Abstract
MicroRNA (miR) are short non-coding RNA sequences of 19–24 nucleotides that regulate gene expression by binding to mRNA target sequences. The miR-29 family of miR (miR-29a, b-1, b-2 and c) is a key player in T-cell differentiation and effector function, with deficiency causing thymic involution and a more inflammatory T-cell profile. However, the relative roles of different miR-29 family members in these processes have not been dissected. We studied the immunological role of the individual members of the miR-29 family using mice deficient for miR-29a/b-1 or miR-29b-2/c in homeostasis and during collagen-induced arthritis. We found a definitive hierarchy of immunological function, with the strong phenotype of miR-29a-deficiency in thymic involution and T-cell activation being reduced or absent in miR-29c-deficient mice. Strikingly, despite elevating the Th1 and Th17 responses, loss of miR-29a conferred near-complete protection from collagen-induced arthritis (CIA), with profound defects in B-cell proliferation and antibody production. Our results identify the hierarchical structure of the miR-29 family in T-cell biology, and identify miR-29a in B cells as a potential therapeutic target in arthritis.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
MicroRNA (miR) are small non-coding RNAs that function as transcriptional modifiers by directly binding to mRNA target sequences, thereby destabilizing the mRNA and inhibiting protein synthesis [1]. Crucial roles in safeguarding the tolerogenic balance in the adaptive immune system, and thereby preventing autoimmunity, have been demonstrated for a number of different microRNAs, such as miR-146a, miR-17-92, miR-21, miR-155, and let-7a [2–6]; however, additional miR with functional roles in autoimmunity are likely to be identified.
The miR-29 family (miR-29a, miR-29b-1, miR-29b-2, and miR-29c) is a family of miR expressed in two genomic clusters: the miR-29a cluster (miR-29a/b-1) and the miR-29c cluster (miR-29b-2/c) [7]. Multiple immunological functions have been reported for the miR-29 family, including protective functions in age-related and infection-induced thymic involution [8], roles in T-cell differentiation, and inhibition of Th1 responses via suppression of T-bet, Eomes, and IFNγ mRNA [9–11] and lymphoid oncogenesis [12, 13], and a contribution to chronic inflammation in multiple sclerosis [11]. The role of the miR-29 family in B cells has been much less studied, with the exception of oncogenic transformation, where miR-29a over-expression promotes leukemia [12].
While multiple immunological functions of the miR-29 family have been defined, relatively little is known about the individual roles of the each cluster, with studies focusing on a single miR-29 family member or using pan-miR-29 blockade. While the seed sequences of each family member are identical, differing expression patterns and non-seed sequences can drive distinct functions for each family member, as recently characterized in the endocrinological context [14]. Here, we study the role of the individual clusters of the miR-29 family (miR-29a/b-1 and miR-29b-2/c) in T-cell development and collagen-induced arthritis (CIA). We find a subservient role for miR-29c in T-cell development, and a protective hierarchy of function in the CIA model, with miR-29a being dominant, revealing a critical function in the B-cell germinal center response.
Materials and methods
Mice
miR-29a/b-1 (miR-29a) and miR-29b-2/c (miR-29c) knockout mice were described previously [8, 14]. For thymic involution, suboptimal doses of 150 μg/mouse Poly(I:C) (Invivogen, CA, USA) [8], or control saline, were injected intraperitoneally on days 0 and 2, with thymic cellularity determined on day 3. Control mice received saline injections. To determine the germinal center response, mice (8–12 wks) were immunized i.p. with 2 × 109 SRBCs. Spleens were analyzed by flow cytometry 8 days after immunization.
Flow cytometry
Surface staining was performed in RPMI containing 2% fetal bovine serum and anti-mouse CD16/CD32 antibodies (from hybridoma supernatant generated in-house). The following antibodies were used in this study: CD11c (N418) (Biolegend), CD138 (281-2) and CD64 (X54-5/7.1.1), (BD-Pharmingen), and B220 (RA3-6B2), CD19 (eBio1D3), CD3 (145-2C11), CD4 (GK1.5 and RM4-5), CD95 (15A7), CXCR5 (SPRCL5), CD44 (IM7), CD62L (MEL-14), CD8α (53–6.7) FoxP3 (FJK-16s), IFNγ (XMG1.2), IgM (eB121-15F9 and II/41), IgD (11-26c), IL-17 (TC11-18H10), IL-4 (BVD6-24G2), PD-1 (J43), GL-7 (GL7), CD43 (eBioR2/60), Gr1 (RB6-8C5), CD11b (M1/70), CD86 (PO3.1), CD24 (M1/69), CD23 (B3B4), CD80 (16-10A1), CD21 (eBio8D9), MHCII (M5/114.15.2), Ly6C (HK1.4), PDCA-1 (eBio927), and CD31 (390) (eBioscience, CA, USA). Nuclear staining for Foxp3 was performed using the Foxp3 staining kit (eBioScience, CA, USA). Cytoplasmic intracellular staining for cytokines was performed following a 4-h stimulation with 50-ng/mL phorbol 12-myristate 13-acetate and 0.5-μg/mL ionomycin in the presence of GolgiStop (Monensin A, BD Biosciences, NJ, USA) using the Cytofix/Cytoperm kit (BD Biosciences, NJ, USA). Dead cell exclusion stain was performed using Zombie dyes (BioLegend, San Diego, CA, USA) according to the manufacturer’s instructions. Flow cytometric data were collected on a BD FACSCanto II Flow Cytometer (BD Biosciences) and analyzed using the FlowJo software (Treestar Inc., OR, USA).
Collagen-induced arthritis
CIA was induced as described in 6–10-week-old mice [15]. A total of 100 μL of chick type II collagen (CII, final concentration 1 mg/ml; Sigma, MO, USA) emulsified in complete Freund’s adjuvant containing 5-mg/ml heat-killed M. tuberculosis H37RA (BD Difco, NJ, USA) was injected intradermally in two sites at the base of the tail. The injection was repeated 21 days later. Animals were monitored every 2 days for erythema and swelling of limbs, and a clinical score (0–3) was given for each paw. At sacrifice, paws were taken and fixed in 4% neutral buffered paraformaldehyde solution and processed for X-ray analysis (Faxitron MX20 instrument, Faxitron Bioptics, AZ, USA) and histology. Serum was collected using serum tubes (Greiner, Vilvoorde, Belgium) and analyzed for anti-collagen antibodies, rheumatoid factor (RF), and IFNγ by ELISA.
Serum analysis
Serum IFNγ (eBioscience, CA, USA) was measured by ELISA according to the manufacturer’s recommendations. The anti-chick collagen II IgG ELISA was performed as described [16]. Rabbit-anti-mouse IgG coupled to horseradish peroxidase (HRP, Southern Biotech, IL, USA) was used as detection antibody. Standard curves were constructed from pooled sera of CII hyper-immunized DBA/1 mice, set at 100,000 units/mL.
Histology
Joints were fixed in 4% neutral buffered paraformaldehyde, decalcified in 5% formic acid, and embedded in paraffin. 7-μM sections were cut and stained with haematoxylin and eosin (H&E, Polysciences, PA, USA) or Safranin O (SafO, Sigma, MO, USA) according to the manufacturer’s recommendations. Inflammation, chondrocyte death, bone destruction, cartilage damage, and proteoglycan (PG) depletion were scored on a scale of 0–3 per feature by a researcher blinded to the experimental groups.
B- and T-cell stimulation in vitro
Total splenocytes were labeled with CFSE (0.25 μM; Molecular Probes) and plated in a 96-well plate at the concentration of 0.25 × 106 cells/well/100 μl for 4 days with the following stimulation: media alone, goat anti-mouse IgM F(ab)2 (20 μg/mL; Jackson Immunoresearch), LPS (10 μg/mL; Sigma-Aldrich), or phorbol myristate acetate (PMA, 50 ng/mL; Sigma-Aldrich) and ionomycin (250 ng/mL; Sigma-Aldrich). Cells were stained and analyzed by flow cytometry on day 4 as described above. Division index was defined as the average number of cell divisions.
Statistical analysis
Statistical significance was determined using the GraphPad Prism 6 software package (GraphPad software, CA, USA). Regular one-way or two-way ANOVA was used followed by Tukey’s or Sidak’s multiple comparisons tests to compare the different groups. Where only two groups were analyzed, the Mann–Whitney test was used. For statistical analysis of arthritis severity, the area under the curve for each individual mouse was determined, and compared to WT using two-way ANOVA. Significance for arthritis incidence was determined by survival curve analysis. P values < 0.05 were considered significant.
Results
Deficiency in miR-29c sensitizes the thymus for inappropriate involution
Our earlier studies showed that mice deficient for thymic expression of miR-29a/b-1 display aberrant thymic involution at an early age [8]. As miR-29b-2/c is also expressed in the thymic epithelium and has an identical seed sequence [8], we sought to determine whether spontaneous thymic involution was also observed following deficiency in the miR-29c locus. Naïve wild-type mice (WT), miR-29b-2/c heterozygous (miR-29c het), and miR-29b-2/c knockout (miR-29c KO) mice were assessed for thymic cellularity and T-cell populations at 9 weeks and at 20–23 weeks of age (Fig. 1a, b). Unlike mice deficient for the miR-29a/b-1 cluster (miR-29a KO mice) [8], the thymic cellularity of miR-29c KO mice was comparable to WT mice at both ages, with no sign of spontaneous involution. Notably, miR-29a heterozygous (miR-29a het) mice showed a partial phenotype, with reduced thymic cellularity in aged mice (Fig. 1b). Likewise, miR-29c KO mice showed no changes in the percentages of double negative (DN), double positive (DP), CD4 single positive (CD4SP), or CD8 single positive (CD8SP) cells (Fig. 1c), in DN subpopulations DN1-DN4 (Fig. 1d), or thymic Foxp3+CD4+ regulatory T cells (Treg, Fig. 1e). These results indicate that miR-29c is less important in thymic function than miR-29a, with no apparent spontaneous phenotype in the knockout.
Increased sensitivity to Poly(I:C)-induced thymic involution in miR-29c-deficient mice. Thymi from wild-type (WT), miR-29a het, miR-29a KO, and miR-29c KO mice were analyzed by flow cytometry in naïve mice (a–e) and in response to poly(I:C) treatment (f). a Thymic cellularity, 9-week-old mice (n = 10,10,7) and b 20–32-week-old mice. (n = 23, 22, 15, 13). c At 20–32 weeks of age, major thymic subsets, (n = 27, 20, 8, 17) and d B220−, double negative (DN) (CD3−CD4−CD8−) subpopulations (n = 27, 19, 14, 17). e Foxp3+ cells as percentage of CD4+ single positive (SP) lymphocytes (n = 21, 18, 13, 6, 14). f Poly(I:C)-induced thymic involution in WT, miR-29c het and miR-29c KO mice (n = 7, 10, 10, 7, 11, 12). Mean ± SEM, *p < 0.05, ***p ≤ 0.001, ****p ≤ 0.0001
miR-29a KO mice not only display spontaneous thymic involution, but are also hypersensitive to poly(I:C)-induced thymic involution [8]. Poly(I:C) injection reproduces the effect of pathogen-associated molecular pattern (PAMP) exposure, such as occurs during viral infection, leading to thymic involution [17]. While miR-29c KO mice did not show spontaneous thymic involution (Fig. 1b), we sought to determine whether a function of miR-29c would be revealed through challenging the thymus. To detect hypersensitivity, we injected suboptimal doses of poly(I:C) in the miR-29c KO mice, at a level which did not induce thymic involution in WT mice (Fig. 1f). Both miR-29c KO mice, and, to a lesser extent, miR-29c het mice exhibited thymic involution after challenge with suboptimal poly(I:C) levels. These results suggest a distinct hierarchy of importance for miR-29 family members in thymic involution, with miR-29a playing the dominant role in preventing inappropriate thymic involution (with both knockout and heterozygous presenting with spontaneous involution), while miR-29c has a subservient, but measurable, function, only revealed using sensitized screens.
miR-29a is the dominant miR-29 family member in peripheral lymphocytes
As the relative expression of miR-29 family members can vary during differentiation, we sought to extend the hierarchical comparison from the thymus to the periphery. Spleen and superficial lymph nodes (LN) of 20–32 week-old naïve WT, miR-29a het, miR-29a KO, miR-29c het and miR-29c KO mice were analyzed by flow cytometry to compare the function of miR-29 family members in peripheral lymphocyte populations. Splenic and lymph node cellularity which were twofold reduced in miR-29a KO mice, however, did not differ in miR-29c het or KO mice (Fig. 2a, b). In miR-29a KO mice, the number of CD4+ and CD8+ T cells in the spleen was not disturbed (Fig. 2c), but the relative contribution of effector-memory cells was increased at the expense of naïve cells (Fig. 2d, e), and the number of Foxp3+ Tregs was increased (Fig. 2f). As with the thymic phenotype, intermediate phenotypes were observed in heterozygous mice. By contrast, these changes were not observed in miR-29c KO mice (Fig. 2d–f). Similar effects were observed with cytokine production, with miR-29a-deficient mice having increased IFNγ and IL-17 production, while miR-29c-deficient mice remained normal (Fig. 2g–i). Together, these results indicate that the importance of the miR-29 family observed in peripheral T cells can be largely, if not exclusively, attributed to miR-29a, with no spontaneous phenotype observed with miR-29c deficiency.
Composition of T-cell subsets in the peripheral lymphoid organs is not dependent on miR-29b-2/c. T-cell subsets in spleen and superficial LN of 20–32-week-old naïve WT, miR-29a het, miR-29a KO, and miR-29c KO mice were analyzed by flow cytometry. a Spleen and b lymph node cellularity (n = 23, 22, 15, 9, 13). c Percentage of CD4+ and CD8+ T cells in the spleen. d Naïve, EM, and CM T cells within CD4+ and e CD8+ T cells in the spleen. f Foxp3+ regulatory T cells as a percentage of CD4+ T cells in the spleen (n = 27, 20, 14, 17). g IFNγ production by CD4+ and h CD8+ T cells after stimulation in vitro, and i IL-17 production by CD4+ T cells after stimulation in vitro (n = 26, 18, 16, 17). Mean ± SEM. *p < 0.05, **p ≤ 0.01, ***p ≤ 0.001, ****p ≤ 0.0001 compared to WT
A hierarchical role for the miR-29 family in autoimmune disease
Analysis of the immune system under homeostatic conditions identified miR-29a as having multiple potent functions, while deficiency in miR-29c, despite the identical seed sequence between the two family members, had no impact. However, these results do not preclude a more subtle phenotype from being revealed upon immunological challenge, such as during autoimmunity. We, therefore, sought to identify the roles of miR-29 family members in autoimmunity, using the model of CIA. Arthritis was induced by collagen immunization in WT, miR-29a het, miR-29a KO, and miR-29c KO mice. Mice were monitored for 45 days through macroscopic inspection of the paws 3 times weekly. Surprisingly, miR-29a KO mice were almost completely protected from CIA, with both the severity and incidence of CIA markedly reduced. Only 1 (out of 9) of the miR-29a KO mice was affected, and the pathology in this mouse was transient and limited to 1 digit (Fig. 3a, b). The miR-29a het and miR-29c KO mice displayed a reduction in severity, albeit not statistically different from the WT mice.
Loss of miR-29 protects from autoimmune pathology in collagen-induced arthritis. Collagen-induced arthritis (CIA) was induced in 12–14 week old WT, miR-29a het, miR-29a KO, and miR-29c KO mice. Arthritis was scored three times weekly until sacrifice on day 45, when serum and paws were taken for downstream analysis. a Macroscopic score of paws (arthritic mice shown only, cumulative scores of 0–3 per paw, n = 13, 10, 9, 8). b Incidence of arthritis for each genotype. c Representative photos of X-ray analysis, H&E stain, and Safranin O stain of the ankle joints for each group. Scale bar = 1 mm. d Pooled X-ray scores of for each group (maximum score per mouse = 8, n = 11, 10, 9, 8). e Detailed histological scores of the ankle joints (maximum score per feature = 3, n = 22, 20, 18, 16 joints per group). f Total histological scores per mouse (n = 11, 10, 9, 8). Mean ± SEM. *p < 0.05, **p ≤ 0.01, ****p ≤ 0.0001
The resistance to CIA observed in miR-29a-deficient mice at the macroscopic level was also observed at the anatomical and histological levels. Ankle joints were visualized by X-ray to determine the extent of bone damage and joint morphology. Damage was apparent in the small joints of the ankle and foot of the WT mice, while very little damage was apparent in miR-29a KO mice (Fig. 3c). Again, an intermediate phenotype was observed for miR-29a het and miR-29c KO mice, although the pooled X-ray scores were not significantly different between groups (Fig. 3d). Additional features of joint pathology were scored on H&E and SafO stained paraffin sections of the large ankle joints. For all features scored (inflammation, chondrocyte death, cartilage damage, proteoglycan depletion, and bone damage), miR-29a KO mice had significantly less severe lesions, or complete absence of pathology (Fig. 3c, e). miR-29a het and miR-29c KO mice also had reduced pathology for all features scored, although only the inflammatory infiltrate in the miR-29a het mice was significantly different from the WT. These results were reflected in the overall histological scores (Fig. 3f). Reduced pathology in miR-29a-deficient mice was accompanied by a poor antibody response to the immunization with collagen, as measured by serum antibody levels of anti-chick and anti-mouse type II collagen (CII) antibodies (Fig. 4a, b), while rheumatoid factor (RF) remained normal (Fig. 4c). Despite increased production of IFNγ by miR-29a KO CD4+ and CD8+ T cells (Fig. 2g, h), IFNγ levels in the serum were not increased during CIA (Fig. 4d), and therefore, protection against CIA cannot be explained by over-expression of IFNγ [18, 19]. Together, these results suggest that miR-29a is essential to suppress inflammatory cytokines, but also to mount an appropriate immunization response. In contrast, miR-29c only had minor or no effects on these biological processes, despite being expressed in the same cell types and sharing the seed sequence with miR-29a.
Reduced production of germinal center B cells in miR-29a KO mice
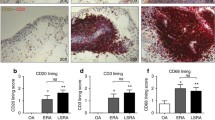
The resistance against arthritis development in the miR-29a KO mice may be a direct result of a reduced immunization response caused by altered B-cell populations or activation. We analyzed the B-cell compartment in the bone marrow (BM), and analyzed both the B-cell compartment and DC populations in the spleens of naïve miR-29a KO mice (Fig. 5). In the BM, we found no difference in B-cell numbers or populations (data not shown). However, although the percentage of B cells in the spleen of naïve miR-29a KO mice was increased (Fig. 5b), the absolute number of B cells was within the normal range (Fig. 5c). There was no difference in the B-cell subsets mature (M), transitional (T1 and T2), marginal zone (MZ), and marginal zone progenitors (MZP) between the WT and miR-29a KO mice (Fig. 5d–f); however, the expression of co-stimulatory molecule CD86 on total B cells, T1/T2, and MZ/MZP was markedly reduced in the miR-29a KO mice, indicative of reduced activation (Fig. 5g–i). An intrinsic defect in miR-29a KO B cells in response to stimulation was confirmed in vitro by stimulation of B cells using IgM and LPS (Fig. 5j, k). Fewer miR-29a KO B cells divided upon stimulation, and those that divided reached a lower number of divisions after 4 days compared to the WT B cells (Fig. 5k). In contrast, this defect was not observed in T cells stimulated with PMA/ionomycin in the same assay (Fig. 5l). As the immunization response also involves DC, we analyzed different DC populations in the spleen of naïve miR-29a KO mice (Fig. 5m, n). We found reduced conventional DC (cDC, Fig. 5m), and in addition a minor reduction of CD80+ cDC (Fig. 5n). These data indicate that, indeed, the miR-29a KO B cells are impaired in activation and proliferation in vitro.
Altered B-cell numbers and activation and reduced DC activation in miR-29a KO mice. Spleens from 6- to 12-week-old naïve WT and miR-29a KO mice (4,4) were analyzed either directly ex-vivo (a–i, m,n) or after stimulation with IgM or LPS in vitro (j–l) by flowcytometry for B-cell and DC subsets and activation markers. a Gating strategy for B-cell populations, b percentage B220+ cells of total splenocytes, c absolute number of B220+ cells in the spleen, d–f B-cell subsets mature, transitional ½, and marginal zone/marginal zone progenitors as % of total B220+ cells, and g–i expression of CD86 on B-cell subsets. j–l Splenocytes were labeled with CFSE and B cells were assessed for proliferation after 4 days of culture. j Representative CFSE histograms of B cells from WT and miR-29a KO mice after stimulation with IgM (filled histograms) or media alone (clear histograms), k division index of B cells after 4 days of IgM or LPS stimulation, l division index of CD4+ and CD8+ T cells after 3-day stimulation with PMA/ionomycin, m pDC and cDC populations in the spleen, and n surface markers of splenic cDC. Mean ± SEM. *p < 0.05
To directly evaluate germinal center populations in vivo, we analyzed the B- and T-cell populations in the spleen after immunization with sheep red blood cells (SRBC, Fig. 6a–c). Following the immunization, miR-29a KO mice had normal CD4+ T-cell responses (Fig. 6d), but with an over-representation of Foxp3+ Treg (Fig. 6e), as previously shown for unimmunized mice (Fig. 2). The T-cell response of miR-29a KO mice to immunization was within the normal range, with normal production of follicular helper T cells (Tfh) (Fig. 6f), coupled with a non-significant increase in follicular regulatory T cells (Tfr), paralleling the increased Treg number (Fig. 6g). Despite the normal follicular T-cell response, germinal center B-cell (GCB) formation was sharply impaired (Fig. 6h), although plasmablasts were not significantly altered (Fig. 6i). Together, these results indicate that miR-29a KO mice have an innate defect in B-cell activation and germinal center production. In the context of an arthritic response, this B-cell defect may account for the reduced autoantibody production and autoimmune pathology manifested by KO mice.
Loss of miR-29a leads to a reduction in germinal center B cells. 6–12-week-old WT, miR-29a het and miR-29a KO mice (n = 7, 2, 4) were immunized with SRBC, and 8 days later, cell populations in the spleen were analyzed by flow cytometry. a Immunization strategy, and b gating strategy for Tfh and Tfr and c GC B cells and plasma cells. d Splenic CD4+ T cells, e splenic Foxp3+ Treg, f Tfh, g Tfr, i GCB, and h plasmablasts 8 days after immunization. Mean ± SEM. *p < 0.05, **p ≤ 0.01
Discussion
The high expression of miR-29 family members in the immune system and the relative enrichment of immunological genes among predicted targets [7] have led to a detailed search for immunological function. The key functions identified for the miR-29 family in the immune system include preservation of thymic tissue during development [8], restraining polarization of T cells towards the Th1 lineage [9] and promoting B-cell oncogenesis [12]. However, these studies have mostly relied on research tools that either specifically target the miR-29a/b-1 cluster [8, 12, 20] or do not differentiate between family members (such as expression of a miR-29 “sponge” [10] or reconstitution studies which negate the differentiation expression patterns [9]). This research design has led to a paucity of information about the relative contribution of the miR-29b-2/c cluster on these same immunological processes.
In this study, by directly comparing deficiency in the two miR-29 clusters, we were able to establish a distinct functional hierarchy. For the known functions of miR-29a in T-cell biology, the functional consequences of miR-29c-deficiency were minor or not detected. Thus, no spontaneous thymic involution was observed for miR-29c-deficient mice, and no elevation of Th1 polarization was detected in the periphery. However, there were indications that the same biological processes are controlled by both miR-29a and miR-29c, as the miR-29c KO mice were sensitive to developing parallel phenotypes upon induction, even if they did not exhibit them spontaneously under homeostatic conditions. These studies even allow a rough baseline of the relative importance of miR-29a and miR-29c clusters to be estimated, as the miR-29c KO was similar, or slightly weaker, than the miR-29a heterozygous mouse. Intriguingly, this same hierarchy and relative importance were observed in a recent analysis of miR-29a and miR-29c clusters in glucose handling [14], despite the processes being controlled by different molecular circuits in different organs. It is tempting to speculate that miR-29a is the primary cluster of the miR-29 family, with miR-29c existing only to boost overall expression levels to avoid the early lethality of complete miR-29 deficiency [14]; however, it is also possible that the hierarchy observed in the immune and endocrine systems may be inverted in other tissues or processes.
The protective effect of miR-29a-deficiency on CIA is counter-intuitive when considering the pro-inflammatory impact, this deficiency has on T cells [9]. A complementary result was observed in Experimental Autoimmune Encephalomyelitis, the mouse model of Multiple Sclerosis [11], which together suggests that miR-29a-deficient T cells, while showing enhanced polarization towards inflammatory lineages, are incapable of promoting effective pathogenic reactions. However, as with other miR, it needs to be considered that miR-29a has a broad expression beyond T cells, and the CIA model is driven by a complex interaction of multiple cell types. Both T cells and B cells are important for disease development, and the local tissue and resident immune cells also shape the nature of the response [15]. Mechanistic dissection of the B-cell compartment led to observations compatible with this model; namely defects in B-cell proliferation, germinal center differentiation, and antibody production.
Thus, it is possible that the function of miR-29a is pro-pathogenic in the T-cell context, but strongly anti-pathogenic in the B-cell context, leading to a net effect of a global knockout of miR-29a which is anti-pathogenic. We note, however, that the arthritic reaction is highly complex, and a role for other cell types cannot be excluded at this stage, including the potential for defective costimulation by B cells and DCs. In this regard, assessment of the arthritic potential of miR-29a using other models (such as B-cell-specific over-expression of miR-29a [12], or using T-cell transfer models with wild-type T cells into miR-29a-deficient hosts) may shed light on the potential utility of miR-29a inhibition as an anti-arthritic treatment.
Abbreviations
- CIA:
-
Collagen-induced arthritis
- CII:
-
Type II collagen
- CFA:
-
Complete Freund’s adjuvant
- DC:
-
Dendritic cell
- GC:
-
Germinal center
- Het:
-
Heterozygous
- HRP:
-
Horseradish peroxidase
- H&E:
-
Haematoxylin and eosin
- IFN:
-
Interferon
- IL:
-
Interleukin
- KO:
-
Knockout
- miR:
-
MicroRNA
- PG:
-
Proteoglycan
- PMA:
-
Phorbol myristate acetate
- RF:
-
Rheumatoid factor
- SafO:
-
Safranin O
- SRBC:
-
Sheep red blood cells
- Teff:
-
Effector T cell
- Th:
-
T helper cell
- Tfh:
-
T follicular helper cell
- Tfr:
-
T follicular regulatory cell
- Tn:
-
Naïve T cell
- Treg:
-
Regulatory T cell
- WT:
-
Wildtype
References
Ambros V (2004) The functions of animal microRNAs. Nature 431:350–355
Boldin MP, Taganov KD, Rao DS, Yang L, Zhao JL, Kalwani M, Garcia-Flores Y, Luong M, Devrekanli A, Xu J, Sun G, Tay J, Linsley PS, Baltimore D (2011) miR-146a is a significant brake on autoimmunity, myeloproliferation, and cancer in mice. J Exp Med 208:1189–1201
Xiao C, Srinivasan L, Calado DP, Patterson HC, Zhang B, Wang J, Henderson JM, Kutok JL, Rajewsky K (2008) Lymphoproliferative disease and autoimmunity in mice with increased miR-17-92 expression in lymphocytes. Nat Immunol 9:405–414
Garchow B, Kiriakidou M (2016) MicroRNA-21 deficiency protects from lupus-like autoimmunity in the chronic graft-versus-host disease model of systemic lupus erythematosus. Clin Immunol 162:100–106
Kurowska-Stolarska M, Alivernini S, Ballantine LE, Asquith DL, Millar NL, Gilchrist DS, Reilly J, Ierna M, Fraser AR, Stolarski B, McSharry C, Hueber AJ, Baxter D, Hunter J, Gay S, Liew FY, McInnes IB (2011) MicroRNA-155 as a proinflammatory regulator in clinical and experimental arthritis. Proc Natl Acad Sci USA 108:11193–11198
Guan H, Fan D, Mrelashvili D, Hao H, Singh NP, Singh UP, Nagarkatti PS, Nagarkatti M (2013) MicroRNA let-7e is associated with the pathogenesis of experimental autoimmune encephalomyelitis. Eur J Immunol 43:104–114
Liston A, Papadopoulou AS, Danso-Abeam D, Dooley J (2012) MicroRNA-29 in the adaptive immune system: setting the threshold. Cell Mol Life Sci 69:3533–3541
Papadopoulou AS, Dooley J, Linterman MA, Pierson W, Ucar O, Kyewski B, Zuklys S, Hollander GA, Matthys P, gray DHD, De Strooper B, Liston A (2012) The thymic epithelial microRNA network elevates the threshold for infection-associated thymic involution via miR-29a mediated suppression of the IFN-α receptor. Nat Immunol 13:181–187
Steiner DF, Thomas MF, Hu JK, Yang Z, Babiarz JE, Allen CDC, Matloubian M, Blelloch R, Ansel KM (2011) MicroRNA-29 regulates T-box transcription factors and interferon-γ production in helper T cells. Immunity 35:169–181
Ma F, Xu S, Liu X, Zhang Q, Xu X, Liu M, Hua M, Li N, Yao H, Cao X (2011) The microRNA miR-29 controls innate and adaptive immune responses to intracellular bacterial infection by targeting interferon-γ. Nat Immunol 12:861–869
Smith KM, Guerau-de-Arellano M, Costinean S, Williams JL, Bottoni A, Mavrikis Cox G, Satoskar AR, Croce CM, Racke MK, Lovett-Racke AE, Whitacre CC (2012) miR-29ab1 deficiency identifies a negative feedback loop controlling Th1 bias that is dysregulated in multiple sclerosis. J Immunol 189:1567–1576
Santanam U, Zanesi N, Efanov A, Costinean S, Palamarchuk A, Hagan JP, Volinia S, Alder H, Rassenti L, Kipps T, Croce CM, Pekarsky Y (2010) Chronic lymphocytic leukemia modeled in mouse by targeted miR-29 expression. Proc Natl Acad Sci USA 107:12210–12215
Kincaid RP, Burke JM, Sullivan CS (2012) RNA virus microRNA that mimics a B-cell oncomiR. Proc Natl Acad Sci USA 109:3077–3082
Dooley J, Garcia-Perez JE, Sreenivasan J, Schlenner SM, Vangoitsenhoven R, Papadopoulou AS, Tian L, Schonefeldt S, Serneels L, Deroose C, Staats KA, Van der Schueren B, De Strooper B, McGuinness OP, Mathieu C, Liston A (2016) The microRNA-29 family dictates the balance between homeostatic and pathological glucose handling in diabetes and obesity. Diabetes 65:53–61
Campbell IK, Hamilton JA, Wicks IP (2000) Collagen-induced arthritis in C57BL/6 (H-2b) mice: new insights into an important disease model of rheumatoid arthritis. Eur J Immunol 30:1568–1575
Campbell IK, Rich MJ, Bischof RJ, Dunn AR, Grail D, Hamilton JA (1998) Protection from collagen-induced arthritis in granulocyte-macrophage colony-stimulating factor-deficient mice. J Immunol 161:3639–3644
Anz D, Thaler R, Stephan N, Waibler Z, Trauscheid MJ, Scholz C, Kalinke U, Barchet W, Endres S, Bourquin C (2009) Activation of melanoma differentiation-associated gene 5 causes rapid involution of the thymus. J Immunol 182:6044–6050
Kelchtermans H, Billiau A, Matthys P (2008) How interferon-gamma keeps autoimmune diseases in check. Trends Immunol 29:479–486
Lee J, Lee J, Park M-K, Lim M-A, Park E-M, Kim E-K, Yang E-J, Lee S-Y, Jhun J-Y, Park S-H, Kim H-Y, Cho M-L (2013) Interferon gamma suppresses collagen-induced arthritis by regulation of Th17 through the induction of indoleamine-2,3-deoxygenase. PLoS One 8:e60900
Braconi C, Kogure T, Valeri N, Huang N, Nuovo G, Costinean S, Negrini M, Miotto E, Croce CM, Patel T (2011) microRNA-29 can regulate expression of the long non-coding RNA gene MEG3 in hepatocellular cancer. Oncogene 30:4750–4756
Acknowledgements
The authors wish to thank Josselyn E. Garcia-Perez, Denise Klatt, Birgitte Walgreen, Monique Helsen, and Alessio Zuppelli for help with experiments, Susann Schönefeldt and Jeason Haughton for help with mouse breeding, and the Leuven University Animalium staff for animal husbandry. This work was supported by the Flemish Institute for Biotechnology (VIB), the Belgian Science Policy Office Interuniversity Attraction Poles program (T-TIME) and the Fonds Wetenschappelijk Onderzoek (FWO) Flanders. AvN was supported by the Leuven University F + fellowship, SMS and SH-B were supported by FWO fellowships.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
All experiments were approved by the Animal Ethics Committee of the University of Leuven.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
A. van Nieuwenhuijze and J. Dooley contributed equally.
Rights and permissions
About this article
Cite this article
van Nieuwenhuijze, A., Dooley, J., Humblet-Baron, S. et al. Defective germinal center B-cell response and reduced arthritic pathology in microRNA-29a-deficient mice. Cell. Mol. Life Sci. 74, 2095–2106 (2017). https://doi.org/10.1007/s00018-017-2456-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-017-2456-6