Abstract
Objectives
This study presents a cost-effectiveness analysis of salt reduction policies to lower coronary heart disease in Syria.
Methods
Costs and benefits of a health promotion campaign about salt reduction (HP); labeling of salt content on packaged foods (L); reformulation of salt content within packaged foods (R); and combinations of the three were estimated over a 10-year time frame. Policies were deemed cost-effective if their cost-effectiveness ratios were below the region’s established threshold of $38,997 purchasing power parity (PPP). Sensitivity analysis was conducted to account for the uncertainty in the reduction of salt intake.
Results
HP, L, and R + HP + L were cost-saving using the best estimates. The remaining policies were cost-effective (CERs: R = $5,453 PPP/LYG; R + HP = $2,201 PPP/LYG; R + L = $2,125 PPP/LYG). R + HP + L provided the largest benefit with net savings using the best and maximum estimates, while R + L was cost-effective with the lowest marginal cost using the minimum estimates.
Conclusions
This study demonstrated that all policies were cost-saving or cost effective, with the combination of reformulation plus labeling and a comprehensive policy involving all three approaches being the most promising salt reduction strategies to reduce CHD mortality in Syria.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Noncommunicable diseases (NCDs) are the leading cause of mortality worldwide, accounting for more than 60 % of all deaths (WHO 2005). This burden is expected to increase over the next few decades, particularly within developing countries that have already experienced a drastic rise in cardiovascular disease (CVD) (Murray and Lopez 1997; WHO 2011). In the Eastern Mediterranean Region (EMR), CVD mortality accounts for nearly one out of three deaths and is primarily due to coronary heart disease (CHD) (WHO 2008). Within Syria alone (population ≈ 21 million; 2010), CHD mortality has increased by two-thirds between 1996 and 2006, and together with stroke accounts for nearly half of the country’s all-cause mortality (Maziak et al. 2007; Rastam et al. 2012).
The recent increase in CHD mortality in Syria can be mostly explained by increases in population systolic blood pressure (SBP). Between 1996 and 2006, nearly 2,700 CHD deaths have been attributed to a 4.5 and 9.5 % increase in SBP among Syrian men and women 25 years and older, respectively (Rastam et al. 2012). Elevated SBP levels, however, can be largely modified by changes in dietary salt intake (He and MacGregor 2004). In fact, the World Health Organization (WHO) estimates that a 5-gram reduction in daily salt intake worldwide has the potential to reduce global CVD rates by 17 % (WHO 2010). As a result, policies that aim to reduce salt intake at the population level have been implemented in high-income nations and have been shown to be cost-effective in reducing CHD (Cappuccio et al. 2011; Cobiac et al. 2010; Selmer et al. 2000; Smith-Spangler et al. 2010; Wang and Labarthe 2011). Low to middle income countries, however, have been slow to adopt such policies and due to their limited resources are likely to be more readily persuaded to do so by a comprehensive cost-effectiveness analysis (CEA) of such policies (Asaria et al. 2007; Murray et al. 2003; WHO 2002).
Under project MedCHAMPS (Mediterranean Studies of Cardiovascular disease and Hyperglycaemia: Analytical Modelling of Population Socio-economic transitions), an extensive cost-effective analysis of salt reduction policies has been conducted in four middle-income Eastern Mediterranean countries (Palestine, Syria, Tunisia, and Turkey) (Mason et al. 2014). This paper extends the original four-country analysis by recommending the best policy option for Syria based on pre-crisis data and discussing the impact of the country’s current socioeconomic and political situation on the study results.
Methods
Dietary salt is typically introduced during the preparation or seasoning of food in the home, and/or the addition of salt by manufacturers during food processing. Both sources are common in many countries of the Eastern Mediterranean. A shift from a traditional diet to a more westernized diet high in saturated fat, cholesterol, salt, and refined carbohydrates has been observed in numerous countries within the region. A large proportion of the population also continues to add salt to the foods that they consume (Musaiger and Al-Hazzaa 2012). Based on the sources of salt consumption in the Eastern Mediterranean region, and the success of previous salt reduction policies in other settings (Appel et al. 2012; Cappuccio et al. 2011), this study evaluated three potential policies: (1) a nationwide health promotion campaign aimed at encouraging individuals to reduce their salt intake; (2) requiring manufacturers to label the salt content on prepackaged foods to provide low-salt food options to the public; and (3) mandatory reformulation requiring manufacturers to lower the salt content of prepackaged foods. Comprehensive strategies involving combinations of the three policies were also included in the analysis. The costs and benefits of each policy option were evaluated over a 10-year period (2010–2020) and compared with those that would accrue in the absence of any policy for reducing dietary salt intake.
The following sections provide a brief summary of the health outcomes, cost calculations, and cost-effectiveness model. Detailed breakdown of the costs calculations are provided elsewhere (Mason et al. 2014). All data used in this analysis preceded the current political crisis in Syria.
Health outcomes
The benefit of each policy option was defined as the number of life-years gained (LYGs) from the decrease in CHD events among Syrian adults (25 years and older). The IMPACT CHD model in Syria (Rastam et al. 2012) was extended to estimate the effect of the policies on CHD mortality. The resulting number of LYGs was then estimated based on the method described by Unal et al. (2005) and Fidan et al. (2007).
Details of the IMPACT CHD model are presented elsewhere (Capewell et al. 2007). Briefly, the model was used to estimate the decline in CHD mortality resulting from projected changes in population risk factors and utilization of CHD treatments over a period of time. The major CVD risk factors included in the model were smoking, SBP, cholesterol, body mass index (BMI), and diabetes. Treatments for the following CHD events in the hospital and community setting were included in the model: myocardial infarction, congestive heart failure, angina, and hypertension. The number of CHD deaths expected under each policy was calculated under the assumptions that (1) current trends in all risk factors, except SBP, and all treatment use continue through 2020 (Rastam et al. 2012), and that (2) SBP levels would decreased by 1.2 mm/Hg (minimum, 0.93 mm/Hg; maximum, 1.47 mm/Hg) for every 1 gram reduction in daily salt intake (He and MacGregor 2004). The number of CHD deaths expected in the absence of any policy was calculated using indirect standardization, assuming that 2010 mortality rates persisted through 2020. The potential number of LYG was then calculated by multiplying the reduction in CHD deaths by the estimated median survival (Capewell et al. 2007; MacIntyre et al. 2000) for those with diagnosed CHD, undiagnosed CHD, and those free of CHD.
Estimates of the effectiveness of each policy were obtained from a review of existing literature (Asaria et al. 2007; Cappuccio et al. 2011; Hooper et al. 2004; Mohan et al. 2009; Smith-Spangler et al. 2010). Estimates were extracted from studies reporting the effectiveness of the individual and combined policies on changing the behavior of general populations. Details of the literature review are discussed in the parent study (Mason et al. 2014). The data regarding reduction in daily salt intake expected over a 10-year period are presented for each policy in column 2 of Table 1. Due to unavailability of Syrian data, salt consumption at baseline (13.75 grams/person/day; minimum, 11 grams/person/day; maximum, 16.5 grams/person/day) was based on data from a neighboring population with expected similarities with the Syrian population (Palestine). Salt intake levels expected under each policy were assumed to not fall under 3 grams/person/day.
Inputs into the IMPACT CHD model were obtained from existing national resources and international literature. Population data for Syria were obtained from the Syrian Bureau of Statistics (CBS 2011); numbers were comparable to those provided by the U.N. Department of Economics and Social Affairs (UN 2011). Past numbers of CHD-related deaths were obtained from the WHO Global Health Observatory (WHO 2004) and cross-validated with data provided by the 2004 Aleppo Household Survey (Maziak et al. 2005). Trends in population risk factors were obtained from two epidemiological studies conducted in Syria: the 2003 STEPwise survey (WHO 2003a) and the 2006 Aleppo Diabetes Survey (Al Ali et al. 2011); and from a neighboring population with expected similarities with the Syrian population (Palestine). Information on CHD patient numbers and treatment uptakes was obtained from hospital and outpatient surveys conducted by the Syrian Center for Tobacco Studies (SCTS) in 2009 for the IMPACT CHD model in Syria (Rastam et al. 2012).
Costs
The net cost of each policy was calculated as the total policy cost minus health care savings related to CHD. All costs were collected for 2010 prices in local currency and then converted to international dollars using purchasing power parity (PPP) exchange rates to allow for international comparisons (UN 2013). All future costs were inflated by the country-specific inflation rate of 4.4 % and then discounted by 3 % (WHO 2003b).
CHD health care savings
Health care costs were calculated as the sum of the treatment costs for CHD events in the hospital and community settings. The total treatment cost of each CHD event was calculated as the product of the unit cost of the treatment, frequency of use per day, length of hospital stay in days (if applicable), number of CHD patients per year, and the uptake level of the treatment. The total cost of each CHD event was obtained by summing the individual costs of all treatments, procedures, and/or medical visits required for the event. The health care savings for each policy were then calculated as the health care cost at baseline minus the health care cost for the given policy.
Treatment costs and utilization were obtained by the MedCHAMPS team from the Ministry of Health and were based on typical reimbursement rates in Syria. Patient numbers and treatment uptakes were extracted from the IMPACT CHD model in Syria (described above in the “Health outcomes” section).
Total policy costs
Total costs were divided into public sector and private sector components. Public sector costs included the cost to implement the health promotion campaign and the cost to develop and enforce a law requiring manufacturers to comply with the labeling and reformulation policies. These costs were based on a combination of comparable past experiences within the country and the opinion of experts (Mason et al. 2014). Private costs consisted of the financial costs to the food industry of labeling salt content on packages and of reformulating the salt content within products. These costs were obtained through interview-based surveys of local manufacturers of food items that are considered major sources of dietary salt, such as dairy products, bakery, butter and margarines, pickles, and salty snacks (Mason et al. 2014).
Implementation costs for the health promotion campaign included costs for promotional materials and publicity through television and radio advertisements. These estimates included the cost of both material and human resources. It was assumed that the health promotion campaign would be repeated annually over the 10-year study period. A single step policy change was assumed for the labeling and reformulation policies. Implementation costs would occur the first year, followed by costs to monitor and enforce the laws associated with each policy. These costs were collected from official departments by the MedCHAMPS team using a pre-tested standardized questionnaire.
Cost-effectiveness model
All costs and benefits were projected annually over a 10-year period and summed to obtain the total cost and benefit of each intervention. Average cost-effectiveness ratios (CER) were calculated and compared to regional cost-effectiveness thresholds, which represents the cost that an individual is willing to pay to gain one additional year of life (WHO 2003b). Policies with ratios <$13,000 PPP/LYG were deemed as very cost effective, and those with ratios between $13,000 and $38,997 PPP/LYG were deemed as cost effective (WHO 2013; UN 2013). Incremental cost-effectiveness ratios were used to compare non-cost-saving policies (WHO 2003b).
Multi-way sensitivity analysis using Brigg’s analysis of extremes was conducted to account for uncertainties in some of the values used in the IMPACT model (Briggs et al. 1994). The model assumed minimum and maximum values to be the lower and upper limits of 95 % confidence intervals, if available, or the best value ± 20 % (Capewell et al. 2007). The minimum and maximum reduction values in daily salt intake expected under each policy were obtained from a review of the literature (Asaria et al. 2007; Cappuccio et al. 2011; Hooper et al. 2004; Mohan et al. 2009; Smith-Spangler et al. 2010).
Results
Benefits
All salt reduction interventions resulted in a gain in life years compared to baseline (Table 1). Nearly 32,000 life years (uncertainty interval: 11,192–49,866 LYGs) could be saved over the 10-year period if all three interventions were implemented; this is nearly six times the number of LYG under the health promotion campaign alone, nearly three times under the labeling campaign alone or reformulation alone, and nearly twice that of reformulation combined with health promotion or with labeling.
Costs
CHD health care costs at baseline are projected to be PPP $3.139 billion over the 10-year period. Each policy resulted in a decrease in CHD-related health care costs, with the combinations involving reformulation resulting in the largest decrease (Table 2). The combination of all three policies resulted in a 4.5 % decrease in health care costs; this was more than twice the decrease expected under reformulation with the health promotion campaign and reformulation with labeling. Costs to the public sector were relatively low for all interventions, ranging from PPP $1.397 million for labeling alone and reformulation alone to PPP $5.634 million for the combination of all three interventions. Private sector costs, on the other hand, were large for all strategies involving reformulation (>PPP $96 million).
The health promotion campaign alone, labeling alone, and the combination of all three policies were cost-saving using the best effectiveness estimates. However, only labeling alone was cost-saving using the minimum effectiveness estimates, while all but the combination of reformulation with the health promotion campaign were cost-saving using the maximum estimates.
Cost-effectiveness
All interventions that were not cost-saving were very cost-effective (<$13,000 PPP/LYG) using both the best and maximum effectiveness estimates (Table 2). The cost per LYG for reformulation plus health promotion and for reformulation plus labeling was less than half of that for reformulation alone. Using the minimum effectiveness estimates, the health promotion campaign alone and reformulation alone were no longer very cost-effective; however, they were cost-effective (<$38,997 PPP/LYG). The cost per LYG for both strategies were nearly three times that of reformulation plus health promotion and of the combination of the three policies; and more than seven times that of reformulation plus labeling (details in Table 2).
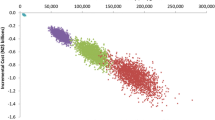
Reformulation alone and reformulation plus health promotion were inferior to reformulation plus labeling policy using the best effectiveness estimates (i.e. they were more costly than reformulation plus labeling with no added benefit) (Fig. 1). Using the minimum effectiveness estimates, the combination of all three policies was also inferior to reformulation plus labeling. Reformulation plus labeling was weakly superior to health promotion alone using the minimum estimates (i.e. health promotion is effective but at a higher marginal cost than reformulation plus labeling). An additional $1,116 PPP/LYG would be required to implement reformulation plus labeling compared to health promotion alone (details in Table 2; Fig. 1).
Cost-effectiveness of salt reduction policies that aim to reduce coronary heart disease among adults 25 years and older in Syria, 2010–2020 HP health promotion campaign, L labeling of salt content on prepackaged foods, R reformulation of salt content in prepackaged foods Costs presented in international dollars using purchasing power parity (PPP). Filled square policies that are cost-saving. Filled triangle policies that are dominated by the alternatives
Discussion
Main findings
This is the first study to examine salt reduction policies to lower CHD mortality in Syria and to discuss the findings within the context of the country’s current political situation. It shows that all tested policies were cost-saving and/or cost-effective. The combination of the health promotion campaign, labeling, and reformulation produced the largest gain in life-years with a net savings over baseline using both the best and maximum estimates. Reformulation plus labeling is the most effective non-cost-saving policy using both the best and minimum estimates. All policies were cost-saving using the maximum estimates, with the exception of reformulation plus health promotion.
Feasibility of the policies in Syria
Almost all of the costs (95–99 %) associated with reformulation were those required to implement the policy. Such costs are expected to fall on food manufacturers and other members of the private sector during the initial year of policy implementation. The cost to implement each policy involving reformulation comprises approximately 3.5 % of private health care expenditures spent in Syria in 2010 (WHO 2013a). Almost all costs associated with the health promotion campaign and labeling policy, on the other hand, are related to policy monitoring costs (100 and 89 %, respectively). The annual cost to monitor these policies, however, comprises less than 0.007 % of the public health care expenditure incurred in Syria in 2010 (WHO 2013a). Similar monitoring costs are expected for reformulation and for reformulation with labeling strategies. Annual costs to monitor reformulation with the health promotion campaign, and the combination of all three policies are slightly larger, comprising approximately 0.02 % of Syria’s public health care expenditure in 2010 (WHO 2013a). Given the significantly lower cost of these policies to the public sector, offering subsidies to food manufacturers to encourage proper implementation of the reformulation policy could be a viable option.
It is important to note that the model building and CEA analysis was conducted from 2010 to 2012, and thus all data used in this study were from the year 2010 or earlier. Many of the assumptions used in the IMPACT model to estimate the benefits of each policy may not be applicable given the current political situation in Syria. For example, projected population estimates and uptake of CHD treatments were based on recent trends occurring prior to 2010. Population numbers and the uptake of treatments, however, have been severely impacted by the current political unrest. As of June 2013, an estimated 1.6 million Syrians have registered as refugees in neighboring countries: over 600,000 in Jordan, 550,000 in Lebanon, and nearly 160,000 in Iraq (WHO 2013b). In addition, more than 80,000 deaths are estimated to have occurred as a result of the crisis (WHO 2013c).
Uptake of CHD treatments are likely to be affected by the targeting of public health workers, health care facilities, and transportation services. Nearly 470 health workers are reported to be currently imprisoned and approximately 15,000 physicians have been forced to flee (Brundtland et al. 2013). Across the country, approximately three out of five public hospitals and two out of five public health centers are out of service or running at limited capacity due to damage, lack of safety, or shortages of fuel and electricity. In addition, three-quarters of ambulances are damaged and over half are completely out of service (WHO 2013d, e). These targeted attacks on the health care sector, together with government restrictions and challenges in the international aid system that prevent delivery of medical supplies and care, have left large parts of Syria completely cut off from medical assistance (Brundtland et al. 2013). The decreased availability of timely and adequate treatment resulting from the current crisis will likely increase future CHD mortality and subsequent health care costs in Syria. Accordingly, our analysis provides best scenario estimates that need to be modified as the final toll of the current crisis on the population and heath care sector becomes available, and as the outline of the rebuilding phase becomes apparent.
Strengths and limitations
An important strength of this study was the inclusion of industry cost data that were collected directly from food manufacturers in Syria through interview-based surveys. The main limitation of the study was the variable completeness and quality of the data. As reported earlier, data from a comparable neighboring population (Palestine) were used, when possible, if Syrian data were unavailable. The source of dietary salt intake and evidence of the effectiveness of the policies to reduce intake were extracted from other countries. These factors may differ in the Syrian population. For instance, the acceptability of a health promotion campaign and the proportion of prepackaged foods produced locally within the country may not be comparable to the countries for which the effectiveness estimates were obtained. However, to account for uncertainties in data quality, sensitivity analysis was used to generate minimum, best, and maximum estimates of the benefit of each policy. Despite all efforts, moreover, complete and reliable data required to compute productivity loss attributed to CHD morbidity were not available for all the region and thus productivity loss was excluded from the cost-effectiveness analysis. However, the inclusion of productivity loss would have only further increased the benefit of the policies without any additional cost; making them even more cost-effective. In addition, the IMPACT CHD model assumed that the 2010 level of CHD rates persisted through the 10-year time frame. Rates, however, are increasing in Syria due to escalating trends in population risk factors (Rastam et al. 2012). Inclusion of rising rates in the model would have, again, resulted in an increase of benefit without any additional cost.
Conclusion
A comprehensive approach involving a nation-wide health promotion campaign, the labeling of salt content on packaged foods, and mandatory reformulation of salt content in manufactured foods is the most promising salt reduction measure to reduce the burden of CHD in Syria using the best and maximum effectiveness estimates. These policy options would save the greatest number of lives with a net savings compared to baseline. The high implementation costs borne by the private sector could be at least partially subsidized by the public sector, with this additional cost to the public sector being offset by a large savings in CHD-related health care costs. A practical option, however, would be to use the most conservative effectiveness estimates, for which the reformulation plus labeling policy would be the most cost-effective policy to reduce the burden of CHD. A shift from secondary to primary prevention of coronary heart disease is particularly vital in Syria given the limited health care resources resulting from the country’s current political situation. This creates an even greater need for the adoption of public health policies that aim to reduce CHD disease through effective and cost-effective policies. Given the current volatile situation of the Syrian population with many unknowns in terms of the health care sector destruction, population change, and political and economic consequences, the current analysis can provide a baseline and roadmap for future steps to help reduce the burden of CHD in Syria.
References
Al Ali R, Rastam S, Fouad FM, Mzayek F, Maziak W (2011) Modifiable cardiovascular risk factors among adults in Aleppo, Syria. Int J Public Health 56(6):653–662
Appel LJ, Angell SY, Cobb LK, Limper HM, Nelson DE, Samet JM et al (2012) Population-wide sodium reduction: The bumpy road from evidence to policy. Ann Epidemiol 22(6):417–425
Asaria P, Chisolm D, Mathers C, Ezzati M, Beaglehole R (2007) Chronic disease prevention: health effects and financial costs of strategies to reduce salt intake and control tobacco use. Lancet 370:2044–2053
Briggs A, Sculpher M, Buxton M (1994) Uncertainty in the economic evaluation of health care technologies: the role of sensitivity analysis. Health Econ 3(2):95–104
Brundtland GH, Glinka E, zur Hausen H, Luiz d’Avila R (2013) Open letter: let us treat patients in Syria. Lancet 382(9897):1019–1020
Capewell S, Critchley J, Unal B (2007). IMPACT, a validated, comprehensive coronary heart disease model: Overview and technical appendices. Accessed 01 November 2013. Available at: http://www.liv.ac.uk/PublicHealth/sc/bua/IMPACT_Model_%20Appendices_May_2007.pdf
Cappuccio F, Capewell S, Lincoln P, McPherson K (2011) Policy options to reduce population salt intake. BMJ 343:d4995
Central Bureau of Statistics (CBS 2011) Central Bureau of Statistics. Available at: http://www.cbssyr.org/index-EN.htm
Cobiac L, Vos T, Veermen L (2010) Cost-effectiveness of interventions to reduce dietary salt intake. Heart 85:1920–1925
Hooper L, Bartlett C, Davey Smith G, Ebrahim S (2004) Advice to reduce dietary salt for prevention of cardiovascular disease. Cochrane Database Syst Rev. Issue 1. doi:10.1002/14651858.CD003656.pub2. (Art No: CD003656)
Fidan D, Unal B, Critchley J, Capewell S (2007) Economic analysis of treatments reducing coronary heart disease mortality in England and Wales, 2000–2010. QJM 100(5):277–289
He F, MacGregor G (2004). Effect of longer-term modest salt reduction on blood pressure. Cochrane Database Syst Rev. Issue 1. doi:10.1002/14651858.CD004937. (Art No: CD004937)
Mason H, Shoaibi A, Ghandour R, O’Flaherty M, Capewell S, Khatib S et al (2014) A cost effectiveness analysis of salt reduction policies to reduce coronary heart disease in four Eastern Mediterranean countries. PLoS One 9(1):e84445. doi:10.1371/journal.pone.0084445
Maziak W, Ward KD, Mzayek F, Rastam S, Bachir ME, Fouad MF et al (2005) Mapping the health and environmental situation in informal zones in Aleppo, Syria: report from the Aleppo household survey. Int Arch Occup Environ Health 78(7):547–558
Maziak W, Rastam S, Mzayek F, Ward KD, Eissenberg T, Keil U (2007) Cardiovascular health among adults in Syria: a model from developing countries. Ann Epidemiol 17(9):713–720
Mohan S, Campbell NR, Willis K (2009) Effective population-wide public health interventions to promote sodium reduction. Can Med Assoc J 181(9):605–609
Murray CJ, Lopez AD (1997) Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet 349(9061):1269–1276
Murray C, Lauer J, Hutubessy R, Neissen L, Tomijima N, Rodgers A et al (2003) Effectiveness and costs of interventions to lower systolic blood pressure and cholesterol: a global and regional analysis in reduction of cardiovascular-disease risk. Lancet 361:717–725
Musaiger AO, Al-Hazzaa HM (2012) Prevalence and risk factors associated with nutrition-related noncommunicable diseases in the Eastern Mediterranean region. Int J Gen Med 5:199–217
Rastam S, Al Ali R, Maziak W, Mzayek F, Fouad FM, O’Flaherty M, Capewell S (2012) Explaining the increase in coronary heart disease mortality in Syria between 1996 and 2006. BMC Public Health 12:754
Selmer R, Kristiansen I, Haglerød A, Graff-Iversen S, Larsen H, Meyer H et al (2000) Cost and health consequences of reducing the population intake of salt. J Epidemiol Community Health 54:697–702
Smith-Spangler C, Juusola J, Enns E, Owens D, Garber A (2010) Population strategies to decrease sodium intake and the burden of cardiovascular disease. Ann Intern Med 152:481–487
Unal B, Critchley JA, Fidan D, Capewell S (2005) Life-years gained from modern cardiological treatments and population risk factors changes in England and Wales, 1981–2000. Am J Public Health 95(1):103–108
United Nations (UN) (2011) Department of Economics and Social Affairs. Accessed 27 January 2011. Available at: http://www.un.org/esa/population/
United Nations (UN) (2013) Purchasing power parities (PPP) conversion factor, local currency unit to international dollar. United Nations Statistics Division. Accessed 10 November 2013. Available at: http://data.un.org/Data.aspx?d=MDG&f=seriesRowID:699
Wang G, Labarthe D (2011) The cost-effectiveness of interventions designed to reduce sodium intake. J Hypertens 29:1693–1699
World Health Organisation (WHO) (2002) World Health Report 2002
World Health Organization (WHO) (2003a) Noncommunicable disease. STEPwise surveillance. Syrian Arab Republic Report. Available at: http://www.emro.who.int/ncd/pdf/stepwise_syria.pdf
World Health Organization (WHO) (2003b) Making choices in health: WHO guide to cost-effectiveness analysis. Edited by Tan-Torres Edejer T, Baltussen R, Adam T, Hutubessy R, Acharya A, Evans DB, Murray CJL. Geneva: World Health Organization
World Health Organization (WHO) (2004) WHO Global Health Observatory. Accessed 10 November 2013. Available at: http://apps.who.int/ghodata/
World Health Organization (WHO) (2005) Preventing chronic diseases: a vital investment. WHO global report. Geneva: World Health Organization
World Health Organization (WHO) (2008) The global burden of disease: 2004 update
World Health Organization (WHO) (2010) Creating an enabling environment for population-based salt reduction strategies: report of a joint technical meeting held by WHO and the Food Standards Agency, United Kingdom
World Health Organization (WHO) (2011) Global status report on non-communicable diseases 2010. World Health Organization, Geneva
World Health Organisation (WHO) (2013) Choosing interventions that are cost effective (WHO-CHOICE: Threshold values for intervention cost effectiveness by region. Accessed 10 November 2013. Available at: http://www.who.int/choice/costs/CER_levels/en/index.html
World Health Organization (WHO) (2013a) Middle Eastern Region: Syrian Arab Republic statistics summary (2002-present). Global Health Observatory Data Repository. Accessed 01 Novemeber 2013. Available at: http://apps.who.int/gho/data/node.country.country-SYR?lang=en
World Health Organization (WHO) (2013b) Syrian Arab Republic, Jordan, Lebanon, Iraq: Situation Report. Issue No. 16. 21 June–9 July, 2013. Accessed 01 November 2013. Available at: http://www.emro.who.int/images/stories/syria/Regional_situation_report_no_16.pdf
World Health Organization (WHO) (2013c) Health impact of the crisis in the Syrian Arab Republic. Emergency preparedness and humanitarian action, 2013. Accessed 01 November 2013. Available at: http://www.emro.who.int/emergency/eha-news/syria-sitrep.html
World Health Organization (WHO) (2013d) Syrian Arab Republic, Jordan, Lebanon, Iraq: Monthly Situation Report. Issue No. 18. 10 August–10 September, 2013. Accessed 01 November 2013. Available at: http://www.emro.who.int/images/stories/syria/documents/Syria_crisis_SitRep_WHO_18_01_Oct.pdf
World Health Organization (WHO) (2013e) Syrian Arab Republic, Jordan, Lebanon, Iraq: monthly situation report (Annex). Issue No. 18. 10 August–10 September, 2013. Accessed 01 November 2013. Available at: http://www.emro.who.int/images/stories/syria/documents/Annex_Sitrep_WHO_18__01-Oct_.pdf
Acknowledgments
This work was funded by the EU FP7 grants for the MedCHAMPS project (MEDiterranean studies of Cardiovascular disease and Hyperglycaemia: Analytical Modelling of Population Socio-economic transitions) and the RESCAP-MED project (RESearch CApacity for Public health in the MEDiterranean).
Author information
Authors and Affiliations
Corresponding author
Additional information
This article is part of the supplement "The rising burden of noncommunicable diseases in four Mediterranean countries and potential solutions".
Rights and permissions
About this article
Cite this article
Wilcox, M.L., Mason, H., Fouad, F.M. et al. Cost-effectiveness analysis of salt reduction policies to reduce coronary heart disease in Syria, 2010–2020. Int J Public Health 60 (Suppl 1), 23–30 (2015). https://doi.org/10.1007/s00038-014-0577-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-014-0577-3