Abstract
Objectives
To examine prospectively the association between US state income inequality and incidence of heart attack.
Methods
We used data from the National Epidemiologic Survey on Alcohol and Related Conditions (n = 34,445). Respondents completed interviews at baseline (2001–2002) and follow-up (2004–2005). Weighted multilevel modeling was used to determine if US state-level income inequality (measured by the Gini coefficient) at baseline was a predictor of heart attack during follow-up, controlling for individual-level and state-level covariates.
Results
In comparison to residents of US states in the lowest quartile of income inequality, those living in the second [Adjusted Odds Ratio (AOR) = 1.71, 95 % CI 1.16–2.53)], third (AOR = 1.81, 95 % CI 1.28–2.57), and fourth (AOR = 2.04, 95 % CI 1.26–3.29) quartiles were more likely to have a heart attack. Similar findings were obtained when we excluded those who had a heart attack prior to baseline.
Conclusions
This study is one of the first to empirically show the longitudinal relationship between income inequality and coronary heart disease. Living in a state with higher income inequality increases the risk for heart attack among US adults.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Heart attack is the number one leading cause of death in the United States (Hoyert and Xu 2012). In 2009, the proportion of total deaths attributed to heart attack was 24.6 % (599,413/2,437,163) and the crude death rate was 195.2 (Kochanek et al. 2011). Coronary Heart Disease (CHD) is the most common type of heart disease, killing more than 385,000 individuals each year (Kochanek et al. 2011). Every year around 715,000 Americans have a heart attack; of these 525,000 are first heart attacks (Go et al. 2013b). As individuals age throughout the lifespan, the risk for CHD and heart attack increases (Go et al. 2013a). However, this risk disproportionately affects lower socioeconomic status groups (Cirera et al. 2013; Franks et al. 2011), partly due to the clustering of CHD risk factors at the lower end of the socioeconomic hierarchy including high blood pressure, high LDL cholesterol, smoking, (2011), diabetes, being overweight or obese, poor diet, physical inactivity, and negative emotions such as depression and anxiety (Centers for Disease Control and Prevention 2011; Alamian and Paradis 2009; Clark et al. 2009; Kawachi et al. 1994; Sharma et al. 2004). Therefore, there is a significant relationship between absolute income and risk for CVD (Franks et al. 2011; Luksiene et al. 2011; Loucks et al. 2009).
The distribution of wealth and incomes in society is an established social determinant of population health that may operate independently from the effect of individual incomes on health (Pickett and Wilkinson 2009). Income inequality has risen sharply during the past four decades among Organization for Economic Co-operation and Development (OECD) nations, and there is growing concern about its damaging effects on population health (Piketty 2014). For example, the average Gini coefficient among all OECD countries was 0.28 in the mid-1980s and by the late 2000s, it had increased by 10 % to 0.31 (OECD 2011). The pattern of income inequality in the United States since the 2008 recession is one in which the top 10 % (and in particular, the top 1 %) has pulled away from the rest of society, while income growth for the bottom 90 % has remained flat (Stiglitz 2012).
High income inequality has been theorized to be harmful to population health because it erodes social cohesion (Stiglitz 2012) and inhibits the ability of governments to offer social and health services (Kawachi and Kennedy 1999). The erosion of social cohesion has been linked with social isolation (Berkman et al. 2014), which can in turn lead to a lower likelihood of participating in physical activity, and an increase in likelihood in adopting maladaptive coping mechanisms such as smoking and overeating (Baumeister et al. 2005; Marmot 2005; Twenge et al. 2002). Physical inactivity and overeating are behavioral risk factors for overweight and obesity, and diabetes (Siegel et al. 2013), which of course are risk factors for heart attack. Also, the erosion of social cohesion hinders the ability of elected officials to govern, as the political process becomes captured by the rent-seeking behavior of the top 1 % (Stiglitz 2012). The result is a society which is increasingly focused on shoring up the interests of the “haves” against the rest (Kawachi and Kennedy 1999). Research has indicated that US States with high income inequality spend a smaller proportion of their state budget on health care and health services (Kawachi and Kennedy 1999).
The perceived stagnation of incomes for the vast majority—combined with the persistent cultural myth of the “American Dream”—also generates frustration and anxiety. To cope with increased anxiety, people are more likely to engage in maladaptive coping behaviors such as smoking, drug use, and overeating (Wilkinson 1997), which are all behavioral risk factors for CHD. In the United States, higher income inequality at the state level has been linked with increased prevalence of overweight/obesity, hypertension, sedentary behavior (Diez-Roux et al. 2000; Due et al. 2009), alcohol and marijuana consumption (Galea et al. 2007), and is associated with higher levels of the cardiovascular biomarkers hsCRP, sICAM-1, and fibrinogen, which are markers for atherosclerosis (Clark et al. 2012). Among industrialized countries, high income inequality has been linked with smoking, eating energy-dense foods and physical inactivity (Kim et al. 2008) and with CHD risk factors such as higher blood pressure, obesity prevalence, coronary heart disease, and stroke (Kim et al. 2008). The design utilized in these studies has been primarily cross-sectional and, therefore the associations relied on prevalent cases, which is problematic because temporality of the exposure and outcome cannot be identified. Longitudinal studies of income inequality and incident disease have remained sparse. To identify whether exposure to state-level income inequality is a predictor of increased risk for CVD risk factors and heart attack, we used a longitudinal study design and a population-based sample to test the hypothesis that increased income inequality leads to a greater risk for heavier weight statuses, anxiety, smoking, hypertension, and heart attack during follow-up.
Methods
Procedures
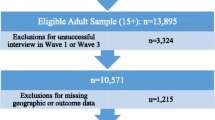
We used data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a representative sample of non-institutionalized US adults aged 18 and older (Grant et al. 2004, 2009). Baseline data collection was carried out in 2001–2002 and included structured diagnostic interviews with 43,093 participants with a response rate of 81 %. Follow-up interviews were conducted between 2004 and 2005 with 34,653 participants responding yielding an 86.7 % response rate of eligible participants. Respondents who participated in both baseline and follow-up questionnaires were included in this investigation. All participants provided written informed consent.
Measures
Area-level covariates
The main exposure was state income inequality, which was measured using the Gini coefficient. The Gini coefficient ranges from 0 (perfect equality, where every household earns exactly the same income) to 1.0 (perfect inequality). The calculation of the Gini coefficient has been described elsewhere (Kennedy et al. 1996). Mathematically the Gini coefficient is defined as one-half of the average difference in incomes between any two individuals randomly sampled from the distribution, normalized on mean income.
For this investigation, the Gini coefficient in each of the 50 states and the District of Columbia was obtained from the 2000 US Census (Hisnanick and Rogers 2007). The distribution of the Gini coefficient among the states was used to categorize the states into quartiles: first (Gini ≤ 0.427), second (Gini = 0.428–0.440), third (Gini = 0.441–0.452), and fourth (Gini > 0.452) quartiles. Other state-level covariates included at the state level included median income, proportion of the state in poverty, proportion black (proportion of the state population that is African-American), population size and census regional division [(1) New England (reference category), (2) Middle Atlantic, (3) East North Central, (4) West North Central, (5) South Atlantic, (6) East North Central, (7) West South Central, (8), Mountain, and (9) Pacific]. The metropolitan statistical area (MSA) was used to determine the type of geographical setting in which the respondent lived at baseline. The setting was defined as urban (within the central city of the MSA), suburban (within the MSA but not within the central city) and rural (not in the MSA). Gini Quartiles were significantly correlated with other state-level characteristics, but were not entirely overlapped with them (correlation coefficients with median income, proportion African-American, proportion poor and state population were −0.26, 0.63, −0.59, and 0.35, respectively.
Individual-level covariates
At baseline, trained interviewers collected sociodemographic data, which included sex, age, total household income in the last 12 months, race/ethnicity (white, black, native, Asian, or Hispanic), education (less than high school, high school, post-secondary, and graduate school) and marital status (couple vs. single).
Outcome measures
At baseline and follow-up, respondents were asked if they had a heart attack or myocardial infarction in the previous year (yes vs. no). Also, interviewers asked if a doctor or health professional had confirmed the diagnosis (yes vs. no). We used two alternative definitions to assess incident heart attack: (1) those who reported experiencing a heart attack (n = 358 including those who had a history of heart attack; and incident cases n = 298, including only those with no history of experiencing a heart attack) and (2) those that reported experiencing a heart attack and reported that a doctor confirmed the diagnosis (n = 327 including those who had a history of heart attack; and incident cases n = 276 including only those with no history of experiencing a heart attack).
Height and weight were measured at baseline and at follow-up, which were then used to determine Body Mass Index (BMI). BMI is equal to mass (kg)/[height (m)]2. Differing thresholds were used to determine four weight status outcomes, which include overweight (BMI ≥ 25 kg/m2), class I obesity (BMI = 30.0–34.9 kg/m2), class II obesity (BMI = 35.0–39.9 kg/m2), and class III obesity (BMI ≥ 40.0 kg/m2).
Respondents were asked at baseline and at follow-up if they had smoked cigarettes in the previous year. If they had answered yes, then they were categorized as a smoker. Participants were also asked if they had high blood pressure or hypertension in the previous year at baseline and follow-up.
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) psychiatric disorders were assessed by Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (Grant et al. 2001). We focused on whether participants qualified for a past-year diagnosis Generalized Anxiety Disorder at baseline and follow-up interviews.
Statistical analyses
Due to the multi-stage sampling design of the NESARC (i.e., multiple participants were sampled from the same primary sampling units, within US States), responses from individuals with the same sampling units are not expected to be independent. Therefore, we used multilevel logistic regression to investigate the prospective association between state-level income inequality and the heart health outcomes such as heart attack, weight status, smoking, hypertension, and anxiety, adjusted for area-level and individual-level characteristics. Additional information regarding the application of this type of analysis in public health research is available elsewhere (Diez-Roux et al. 2000).
To investigate the prospective association between income inequality and the heart health outcomes, we fitted the following groups of models. The first set of analyses involved a null model, with just the outcome, which provides the overall predicted probability and the 95 % plausible value range of the degree of variability between states in risk of each outcome (Table 2). The overall predicted probability indicates the average probability of observing the particular CHD outcome across all US States (Raudenbush and Bryk 2002). The 95 % value range describes the range within which the predicted probability varies across all US States (Raudenbush and Bryk 2002). This should not be confused with confidence intervals, which measure the precision of fixed-effect estimates, whereas the plausible value range measures the estimated variation across US States. Formulas to calculate the overall predicted probability and plausible value range have been provided in Appendix 1. Next, the crude relationship between income inequality and each cardiovascular outcome was estimated. Then, individual-level and state-level sociodemographic characteristics were added to the models. Finally, a cross-level sex by state-level income inequality interaction was tested. Analyses were conducted in two separate groups of models. First, the prospective relationship between income inequality and the health outcomes was investigated in the entire analytic sample (Table 3). Then, the prospective relationship between income inequality and the health outcomes was re-examined after excluding participants who have had a history of heart attack, overweight status, obesity (classes I–III), anxiety, smoking status, and hypertension at baseline (Table 4). Models excluding those with a history of each outcome were conducted separately. This addresses the hypothesis about whether the association between income inequality and CHD is due to the effect of inequality on incidence (i.e., new onset), or whether it is due to the effect of inequality on disease prognosis (i.e., risk of re-infarction among people with existing disease).
For all analyses, multilevel modeling was used to account for clustering of NESARC respondents within primary sampling units (PSU) and within the US states. In other words, the intercepts of state and PSU covariates were allowed to vary. The NESARC’s Wave 2 sampling weights were incorporated into the analyses; these weights account for selection probabilities, participant non-response across both waves, and post-stratify the sample according to the demographics of the US population in 2000. Analyses were performed using Stata (V.12.0) and HLM 6.04 (Hierarchical Linear Modeling, Scientific Software International, Chicago, IL, USA).
Results
Characteristics measured at baseline (n = 43,093) and at follow-up (n = 34,445) of the adults participating in the NESARC are presented in Table 1. Slightly over half the sample was female (52.1 %). At baseline, approximately, 70.9, 11.1, 2.1, 4.4, and 11.6 % were white, black, native, Asian, and Hispanic, respectively. Also, 28.4, 38.9, and 32.7 % reported their household income as low, moderate, and high, respectively. Of the sample, 29.5, 50.7, and 19.7 % resided in urban, suburban, and rural settings, respectively. The average age was 46.4 years (SD = 18.2). There were more respondents living in the most unequal states in comparison to the most equal. For example, at follow-up, the number of people in the 1st, 2nd, 3rd, and 4th Gini Quartiles was 3572 (12.2 %), 6922 (21.4 %), 8527 (26.1 %), and 15,424 (40.3 %), respectively. The number of confirmed heart attacks within the first, second, third, and fourth Gini quartile States was 29 (0.8 %), 69 (1.0 %), 85(1.0 %), and 144 (0.9 %), respectively. The number of new cases of heart attack and the cumulative incidence within the first, second, third, and fourth Gini quartile States was 26 (0.7 %), 63 (0.9 %), 76 (0.9 %), and 118 (0.8 %), respectively.
The distribution of income inequality across the 50 states and District of Columbia is also found in Table 1. For example, the mean (standard deviation), median, Inter Quartile Range (IQR), and range of Gini coefficient across the US States include 0.44 (SD = 0.02), 0.44, 0.025, and 0.293–0.529, respectively. Also, the average state median income, proportion black, proportion poor, and state population were $41,468 (SD = 6,290), 10.8 % (SD = 11.8), 11.5 % (SD = 3.1), and 5,518,077 (SD = 6164026), respectively.
The overall predictive probability and the plausible value ranges determined from the intercept-only models for cardiovascular outcomes are presented (Table 2). The overall predicted probability is the estimated proportion of all NESARC participants experiencing the outcome. The plausible value range indicates that there is variation across the US states. For example, the plausible value range, or the range of proportion experiencing the outcomes estimates across the US states, for heart attack from the incident and recurrent and incident only analyses were 0.5–1.9 %, and 0.4–1.9 %, respectively (Table 2). Also, the plausible value range of overweight status among the US states from the prospective, and incident analyses were 48.5–76.9 %, and 18.8–25.9 %, respectively. These findings indicate that the cardiovascular outcomes varied across the US states.
Analyses of all Wave 2 outcomes
When unadjusted relationships were tested, in comparison to individuals living in the first quartile of Gini index, individuals in the second (OR = 1.49, 95 % CI = 1.07, 2.09), third (OR = 1.36, 95 % CI = 1.08, 1.72), and fourth (OR = 1.45, 95 % CI = 1.15, 1.83) quartiles were significantly more likely to have a heart attack at follow-up (results not shown). Similarly, increased risk for reporting other outcomes with increased risk for Gini index was obtained when heart attack confirmed by a doctor, obese status (class III) and hypertension were the outcomes (results not shown).
When state-level and individual-level characteristics were included in the models, in comparison to those living in the lowest Gini quartile, the risk for heart attack at follow-up was Adjusted Odds Ratio (AOR) = 1.71 (95 % CI = 1.16, 2.53), AOR = 1.81 (95 % CI = 1.28, 2.57), and AOR = 2.04 (95 % CI = 1.26, 3.29) for those in the second, third, and fourth quartile of inequality, respectively (test for linear trend, p = 0.073) (Table 3). Participants living in the second (AOR = 1.69, 95 % CI = 1.10, 2.60), third (AOR = 1.60, 95 % CI = 1.09, 2.35), and fourth (AOR = 1.86, 95 % CI = 1.13, 3.06) Gini quartiles were more likely to report experiencing a heart attack confirmed by a doctor. The inequality by income cross-level interaction was not significant, indicating that the association between income inequality and risk for heart attack did not vary across household income levels. Of the other CHD outcomes, income inequality was associated with only class III obesity. Participants living in the second (AOR = 1.51, 95 % CI = 1.16, 1.98) and third (AOR = 1.46, 95 % CI = 1.12, 1.91) Gini quartiles were more likely to be obese (class III) at follow-up (Table 3). Although the crude relationship between income inequality and increased risk for hypertension was significant, its effect was attenuated when adjusted for confounders. The associations between income inequality and both anxiety and smoking were not significant.
Analysis of incident outcomes
Income inequality was also associated with new cases of heart attack. The crude analysis indicated that in comparison to those who lived in the first Gini quartile, those living in the second, third, and fourth quartiles were OR = 1.51 (95 % CI = 1.06, 2.16),OR = 1.33(95 % CI = 1.00, 1.77), and OR = 1.29 (95 % CI = 0.99, 1.68) more likely to have a heart attack at follow-up, respectively. Similar findings were obtained when the outcome was heart attack confirmed by a doctor (results were not shown).
When state-level and individual-level characteristics were included in the analyses, in comparison to the first Gini quartile, those living in the second, third, and fourth Gini quartiles were AOR = 1.67 (95 % CI = 1.13, 2.47), AOR = 1.68 (95 % CI = 1.18, 2.40), and AOR = 1.95 (95 % CI = 1.20, 3.17), respectively, were more likely to experience a heart attack at follow-up (Table 4). Again, the inequality by income cross-level interaction was not significant. Similar to the findings in which all participants were included at baseline, respondents living in the second (AOR = 1.68, 95 % CI = 1.09, 2.59), third (AOR = 1.50, 95 % CI = 1.01, 2.23), and fourth (AOR = 1.77, 95 % CI = 1.06, 2.95) quartiles were more likely to report experiencing a confirmed heart attack. Income inequality was not significantly associated with anxiety, smoking status, or hypertension among incident cases. Similar to the prospective analysis including all respondents, income inequality was associated with the likelihood of becoming obese (class III) among new cases with no apparent linear trend (Table 4). For example, among those who lived in the second (AOR = 1.61, 95 % CI = 1.16, 2.23) and third (AOR = 1.55, 95 % CI = 1.08, 2.22) Gini quartiles, in comparison to those in the most equal quartiles, there was a significant risk of becoming obese (class III) (Table 4).
For both sets of adjusted analyses, the following groups had lower risks of heart attack during follow-up: females (vs. males), younger individuals (vs. older), and those with moderate and high household incomes (in comparison to those with low household incomes) (Tables 3, 4).
Discussion
This current study is one of the first to investigate the prospective association between US state-level income inequality and heart attack in a representative sample of the US population. Results from previous ecological and cross-sectional studies describing the association between greater income inequality and greater prevalence or risk of CHD indicators are consistent with our findings (Clark et al. 2012; Diez-Roux et al. 2000; Kim et al. 2008; Massing et al. 2004). Our results indicate that income inequality is an important predictor of an increased risk of heart attack and Obesity (class III), but not any of the other CHD indicators such as smoking, hypertension, or other weight status, after adjusting for individual- and state-level characteristics. One possible explanation for our findings may be that the association between income inequality and increased risk for heart attack is not mediated through these pathways (i.e., increased smoking behavior, hypertension, or mental disorders). For example, the mechanism linking inequality to heart disease may be through increased risk for obesity (which we observed), or some other pathway that we were not able to test using the NESARC, such as inflammation.
Our findings extend the evidence summarized in a previous meta-analysis of studies of the association between inequality and health, which found that income inequality is associated with excess mortality and risk of poor self-rated health (Kondo et al. 2009). We found no evidence of a cross-level interaction between income inequality and sex, i.e., the association between inequality and risk of heart attack was similar in men and women. Also, we found no evidence of a significant cross-level interaction between income inequality and individual-level income, i.e., the association between inequality and risk for heart attack did not differ across incomes. This is an indication that income inequality is associated with CHD across all socioeconomic groups, i.e., low-, middle-, and high-income groups.
This study’s results should be interpreted in light of several limitations. Measurement of the outcome was based on self-report, which is prone to misclassification (both false positive and false negative reporting). To the extent that such misclassification was non-differential, i.e., unrelated to exposure status (whether they lived in a high or low inequality state), the resulting bias is likely to have attenuated our associations in the direction of the null.
Also, information was not available on participants’ state of residence at follow-up. Therefore, the risk on CHD outcomes from moving from an equal state to an unequal (or vice versa) could not be determined. Only two time points were collected, separated by 3 years. The effect of income inequality on CHD outcomes might take longer periods of time.
One proposed mechanism underlying the association between income inequality and health is via stressful social comparisons. The most direct test of this hypothesis is through the use of measures of relative deprivation, such as the Yitzhaki index (Adjaye-Gbewonyo and Kawachi 2012). Under this approach, an index of relative deprivation (in the space of incomes) is calculated for each individual, based on the sum of the distances between each individual’s income and the incomes of every other individual in that person’s reference group. According to the theory, the greater the gap between an individual’s own income and the incomes of everyone else in that person’s reference group, the more frustration generated. Consistent with this theory, the Yitzhaki index has been linked to stress-related health outcomes such as smoking, obesity, and mental health services utilization (Eibner et al. 2004). Although we did not directly test the relative deprivation theory, our finding of a link between income inequality and risk of heart attack is consistent with it. Stress resulting from these comparisons might potentially have a negative impact on health behaviors leading to upstream CHD health conditions and illness. For example, stress has been associated with a decreased likelihood in participating in physical activity (Stults-Kolehmainen and Sinha 2014) and an increased likelihood in participating in sedentary behavior and dietary intake of caloric-dense foods (Ng and Jeffery 2003; Oliver et al. 2000; Pendleton et al. 2001).
An alternative account of income inequality posits a contextual mechanism, whereby growing inequality erodes social cohesion and underinvestment in social goods and programs such as public health, education, and social welfare. Also, low social cohesion has been linked with behavioral risk factors of CHD, such as physical inactivity and smoking (Cradock et al. 2009; McNeill et al. 2006; Patterson et al. 2004; Reitzel et al. 2013). Social isolation, stemming from low social cohesion, has shown to be associated with physical inactivity, eating behavior and smoking (Reitzel et al. 2013; Shankar et al. 2011). Also, according to this theory, income inequality could threaten a broad range of health outcomes that are themselves linked to investments in the upstream social determinants of health. This theory anticipates that inequality should be linked not just to heart attack but to other outcomes such as infant mortality, homicide, and infectious diseases (Wilkinson and Pickett 2006). Although our study did not specifically test intervening mechanisms (such as state-level differences in investments in public health and education), our finding of a contextual influence of state-level inequality on risk of heart disease is equally compatible with this theory (Kawachi and Kennedy 1999).
Our conclusions were similar whether we included or excluded individuals with a history of heart disease at baseline. This suggests that inequality is associated with new onset of disease as well as disease prognosis. A recent study used data collected from patients aged 65 years and older, and hospitalized in 2006–2008 with a principal diagnosis of acute myocardial infarction, heart failure or pneumonia (Lindenauer et al. 2013). They observed income inequality at the US state level was associated with rehospitalization for acute myocardial infarction, heart failure and pneumonia (Lindenauer et al. 2013).
In summary, this study demonstrates that state-level income inequality is a predictor of CHD outcomes such as heart attack and obesity at follow-up, but not smoking, hypertension, or a diagnosis of Generalized Anxiety Disorder. Respondents living in more unequal states were significantly more likely to have a heart attack at follow-up. Further investigation to gain a better understanding of how income inequality leads to increased risk for CHD, such as the erosion of social cohesion and solidarity, or increased inaccessibility to health and social services, is warranted. In addition, research is needed that examines cardiovascular outcomes in relation to changes in CHD outcomes across varying time periods, which would quantify the expected benefits on health of state-level policies to reduce income inequality.
References
Adjaye-Gbewonyo K, Kawachi I (2012) Use of the Yitzhaki Index as a test of relative deprivation for health outcomes: a review of recent literature. Soc Sci Med 75(1):129–137. doi:10.1016/j.socscimed.2012.03.004
Alamian A, Paradis G (2009) Clustering of chronic disease behavioral risk factors in Canadian children and adolescents. Prev Med 48(5):493–499. doi:10.1016/j.ypmed.2009.02.015
Baumeister RF, DeWall CN, Ciarocco NJ et al (2005) Social exclusion impairs self-regulation. J Pers Soc Psychol 88(4):589–604. doi:10.1037/0022-3514.88.4.589
Berkman LF, Kawachi I, Glymour M (2014) Social epidemiology, 2nd edn. Oxford University Press
Cirera L, Huerta JM, Chirlaque MD et al (2013) Unfavourable life-course social gradient of coronary heart disease within Spain: a low-incidence welfare-state country. Int J Public Health 58(1):65–77. doi:10.1007/s00038-012-0374-9
Clark AM, DesMeules M, Luo W et al (2009) Socioeconomic status and cardiovascular disease: risks and implications for care. Nat Rev Cardiol 6(11):712–722. doi:10.1038/nrcardio.2009.163
Clark CR, Ridker PM, Ommerborn MJ et al (2012) Cardiovascular inflammation in healthy women: multilevel associations with state-level prosperity, productivity and income inequality. BMC Public Health 12:211. doi:10.1186/1471-2458-12-211
Cradock AL, Kawachi I, Colditz GA et al (2009) Neighborhood social cohesion and youth participation in physical activity in Chicago. Soc Sci Med 68(3):427–435. doi:10.1016/j.socscimed.2008.10.028
Diez-Roux AV, Link BG, Northridge ME (2000) A multilevel analysis of income inequality and cardiovascular disease risk factors. Soc Sci Med 50(5):673–687
Due P, Damsgaard MT, Rasmussen M et al (2009) Socioeconomic position, macroeconomic environment and overweight among adolescents in 35 countries. Int J Obes 33(10):1084–1093. doi:10.1038/ijo.2009.128
Eibner C, Sturn R, Gresenz CR (2004) Does relative deprivation predict the need for mental health services? J Ment Health Policy 7(4):167–175
Franks P, Winters PC, Tancredi DJ et al (2011) Do changes in traditional coronary heart disease risk factors over time explain the association between socio-economic status and coronary heart disease? BMC Cardiovasc Disord 11:28. doi:10.1186/1471-2261-11-28
Galea S, Ahern J, Tracy M et al (2007) Neighborhood income and income distribution and the use of cigarettes, alcohol, and marijuana. Am J Prev Med 32(6 Suppl):S195–S202. doi:10.1016/j.amepre.2007.04.003
Go AS, Mozaffarian D, Roger VL et al (2013a) Executive summary: heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 127(1):143–152. doi:10.1161/CIR.0b013e318282ab8f
Go AS, Mozaffarian D, Roger VL et al (2013b) Heart disease and stroke statistics—2013 update: a report from the American Heart Association. Circulation 127(1):e6–e245. doi:10.1161/CIR.0b013e31828124ad
Grant BF, Dawson DA, Hasin DS (2001) The alcohol use disorder and associated disabilities interview schedul-DSM-IV version. National Institute on Alcohol Abuse and Alcoholism, Bethesda
Grant BF, Dawson DA, Stinson FS et al (2004) The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug Alcohol Depend 74(3):223–234. doi:10.1016/j.drugalcdep.2004.02.004
Grant BF, Goldstein RB, Chou SP et al (2009) Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry 14(11):1051–1066. doi:10.1038/mp.2008.41
Hisnanick JJ, Rogers AL (2007) Household income inequality measured based on the ACS data: 2000–2005 program participation and income transfers branch. Housing and Household Economic Statistics Division. U.S. Census Bureau
Hoyert DL, Xu J (2012) Deaths: Preliminary Data for 2011. In: Statistics DoV (ed). vol 61. National Vital Statistics Reports
Kawachi I, Kennedy BP (1999) Income inequality and health: pathways and mechanisms. Health Serv Res 34(1 Pt 2):215–227
Kawachi I, Sparrow D, Vokonas PS et al (1994) Symptoms of anxiety and risk of coronary heart disease. The Normative Aging Study. Circulation 90(5):2225–2229
Kennedy BP, Kawachi I, Prothrow-Stith D (1996) Income distribution and mortality: cross sectional ecological study of the Robin Hood index in the United States. BMJ 312(7037):1004–1007
Kim D, Kawachi I, Hoorn SV et al (2008) Is inequality at the heart of it? Cross-country associations of income inequality with cardiovascular diseases and risk factors. Soc Sci Med 66(8):1719–1732. doi:10.1016/j.socscimed.2007.12.030
Kochanek KD, Xu J, Murphy BS, et al (2011) Deaths: final data for 2009. In: Statistics DoV (ed). vol 60. National Vital Statistics Reports
Kondo N, Sembajwe G, Kawachi I et al (2009) Income inequality, mortality, and self rated health: meta-analysis of multilevel studies. BMJ 339:b4471. doi:10.1136/bmj.b4471
Lindenauer PK, Lagu T, Rothberg MB et al (2013) Income inequality and 30 day outcomes after acute myocardial infarction, heart failure, and pneumonia: retrospective cohort study. BMJ 346:f521. doi:10.1136/bmj.f521
Loucks EB, Lynch JW, Pilote L et al (2009) Life-course socioeconomic position and incidence of coronary heart disease: the Framingham Offspring Study. Am J Epidemiol 169(7):829–836. doi:10.1093/aje/kwn403
Luksiene DI, Baceviciene M, Tamosiunas A et al (2011) Health, alcohol and psychosocial factors in Eastern Europe study: dietary patterns and their association with socio-demographic factors in the Lithuanian urban population of Kaunas city. Int J Public Health 56(2):209–216. doi:10.1007/s00038-010-0170-3
Marmot M (2005) Social determinants of health inequalities. Lancet 365(9464):1099–1104. doi:10.1016/S0140-6736(05)71146-6
Massing MW, Rosamond WD, Wing SB et al (2004) Income, income inequality, and cardiovascular disease mortality: relations among county populations of the United States, 1985 to 1994. South Med J 97(5):475–484
McNeill LH, Kreuter MW, Subramanian SV (2006) Social environment and physical activity: a review of concepts and evidence. Soc Sci Med 63(4):1011–1022. doi:10.1016/j.socscimed.2006.03.012
Centers for Disease Control and Prevention (2011) Million hearts: strategies to reduce the prevalence of leading cardiovascular disease risk factors–United States. MMWR Morb Mortal Wkly Rep 60(36):1248–1251
Ng DM, Jeffery RW (2003) Relationships between perceived stress and health behaviors in a sample of working adults. Health Psychol 22(6):638–642. doi:10.1037/0278-6133.22.6.638
OECD (2011) Growing income inequality in OECD countries: what drives it and how can policy tackle it?
Oliver G, Wardle J, Gibson EL (2000) Stress and food choice: a laboratory study. Psychosom Med 62(6):853–865
Patterson JM, Eberly LE, Ding Y, Hargreaves M (2004) Associations of smoking prevalence with individual and area level social cohesion. J Epidemiol Community Health 58(8):692–697. doi:10.1136/jech.2003.009167->
Pendleton VR, Willems E, Swank P et al (2001) Negative stress and the outcome of treatment for binge eating. Eat Disord 9(4):351–360. doi:10.1080/106402601753454912
Pickett KE, Wilkinson RG (2009) The spirit level: why greater equality makes societies stronger. Bloomsbury Press, New York
Piketty T (2014) Capital in the Twenty-First Century (trans: Goldhammer A). Harvard University Press, United States
Raudenbush SW, Bryk AS (2002) Hierarchical linear models: applications and data analysis methods (Advanced Quantitative Techniques in Social Sciences), 2nd edn. Sage Publications Inc, Thousand Oaks
Reitzel LR, Kendzor DE, Castro Y et al (2013) The relation between social cohesion and smoking cessation among Black smokers, and the potential role of psychosocial mediators. Ann Behav Med 45(2):249–257. doi:10.1007/s12160-012-9438-6
Shankar A, McMunn A, Banks J, Steptoe A (2011) Loneliness, social isolation, and behavioral and biological health indicators in older adults. Health Psychol 30(4):377–385. doi:10.1037/a0022826
Sharma S, Malarcher AM, Giles WH et al (2004) Racial, ethnic and socioeconomic disparities in the clustering of cardiovascular disease risk factors. Ethn Dis 14(1):43–48
Siegel M, Luengen M, Stock S (2013) On age-specific variations in income-related inequalities in diabetes, hypertension and obesity. Int J Public Health 58(1):33–41. doi:10.1007/s00038-012-0368-7
Stiglitz JE (2012) The price of inequality: how today’s divided society endangers our future. W.W. Norton and Company, New York City
Stults-Kolehmainen MA, Sinha R (2014) The effects of stress on physical activity and exercise. Sports Med 44(1):81–121. doi:10.1007/s40279-013-0090-5
Twenge JM, Catanese KR, Baumeister RF (2002) Social exclusion causes self-defeating behavior. J Pers Soc Psychol 83(3):606–615
Wilkinson RG (1997) Socioeconomic determinants of health. Health inequalities: relative or absolute material standards? BMJ 314(7080):591–595
Wilkinson RG, Pickett KE (2006) Income inequality and population health: a review and explanation of the evidence. Soc Sci Med 62(7):1768–1784. doi:10.1016/j.socscimed.2005.08.036
Acknowledgments
This work was supported by NIH-grant number MH087544. RP was a Canadian Institutes of Health Research postdoctoral fellowship recipient #234617.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Pabayo, R., Kawachi, I. & Gilman, S.E. US State-level income inequality and risks of heart attack and coronary risk behaviors: longitudinal findings. Int J Public Health 60, 573–588 (2015). https://doi.org/10.1007/s00038-015-0678-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-015-0678-7