited number of independent variables which could be included in the models narrowed the scope of our analysis. Regarding the definition of GPs’ regular alcohol consumption, we used the definition of the French focal point of the REITOX (Réseau Européen d’Information sur les Drogues et les Toxicomanies) related to the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) (French Reitox National Focal Point 2015). However, for measuring alcohol consumption in the previous week, the same question as in a 2003 survey—which is the only past measure of GPs’ alcohol consumption in France—was used to be able to have at least one benchmark (Gautier 2005). This question relates to four distinct alcohol types; we thus used the combined variable for drinking 3 days a week or more for at least one type of alcohol. But many other questionnaires could have been used for measuring alcohol consumption, for instance the alcohol use disorder identification test (AUDIT) (Bohn et al. 1995) which might have led to looking at the problem from a different perspective and thus have led to different findings. Concerning smoking, our study allows for identifying GPs screening at least once with all their pregnant patients; however, the WHO guidelines (WHO 2013) indicate that smoking habits should be asked at every antenatal care visit and based on these guidelines, appropriate screening was probably lower than what we measured.
Most of these limitations relate to the fact that the survey was not specifically designed for this particular study, as it addressed many topics in the field of GPs’ obstetrics and gynaecology practices. More research is required to understand why we observe disparities of practices between GPs, and to address whether this heterogeneity is even more acute in the case of populations for which prevention guidelines are not as clear as those concerning pregnant women.
References
Ampt AJ, Amoroso C, Harris MF, McKenzie SH, Rose VK, Taggart JR (2009) Attitudes, norms and controls influencing lifestyle risk factor management in general practice. BMC Fam Pract 10:59. https://doi.org/10.1186/1471-2296-10-59
Andler R et al (2016) Tobacco consumption and e-cigarette use in France in 2015: preliminary results from the 2015 cancer barometer. Bull Épidémiol Hebd 30–31:502–507
Barlet M, Coldefy M, Collin C, Lucas-Gabrielli V (2012) L’Accessibilité potentielle localisée (APL): une nouvelle mesure de l’accessibilité aux médecins généralistes libéraux. Questions d’économie de la santé. IRDES, Paris
Beck F, Guignard R, Obradovic I, Gautier A, Karila L (2011) Increasing trends in screening for addictives behaviors among general practitioners in France. Rev D’epidemiol Sante Publique 59:285–294. https://doi.org/10.1016/j.respe.2011.03.059
Bloch J, Cans C, de Vigan C, de Brosses L, Doray B, Larroque B, Perthus I (2008) Feasibility of the foetal alcohol syndrome surveillance. Arch Pediatr 15:507–509. https://doi.org/10.1016/s0929-693x(08)71814-1
Blondel B, Lelong N, Kermarrec M, Goffinet F (2012) Trends in perinatal health in France from 1995 to 2010. Results from the French National Perinatal Surveys. J Gynecol Obstet Biol Reprod 41:e1–e15. https://doi.org/10.1016/j.jgyn.2012.04.014
BMA (2016) Alcohol and pregnancy—preventing and managing fetal alcohol spectrum disorders. British Medical Association, BMA House, Tavistock Square, London
Bohn MJ, Babor TF, Kranzler HR (1995) The alcohol use disorders identification test (AUDIT): validation of a screening instrument for use in medical settings. J Stud Alcohol 56:423–432
Brown J et al (2016) Comparison of brief interventions in primary care on smoking and excessive alcohol consumption: a population survey in England. Br J Gen Pract 66:e1–9. https://doi.org/10.3399/bjgp16x683149
Buyck J-F et al (2016) Attitudes et pratiques des médecins généralistes dans le cadre du suivi de la grossesse. DREES (0977), 8p
Castles A, Adams EK, Melvin CL, Kelsch C, Boulton ML (1999) Effects of smoking during pregnancy five meta-analyses. Am J Prev Med 16:208–215
Chamberlain C, O’Mara-Eves A, Porter J, Coleman T, Perlen SM, Thomas J, McKenzie JE (2017) Psychosocial interventions for supporting women to stop smoking in pregnancy. Cochrane Database Syst Rev 2:Cd001055. https://doi.org/10.1002/14651858.cd001055.pub5
Cogordan C, Nguyen-Thanh V, Richard J-B (2016) Alcool et grossesse: connaissances et perception des risques. Alcool Addictol 38:181–190
Collange F, Fressard L, Pulcini C, Sebbah R, Peretti-Watel P, Verger P (2016) General practitioners’ attitudes and behaviors toward HPV vaccination: a French national survey. Vaccine 34:762–768. https://doi.org/10.1016/j.vaccine.2015.12.054
Crawford-Williams F, Steen M, Esterman A, Fielder A, Mikocka-Walus A (2015) “If you can have one glass of wine now and then, why are you denying that to a woman with no evidence”: knowledge and practices of health professionals concerning alcohol consumption during pregnancy Women. Birth 28:329–335. https://doi.org/10.1016/j.wombi.2015.04.003
De Col P, Baron C, Guillaumin C, Bouquet E, Fanello S (2010) Influence of smoking among family physicians on their practice of giving minimal smoking cessation advice in 2008. A survey of 332 general practitioners in Maine-et-Loire. Rev Mal Respir 27:431–440. https://doi.org/10.1016/j.rmr.2010.03.001
Dumas A (2015) Smoking, pregnancy and breastfeeding: exposure, knowledge and risk perceptions. Bull Épidémiol Hebd 17–18:301–307
Engdahl B, Nilsen P (2011) Receiving an alcohol enquiry from a physician in routine health care in Sweden: a population-based study of gender differences and predictors. Int J Environ Res Public Health 8:1296–1307. https://doi.org/10.3390/ijerph8051296
Euro-Peristat (2013) Project with SCPE and EUROCAT. European Perinatal Health Report. The health and care of pregnant women and babies in Europe in 2010. https://www.europeristat.com
Feodor Nilsson S, Andersen PK, Strandberg-Larsen K, Nybo Andersen AM (2014) Risk factors for miscarriage from a prevention perspective: a nationwide follow-up study. BJOG 121:1375–1384. https://doi.org/10.1111/1471-0528.12694
French Reitox National Focal Point (2015) France, new developments, trends. In: Beck F (ed) 2014 national report (2013 data) to the EMCDDA by the Reitox National Focal Point France. New development, trends. OFDT, Saint-Denis
Gautier A (2005) General practitioners/pharmacists health barometer 2003. Health barometers. INPES, Saint-Denis
Gautier A (2011) General practitioners health barometer 2009. Health barometers. INPES, Saint-Denis
Geirsson M, Bendtsen P, Spak F (2005) Attitudes of Swedish general practitioners and nurses to working with lifestyle change, with special reference to alcohol consumption. Alcohol Alcohol 40:388–393. https://doi.org/10.1093/alcalc/agh185
Gelly J et al (2014) Profile of French general practitioners providing opportunistic primary preventive care–an observational cross-sectional multicentre study. Fam Pract 31:445–452. https://doi.org/10.1093/fampra/cmu032
Herrmann M, King K, Weitzman M (2008) Prenatal tobacco smoke and postnatal secondhand smoke exposure and child neuro development. Curr Opin Pediatr 20:184–190. https://doi.org/10.1097/mop.0b013e3282f56165
Hughes JR, Keely J, Naud S (2004) Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction 99:29–38
Ifop, Santé publique France (2013) Counseling for alcohol consumption and smoking among pregnant women (Unpublished study)
Kesmodel US (2016) Risks and guidelines for the consumption of alcohol during pregnancy. World J Obstet Gynecol 5:162–174
Ketterer F et al (2014) What factors determine Belgian general practitioners’ approaches to detecting and managing substance abuse? A qualitative study based on the I-Change Model. BMC Fam Pract 15:119. https://doi.org/10.1186/1471-2296-15-119
Le Maréchal M et al (2015) Design of a national and regional survey among French general practitioners and method of the first wave of survey dedicated to vaccination. Méd Maladies Infectieuses 45:403–410. https://doi.org/10.1016/j.medmal.2015.09.005
Malloy MH, Hoffman HJ, Peterson DR (1992) Sudden infant death syndrome and maternal smoking. Am J Public Health 82:1380–1382
McNeill A, Guignard R, Beck F, Marteau R, Marteau TM (2015) Understanding increases in smoking prevalence: case study from France in comparison with England 2000–10. Addiction 110:392–400. https://doi.org/10.1111/add.12789
Miyake Y, Tanaka K, Okubo H, Sasaki S, Arakawa M (2014) Alcohol consumption during pregnancy and birth outcomes: the Kyushu Okinawa Maternal and Child Health Study. BMC Pregnancy Childbirth 14:79. https://doi.org/10.1186/1471-2393-14-79
Raude J, Fressard L, Gautier A, Pulcini C, Peretti-Watel P, Verger P (2016) Opening the ‘Vaccine Hesitancy’ black box: how trust in institutions affects French GPs’ vaccination practices. Exp Rev Vaccines 15:937–948. https://doi.org/10.1080/14760584.2016.1184092
Richard JB, Beck F (2016) Long-term trends in tobacco and alcohol consumption in France through the lens of gender and social inequalities. Bull Épidémiol Hebd 7–8:126–133
Santé Publique France (2018a) Grossesse Sans Tabac http://www.tabac-info-service.fr/J-arrete-de-fumer/Grossesse-sans-tabac. Accessed 01 Mar 2018
Santé publique France (2018b) L’alcool et la grossesse http://www.alcool-info-service.fr/alcool/consequences-alcool/grossesse-femme-enceinte. Accessed 01 Mar 2018
Saurel-Cubizolles MJ, Prunet C, Blondel B (2013) Alcohol consumption during pregnancy and perinatal health in France in 2010. Bull Épidémiol Hebd 16–18:180–185
Tam CW, Zwar N, Markham R (2013) Australian general practitioner perceptions of the detection and screening of at-risk drinking, and the role of the AUDIT-C: a qualitative study. BMC Fam Pract 14:121. https://doi.org/10.1186/1471-2296-14-121
Underner M, Ingrand P, Allouch A, Laforgue AV, Migeot V, Defossez G, Meurice JC (2006) Influence of smoking among family physicians on their practice of giving minimal smoking cessation advice. Rev Mal Respir 23:426–429
U.S. Department of Health and Human Services (2014) The health consequences of smoking: 50 years of progress. A report of the surgeon general. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health
Valero De Bernabe J, Soriano T, Albaladejo R, Juarranz M, Calle ME, Martinez D, Dominguez-Rojas V (2004) Risk factors for low birth weight: a review. Eur J Obstet Gynecol Reprod Biol 116:3–15. https://doi.org/10.1016/j.ejogrb.2004.03.007
Verger P et al (2015) Vaccine hesitancy among general practitioners and its determinants during controversies: a national cross-sectional survey in France. EBio Med 2:891–897. https://doi.org/10.1016/j.ebiom.2015.06.018
WHO (2013) WHO guidelines approved by the guidelines review committee. In: WHO recommendations for the prevention and management of tobacco use and second-hand smoke exposure in pregnancy. World Health Organization, Geneva
WHO (2014) WHO guidelines approved by the guidelines review committee. In: Guidelines for the identification and management of substance use and substance use disorders in pregnancy. World Health Organization, Geneva
Acknowledgements
We thank Romain Guignard, Jean-Baptiste Richard and Arnaud Gautier for their advice during the data analysis and Manon Jeuland for her help with the bibliographic research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
All Authors declares that they have no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Andler, R., Cogordan, C., Pasquereau, A. et al. The practices of French general practitioners regarding screening and counselling pregnant women for tobacco smoking and alcohol drinking. Int J Public Health 63, 631–640 (2018). https://doi.org/10.1007/s00038-018-1103-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-018-1103-9