Abstract
Hematopoiesis is hierarchically orchestrated by a very small population of hematopoietic stem cells (HSCs) that reside in the bone-marrow niche and are tightly regulated to maintain homeostatic blood production. HSCs are predominantly quiescent, but they enter the cell cycle in response to inflammatory signals evoked by severe systemic infection or injury. Thus, hematopoietic stem and progenitor cells (HSPCs) can be activated by pathogen recognition receptors and proinflammatory cytokines to induce emergency myelopoiesis during infection. This emergency myelopoiesis counterbalances the loss of cells and generates lineage-restricted hematopoietic progenitors, eventually replenishing mature myeloid cells to control the infection. Controlled generation of such signals effectively augments host defense, but dysregulated stimulation by these signals is harmful to HSPCs. Such hematopoietic failure often results in blood disorders including chronic inflammatory diseases and hematological malignancies. Recently, we found that interleukin (IL)-27, one of the IL-6/IL-12 family cytokines, has a unique ability to directly act on HSCs and promote their expansion and differentiation into myeloid progenitors. This process resulted in enhanced production of neutrophils by emergency myelopoiesis during the blood-stage mouse malaria infection. In this review, we summarize recent advances in the regulation of myelopoiesis by proinflammatory cytokines including type I and II interferons, IL-6, IL-27, granulocyte colony-stimulating factor, macrophage colony-stimulating factor, and IL-1 in infectious diseases.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hematopoietic stem cells
Blood cells must be continuously replaced because of their finite life span, and they are generated by the expansion and differentiation of a very small population of hematopoietic stem cells (HSCs) [1]. HSCs, therefore, have the dual capacity to self-renew and differentiate to generate all blood cell lineages. Self-renewal is the ability of HSCs to divide asymmetrically or symmetrically to produce one or two daughter stem cells that have a developmental potential similar to the mother cell. This ability is essential for HSCs to expand their numbers during development and maintain the proper HSC pool. HSCs also have an ability to differentiate. In this process, they lose their self-renewal capacity and generate various progenitor cells including multipotent progenitors (MPPs) and lineage-restricted progenitors that proliferate vigorously, resulting in the production of functional mature blood cells. Therefore, hematopoiesis is hierarchically organized, with the most immature and rare cell population, HSCs, located at the top of the hematopoietic hierarchy [2, 3]. Because frequent chromosomal replications generally increase the risk of oncogenic DNA mutations, HSCs are dormant and quiescent to maintain their genomic integrity and to avoid unnecessary proliferation and resultant exhaustion [4]. However, in response to various stimuli such as irradiation and cytotoxic chemotherapy, HSCs can replicate and proliferate. Moreover, because HSCs express receptors for cytokines and chemokines, as well as pattern recognition receptors such as Toll-like receptors (TLRs), HSCs can respond to signals from other cells and sense pathogens directly during infection or inflammation.
Bone-marrow niche
The specialized microenvironment in the bone marrow (BM) that crucially regulates HSC dormancy, survival, and function through various soluble factors such as cytokines and cell contact-dependent interactions is called the BM niche. Various cell types including osteoblasts, perivascular cells, endothelial cells (ECs), mesenchymal stem/stromal cells (MSCs), T cells, B cells, dendritic cells (DCs), and macrophages contribute to maintenance of the BM niche (Fig. 1a). Most HSCs reside in close proximity to sinusoids and blood vessels in the trabecular bone area of the BM. C-X-C motif ligand 12 (CXCL12) and stem cell factor (SCF), which are produced by ECs and perivascular cells in the BM, play critical roles in HSC maintenance [5,6,7]. BM-resident memory-type CD4+ and CD8+ T cells localized in the trabecular bone area promote the formation of the perivascular BM niche by secreting cytokines necessary for HSC maintenance, such as interleukin (IL)-3 and granulocyte macrophage colony-stimulating factor (GM-CSF) [8]. In addition, nonmyelinating Schwann cells located around the blood vessels in the BM maintain HSC dormancy by secreting transforming growth factor-β [9].
Regulation of myelopoiesis under homeostatic and pathogenic conditions. a Under normal homeostatic hematopoiesis, HSCs reside in the perivascular region of the BM, the so-called BM niche, and MSCs, ECs, and pericytes regulate HSC dormancy and differentiation through cytokines and cell contact–dependent signals such as Notch. b In severe infection, myeloid cells need to be replenished from HSCs and progenitors in BM because of their low proliferative activity, a process called emergency myelopoiesis. HSCs can directly sense the presence of pathogens via pattern recognition receptors such as TLRs and proinflammatory cytokines, and they expand and differentiate into mature myeloid cells to control the infection
Emergency myelopoiesis
Although adaptive immune cells such as T cells and B cells can vigorously proliferate in an antigen-specific manner, myeloid cells such as macrophages and neutrophils need to be replenished from hematopoietic stem and progenitor cells (HSPCs) in BM because of their low proliferative activity. HSCs are predominantly quiescent, but they are activated and enter the cell cycle in response to inflammatory signals evoked by severe systemic infection or injury. Such inflammatory signals induce “emergency myelopoiesis,” which triggers differentiation of HSPCs and counterbalances the loss of cells (Fig. 1b) [10,11,12,13,14]. HSCs eventually give rise to lineage-restricted hematopoietic progenitors, which replenishes mature blood cells, preferentially the myeloid lineage in the process of emergency myelopoiesis. Similar to immune cells, HSPCs can be activated by TLR ligands and inflammatory cytokines [14]. Many immune and nonimmune cells, including HSPCs and ECs, express TLRs and cytokine receptors. Activation of these receptors on these cells leads to production of several proinflammatory cytokines and chemokines that promote emergency myelopoiesis.
Purpose
Thus, homeostasis of HSCs is tightly regulated by signals such as cytokines and TLR ligands expressed by the BM niche. However, aberrant signals to HSPCs induce hematopoietic failure, often resulting in blood diseases including chronic inflammatory diseases and hematological malignancies [15,16,17]. Therefore, it is crucial to clarify how proinflammatory cytokines and TLR ligands regulate HSC function, expansion, and differentiation under pathogenic conditions. The detailed roles of TLRs in myelopoiesis and their underlying molecular mechanisms are beyond the scope of this review, but they have been described in other excellent reviews [18, 19]. Recently, we found that IL-27, one of the IL-6/IL-12 family cytokines, has a unique ability to directly act on HSCs and promote their expansion and differentiation into myeloid progenitors, resulting in enhanced emergency myelopoiesis to control malaria infection [20, 21]. Here, we focus on only proinflammatory cytokines including type I and II interferons (IFNs), gp130-related cytokines such as IL-6 and IL-27, G-CSF, M-CSF, and IL-1, which have provided us new and important insights into the regulation of myelopoiesis. We summarize these recent advances in this review.
Type I IFNs, IFN-α/β
Characteristics: anti-viral and antiproliferative cytokines
IFNs are anti-viral cytokines produced by host cells in response to viruses, bacteria, parasites, and tumors [22]. Type I IFNs, which include multiple types of IFN-α and a single IFN-β, are produced broadly by various types of cells, such as fibroblasts and monocytes, and inhibit production and replication of viral RNA and DNA. The cell surface receptor complex IFN-α/β receptor is composed of IFN-α receptor (IFNAR)1 and IFNAR2 subunits. Type I IFNs induce an antiproliferative, proapoptotic state that prevents hosts from being infected. IFN-α is used to treat chronic myeloid leukemia as well as hepatitis B and C, because type I IFNs induce direct and indirect antiproliferative effects on immature hematopoietic cells in vivo.
Roles in infection: proliferative, and suppressive effects of IFN-α on HSC functions by acute and chronic stimulation, respectively
The impact of IFN-α/β on hematopoiesis was mainly investigated using a viral infection model with lymphocytic choriomeningitis virus (LCMV) and injection of poly(I:C), an inducer of type I IFN signaling, IFN-α itself, or mice deficient for IFN-α/β and IFNAR subunits. The effects of infection with noncytopathic LCMV on hematopoiesis in the BM using IFNAR-deficient and IFNGR-deficient mice was previously investigated [23]. The infection greatly reduced the cellularity of hematopoietic progenitors in the BM of wild-type mice and IFNGR-deficient mice but not in IFNAR-deficient mice, indicating that IFN-α/β, but not IFN-γ, plays a critical role in the transient BM aplasia during acute LCMV infection. The role of IFN-α/β in hematopoiesis was also explored using mice deficient for IFN regulatory factor 2, a transcriptional suppressor of type I IFN signaling, IFN-α induced proliferation and exhaustion in HSCs, and IFN regulatory factor 2 preserved their self-renewal and multilineage differentiation capacity [11]. In addition, injection of poly(I:C) or IFN-α induced HSC proliferation, but chronic type I IFN signaling further reduced the number of quiescent HSCs. Intriguingly, combined treatment with poly(I:C) and the antiproliferative chemotherapeutic agent 5-fluorouracil augmented exogenous HSC engraftment and hematopoietic reconstitution, leading to improvements in BM transplantation. Another murine study also demonstrated that HSCs efficiently exit G0 and enter an active cell cycle in response to treatment with IFN-α through signal transducer and activator of transcription (STAT) 1 and PKB/Akt pathways together with up-regulation of stem cell antigen-1 (Sca-1) [12]. Interestingly, dormant HSCs were shown to be resistant to 5-fluorouracil, whereas HSCs pre-treated or primed with IFN-α and thus induced to proliferate were efficiently eliminated by 5-fluorouracil exposure. Conversely, competitive repopulation assays revealed that HSCs chronically activated by IFN-α are functionally compromised and rapidly outcompeted by IFNAR-deficient cells. Thus, chronic activation of IFN-α signaling in HSCs impairs their function, whereas acute IFN-α treatment promotes the proliferation of dormant HSCs in vivo, raising the possibility of new applications for combination therapy with IFN-α and antitumor agents to target cancer stem cells. Cancer stem cells are considered to be the main reason for failure of treatment and relapse [24,25,26]. Irradiation and cytotoxic drugs cannot induce their cell death, because their mechanism of action requires active cell division, which is absent in dormant cells. In addition, HSCs express drug efflux proteins that are critically important for multidrug resistance. Consistent with these results, it was also demonstrated that HSCs transiently proliferate in response to acute IFN-α exposure, but chronic IFN-α exposure rapidly makes these HSCs return to quiescence to avoid being killed by IFN-α [27]. This phenomenon may serve as a safeguard mechanism to ensure survival of the HSC pool during chronic IFN-α exposure.
Because infections are also associated with a high risk of extensive platelet consumption, the mechanism coordinating the rapid regeneration of the platelet pool during infection using poly(I:C) was investigated [28]. In response to acute inflammation induced by poly(I:C), stem-like megakaryocyte-committed progenitors became activated and matured, producing megakaryocyte proteins from pre-existing transcripts and leading to an efficient replenishment of platelets that were lost during inflammation. Thus, an emergency machinery counteracts life-threatening platelet depletions through type I IFNs during acute inflammation.
Type II IFN, IFN-γ
Characteristics: antiproliferative, proapoptotic, and immune stimulatory cytokine
Type II IFN is IFN-γ, an immune IFN that is produced by T cells and natural killer (NK) cells activated by IL-12 [29]. The receptor consists of IFNGR1 and IFNGR2. IFN-γ plays a critical role in cellular immune responses against pathogens via up-regulation of MHC class I and II, augmentation of Th1 immune responses, and activation and differentiation of macrophages [30, 31]. In addition, IFN-γ induces an antiproliferative, proapoptotic state that prevents hosts from being infected.
The role of IFNs, especially IFN-γ, in HSC regulation is more complex and controversial, with several conflicting reports of positive and negative effects on hematopoiesis. Although its inhibitory effects on hematopoiesis and suppressive effects on hematopoietic progenitors were previously reported [32, 33], IFN-γ was also demonstrated to stimulate HSC proliferation in synergy with other cytokines such as IL-3 and IL-6 [34, 35]. However, comparing these results is difficult, because the HSC markers used in each study differ. In particular, Sca-1 is an IFN-responsive molecule and highly up-regulated on many hematopoietic cells in response to IFNs [27, 36, 37]. Therefore, lineage−Sca-1−c-Kit+ (LS−K) cells, which are generally myeloid-restricted progenitor cells, become positive for Sca-1 and cannot be distinguished from the real multipotent lineage−Sca-1+c-Kit+ (LSK) cells, hence contaminating the LSK population and confounding analysis of it. Alternatively, these discrepancies also may be explained by compensatory mechanisms including IFN-mediated secretion of other cytokines such as IL-6 [38], IL-27 [21], and fms-related tyrosine kinase 3 ligand [39].
Roles in infection: indirect proliferative effects of IFN-γ on HSPCs promoting emergency myelopoiesis
The impact of IFN-γ on hematopoiesis was mainly investigated using infection models with various pathogens and injection of IFN-γ itself, or mice deficient for IFN-γ and IFNGR subunits. Th1 cell products, but not those of Th2 cells, were shown to induce a rapid expansion of LSK cells in vivo and in vitro in an IFN-γ/STAT1-dependent manner [40]. The IFN-γ-induced LSK cells showed increased ability to bias toward myeloid cell differentiation. Moreover, a study using a mouse model of Mycobacterium avium infection showed that an increased proportion of not only intermediate blood progenitors, but also long-term repopulating HSCs (LT-HSCs), proliferate during the infection via IFN-γ-dependent, but IFN-α-independent, signaling [13] (Fig. 2A). IFN-γ was sufficient to promote LT-HSC proliferation in vivo, and HSCs from IFN-γ-deficient mice had a lower proliferative rate, indicating that IFN-γ plays critical roles as a regulator of HSCs during both homeostasis and infection. A mouse model of the emerging tick-borne disease ehrlichiosis was used to address how infection affects hematopoietic function [41]. Infection with the intracellular bacterium Ehrlichia muris, which causes anemia and thrombocytopenia, was demonstrated to induce the transient proliferation and expansion of BM LSK cells via IFN-γ signaling, accompanied by a loss of dormant LT-HSCs and a bias toward myeloid cell differentiation. Thus, inflammatory signals elicited during acute infection promote HSCs to undergo a rapid, IFN-γ-dependent, transient shift from dormancy to proliferation and expansion, resulting in augmented emergency myelopoiesis to control the infection. A possible molecular mechanism whereby IFN-γ impairs maintenance of HSCs by directly reducing their proliferative ability as well as the restoration of HSC numbers upon LMCV infection was examined [36]. IFN-γ was demonstrated to reduce thrombopoietin-mediated phosphorylation of STAT5, an important positive regulator of HSC self-renewal, in a manner dependent on suppressor of cytokine signaling 1. This finding may partly explain BM failure in chronic inflammatory conditions such as aplastic anemia and HIV. However, when HSCs sense external stimuli, their adhesion status is also critical for determining HSC fate. The cell surface integrin αvβ3 is activated through adhesion of HSCs to extracellular matrix and niche cells, and the signaling through this integrin contributes to the maintenance of HSCs by stimulating long-term repopulating activity in collaboration with thrombopoietin [42]. Nevertheless, the suppressive effect of IFN-γ on HSCs was recently demonstrated to be further intensified by integrin αvβ3 via enhanced activation of STAT1 through the augmentation of serine 727 phosphorylation [43].
Roles of proinflammatory cytokines in the regulation of myelopoiesis under pathogenic conditions such as infection. a IFN-γ secreted from CTLs directly acts on HSCs, thereby favoring monocytic differentiation. Moreover, IFN-γ stimulates BM MSCs to release IL-6, which promotes monocytopoiesis from MPPs. Bacterial infection activates MPPs through TLRs to release IL-6, which promotes granulopoiesis from MPPs. b IL-27 is a limited unique cytokine directly acting on HSCs to promote differentiation into myeloid progenitors during emergency myelopoiesis. Among various types of hematopoietic cells in the BM, IL-27 predominantly and continuously promotes the expansion of LSK cells only, especially LT-HSCs and MyRPs with long-term repopulating activity, and differentiates them into myeloid progenitors in synergy with SCF. Blood-stage malaria infection induces IFN-γ production from CD4+ T cells and NK cells, which may stimulate MSCs to produce IL-27. IL-27 then directly acts on HSCs and promotes the differentiation into myeloid progenitors, resulting in enhanced production of neutrophils to remove malaria-infected RBCs. c HSCs are held within the BM by adhesive interactions and the chemoattraction provided by CXCL12/CXCR4 signaling. G-CSF triggers the expansion of neutrophils and their precursors, creating a proteolytic environment leading to the degradation of adhesive interactions between chemokines and their receptors. Bacteria and their fragments stimulate TLR-expressing ECs but not HSPCs and consequently produce large amounts of G-CSF, which promotes enhanced proliferation of HSPCs and differentiation into neutrophils
Myeloid cells play a critical role in the resolution of red blood cells (RBCs) infected with malaria parasite. After infection with the mouse malaria parasite Plasmodium (P.) chabaudi, an IL-7Rα+c-Kithigh progenitor subset emerges that has both lymphoid and myeloid potential in vitro [44]. After transfer into malaria-infected mice, the progenitors were demonstrated to give rise to mainly myeloid cells that are important for the clearance of infected erythrocytes via IFN-γ signaling in hematopoietic progenitors. Moreover, the importance of the earliest myeloid-restricted progenitors in acute infection with P. chabaudi was noted [37]. The rapid disappearance of these infection-induced myeloid progenitors from the BM was revealed to be accompanied by contraction of the functional myeloid potential in the BM. This process was highly dependent on IFN-γ but independent of TLR in an irradiation-resistant stromal compartment; in addition, IFN-γ was crucial for mobilization of CCR2-expressing HPSCs out of the BM through IFN-γ-induced chemokines, thereby transiently establishing myelopoiesis in the spleen to resolve malaria-infected RBCs.
Although IFN-γ thus controls HSC activation, the underlying molecular mechanism remains largely unknown. The IFN-inducible GTPase Lrg-47 (Irgm1), a critical molecule for host defense, was revealed to inhibit baseline HSC proliferation and to be necessary for a normal HSC response to chemical and infectious stimuli [45]. Irgm1-deficient HSCs were over-proliferating and severely impaired in functional repopulation assays. The molecular basis for these defects was further investigated, and it was found that Irgm1-deficient HSCs showed up-regulation of IFN-response and cell-cycle genes [46]. The defects in hyperproliferation, self-renewal, and autophagy of Irgm1-deficient HSCs were normalized in Irgm1/IFNGR1- and Irgm1/STAT1-double-knockout mice, and the number of HSCs was reduced in aged Irgm1-deficient mice. Thus, negative feedback inhibition of IFN signaling by Irgm1 is necessary to prevent hyperproliferation and depletion of HSCs, preserving HSC number and function.
IL-6
Characteristics: a multifunctional cytokine important for regulation of hematopoiesis as well as immune responses
IL-6 is a multifunctional cytokine that plays critical roles in the immune system as well as in a variety of biological processes including hematopoiesis. It is a primary regulator of both acute and chronic inflammation [47]. The IL-6 receptor consists of a ligand-binding IL-6-receptor α chain (IL-6Rα) and signal-transducing subunit β-receptor glycoprotein 130 (gp130), where Janus kinase (JAK) 1/2, tyrosine kinase 2, and STAT3 bind. IL-6 is secreted by T cells and macrophages in response to infection, trauma, burns, and other tissue damage, resulting in inflammation. IL-6 is responsible for stimulating acute phase protein synthesis as well as the production of neutrophils in the BM. IL-6 also supports the growth of B cells, is required for resistance against various infections, and is secreted by osteoblasts to stimulate osteoclast formation. IL-6 is unique in signaling through not only membrane-bound IL-6Rα but also sIL-6Rα together with ubiquitously expressed gp130 [48, 49].
Roles in infection: stimulation of MPPs by IL-6 produced by MPPs and MSCs promotes emergency myelopoiesis
Although IL-6 is not necessary for maintaining homeostatic blood cell levels, it plays a critical role in hematopoietic lineage development under inflammatory conditions [50]. IL-6Rα is expressed on MPPs and downstream myeloid progenitors, but not on LT-HSCs and short-term repopulating HSCs [51]. Stimulation of these MPPs by IL-6 dramatically induced myeloid cell differentiation while blocking the generation of CD19+ B cells. The regulation of hematopoiesis by specific CD8+ T cells (CTLs), which play a major role in host defense against intracellular pathogens, was further analyzed during acute LCMV infection [38]. Although IFN-γ produced by CTLs did not primarily affect HSPCs directly, IFN-γ promoted the production of IL-6 in BM MSCs, which increased the number of early MPPs and committed myeloid precursors in the BM, thereby promoting the accumulation of myeloid cells in the periphery and clearance of the infection (Fig. 2a). Consistent with this, HSPCs, specifically short-term repopulating HSCs and MPPs, can directly respond to bacterial components via the TLR/nuclear factor κB axis and produce large amounts of cytokines including IL-6 [52] (Fig. 2a). Interestingly, the amounts produced by HSPCs were much greater than those produced by conventional immune cells such as myeloid cells and lymphocytes.
IL-27
Characteristics: a unique cytokine with both pro- and anti-inflammatory properties
IL-27 belongs to the IL-6/IL-12 family of cytokines and plays important roles in immune regulation with both proinflammatory and anti-inflammatory properties acting on various types of cells, such as T cells, B cells, macrophages, and DCs [53,54,55,56]. IL-27 consists of p28 and Epstein–Barr virus-induced gene 3 (EBI3), and it strongly activates both STAT1 and STAT3, which bind to respective IL-27R subunits, the unique subunit WSX-1, and gp130, a common receptor subunit in many of the IL-6 family cytokines. IL-27 augments the early induction of Th1 differentiation and CTL generation [57, 58], whereas it inhibits the differentiation of naive CD4+ T cells into Th2 and Th17 cells and suppresses proinflammatory cytokine production, resulting in reduced development of allergic and autoimmune diseases. Moreover, IL-27 promotes IL-10 production by various Th cells and the generation of IL-10-producing regulatory T (Treg) cells, or Tr1 cells [59,60,61]. Recently, IL-27 was demonstrated to play a critical role in induction of Treg function during autoimmune inflammation [62].
Roles in infection: a novel direct HSC-acting cytokine promoting emergency myelopoiesis
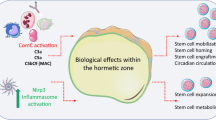
Since IL-27 can efficiently activate both STAT1 and STAT3, which are also activated by IFNs and IL-6, respectively, the role of IL-27 in hematopoiesis has logically been investigated. We first demonstrated that IL-27 in synergy with SCF directly acts on HSCs and promotes their early differentiation in vitro and in vivo [20]. A population highly enriched in mouse HSCs, CD34−KSL cells, was revealed to express both IL-27 receptor subunits, and cultures of these cells with IL-27 and SCF in vitro expanded progenitors including short-term repopulating HSCs and LT-HSCs. Transgenic mice expressing abundant IL-27 also showed enhanced myelopoiesis in the BM and extramedullary hematopoiesis in the spleen with splenomegaly [20]. Moreover, IL-27 similarly promoted the expansion and differentiation of human CD34+ HSCs. Recently, we further clarified that IL-27 is a limited unique cytokine directly acting on HSCs to promote differentiation into myeloid progenitors [21] (Fig. 2b). Among various types of hematopoietic cells in BM, IL-27 predominantly and continuously promoted the expansion of LSK cells only, especially LT-HSCs and myeloid-restricted progenitor cells (MyRPs) with long-term repopulating activity, as well as differentiation into myeloid progenitors in synergy with SCF (Fig. 3). These progenitors showed enhanced potential to differentiate into migratory DCs, neutrophils, and mast cells and less so into macrophages and basophils, but not into plasmacytoid DCs, conventional DCs, T cells, and B cells. Interestingly, among various cytokines, IL-27 had the strongest ability to enhance the expansion of LSK cells and their differentiation into myeloid progenitors that retained the LSK phenotype over a long period [21].
Role of IL-27 in hematopoiesis. LT-HSCs have the capacity to self-renew over the entire life span, and they give rise to all cell types of the BM and peripheral blood. Other pluripotent progenitors (e.g., short-term repopulating HSCs and MPPs) have less self-renewal capacity. Together, these cell types mainly constitute the HSPC population. MPPs are thought to differentiate into the two main branches of hematopoietic development that are the common lymphoid progenitor (CLP) and the common myeloid progenitor (CMP). IL-27 directly activates LT-HSCs and MyRPs with long-term repopulating activity together with SCF and promotes the differentiation into the myeloid progenitors, M-CSFR+Flt3−CD16/32+ LSKs. CDP, common DC progenitor; GMP, granulocyte and macrophage progenitor; MDP, macrophage DC progenitor; MEP, megakaryocyte and erythrocyte progenitor
In the blood stage of malaria infection model with the attenuated variant P. berghei XAT derived from the lethal strain P. berghei NK65, IFN-γ production induced by IL-12 and phagocytic cells in the spleen were previously demonstrated to play critical roles in controlling parasitemia to remove infected RBCs [63, 64]. Recently, it was reported that the blood stage of P. chabaudi infection induces mobilization of early myeloid progenitor cells out of BM, thereby transiently establishing myelopoiesis in the spleen through IFN-γ to resolve the infection [37, 44]. In line with these results, WSX-1-deficient mice showed more increased parasitemia than wild-type mice early in the infection with P. berghei XAT. The infection was revealed to enhance IL-27 expression through IFN-γ production in the BM and spleen, and IL-27 then promoted the expansion and differentiation of LSK cells into myeloid progenitors, enhancing the production of neutrophils to control the infection [21] (Fig. 4). Thus, IL-27 is a novel cytokine that directly acts on HSCs and promotes emergency myelopoiesis.
Promotion of emergency myelopoiesis during blood-stage malaria infection by IL-27. In the blood stage of malaria infection model with the attenuated variant P. berghei XAT derived from the lethal strain P. berghei NK65, IFN-γ production induced by IL-12 and phagocytic cells in the spleen play critical roles in controlling parasitemia to remove infected RBCs. The malaria infection induces splenomegaly and extramedullary hematopoiesis by augmenting IL-27 expression in the BM and spleen via enhanced production of IFN-γ from T cells and NK cells. IL-27 then directly acts on HSCs and promotes their expansion and differentiation into myeloid progenitors together with SCF, resulting in increased production of neutrophils to control the malaria infection. Thus, IL-27 is a novel cytokine that directly acts on HSCs and promotes emergency myelopoiesis
On the other hand, the antitumor efficacy of IL-27 was first demonstrated by us in 2004 using a transplanted mouse tumor model [65]. Then, evidence obtained using a variety of preclinical mouse models indicated that IL-27 has potent antitumor activity against various types of tumors without apparent adverse effects through multiple mechanisms depending on the characteristics of individual tumors [66, 67]. We have recently elucidated a novel mechanism, whereby IL-27 exerts potent antitumor activity through myeloid cells [68]. Although the mouse transplantable tumor model genetically engineered to secrete IL-27 significantly decreased tumor growth [69, 70], we noticed that the number of tumor-infiltrating cells including CD11b+ myeloid cells greatly increased. Similar to the results obtained in the malaria infection model [21], IL-27 was revealed to act directly on BM HSCs and promote the expansion and differentiation into myeloid progenitors, which have enhanced ability to differentiate into antitumorigenic M1 macrophages in tumor-bearing mice [68].
Supporting the effect of IL-27 on hematopoiesis in the BM, a very unique property of the p28 subunit of IL-27 was reported. This subunit has a polyglutamic acid domain, which is very similar to the acidic domain with hydroxyapatite-binding properties and bone tropism to bone sialoprotein (Fig. 2b) [71]. In addition, bone cells such as osteoclasts and osteoblasts were demonstrated to be a source of IL-27 in response to signals through TLRs and cytokines [72]. Because IL-27 has potent antitumoral activity, it could be useful for therapeutic applications targeting hematologic tumor or solid tumor metastasis with bone tropism.
G-CSF
Characteristics: HSC mobilizing cytokine
G-CSF was the first cytokine to be identified and rapidly enter clinical trials. G-CSF was initially used to promote the production of neutrophils in patients with chemotherapy-induced neutropenia [73, 74]. Subsequently, G-CSF was revealed to have an ability to mobilize HSCs from the BM into the blood [75, 76]. G-CSF is a cytokine that signals through its homodimer receptor, G-CSFR, and plays important roles in hematopoiesis by inducing the production of granulocytes in response to infection [77]. G-CSFR is mainly expressed in hematopoietic cells, and G-CSF activates the JAK2/STAT3 signaling pathway. The plasma G-CSF level is normally low, but rise rapidly in response to infection and subsequently decline with recovery [78, 79]. Many tissues including ECs, macrophages, epithelial cells, and fibroblasts can produce G-CSF when stimulated with inflammatory stimuli such as lipopolysaccharide, IFN-β, and IL-17 [80, 81]. The release of G-CSF into the bloodstream by tissues stimulates production of neutrophils within the BM and mobilization from it.
Although the response of hematopoietic cells to G-CSF is essential for HSC mobilization, the effect is indirect, and a specific response of HSCs to G-CSF is not required [82]. HSCs are held within the BM by adhesive interactions and the chemoattraction provided by CXCL12/CXCR4 signaling [83]. G-CSF triggers the expansion of neutrophils and their precursors, creating a proteolytic environment that leads to the degradation of adhesive interactions between chemokines and their receptors [84] (Fig. 2c). G-CSF also stimulates the peripheral sympathetic nervous system [85], increasing catecholamine concentrations, which in turn reduces osteoblasts as well as CXCL12 production by Nestin+ MSC via effects on CD169+ BM macrophages [86]. G-CSF also decreases CXCL12 production by CXCL12-abundant reticular (CAR) cells [87]. Thus, G-CSF dramatically decreases the concentrations of CXCL12 within the BM microenvironment.
Roles in infection: HSC mobilizing cytokine essential for homeostatic granulopoiesis
G-CSF-deficient and G-CSFR-deficient mice showed a 70–90% reduction in circulating neutrophils, indicating an essential role of G-CSF in homeostatic granulopoiesis [88, 89]. In addition, because G-CSF can mediate HSPC mobilization from the BM into the circulation, it is used clinically as a mobilizing agent to prepare a source of HSC for transplantations [90]. G-CSF administration can activate dormant HSCs and increase the proportion of HSCs, resulting in the promotion of granulopoiesis [75]. Dormant HSCs are preferentially mobilized to the peripheral blood on G-CSF treatment without stimulation of their proliferation [91]. Instead, G-CSF-mediated proliferation is restricted to CD41+ HSCs, which function with short term, and primarily myeloid, regenerative potential. To define which cell type is responsible for G-CSF-dependent mobilization, a series of chimeric mice were generated and analyzed using BM transplantation. Expression of the G-CSFR on HSCs was not required for their mobilization by G-CSF, and thus, G-CSFR-dependent signals act in trans to mobilize HSCs from the BM [82]. Another study used tissue-specific myeloid differentiation primary response gene 88 (MYD88)-deficient mice and in vivo lipopolysaccharide administration to model severe bacterial infection with Escherichia coli [92]. The findings revealed that endothelial cells, but not hematopoietic cells, hepatocytes, pericytes, or BM stromal cells, are required for emergency granulopoiesis, biasing of myeloid progenitors toward granulocyte–macrophage progenitors, resulting in accelerated production of neutrophils after lipopolysaccharide stimulation (Fig. 2c).
M-CSF
Characteristics: macrophage differentiating cytokine
M-CSF is a hematopoietic growth factor that plays important roles in the proliferation, differentiation, and survival of monocytes, macrophages, and BM progenitor cells by interacting with its receptor M-CSFR [93]. M-CSF is broadly expressed and detected in the blood circulation and regulates steady-state myelopoiesis. M-CSFR is predominantly expressed by the monocyte and macrophage lineages including osteoclasts and a subset of CD11b+ DCs and their precursors [94]. In addition, M-CSFR expression is reported on neural precursors and trophoblasts [94]. Mice deficient for M-CSF or M-CSFR exhibit skeletal, sensory, and reproductive abnormalities caused by severe deficiencies in tissue macrophages and osteoclasts [95].
Roles in infection: instructive differentiation of HSCs by M-CSF into myeloid cells
M-CSF is produced during infection and increases the generation of myeloid cells from lineage-committed progenitors. The ability of M-CSF to induce myeloid commitment divisions in HSCs is restricted by the monocytic transcription factor MafB [96]. MafB-deficient HSCs were shown to enhance sensitivity specifically to M-CSF and activate the myeloid master regulator PU.1, thereby skewing toward myeloid differentiation. In general, cell-fate choice of HSCs has been explained by the stochastic model [97]. However, M-CSF, but not GM-CSF or G-CSF, was demonstrated to directly induce the myeloid master regulator PU.1 at a single-cell level and instruct myeloid cell-fate change on mouse HSCs to myeloid cells, independently of selective survival or proliferation [98]. Of note, M-CSF did not compromise long-term repopulating activity of HSCs. Moreover, myeloablative treatment preceding HSC and progenitor cell transplantation is accompanied by severe myeloid cytopenia and increased susceptibility to infections in the lag period before hematopoietic recovery. Therefore, whether M-CSF might be effective in ameliorating myeloid cytopenias and in protecting from infection after hematopoietic cell transplantation was recently investigated [99]. M-CSF treatment during transplantation or after infection with clinically relevant pathogens Pseudomonas aeruginosa and Aspergillus fumigatus increased myelopoiesis and improved survival with decreased pathogen load, even for early infections and single-dose treatments. In contrast, G-CSF showed less efficient cell recovery and no protective activity against the pathogens. Thus, M-CSF treatment during hematopoietic cell transplantation could be more efficient in myeloid cell commitment of HSCs with less side effects than clinically used G-CSF.
IL-1
Characteristics: a key proinflammatory cytokine
The IL-1 family comprises 11 cytokines that play a critical role in the initiation of proinflammatory responses to infections or sterile insults by up-regulating expression of integrins on leukocytes and ECs [100]. IL-1 consists of two related genes, IL-1α and IL-1β, which have similar biological activities with distinct regulation. Their receptor complex is composed of IL-1RI and IL-1R accessory protein (IL-1RAP), together with downstream adaptor protein MYD88. IL-1RAP-deficient mice show completely abrogated cellular responses to IL-1 [101]. IL-1 receptor antagonist (IL-1RA) regulates IL-1α and IL-1β proinflammatory activity by competing with them for binding sites of the receptor. IL-1 is a key proinflammatory signal that rapidly augments host defense in innate immunity, but also induces tissue destruction in autoimmune and inflammatory diseases [102].
Roles in infection: reversible impairment of HSC function by chronic IL-1 stimulation
Acute IL-1 signaling leads to increased myeloid cell production both in culture and in response to infection, irradiation or myeloablative chemotherapy [103,104,105]. In contrast, chronic IL-1 production is associated with many of inflammatory diseases such as rheumatoid arthritis, type 2 diabetes, and obesity, which are characterized by severe hematological disorders including overproduction of tissue-damaging myeloid cells and chronic anemia [106,107,108]. The mechanism whereby IL-1 communicates with HSCs and the consequence for HSC activity was clarified [109]. In preclinical models, IL-1 promotes HSC differentiation biased into the myeloid lineage, in part through activation of PU.1 signaling [109]. While acute IL-1 exposure contributes to HSC regeneration after myeloablation and transplantation [109, 110], chronic exposure promotes uncontrolled HSC division, lost of self-renewal activity, and eventual exhaustion of the HSC pool [109]. However, this damaging effect was transient and recovered to a normal phenotype after withdrawal of IL-1.
Conclusion
In the BM, which is an important site for hematopoiesis, memory T cells and antibody-producing plasma cells are recruited and retained long term. Diverse cells including these T and B cells, ECs, osteoblasts, and MSCs constitute the BM niche. Extensive recent research has indicated that the myelopoiesis in the BM is tightly regulated by inflammatory signals elicited via proinflammatory cytokines produced from activated T cells as well as from innate myeloid cells in a cell contact-dependent manner during emergency myelopoiesis. Therefore, a better understanding of the roles of proinflammatory cytokines in myeloid hematopoiesis could open a novel avenue to develop therapies against diseases including infectious diseases and hematological malignancies.
Abbreviations
- BM:
-
Bone marrow
- CAR:
-
C-X-C motif ligand 12-abundant reticular
- CTL:
-
Cytotoxic CD8+ T cell
- CXCL:
-
C-X-C motif ligand
- DC:
-
Dendritic cell
- EC:
-
Endothelial cell
- G-CSF:
-
Granulocyte colony-stimulating factor
- gp130:
-
β-Receptor glycoprotein 130
- GM-CSF:
-
Granulocyte macrophage colony-stimulating factor
- HSC:
-
Hematopoietic stem cell
- HSPC:
-
Hematopoietic stem and progenitor cell
- IFN:
-
Interferon
- IFNAR:
-
IFN-α receptor
- IL:
-
Interleukin
- JAK:
-
Janus kinase
- LCMV:
-
Lymphocytic choriomeningitis virus
- LSK:
-
Lineage−Sca-1+c-Kit+
- LT-HSC:
-
Long-term repopulating hematopoietic stem cell
- M-CSF:
-
Macrophage colony-stimulating factor
- MDSC:
-
Myeloid-derived suppressor cell
- MPP:
-
Multipotent progenitor
- MYD88:
-
Myeloid differentiation primary response gene 88
- MyRP:
-
Myeloid-restricted progenitor cell
- MSC:
-
Mesenchymal stem/stromal cell
- NK:
-
Natural killer
- P. :
-
Plasmodium
- R:
-
Receptor
- RBC:
-
Red blood cell
- Sca-1:
-
Stem cell antigen-1
- SCF:
-
Stem cell factor
- STAT:
-
Signal transducer and activator of transcription
- Th:
-
Helper T
- TLR:
-
Toll-like receptor
- Treg:
-
Regulatory T
References
Orkin SH, Zon LI (2008) Hematopoiesis: an evolving paradigm for stem cell biology. Cell 132(4):631–644. https://doi.org/10.1016/j.cell.2008.01.025
Oguro H, Ding L, Morrison SJ (2013) SLAM family markers resolve functionally distinct subpopulations of hematopoietic stem cells and multipotent progenitors. Cell Stem Cell 13(1):102–116. https://doi.org/10.1016/j.stem.2013.05.014
Pang WW, Price EA, Sahoo D, Beerman I, Maloney WJ, Rossi DJ, Schrier SL, Weissman IL (2011) Human bone marrow hematopoietic stem cells are increased in frequency and myeloid-biased with age. Proc Natl Acad Sci USA 108(50):20012–20017. https://doi.org/10.1073/pnas.1116110108
Mohrin M, Bourke E, Alexander D, Warr MR, Barry-Holson K, Le Beau MM, Morrison CG, Passegue E (2010) Hematopoietic stem cell quiescence promotes error-prone DNA repair and mutagenesis. Cell Stem Cell 7(2):174–185. https://doi.org/10.1016/j.stem.2010.06.014
Ding L, Morrison SJ (2013) Haematopoietic stem cells and early lymphoid progenitors occupy distinct bone marrow niches. Nature 495(7440):231–235. https://doi.org/10.1038/nature11885
Ding L, Saunders TL, Enikolopov G, Morrison SJ (2012) Endothelial and perivascular cells maintain haematopoietic stem cells. Nature 481(7382):457–462. https://doi.org/10.1038/nature10783
Mendez-Ferrer S, Michurina TV, Ferraro F, Mazloom AR, Macarthur BD, Lira SA, Scadden DT, Ma’ayan A, Enikolopov GN, Frenette PS (2010) Mesenchymal and haematopoietic stem cells form a unique bone marrow niche. Nature 466(7308):829–834. https://doi.org/10.1038/nature09262
Monteiro JP, Benjamin A, Costa ES, Barcinski MA, Bonomo A (2005) Normal hematopoiesis is maintained by activated bone marrow CD4+ T cells. Blood 105(4):1484–1491. https://doi.org/10.1182/blood-2004-07-2856
Yamazaki S, Ema H, Karlsson G, Yamaguchi T, Miyoshi H, Shioda S, Taketo MM, Karlsson S, Iwama A, Nakauchi H (2011) Nonmyelinating Schwann cells maintain hematopoietic stem cell hibernation in the bone marrow niche. Cell 147(5):1146–1158. https://doi.org/10.1016/j.cell.2011.09.053
Takizawa H, Boettcher S, Manz MG (2012) Demand-adapted regulation of early hematopoiesis in infection and inflammation. Blood 119(13):2991–3002. https://doi.org/10.1182/blood-2011-12-380113
Sato T, Onai N, Yoshihara H, Arai F, Suda T, Ohteki T (2009) Interferon regulatory factor-2 protects quiescent hematopoietic stem cells from type I interferon-dependent exhaustion. Nat Med 15(6):696–700. https://doi.org/10.1038/nm.1973
Essers MA, Offner S, Blanco-Bose WE, Waibler Z, Kalinke U, Duchosal MA, Trumpp A (2009) IFNalpha activates dormant haematopoietic stem cells in vivo. Nature 458(7240):904–908. https://doi.org/10.1038/nature07815
Baldridge MT, King KY, Boles NC, Weksberg DC, Goodell MA (2010) Quiescent haematopoietic stem cells are activated by IFN-gamma in response to chronic infection. Nature 465(7299):793–797. https://doi.org/10.1038/nature09135
Boettcher S, Ziegler P, Schmid MA, Takizawa H, van Rooijen N, Kopf M, Heikenwalder M, Manz MG (2012) Cutting edge: LPS-induced emergency myelopoiesis depends on TLR4-expressing nonhematopoietic cells. J Immunol 188(12):5824–5828. https://doi.org/10.4049/jimmunol.1103253
Boettcher S, Manz MG (2016) Sensing and translation of pathogen signals into demand-adapted myelopoiesis. Curr Opin Hematol 23(1):5–10. https://doi.org/10.1097/MOH.0000000000000201
Mirantes C, Passegue E, Pietras EM (2014) Pro-inflammatory cytokines: emerging players regulating HSC function in normal and diseased hematopoiesis. Exp Cell Res 329(2):248–254. https://doi.org/10.1016/j.yexcr.2014.08.017
Clapes T, Lefkopoulos S, Trompouki E (2016) Stress and non-stress roles of inflammatory signals during HSC emergence and maintenance. Front Immunol 7:487. https://doi.org/10.3389/fimmu.2016.00487
Boiko JR, Borghesi L (2012) Hematopoiesis sculpted by pathogens: toll-like receptors and inflammatory mediators directly activate stem cells. Cytokine 57(1):1–8. https://doi.org/10.1016/j.cyto.2011.10.005
Monlish DA, Bhatt ST, Schuettpelz LG (2016) The role of toll-like receptors in hematopoietic malignancies. Front Immunol 7:390. https://doi.org/10.3389/fimmu.2016.00390
Seita J, Asakawa M, Ooehara J, Takayanagi S, Morita Y, Watanabe N, Fujita K, Kudo M, Mizuguchi J, Ema H, Nakauchi H, Yoshimoto T (2008) Interleukin-27 directly induces differentiation in hematopoietic stem cells. Blood 111(4):1903–1912. https://doi.org/10.1182/blood-2007-06-093328
Furusawa J, Mizoguchi I, Chiba Y, Hisada M, Kobayashi F, Yoshida H, Nakae S, Tsuchida A, Matsumoto T, Ema H, Mizuguchi J, Yoshimoto T (2016) Promotion of expansion and differentiation of hematopoietic stem cells by interleukin-27 into myeloid progenitors to control infection in emergency myelopoiesis. PLoS Pathog 12(3):e1005507. https://doi.org/10.1371/journal.ppat.1005507
Isaacs A, Lindenmann J (1957) Virus interference. I. The interferon. Proc R Soc Lond B Biol Sci 147(927):258–267
Binder D, Fehr J, Hengartner H, Zinkernagel RM (1997) Virus-induced transient bone marrow aplasia: major role of interferon-alpha/beta during acute infection with the noncytopathic lymphocytic choriomeningitis virus. J Exp Med 185(3):517–530
Lapidot T, Sirard C, Vormoor J, Murdoch B, Hoang T, Caceres-Cortes J, Minden M, Paterson B, Caligiuri MA, Dick JE (1994) A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature 367(6464):645–648. https://doi.org/10.1038/367645a0
Riether C, Schurch CM, Ochsenbein AF (2015) Regulation of hematopoietic and leukemic stem cells by the immune system. Cell Death Differ 22(2):187–198. https://doi.org/10.1038/cdd.2014.89
Schepers K, Pietras EM, Reynaud D, Flach J, Binnewies M, Garg T, Wagers AJ, Hsiao EC, Passegue E (2013) Myeloproliferative neoplasia remodels the endosteal bone marrow niche into a self-reinforcing leukemic niche. Cell Stem Cell 13(3):285–299. https://doi.org/10.1016/j.stem.2013.06.009
Pietras EM, Lakshminarasimhan R, Techner JM, Fong S, Flach J, Binnewies M, Passegue E (2014) Re-entry into quiescence protects hematopoietic stem cells from the killing effect of chronic exposure to type I interferons. J Exp Med 211(2):245–262. https://doi.org/10.1084/jem.20131043
Haas S, Hansson J, Klimmeck D, Loeffler D, Velten L, Uckelmann H, Wurzer S, Prendergast AM, Schnell A, Hexel K, Santarella-Mellwig R, Blaszkiewicz S, Kuck A, Geiger H, Milsom MD, Steinmetz LM, Schroeder T, Trumpp A, Krijgsveld J, Essers MA (2015) Inflammation-induced emergency megakaryopoiesis driven by hematopoietic stem cell-like megakaryocyte progenitors. Cell Stem Cell 17(4):422–434. https://doi.org/10.1016/j.stem.2015.07.007
Billiau A, Matthys P (2009) Interferon-gamma: a historical perspective. Cytokine Growth Factor Rev 20(2):97–113. https://doi.org/10.1016/j.cytogfr.2009.02.004
Bach EA, Aguet M, Schreiber RD (1997) The IFN gamma receptor: a paradigm for cytokine receptor signaling. Annu Rev Immunol 15:563–591. https://doi.org/10.1146/annurev.immunol.15.1.563
Farrar MA, Schreiber RD (1993) The molecular cell biology of interferon-gamma and its receptor. Annu Rev Immunol 11:571–611. https://doi.org/10.1146/annurev.iy.11.040193.003035
Maciejewski J, Selleri C, Anderson S, Young NS (1995) Fas antigen expression on CD34+ human marrow cells is induced by interferon gamma and tumor necrosis factor alpha and potentiates cytokine-mediated hematopoietic suppression in vitro. Blood 85(11):3183–3190
Snoeck HW, Van Bockstaele DR, Nys G, Lenjou M, Lardon F, Haenen L, Rodrigus I, Peetermans ME, Berneman ZN (1994) Interferon gamma selectively inhibits very primitive CD342+ CD38− and not more mature CD34+ CD38+ human hematopoietic progenitor cells. J Exp Med 180(3):1177–1182
Kawano Y, Takaue Y, Hirao A, Abe T, Saito S, Matsunaga K, Watanabe T, Hirose M, Ninomiya T, Kuroda Y et al (1991) Synergistic effect of recombinant interferon-gamma and interleukin-3 on the growth of immature human hematopoietic progenitors. Blood 77(10):2118–2121
Brugger W, Mocklin W, Heimfeld S, Berenson RJ, Mertelsmann R, Kanz L (1993) Ex vivo expansion of enriched peripheral blood CD34+ progenitor cells by stem cell factor, interleukin-1 beta (IL-1 beta), IL-6, IL-3, interferon-gamma, and erythropoietin. Blood 81(10):2579–2584
de Bruin AM, Demirel O, Hooibrink B, Brandts CH, Nolte MA (2013) Interferon-gamma impairs proliferation of hematopoietic stem cells in mice. Blood 121(18):3578–3585. https://doi.org/10.1182/blood-2012-05-432906
Belyaev NN, Biro J, Langhorne J, Potocnik AJ (2013) Extramedullary myelopoiesis in malaria depends on mobilization of myeloid-restricted progenitors by IFN-gamma induced chemokines. PLoS Pathog 9(6):e1003406. https://doi.org/10.1371/journal.ppat.1003406
Schurch CM, Riether C, Ochsenbein AF (2014) Cytotoxic CD8+ T cells stimulate hematopoietic progenitors by promoting cytokine release from bone marrow mesenchymal stromal cells. Cell Stem Cell 14(4):460–472. https://doi.org/10.1016/j.stem.2014.01.002
Guermonprez P, Helft J, Claser C, Deroubaix S, Karanje H, Gazumyan A, Darasse-Jeze G, Telerman SB, Breton G, Schreiber HA, Frias-Staheli N, Billerbeck E, Dorner M, Rice CM, Ploss A, Klein F, Swiecki M, Colonna M, Kamphorst AO, Meredith M, Niec R, Takacs C, Mikhail F, Hari A, Bosque D, Eisenreich T, Merad M, Shi Y, Ginhoux F, Renia L, Urban BC, Nussenzweig MC (2013) Inflammatory Flt3l is essential to mobilize dendritic cells and for T cell responses during Plasmodium infection. Nat Med 19(6):730–738. https://doi.org/10.1038/nm.3197
Zhao X, Ren G, Liang L, Ai PZ, Zheng B, Tischfield JA, Shi Y, Shao C (2010) Brief report: interferon-gamma induces expansion of Lin(−)Sca-1(+)C-Kit(+) Cells. Stem Cells 28(1):122–126. https://doi.org/10.1002/stem.252
MacNamara KC, Jones M, Martin O, Winslow GM (2011) Transient activation of hematopoietic stem and progenitor cells by IFNgamma during acute bacterial infection. PLoS One 6(12):e28669. https://doi.org/10.1371/journal.pone.0028669
Umemoto T, Yamato M, Ishihara J, Shiratsuchi Y, Utsumi M, Morita Y, Tsukui H, Terasawa M, Shibata T, Nishida K, Kobayashi Y, Petrich BG, Nakauchi H, Eto K, Okano T (2012) Integrin-alphavbeta3 regulates thrombopoietin-mediated maintenance of hematopoietic stem cells. Blood 119(1):83–94. https://doi.org/10.1182/blood-2011-02-335430
Umemoto T, Matsuzaki Y, Shiratsuchi Y, Hashimoto M, Yoshimoto T, Nakamura-Ishizu A, Petrich B, Yamato M, Suda T (2017) Integrin alphavbeta3 enhances the suppressive effect of interferon-gamma on hematopoietic stem cells. EMBO J 36(16):2390–2403. https://doi.org/10.15252/embj.201796771
Belyaev NN, Brown DE, Diaz AI, Rae A, Jarra W, Thompson J, Langhorne J, Potocnik AJ (2010) Induction of an IL7-R(+)c-Kit(hi) myelolymphoid progenitor critically dependent on IFN-gamma signaling during acute malaria. Nat Immunol 11(6):477–485. https://doi.org/10.1038/ni.1869
Feng CG, Weksberg DC, Taylor GA, Sher A, Goodell MA (2008) The p47 GTPase Lrg-47 (Irgm1) links host defense and hematopoietic stem cell proliferation. Cell Stem Cell 2(1):83–89. https://doi.org/10.1016/j.stem.2007.10.007
King KY, Baldridge MT, Weksberg DC, Chambers SM, Lukov GL, Wu S, Boles NC, Jung SY, Qin J, Liu D, Songyang Z, Eissa NT, Taylor GA, Goodell MA (2011) Irgm1 protects hematopoietic stem cells by negative regulation of IFN signaling. Blood 118(6):1525–1533. https://doi.org/10.1182/blood-2011-01-328682
Ishihara K, Hirano T (2002) IL-6 in autoimmune disease and chronic inflammatory proliferative disease. Cytokine Growth Factor Rev 13(4–5):357–368
Schaper F, Rose-John S (2015) Interleukin-6: biology, signaling and strategies of blockade. Cytokine Growth Factor Rev 26(5):475–487. https://doi.org/10.1016/j.cytogfr.2015.07.004
Scheller J, Chalaris A, Schmidt-Arras D, Rose-John S (2011) The pro- and anti-inflammatory properties of the cytokine interleukin-6. Biochim Biophys Acta 1813(5):878–888. https://doi.org/10.1016/j.bbamcr.2011.01.034
Maeda K, Baba Y, Nagai Y, Miyazaki K, Malykhin A, Nakamura K, Kincade PW, Sakaguchi N, Coggeshall KM (2005) IL-6 blocks a discrete early step in lymphopoiesis. Blood 106(3):879–885. https://doi.org/10.1182/blood-2005-02-0456
Reynaud D, Pietras E, Barry-Holson K, Mir A, Binnewies M, Jeanne M, Sala-Torra O, Radich JP, Passegue E (2011) IL-6 controls leukemic multipotent progenitor cell fate and contributes to chronic myelogenous leukemia development. Cancer Cell 20(5):661–673. https://doi.org/10.1016/j.ccr.2011.10.012
Zhao JL, Ma C, O’Connell RM, Mehta A, DiLoreto R, Heath JR, Baltimore D (2014) Conversion of danger signals into cytokine signals by hematopoietic stem and progenitor cells for regulation of stress-induced hematopoiesis. Cell Stem Cell 14(4):445–459. https://doi.org/10.1016/j.stem.2014.01.007
Pflanz S, Timans JC, Cheung J, Rosales R, Kanzler H, Gilbert J, Hibbert L, Churakova T, Travis M, Vaisberg E, Blumenschein WM, Mattson JD, Wagner JL, To W, Zurawski S, McClanahan TK, Gorman DM, Bazan JF, de Waal Malefyt R, Rennick D, Kastelein RA (2002) IL-27, a heterodimeric cytokine composed of EBI3 and p28 protein, induces proliferation of naive CD4 + T cells. Immunity 16(6):779–790. https://doi.org/10.1016/S1074-7613(02)00324-2
Hall AO, Silver JS, Hunter CA (2012) The Immunobiology of IL-27. Adv Immunol 115:1–44. https://doi.org/10.1016/b978-0-12-394299-9.00001-1
Mizoguchi I, Higuchi K, Mitobe K, Tsunoda R, Mizuguchi J, Yoshimoto T (2013) Interleukin-27: regulation of immune responses and disease development by a pleiotropic cytokine with pro- and anti-inflammatory properties. In: Yoshimoto T, Yoshimoto T (eds) Cytokine frontiers: regulation of immune responses in health and disease. Springer, Tokyo, pp 353–375
Yoshida H, Hunter CA (2015) The immunobiology of interleukin-27. Annu Rev Immunol 33:417–443. https://doi.org/10.1146/annurev-immunol-032414-112134
Morishima N, Owaki T, Asakawa M, Kamiya S, Mizuguchi J, Yoshimoto T (2005) Augmentation of effector CD8+ T cell generation with enhanced granzyme B expression by IL-27. J Immunol 175(3):1686–1693
Schneider R, Yaneva T, Beauseigle D, El-Khoury L, Arbour N (2011) IL-27 increases the proliferation and effector functions of human naive CD8+ T lymphocytes and promotes their development into Tc1 cells. Eur J Immunol 41(1):47–59. https://doi.org/10.1002/eji.201040804
Awasthi A, Carrier Y, Peron JP, Bettelli E, Kamanaka M, Flavell RA, Kuchroo VK, Oukka M, Weiner HL (2007) A dominant function for interleukin 27 in generating interleukin 10-producing anti-inflammatory T cells. Nat Immunol 8(12):1380–1389. https://doi.org/10.1038/ni1541
Fitzgerald DC, Zhang GX, El-Behi M, Fonseca-Kelly Z, Li H, Yu S, Saris CJ, Gran B, Ciric B, Rostami A (2007) Suppression of autoimmune inflammation of the central nervous system by interleukin 10 secreted by interleukin 27-stimulated T cells. Nat Immunol 8(12):1372–1379
Stumhofer JS, Silver JS, Laurence A, Porrett PM, Harris TH, Turka LA, Ernst M, Saris CJ, O’Shea JJ, Hunter CA (2007) Interleukins 27 and 6 induce STAT3-mediated T cell production of interleukin 10. Nat Immunol 8(12):1363–1371
Do J, Kim D, Kim S, Valentin-Torres A, Dvorina N, Jang E, Nagarajavel V, DeSilva TM, Li X, Ting AH, Vignali DAA, Stohlman SA, Baldwin WM 3rd, Min B (2017) Treg-specific IL-27Ralpha deletion uncovers a key role for IL-27 in Treg function to control autoimmunity. Proc Natl Acad Sci USA 114(38):10190–10195. https://doi.org/10.1073/pnas.1703100114
Yoshimoto T, Yoneto T, Waki S, Nariuchi H (1998) Interleukin-12-dependent mechanisms in the clearance of blood-stage murine malaria parasite Plasmodium berghei XAT, an attenuated variant of P. berghei NK65. J Infect Dis 177(6):1674–1681
Yoneto T, Waki S, Takai T, Tagawa Y, Iwakura Y, Mizuguchi J, Nariuchi H, Yoshimoto T (2001) A critical role of Fc receptor-mediated antibody-dependent phagocytosis in the host resistance to blood-stage Plasmodium berghei XAT infection. J Immunol 166(10):6236–6241
Hisada M, Kamiya S, Fujita K, Belladonna ML, Aoki T, Koyanagi Y, Mizuguchi J, Yoshimoto T (2004) Potent antitumor activity of interleukin-27. Cancer Res 64(3):1152–1156. https://doi.org/10.1158/0008-5472.CAN-03-2084
Yoshimoto T, Chiba Y, Furusawa JI, Xu M, Tsunoda R, Higuchi K, Mizoguchi I (2015) Potential clinical application of interleukin-27 as an antitumor agent. Cancer Sci. https://doi.org/10.1111/cas.12731
Mizoguchi I, Chiba Y, Furusawa JI, Xu M, Tsunoda R, Higuchi K, Yoshimoto T (2015) Therapeutic potential of interleukin-27 against cancers in preclinical mouse models. Oncoimmunology 4(10):e1042200. https://doi.org/10.1080/2162402X.2015.1042200
Chiba Y, Mizoguchi I, Furusawa J, Hasegawa H, Ohashi M, Xu M, Owaki T, Yoshimoto T (2017) Interleukin-27 exerts its antitumor effects by promoting differentiation of hematopoietic stem cells to M1 macrophages. Cancer Res. https://doi.org/10.1158/0008-5472.CAN-17-0960
Shimizu M, Shimamura M, Owaki T, Asakawa M, Fujita K, Kudo M, Iwakura Y, Takeda Y, Luster AD, Mizuguchi J, Yoshimoto T (2006) Antiangiogenic and antitumor activities of IL-27. J Immunol 176(12):7317–7324
Yoshimoto T, Morishima N, Mizoguchi I, Shimizu M, Nagai H, Oniki S, Oka M, Nishigori C, Mizuguchi J (2008) Antiproliferative activity of IL-27 on melanoma. J Immunol 180(10):6527–6535
Tormo AJ, Beaupre LA, Elson G, Crabe S, Gauchat JF (2013) A polyglutamic acid motif confers IL-27 hydroxyapatite and bone-binding properties. J Immunol 190(6):2931–2937. https://doi.org/10.4049/jimmunol.1201460
Larousserie F, Bsiri L, Dumaine V, Dietrich C, Audebourg A, Radenen-Bussiere B, Anract P, Vacher-Lavenu MC, Devergne O (2017) Frontline science: human bone cells as a source of IL-27 under inflammatory conditions: role of TLRs and cytokines. J Leukoc Biol 101(6):1289–1300. https://doi.org/10.1189/jlb.3HI0616-280R
Bronchud MH, Scarffe JH, Thatcher N, Crowther D, Souza LM, Alton NK, Testa NG, Dexter TM (1987) Phase I/II study of recombinant human granulocyte colony-stimulating factor in patients receiving intensive chemotherapy for small cell lung cancer. Br J Cancer 56(6):809–813
Gabrilove JL, Jakubowski A, Scher H, Sternberg C, Wong G, Grous J, Yagoda A, Fain K, Moore MA, Clarkson B et al (1988) Effect of granulocyte colony-stimulating factor on neutropenia and associated morbidity due to chemotherapy for transitional-cell carcinoma of the urothelium. N Engl J Med 318(22):1414–1422. https://doi.org/10.1056/NEJM198806023182202
Tamura M, Hattori K, Nomura H, Oheda M, Kubota N, Imazeki I, Ono M, Ueyama Y, Nagata S, Shirafuji N et al (1987) Induction of neutrophilic granulocytosis in mice by administration of purified human native granulocyte colony-stimulating factor (G-CSF). Biochem Biophys Res Commun 142(2):454–460
Duhrsen U, Villeval JL, Boyd J, Kannourakis G, Morstyn G, Metcalf D (1988) Effects of recombinant human granulocyte colony-stimulating factor on hematopoietic progenitor cells in cancer patients. Blood 72(6):2074–2081
Demetri GD, Griffin JD (1991) Granulocyte colony-stimulating factor and its receptor. Blood 78(11):2791–2808
Cebon J, Layton JE, Maher D, Morstyn G (1994) Endogenous haemopoietic growth factors in neutropenia and infection. Br J Haematol 86(2):265–274
Kawakami M, Tsutsumi H, Kumakawa T, Abe H, Hirai M, Kurosawa S, Mori M, Fukushima M (1990) Levels of serum granulocyte colony-stimulating factor in patients with infections. Blood 76(10):1962–1964
Sano E, Ohashi K, Sato Y, Kashiwagi M, Joguchi A, Naruse N (2007) A possible role of autogenous IFN-beta for cytokine productions in human fibroblasts. J Cell Biochem 100(6):1459–1476. https://doi.org/10.1002/jcb.21128
Fossiez F, Djossou O, Chomarat P, Flores-Romo L, Ait-Yahia S, Maat C, Pin JJ, Garrone P, Garcia E, Saeland S, Blanchard D, Gaillard C, Das Mahapatra B, Rouvier E, Golstein P, Banchereau J, Lebecque S (1996) T cell interleukin-17 induces stromal cells to produce proinflammatory and hematopoietic cytokines. J Exp Med 183(6):2593–2603
Liu F, Poursine-Laurent J, Link DC (2000) Expression of the G-CSF receptor on hematopoietic progenitor cells is not required for their mobilization by G-CSF. Blood 95(10):3025–3031
Levesque JP, Hendy J, Takamatsu Y, Simmons PJ, Bendall LJ (2003) Disruption of the CXCR4/CXCL12 chemotactic interaction during hematopoietic stem cell mobilization induced by GCSF or cyclophosphamide. J Clin Invest 111(2):187–196. https://doi.org/10.1172/JCI15994
Pelus LM, Bian H, King AG, Fukuda S (2004) Neutrophil-derived MMP-9 mediates synergistic mobilization of hematopoietic stem and progenitor cells by the combination of G-CSF and the chemokines GRObeta/CXCL2 and GRObetaT/CXCL2delta4. Blood 103(1):110–119. https://doi.org/10.1182/blood-2003-04-1115
Katayama Y, Battista M, Kao WM, Hidalgo A, Peired AJ, Thomas SA, Frenette PS (2006) Signals from the sympathetic nervous system regulate hematopoietic stem cell egress from bone marrow. Cell 124(2):407–421. https://doi.org/10.1016/j.cell.2005.10.041
Chow A, Lucas D, Hidalgo A, Mendez-Ferrer S, Hashimoto D, Scheiermann C, Battista M, Leboeuf M, Prophete C, van Rooijen N, Tanaka M, Merad M, Frenette PS (2011) Bone marrow CD169+ macrophages promote the retention of hematopoietic stem and progenitor cells in the mesenchymal stem cell niche. J Exp Med 208(2):261–271. https://doi.org/10.1084/jem.20101688
Semerad CL, Christopher MJ, Liu F, Short B, Simmons PJ, Winkler I, Levesque JP, Chappel J, Ross FP, Link DC (2005) G-CSF potently inhibits osteoblast activity and CXCL12 mRNA expression in the bone marrow. Blood 106(9):3020–3027. https://doi.org/10.1182/blood-2004-01-0272
Lieschke GJ, Grail D, Hodgson G, Metcalf D, Stanley E, Cheers C, Fowler KJ, Basu S, Zhan YF, Dunn AR (1994) Mice lacking granulocyte colony-stimulating factor have chronic neutropenia, granulocyte and macrophage progenitor cell deficiency, and impaired neutrophil mobilization. Blood 84(6):1737–1746
Liu F, Wu HY, Wesselschmidt R, Kornaga T, Link DC (1996) Impaired production and increased apoptosis of neutrophils in granulocyte colony-stimulating factor receptor-deficient mice. Immunity 5(5):491–501
Anasetti C, Logan BR, Lee SJ, Waller EK, Weisdorf DJ, Wingard JR, Cutler CS, Westervelt P, Woolfrey A, Couban S, Ehninger G, Johnston L, Maziarz RT, Pulsipher MA, Porter DL, Mineishi S, McCarty JM, Khan SP, Anderlini P, Bensinger WI, Leitman SF, Rowley SD, Bredeson C, Carter SL, Horowitz MM, Confer DL, Blood Marrow Transplant, Clinical Trials N (2012) Peripheral-blood stem cells versus bone marrow from unrelated donors. N Engl J Med 367(16):1487–1496. https://doi.org/10.1056/NEJMoa1203517
Bernitz JM, Daniel MG, Fstkchyan YS, Moore K (2017) Granulocyte colony-stimulating factor mobilizes dormant hematopoietic stem cells without proliferation in mice. Blood 129(14):1901–1912. https://doi.org/10.1182/blood-2016-11-752923
Boettcher S, Gerosa RC, Radpour R, Bauer J, Ampenberger F, Heikenwalder M, Kopf M, Manz MG (2014) Endothelial cells translate pathogen signals into G-CSF-driven emergency granulopoiesis. Blood 124(9):1393–1403. https://doi.org/10.1182/blood-2014-04-570762
Ushach I, Zlotnik A (2016) Biological role of granulocyte macrophage colony-stimulating factor (GM-CSF) and macrophage colony-stimulating factor (M-CSF) on cells of the myeloid lineage. J Leukoc Biol 100(3):481–489. https://doi.org/10.1189/jlb.3RU0316-144R
Jones CV, Ricardo SD (2013) Macrophages and CSF-1: implications for development and beyond. Organogenesis 9(4):249–260. https://doi.org/10.4161/org.25676
Dai XM, Ryan GR, Hapel AJ, Dominguez MG, Russell RG, Kapp S, Sylvestre V, Stanley ER (2002) Targeted disruption of the mouse colony-stimulating factor 1 receptor gene results in osteopetrosis, mononuclear phagocyte deficiency, increased primitive progenitor cell frequencies, and reproductive defects. Blood 99(1):111–120
Sarrazin S, Mossadegh-Keller N, Fukao T, Aziz A, Mourcin F, Vanhille L, Kelly Modis L, Kastner P, Chan S, Duprez E, Otto C, Sieweke MH (2009) MafB restricts M-CSF-dependent myeloid commitment divisions of hematopoietic stem cells. Cell 138(2):300–313. https://doi.org/10.1016/j.cell.2009.04.057
Till JE, McCulloch EA, Siminovitch L (1964) A stochastic model of stem cell proliferation, based on the growth of spleen colony-forming cells. Proc Natl Acad Sci USA 51:29–36
Mossadegh-Keller N, Sarrazin S, Kandalla PK, Espinosa L, Stanley ER, Nutt SL, Moore J, Sieweke MH (2013) M-CSF instructs myeloid lineage fate in single haematopoietic stem cells. Nature 497(7448):239–243. https://doi.org/10.1038/nature12026
Kandalla PK, Sarrazin S, Molawi K, Berruyer C, Redelberger D, Favel A, Bordi C, de Bentzmann S, Sieweke MH (2016) M-CSF improves protection against bacterial and fungal infections after hematopoietic stem/progenitor cell transplantation. J Exp Med 213(11):2269–2279. https://doi.org/10.1084/jem.20151975
Dinarello CA, van der Meer JW (2013) Treating inflammation by blocking interleukin-1 in humans. Semin Immunol 25(6):469–484. https://doi.org/10.1016/j.smim.2013.10.008
Cullinan EB, Kwee L, Nunes P, Shuster DJ, Ju G, McIntyre KW, Chizzonite RA, Labow MA (1998) IL-1 receptor accessory protein is an essential component of the IL-1 receptor. J Immunol 161(10):5614–5620
Dinarello CA, Simon A, van der Meer JW (2012) Treating inflammation by blocking interleukin-1 in a broad spectrum of diseases. Nat Rev Drug Discov 11(8):633–652. https://doi.org/10.1038/nrd3800
Hestdal K, Ruscetti FW, Chizzonite R, Ortiz M, Gooya JM, Longo DL, Keller JR (1994) Interleukin-1 (IL-1) directly and indirectly promotes hematopoietic cell growth through type I IL-1 receptor. Blood 84(1):125–132
Morrissey P, Charrier K, Bressler L, Alpert A (1988) The influence of IL-1 treatment on the reconstitution of the hemopoietic and immune systems after sublethal radiation. J Immunol 140(12):4204–4210
Damia G, Komschlies KL, Futami H, Back T, Gruys ME, Longo DL, Keller JR, Ruscetti FW, Wiltrout RH (1992) Prevention of acute chemotherapy-induced death in mice by recombinant human interleukin 1: protection from hematological and nonhematological toxicities. Cancer Res 52(15):4082–4089
Smith MA, Knight SM, Maddison PJ, Smith JG (1992) Anaemia of chronic disease in rheumatoid arthritis: effect of the blunted response to erythropoietin and of interleukin 1 production by marrow macrophages. Ann Rheum Dis 51(6):753–757
Dinarello CA (2005) Blocking IL-1 in systemic inflammation. J Exp Med 201(9):1355–1359. https://doi.org/10.1084/jem.20050640
Cain D, Kondo M, Chen H, Kelsoe G (2009) Effects of acute and chronic inflammation on B-cell development and differentiation. J Invest Dermatol 129(2):266–277. https://doi.org/10.1038/jid.2008.286
Pietras EM, Mirantes-Barbeito C, Fong S, Loeffler D, Kovtonyuk LV, Zhang S, Lakshminarasimhan R, Chin CP, Techner JM, Will B, Nerlov C, Steidl U, Manz MG, Schroeder T, Passegue E (2016) Chronic interleukin-1 exposure drives haematopoietic stem cells towards precocious myeloid differentiation at the expense of self-renewal. Nat Cell Biol 18(6):607–618. https://doi.org/10.1038/ncb3346
Jovcic G, Ivanovic Z, Biljanovic-Paunovic L, Bugarski D, Stosic-Grujicic S, Milenkovic P (1996) The effect of IL-1 receptor antagonist on the proliferation of hematopoietic progenitor cells in regenerating bone marrow. Leukemia 10(3):564–569
Acknowledgements
This study was supported in part by a Grant-in-aid and the Private University Strategic Research Based Support Project from the Ministry of Education, Culture, Sports, Science, and Technology, Japan.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chiba, Y., Mizoguchi, I., Hasegawa, H. et al. Regulation of myelopoiesis by proinflammatory cytokines in infectious diseases. Cell. Mol. Life Sci. 75, 1363–1376 (2018). https://doi.org/10.1007/s00018-017-2724-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-017-2724-5