Abstract
Hypertensive renal disease occurs at increased frequency among the relatives of patients with this disease compared to individuals who lack a family history of disease. This suggests a heritable risk in which genetic variation may play a role. These observations have motivated a search for genetic variation contributing to this risk in both experimental animal models and in human populations. Studies of animal models indicate the capacity of natural genetic variants to contribute to disease risk and have produced a few insights into the disease mechanism. In its current phase, human population genetic studies have sought to associate genetic variation with disease in large populations by testing genotypes at a large number of common genetic variations in the genome, expecting that common genetic variants contributing to renal disease risk will be identified. These genome-wide association studies (GWAS) have been productive and are a clear technical success; they have also identified narrowly defined loci and genes containing variation contributing to disease risk. Further extension and refinement of these GWAS are likely to extend this success. However, it is also clear that few additional variants with substantial effects accounting for the greatest part of heritability will be uncovered by GWAS. This raises an interesting biological question regarding where the remaining unaccounted heritable risk may be located. At present, much consideration is being given to this question and to the challenge of testing hypotheses that lead from the various alternative mechanisms under consideration. One result of the progress of GWAS is likely to be a renewed interest in mechanisms by which related individuals can share and transmit traits independently of Mendelian inheritance. This paper reviews the current progress in this area and considers other mechanisms by which familial aggregation of risk for renal disease may arise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The introduction of life-saving renal dialysis therapy for patients with end-stage renal disease (ESRD) created a dilemma in medical practice prompted by the availability and cost of this treatment. In the United States, a decision was made that federal Medicare funds would support this treatment so that rationing of therapy and the difficult process of developing patient selection criteria could be largely avoided. A decision was also made to track data from individuals reaching ESRD by creating a national register and compiling a number of attributes from patients entered into the register. This has provided a clear view of the growth in incidence of ESRD over the last decades as well as in the co-morbid conditions to which loss of renal function was attributed [1]. Diabetes and high blood pressure are the main diseases correlated to renal disease (Fig. 1) and the growth in frequency of these two co-morbidities may have made an important contribution to increased incidence of ESRD. However, co-morbid conditions correlated with ESRD are themselves not well segregated, so many subjects in whom ESRD is attributed to diabetes are also likely to have hypertension because of the frequent concurrence of these diseases. Most importantly, the presence of declining renal function well in advance of ESRD is strongly associated with early occurrence of other cardiovascular disease, so that in most patients the decline in renal function is more often interrupted by death from cardiovascular disease than progression to ESRD [2, 3]. Among those reaching ESRD, the prognosis is poor, with 5-year mortality similar to that of patients diagnosed with metastatic cancer and with a total annual mortality approximately equal to that of breast and prostate cancer combined.
End-stage renal disease is recognized principally by a decline of glomerular filtration rate that is estimated indirectly through the accumulation of creatinine, or other markers, in serum that are excreted by glomerular filtration and which are produced at a relatively constant rate. Loss of filtration function is usually associated with and preceded by varying degrees of protein loss in the urine. The progression of disease within the kidneys of hypertensive patients that leads to loss of functional glomeruli and tubules and their irretrievable replacement with scar are usually monitored only by their effects on downstream markers. The underlying disease mechanisms in the renal tissue are not routinely sampled for diagnosis and monitoring and are generally not understood. The fact that risk of decline in renal function is not distributed randomly among patients with diabetes and hypertension, but rather shows clustering in families suggests a heritable mechanism of risk. This in turn provides an attractive opportunity: by defining the genes and variants that create heritable susceptibility, insight may be obtained into the mechanisms by which some individuals resist advancing disease while others succumb. From such insight, the current vacuum of therapy that specifically targets disease mechanisms might be filled. This review will consider the evidence that susceptibility to progressive renal disease in hypertension aggregates in families, review the approaches used to seek genes involved in such susceptibility and the progress that has resulted, and will examine other areas in which progress towards understanding how kidneys get injured in some hypertensive patients may occur.
The familial origins of hypertensive renal disease
Most hypertensive patients do not develop kidney disease [4]. Patients developing renal disease and advancing to ESRD often have relatives that also experience progressive loss of renal function [5]. This increased occurrence among relatives can indicate risk created by allelic sharing and can suggest future disease risk in individuals with predisposing diseases such as diabetes and hypertension. The concurrence of renal disease among relatives has been assessed in several studies and in several populations. In the southern US, nearly 19 % of ESRD patients with hypertension had a first or second-degree relative with ESRD [6]. Familial risk does not appear to be equal among individuals of different racial origins. This also suggests the possibility of heritability because the genetic variation creating risk is likely to be present at different frequencies in different populations. Compared to Caucasians, persons with African ancestry that are treated with dialysis were observed to have a higher likelihood of a first or second-degree relative with ESRD (~23 vs. 14 %) [6].
The role of the kidney in contributing to blood pressure regulation suggests that the relationship between hypertension and renal disease might be cause and effect. So it is necessary to determine whether familial risk of ESRD is confounded by the familial aggregation of hypertension or whether risk of renal disease arises independently. This question has been investigated to reveal that when family history of hypertension and other potential risk-aggravating factors are controlled for, ESRD risk is preserved among related individuals [7]. Interestingly, similar observations have been made regarding risk of progressive renal disease in diabetics [8–11], suggesting that both hypertension and diabetes are co-morbid with renal injury, but in both these pre-disposing conditions the susceptibility to adverse renal outcomes is largely determined by independent familial risk.
Several animal models illuminate this issue of independence of risk for renal damage in the presence of hypertension. In the Fawn-hooded rat, a model of nephrotic proteinuria, two independent loci have been identified, one contributing to proteinuria, the other to blood pressure regulation [12]. However, this model is not a rich facsimile for hypertension-associated renal disease in humans. The spontaneously hypertensive rat (SHR) was produced by selective breeding on the trait of elevated blood pressure and resulted in several closely related lines sharing the hypertensive trait, but differing in susceptibility to renal disease [13]. This model provides a richer phenotypic spectrum in which glomerular and tubulo-interstitial injury co-exist with significant proteinuria in the presence of inflammatory changes and renal fibrosis. There is evidence from mapping and association studies of genetic separation of some renal injury traits from loci affecting blood pressure in SHR lines [13, 14]. However, further work is required to clarify whether a single well-mapped locus by which blood pressure levels differ across renal injury-prone and -resistant SHR lines contains genetic variation affecting blood pressure directly or whether blood pressure is affected secondary to renal injury [14].
The genetic architecture of renal disease susceptibility
The last 10 years has seen remarkable progress in the identification of genetic variation responsible for heritable renal diseases that show simple Mendelian genetics. The genetic architecture of heritable risk of renal disease in hypertension may arise from single genetic susceptibilities in affected pedigrees, or may reflect transmission of genetic susceptibility at more than one locus in the genome. In the broader population, the allelic spectrum of susceptibility is unknown [15]. The pathogenesis of renal injury is complex and may involve diverse genetic risks including those specifically affecting glomerular structure, those that may produce proteinuria without initial structural damage to the glomerulus, those that may specifically damage tubular structure or function, those that can be associated with more or less inflammatory injury and those which can determine whether disease terminates by replacement of functional renal epithelium with fibrotic scar or with recovery of epithelial function. The decline of renal function in hypertensive patients may include all of these outcomes arising from a single genetic cause. Alternatively, the destruction of renal clearance may be driven by several genetic variants affecting more than one element of pathogenesis.
The complex evolution of renal disease and its impact on multiple elements of normal renal function, its interaction with inflammatory responses, and the participation of immune mechanisms in tissue injury all pose a significant hurdle to progress. This hurdle is made only more difficult by the presence of underlying genetic complexity. One approach to address the complexity of pathology is to disassemble the disease into components that may be more closely attributable to specific underlying genetic variation. These disease elements constitute intermediate phenotypes and include such readily measured traits as albumin excretion and serum creatinine or cystatin c concentration. Many of the desirable intermediate phenotypes can only be assessed by direct analysis of renal tissue. However, routine renal biopsy is not possible across the large numbers of mostly unaffected individuals needed for a population-scale study.
Placing renal disease risk on a map
Success in the application of mapping approaches to rare Mendelian disease prompted the extension of these mapping studies to common disease with more complex patterns of inheritance. These efforts began with the 2001 report from the HyperGEN study of 215 African American (AA) and 265 white hypertensive sibships in which creatinine clearance had been estimated from measurements of serum and urinary creatinine and in which a panel of nearly 400 microsatellite markers distributed across the genome were genotyped [16]. This population was found to have moderate heritability of creatinine clearance that was similar in both whites and AAs. Mapping produced peak LOD scores on chromosome 3 for both populations, however, these peaks were clearly separate, indicating the related underlying genetic variation was different in the two racial groups. Unfortunately, linkage mapping is limited in its ability to precisely localize causative genetic variation and the specific genetic variation to which these peaks are attributable remains unknown. These initial efforts to map genetic loci influencing renal parameters were extended to include proteinuria. These traits were also shown to be heritable with the effect of genes on the trait estimated to range up to 49 % for urinary albumin excretion (Mixed Caucasian and African American [17]).
A study of urinary albumin excretion in an expanded HyperGEN population of hypertensives was also used to examine heritability of renal disease traits and to perform linkage analysis [17]. The expanded population was made of individuals with a hypertensive proband and at least one hypertensive sibling and again comprised a similar number of white and black Americans. Heritability of urinary albumin excretion was strong with 49 % or trait variance attributed to the effect of genes. Two suggestive LOD peaks were obtained, but this time in the combined population and located on chromosomes 12 and 19. Linkage studies of albuminuria in the Framingham population revealed lower levels of heritability (20 %) while mapping suggested the presence of genetic variation contributing to albuminuria on chromosome 8 and this effect was noted both in the overall population as well as in a subset enriched for hypertension [18]. The lack of clear and distinct LOD peaks suggests complexity in the underlying genetic susceptibility to these measures of renal function and reveals no concordance between loci linked to glomerular filtration and to albuminuria. To investigate the relationship between these two variables further, both were examined in a bivariate linkage study in the HyperGEN population [19]. The mapped LOD score peaks were again only suggestive, and again lack substantial concurrence with earlier mapping efforts and again suggested that there was no detectable overlap between loci that may be involved in albuminuria and in glomerular filtration. Studies in a Mexican-American population used similar approaches to estimate heritability for serum creatinine, creatinine clearance, estimated GFR, and albumin excretion [20]. Heritability of each was statistically significant and moderate, ranging from 19–25 %. Linkage mapping identified several LOD peaks for these traits with no evidence of overlap between traits reflecting GFR (serum creatinine, creatinine clearance, and eGFR) and albuminuria.
Linkage analysis studies further strengthened the evidence for heritability of renal function traits, but at the same time revealed the difficulty that would need to be confronted to move forward to identification of causative genetic variation. These difficulties flow from the inconsistent results of mapping studies across and within populations, the poor localization of linkage peaks that result in regions containing many genes, and the lack of major genetic effects associated with linkage peaks. At the same time, the identification of a large number of single-nucleotide polymorphisms (SNP) in diverse human populations provided the impetus for the initiation of genome-wide association studies (GWAS), which offered some opportunity to overcome these obstacles to the search for genetic variation underlying heritability.
GWAS: halting progress
A genome-wide association study is a population-based approach, while linkage analysis is performed on collections of affected pedigrees. GWAS uses stable SNP variation and surveys these markers across the genome at very high density. The capacity to genotype hundreds of thousands of SNPs per individual with very high accuracy (and at moderate cost) has been an important predicate to the successful application of this approach. Knowledge of the relative frequency of these SNP alleles in the study population permits selection of SNPs whose allelic variants commonly occur in the population and for which both forms of the bi-allelic variants at each site are also relatively frequent. The underlying principle of GWAS mapping is that genetic recombination erodes linkage between adjacent non-causative SNP markers and trait variation in a population and this erosion is proportionate to the frequency of recombination between the causative variants and the marker variant. Thus, a very dense panel of informative markers will show retention of linkage disequilibrium only between the causative variation and markers that are close to it. Effective marker density can be increased further by imputation, a statistical process that uses linkage disequilibrium to predict the likely allelic state of adjacent untyped SNPs [21, 22]. Compared to linkage analysis, this gives GWAS a fine-scale resolution that can reveal the trait-associated gene.
Such resolution, however, is achievable only with an associated statistical impediment. This is created by the fact that the GWAS test is a unique hypothesis for essentially every SNP genotyped. This requires adjustment of significance thresholds for the large numbers of markers tested; typically a p value of 5 × 10−8 is used. This places a premium on the use of a large study population size in the discovery phase of mapping. A combination of one or more populations may be used in the discovery phase and additional populations may be used to independently replicate initial findings [23, 24].
It appears that the GWAS research cycle will be a rather short one. A number of GWAS studies of renal function have been reported that provide sufficient insight to examine what has been learned and whether the optimistic view that such studies will be successful in identifying genes containing variation with sizeable effects on renal function is likely to be attained. Four main conclusions can be reached at this point. First, the approach is a technical success: investigations of indirect phenotypes of renal function can be coupled with very high throughput genotyping technologies and applied across thousands of subjects to produce reliable and replicable results. Second, GWAS studies are able to reliably identify genetic variation closely linked to genes contributing to measures of renal function and disease [25–28]. Thirdly, with one exception discussed below, genes containing variation with large effects on renal function are not uncovered by this method. Finally, much of the heritability that has been identified in traits of renal function and disease is not explained by the discoveries that GWAS has brought to light.
Measures of renal function and renal disease used in GWAS studies include creatinine clearance calculated from serum and urinary creatinine, estimated glomerular filtration rate (eGFR) calculated from serum creatinine or from serum cystatin c levels and albumin excretion. The study populations used are generally not selected for renal disease and are therefore not chosen because of the presence of hypertension. These populations include individuals with and without diminished renal function, with and without hypertension, and with and without diabetes. The typical study design has included a discovery phase in one or more populations and a replication phase to test the reproducibility of the discoveries in an independent population. This design is effective at eliminating false-positives. However, it incurs some risk of eliminating true-positives that fail to replicate in the smaller follow-up study.
A notable aspect of renal function GWAS studies is that several of the variants identified as associated with renal traits (CST3, GATM, CPS1, SLC22A2, TMEM60, WDR37, SLC6A13, WDR72, and TBX2) were probably identified because they directly affect the renal function marker assessed in the study rather than reflecting the underlying function the marker is intended to indicate [26, 27]. Cystatin c is a secreted protein used as an indicator of renal filtration. Variation in CST3, which encodes cystatin c, has been associated with serum cystatin c levels and estimated GFR. However, the underlying genetic variation probably affects serum levels of cystatin c directly, rather than through any effect on renal function. Several genes containing variation associated with eGFR estimated from serum creatinine levels, but not eGFR estimated from serum cystatin levels appear likely to be involved in creatinine synthesis or secretion [29]. While these findings are not helpful in understanding the genetic basis of renal disease, they are testimony to the sensitivity and reliability of the GWAS approach, revealing that even variants with quite small allelic effects can be routinely uncovered.
Other genes were found to be associated with renal function that did not appear to affect renal function marker scores directly. However, often the relationship between these genes and their mechanism to induce alterations in renal function is not very clear and the magnitude of the effect of the allelic variants on renal function is generally very small. Further, the effects attributable to each of these variants can account for only a part of the total heritability of these traits. For example, ANXA9 encodes an annexin that differs in its calcium-dependent binding properties compared to other annexins, but its explicit function in the kidney is not well defined. Stanniocalcin 1 (STC1) may have anti-inflammatory properties by acting in the regulation of mitochondrial anti-oxidant pathways [30, 31]. Uromodulin links adaptive and innate immunity in the urinary tract via the Toll-like receptor (TLR4), suggesting defense from Gram-negative bacterial infection [32].
By excluding the likely presence of common genetic variants with large phenotypic effects, GWAS studies have added some clarity to the genetic architecture of heritable risk of loss of renal function. They have shown that this risk is real, they have identified genes through which this risk may be manifest, and they have shown that the effects associated with individual common alleles are smaller than expected. These findings are unlikely to impact the clinical approach to this disease. Genes containing variants with moderate to large effects have not been identified. These studies have not fully clarified whether the set of alleles creating susceptibility to hypertension and the set of alleles creating susceptibility to renal injury in hypertension overlap. GWAS studies in which blood pressure genetics and renal function genetics have been the primary focus have yield only limited support for such overlap. Genes containing variation that may be relevant to both blood pressure and renal function include UMOD [27, 33, 34] and ATXN2 [27, 35]. While the optimistic view of GWAS studies was that they would identify common variants with substantial trait effects, the diminished outcomes are balanced by the fact that GWAS studies have led to important clarification of the field. This in turn can sharpen the focus on other hypotheses by which genetic and other mechanisms might account for familiality of disease risk.
Admixture aids GWAS progress
Hypertensive renal disease is notably frequent among African Americans (AAs) [5] and the heritability of indicators of renal injury is generally higher in this subpopulation [6, 36]. This suggests that in AAs alleles that are enriched due to ancestry may include alleles creating susceptibility to renal disease. Admixture mapping uses populations containing individuals of mixed ancestries. Divergence in the presence or frequency of allelic variants in populations with different ancestry provides a means to identify among admixed individuals those segments of the genome that reflect the different origins of their mixed ancestry. With continued mixing over many generations, these regions are broken down by recombination and are less distinct. If admixture has extended over only a few generations, identification of the origin of different haplotypes present across the genome is reliably achievable with high-density SNP markers containing SNPs known to have different population distribution and frequency. Admixture mapping seeks to identify the genomic regions inherited from the high disease incidence ancestral population that occurs at higher frequency in admixed populations in those individuals affected by a disease than in unaffected individuals [37].
Genome-wide admixture mapping has been used successfully to identify a major genetic locus affecting risk of reduced renal function in African Americans. The risk appears to be dissociated from diabetic renal injury, but not from renal injury attributable to hypertension or HIV infection. The mapped region contains two genes that may be involved in pathogenesis, MYH9, an unconventional myosin, and APOL1, an apolipoprotein [38, 39]. Variation in MYH9 is strongly associated with disease risk, but variation in the adjacent APOL1 gene appears to provide resistance to trypanosome infection [40, 41]. This presents the possibility that selection has acted on this locus to increase the frequency of an allele of APOL1 that is adaptive in geographic regions, such as parts of Africa, with endemic trypanosome infection. Renal risk-enhancing alleles of MYH9 (in linkage disequilibrium with the APOL1) may have increased in frequency in this population as a result of the action of selection on the adaptive APOL1 variation. There remain important unanswered questions, however, that illustrate the difficulty that can be encountered even when causative variation with large trait effects is mapped at very fine resolution. The precise variation contributing to disease risk is not yet known, and consequently the disease mechanism is also not understood at a cell and molecular level. Mutation in MYH9 is associated with Mendelian glomerular disease [42, 43] and proteinuria in MYH9 knockout mice that have been treated with nephrotoxins [44]. This indicates the possible importance of MYH9 in development of renal disease in hypertensive AAs. However, the evidence implicating MYH9 variation in humans is incomplete, and is complicated by the fact that APOL1 variants have a stronger association with disease [40, 45].
GWAS and epistasis
Genome-wide association studies were designed to test the hypothesis that allelic variation contributing to heritability of common disease would involve a limited number of common alleles of relatively large effect, as predicted in the “common disease:common gene” hypothesis. The capacity of the variation that has been uncovered by GWAS studies to account fully for the heritable effects on disease risk is frequently limited, resulting in the term “missing heritability” to describe the shortfall. Consequently, the underlying presumptions that have motivated GWAS are now under reconsideration, and it is possible that other mechanisms may account for the gap between what GWAS set out to achieve and what has been accomplished.
It is worth considering the alternative explanations that may account for the incomplete success of GWAS to uncover variation (excluding the MYH9/APOL1 locus) that contributes to heritability of renal disease risk and to examine the challenges to investigate them. One possibility is that heritability is attributable to a substantial number of rare variants in the population that have large effects, but in relatively few individuals. GWAS cannot effectively investigate this type of genetic architecture and was never intended to discover such genes.
Another possibility is that interactions between multiple susceptibility variants combine to produce non-additive effects on traits. This interaction is called epistasis. It contemplates that, in an outbred population like humans, there is extensive genetic diversity comprising independent loci containing allelic variants that can have relatively large effects on traits. Within any individual, many such variants may exist and most of the effects of each of the variants present are non-additive. This might be because a variant acts on a trait to alter a critical element of a biological pathway affecting the trait. If another variant at another locus produces a similar effect on the same trait, it may not be able to perturb the trait further in the presence of the first variant. This will tend to mask the effect of the second variant. It has recently been proposed that GWAS has in fact largely discovered the variants that cause most of the heritability of the polygenic traits they have investigated [46]. It is proposed that these traits depend on a rate-limiting value influenced by inputs from multiple pathways and that, as the number of inputs to this rate-limiting value increases, so the influence of epistatic interactions that are sub-additive is likely to increase. Thus, the amount of the heritability of the trait that is explained is lessened as the number of inputs increases.
There are some experimental models in which such interactions tend to support this view. For example, data obtained in several rodent consomic strains in which individual chromosomes from one inbred strain are replaced with chromosomes from another inbred strain differing in a trait. It has been observed that many single chromosomal replacements can affect the trait value and that, if summed together additively, the effect of the replacements can far exceed the size of the trait difference across the progenitor strains [47]. This implies that epistatic interaction in the progenitor strains prevents the trait from reaching the summed levels implied by the isolated effects arising from individual chromosomes. While this data is quite convincing, it is notable that selective breeding of outbred strains is often highly successful in driving phenotypic effects far in excess of the variance observed in these strains [48]. This implies the presence in the progenitors of genetic variation that can be aggregated by selective breeding without substantial loss attributable to sub-additive effects. Indeed, in at least one model of renal disease involving natural allelic variation, epistatic interactions have been shown to generate greater than additive trait effects [49]. Unfortunately, epistasis is a challenging property to investigate in human populations. The problem of detecting epistasis is increased by the potentially high dimensionality of the task.
G and E
The effect of genetic variation on a trait may be highly sensitive to different inputs an individual receives from its environment. It is very challenging to uncover genetic variants that have this property. In human population genetics studies, there is no possibility to control environmental exposures. These can be investigated by extensive subject profiling, for example through collection of dietary information via recall or through the detection of environmental exposures via analysis of urine or serum. However, it may be necessary to study populations containing members with markedly different environmental exposures to identify the main effects, and the cost and complexity created by such studies is an obstacle.
Questions unanswered by GWAS because they were unasked
The reliance of GWAS on pre-designed high-throughput genotyping systems can lead to gaps in the analysis. For example, common SNP variation in some genomic regions may be poorly represented on these genotyping platforms. Another possibility is that forms of genetic variation such as copy number variants, deletions, insertions and inversions, may be involved in trait modification. These types of variation are not directly tested by high-throughput genotyping platforms targeting SNPs, though some SNP-based methods attempt to account for them when they are known.
Non-Mendelian inheritance
The extraordinary success that has been accomplished by applying Mendelian principles to understanding single gene traits provided the foundation for GWAS studies directed at complex traits. GWAS relies on the concepts of chromosomal inheritance and Mendelian genetics. However, single gene traits differ from complex traits: they typically have high heritability, moderate to high penetrance, and generate distinct phenotypes affecting a small number of individuals. One intriguing possibility is that heritability unaccounted for by GWAS may be transmitted through mechanisms other than Mendelian chromosomal inheritance. It is important to consider this possibility because heritability estimates for complex disease traits are typically made in nuclear families. However, GWAS studies are population studies, not family studies. Thus, the heritability gap might result from mechanisms of trait sharing that operate among closely related individuals, but that may not be similarly discernable across populations.
Non-Mendelian inheritance occurs through a number of well-recognized mechanisms. Inheritance of traits can be extra-nuclear, dependent on sequence differences in the mitochondrial genome so that inheritance is entirely determined by the allelic state of the mother. De novo mutation provides another mechanism and is most notably associated with genomic instability arising in trinucleotide repeats. These can result in the emergence of heritable traits in which parents and progeny do not share alleles. Gene conversion provides another mechanism leading to non-Mendelian trait transmission. Gene conversion occurs during genomic sequence repair after recombination and involves the use of one chromosomal strand to repair the strand acquired from the other parent, resulting in the conversion of one parental allele to the state of the other diploid allele and a loss of heterozygosity at the repaired locus.
The genes that are passed from parents to progeny may be subject to modifications that do not alter their DNA sequence, but do affect the expression of the modified allele. The broad term for phenomena in which parental factors influence traits in progeny by marking genomic DNA is “epigenetics”. This genetic imprinting is a recently evolved mechanism of epigenetic inheritance present only in marsupials and placental mammals. This is a mechanism in which certain genes are expressed in a parent-of-origin-specific manner and which depends on germ-line methylation of progeny DNA, notably in the cytosine and guanine-rich promoter regions of certain genes. Maternal influences during gestation may result in epigenetic silencing of either paternal or maternal alleles. This mechanism of divergence from Mendelian control over traits may have its origins in the role of the mother in the pre- and post-natal provisioning of offspring with resources [50, 51]. The metabolic cost to the mother of raising progeny is greater than the cost to the father. This creates a potential conflict between maternal and paternal “interests” that may be manifest through paternal alleles that tend to drive higher maternal resource consumption and maternal mechanisms to suppress progeny resource consumption that is directed by paternal alleles. Imprinting ultimately gives greater control over progeny phenotype (and therefore maternal resource consumption) through the action of maternally directed imprinting mechanisms [51]. Imprinting is a durable, but transitory process, requiring erasure and re-establishment at each generation (during gametogenesis and in the early embryo), and perhaps thereby permitting some scope for adaptive responses driven by environmental inputs, such as nutrition, an epigenetic mechanisms with origins as ancient as insects [52].
Epigenetics via other means
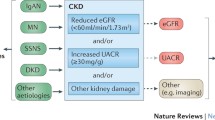
The availability of inbred rodent strains provides a simplified genetic platform on which non-Mendelian inheritance patterns might be more clearly recognizable than in outbred populations. Nadeau and colleagues [53] have reported interesting studies investigating heritable traits in which phenotype is transmitted in the absence of a causative genotype. These studies utilize consomic mouse lines derived from two inbred mice strains constituting a panel of lines in which a single chromosomal substitution has been made so that each consomic line has all of the chromosomes of its inbred progenitor line, except for one that has been introgressed from another inbred strain. Two matings were made: one involving a pair of non-consomic inbred mice of the same strain and another involving an inbred female of the same strain mated to a consomic male that is genetically identical to this female except that this male contains the Y chromosome derived from a different strain (Fig. 2). The female progeny do not possess a Y chromosome so progeny of both the first and second of the two preceding crosses are genetically identical. However, the progeny may not be phenotypically identical. Phenotypic differences between the two sets of female progeny cannot be attributable to Mendelian genetic differences.
Breeding design for testing the effect of transgenerational effects attributable to the Y chromosome. The breeding pair on the left side comprises a male and female of the “A” inbred strain. The pair on the right side comprises a female of the A strain, and a consomic male of the A strain in which the Y chromosome of the “B” strain has been introgressed. The female progeny of both matings will lack any Y chromosome and will therefore be genetically identical to females of the inbred A strain. If the Y chromosome from the B strain produces transgeneration traits then phenotypes in the two genetically identical female progeny may differ
These strains provide an interesting platform to assess the frequency and magnitude of traits that are heritable, but that are not attributable to the transmission of genes. Nadeau has used crosses between consomic lines to assess the typical frequency and magnitude of Mendelian traits arising from the transmission of autosomes in such crosses and has then investigated whether and with what frequency and magnitude traits are transmitted that are attributable only to the untransmitted Y chromosome [53]. After surveying a diverse array of behavioral traits, they concluded that traits arising from the non-transmitted paternal Y chromosome were similar in frequency and magnitude to those attributable to the transmitted autosomes. This raises a rather vexing question: how can traits be transmitted in the absence of differences in DNA? These investigators endeavored to control or eliminate confounding social or environmental factors. Their findings are particularly perplexing because of the small number of genes on the Y chromosome and raise a number of important questions. For example, if such heritable transgenerational effects can arise from the Y chromosome, can they also arise from the autosomes and X chromosome? And what could be the molecular basis of such effects? Are they wholly dependent on the genotype of the Y chromosome or do they involve interaction between the paternal genotype and the progeny genotype so that the untransmitted Y chromosome effect may be different in one genetic background than in another? At present, there is little knowledge that can explain these observations at the molecular level. Perhaps they are attributable to paternal effects to induce DNA modifications or histone methylation in the progeny genome. Perhaps there is an additional mechanism of maternal and paternal genetic competition that affects traits more broadly than resource competition and exists at a molecular level that is not yet understood. What is clear is that, if these same genetic mechanisms are at work in human populations, they might easily affect complex traits and uncouple the relationship between genotype and phenotype that is the foundation of Mendelian genetic investigations. The transgenerational traits that have been described are behavioral traits, however, there is also evidence of transgenerational trait transmission from the paternal lineage that affects metabolic traits [9, 54].
The enduring gift of immunity
The transmission of pre-formed immunological competence in the form of maternal immunoglobulins to progeny whose immune systems are immature is an important mechanism for providing progeny with adaptive advantages via transfer of non-genomic maternal resources. This adaptive advantage provides another method by which progeny phenotype can be shaped independently of its DNA. Trans-generational immune molecule transfer appears to have a more ancient evolutionary history than genetic imprinting. Although transfer through the placenta is a key route of immunoglobulin transfer in mammals, immunoglobulin provisioning precedes the evolution of placental mammals. Its occurrence in birds and mammals through the transfer of immunoglobulins either via the yolk, the placenta, and lactation is well understood [55–57]. Indeed, such protection with pre-formed natural defense molecules precedes even the development of immunoglobulins and occurs even in insects [58]. The most obvious benefit of maternal progeny immunoglobulin transfer is the provision of temporary passive immunity to the progeny until their own immune systems are able to react to interaction with antigens. However, there are secondary implications that can persistently shape progeny traits over a much larger part of the progeny lifespan. This is well illustrated by experiments in inbred rodent models where maternal immunoglobulin transmission to progeny has a strong impact on the penetrance of traits involving diseases such as type 1 diabetes and atherosclerosis [59, 60]. These effects endure beyond the period of passive immunization, and may persist over more than one generation [61], suggesting that maternal immunoglobulin shapes the future reactivity of the progeny immune system [62–64].
Immunoglobulin transfer between mother and progeny may have effects by influencing the subsequent development of the progeny immune system, reflecting the operation of the immune system as an information network [65]. The immune system reacts to foreign substances by producing antibodies. However, in addition to this outward surveillance, the immune system is also self-monitoring and self-reacting. Antibodies generated to an antigen are the result of a B cell response and clonal selection that includes differential usage of many exons encoding structural elements of immunoglobulin [66] and recombination events that generate novel somatic DNA sequence to optimize antigen recognition [67]. The resulting antibodies are called idiotypic antibodies. The recombination of variable regions of immunoglobulin results in the production of immunoglobulins that are themselves immunogenic because they contain amino acid sequences different from those in the animal’s germ line. Thus, a network of antibody responses may result from exposure to a single antigen to include outwardly looking idiotypic antibodies as well as inwardly looking anti-idiotypic antibodies produced in response to the idiotypic antibodies (and anti-anti-idiotypic antibodies, etc.). Remarkably, progeny immune responses can be shaped over long periods of time by exposure to maternally transmitted idiotypic antibodies, and also to anti-idiotypic antibodies [64]. Thus, the whole network of immunoglobulins produced in response to maternal antigen exposure has the capacity to convey information to progeny that shapes the progeny’s immune response to subsequent antigen exposure. This may be highly relevant to genetic studies of autoimmune diseases. For example, asthma has substantial heritability and involves IgE-mediated responses to allergens [68, 69]. The genotype:phenotype relationship of the asthma trait may be uncoupled by non-genetic mechanisms arising from maternal immunoglobulin transfer where progeny response to asthma-inducing allergens can be heavily modified by maternally transferred immunoglobulin [64].
Work in the rat SHR model of arterial hypertension indicates that blood pressure traits are strongly influenced by exposure both to the maternal uterine environment, as shown by SHR embryo transfer experiments into normotensive recipients, and by changes in the neonatal environment such as fostering of pups to normotensive surrogate mothers [70–72]. Furthermore, there is extensive sequence variation in the immunoglobulin heavy chain locus that appears to affect susceptibility to kidney disease in this model of hypertension [73]. Similar allotypic germ-line variation occurs in human immunoglobulins and has the potential to affect traits in a number of human diseases that have an inflammatory component [74–78]. Unfortunately, this germ-line variation is absent from the HapMap collection of SNPs used in the design of GWAS genotyping systems, so the involvement of SNP variation in this locus in diseases and traits tested by GWAS may not be recognized [79].
Conclusions
Single-nucleotide polymorphism markers that closely pinpoint genes and other genome sequences that may influence risk of renal disease in hypertension have been reliably uncovered by GWAS studies. GWAS can be extended to include larger study populations or to refine disease phenotypes to maximize the discovery of such variants. However, these studies seem unlikely to be able to explain the larger part of the heritable risk of renal diseases. Other factors may contribute to familial aggregation of risk of hypertensive renal disease. These include rare genetic variants, epistatic interactions among genetic variants, gene–environment interactions and mechanisms of transgenerational inheritance that arise from altered gene expression resulting from histone modification and DNA methylation, and the transgenerational transmission of proteins from parent to progeny.
Abbreviations
- AA:
-
African American
- eGFR:
-
Estimated glomerular filtration rate
- ESRD:
-
End-stage renal disease
- GWAS:
-
Genome-wide association study
- SHR:
-
Spontaneously hypertensive rat
- SNP:
-
Single-nucleotide polymorphism
References
Collins AJ Unites States Renal Data System, Annual Report 2011. http://www.usrds.org/
Matsushita K, van der Velde M, Astor BC, Woodward M, Levey AS, de Jong PE, Coresh J, Gansevoort RT (2010) Association of estimated glomerular filtration rate and albuminuria with all-cause and cardiovascular mortality in general population cohorts: a collaborative meta-analysis. Lancet 375(9731):2073–2081
Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY (2004) Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 351(13):1296–1305
Freedman BI (2003) Susceptibility genes for hypertension and renal failure. J Am Soc Nephrol 14(7 Suppl 2):S192–S194
Freedman BI, Spray BJ, Tuttle AB, Buckalew VM Jr (1993) The familial risk of end-stage renal disease in African Americans. Am J Kidney Dis 21(4):387–393
Freedman BI, Soucie JM, McClellan WM (1997) Family history of end-stage renal disease among incident dialysis patients. J Am Soc Nephrol 8(12):1942–1945
Lei HH, Perneger TV, Klag MJ, Whelton PK, Coresh J (1998) Familial aggregation of renal disease in a population-based case-control study. J Am Soc Nephrol 9(7):1270–1276
Spray BJ, Atassi NG, Tuttle AB, Freedman BI (1995) Familial risk, age at onset, and cause of end-stage renal disease in white Americans. J Am Soc Nephrol 5(10):1806–1810
Yazbek SN, Spiezio SH, Nadeau JH, Buchner DA (2010) Ancestral paternal genotype controls body weight and food intake for multiple generations. Hum Mol Genet 19(21):4134–4144
Freedman BI, Tuttle AB, Spray BJ (1995) Familial predisposition to nephropathy in African Americans with non-insulin-dependent diabetes mellitus. Am J Kidney Dis 25(5):710–713
Faronato PP, Maioli M, Tonolo G, Brocco E, Noventa F, Piarulli F, Abaterusso C, Modena F, de Bigontina G, Velussi M, Inchiostro S, Santeusanio F, Bueti A, Nosadini R (1997) Clustering of albumin excretion rate abnormalities in Caucasian patients with NIDDM. The Italian NIDDM Nephropathy Study Group. Diabetologia 40(7):816–823
Brown DM, Provoost AP, Daly MJ, Lander ES, Jacob HJ (1996) Renal disease susceptibility and hypertension are under independent genetic control in the fawn-hooded rat. Nat Genet 12(1):44–51
Gigante B, Rubattu S, Stanzione R, Lombardi A, Baldi A, Baldi F, Volpe M (2003) Contribution of genetic factors to renal lesions in the stroke-prone spontaneously hypertensive rat. Hypertension 42(4):702–706
Bell R, Herring SM, Gokul N, Monita M, Grove ML, Boerwinkle E, Doris PA (2011) High-resolution identity by descent mapping uncovers the genetic basis for blood pressure differences between SHR lines. Circ Cardiovasc Genet 4(3):223–231
Schelling JR, Zarif L, Sehgal A, Iyengar S, Sedor JR (1999) Genetic susceptibility to end-stage renal disease. Curr Opin Nephrol Hypertens 8(4):465–472
DeWan AT, Arnett DK, Atwood LD, Province MA, Lewis CE, Hunt SC, Eckfeldt J (2001) A genome scan for renal function among hypertensives: the HyperGEN study. Am J Hum Genet 68(1):136–144
Freedman BI, Beck SR, Rich SS, Heiss G, Lewis CE, Turner S, Province MA, Schwander KL, Arnett DK, Mellen BG (2003) A genome-wide scan for urinary albumin excretion in hypertensive families. Hypertension 42(3):291–296
Fox CS, Yang Q, Guo CY, Cupples LA, Wilson PW, Levy D, Meigs JB (2005) Genome-wide linkage analysis to urinary microalbuminuria in a community-based sample: the Framingham Heart Study. Kidney Int 67(1):70–74
Leon JM, Freedman BI, Miller MB, North KE, Hunt SC, Eckfeldt JH, Lewis CE, Kraja AT, Djousse L, Arnett DK (2007) Genome scan of glomerular filtration rate and albuminuria: the HyperGEN study. Nephrol Dial Transplant 22(3):763–771
Arar N, Nath S, Thameem F, Bauer R, Voruganti S, Comuzzie A, Cole S, Blangero J, MacCluer J, Abboud H (2007) Genome-wide scans for microalbuminuria in Mexican Americans: the San Antonio Family Heart Study. Genet Med 9(2):80–87
Anderson CA, Pettersson FH, Barrett JC, Zhuang JJ, Ragoussis J, Cardon LR, Morris AP (2008) Evaluating the effects of imputation on the power, coverage, and cost efficiency of genome-wide SNP platforms. Am J Hum Genet 83(1):112–119
Balding DJ (2006) A tutorial on statistical methods for population association studies. Nat Rev Genet 7(10):781–791
Ehret GB, Munroe PB, Rice KM, Bochud M, Johnson AD, Chasman DI, Smith AV, Tobin MD, Verwoert GC, Hwang SJ, Pihur V, Vollenweider P, O’Reilly PF, Amin N, Bragg-Gresham JL, Teumer A, Glazer NL, Launer L, Hua Zhao J, Aulchenko Y, Heath S, Sober S, Parsa A, Luan J, Arora P, Dehghan A, Zhang F, Lucas G, Hicks AA, Jackson AU, Peden JF, Tanaka T, Wild SH, Rudan I, Igl W, Milaneschi Y, Parker AN, Fava C, Chambers JC, Fox ER, Kumari M, Jin Go M, van der Harst P, Hong Linda Kao W, Sjogren M, Vinay DG, Alexander M, Tabara Y, Shaw-Hawkins S, Whincup PH, Liu Y, Shi G, Kuusisto J, Tayo B, Seielstad M, Sim X, Hoang Nguyen KD, Lehtimaki T, Matullo G, Wu Y, Gaunt TR, Charlotte Onland-Moret N, Cooper MN, Platou CG, Org E, Hardy R, Dahgam S, Palmen J, Vitart V, Braund PS, Kuznetsova T, Uiterwaal CS, Adeyemo A, Palmas W, Campbell H, Ludwig B, Tomaszewski M, Tzoulaki I, Palmer ND, Aspelund T, Garcia M, Chang YP, O’Connell JR, Steinle NI, Grobbee DE, Arking DE, Kardia SL, Morrison AC, Hernandez D, Najjar S, McArdle WL, Hadley D, Brown MJ, Connell JM, Hingorani AD, Day IN, Lawlor DA, Beilby JP, Lawrence RW, Clarke R, Hopewell JC, Ongen H, Dreisbach AW, Li Y, Hunter Young J, Bis JC, Kahonen M, Viikari J, Adair LS, Lee NR, Chen MH, Olden M, Pattaro C, Hoffman Bolton JA, Kottgen A, Bergmann S, Mooser V, Chaturvedi N, Frayling TM, Islam M, Jafar TH, Erdmann J, Kulkarni SR, Bornstein SR, Grassler J, Groop L, Voight BF, Kettunen J, Howard P, Taylor A, Guarrera S, Ricceri F, Emilsson V, Plump A, Barroso I, Khaw KT, Weder AB, Hunt SC, Sun YV, Bergman RN, Collins FS, Bonnycastle LL, Scott LJ, Stringham HM, Peltonen L, Perola M, Vartiainen E, Brand SM, Staessen JA, Wang TJ, Burton PR, Soler Artigas M, Dong Y, Snieder H, Wang X, Zhu H, Lohman KK, Rudock ME, Heckbert SR, Smith NL, Wiggins KL, Doumatey A, Shriner D, Veldre G, Viigimaa M, Kinra S, Prabhakaran D, Tripathy V, Langefeld CD, Rosengren A, Thelle DS, Maria Corsi A, Singleton A, Forrester T, Hilton G, McKenzie CA, Salako T, Iwai N, Kita Y, Ogihara T, Ohkubo T, Okamura T, Ueshima H, Umemura S, Eyheramendy S, Meitinger T, Wichmann HE, Shin Cho Y, Kim HL, Lee JY, Scott J, Sehmi JS, Zhang W, Hedblad B, Nilsson P, Davey Smith G, Wong A, Narisu N, Stancakova A, Raffel LJ, Yao J, Kathiresan S, O’Donnell CJ, Schwartz SM, Arfan Ikram M, Longstreth Jr WT, Mosley TH, Seshadri S, Shrine NR, Wain LV, Morken MA, Swift AJ, Laitinen J, Prokopenko I, Zitting P, Cooper JA, Humphries SE, Danesh J, Rasheed A, Goel A, Hamsten A, Watkins H, Bakker SJ, van Gilst WH, Janipalli CS, Radha Mani K, Yajnik CS, Hofman A, Mattace-Raso FU, Oostra BA, Demirkan A, Isaacs A, Rivadeneira F, Lakatta EG, Orru M, Scuteri A, Ala-Korpela M, Kangas AJ, Lyytikainen LP, Soininen P, Tukiainen T, Wurtz P, Twee-Hee Ong R, Dorr M, Kroemer HK, Volker U, Volzke H, Galan P, Hercberg S, Lathrop M, Zelenika D, Deloukas P, Mangino M, Spector TD, Zhai G, Meschia JF, Nalls MA, Sharma P, Terzic J, Kranthi Kumar MV, Denniff M, Zukowska-Szczechowska E, Wagenknecht LE, Gerald RFF, Charchar FJ, Schwarz PE, Hayward C, Guo X, Rotimi C, Bots ML, Brand E, Samani NJ, Polasek O, Talmud PJ, Nyberg F, Kuh D, Laan M, Hveem K, Palmer LJ, van der Schouw YT, Casas JP, Mohlke KL, Vineis P, Raitakari O, Ganesh SK, Wong TY, Shyong Tai E, Cooper RS, Laakso M, Rao DC, Harris TB, Morris RW, Dominiczak AF, Kivimaki M, Marmot MG, Miki T, Saleheen D, Chandak GR, Coresh J, Navis G, Salomaa V, Han BG, Zhu X, Kooner JS, Melander O, Ridker PM, Bandinelli S, Gyllensten UB, Wright AF, Wilson JF, Ferrucci L, Farrall M, Tuomilehto J, Pramstaller PP, Elosua R, Soranzo N, Sijbrands EJ, Altshuler D, Loos RJ, Shuldiner AR, Gieger C, Meneton P, Uitterlinden AG, Wareham NJ, Gudnason V, Rotter JI, Rettig R, Uda M, Strachan DP, Witteman JC, Hartikainen AL, Beckmann JS, Boerwinkle E, Vasan RS, Boehnke M, Larson MG, Jarvelin MR, Psaty BM, Abecasis GR, Chakravarti A, Elliott P, van Duijn CM, Newton-Cheh C, Levy D, Caulfield MJ, Johnson T (2011) Genetic variants in novel pathways influence blood pressure and cardiovascular disease risk. Nature 478:103–109
Wellcome Trust Case Control Consortium (2007) Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature 447(7145):661–678
Chambers JC, Zhang W, Lord GM, van der Harst P, Lawlor DA, Sehmi JS, Gale DP, Wass MN, Ahmadi KR, Bakker SJ, Beckmann J, Bilo HJ, Bochud M, Brown MJ, Caulfield MJ, Connell JM, Cook HT, Cotlarciuc I, Davey Smith G, de Silva R, Deng G, Devuyst O, Dikkeschei LD, Dimkovic N, Dockrell M, Dominiczak A, Ebrahim S, Eggermann T, Farrall M, Ferrucci L, Floege J, Forouhi NG, Gansevoort RT, Han X, Hedblad B, Homan van der Heide JJ, Hepkema BG, Hernandez-Fuentes M, Hypponen E, Johnson T, de Jong PE, Kleefstra N, Lagou V, Lapsley M, Li Y, Loos RJ, Luan J, Luttropp K, Marechal C, Melander O, Munroe PB, Nordfors L, Parsa A, Peltonen L, Penninx BW, Perucha E, Pouta A, Prokopenko I, Roderick PJ, Ruokonen A, Samani NJ, Sanna S, Schalling M, Schlessinger D, Schlieper G, Seelen MA, Shuldiner AR, Sjogren M, Smit JH, Snieder H, Soranzo N, Spector TD, Stenvinkel P, Sternberg MJ, Swaminathan R, Tanaka T, Ubink-Veltmaat LJ, Uda M, Vollenweider P, Wallace C, Waterworth D, Zerres K, Waeber G, Wareham NJ, Maxwell PH, McCarthy MI, Jarvelin MR, Mooser V, Abecasis GR, Lightstone L, Scott J, Navis G, Elliott P, Kooner JS (2010) Genetic loci influencing kidney function and chronic kidney disease. Nat Genet 42(5):373–375
Kottgen A, Glazer NL, Dehghan A, Hwang SJ, Katz R, Li M, Yang Q, Gudnason V, Launer LJ, Harris TB, Smith AV, Arking DE, Astor BC, Boerwinkle E, Ehret GB, Ruczinski I, Scharpf RB, Chen YD, de Boer IH, Haritunians T, Lumley T, Sarnak M, Siscovick D, Benjamin EJ, Levy D, Upadhyay A, Aulchenko YS, Hofman A, Rivadeneira F, Uitterlinden AG, van Duijn CM, Chasman DI, Pare G, Ridker PM, Kao WH, Witteman JC, Coresh J, Shlipak MG, Fox CS (2009) Multiple loci associated with indices of renal function and chronic kidney disease. Nat Genet 41(6):712–717
Kottgen A, Pattaro C, Boger CA, Fuchsberger C, Olden M, Glazer NL, Parsa A, Gao X, Yang Q, Smith AV, O’Connell JR, Li M, Schmidt H, Tanaka T, Isaacs A, Ketkar S, Hwang SJ, Johnson AD, Dehghan A, Teumer A, Pare G, Atkinson EJ, Zeller T, Lohman K, Cornelis MC, Probst-Hensch NM, Kronenberg F, Tonjes A, Hayward C, Aspelund T, Eiriksdottir G, Launer LJ, Harris TB, Rampersaud E, Mitchell BD, Arking DE, Boerwinkle E, Struchalin M, Cavalieri M, Singleton A, Giallauria F, Metter J, de Boer IH, Haritunians T, Lumley T, Siscovick D, Psaty BM, Zillikens MC, Oostra BA, Feitosa M, Province M, de Andrade M, Turner ST, Schillert A, Ziegler A, Wild PS, Schnabel RB, Wilde S, Munzel TF, Leak TS, Illig T, Klopp N, Meisinger C, Wichmann HE, Koenig W, Zgaga L, Zemunik T, Kolcic I, Minelli C, Hu FB, Johansson A, Igl W, Zaboli G, Wild SH, Wright AF, Campbell H, Ellinghaus D, Schreiber S, Aulchenko YS, Felix JF, Rivadeneira F, Uitterlinden AG, Hofman A, Imboden M, Nitsch D, Brandstatter A, Kollerits B, Kedenko L, Magi R, Stumvoll M, Kovacs P, Boban M, Campbell S, Endlich K, Volzke H, Kroemer HK, Nauck M, Volker U, Polasek O, Vitart V, Badola S, Parker AN, Ridker PM, Kardia SL, Blankenberg S, Liu Y, Curhan GC, Franke A, Rochat T, Paulweber B, Prokopenko I, Wang W, Gudnason V, Shuldiner AR, Coresh J, Schmidt R, Ferrucci L, Shlipak MG, van Duijn CM, Borecki I, Kramer BK, Rudan I, Gyllensten U, Wilson JF, Witteman JC, Pramstaller PP, Rettig R, Hastie N, Chasman DI, Kao WH, Heid IM, Fox CS (2010) New loci associated with kidney function and chronic kidney disease. Nat Genet 42(5):376–384
Pattaro C, De Grandi A, Vitart V, Hayward C, Franke A, Aulchenko YS, Johansson A, Wild SH, Melville SA, Isaacs A, Polasek O, Ellinghaus D, Kolcic I, Nothlings U, Zgaga L, Zemunik T, Gnewuch C, Schreiber S, Campbell S, Hastie N, Boban M, Meitinger T, Oostra BA, Riegler P, Minelli C, Wright AF, Campbell H, van Duijn CM, Gyllensten U, Wilson JF, Krawczak M, Rudan I, Pramstaller PP (2010) A meta-analysis of genome-wide data from five European isolates reveals an association of COL22A1, SYT1, and GABRR2 with serum creatinine level. BMC Med Genet 11:41
Kottgen A (2010) Genome-wide association studies in nephrology research. Am J Kidney Dis 56(4):743–758
Sheikh-Hamad D (2010) Mammalian stanniocalcin-1 activates mitochondrial antioxidant pathways: new paradigms for regulation of macrophages and endothelium. Am J Physiol Renal Physiol 298(2):F248–F254
Wang Y, Huang L, Abdelrahim M, Cai Q, Truong A, Bick R, Poindexter B, Sheikh-Hamad D (2009) Stanniocalcin-1 suppresses superoxide generation in macrophages through induction of mitochondrial UCP2. J Leukoc Biol 86(4):981–988
Saemann MD, Weichhart T, Zeyda M, Staffler G, Schunn M, Stuhlmeier KM, Sobanov Y, Stulnig TM, Akira S, von Gabain A, von Ahsen U, Horl WH, Zlabinger GJ (2005) Tamm-Horsfall glycoprotein links innate immune cell activation with adaptive immunity via a Toll-like receptor-4-dependent mechanism. J Clin Invest 115(2):468–475
Kottgen A, Hwang SJ, Larson MG, Van Eyk JE, Fu Q, Benjamin EJ, Dehghan A, Glazer NL, Kao WH, Harris TB, Gudnason V, Shlipak MG, Yang Q, Coresh J, Levy D, Fox CS (2010) Uromodulin levels associate with a common UMOD variant and risk for incident CKD. J Am Soc Nephrol 21(2):337–344
Padmanabhan S, Melander O, Johnson T, Di Blasio AM, Lee WK, Gentilini D, Hastie CE, Menni C, Monti MC, Delles C, Laing S, Corso B, Navis G, Kwakernaak AJ, van der Harst P, Bochud M, Maillard M, Burnier M, Hedner T, Kjeldsen S, Wahlstrand B, Sjogren M, Fava C, Montagnana M, Danese E, Torffvit O, Hedblad B, Snieder H, Connell JM, Brown M, Samani NJ, Farrall M, Cesana G, Mancia G, Signorini S, Grassi G, Eyheramendy S, Wichmann HE, Laan M, Strachan DP, Sever P, Shields DC, Stanton A, Vollenweider P, Teumer A, Volzke H, Rettig R, Newton-Cheh C, Arora P, Zhang F, Soranzo N, Spector TD, Lucas G, Kathiresan S, Siscovick DS, Luan J, Loos RJ, Wareham NJ, Penninx BW, Nolte IM, McBride M, Miller WH, Nicklin SA, Baker AH, Graham D, McDonald RA, Pell JP, Sattar N, Welsh P, Munroe P, Caulfield MJ, Zanchetti A, Dominiczak AF (2010) Genome-wide association study of blood pressure extremes identifies variant near UMOD associated with hypertension. PLoS Genet 6(10):e1001177
Ikram MK, Sim X, Jensen RA, Cotch MF, Hewitt AW, Ikram MA, Wang JJ, Klein R, Klein BE, Breteler MM, Cheung N, Liew G, Mitchell P, Uitterlinden AG, Rivadeneira F, Hofman A, de Jong PT, van Duijn CM, Kao L, Cheng CY, Smith AV, Glazer NL, Lumley T, McKnight B, Psaty BM, Jonasson F, Eiriksdottir G, Aspelund T, Harris TB, Launer LJ, Taylor KD, Li X, Iyengar SK, Xi Q, Sivakumaran TA, Mackey DA, Macgregor S, Martin NG, Young TL, Bis JC, Wiggins KL, Heckbert SR, Hammond CJ, Andrew T, Fahy S, Attia J, Holliday EG, Scott RJ, Islam FM, Rotter JI, McAuley AK, Boerwinkle E, Tai ES, Gudnason V, Siscovick DS, Vingerling JR, Wong TY (2010) Four novel Loci (19q13, 6q24, 12q24, and 5q14) influence the microcirculation in vivo. PLoS Genet 6(10):e1001184
Turner ST, Kardia SL, Mosley TH, Rule AD, Boerwinkle E, de Andrade M (2006) Influence of genomic loci on measures of chronic kidney disease in hypertensive sibships. J Am Soc Nephrol 17(7):2048–2055
Chakraborty R, Weiss KM (1988) Admixture as a tool for finding linked genes and detecting that difference from allelic association between loci. Proc Nat Acad Sci 85(23):9119–9123
Kao WH, Klag MJ, Meoni LA, Reich D, Berthier-Schaad Y, Li M, Coresh J, Patterson N, Tandon A, Powe NR, Fink NE, Sadler JH, Weir MR, Abboud HE, Adler SG, Divers J, Iyengar SK, Freedman BI, Kimmel PL, Knowler WC, Kohn OF, Kramp K, Leehey DJ, Nicholas SB, Pahl MV, Schelling JR, Sedor JR, Thornley-Brown D, Winkler CA, Smith MW, Parekh RS (2008) MYH9 is associated with nondiabetic end-stage renal disease in African Americans. Nat Genet 40(10):1185–1192
Kopp JB, Smith MW, Nelson GW, Johnson RC, Freedman BI, Bowden DW, Oleksyk T, McKenzie LM, Kajiyama H, Ahuja TS, Berns JS, Briggs W, Cho ME, Dart RA, Kimmel PL, Korbet SM, Michel DM, Mokrzycki MH, Schelling JR, Simon E, Trachtman H, Vlahov D, Winkler CA (2008) MYH9 is a major-effect risk gene for focal segmental glomerulosclerosis. Nat Genet 40(10):1175–1184
Genovese G, Friedman DJ, Ross MD, Lecordier L, Uzureau P, Freedman BI, Bowden DW, Langefeld CD, Oleksyk TK, Uscinski Knob AL, Bernhardy AJ, Hicks PJ, Nelson GW, Vanhollebeke B, Winkler CA, Kopp JB, Pays E, Pollak MR (2010) Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science 329(5993):841–845
Pollak MR (2008) Kidney disease and African ancestry. Nat Genet 40(10):1145–1146
Seri M, Pecci A, Di Bari F, Cusano R, Savino M, Panza E, Nigro A, Noris P, Gangarossa S, Rocca B, Gresele P, Bizzaro N, Malatesta P, Koivisto PA, Longo I, Musso R, Pecoraro C, Iolascon A, Magrini U, Rodriguez Soriano J, Renieri A, Ghiggeri GM, Ravazzolo R, Balduini CL, Savoia A (2003) MYH9-related disease: May-Hegglin anomaly, Sebastian syndrome, Fechtner syndrome, and Epstein syndrome are not distinct entities but represent a variable expression of a single illness. Medicine 82(3):203–215
Ghiggeri GM, Caridi G, Magrini U, Sessa A, Savoia A, Seri M, Pecci A, Romagnoli R, Gangarossa S, Noris P, Sartore S, Necchi V, Ravazzolo R, Balduini CL (2003) Genetics, clinical and pathological features of glomerulonephritis associated with mutations of nonmuscle myosin IIA (Fechtner syndrome). Am J Kidney Dis 41(1):95–104
Johnstone DB, Zhang J, George B, Leon C, Gachet C, Wong H, Parekh R, Holzman LB (2011) Podocyte-specific deletion of Myh9 encoding nonmuscle myosin heavy chain 2A predisposes mice to glomerulopathy. Mol Cell Biol 31(10):2162–2170
Tzur S, Rosset S, Shemer R, Yudkovsky G, Selig S, Tarekegn A, Bekele E, Bradman N, Wasser WG, Behar DM, Skorecki K (2010) Missense mutations in the APOL1 gene are highly associated with end-stage kidney disease risk previously attributed to the MYH9 gene. Hum Genet 128(3):345–350
Zuk O, Hechter E, Sunyaev SR, Lander ES (2012) The mystery of missing heritability: genetic interactions create phantom heritability. Proc Nat Acad Sci (in press) PMID: 22223662
Shao H, Burrage LC, Sinasac DS, Hill AE, Ernest SR, O’Brien W, Courtland HW, Jepsen KJ, Kirby A, Kulbokas EJ, Daly MJ, Broman KW, Lander ES, Nadeau JH (2008) Genetic architecture of complex traits: large phenotypic effects and pervasive epistasis. Proc Natl Acad Sci USA 105(50):19910–19914
Crow JF (2010) On epistasis: why it is unimportant in polygenic directional selection. Philos Trans R Soc Lond B Biol Sci 365(1544):1241–1244
Van Dijk SJ, Specht PA, Lazar J, Jacob HJ, Provoost AP (2006) Synergistic QTL interactions between Rf-1 and Rf-3 increase renal damage susceptibility in double congenic rats. Kidney Int 69(8):1369–1376
Das R, Hampton DD, Jirtle RL (2009) Imprinting evolution and human health. Mamm Genome 20(9–10):563–572
Moore T, Haig D (1991) Genomic imprinting in mammalian development: a parental tug-of-war. Trends Genet 7(2):45–49
Kucharski R, Maleszka J, Foret S, Maleszka R (2008) Nutritional control of reproductive status in honeybees via DNA methylation. Science 319(5871):1827–1830
Nelson VR, Spiezio SH, Nadeau JH (2010) Transgenerational genetic effects of the paternal Y chromosome on daughters’ phenotypes. Epigenomics 2(4):513–521
Dunn GA, Bale TL (2011) Maternal high-fat diet effects on third-generation female body size via the paternal lineage. Endocrinology 152(6):2228–2236
Grindstaff JL, Hasselquist D, Nilsson JK, Sandell M, Smith HG, Stjernman M (2006) Transgenerational priming of immunity: maternal exposure to a bacterial antigen enhances offspring humoral immunity. Proc Biol Sci 273(1600):2551–2557
Hasselquist D, Nilsson JA (2009) Maternal transfer of antibodies in vertebrates: trans-generational effects on offspring immunity. Philos Trans R Soc Lond B Biol Sci 364(1513):51–60
Reid JM, Arcese P, Keller LF, Hasselquist D (2006) Long-term maternal effect on offspring immune response in song sparrows Melospiza melodia. Biol Lett 2(4):573–576
Sadd BM, Kleinlogel Y, Schmid-Hempel R, Schmid-Hempel P (2005) Trans-generational immune priming in a social insect. Biol Lett 1(4):386–388
Greeley SA, Katsumata M, Yu L, Eisenbarth GS, Moore DJ, Goodarzi H, Barker CF, Naji A, Noorchashm H (2002) Elimination of maternally transmitted autoantibodies prevents diabetes in nonobese diabetic mice. Nat Med 8(4):399–402
Yamashita T, Freigang S, Eberle C, Pattison J, Gupta S, Napoli C, Palinski W (2006) Maternal immunization programs postnatal immune responses and reduces atherosclerosis in offspring. Circ Res 99(7):e51–e64
Lundin BS, Dahlman-Hoglund A, Pettersson I, Dahlgren UI, Hanson LA, Telemo E (1999) Antibodies given orally in the neonatal period can affect the immune response for two generations: evidence for active maternal influence on the newborn’s immune system. Scand J Immunol 50(6):651–656
Matson AP, Thrall RS, Rafti E, Puddington L (2009) Breastmilk from allergic mothers can protect offspring from allergic airway inflammation. Breastfeeding Med 4(3):167–174
Polte T, Hansen G (2008) Maternal tolerance achieved during pregnancy is transferred to the offspring via breast milk and persistently protects the offspring from allergic asthma. Clin Exp Allergy 38(12):1950–1958
Lange H, Kiesch B, Linden I, Otto M, Thierse HJ, Shaw L, Maehnss K, Hansen H, Lemke H (2002) Reversal of the adult IgE high responder phenotype in mice by maternally transferred allergen-specific monoclonal IgG antibodies during a sensitive period in early ontogeny. Eur J Immunol 32(11):3133–3141
Jerne NK (1985) The generative grammar of the immune system. Science 229(4718):1057–1059
Lefranc MP, Clement O, Kaas Q, Duprat E, Chastellan P, Coelho I, Combres K, Ginestoux C, Giudicelli V, Chaume D, Lefranc G (2005) IMGT-Choreography for immunogenetics and immunoinformatics. In Silico Biol 5(1):45–60
Teng G, Papavasiliou FN (2007) Immunoglobulin somatic hypermutation. Annu Rev Genet 41:107–120
Hopkin J, Cookson W (2006) Genetic variation in the beta subunit of the high affinity IgE receptor and atopy and asthma. Clin Exp Allergy 36(7):855–857
Weidinger S, Gieger C, Rodriguez E, Baurecht H, Mempel M, Klopp N, Gohlke H, Wagenpfeil S, Ollert M, Ring J, Behrendt H, Heinrich J, Novak N, Bieber T, Kramer U, Berdel D, von Berg A, Bauer CP, Herbarth O, Koletzko S, Prokisch H, Mehta D, Meitinger T, Depner M, von Mutius E, Liang L, Moffatt M, Cookson W, Kabesch M, Wichmann HE, Illig T (2008) Genome-wide scan on total serum IgE levels identifies FCER1A as novel susceptibility locus. PLoS Genet 4(8):e1000166
Cierpial MA, McCarty R (1987) Hypertension in SHR rats: contribution of maternal environment. Am J Physiol 253(4 Pt 2):H980–H984
Di Nicolantonio R, Koutsis K, Westcott KT, Wlodek ME (2006) Relative contribution of the prenatal versus postnatal period on development of hypertension and growth rate of the spontaneously hypertensive rat. Clin Exp Pharmacol Physiol 33(1–2):9–16
Lee JY, Azar SH (2010) Wistar-Kyoto and spontaneously hypertensive rat blood pressure after embryo transfer into different wombs and cross-suckling. Exp Biol Med (Maywood) 235(11):1375–1384
Herring SM, Gokul N, Monita M, Bell R, Boerwinkle E, Wenderfer SE, Braun MC, Doris PA (2011) Immunoglobulin locus associates with serum IgG levels and albuminuria. J Am Soc Nephrol 22(5):881–889
Oxelius VA (2008) Immunoglobulin constant heavy G subclass chain genes in asthma and allergy. Immunol Res 40(2):179–191
Puttick AH, Briggs DC, Welsh KI, Williamson EA, Jacoby RK, Jones VE (1990) Genes associated with rheumatoid arthritis and mild inflammatory arthritis. II. Association of HLA with complement C3 and immunoglobulin Gm allotypes. Ann Rheum Dis 49(4):225–228
Schernthaner G, Mayr WR (1984) Immunoglobulin allotype markers and HLA DR genes in type I diabetes mellitus. Metabolism 33(9):833–836
Field LL (1991) Non-HLA region genes in insulin dependent diabetes mellitus. Baillieres Clin Endocrinol Metab 5(3):413–438
Field LL, Stephure DK, McArthur RG (1991) Interaction between T cell receptor beta chain and immunoglobulin heavy chain region genes in susceptibility to insulin-dependent diabetes mellitus. Am J Hum Genet 49(3):627–634
Pandey JP (2010) Genome-wide association studies and assessment of risk of disease. N Engl J Med 363(21):2076–2077
Acknowledgments
The author is grateful to Stacy Herring for technical assistance and for the following research grants NIH R01 DK069632 (to PAD) R01 DK081866 (to PAD) and AHA 09GRNT2240045 (to PAD).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Doris, P.A. Genetic susceptibility to hypertensive renal disease. Cell. Mol. Life Sci. 69, 3751–3763 (2012). https://doi.org/10.1007/s00018-012-0996-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-012-0996-3