Abstract
Objective
To report the prevalence and trends of the BMI of Portuguese adolescents in 2002, 2006 and 2010.
Methods
4138 boys and 4472 girls self-reported weight, height, physical activity, perception of health and life satisfaction.
Results
For adolescents aged 11–13 years, the prevalence of overweight/obesity decreased from 23.5 % in 2002 to 20.7 % in 2010, using IOTF cutoff points, and decreased from 32.4 to 28.4 % between 2002 and 2010 using WHO cutoff points. For adolescents aged 15–17 years, the prevalence increased from 13.9 to 16.8 % between 2002 and 2010 using IOTF cutoff, and increased from 14.8 % in 2002 to 18.2 % in 2010 when using WHO cutoff points. Although the prevalence decreased among younger adolescents and increased among older ones, the differences were not significant. Physical activity in the last 7 days (p < 0.05), better life satisfaction (p < 0.05) and perception of health (p < 0.001) predicted lower body mass index z score.
Conclusions
Overall, there have been no significant changes in overweight and obesity prevalence in Portuguese adolescents from 2002 to 2010. However, the prevalence remains high and therefore it is important to continue surveillance.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The World Health Organization (WHO) has considered overweight and obesity a global epidemic that affects developed and developing countries (Speiser et al. 2005). It is a significant public health concern threatening the viability of basic health care delivery because its prevalence appears to be increasing throughout the world (Onis et al. 2010; Wang and Lobstein 2006). Among children and adolescents, overweight and obesity are associated with several health problems such as: metabolic syndrome, obstructive sleep apnoea, lipid and lipoprotein concentration, diabetes type II, and hypertension (Speiser et al. 2005; Steinberger et al. 2005).
The prevalence of overweight and obesity in adolescents increased throughout the world during the 1980s and 1990s (WHO 2000). However, although the prevalence of the overweight and obesity pandemic continues to increase in certain countries or regions (Martinez-Vizcaino et al. 2012; Masuet-Aumatell et al. 2013), evidence for continuing increases is not universal (de Wilde et al. 2014), and is now reported to have plateaued in some westernized countries (Morgen et al. 2013; O’Dea et al. 2011; Olds et al. 2011; Rokholm et al. 2010). Collecting epidemiological data of overweight and obesity is important, because it helps to characterize the population weight status (O’Dea and Dibley 2014) and supports the development of preventive programs (Pettman et al. 2014). This is mainly important in countries like Portugal, because the prevalence of overweight and obesity is considered high among adolescents (Sardinha et al. 2011). Sardinha et al. (2011) reported that using International Obesity Task Force (IOTF) cutoff points the prevalence of overweight and obesity was 21.6 %, whereas the prevalence of overweight and obesity was 32.1 % when using WHO cutoff points.
Besides the epidemiological data, it is also important to identify the correlate factors of overweight and obesity, to intervene more accurately to prevent or fight against overweight and obesity. There is some evidence that physical activity may prevent weight gain and obesity (Reiner et al. 2013), and that sedentary behaviours, such as screen-based media have been linked to overweight and obesity (Prentice-Dunn and Prentice-Dunn 2012). Moreover, life satisfaction, an important aspect of well-being for adolescents, is associated with overweight and obesity (Wadsworth and Pendergast 2014), as well as subjective health perception (Herman et al. 2014).
The observation of the levelling off of overweight and obesity in most studies is simply based on trends (Morgen et al. 2013; O’Dea et al. 2011). There are no observations of the prevalence, and changes in the prevalence across the ages among different generations of adolescents. It is important to analyse the pattern of the prevalence as age increases, and to improve our understanding of the increasing or levelling off of overweight and obesity among adolescents. Thus, using a national representative sample of Portuguese adolescents, the aim of the study was to report the prevalence of weight status of Portuguese adolescents from 2002 to 2010; and to analyse the trends of overweight and obesity of two generations over the years (adolescents aged 11–13 in 2002 and aged 15–17 in 2006; and adolescents aged 11–13 in 2006 and aged 15–17 in 2010). As a western country, we hypothesized that the prevalence of overweight and obesity among Portuguese adolescents decreases as age increases, and that it is relatively stable throughout the last years for each age group. Furthermore, we also hypothesized that physical activity, life satisfaction and perception of health were negatively related with body mass index (BMI).
Methods
Participants and procedures
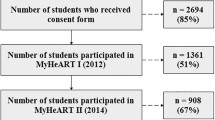
This study is based on data from the Health Behaviour in School-Aged Children (HBSC) Portuguese cross-sectional survey. HBSC Portugal is one of 43 countries and regions across Europe and North America that make up the HBSC Network. Collected data are used to gain new insight into young people’s health and well-being, to understand the social and psychological determinants of health, and to incorporate policies to improve young people’s lives. The sample consisted of 4138 boys and 4472 girls aged 11–17 years (M = 13.8, SD = 2.0), from the HBSC Portuguese survey in 2002 (n = 3099), 2006 (n = 2573), and 2010 (n = 2938) attending grades 6 and 10. In accordance with HBSC guidelines, a random-sampling procedure was used (Roberts et al. 2009). The strategy followed a systematic multi-stage cluster technique, whereby individual students are nested in school classes that are nested within schools. The Portuguese HBSC survey included a representative sample of students from 125 public schools, with weighted distributions reflecting the distribution of Portuguese students in grades 6, 8, and 10 (for the present study only adolescents attending grades 6 and 10 were utilized). All Portuguese administrative regions (Alentejo, Algarve, Centro, Lisboa, Norte, and Madeira) participated with the exception of autonomous regions of the Azores. The administration of the surveys was conducted according to standard guidelines from the HBSC survey protocol (Currie et al. 2000); the survey was carried out by trained school teachers during class time. Questionnaires were administered between January and February in 2002, 2006 and 2010. Participation was voluntary and questionnaires were answered anonymously. Research was in accordance with the Ethical Committee of Porto Medical School and the National Data Protection System. All school administrators gave their consent, legal guardians gave written informed consent, and students provided assent.
Body mass index
Current weight (to the nearest 0.5 kg) and height (to the nearest 0.5 cm) were self-reported. Adolescents were aware of their weight and height because they perform a physical fitness test (FitnessGram) several times a year, and physical education teachers provided them with information about their weight and height. Self-reported weight and height is a valid tool for BMI estimates of overweight and obesity in epidemiological studies (Fonseca et al. 2010). It is also frequently used as an alternative to anthropometric measures in large-scale studies, for reasons of convenience or cost (Fonseca and Gaspar de Matos 2005). BMI was then calculated based on mass (kilograms) divided by height (square metres). Adolescents were classified into underweight, normal weight, overweight and obese categories according to age- and sex-specific cutoff points proposed by the IOTF (Cole et al. 2000) and by the WHO (2007). The underweight adolescents group was small, so this category was out of the analysis and these adolescents were added into the normal weight category.
Potential correlates of body mass index
To assess physical activity, adolescents were provided with a definition of physical activity (Caspersen et al. 1985), and then were asked, “How many days did you practice physical activity during the last 7 days?” (Prochaska et al. 2001). Answers were given on an 8-point scale (1 = none to 8 = daily). A test–retest reliability of the reported physical activity was carried out within a 1-week interval across 90 adolescents. Using intra-class correlation coefficient (ICC), the reliability was high (ICC = 0.90).
Two screen-based media use were assessed: television/video/DVD watching and computer use. Adolescents were asked to indicate the customary time (hours per day) they spent on each activity. The test–retest reliability of these recreational sedentary behaviours was carried out within a 1-week interval across 90 participants. The reliability was good, with ICC of 0.89, confirming the reliability of these questions for surveillance of school students (Schmitz et al. 2004).
Life satisfaction was assessed by the Cantril Self-Anchoring Striving Scale (Cantril 1965). Adolescents rated their quality of life on a 10-point ladder, with zero being the ‘worst possible life’ and ten being the ‘best possible life’. Perception of health was assessed through the question, “How would you rate your health?” Answers were given, through selection, on a 4-point scale (poor, fair, good, and excellent) (Fosse and Haas 2009). The test–retest reliability of the self-rated quality of life and self-rated health were carried out within a 1-week interval across 90 participants. The reliability was good, with ICC of 0.87 and 0.93, respectively.
Data analysis
Descriptive statistics were calculated (means, standard deviation and percentages) for the entire sample and according to both HBSC survey years (2002, 2006, and 2010). Student t test and Chi square were used to assess differences in BMI z score and in BMI categories (IOTF and WHO cutoff points) among younger and older adolescents from the same generation (generation 1: adolescents aged 11–13 in 2002 and aged 15–17 in 2006; generation 2: adolescents aged 11–13 in 2006 and aged 15–17 in 2010). It is important to mention that almost all adolescents aged 11–13 in 2002 and 2006 were the same adolescents aged 15–17 in 2006 and 2010, respectively. Therefore, it is not a genuine within-subjects design, because paired sample data was not used. The effects of each potential correlate on BMI z score were assessed by a linear regression analysis. All statistical analyses were performed using IBM SPSS Statistics 22.0. The level of significance was set at 0.05.
Results
Table 1 shows the characteristics of adolescents in each gender and age group from different cohorts.
The prevalence of normal weight, overweight and obesity over the years among adolescents aged 11–13 and 15–17 is presented in Fig. 1a, b. For adolescents aged 11–13 years, the prevalence of overweight and obesity decreased from 23.5 % in 2002 to 20.7 % in 2010, using IOTF cutoff points, and decreased from 32.4 % to 28.4 between 2002 and 2010 when using WHO cutoff points. Nonetheless, the decrease was not significant (IOTF: χ 2(2) = 3.993, p = 0.136; WHO: χ 2(2) = 5.282, p = 0.071). For those aged 15–17 years the prevalence of overweight and obesity increased from 13.9 to 16.8 % between 2002 and 2010 using the IOTF cutoff, while the prevalence of overweight and obesity increased from 14.8 % in 2002 to 18.2 % in 2010, when using WHO cutoff points. However, the increase was not significant (IOTF: χ 2(2) = 4.622, p = 0.099; WHO: χ 2(2) = 6.429, p = 0.050).
a Prevalence of normal weight, overweight and obesity of 11- to 13-year-old adolescents in 2002, 2006 and 2010, according International Obesity Task Force (IOTF) and World Health Organization (WHO) cutoff points; Portugal. b Prevalence of normal weight, overweight and obesity of 15- to 17-year-old adolescents in 2002, 2006 and 2010, according International Obesity Task Force (IOTF) and World Health Organization (WHO) cutoff points; Portugal
Table 2 presents results from two adolescent generations. Adolescents aged 11–13 in 2002 were aged 15–17 in 2006; and those aged 11–13 in 2006 were aged 15–17 in 2010. For both generations of adolescents, the prevalence of overweight decreased significantly as age increased (χ 2(1) = 27.527, p < 0.001 and χ 2(1) = 23.048, p < 0.001, respectively). Although a decrease in BMI z score was also observed in both generations over the years, the results were not statistically significant.
Table 3 presents potential correlation of BMI z score for the entire sample, adjusted for age and gender. Physical activity in the last 7 days (β = −0.01, 95 % CI −0.02 to 0.00; p < 0.05), better life satisfaction (β = −0.01, 95 % CI −0.03 to 0.00; p < 0.05), and perception of health (β = −0.18, 95 % CI −0.22 to −0.15; p < 0.001) predicted lower BMI z scores.
Considering that the model presented in Table 3 was significant and BMI z score was explained by some factors (physical activity in the last 7 days, life satisfaction and perception of health), several analyses were performed to observe whether BMI z score could be explained by different potential factors in each generation. The results are presented in Table 4. For generation 1, physical activity in the last 7 days (β = −0.03, 95 % CI −0.05 to 0.00; p < 0.05), life satisfaction (β = −0.03, 95 % CI −0.06 to 0.00; p < 0.05), and perception of health (β = −0.16, 95 % CI −0.24 to −0.09; p < 0.001) were negatively related to BMI z score for adolescents aged 11–13. As adolescents get older (15–17 years of age), the only factor that significantly predicted the BMI z score was perception of health (β = −0.23, 95 % CI −0.32 to −0.14; p < 0.001). For generation 2, among the younger adolescents physical activity in the last 7 days (β = −0.05, 95 % CI −0.08 to −0.02; p < 0.01) and perception of health (β = –0.13, 95 % CI −0.21 to −0.04; p < 0.001) were related to BMI z score. Of those correlating factors, only perception of health (β = −0.19, 95 % CI −0.27 to −0.11; p < 0.001) remained significantly related to BMI z score for older adolescents.
Discussion
This study described the prevalence of self-reported weight status among Portuguese adolescents from 2002 to 2010. Results from the present study showed that the prevalence of normal weight, overweight, and obesity was not significantly different over the years independent of age. This suggests that the prevalence of overweight (including obesity) during this time was relatively stable. Moreover, when comparing the prevalence of overweight and obesity data from this study to the study carried out by Sardinha et al. (2011) that body height and body weight were determined by standard anthropometric methods, the results are quite similar. This partially confirms that self-reported weight status might be a feasible method to determine prevalence of overweight and obesity in the adolescent population.
Although the prevalence of overweight is still increasing in some countries and regions (Masuet-Aumatell et al. 2013; Zhang and Wang 2013), in some other parts of the world a levelling off, among children and adolescents, can be seen. In a study using data from HBSC Danish survey (Morgen et al. 2013), a tendency to levelling off, or even a decline in the prevalence rates for overweight and obesity for adolescents, was observed in the period from 2002 to 2010 (the same time period used in the present study). This trend is quite similar to the present results, being reinforced by the fact that the IOFT and WHO cutoff points revealed similar trends among adolescents. Similarly, O’Dea and Dibley (2014), using a large national survey of Australian school students, found that the prevalence of overweight and obesity did not increase in the adolescent population overall between 2006 and 2012. The aforementioned studies and the present study, based on Portuguese adolescents from 2002 to 2010, contribute to the growing evidence of the observed stabilization of the prevalence of overweight and obesity (Ogden et al. 2014; Olds et al. 2011; Rokholm et al. 2010). Moreover, it was also observed that the prevalence of overweight and obesity decreased over the years among two different generations of adolescents. These findings support the recent literature from various countries, such as: Japan, Russia, the United States, and several European countries (Olds et al. 2011; Rokholm et al. 2010), and serve to confirm that adolescent overweight and obesity may have plateaued in recent decades.
Since only recently several studies have addressed the levelling off in childhood obesity, the reasons for stagnation of a growing number of countries are yet unclear. There is not an understanding of the dynamics behind the recent stable prevalence of overweight and obesity among adolescents. It is important to uncover these dynamics to understand the trends reported here and in similar studies. Some plausible explanations have been proposed. One reason could be that being overweight has been recognized as a public health concern, which has led to the introduction of programs to promote physical activity and healthy eating habits. In Portugal, a considerable number of initiatives for preventing the development of obesity have been implemented, such as Platform Against Obesity, for the population (http://www.plataformacontraaobesidade.dgs.pt) or Physical Activity and Family-based Intervention in Paediatric Obesity Prevention, in the School Setting (PESSOA Project), focusing on school-age adolescents (http://programapessoa.dgidc.min-edu.pt/). These programs might create a general consciousness about the health problems attributed to overweight and obesity, and may consequently help people to change their practices and adopt healthier lifestyles. Another explanation proposed by Morgen et al. (2013) is that, perhaps, children with a predisposition to becoming overweight have already become overweight, and thus a saturation equilibrium was achieved. Moreover, a levelling off of overweight and obesity could be due to the relationship between prevalence and incidence. The prevalence is the product of incidence rate and duration. Therefore, a stable prevalence could indicate that the incidence rate of overweight and obesity continues at the same level, since no decline in the prevalence is evident (Rokholm et al. 2010).
The observed correlations of BMI z score were physical activity, for the younger adolescents, and perception of health. The relationship between physical activity and a decrease in overweight adolescents is not clear, and this study’s results should be interpreted with caution, because the association was only observed for the younger adolescents. It seems that there is a need to limit the extrapolation of the importance of physical activity in combating obesity. Although physical activity augments energy expenditure, most community- and school-based interventions employed to treat and prevent overweight, based on physical activity, do not have a significant impact on weight status when BMI is used as a measure of weight status. This is because BMI does not discriminate between lean and fat mass (Klakk et al. 2013; Waters et al. 2014). On the other hand, results for the perception of health corroborated through other studies among young people found that overweight and obesity is negatively related with self-rated health, even in the absence of chronic disease conditions (Herman et al. 2014).
Screen time has been reported to be related with adiposity (Boone et al. 2007). An association between time spent watching television and overweight and obesity was found in other studies (Campagnolo et al. 2008; de Jong et al. 2013), but not a relationship between computer use and weight status (de Jong et al. 2013; Marques et al. 2014). In the present study, the absence of association between television viewing, and computer used, and BMI could due to the fact that television viewing and computer used are not directly associated with physical activity (de Jong et al. 2013; Marques et al. 2014), which means that adolescents can spent a considerable amount of time on sedentary behaviours and then engage in enough physical activity to increase energy expenditure.
Some limitations and strengths should be addressed to qualify the conclusion. Height and weight were self-reported when calculating BMI. Therefore, these values are subject to bias and, additionally, BMI does not discriminate between lean and fat mass. However, self-reporting weight and height is considered a valid tool for BMI estimates in epidemiological studies (Fonseca et al. 2010), and BMI has been shown to correlate highly with dual-energy X-ray absorptiometry of body fatness in adolescents (Steinberger et al. 2005). Although some inferences may be possible because the study utilized nationally representative samples on all three data collection moments to analyse different generations, it is not a genuine within-subjects design because paired sample data of weight status was not used. Another limitation is the use of single item measures. However, single-response items are useful and have been developed for cross-cultural comparisons (Bobakova et al. 2015). Studies have demonstrated evidence of construct validity and reliability of single item measures (Prochaska et al. 2001; Schmitz et al. 2004). The main strength of this study includes the sample size (national and representative in all survey years) and the use of an international definition for overweight status that allows a comparison among the survey years and among other studies that use the same definition.
References
Bobakova D, Hamrik Z, Badura P, Sigmundova D, Nalecz H, Kalman M (2015) Test–retest reliability of selected physical activity and sedentary behaviour HBSC items in the Czech Republic, Slovakia and Poland. Int J Public Health 60(1):59–67. doi:10.1007/s00038-014-0628-9
Boone JE, Gordon-Larsen P, Adair LS, Popkin BM (2007) Screen time and physical activity during adolescence: longitudinal effects on obesity in young adulthood. Int J Behav Nutr Phys Act 4:26. doi:10.1186/1479-5868-4-26
Campagnolo PD, Vitolo MR, Gama CM, Stein AT (2008) Prevalence of overweight and associated factors in southern Brazilian adolescents. Public Health 122(5):509–515. doi:10.1016/j.puhe.2007.08.002
Cantril H (1965) The pattern of human concerns. Rutgers University Press, New Brunswick
Caspersen CJ, Powell KE, Christenson GM (1985) Physical activity, exercise, and physical fitness: definitions and distinctions for health-related research. Public Health Rep 100(2):126–131
Cole TJ, Bellizzi MC, Flegal KM, Dietz WH (2000) Establishing a standard definition for child overweight and obesity worldwide: international survey. BMJ 320(7244):1240–1243. doi:10.1136/bmj.320.7244.1240
Currie C, Hurrelmann K, Settertobulte W, Smith R, Todd J (2000) Health and health behavior among young people. Health behaviour in school-aged children: a WHO cross-national study (HBSC). World Health Organization, Copenhagen
de Jong E, Visscher TL, HiraSing RA, Heymans MW, Seidell JC, Renders CM (2013) Association between TV viewing, computer use and overweight, determinants and competing activities of screen time in 4- to 13-year-old children. Int J Obes 37(1):47–53. doi:10.1038/ijo.2011.244
de Wilde JA, Verkerk PH, Middelkoop BJ (2014) Declining and stabilising trends in prevalence of overweight and obesity in Dutch, Turkish, Moroccan and South Asian children 3–16 years of age between 1999 and 2011 in the Netherlands. Arch Dis Child 99(1):46–51. doi:10.1136/archdischild-2013-304222
Fonseca H, Gaspar de Matos M (2005) Perception of overweight and obesity among Portuguese adolescents: an overview of associated factors. Eur J Public Health 15(3):323–328. doi:10.1093/eurpub/cki071
Fonseca H, Silva AM, Matos MG et al (2010) Validity of BMI based on self-reported weight and height in adolescents. Acta Paediatr 99(1):83–88. doi:10.1111/j.1651-2227.2009.01518.x
Fosse NE, Haas SA (2009) Validity and stability of self-reported health among adolescents in a longitudinal, nationally representative survey. Pediatrics 123(3):e496–e501. doi:10.1542/peds.2008-1552
Herman KM, Sabiston CM, Tremblay A, Paradis G (2014) Self-rated health in children at risk for obesity: associations of physical activity, sedentary behaviour, and BMI. J Phys Act Health 11(3):543–552. doi:10.1123/jpah.2012-0124
Klakk H, Chinapaw M, Heidemann M, Andersen LB, Wedderkopp N (2013) Effect of four additional physical education lessons on body composition in children aged 8–13 years—a prospective study during two school years. BMC Pediatr 13:170. doi:10.1186/1471-2431-13-170
Marques A, Sallis JF, Martins J, Diniz J, Carreiro da Costa F (2014) Correlates of urban children’s leisure-time physical activity and sedentary behaviors during school days. Am J Hum Biol 26(3):407–412. doi:10.1002/ajhb.22535
Martinez-Vizcaino V, Martinez MS, Pacheco BN et al (2012) Trends in excess of weight, underweight and adiposity among Spanish children from 2004 to 2010: the Cuenca Study. Public Health Nutr 15(12):2170–2174. doi:10.1017/S1368980012003473
Masuet-Aumatell C, Ramon-Torrell JM, Banque-Navarro M, Davalos-Gamboa Mdel R, Montano-Rodriguez SL (2013) Prevalence of overweight and obesity in children and adolescents from Cochabamba (Bolivia); a cross-sectional study. Nutr Hosp 28(6):1884–1891. doi:10.3305/nutrhosp.v28in06.6881
Morgen CS, Rokholm B, Brixval CS et al. (2013) Trends in prevalence of overweight and obesity in Danish infants, children and adolescents—are we still on a plateau? Plos One 8(7):1–10. doi:10.1371/journal.pone.0069860
O’Dea JA, Dibley MJ (2014) Prevalence of obesity, overweight and thinness in Australian children and adolescents by socioeconomic status and ethnic/cultural group in 2006 and 2012. Int J Public Health 59(5):819–828. doi:10.1007/s00038-014-0605-3
O’Dea JA, Nguyen Hoang TD, Dibley MJ (2011) Plateau in obesity and overweight in a cross sectional study of low, middle and high socioeconomic status schoolchildren between 2004 and 2009. Int J Public Health 56(6):663–667. doi:10.1007/s00038-011-0280-6
Ogden CL, Carroll MD, Kit BK, Flegal KM (2014) Prevalence of childhood and adult obesity in the United States, 2011–2012. JAMA 311(8):806–814. doi:10.1001/jama.2014.732
Olds T, Maher C, Shi ZM et al (2011) Evidence that the prevalence of childhood overweight is plateauing: data from nine countries. Int J Pediatr Obes 6(5–6):342–360. doi:10.3109/17477166.2011.605895
Onis M, Blossner M, Borghi E (2010) Global prevalence and trends of overweight and obesity among preschool children. Am J Clin Nutr 92(5):1257–1264. doi:10.3945/ajcn.2010.29786
Pettman T, Magarey A, Mastersson N, Wilson A, Dollman J (2014) Improving weight status in childhood: results from the eat well be active community programs. Int J Public Health 59(1):43–50. doi:10.1007/s00038-013-0455-4
Prentice-Dunn H, Prentice-Dunn S (2012) Physical activity, sedentary behavior, and childhood obesity: a review of cross-sectional studies. Psychol Health Med 17(3):255–273. doi:10.1080/13548506.2011.608806
Prochaska JJ, Sallis JF, Long B (2001) A physical activity screening measure for use with adolescents in primary care. Arch Pediatr Adolesc Med 155(5):554–559
Reiner M, Niermann C, Jekauc D, Woll A (2013) Long-term health benefits of physical activity—a systematic review of longitudinal studies. BMC Public Health 13:813. doi:10.1186/1471-2458-13-813
Roberts C, Freeman J, Samdal O et al (2009) The Health Behaviour in School-aged Children (HBSC) study: methodological developments and current tensions. Int J Public Health 54(Suppl 2):140–150. doi:10.1007/s00038-009-5405-9
Rokholm B, Baker JL, Sorensen TI (2010) The levelling off of the obesity epidemic since the year 1999—a review of evidence and perspectives. Obes Rev 11(12):835–846. doi:10.1111/j.1467-789X.2010.00810.x
Sardinha LB, Santos R, Vale S et al (2011) Prevalence of overweight and obesity among Portuguese youth: a study in a representative sample of 10–18-year-old children and adolescents. Int J Pediatr Obes 6(2–2):E124–E128. doi:10.3109/17477166.2010.490263
Schmitz KH, Harnack L, Fulton JE et al (2004) Reliability and validity of a brief questionnaire to assess television viewing and computer use by middle school children. J Sch Health 74(9):370–377
Speiser PW, Rudolf MC, Anhalt H et al (2005) Childhood obesity. J Clin Endocrinol Metab 90(3):1871–1887. doi:10.1210/jc.2004-1389
Steinberger J, Jacobs DR, Raatz S, Moran A, Hong CP, Sinaiko AR (2005) Comparison of body fatness measurements by BMI and skinfolds vs dual energy X-ray absorptiometry and their relation to cardiovascular risk factors in adolescents. Int J Obes 29(11):1346–1352. doi:10.1038/sj.ijo.0803026
Wadsworth T, Pendergast PM (2014) Obesity (sometimes) matters: the importance of context in the relationship between obesity and life satisfaction. J Health Soc Behav 55(2):196–214. doi:10.1177/0022146514533347
Wang Y, Lobstein T (2006) Worldwide trends in childhood overweight and obesity. Int J Pediatr Obes 1(1):11–25
Waters E, Silva-Sanigorski A, Burford BJ et al (2014) Interventions for preventing obesity in children. Sao Paulo Med J 132(2):128–129
WHO (2000) Obesity: preventing and managing the global epidemic: report of a WHO consultation. World Health Organization, Geneva
WHO (2007) Growth reference data for 5–19 years. http://www.who.int/growthref/who2007_bmi_for_age/en/. Accessed 15 April 2015
Zhang YX, Wang SR (2013) Rural-urban comparison in prevalence of overweight and obesity among adolescents in Shandong, China. Ann Hum Biol 40(3):294–297. doi:10.3109/03014460.2013.772654
Acknowledgments
The HBSC study in Portugal was funded by public funds: Ministry of Health and Ministry of Education and Science. We thank Professor Bruce Jones for revising the document.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Marques, A., de Matos, M.G. Trends in prevalence of overweight and obesity: are Portuguese adolescents still increasing weight?. Int J Public Health 61, 49–56 (2016). https://doi.org/10.1007/s00038-015-0758-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-015-0758-8