Abstract
The protective effect of high density lipoproteins (HDL) against atherosclerosis is mainly attributed to their capacity to transport excess cholesterol from peripheral tissues back to the liver for further elimination into the bile, a process called reverse cholesterol transport (RCT). Recently, the importance of the P2Y13 receptor (P2Y13-R) was highlighted in HDL metabolism since HDL uptake by the liver was decreased in P2Y13-R deficient mice, which translated into impaired RCT. Here, we investigated for the first time the molecular mechanisms regulating cell surface expression of P2Y13-R. When transiently expressed, P2Y13-R was mainly detected in the endoplasmic reticulum (ER) and strongly subjected to proteasome degradation while its homologous P2Y12 receptor (P2Y12-R) was efficiently targeted to the plasma membrane. We observed an inverse correlation between cell surface expression and ubiquitination level of P2Y13-R in the ER, suggesting a close link between ubiquitination of P2Y13-R and its efficient targeting to the plasma membrane. The C-terminus tail exchange between P2Y13-R and P2Y12-R strongly restored plasma membrane expression of P2Y13-R, suggesting the involvement of the intra-cytoplasmic tail of P2Y13-R in expression defect. Accordingly, proteasomal inhibition increased plasma membrane expression of functionally active P2Y13-R in hepatocytes, and consequently stimulated P2Y13-R-mediated HDL endocytosis. Importantly, proteasomal inhibition strongly potentiated HDL hepatic uptake (>200 %) in wild-type but not in P2Y13-R-deficient mice, thus reinforcing the role of P2Y13-R expression in regulating HDL metabolism. Therefore, specific inhibition of the ubiquitin–proteasome system might be a novel powerful HDL therapy to enhance P2Y13-R expression and consequently promote the overall RCT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Several prospective studies have established that the plasma level of high density lipoprotein (HDL) cholesterol (HDL-C) is an independent negative risk factor for coronary heart diseases and thus represents a major protective factor against atherosclerosis. HDL exert direct vasculo-protective functions through their anti-inflammatory, anti-oxidant, anti-thrombotic and cyto-protective properties, but their main atheroprotective action is attributed to their metabolic role in reverse cholesterol transport (RCT), a process whereby excess cell cholesterol is taken up from peripheral cells (cholesterol efflux), processed into HDL particles, and then later delivered to the liver (cholesterol uptake) for further metabolism and bile excretion. Reverse cholesterol transport relies on specific interactions between HDL particles and both peripheral cells and hepatocytes. Among cellular proteins interacting with HDL, some contribute to the cholesterol efflux such as cellular ATP binding cassette transporters ABCA1 and ABCG1 [1], whereas others are involved in hepatic HDL cholesterol uptake. To date, two distinct cell surface receptors are known to contribute to HDL uptake by the liver: (1) the scavenger receptor class B type I (SR-BI) that is involved in selective uptake of cholesterol ester from HDL [2], and (2) the membrane-associated ecto-F1-ATPase identified as a high affinity receptor for the major protein component of HDL, apolipoprotein A-I (apoA-I), and involved in the uptake of both protein and lipid moieties of the HDL particles, a process called HDL holoparticle endocytosis [3]. Basically, apoA-I binds the ecto-F1-ATPase at the cell surface of hepatocytes, promoting ATP hydrolysis into ADP which in turn leads to subsequent activation of a G-protein coupled receptor (GPCR)—namely P2Y13 receptor (P2Y13-R). P2Y13-R activation leads to a Rho/ROCKI signaling pathway and actin cytoskeleton reorganization that eventually stimulate HDL holoparticle endocytosis through an unknown low affinity receptor that is different from SR-BI [3–5].
We and others recently highlighted the physiological importance of P2Y13-R in vivo since RCT was impaired in mice deficient for P2Y13-R [6, 7]. Conversely, in vivo P2Y13-R activation by bolus injection of its partial agonist Cangrelor (AR-C69931MX) increased biliary lipid secretions in wild-type but not P2Y13-R knock-out mice [6]. Similarly, chronic pharmacological activation of P2Y13-R by Cangrelor in mice increased hepatic HDL uptake and bile acid secretion [8]. Thus, P2Y13-R appears as a promising pharmacological target in the field of emergent HDL therapies aiming at modulating RCT and treating/preventing the development of atherosclerosis. Interestingly, nowadays, an important concept is that increasing HDL-C levels may not necessarily be the optimal target for the development of new therapies targeted toward HDL, because the protective ability of HDL may be more related to cholesterol elimination through the RCT pathway. Thus, some new therapeutic approaches are now focusing on promoting RCT, without necessarily raising HDL-C levels per se, supporting the notion that the function of HDL is more important than its concentration. Therefore, therapies that improve HDL “function”, even if they do not increase HDL-C levels, may have important anti-atherogenic and vascular protective effects. With this in mind, we hypothesized that enhancing P2Y13-R expression at the cell surface of hepatocytes could be highly relevant to increasing HDL hepatic uptake and consequently promoting RCT and cholesterol elimination.
P2Y13-R belongs to the GPCR family and shares a high homology sequence with P2Y12 receptor (P2Y12-R), another ADP receptor, as well as similar functional features such as Gαi protein coupling [9]. In addition to cholesterol metabolism, P2Y13-R has also been implicated in other physiological processes, including neuronal differentiation [10], insulin secretion [11], mast cell degranulation [12], ATP release by red blood cells [13], or bone homeostasis [14]. However, so far, the molecular mechanisms that regulate trafficking and cell surface expression of P2Y13-R have not been investigated.
In this study, we investigated for the first time the regulation of cell surface expression of P2Y13-R. To our surprise, we found that P2Y13-R exhibited poor general protein expression as well as poor cell surface expression in different cell types when compared to P2Y12-R. Interestingly, we demonstrated that P2Y13-R was subjected to a constitutive ubiquitination in the endoplasmic reticulum (ER), thus promoting proteasome-mediated receptor degradation, and thereby preventing its expression at the plasma membrane. Finally, we also demonstrated that proteasomal inhibition, which drastically increased cell surface expression of P2Y13-R in HepG2 cells, greatly potentiated P2Y13-R-mediated hepatic HDL endocytosis in vivo, thus giving promising applications for future improvements for HDL therapies.
Materials and methods
Constructs and reagents
P2Y13 (NCBI Reference Sequence: NM_176894), P2Y12 (NCBI Reference Sequence: NM_022788) and chimerical receptors were amplified by PCR and subcloned into pEGFP-N1, pRLuc8-N1 or fused myc epitope. P2Y12 cDNA was a generous gift from C. Gachet (UMR-S949 INSERM, Strasbourg, France) and Ub-GFP2 construct was a generous gift from M. Bouvier (University of Montréal, Montréal, Canada). MG-132 was purchased from Sigma (St. Louis, MO, USA) and bortezomib from Sequoia Research Products (Berkshire, UK).
Cell culture and transfection
HeLa cells (human cervix adenocarcinoma), HepG2 cells (human liver hepatocellular carninoma) and HEK293T cells (human embryonic kidney) were maintained in DMEM Glutamax (Sigma) supplemented with 10 % fetal bovine serum (Life Technologies) and 100 μg/mL penicillin/streptomycin in a humidified atmosphere containing 5 % CO2. HepG2 cells were grown on collagen I-coated dishes. Transient transfections were performed using X-tremeGENE 9 DNA Transfection Reagent (Roche Applied Science) for HeLa and HepG2 cells and using polyethylenimine (PEI, Polysciences) for HEK293T cells.
Quantification of cell surface receptors by ELISA
Cells were split into 24-well plates and transiently transfected with pcDNA3.1 (+) (control) or vectors encoding N-terminally myc-tagged receptors. Twenty-four hours post-transfection, cells were treated or not with proteasome inhibitors as indicated for 16 h at 37 °C. The,n cells were fixed in 4 % paraformaldehyde, saturated with PBS containing 1 % bovine serum albumin and incubated with the primary anti-myc antibody (Clone 9E10; Santa Cruz Biotechnology) and then with HRP-labeled secondary antibody (Sigma). After washing, cells were incubated with HRP substrate: TMB (3,39,5,59-tetramethylbenzidine). The reaction was stopped with HCl 1 N, and the plates were read at 450 nm in a microplate reader (Varioscan Flash, Thermo Electron). The 570- nm optic density (background) was subtracted.
Microscopy
Cells were fixed in 4 % paraformaldehyde, permeabilized with 0.05 % saponin when necessary, saturated with PBS containing 10 % fetal bovine serum and incubated with the primary antibody and then with Cy3-labeled secondary antibody (Jackson Immunoresearch Laboratories). Pictures were captured using a Zeiss LSM 710 META confocal microscope equipped with a ×63 Plan-Apochromat objective.
Western blot
For protein analysis, cell lysates (50 μg) were subjected to SDS-PAGE electrophoresis under reducing conditions, transferred onto PVDF membranes (Millipore), and analyzed by immunoblotting according to standard protocols using indicated antibodies. We used a mouse monoclonal antibody against Myc (clone 9E10) from BD Biosciences, and a mouse monoclonal antibody against GAPDH from Santa Cruz Biotechnology. HRP-labeled secondary antibodies were from Sigma.
Cell fractionation
Cell fractionation was performed as previously described [15]. Briefly, cells were washed with cold PBS, scraped off, and lysed with cold hypotonic lysis buffer (20 mM HEPES, pH 7.4; 2 mM EDTA; 2 mM EGTA; 6 mM magnesium chloride) containing protease inhibitors. After homogenization using a tight-fitting dounce, and removal of cellular debris and unlysed cells by centrifugation, the supernatant was adjusted to a final concentration of 0.2 M sucrose. A discontinuous sucrose step gradient was made using lysis buffer. Cell lysate was applied to the top of discontinuous sucrose step gradient (0.5, 0.9, 1.2, 1.35, 1.5, and 2 M) and centrifuged for 16 h at 130,000g. Fractions were then subjected to fluorescence/luminescence analysis and to BRET measurements.
Bioluminescence resonance energy transfer measurement
Constructs encoding RLuc8-fused receptors and GFP2-tagged ubiquitin were transiently cotransfected into HEK293T cells as indicated in the figure legends. Forty-eight hours after transfection, cells were washed with PBS and resuspended in PBS containing 0.1 % (w/v) glucose at room temperature. Cells were then distributed (80 μg of proteins per well) in a 96-well microplate (Wallac, PerkinElmer Life and Analytical Sciences). BRET2 between RLuc8 and GFP2 was measured after the addition of the RLuc8 substrate coelenterazine 400a (5 μM, Interchim). BRET2 readings were collected using a modified Infinite F500 (Tecan). The BRET signal was calculated by the ratio of emission of GFP2 (510–540 nm) to RLuc8 (BRET2, 370–450 nm).
Fluorescent HDL endocytosis
HDL were fluorescently labeled with Alexa Fluor® 568 dye according the instructions of manufacturer (Life technologies). Then, 100 μg/mL Alexa Fluor® 568-HDL particles were endocytosed for 15 min at 37 °C in HepG2 cells. Cells were washed 3 times in serum-free DMEM, and then dissociation of extracellular membrane-bound HDL was performed at 4 °C in serum-free DMEM for 90 min. Following washes, cells were fixed using 4 % paraformaldehyde and examined using an Olympus IX81 microscope. Quantification was done using Image J software.
Perfused mouse liver experiments
C57BL/6 wild-type mice and P2Y13-R−/− littermates were used in this study, as previously described [6]. Mice were caged in animal rooms with alternating 12 h periods of light (0700–1900 hours) and dark (1900–0700 hours) and fed ad libitum with a normal mouse chow diet (# R04-10; SAFE, France). All animal procedures were performed in accordance with the guidelines of the Committee on Animals of the Midi-Pyrénées Ethics Committee on Animal Experimentation and with the French Ministry of Agriculture license. For experiments, mice (10–12 weeks old) were treated twice at a 5-day interval with 0.5 mg/kg of bortezomib or the vehicle (PBS) by subcutaneous injection. Five days after the second injection, mice were anesthetized by intraperitoneal injection of ketamine hydrochloride and xylazine hydrochloride. The liver was perfused in situ for 10 min at 37 °C with PBS (Invitrogen) containing 50 μg proteins/mL of 125I-HDL3 (specific radioactivities ranged from 1,000 to 1,500 cpm/ng of proteins). Livers were extensively washed at 4 °C in PBS and radioactivity associated with the liver was counted (n ≥ 6 per group).
Results
P2Y13 receptor is poorly expressed and does not exhibit cell surface expression
To investigate cell surface expression of P2Y13-R, we first tagged the receptor with a myc epitope in N-terminus extracellular region (Myc-P2Y13) and transiently expressed the construct in HeLa cells. Surprisingly, Myc-P2Y13 was detected at very low levels and in only a few cells (Fig. 1a). Interestingly, when detected, Myc-P2Y13 receptor was rarely found at the plasma membrane and mostly localized in the endoplasmic reticulum (ER) as shown by the colocalization with DsRed2-ER marker (Fig. 1b). By contrast, when overexpressed, Myc-P2Y12 receptor, another ADP receptor, was strongly detected in almost all the cells and exhibited efficient plasma membrane targeting (Fig. 1a).
P2Y13 receptor is poorly expressed and does not exhibit cell surface expression. a HeLa cells expressing N-terminally Myc-tagged P2Y13 or P2Y12 were processed for immunofluorescence using an anti-myc antibody. Nuclei were stained with 5 μg/mL DAPI. Scale bar 10 μm. b HeLa cells co-expressing Myc-P2Y13 and the ER marker, DsRed2-ER, were processed for immunofluorescence using an anti-myc antibody. Nuclei were stained with 5 μg/mL DAPI. Scale bar 10 μm. c HEK293T cells were transfected with identical amounts of DNA constructs encoding RLuc8-tagged receptors and luciferase intensity was measured 48 h after transfection. Results are expressed as the mean ± SEM of at least three independent experiments and analyzed by paired t test (***p < 0.001). d HeLa cells expressing Myc-tagged P2Y13 or P2Y12 were analyzed by ELISA using an anti-myc antibody to quantify cell surface expression of the different receptors. Results are expressed as the mean of at least three independent experiments and analyzed by paired t test (***p < 0.001). Standard errors are indicated. e HeLa cells were transfected with increasing amounts of vectors encoding N-terminally Myc-tagged P2Y13 or P2Y12 (ranging from 15 to 500 ng/well). Then, cell surface expression of the different receptors was analyzed by ELISA using an anti-myc antibody. Results are expressed as the mean of at least three independent experiments. Standard errors are indicated
We further confirmed these observations by precisely quantifying total expression of each receptor as well as receptor density at the plasma membrane. For that purpose, we fused P2Y13 or P2Y12 receptors either with a Renilla luciferase tag (RLuc8) in their C-terminus region or with a myc epitope in N-terminus extracellular region as mentioned above. After transfection of identical amounts of the different receptor-encoding vectors, luciferase luminescence was measured as an indicator of total receptor expression (Fig. 1c) while cell surface density of myc-tagged receptors was classically determined by ELISA and revealed with an anti-myc antibody on non-permeabilized cells (Fig. 1d). In agreement with fluorescence imaging experiments, the results showed a huge difference in receptor expression levels between P2Y13 and P2Y12 receptors. Indeed, P2Y13-R was poorly expressed (Fig. 1c), and almost not detected at the plasma membrane (Fig. 1d) compared to P2Y12-R. To rule out any variations in transfection efficiency between vectors encoding P2Y13 and P2Y12 receptors which could in part support receptor expression differences, we quantified cell surface expression of both P2Y12 and P2Y13 receptors following transfection of increasing amounts of each encoding vector (Fig. 1e). While detection of P2Y12-R was increased with increasing amounts of encoding vector until reaching a plateau, P2Y13-R was still undetectable, even after transfection with the highest amount of encoding vector (Fig. 1e). Similar results were obtained when the two P2Y receptors were expressed in other cell lines, including HepG2 cells, indicating that the regulation of P2Y13-R expression did not depend on the cell type (Supplementary Fig. S1).
Altogether, these data demonstrate that P2Y13-R is poorly expressed, and mostly retained in the ER.
P2Y13 receptor expression is regulated through its C-terminal tail
P2Y13-R displays high homology sequence with P2Y12-R, especially in transmembrane domains, and alignment between P2Y13-R and P2Y12-R amino acid sequences reveals that both receptors share ~50 % identity and ~70 % homology. The highest variability is found in the C-terminus cytoplasmic tail, which is known to regulate GPCR trafficking and expression (Fig. 2a). To evaluate the influence of the C-terminus tail of P2Y13-R in cell surface expression of this receptor, we constructed two chimeric receptors consisting of the exchange of the C-terminus tail of P2Y13 and P2Y12 between the two receptors, namely P2Y13-12 (P2Y13-R core domain containing the C-terminus tail of P2Y12-R) and P2Y12-13 (P2Y12-R core domain containing the C-terminus tail of P2Y13-R) (Fig. 2b). Wild-type and chimeric receptors were C-terminally fused to GFP or RLuc8 and next transiently expressed in HeLa cells to investigate expression levels of the receptors. Strikingly, the replacement of the C-terminus tail of P2Y13-R by the one of P2Y12-R strongly increased general expression of P2Y13-R (Fig. 2c, d) and restored its cell surface expression (Fig. 2c), suggesting that the cytoplasmic tail of P2Y13-R was involved in the specific expression defect of this receptor. Conversely, the P2Y12-13 chimera total expression was significantly reduced compared to P2Y12-R expression (Fig. 2d), thus demonstrating that the C-terminus tail of P2Y13-R could drive the degradation of a part of P2Y12-R. Cell surface expression of myc-tagged receptors was further quantified by ELISA experiments (Fig. 2e) and revealed by using an anti-myc antibody on non-permeabilized cells. Again, and in agreement with fluorescence imaging, P2Y13-R expression at the plasma membrane was markedly and significantly increased when its C-terminus tail was replaced by the one of P2Y12-R. However, whereas the replacement of the C-terminus tail of P2Y12-R by the one of P2Y13-R decreased total expression level of P2Y12-R, it did not impact on P2Y12-R cell surface expression (Fig. 2d, e), suggesting that the C-terminal of P2Y13-R was most probably regulating receptor expression in the ER rather than receptor cell surface trafficking per se.
Surface expression of P2Y13 receptor is regulated through its C-terminal tail. a Alignment of amino acid sequences of the C-terminus tail of human P2Y12 and P2Y13. b Schematic representation of P2Y13, P2Y12 as well as chimerical receptors consisting of the exchange of the C-terminus tail of P2Y13 and P2Y12 receptors. c HeLa cells expressing N-terminally Myc-tagged P2Y13, P2Y12 or the two chimeras P2Y13-12 or P2Y12-13 were processed for immunofluorescence using an anti-myc antibody. Nuclei were stained with 5 μg/mL DAPI. Scale bar 10 μm. d HEK293T cells were transfected with identical amounts of DNA constructs encoding RLuc8-tagged P2Y13, P2Y12 or the two chimeras P2Y13-12 or P2Y12-13 and luciferase intensity was measured 48 h after transfection. Results are expressed as the mean ± SEM of at least three independent experiments and analyzed by paired t test (**p < 0.005, ***p < 0.001). e HeLa cells expressing N-terminally Myc-tagged P2Y13, P2Y12 or the two chimeras P2Y13-12 or P2Y12-13 were analyzed by ELISA using an anti-myc antibody to quantify cell surface expression of the different receptors. Results are expressed as the mean of at least three independent experiments and analyzed by paired t test (**p < 0.005). Standard errors are indicated
Altogether, these data demonstrated that the expression of P2Y13-R is tightly regulated through its C-terminus intra-cytoplasmic tail.
P2Y13 receptor is constitutively ubiquitinated at steady state
The ER constitutes the limiting compartment for GPCR maturation and thus expression. Generally, misfolded transmembrane receptors in the ER then become ubiquitinated to finally undergo proteasomal degradation [16]. Given the propensity of P2Y13-R to naturally limit its expression in the ER, we thus hypothesized that expression of P2Y13-R might be regulated through ubiquitination of its C-terminus tail. To test this hypothesis, we monitored the real-time ubiquitination of the P2Y13-R and P2Y12-R in living cells using BRET2 (Bioluminescence Resonance Energy Transfer)-based ubiquitination probes as previously described [17]. This assay is based on the nonradiative transfer of energy between a luminescent energy donor (here, Renilla luciferase, RLuc8) fused to the protein of interest and a fluorescent energy acceptor (here, green fluorescent protein, GFP2) fused to the N-terminus of ubiquitin (GFP2-Ub), which has been previously successfully used to study the dynamic ubiquitination of signaling proteins [17]. Therefore, to monitor P2Y13-R and P2Y12-R ubiquitination, wild-type and chimeric P2Y13 and P2Y12 receptors were fused to their C-terminal to RLuc8 and receptor ubiquitination was measured using the GFP2-Ub fusion protein (Fig. 3a). We first performed saturation BRET curves [18] in HEK293T cells by co-expressing a constant level of P2Y13-RLuc8 or P2Y12-RLuc8 encoding vector with increasing concentrations of GFP2-Ub. As shown in Fig. 3b, a basal BRET2 signal could be detected between P2Y13-R and ubiquitin which increased hyperbolically as a function of the GFP2-Ub expression level and saturated at high GFP2-Ub concentration, thus demonstrating the specificity of the BRET signal, and consequently that P2Y13-R undergoes constitutive ubiquitination (Fig. 3b). By contrast, a very weak BRET2 signal was detected when experiments were performed with P2Y13-RLuc8 receptor and soluble GFP2 as a negative control. This BRET signal is independent of the GFP2 expression level leading to linear saturation BRET curves, most likely reflecting bystander BRET (random collision) (Fig. 3b). Similar results were obtained when measuring ubiquitination of P2Y12-R, indicating that P2Y12-R also undergoes basal ubiquitination (Fig. 3c). However, it is noteworthy that the basal BRET ratio between P2Y12-R-RLuc8 and GFP2-Ub was much lower than that measured in the presence of P2Y13-R, which could be indicative of less P2Y12-R basal ubiquitination.
P2Y13 receptor is highly ubiquitinated at steady state. a Schematic representation of BRET2 assay between P2Y13-RLuc8 and GFP2-Ub. Upon degradation of its substrate (DeepBlueC coelenterazine), the RLuc8 fused to the C-terminus of the P2Y13 receptor emits a blue light with an emission peak at 395 nm. If the P2Y13 receptor is ubiquitinated, a nonradiative transfer of energy will occur between RLuc8 and the GFP2 fused to the N-terminus of ubiquitin, resulting in re-emission of light with an emission peak at 510 nm. HEK293T cells were co-transfected with constant concentrations of P2Y13-RLuc8 (b) or P2Y13-RLuc8 (c) DNA constructs and increasing concentrations of plasmids encoding GFP2-Ub or GFP2 alone as control. The curves were fitted using a nonlinear regression equation, assuming a single binding site (GraphPad Prism). d BRET2 was measured on HEK293T cells co-expressing RLuc8-tagged receptor and GFP2-Ub. Results are expressed as the mean ± SEM of at least three independent experiments and analyzed by paired t test (*p < 0.05, **p < 0.005). In the inset, HEK293T cells were transfected with DNA constructs encoding RLuc8-tagged receptors and luciferase intensity was measured 48 h after transfection. Results are expressed as the mean ± SEM of at least three independent experiments
Interestingly, when BRET was measured between P2Y13-12 chimeric receptor and GFP2-Ub, the signal was significantly decreased when compared to wild-type P2Y13-R. Conversely, when considering P2Y12-13 receptor, the ubiquitination was significantly increased compared to wild-type P2Y12 (Fig. 3d). The differences in the BRET signals detected between GFP2-Ub and the different P2Y receptors could not rely on variations in receptor expression since all BRET2 experiments were performed using similar luminescence levels indicative of receptor expression (Fig. 3d, see inset).
Altogether, these results indicated that P2Y13-R, and most likely its C-terminus tail, was highly ubiquitinated at steady state when compared to P2Y12-R. Moreover, the data showed an inverse correlation between cell surface expression and ubiquitination level of P2Y13-R, suggesting a close link between ubiquitination of P2Y13-R and its efficient targeting to the plasma membrane.
P2Y13 receptor is ubiquitinated in the endoplasmic reticulum
BRET signals measuring ubiquitination of P2Y receptors were conducted on intact cells and thus cannot provide direct information on the subcellular localization of the detected interactions. Therefore, we performed BRET measurements after cell fractionation using sucrose step gradient to determine the precise location of the P2Y13-R ubiquitination. After cell membrane solubilization and fractionation, luciferase intensity (Fig. 4a) and BRET2 assay (Fig. 4b) were assessed on each fraction to detect P2Y13-R expression and ubiquitination, respectively. The gamma-aminobutyric acid (GABA) B receptor R1 (GABA B-R1), another GPCR which is retained in the ER [19], was used as an index of ER membrane enrichment while P2Y12-R represents an indicator of the plasma membrane (PM)-enriched fractions. As expected, P2Y12-R was mainly found in fractions 4–6 whereas GABA B-R1 was mainly detected in fractions 7–10, thus delineating the distribution of PM- and ER-enriched fractions, respectively (Fig. 4a). Despite low expression, P2Y13-R could be detected in both PM- and ER-enriched fractions (Fig. 4a). Interestingly, when we measured BRET between P2Y13-RLuc8 and GFP2-Ub on sucrose fractions, we observed that BRET2 signal was mostly detected in ER-enriched fractions—and not in PM-enriched fractions—(Fig. 4b), demonstrating that ubiquitination of P2Y13-R occurred mainly in the ER.
P2Y13 receptor is ubiquitinated in the endoplasmic reticulum HEK293T cells co-expressing RLuc8-tagged receptor and GFP2-Ub (filled square) were lyzed and applied to the top of a discontinuous sucrose gradient. Fractions were collected and subjected to luminescence analysis (a) and to BRET measurements (b). RLuc8-tagged P2Y12 receptor (filled circle) and RLuc-fused GABA B1 receptor (filled triangle) is used as marker of plasma membrane (PM) and endoplasmic reticulum (ER), respectively. The subcellular distribution patterns of receptors as well as BRET values are representative of at least three independent experiments
Proteasome inhibition induces expression of P2Y13 receptor at the cell surface of human hepatocytes
Since proteasomal proteolysis is closely linked to the ubiquitination of the target molecules for degradation, we analyzed whether P2Y13-R was degraded through proteasome by using specific inhibitors. After proteasomal inhibition with MG-132, a strong expression of P2Y13-GFP was observed in almost all the cells (Fig. 5a). By contrast, when we inhibited the lysosomal degradative pathway with leupeptin, an inhibitor of lysosomal enzymes, P2Y13-GFP expression was not modified, and the receptor was still poorly detected (Fig. 5a), as in non-treated cells (Fig. 1a). Consistent with these observations, western blot analysis showed that P2Y13-GFP was not detected after overexpression in HeLa cells, much like after leupeptin treatment. Conversely, inhibition of proteasome induced a strong expression of P2Y13-GFP (Fig. 5b).
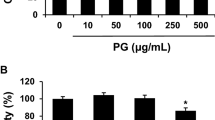
Proteasome inhibition promotes cell surface expression of P2Y13 receptor. a HeLa cells expressing P2Y13-GFP were treated for 16 h with 250 μg/mL leupeptin or 10 μM MG-132 and then analyzed by fluorescence microscopy. Nuclei were stained with 5 μg/mL DAPI. Scale bar 10 μm. b HeLa cells expressing P2Y13-GFP or not (Ctrl) were treated or not (−) for 16 h with 250 μg/mL leupeptin (leu) or 10 μM MG-132 (MG). Cell lysates were analyzed by SDS gel electrophoresis and western blotting using an anti-GFP antibody. c HepG2 cells expressing GFP-tagged P2Y13 were treated or not with 2 μM MG-132 or 2 μM bortezomib for 16 h and then analyzed by fluorescence microscopy. Nuclei were stained with 5 μg/mL DAPI. Scale bar 10 μm. d HepG2 cells expressing N-terminally Myc-tagged P2Y13 or not (Ctrl) were treated or not (−) with 2 μM MG-132 (MG) or 2 μM bortezomib (Bort) for 16 h. Cell lysates were then analyzed by SDS gel electrophoresis and western blotting using an anti-myc antibody. GAPDH was used as equal loading marker. (e) HepG2 cells expressing or not (Ctrl) N-terminally myc-tagged P2Y13 were treated or not (−) with different concentrations of MG-132 or bortezomib for 16 h. Cell surface expression of P2Y13 receptor was then analyzed by ELISA using an anti-myc antibody. Results are expressed as the mean ± SEM of at least three independent experiments and analyzed by paired t test (*p < 0.05, **p < 0.005)
Altogether, these data showed that P2Y13-R was degraded through the proteasome pathway.
We then investigated the effects of proteasomal inhibition on cell surface expression of P2Y13-R in human hepatocytes, using HepG2 cells. When expressed in HepG2 cells, much like in HeLa cells, P2Y13-R was still poorly expressed and mostly detected in the ER as shown by the colocalization with the DsRed2-ER marker (Supplementary Fig S1). In agreement with our results obtained on HeLa cells (Fig. 5a, b), proteasome inhibition with two different specific inhibitors—MG-132 or bortezomib—led to an increase in P2Y13-R expression compared to non-treated cells as demonstrated by both fluorescence (Fig. 5c) and western blot (Fig. 5d) experiments. Interestingly, proteasome inhibition induced a striking accumulation of the receptor at the cell surface (Fig. 5c). Expression of P2Y13-R at the plasma membrane was further quantified by ELISA assay after expression of N-terminally myc-tagged receptor. Both MG-132 and bortezomib treatment induced a significant increase of cell surface expression of P2Y13-R (Fig. 5e). Thus, proteasome inhibition on human hepatocytes promotes plasma membrane expression of P2Y13-R.
Proteasome inhibition promotes P2Y13-mediated hepatic HDL uptake
Since proteasome inhibition induced a strong expression of P2Y13-R at the cell surface of hepatocytes (Fig. 5c, e), we first examined HDL uptake in HepG2 cells by using fluorescent HDL3 after MG-132 treatment. Endocytosis of fluorescent AlexaFluor®568HDL3 particles showed a weak pattern in non-treated hepatocytes. In contrast, when cells were treated with proteasome inhibitor MG-132, the staining was strikingly increased, suggesting that promoting P2Y13-R at the cell surface greatly enhanced HDL endocytosis in hepatocytes (Fig. 6a, b).
Proteasome inhibition stimulates P2Y13-mediated HDL hepatic uptake. a HepG2 cells were treated or not (Ctrl) with 10 μM MG-132 for 16 h, then incubated for 15 min at 37 °C with 100 μg/mL AlexaFluor568®-labeled HDL and then analyzed by fluorescence microscopy. Scale bar 200 μm. b Endocytosis of AlexaFluor568®-labeled HDL described in (a) was quantified. Results are expressed as the mean ± SEM of at least three independent experiments and analyzed by paired t test (***p < 0,001). c Wild-type (WT) or P2Y13-R knock-out mice (P2Y 13 KO) were administered twice at a 5-day interval either 0.5 mg/kg/day bortezomib or the vehicle (saline) by subcutaneous injection. Five days after the second injection, hepatic uptake of radiolabeled 125I-HDL was measured as described in “Materials and methods”. Values are expressed as the mean ± SEM. n = 5–6 mice at least for each group. Data are analyzed by Mann–Whitney test (**p < 0,005, ns not significant)
Therefore, we investigated the hepatic HDL uptake in vivo after bortezomib injection in both wild-type mice and P2Y13-R-deficient mice. Hepatic uptake of radiolabeled 125I-HDL3 in wild-type mice was dramatically increased after bortezomib treatment (+233 ± 29 %). Remarkably, proteasome inhibition no longer stimulated HDL uptake in liver from P2Y13-R-deficient mice (Fig. 6c), demonstrating that bortezomib-induced hepatic HDL uptake was specifically mediated by P2Y13-R.
Altogether, these data suggested that proteasomal inhibition promoted plasma membrane expression of functionally active P2Y13-R, and consequently greatly potentiated P2Y13-mediated HDL endocytosis by the liver.
Discussion
Regulation of P2Y13-R cell surface expression is a key step in modulating hepatic HDL uptake, but the underlying mechanisms remained unknown. In this study, we investigated for the first time the regulation of P2Y13-R expression and provided evidence that P2Y13-R is tightly regulated by constitutive ubiquitination in the ER, and subsequent proteasome degradation. We also unraveled the role of the C-terminus tail in P2Y13-R ubiquitination and plasma membrane expression, since the exchange of the intra-cytoplasmic tail of P2Y13-R with the one of P2Y12-R led to a concomitant decrease of receptor ubiquitination and an increase of cell surface expression of P2Y13-R.
In our previous work, we showed that stimulating P2Y13-R activation by using a P2Y13-R agonist—namely Cangrelor—stimulated HDL uptake (>34.9 %) [6]. We showed here that proteasome inhibition induced a much more potent up-regulation of HDL endocytosis (>233 %), suggesting that probably, increasing P2Y13-R expression at the cell surface—rather than stimulating P2Y13-R activation—might be a better way to increase HDL endocytosis. With this in mind, we hypothesized that, in normal conditions, P2Y13-R is weakly expressed at the cell surface of hepatocytes, and is responsible for basal hepatic HDL uptake. By contrast, under certain conditions—which are still unknown but which could include fasting or low cholesterol diet—P2Y13-R expression might be rapidly and strongly increased at the cell surface to achieve HDL uptake in the liver. Such a tight regulation of P2Y13-R expression could be mediated by inhibiting the degradation process through activation/expression of specific deubiquitinating enzymes which would rescue the receptor from proteasome degradation. Alternatively, it is also possible that E3 ubiquitin ligases responsible for receptor ubiquitination were down-regulated. Interestingly, the expression/activation of deubiquitinating enzymes as well as E3 ubiquitin ligases should be fine-tuned, and an increasing number of reports showed that those enzymes could be spatially and temporally regulated during physiological or pathophysiological conditions including embryogenesis or cancer [20, 21].
It is now established that basal ubiquitination and deubiquitination are important for controlling cell surface expression and cellular responsiveness of various GPCR [22]. While ligand-induced ubiquitination usually serves as a sorting signal to target receptor to lysosomal degradation, non-ligand-mediated ubiquitination can relay distinct functions, including regulation of trafficking and receptor density at the cell surface.
Constitutive ubiquitination of GPCR can occur at the plasma membrane to regulate cell surface level of receptors. In Drosophila, ubiquitination of the GPCR-related seven transmembrane protein Smo—a signal transducer in Hedgehog signaling—plays a key role in the downregulation of Smo in the absence of the ligand. In the presence of ligand Hedgehog, the deubiquitinating enzyme UBPY/USP8 prevents Smo ubiquitination, thereby promoting Smo accumulation at the cell surface [23, 24]. Similarly, under basal conditions, the chemokine receptor CXCR7 is constitutively ubiquitinated at the cell surface, and activation of CXCR7 by CXCL12 induced a rapid receptor deubiquitination. Importantly, a CXCR7 mutant in which all lysine residues in the C-terminus tail had been replaced by alanines is no longer detected at the cell surface, demonstrating that ubiquitination is a key modification responsible for the correct trafficking of CXCR7 from and to the plasma membrane [25].
However, the ubiquitination status of GPCR can also directly be modulated in the ER, thereby affecting the density of functional receptors at the cell surface and cellular responsiveness. Accordingly, we demonstrated here that the ubiquitination status of P2Y13-R in the ER is inversely correlated with cell surface expression. Much like P2Y13-R, the adenosine receptor A2A is also subjected to ubiquitination in the ER, promoting subsequent proteasome degradation of functional newly synthesized receptors. Interestingly, the deubiquitinating enzyme USP4 has been shown to deubiquitinate the adenosine receptor A2A during biogenesis, resulting in an increased cell surface expression of functionally active A2A receptor [26]. Hence, proteasome-mediated degradation does not only seem to be restricted to misfolded proteins, and it is tempting to speculate that some properly folded P2Y13-R are targeted for proteasome degradation at steady state and released to the cell surface by deubiquitination. Proteasome inhibition might overcome the degradation machinery, leading to the escape of some functional P2Y13-R towards the plasma membrane. This would be in agreement with our results showing that proteasomal inhibition drastically potentiated hepatic HDL uptake in wild-type mice but not in P2Y13 knock-out mice.
Interestingly, ubiquitin proteasome system has been already described in cholesterol metabolism. Indeed, proteasome inhibition strongly increases protein expression of ATP-binding cassette transporters ABCA1/ABCG1 [27], which both play essential roles in cholesterol efflux from macrophages [28]. Likewise, gp78, another E3 ubiquitin ligase, is involved in the sterol-induced degradation of the enzyme 3-hydroxy-3-methylglutaryl coenzyme A (HMG CoA) reductase in the ER [29, 30]. The HMG CoA reductase catalyzes the rate-limiting reaction of cholesterol synthesis and is inhibited by the statins that are widely used in cholesterol-lowering therapies to reduce the incidence of coronary artery diseases. In this case, gp78-mediated ubiquitination marks the reductase for proteasome degradation when cellular sterol levels rise. Thus, the ubiquitin–proteasome system seems to regulate central pathways for regulation of cholesterol metabolism and thus might constitute a new attractive target to control dyslipidemia.
In addition, Idol (inductible degrader of the LDL receptor), an E3 ubiquitin ligase, ubiquitinates the precursor of LDL receptor (LDLR), thereby targeting it for degradation. Consequently, Idol knockdown in hepatocytes increases LDLR protein levels and promotes LDL uptake [31]. Hence, given the importance of both HDL- and LDL-cholesterol metabolism in cardiovascular disease risk, a better understanding of those ubiquitin-regulated pathways could lead to new therapeutic opportunities.
In addition to ubiquitination, many additional/complementary mechanisms could limit surface expression of P2Y13-R as already described for many other GPCR. In particular, some receptors might necessitate the specialized assistance of general or specific chaperone/escort proteins in the ER to fold properly and exit from the ER to navigate towards the Golgi [32]. Glycosylation may also represent an absolute requirement for the cell surface expression of some GPCR. Thus, mutations in the glycosylation sites of AT1a angiotensin II receptor resulted in the retention of mutated receptors in the ER [33]. Finally, homo- or heterodimerization has now been well described to participate to the proper export of some GPCR to the plasma membrane and might represent a prerequisite to pass quality-control checkpoints along the biosynthetic pathway. Interestingly, olfactory receptors, which are notoriously difficult to express on their own, reached the plasma membrane upon heterodimerization with the β2-adrenoceptor [34].
We previously studied pharmacological activation of the P2Y13-R by its partial agonist, the Cangrelor. Of note, we demonstrated that Cangrelor administration in mice could promote hepatic HDL endocytosis and biliary lipid excretion and might thus represent a new therapeutic approach to improve hepatobiliary RCT [6, 8]. However, the lack of oral bioavailability of Cangrelor and its very short half-life, as well as its antagonistic action on P2Y12-R, preclude its clinical use. It will therefore be a tremendous challenge to develop an uncharged agonist of P2Y13-R suitable for oral administration. An alternative and attractive way to stimulate P2Y13-R pathway for HDL endocytosis would be to increase the expression of functional P2Y13-R by selectively targeting the ubiquitin–proteasome system that recognizes the receptor as a substrate and thus rescuing P2Y13-R from its proteasome degradation. In this context, identification of E3 ligase or deubiquitinating enzymes specific for the regulation of P2Y13-R ubiquitination in the ER might provide the basis for a novel therapeutic strategy to enhance hepatobiliary RCT and ultimately prevent or treat atherosclerosis.
References
Yvan-Charvet L, Matsuura F, Wang N et al (2007) Inhibition of cholesteryl ester transfer protein by torcetrapib modestly increases macrophage cholesterol efflux to HDL. Arterioscler Thromb Vasc Biol 27:1132–1138
Acton S, Rigotti A, Landschulz KT et al (1996) Identification of scavenger receptor SR-BI as a high density lipoprotein receptor. Science 271:518–520
Martinez LO, Jacquet S, Esteve J et al (2003) Ectopic b -chain of ATP synthase is an apolipoprotein A-I receptor in hepatic HDL endocytosis. Nature 421:75–79
Jacquet S, Malaval C, Martinez LO et al (2005) The nucleotide receptor P2Y13 is a key regulator of hepatic high-density lipoprotein (HDL) endocytosis. Cell Mol Life Sci 62:2508–2515
Malaval C, Laffargue M, Barbaras R et al (2009) RhoA/ROCK I signalling downstream of the P2Y13 ADP-receptor controls HDL endocytosis in human hepatocytes. Cell Signal 21:120–127
Fabre AC, Malaval C, Ben Addi A, et al. (2010) P2Y13 receptor is critical for reverse cholesterol transport. Hepatology 52:1477–83
Blom D, Yamin T-T, Champy M-F et al (2010) Altered lipoprotein metabolism in P2Y(13) knockout mice. Biochim Biophys Acta 1801:1349–1360
Serhan N, Cabou C, Verdier C et al (2013) Chronic pharmacological activation of P2Y13 receptor in mice decreases HDL-cholesterol level by increasing hepatic HDL uptake and bile acid secretion. Biochim Biophys Acta 1831:719–725
Communi D, Gonzalez NS, Detheux M et al (2001) Identification of a novel human ADP receptor coupled to G(i). J Biol Chem 276:41479–41485
Yano S, Tsukimoto M, Harada H, Kojima S (2012) Involvement of P2Y13 receptor in suppression of neuronal differentiation. Neurosci Lett 518:5–9
Amisten S, Meidute-Abaraviciene S, Tan C et al (2010) ADP mediates inhibition of insulin secretion by activation of P2Y13 receptors in mice. Diabetologia 53:1927–1934
Gao Z-G, Ding Y, Jacobson K (2010) P2Y(13) receptor is responsible for ADP-mediated degranulation in RBL-2H3 rat mast cells. Pharmacol Res 62:500–505
Wang L, Olivecrona G, Götberg M et al (2005) ADP acting on P2Y13 receptors is a negative feedback pathway for ATP release from human red blood cells. Circ Res 96:189–196
Wang N, Robaye B, Agrawal A (2012) Reduced bone turnover in mice lacking the P2Y13 receptor of ADP. Mol Endocrinol 26:142–152
Terrillon S, Durroux T, Mouillac B, et al. (2003) Oxytocin and vasopressin V1a and V2 receptors form constitutive homo- and heterodimers during biosynthesis. Mol Endocrinold) 17:677–91
Vembar S, Brodsky J (2008) One step at a time: endoplasmic reticulum-associated degradation. Nat Rev Mol Cell Biol 9:944–957
Perroy J, Pontier S, Charest PG et al (2004) Real-time monitoring of ubiquitination in living cells by BRET. Nat Methods 1:203–208
Mercier J-F, Salahpour A, Angers S et al (2002) Quantitative assessment of beta 1- and beta 2-adrenergic receptor homo- and heterodimerization by bioluminescence resonance energy transfer. J Biol Chem 277:44925–44931
Margeta-mitrovic M, Jan YN, Jan LY, Francisco S (2000) GABA B receptor heterodimerization. Neuron 27:97–106
Seliger B, Fedorushchenko A, Brenner W et al (2007) Ubiquitin COOH-terminal hydrolase 1: a biomarker of renal cell carcinoma associated with enhanced tumor cell proliferation and migration. Clin Cancer Res 13:27–37
Li D, Zhang J, Huang W et al (2013) Up-regulation of Smurf1 after spinal cord injury in adult rats. J Mol Histol 44:381–390
Dores MR, Trejo J (2012) Ubiquitination of G protein-coupled receptors: functional implications and drug discovery. Mol Pharmacol 82:563–570
Xia R, Jia H, Fan J et al (2012) USP8 promotes smoothened signaling by preventing its ubiquitination and changing its subcellular localization. PLoS Biol 10:e1001238
Li S, Chen Y, Shi Q et al (2012) Hedgehog-regulated ubiquitination controls smoothened trafficking and cell surface expression in Drosophila. PLoS Biol 10:e1001239
Canals M, Scholten DJ, De Munnik S et al (2012) Ubiquitination of CXCR7 controls receptor trafficking. PLoS ONE 7:e34192
Milojevic T, Reiterer V, Stefan E et al (2006) The ubiquitin-specific protease Usp4 regulates the cell surface level of the A 2a receptor. Mol Pharmacol 69:1083–1094
Ogura M, Ayaori M, Terao Y et al (2011) Proteasomal inhibition promotes ATP-binding cassette transporter A1 (ABCA1) and ABCG1 expression and cholesterol efflux from macrophages in vitro and in vivo. Arterioscler Thromb Vasc Biol 31:1980–1987
Cavelier C, Lorenzi I, Rohrer L, Von Eckardstein A (2006) Lipid efflux by the ATP-binding cassette transporters ABCA1 and ABCG1. Biochim Biophys Acta 1761:655–666
Song B-L, Sever N, DeBose-Boyd R (2005) Gp78, a membrane-anchored ubiquitin ligase, associates with Insig-1 and couples sterol-regulated ubiquitination to degradation of HMG CoA reductase. Mol Cell 19:829–840
Jo Y, Lee PCW, Sguigna PV, DeBose-Boyd R (2011) Sterol-induced degradation of HMG CoA reductase depends on interplay of two INSIGs and two ubiquitin ligases, gp78 and Trc8. Proc Natl Acad Sci USA 108:20503–20508
Zelcer N, Hong C, Boyadjian R, Tontonoz P (2009) LXR regulates cholesterol uptake through Idol-dependent ubiquitination of the LDL receptor. Science 325:100–104
Achour L, Labbé-Jullié C, Scott MGH, Marullo S (2008) An escort for GPCRs: implications for regulation of receptor density at the cell surface. Trends Pharmacol Sci 29:528–535
Deslauriers B, Ponce C, Lombard C et al (1999) N-glycosylation requirements for AT1a angiotensin II receptor delivery to the plasma membrane. Biochem J 339:397–405
Hague C, Uberti M, Chen Z et al (2004) Olfactory receptor surface expression is driven by association with the beta2-adrenergic receptor. Proc Natl Acad Sci USA 101:13672–13676
Acknowledgments
We thank Nabila Mansouri for technical assistance. We also thank Sophie Allart and Astrid Canivet for technical assistance at the cellular imaging facility (INSERM UMR 1043, Toulouse), the technical service of the animal facility (Genotoul Anexplo Platform) and the DNA sequencing platform (Plateau de génomique GeT-Purpan de la plateforme Génome et Transcriptome de la génopole de Toulouse). This study was supported by the INSERM Avenir Grant, the National Research Agency (ANR Emergence and GENO #102 01) and the Midi-Pyrénées Region. Véronique Pons was supported by the Fondation pour La Recherche Médicale (FRM) and INSERM.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
18_2013_1471_MOESM1_ESM.tif
Supplementary material 1 (TIFF 1634 kb) Supplementary Figure S1: P2Y13 receptor is poorly expressed in HepG2 cells. a HepG2 cells expressing N-terminally Myc-tagged P2Y13 or P2Y12 were processed for immunofluorescence using an anti-myc antibody. Nuclei were stained with 5 μg/mL DAPI. Scale bar 10 μm. b HepG2 cells co-expressing Myc-P2Y13 and the ER marker, DsRed2-ER, were processed for immunofluorescence using an anti-myc antibody. Nuclei were stained with 5 μg/mL DAPI. Scale bar 10 μm. c HepG2 cells expressing Myc-tagged P2Y13 or P2Y12 or not (Ctrl) were analyzed by ELISA using an anti-myc antibody to quantify cell surface expression of the different receptors. Results are expressed as the mean of at least three independent experiments and analyzed by paired t test (***p < 0.001). Standard errors are indicated
Rights and permissions
About this article
Cite this article
Pons, V., Serhan, N., Gayral, S. et al. Role of the ubiquitin–proteasome system in the regulation of P2Y13 receptor expression: impact on hepatic HDL uptake. Cell. Mol. Life Sci. 71, 1775–1788 (2014). https://doi.org/10.1007/s00018-013-1471-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-013-1471-5