Abstract
Objectives
We examined the effects of duration of residence and age at immigration on mortality among US-born and foreign-born Hispanics aged 25 and older.
Methods
We analyzed the National Health Interview Survey-National Death Index linked files from 1997–2009 with mortality follow-up through 2011. We used Cox proportional hazard models to examine the effects of duration of US residence and age at immigration on mortality for US-born and foreign-born Hispanics, controlling for various demographic, socioeconomic and health factors. Age at immigration included 4 age groups: <18, 18–24, 25–34, and 35+ years. Duration of residence was 0–15 and >15 years.
Results
We observed a mortality advantage among Hispanic immigrants compared to US-born Hispanics only for those who had come to the US after age 24 regardless of how long they had lived in the US. Hispanics who immigrated as youths (<18) did not differ from US-born Hispanics on mortality despite duration of residence.
Conclusions
Findings suggest that age at immigration, rather than duration of residence, drives differences in mortality between Hispanic immigrants and the US-born Hispanic population.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The negative relationship between socioeconomic status and adult mortality and health status has long been considered a “social fact” in the USA (Montez et al. 2011; NCHS 2012). The health and mortality experience of Hispanics in the USA, however, seems to belie this “fact”. Epidemiologic research found that Hispanics generally experienced lower mortality and disease prevalence rates than non-Hispanic (NH) whites and NH blacks. This advantage was referred to as a paradox (Markides and Coreil 1986; Sorlie et al. 1993; Liao et al. 1998) in that Hispanics in general exhibited lower levels of education, higher poverty rates and lower health insurance coverage than NH whites and NH blacks, factors usually associated with poor health and mortality outcomes. Some researchers concluded that the Hispanic advantage in health and mortality was due to selective migration or the healthy immigrant effect, that those who immigrate are healthier than those who do not (Palloni and Ewbank 2004; Markides and Eschbach 2005).
Alternative explanations of the Hispanic mortality advantage focused on methodological issues such as the underreporting of Hispanic mortality in death records and the salmon bias theory which posits that many immigrant deaths are not reported in US vital records because many immigrants return to their home countries to die (Palloni and Arias 2004; Smith and Bradshaw 2006). Subsequent research (Arias et al. 2010) found that only about 5 % of Hispanic mortality is underreported on US death certificates. Turra and Elo (2008) used Social Security data to compare mortality among older Hispanics who died in the USA to those whose deaths occurred outside of the USA, concluding that although there is evidence of the salmon bias, the effect was too small to fully explain the mortality advantage of Hispanics.
Other research examined differences in health and mortality among US-born and foreign-born Hispanics and by duration of residence in the USA (Cho et al. 2004; Borrell and Crawford 2009; Koya and Egede 2007; Eschbach et al. 2007; Markides and Eschbach 2011). Findings that immigrants often have better health outcomes and favorable mortality than US-born NH whites and US-born Hispanics support both the healthy immigrant hypothesis and the cultural buffering theory that immigrant cultural norms and values delay the adoption of unhealthy behaviors found in the USA, such as smoking, alcohol use, unhealthy eating habits and exposure to stressors (Wilkinson et al. 2005; Kaestner et al. 2009). The buffering effects of culture were found to decrease with duration of residence and were not found among US-born Hispanics. For example, subsequent research documented increased body mass index (BMI) among immigrant subgroups after 10 years in the USA (Goel et al. 2004); lower allostatic load among recent immigrant Mexicans compared to US-born Mexican Americans (Peek et al. 2010); increased prevalence of diabetes by length of residence (Oza-Frank et al. 2011); and a reduced advantage for self-reported health, activity limitations and bed days among longer term immigrants (Cho et al. 2004).
While longer residence in the USA reduces the initial advantage of Hispanic immigrants, age at immigration has also been found to affect the adoption of unhealthy risk behaviors and the prevalence of chronic conditions (Roshania et al. 2008; Oza-Frank and Venkat Narayan 2009; Li and Wen 2013). That is, those who immigrate to the USA at younger ages are more negatively “acculturated” than those who immigrate at older ages regardless of duration of residence in the USA.
We examine mortality, looking at the effects of nativity, duration of residence and age at immigration among Hispanics. We draw upon Rumbaut’s (2004) typology of life stages to construct our age at immigration categories. In Rumbaut’s conceptualization, the life stage at which immigration occurs substantially affects both the pace and the degree of acculturation among immigrants thus those who arrive at younger ages should be differentiated from those who arrive at older ages. A small subset of prior research has focused on the combined effects of age at immigration and duration of residence on health behaviors and outcomes such as obesity (Roshania et al. 2008; Oza-Frank and Venkat Narayan 2009); smoking and substance use (Wilkinson et al. 2005; Li and Wen 2013) but the combined effects of these variables on mortality have not been examined.
We analyze the mortality experience of Hispanic immigrants by age at immigration and duration of residence comparing them to Hispanics born in the USA who would be most exposed to “negative acculturation factors” and expected to exhibit poorer health and mortality than foreign-born Hispanics. Examination of mortality highlights unique patterns in the Hispanic population and identifies factors that affect the health and well-being of the Hispanic population.
Methods
Data
This study uses the 1997–2009 National Health Interview Survey (NHIS) restricted-use data linked to death certificate records from the National Death Index (NDI) produced by the National Center for Health Statistics (NCHS). The NHIS, a cross-sectional household interview survey, has been conducted continuously since 1957; its main objective is to monitor the health of the US population on a broad range of health topics. The sampling plan follows a multistage area probability design that provides a representative sampling of households and non-institutional group quarters. African-Americans, Hispanics, Asians and people over age 65 are oversampled. Face-to-face household interviews are conducted. Final response rates for the years 1997–2009 ranged from 63 to 80 % (NCHS 2010).
The NHIS-NDI-linked mortality files link NHIS participants from 1986 to 2009 to death certificate records from the NDI and provide mortality follow-up data from the date of NHIS interview through December 31, 2011. To link NHIS participants with NDI records, NCHS used a probabilistic matching algorithm based on social security number; first name, middle initial and last name; month, day and year of birth; gender; father’s surname, state of birth; race; state of residence and marital status (NCHS 2013). Overall linkage rates varied from 86 to 92 % over the study years.
Because race/ethnicity is self-reported by an NHIS respondent, ethnic misclassification is not a problem with the NHIS-NDI-linked mortality files. However, other data issues could affect analyses based on these files. Hispanic mortality may still be somewhat underestimated because of the salmon bias. Lariscy (2011) identified problems with the quality of record linkages between the NHIS and mortality files, particularly for the Hispanic and Hispanic foreign-born population, leading to biased mortality estimates. Because education is included in the analyses, the study sample is further restricted to those aged 25 and over as some younger adults have not finished their educational careers.
Analyses
The outcome of interest is death by December 31, 2011. Duration of follow-up was calculated using day, month and year of NHIS interview and of death. The primary predictor variable describes individuals’ immigration status. Immigrant Hispanics are described in two ways: (1) age at immigration, and (2) duration of residence in the USA. Age at immigration (AI) is divided into four categories: age 0–17 (youth), age 18–24 (transition to adulthood), age 25–34 (young adulthood) and age 35+ (older adulthood). Duration of residence (DOR) consists of two categories: 0–15 years (recent immigrants) and >15 years (long-term immigrants). When these two variables are combined, immigrants fall into one of eight groups. US-born Hispanics serve as the reference category. By definition, they have the most exposure to the USA. Because island-born Puerto Ricans face adjustment and acculturation issues when moving to the US mainland, they are combined with immigrants.
The demographic control variables are age (at interview), sex, Hispanic national origin and marital status. Age is highly and positively correlated with the risk of death; males have higher death rates than females. Being married is often associated with better health and well-being so those who are currently married are compared to all others (widowed, separated/divorced, never married). Because health outcomes, including mortality, vary by Hispanic national origin group, we control for Hispanic subgroup: Mexican, Puerto Rican, Cuban and Other (Murphy et al. 2013).
People of higher socioeconomic status (SES) also have lower odds of dying than disadvantaged individuals. The SES control variables included are: education, poverty status, and employment status. Education is categorized as: less than high school, high school diploma or equivalent, some college and college degree or more. Poverty status is based on household income; the four categories are: <100, 100–199, 200–399 and ≥400 % of the federal poverty level (FPL). Respondents are categorized as working full-time versus other statuses. Behaviors that affect health are related to their odds of death. The health-related behaviors included in the analyses are smoking status (current, former, never); current heavy drinker (7+ drinks per week for women, 14+ for men); Body Mass Index (BMI) status [underweight (BMI < 18.5), healthy weight (BMI 18.5–24.9), overweight (BMI 25.0–29.9), obese (BMI > 29.9)]; and physical activity (none, activity that does not meet 2008 federal guidelines recommending at least 75 min of vigorous activity or 150 min of moderate activity weekly (US HHS 2008), and physical activity that meets these guidelines).The final control variable describes whether persons had any of a list of chronic conditions (ever had a stroke, cancer, heart disease or diabetes).
Descriptive analyses test for differences in the percentage of Hispanics that die between immigrants and the US-born, and within the immigrant sample across DOR and AI categories. Control variables are also compared across the immigration categories.
Multivariate Cox proportional hazards survival analysis models estimate the odds of death by AI and DOR. Survival analyses use information from all cases including censored cases to estimate the association between immigration factors and the risk of dying, net of control variables. All analyses were carried out using the statistical package SUDAAN 11.0.1, and used weights provided by NCHS.
Results
Descriptive analyses
Over a third of the sample was US-born (37.1 %), 28.4 % were recent immigrants and 34.3 % were long-term immigrants (Table 1). Of the sample, 15.6 % were immigrants who arrived before age 18 (youth), 19.7 % were age 18–24 at arrival (transitioning to adulthood), 16.7 % were 25–34 (young adulthood) and 10.7 % immigrated at 35 or older (older adulthood).
Among long-term immigrants, the percent who died rose with AI. Among recent immigrants, the percent who died was lower among those with AI < 35 than those with AI of 35+. In comparison, 6.1 % of US-born Hispanics had died. Mean age rose with both AI and DOR. US-born Hispanics averaged 43.5 years. The percentage of male immigrants generally declined with increasing AI; 48.3 % of US-born Hispanics were male. The percentage of Mexican immigrants was higher among those with AI < 25 than those who arrived older for both recent and long-term immigrants; the percentage who were Cuban or Other generally increased with AI. Two-thirds of US-born Hispanics were of Mexican origin.
The percentage with less than high school rose with AI among long-term immigrants but not among recent immigrants. US-born Hispanics were the least likely to be high school dropouts; 15.1 % had a college degree. Roughly 30 % of all recent immigrants lived in poverty (<100 % FPL). Among long-term immigrants, the percentage in poverty generally rose with AI. US-born Hispanics were the least likely to be living in poverty. Among long-term immigrants, the percentage who worked full-time generally declined with AI; among recent immigrants, the older-adult immigrants were less likely to work full-time than those with AI < 35. The percentage of immigrants who were married varied from 56.0 to 73.2 %; 58.1 % of US-born Hispanics were married.
Among recent immigrants, the percentage who were obese was higher among those with AI of 35+ than among those who were younger when they arrived; among long-term immigrants, the percentage who were obese was lower among older-adult immigrants than among youth immigrants. About a third (34.9 %) of US-born Hispanics was obese. The percentage of recent immigrants who never smoked was higher for youth immigrants (79.2 %) than for older-adult immigrants (67.8 %) but did not vary by AI for long-term immigrants. The percentage who were current smokers was stable across AI categories among recent immigrants and declined for long-term immigrants. Three in five (60.3 %) US-born Hispanics never smoked; 21.1 % were current smokers. The heavy-drinking percentage ranged from 1.5 to 2.7 % among all immigrants and was 4.8 % for US-born Hispanics. The percentage of immigrants who did not engage in any physical activity rose with AI for all immigrants. Roughly one-third of all youth immigrants engaged in recommended physical activity as did about one in five immigrants with AI ≥ 35. Four in ten (39.1 %) US-born Hispanics engaged in the recommended amount of physical activity and two in ten (19.2 %) had at least one chronic condition. The percentage with a chronic condition rose with AI among both recent and long-term immigrants; for each AI group, the percentage was higher among long-term than recent immigrants. Moreover, among recent immigrants, the percentage with a chronic condition among those with AI ≥ 35 was six times that of those with AI < 25. Among long-term immigrants, in comparison, those with AI ≥ 35 were three times more likely to have a chronic condition than those with AI < 18. Among long-term immigrants, the percentage with at least one chronic condition rose with AI; among recent immigrants, the oldest arrivals were several times more likely to report a chronic condition than younger arrivals. One in five (19.2 %) US-born Hispanics reported a chronic condition.
Survival analysis
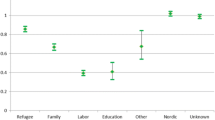
Table 2 presents survival analysis results specifying the effects of DOR and AI on mortality differences between immigrant Hispanics and US-born Hispanics, net of controls. Controlling only for age (Model 1), immigrants who came to the USA as older adults were less likely to die than the US-born regardless of how long they had lived in the USA. Among those who immigrated to the USA as young adults, only those who had lived in the USA for >15 years were advantaged with respect to mortality compared to US-born Hispanics; recent young-adult immigrants were just as likely as US-born Hispanics to have died by the end of 2011. Immigrants who were transitioning from youth to adulthood at the time they arrived in the USA and immigrants who came to the USA as youths were similar to the US-born with respect to mortality regardless of how long they had lived in the USA.
Adjusting for other demographic factors and SES (Model 2), immigrants with AI ≥ 25 were less likely than US-born Hispanics to die regardless of their duration of residence. In addition, recent immigrants who arrived as young adults were only 64 % as likely to die as the US-born. However, long-term immigrants who arrived as young adults did not differ from the US-born in their odds of dying. Both recent and long-term immigrants who arrived as youths did not differ significantly from their US-born counterparts with respect to mortality. Having a college education, income ≥200 % FPL, working full-time and being married were all associated with lower mortality.
Model 3 includes all analytic variables, controlling for demographic characteristics, SES, health risk behaviors and the presence of at least one chronic condition. Young-adult and older-adult arrivals had lower odds of mortality than US-born Hispanics regardless of how long they had resided in the USA. Similarly, recent immigrants who were transitioning to adulthood when they arrived had lower odds of death than US-born Hispanics. However, this pattern did not hold for the long-term transitioning adult immigrants, who were just as likely to die as US-born Hispanics. The mortality experience of youth immigrants did not significantly differ from US-born Hispanics regardless of how long they had lived in the USA. Net of all controls, recent and long-term immigrants with AI < 18 were just as likely to die as US-born Hispanics, and the same was true for long-term immigrants with AI of 18–24.
Age was positively associated with the odds of dying; males were more likely than females to die. Cubans were more likely to die than Mexicans; Other Hispanics were less likely. Hispanics with a college degree had lower odds of dying than those who did not finish high school. Hispanics living ≥200 % FPL had lower odds of dying than those living <100 % FPL. Persons employed full-time were less likely to die than other persons and married Hispanics had lower odds of death than unmarried Hispanics. Underweight persons were almost twice as likely to die as those of healthy weight; overweight persons were less likely to die than healthy weight persons. Smoking was associated with higher odds of dying. Higher physical activity was associated with lower odds of dying. Persons with at least one chronic condition were almost twice as likely to die as those with no such conditions.
Discussion
Our results expand prior research on the mortality patterns of foreign-born Hispanics compared to US-born Hispanics. We explore the combined effect of duration of residence and age at immigration on mortality. Our four age at immigration categories are based on Rumbaut’s (2004) categories; using meaningful life phases to define these categories allows us to better discriminate the effects of age at immigration on health and mortality. Rumbaut’s model posits differences in the pace and degree of adaptation by the life phase at which people immigrate. Those who immigrate at younger ages constitute the 1.5 generation based on their level of exposure to US culture through school and peer associations; that is, they have “come of age” in the USA, while those who immigrated during adulthood are less likely to fully adopt the customs and behaviors of the host country, instead retaining the customs, language and behaviors of their culture of origin.
US-born Hispanics are exposed to US culture throughout their lives and are predicted to be more likely to practice poor eating habits, tobacco use and heavy alcohol use than their Hispanic immigrant counterparts, leading to worse health outcomes and higher mortality. Studies have found that Hispanic immigrants initially do experience better health and lower mortality than US-born Hispanics (Palloni and Arias 2004; Borrell and Crawford 2009) even after controlling for age and SES, but that the advantage diminishes over time due to negative acculturation (Abraido-Lanza et al. 2005; Cho et al. 2004; Antecol and Bedard 2004), the process by which immigrants gradually adopt the poor health habits of the US non-immigrant population. In this explanation, longer US residence will erode any healthy immigrant advantage and the health of immigrants will increasingly resemble that of the US-born. Others have suggested that age at immigration affects the degree of acculturation (Roshania et al. 2008). For example, Rumbaut (2004) found that immigrants who came to the USA as youths (<18 years) were more likely to report themselves as proficient in English (an indirect measure of acculturation) than older immigrants; Angel et al. (2001, 2010) suggested that later-life immigrants are more dependent upon family than those immigrating at an earlier age, indicating they are less likely to interact with and adopt the culture (both positive and negative) of the host country.
We observed a consistent mortality advantage among Hispanic immigrants compared to US-born Hispanics only for those who had come to the USA at age 25+ (as young adults aged 25–34 or older adults aged 35+) regardless of duration of US residence. In Rumbaut’s model, these are individuals who for the most part have completed school and are immigrating for jobs and for better opportunities for their children and may be less exposed to and/or receptive to cultural influences than younger immigrants. In contrast, Hispanics who immigrated as youths (<18) did not differ from US-born Hispanics with respect to mortality regardless of the number of years lived in the USA. In our analysis, duration of residence—whether someone had lived in the USA for ≤15 years or >15 years—affected only immigrants who were aged 18–24 at US arrival. Namely, those who had been in the USA for ≤15 years were less likely than US-born Hispanics to have died, but those in the USA for >15 years were just as likely to die as US-born Hispanics.
These findings suggest that age at immigration, rather than duration of residence, generally drives differences in mortality between Hispanic immigrants and the US-born Hispanic population. Within the 18–24-year-old group, which had a different pattern, degree of acculturation and the pace of adoption of both positive and negative host country behaviors may vary depending upon whether they immigrated to the USA to continue with school, or to work and whether they came with young children or alone (Rumbaut 2004). These different life stages could affect the degree to which the 18–24-year olds embrace the new culture or retain older, more traditional customs. As Rumbaut (2004) suggests, immigrants aged 18–24 are at a transitional stage between youth and full adulthood and may fall somewhere in between with respect to life style choices.
Additional analyses (not shown) using NH Whites as the reference category revealed a similar mortality advantage for those who immigrated at age 25+ irrespective of duration of US residence. These findings support negative acculturation theory suggesting that younger immigrants may be more susceptible to the adoption of unhealthy behaviors than those who immigrate at older ages (Wilkinson et al. 2005; Roshania et al. 2008; Rumbaut 2004). Health habits and life style choices may be well established and less malleable by the age of 25, protecting older adult immigrants from adopting the risky behaviors of a new culture. As seen in Table 1, although US-born Hispanics had higher education and income than the four immigrant groups, they exhibited the highest rates of smoking and excess alcohol intake and were more likely to be obese. Moreover, higher rates of meeting exercise guidelines among US-born Hispanics, while counter-intuitive in the face of higher obesity rates, point to a possible advantage in the availability of leisure time for US-born Hispanics, along with greater access to resources for leisure time pursuits.
We did not address historical period of immigration, that is, whether the effects of age at immigration vary across immigrant cohorts which may have faced different economic and immigration environments when they immigrated. What remains unknown is whether the effects of age at immigration on health behaviors, disease prevalence and mortality among Hispanic immigrants vary by the time period in which they came to the USA. Another limitation of the study is the use of self-reported data on height and weight and health behaviors such as tobacco use, alcohol consumption and leisure time activity. Although underreporting of weight may have biased the results, research using NHANES III found that immigrant women were generally less likely to underreport weight than native US women, while native and immigrant men were equally likely to underreport their weight (Antecol and Bedard 2004). Socially desirable responses to questions on tobacco use and alcohol consumption may also have led to underreporting of high-risk behaviors.
We underestimate mortality due to data issues related to NHIS-NDI linkage quality and salmon bias. Additionally, it is unclear whether return migration is associated with age at immigration. Moreover, this study does not capture whether immigrants remained in the USA continuously from the date of their initial entrance or moved back and forth between their home country and the USA, possibly affecting the extent of their exposure to US cultural norms and behaviors. Nor does the study capture the extent to which immigrant acculturation is affected by residence in ethnic enclaves. Our study omits direct measures of social support and acculturation, such as availability of friends and family who can provide guidance, financial assistance or emotional support, primary language and residential integration. We instead used duration of residence as an indirect measure of acculturation.
Our findings do indicate that in assessing the effect of nativity and duration of residence on Hispanic mortality, it may be important to focus more on age at immigration. The 18–24-year-old immigrant group merits further study of the forces that affect the degree of acculturation among young adult immigrants, as well as the pace of acculturation. Of interest too is whether the health and mortality experience of immigrants from other regions varies by age at immigration. Immigrants increasingly contribute to the racial and ethnic diversity of the US population, and identifying factors that may improve the health and well-being of all groups and reduce disparities in the USA is a key objective of the Healthy People 2020 public health initiative (US HHS 2010).
References
Abraido-Lanza AF, Chao MT, Florez KR (2005) Do healthy behaviors decline with greater acculturation?: Implications for the Latino mortality paradox. Soc Sci Med 61:1243–1255
Angel JL, Buckley CJ, Sakamoto A (2001) Duration or disadvantage? exploring nativity, ethnicity, and health in midlife. J Gerontol Soc Sci 56B(5):S275–S284
Angel RJ, Angel JL, Venegas CD, Bonazzo C (2010) Shorter stay, longer life: age at migration and mortality among the older Mexican-origin population. J Aging Health 22(7):914–931
Antecol H, Bedard K (2004) Unhealthy assimilation: do immigrants converge to American weights? (2004). Claremont Colleges Economics Departments Working Paper No. 2004-06. Available at SSRN: http://ssrn.com/abstract=722805
Arias E, Eschbach K, Schauman WS, Backlund EL, Sorlie PD (2010) The hispanic mortality advantage and ethnic misclassification on US death certificates. Am J Public Health 100(S1):S171–S177
Borrell LN, Crawford ND (2009) All-cause mortality among hispanics in the United States: exploring heterogeneity by nativity status, country of origin, and race in the National Health Interview Survey-linked mortality files. Ann Epidemiol 19(5):336–343
Cho Y, Frisbie WP, Hummer RA, Rogers RG (2004) Nativity, duration of residence, and the health of hispanic adults in the United States. Int Migrat Rev 38(1):184–211
Eschbach K, Stimpson JP, Kuo YF, Goodwin JS (2007) Mortality of Hispanic immigrants and US-born Hispanics at younger ages: a re-examination of recent patterns. Am J Public Health 97(7):1297–1304
Goel MS, McCarthy EP, Phillips RS, Wee CC (2004) Obesity among US immigrant subgroups by duration of residence. JAMA 292:2860–2867
Kaestner R, Pearson JA, Keene D, Geronimus AT (2009) Stress, allostatic load and health of Mexican immigrants. Soc Sci Q 90(5):1089–1111
Koya DL, Egede LE (2007) Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med 22(6):841–846
Lariscy JT (2011) Differential record linkage by Hispanic ethnicity and age in linked mortality studies: implications for the epidemiologic paradox. J Aging Health 23(8):1263–1284
Li K, Wen M (2013) Substance use, age at immigration, and length of residence among adult immigrants in the United States. J Immigrant Minority Health 17:156–164
Liao Y, Cooper RS, Cao G, Durazo-Arvizu R, Kaufman JS, Luke A, McGee DL (1998) Mortality patterns among adult Hispanics: findings from the NHIS, 1986 to 1990. Am J Public Health 88(2):227–232
Markides KS, Coreil J (1986) The Health of Hispanics in the southwestern United States: an epidemiologic paradox. Public Health Rep 101(3):253–265
Markides KS, Eschbach K (2005) Aging, migration and mortality: current status of research on the hispanic paradox. J Gerontol Psychol Soc Sci 60B:68–72
Markides KS, Eschbach K (2011) Hispanic paradox in adult mortality in the United States. In: Rogers RG, Crimmons EM (eds) International Handbook of Adult Mortality, International Handbooks of Population, vol 2. Springer, New York, pp 227–240
Montez JK, Hummer RA, Haywood MD, Woo H, Rogers RG (2011) Trends in the educational gradient of US adult mortality from 1986 through 2006 by race, gender, and age group. Res Aging 33(2):145–171
Murphy SL, Xu J, Kochanek KD (2013) Deaths: final data for 2010. Natl Vital Stat Rep 61(4):1–118
National Center for Health Statistics (2010) 2009 National Health Interview Survey (NHIS) Public Use Data Release: NHIS Survey Description. Hyattsville, MD. Available at: http://ftp.cdc.gov/pub/health_statistics/nchs/Dataset_Documentation/NHIS/2009/srvydesc.pdf
National Center for Health Statistics (2012) Health United States, 2011: with special feature on socioeconomic status and health. Hyattsville, MD. DHHS Pub No. 2012-1232
National Center for Health Statistics (2013) NCHS 2011 linked mortality files matching methodology. Hyattsville, MD. Available at: http://www.cdc.gov/nchs/data/datalinkage/2011_linked_mortality_file_matching_methodology.pdf
Oza-Frank R, Venkat Narayan KM (2009) Effect of length of residence on overweight by region of birth and age at arrival among US immigrants. Public Health Nutr 13(6):868–875
Oza-Frank R, Stephenson R, Venkat Narayan KM (2011) Diabetes prevalence by length of residence among US immigrants. J Immigr Minor Health 13:1–8
Palloni A, Arias E (2004) Paradox lost: explaining the Hispanic adult mortality advantage. Demography 41(3):385–415
Palloni A, Ewbank DC (2004) Selection processes in the study of racial and ethnic differentials in adult health and mortality. In: Anderson NB, Bulatao RA, Cohen B (eds) Critical perspectives on racial and ethnic differences in health in late life. National Academies Press, Washington, DC, pp 171–226
Peek MK, Cutchin MP, Salinas JJ, Sheffield KM, Eschbach K, Stowe RP, Goodwin JS (2010) Allostatic load among non-Hispanic Whites, non-Hispanic Blacks, and people of Mexican origin: effects of ethnicity, nativity, and acculturation. Am J Public Health 100(5):940–946
Roshania R, Venkat Narayan KM, Oza-Frank R (2008) Age at arrival and risk of obesity among US immigrants. Obesity 16(12):2669–2675
Rumbaut RG (2004) Age, Life Stages, and generational cohorts: decomposing immigrant first and second generations in the United States. Int Migrat Rev 38(3):1160–1205
Smith DP, Bradshaw BS (2006) Rethinking the Hispanic paradox: death rates and life expectancy for US non-hispanic white and hispanic populations. Am J Public Health 96(9):1686–1692
Sorlie PD, Backlund E, Johnson NJ, Rogot E (1993) Mortality by Hispanic status in the United States. J Am Med Assoc 270(20):2464–2468
Turra CM, Elo IT (2008) The impact of salmon bias on the Hispanic mortality advantage: new evidence from social security data. Popul Res Policy Rev 27(5):515–530
US Department of Health and Human Services (2008) 2008 Physical Activity Guidelines for Americans. Washington, DC: ODPHP Publication No. U0036. http://www.health.gov/paguidelines/pdf/paguide.pdf. Accessed 3 July 2012
US Department of Health and Human Services (2010) Healthy People 2020. Washington, DC: ODPHP Publication No. B0132. http://www.healthypeople.gov/sites/default/files/HP2020_brochure_with_LHI_508_FNL.pdf. Accessed 25 Feb 2013
Wilkinson AV, Spitz MR, Strom SS, Prokhorov AV, Barcenas CH, Cao YC, Saunders KC, Bondy ML (2005) Effects of nativity, age at migration, and acculturation on smoking among adult Houston residents of Mexican descent. Am J Public Health 95(6):1043–1049
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Holmes, J.S., Driscoll, A.K. & Heron, M. Mortality among US-born and immigrant Hispanics in the US: effects of nativity, duration of residence, and age at immigration. Int J Public Health 60, 609–617 (2015). https://doi.org/10.1007/s00038-015-0686-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-015-0686-7