Abstract
Objective
To identify the major risk factors for non-communicable diseases (NCDs) among the population of the capital city Male.
Methods
We undertook a cross-sectional survey among the 25–64-year-age group using a multi-stage sampling method with households as sampling unit. Information on behavioral, physiological, and biochemical risk factors was obtained through standardized methods as recommended by the STEPS survey guideline of the World Health Organization. Age-adjusted prevalence was calculated using the census figures for the year 2000.
Results
Among 2,028 individuals who participated in the survey, complete biochemical data were available for 1,506 subjects. The prevalence of NCD risk factors was high among both men and women in low education group: current smoking (39.9, 9.9%); overweight (BMI ≥ 23 kg/m2) (60.8, 65.5%); abdominal obesity (24.2, 54.1%); raised blood pressure (29.7, 32.9%); raised blood glucose (4.3, 4.7%); hypercholesterolemia (53.7, 54.9%).
Conclusion
The significant burden posed by the NCD risk factors along with the gender and socioeconomic differentials point to the need for public health action. The Ministry of Health has already initiated a comprehensive response to this threat. The experience and lessons from this survey will be useful for developing a comprehensive and sustainable surveillance system in the country.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Rapid changes in demography, and social and economic development play an important role in the emergence of non-communicable diseases (NCDs) as a public health problem. This is no longer restricted to developed countries but is also true for developing countries in the South-East Asian Region (SEAR). The increasing burden of NCDs threatens to overwhelm already stretched health services in these countries. The selected major NCDs (heart disease, stroke, diabetes, cancer, and respiratory disease) together account for a major share of the total burden of NCDs, globally. The risk factors underlying these major NCDs are well documented and are shared (World Health Organization 2008).
The World Health Report 2002 made a strong case for focusing on risks and risk factors for assessment as well as interventions (WHO 2002b). The WHO STEPwise approach to risk factor surveillance (STEPs) was developed by the WHO Cross Cluster Surveillance team in the year 2000 (WHO 2008). The STEPS approach focuses on obtaining core data on the established risk factors that determine the major disease burden. The rationale for the inclusion of these core risk factors include the following:
-
They have the greatest impact on NCD mortality and morbidity.
-
There is evidence that their modification is possible and effective in primary prevention.
-
The measurement has been validated and can be obtained while following appropriate ethical standards.
The WHO STEPwise approach to chronic disease risk factor surveillance provides an entry point for low- and middle-income countries to get started on chronic disease surveillance activities. It is sufficiently flexible to allow each country to expand on the core variables and risk factors, and to incorporate optional modules related to local or regional interests. It is also designed to help countries build and strengthen their capacity to conduct surveillance.
The countries in SEAR have limited experience and capacity in handling NCDs as they have been focusing more on maternal and child health as well as infectious diseases. Therefore, the first round of risk factor surveys was carried out in countries of SEAR with twin objectives of generating local data on risk factors as well as of building capacity in countries for NCD risk factor surveillance.
In this context, the Health Ministry of Maldives carried out the STEPS survey. Here, we report the findings of the STEPS survey carried out in Male, the capital of Maldives. Due to logistic reasons of islands being distributed across Indian Ocean and the fact that Male accounts for one-third of the Maldives’s population, the study was restricted to the capital Male.
Methods
Study setting
The republic of Maldives consists of 1,192 tiny coral islands, out of which 193 are inhabited, and 91 islands developed as tourist resorts. Male is the capital island of the Maldives and the main urban and commercial center of the country. Immigration to Male from other islands is very high with the population, and housing census of 2006 showed annual population growth rate of 5.7%. The major industries in the country are fishing and tourism. Maldives’ only export is fish and fishery products. Vegetables and fruits are mainly imported from the neighboring countries. The per capita gross national income (GNI) for 2005 was 2,390 US$, and population below international poverty line of >1 US$ per day was less than 1% (WHO 2007a, b).
The health system of the country is organized into a five-tier referral health care delivery system. At the lowest level are the community health workers at health posts and at the top are the tertiary level hospitals. The health system in the Maldives is an integrated one in which the government provides both preventive and curative care. In the private sector, there is one major tertiary hospital located in Male, and clinics throughout the country. Some of the private clinics provide laboratory services. There are some NGOs working in the area of non-communicable disease with public health functions. Patients with non-communicable diseases are treated primarily at regular clinics (government and private) in the islands and atoll hospitals. A full range of tests and medications are not available at all sites in the Maldives for the management of non-communicable diseases. The quality of care is considered to be higher in Male and at the regional hospitals, so patients generally seek care at these hospitals.
The data derived from vital registration and medical certification of cause of deaths show that almost half of the deaths are attributable to the NCDs (WHO 2002a). The data on diseases are limited to hospital-based record of the only public sector tertiary hospital in the country. The first national tobacco prevalence survey conducted in 1997 revealed that 57% of males and 29% of females were smokers (Department of Public Health 1997). Information about other NCD risk factors has been scanty or absent.
Sample size and sampling
As suggested by STEPS approach, it was decided to have 250 subjects between 25 and 64 years in each of the eight groups (age by 10-year interval for both sexes) totaling to 2,000 subjects. A multistage sampling strategy was used. The data from the census done in the year 2000 were used for sampling frame (Ministry of Planning and National Development 2000). All the four wards of Male, Henveiru, Galolhu, Machchangolhi, and Maafannu, were selected. In each ward, number of households to be selected from each ward was proportionate to its size. The selection of households in each ward was by systematic sampling. Out of the listed 5,585 households, a total of 2,000 households were to be selected. The houses which could not be contacted or refused were replaced with the nearest house. After listing all the eligible in the households, one person was selected by draw of lots. A record was maintained concurrently to look at the age and sex distribution of the sample. After initial scrutiny it was apparent that getting the required number in men and older age groups was going to be difficult. Therefore, in the later part of the survey, these groups were preferentially selected. However, figures have been weighted to take into account the differences between population age-structure and the distribution of study subjects.
Study instrument
The STEPS instrument developed by WHO was utilized for the data collection, and the standard generic guidelines were followed throughout the process of data collection and data processing (WHO 2008). All the three STEPS were covered which includes data on behavioral measures, physiological, and biochemical measures. The generic STEPS instrument developed by WHO was adapted, translated, and pre-tested. The educational level was graded as illiterate/basic literacy if they did not attend school or could just read and write their names, studied up to fifth grade (primary), up to tenth grade (secondary), and more than ten grades. The monthly household income was measured as a categorical variable (<1,000, 1,000–5,000, 5,000–10,000, 10,000–15,000, and >15,000). Questions on alcohol consumption were omitted from the study due to the reason that it is prohibited by religion as well as its very low known use. One serving of vegetable was considered to be 1 cup of raw green leafy vegetables, 1/2 cup of other vegetables (cooked or chopped raw) or 1/2 cup of vegetable juice. One serving of fruit was considered to be 1 medium-sized piece of apple, banana or orange, 1/2 cup of chopped, cooked, canned fruit or 1/2 cup of fruit juice, not artificially flavored. To gather information on physical activity, the information was gathered on three broad domains viz., physical activity at work, transport-related physical activity, and leisure-time physical activity.
Measurement
All the staff involved in the survey was trained for 2 days in sample selection procedures, interview techniques, and measurement of blood pressure and anthropometrics. The pilot test of the survey for Step 1 (questionnaire) and Step 2 (physiological measurements) was carried out during end of 2003. The field data collection was carried out from April 2004 to October 2004. The measurement of height and weight was done using standardized SECA instruments. The digital weighing scale utilized was regularly compared against a standard weight. Waist measurements were done using non-stretchable measuring tapes. Blood pressure recordings were done using a digital sphygmomanometer with an adult-sized cuff. The weight measurements were done till nearest 0.1 kg, height and waist till nearest 0.1 cm and blood pressure till nearest 1 mmHg. The pregnant women were excluded for the component of obesity measurement. Blood samples for biochemical measurements were collected at the household and were sent to the laboratory for processing within 2 h of collection. The biochemical analysis for blood glucose and lipid profile was conducted at the laboratory at Indira Gandhi Memorial Hospital. Glucose was estimated by GOD-PAP method using enzymatic kits from RANDOX. Cholesterol was estimated by CHOD-PAP method and triglycerides by GPO-PAP method using enzymatic kits from Bayer Diagnostic Reagents. HDL was estimated by precipitation with phosphotungstate/MgCl2 followed by estimation of cholesterol in supernatant by the enzymatic kit method.
Definitions
The definitions used for various parameters were as per the WHO STEPS guidelines (WHO 2008). Current daily smokers were defined as those who were currently smoking cigarettes, bidis or hookah daily. Inadequate intake of fruits and vegetable was defined as consuming less than five servings in a day. A person was labeled as inactive if he/she was inactive in all the three domains of work, transport, and leisure. Raised blood pressure was defined as systolic blood pressure ≥140 mmHg and/or diastolic blood pressure ≥90 mmHg or under medication (NHLBI 2005). Body mass index (BMI) was calculated, and overweight was defined as BMI ≥ 23 kg/m2; abdominal obesity was diagnosed when waist circumference (WC) was >90 cm in men and >80 cm in women in accordance with the recommendations of World Health Organization for Asian adults (WHO 2000). Raised blood sugar or hyperglycemia was defined when fasting blood glucose was ≥7.0 mmol/dl, while criteria for impaired fasting glucose (IFG) was a fasting glucose level ≥6.1 to <7.0 mmol/l (WHO 1999). Hypercholesterolemia was defined by a fasting total serum cholesterol (TC) level ≥5.2 mmol/dl, and hypertriglyceridemia was defined by a fasting serum triglyceride level ≥1.73 mmol/dl (NCEP 2001). Low HDL cholesterol level was defined as a fasting serum HDL level <1.04 mmol/dl among men and <1.30 mmol/dl among women.
For surveillance, mean levels of risk factors in the population serve as the best indicators of their status in the community. We also present results of the risk factors by selected cut-offs. However, different cut-offs have been recommended by different agencies at different times—be it obesity, diabetes, hypercholesterolemia, etc. It may also be pointed out that the objective of the survey was not to assess the prevalence of diseases. Raised blood sugar and blood pressure levels reported in the survey are not true measures of prevalence of diabetes and hypertension, respectively.
Statistical analysis
To compare proportions and group, mean χ 2 test and student’s t test were used, respectively. Analyses for the linear trend in proportions were done by Chi-square for trend using the STATCALC function in the Epi Info software (Centers for Disease Prevention and Control, Atlanta, GA, USA; Version 3.4.3). Remaining analyses were carried out using SPSS software package (SPSS Inc., Chicago, IL, USA; version 11.5). For estimating age-adjusted prevalence figures, population weights based on the data from census in 2000 were used.
Results
Demographic characteristics
A total of 2,028 individuals (men 934, women 1,094) residing in Male participated in the STEPS survey (Table 1). The refusal rate was 20.8% for participation in questionnaire and anthropometry. Among them, 1,562 subjects (77.02%) enrolled for the Step 3 component (biochemical component) and complete set of biochemical measurements available for 1,506 subjects. The demographic and socioeconomic characteristics of the sample are given in Table 1.
Illiterates and subjects having basic literacy (37.7%) comprised the single largest group in the sample. About one-fourth (28.9%) of the subjects were employed in government jobs, while 14.2% were in private sector. Almost two-third of the women were involved in household work. More than a quarter (28.8%) of the subjects belonged to families with annual household income of >5,000 Maldives Rufiyaa (MVR; 1 US$ = 12.8 MVR). Upper income group (>15,000 MVR) accounted for 16.3%.
Prevalence and levels of risk factors
Tobacco use
One-fourth (24.1%) of the subjects were current smokers with 89.0% of the current smokers smoking daily (Tables 2, 3). The initiation of smoking was at a mean age of 21.2 ± 14.6 years. The most common tobacco product among smokers was cigarette with a median consumption of 15 cigarettes per day. A small proportion (5.9%) of the subjects were using smokeless forms of tobacco and a three quarter of them (75.6%) were consuming it daily. The most common form of smokeless form of tobacco was chewing tobacco.
Diet
Fruits and vegetables were consumed on a median of 3 days per week each with a median of one serving per day. Only 2.7% of the subjects had five or more servings of fruits and vegetables a day. The most common type of oil/fat used for preparation of meals was vegetable oils (79.8%).
Physical activity
A large majority (93.1%) of respondent’s work-related activities involved mostly sitting or standing with walking for no more than 10 min at a time. Two-third of the subjects (66.5%) did at least 10 min of walking/cycling per day. Most (93.4%) of the subjects were not involved in any physical activity for recreation, sport or leisure. This meant that 30.2% of the population was physically inactive in all domains of physical activity.
Overweight/obesity
As per the definition of the World Health Organization for Asian adults (BMI ≥ 23 kg/m2), two-third of the subjects (63.3%) were overweight/obese. The overall prevalence of overweight in accordance with international cut-point (BMI ≥ 25 kg/m2) was 43.5% with an increase in the prevalence with the age decile. The overall prevalence of abdominal obesity was 40.0% with more than half the women being abdominally obese. Abdominal obesity increased by age with prevalence reaching as high as 75% among those more than 55-year-old.
High blood pressure
More than two-third (69.8%) of the subjects had their blood pressure measured in the previous 12 months, while that of 21.6% of the subjects measured their BP 1–5 years earlier. The proportion of newly diagnosed subjects for hypertension in the previous 1 year was 10.5, and 69.0% of them were on drugs for controlling hypertension prescribed by health care personnel. The overall prevalence of high blood pressure was 31.5%. Sixty-two percent of hypertensive subjects were taking medication, and 41.4% of those on treatment had their blood pressure levels under control (SBP < 140; DBP < 90 mmHg).
Biochemical risk factors
Hypercholesterolemia, hypertriglyceridemia, and low HDL-cholesterol level were observed among 54.4, 22.1, and 49.17% of the subjects, respectively. The overall prevalence of raised blood glucose (fasting blood glucose ≥7.0 mmol/dl) and impaired fasting glycaemia (fasting blood glucose ≥6.1–7.0 mmol/dl) was 4.5 and 3.0%, respectively. The highest prevalence of hyperglycemia (15.7%) was observed among the age group of 55–64 years.
Gender and NCD risk factors
As evident from Table 3, the smoking rates (p < 0.001) and physical inactivity (p < 0.001) were significantly higher among men, while there was no substantial difference in the fruit and vegetable intake (p = 0.59). The overall mean level of waist circumference (p = 0.001), systolic blood pressure (p = 0.002), and triglyceride (p < 0.001) were significantly higher among men, while women had significantly higher mean level of body mass index (p < 0.001) and HDL cholesterol level (p < 0.001). Despite lower mean waist circumference, the prevalence of abdominal obesity was much higher among females (p < 0.001) due to lower cut-offs for women. The mean triglyceride level was significantly higher among men across all age groups (except for 55–64 age decile), while mean HDL level was significantly higher among women across all age groups (Table 2).
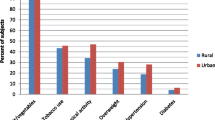
Socioeconomic status and NCD risk factors
The prevalence of current smoking, overweight/obesity, abdominal obesity, high blood pressure, diabetes, and hypercholesterolemia were significantly higher among low education group (Table 4). The gradients in the risk factor level were more prominent across education groups than income groups. The levels of physical inactivity were low among the more-educated and high-income groups.
Discussion
This study documents the high prevalence of risk factors for NCD in the population of Male where more than a quarter of the population of Maldives resides. The prevalence of current smoking, overweight/obesity, abdominal obesity, hypertension, hypercholesterolemia, and low HDL level was very high in the sample particularly among women and low education group. Although the prevalence of work and leisure-time physical inactivity was very high, travel related physical activity (walking or cycling for work or other activity) was present in two-third of the subjects. The consumption of fruits and vegetables was limited to a median of one serving per day.
It should, however, be noted that the survey had some methodological limitations. For logistic reasons, the study attempted to be only representative of Male. However, the use of sampling frame from Census of the year 2000 with reported high levels of in migration along with a change in sampling strategy at the later part of the survey to enable sufficient representation of elder age group have partly compromised the representativeness. However, this would be one of the lessons learnt when the country moves toward setting up its surveillance system. Also, due to the limitations of the instrument used for measuring physical activity (in terms of screening people who do and who do not do physical activity), it is possible that physical inactivity (especially work-related) is overestimated.
While this study establishes the high prevalence of risk factors, the determinants of these risk factors requires a more in-depth understanding. Male being an island city has its own unique features which need to be kept in mind. For example, the country is almost entirely dependent on imports for fruits and vegetables. Anecdotal evidence suggests that fruit intake is restricted to high-income groups. Unlike in other settings therefore, seasonality would be a less important issue. Male is an entirely urban area with little geographical spread which is an important consideration when considering physical activity promotion strategies. The proportion of people whose blood pressure was measured was high probably due to Male being a small island city with high density population with good access to health care services in the capital city.
These estimates compare with estimates for other countries in the South-East Asia region, which conducted similar surveys using the WHO STEPwise approach (Anand et al. 2007; Ng et al. 2006). Given the fact that countries in the region share similar sociocultural contexts and have trade relations with each other, it makes sense for these countries to share their experiences, capacities and co-ordinate their efforts. This calls for a better networking between countries for NCD prevention and control which is being facilitated by the WHO in this region (WHO 2005).
The STEPS survey highlights the reversal of social gradient (higher occurrence of risk factors in the low socioeconomic group) for NCD risk factors in Male. Similar gradients were observed in the Indian urban population as well (Reddy et al. 2007). This corrects the common misperception that these diseases are mainly seen in rich and educated. As the lower social class can ill afford to spend on treatment of these diseases, there is a need for government to initiate measures for prevention and control of NCDs. Surveillance data have been used to measure and address inequities in health in countries as diverse as Americas and countries of Central and Eastern Europe (Merkin et al. 2009; Kunst 2009).
In response to the survey, the Ministry of Health, Maldives formulated the National Strategic Plan 2008–2010 for prevention and control of non-communicable diseases. The Health Master Plan looks at strategic targets for the prevention of chronic non-communicable diseases, which were based on the results of the risk factor survey. The goal of the strategic plan is to direct comprehensive and coordinated action aimed to reduce health, social, and economic burden of NCDs in Maldives. It sets out priorities, actions, and a timeframe for prevention and control of NCDs between 2008 and 2010 at national level. By 2010 measurable progress should be seen at central, regional, and island levels toward implementation of the health master plan targets related to:
-
strengthening the evidence base for NCD prevention and control by assessing the burden of NCDs and their risk factors;
-
advocacy, communication, and community mobilization focusing on behavioral change;
-
strengthening capacity at all sectors to develop and implement NCD prevention and control plans and programmes;
-
building partnerships involving public and private sectors and civil society for NCD prevention and control;
-
improving quality, and access to early detection and management of major NCDs;
-
monitoring and evaluating performance.
In future, this strategic plan will need to be evaluated and the data from this survey will provide the baseline measures to assess the effectiveness of the program in changing these outcome variables. The routine monitoring of socioeconomic inequalities in health as well as the evaluation of the health equity impact of policy measures and actions are critical to improve health and health-system outcomes (Madarasova-Geckova 2009).
In summary, the data generated from this survey has documented that NCD risk factors pose a significant burden in the capital city of Maldives. The gender and socioeconomic differentials point to the need for instituting public health action against NCDs. The Ministry of Health needs to focus on implementation and evaluation of the strategies identified above. The experience and lessons gained from this survey will be useful for development of a comprehensive and sustainable surveillance system in the country.
References
Anand K, Shah B, Yadav K, Singh R, Mathur P, Paul E, Kapoor SK (2007) Are the urban poor vulnerable to non-communicable diseases? A survey of risk factors for non-communicable diseases in urban slums of Faridabad. Natl Med J India 20(3):115–120
Department of Public Health (1997) Smoking survey, Malè
Kunst A (2009) Socioeconomic inequalities in health in Central and Eastern Europe: synthesis of results of eight new studies. Int J Public Health 54:197–200
Madarasova-Geckova A (2009) Can research contribute to the public capacity for activities that reduce socioeconomic inequalities in health? Int J Public Health 54:201–202
Merkin SS, Karlamangla A, Crimmins E, Charette SL, Hayward M, Kim JK, Koretz B, Seeman T (2009) Education differentials by race and ethnicity in the diagnosis and management of hypercholesterolemia: a national sample of US adults (NHANES 1999–2002). Int J Public Health 54(3):166–174
Ministry of Planning and National Development. (2000) Population and Housing Census of Maldives 2000, Republic of Maldives. Available from http://www.planning.gov.mv/publications/Pop_housing_census2000/index_p.htm
National Cholesterol Education Program (2001) Executive summary of the third report of the National Cholesterol Education Program Expert Panel on detection, evaluation, and treatment of high blood cholesterol in adults (Adult Treatment Panel-III). JAMA 285:2486–2497
National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure; National High Blood Pressure Education Program Coordinating Committee (2005) The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 289:2560–2572
Ng N, Stenlund H, Bonita R, Hakimi M, Wall S, Weinehall L (2006) Preventable risk factors for noncommunicable diseases in rural Indonesia: prevalence study using WHO STEPS approach. Bull World Health Organ 84(4):305–313
Reddy KS, Prabhakaran D, Jeemon P, Thankappan KR, Joshi P, Chaturvedi V et al (2007) Educational status and cardiovascular risk profile in Indians. Proc Natl Acad Sci USA 104:16263–16268
World Health Organization (1999) Definition, diagnosis and classification of diabetes mellitus and its complications: report of a WHO consultation. Part 1: diagnosis and classification of diabetes mellitus. WHO, Department of Noncommunicable Disease Surveillance, Geneva
World Health Organization (2000) Regional Office for the Western Pacific of the World Health Organization. International Association for the Study of obesity and international obesity task force. The Asia Pacific perspective: redefining obesity and its treatment. Health Communications Australia Pty Limited, Sydney
World Health Organization (2002) Noncommunicable diseases in South-east Asia Region—a profile. SEA/NCD/54 Regional Office for South-east Asia, New Delhi, pp 28–29
World Health Organization (2002) World Health Report 2002—reducing risks, promoting healthy life. Geneva
World Health Organization (2005) South East Asia Network for noncommunicable disease prevention and control. Report of the WHO Meeting, Bandos, Maldives, 7–10 November 2005. New Delhi World Health Organization, Regional Office for South-east Asia, 2006, SEA-NCD-71
World Health Organization Country Office for Maldives (2007a) WHO Country Cooperation Strategy 2007–2011. WHO, Republic of Maldives
World Health Organization. Regional Office for South-East Asia (2007b) 11 health questions about the 11 SEAR countries. New Delhi
World Health Organization (2008) The WHO STEPwise approach to Surveillance of chronic noncommunicable diseases risk factors. http://www.who.int/chp/steps/en. Accessed 2 Apr 2008
Acknowledgment
The authors acknowledge the technical support provided by World Health Organization particularly Dr. Jorge Mario Luna, WHO representative to Maldives and Dr. Ohn Kyaw and Dr. Rajesh Pandav of the WHO Country Office, Maldives and Dr. Jerzy Leowski, Regional Adviser, Noncommunicable Diseases, WHO Regional Office for South-East Asia. The field support provided by Diabetes and Cancer Society of Maldives for the clinical part of the survey and by Indira Gandhi Memorial Hospital (IGMH) for the laboratory work is appreciated. The assistance provided by VS Ajay, Research Fellow, Initiative for Cardiovascular Health in Developing Countries, New Delhi, India in statistical analysis and manuscript preparation is acknowledged.
Conflict of interest statement
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aboobakur, M., Latheef, A., Mohamed, A.J. et al. Surveillance for non-communicable disease risk factors in Maldives: results from the first STEPS survey in Male. Int J Public Health 55, 489–496 (2010). https://doi.org/10.1007/s00038-009-0114-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00038-009-0114-y