Abstract
The surface-expressed transmembrane CX3C chemokine ligand 1 (CX3CL1/fractalkine) induces firm adhesion of leukocytes expressing its receptor CX3CR1. After shedding by the disintegrins and metalloproteinases (ADAM) 10 and 17, CX3CL1 also acts as soluble leukocyte chemoattractant. Here, we demonstrate that transmembrane CX3CL1 expressed on both endothelial and epithelial cells induces leukocyte transmigration. To investigate the underlying mechanism, we generated CX3CR1 variants lacking the intracellular aspartate-arginine-tyrosine (DRY) motif or the intracellular C-terminus which led to a defect in intracellular calcium response and impaired ligand uptake, respectively. While both variants effectively mediated firm cell adhesion, they failed to induce transmigration and rather mediated retention of leukocytes on the CX3CL1-expressing cell layer. Targeting of ADAM10 led to increased adhesion but reduced transmigration in response to transmembrane CX3CL1, while transmigration towards soluble CX3CL1 was not affected. Thus, transmembrane CX3CL1 mediates leukocyte transmigration via the DRY motif and C-terminus of CX3CR1 and the activity of ADAM10.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Recruitment of leukocytes to sites of inflammation is a multistep process governed by cytokines, adhesion molecules, and chemokines [1]. In vivo data from mice and humans demonstrate that the chemokine CX3CL1 (fractalkine) contributes to leukocyte recruitment and thereby promotes the progression of inflammatory diseases such as atherosclerosis [2–5]. CX3CL1 is expressed as a cell-surface protein on dendritic, epithelial, neuronal, smooth-muscle, and endothelial cells [6]. The molecule consists of a chemokine domain, a highly glycosylated mucin-like stalk, a transmembrane domain, and a short cytoplasmic tail [7]. The ectodomain of CX3CL1 can be released from the cell surface by proteolytic cleavage involving the membrane-expressed disintegrin and metalloproteinase 10 (ADAM10) and ADAM17 [8, 9].
CX3CL1 binds to a single receptor (CX3CR1) that is expressed on several leukocyte subsets including monocytes, NK cells, T cell populations, and microglia [10–12]. CX3CR1 belongs to the group of G protein-coupled heptahelical receptors (GPCR). Throughout the GPCR super-family, several highly conserved motifs have been identified. The DRY (aspartate-arginine-tyrosine) sequence in the second intracellular loop is required for activation of inhibitory G (Gi) proteins [13, 14] whereas the NPX(2-3)Y [asparagine-proline-X(2-3)-tyrosine, X = leucine, isoleucine, valine] motif located in the seventh transmembrane region of most GPCR contributes to ligand binding, activation and internalization of the receptor [15, 16]. Additionally, GPCR typically carry several Ser-residues within the intracellular C-terminal region which can become phosphorylated by G protein-coupled receptor kinases and mediate interaction with β-arrestin and desensitization of the receptor towards its ligand [17]. The typical DRY sequence, the NPX(2-3)Y motif and several C-terminal Ser-residues are also found within CX3CR1 and likely play a role in CX3CR1 signaling and function.
Transmembrane as well as soluble CX3CL1 bind to CX3CR1 and contribute to leukocyte recruitment. However, both CX3CL1 variants mediate different steps of the recruitment process and employ distinct mechanisms. Transmembrane CX3CL1 serves as an adhesion molecule mediating enhanced leukocyte adhesion to endothelial cells under flow conditions. This activity is largely independent of CX3CR1-mediated Gi protein activation and predominantly a result of the physical interaction of the transmembrane chemokine with its receptor [12, 18–20]. This interaction can be resolved by regulated cleavage of the chemokine leading to the detachment of bound cells [21]. By contrast, soluble CX3CL1 acts as a chemoattractant inducing directional cell migration via CX3CR1 signaling and activation of Gi proteins [12]. As shown by mutation of murine CX3CR1, the DRY motif is required for CX3CR1-induced chemotaxis [19].
To date, in vitro studies have only addressed adhesion by transmembrane CX3CL1 and migration by soluble recombinant CX3CL1. Here, we examined transcellular migration of leukocytes in response to transmembrane CX3CL1 and elucidate details of the involved mechanisms. We demonstrate that transmembrane CX3CL1, when expressed on cytokine-stimulated umbilical vein endothelial cells (HUVEC) or on immortalized CX3CL1-transfected bladder carcinoma epithelial cells (ECV304), not only induces adhesion but also transcellular migration of leukocytes. In contrast to cell adhesion, transmigration requires signaling of CX3CR1 by the DRY motif and integrity of the receptor’s C-terminus. In addition to CX3CR1 signaling, proteolytic activity of ADAM10 is required for CX3CL1-induced transmigration, as shown by inhibition and transcriptional silencing of the protease, indicating that proteolytic cleavage is necessary to release the adherent leukocytes to allow CX3CL1-induced transmigration.
Materials and methods
Recombinant proteins, antibodies, fluorescent dyes, media, inhibitors
Recombinant human CX3CL1 (chemokine domain), human CC-chemokine ligand 2 (CCL2), human IFN-γ and human TNF-α were obtained from Peprotech (Hamburg, Germany). Alexa-Fluor647-labeled CX3CL1 chemokine domain was from Almac (Craigavon, Ireland). PE-conjugated rat monoclonal antibody against human CX3CR1 (IgG2bκ) (clone 2A9-1) was obtained from MBL (Woburn, MA, USA), isotype control phycoerythrin (PE)-conjugated rat IgG2bκ (clone RTK4530) was from Abcam (Cambridge, UK), and PE-conjugated anti-hIgG1-Fc antibody was from Jackson (Newmarket, UK). Mouse monoclonal antibodies against human ADAM10 (clone 163003) and ADAM17 (clone 111633), respectively, as well as mouse IgG2b and IgG1 isotype controls were obtained from R&D Systems (Wiesbaden, Germany). PE-conjugated anti-mouse antibody was from Jackson. Neutralizing monoclonal antibodies to CX3CL1 (clone 51637), ICAM-1 (clone BBIG-I1) and IgG1 isotype control (clone 11711) were obtained from R&D Systems. Fluo-3-acetoxymethylester (Fluo-3-AM) and CalceinAM were from Molecular Probes (Leiden, Netherlands). Media (RPMI1640, DMEM, M199), fetal calf serum (FCS) and bovine serum albumin (BSA) were from PAA (Pasching, Austria). Low serum endothelial cell growth medium including supplements was from Promocell (Heidelberg, Germany). The metalloproteinase inhibitors GW280264X and GI254023X were described previously [9]. Pertussis toxin was purchased from Calbiochem (Hamburg, Germany).
DNA constructs
Human CX3CR1 cDNA was amplified from human peripheral blood mononuclear cells (PBMC) using the following primers: 5′-GAATTCACCATGGATCAGTTCCCTGAATCAGT-3′ (CX3CR1 sense) and 5′-CTCGAGTCAGAGAAGGAGCAATGCATCTCCATCA-3′ (CX3CR1 antisense). cDNA for the truncation variant (S319X) was generated by using an antisense primer with stop codon: 5′-CGGTGAAGAATATGCTTCCAAAAAAGCCGTA-3′. cDNA for other receptor variants was generated by site-directed mutagenesis via ligation PCR. An upstream fragment was amplified using the CX3CR1 sense primer and the following antisense primers: 5′-CGGTGATGAAGAATATGCTTCCAAAAAAGCCGTA-3′ (for R127N) and 5′-CAACAATGGCTAAATGCAACCGTCT-3′ (for N289A and Y293A). A downstream fragment was generated with antisense primer for CX3CR1 and sense primers carrying the desired mutations as follows: 5′-TCATCAGCATTGATAACTACCTGG-CCATCGTCCT-3′ (for R127N), 5′-CCTGG-CTCCTCTCATCTATGCATTT-3′ (for N289A) or 5′-CCTGAATCCTCTCATCGCTGCATTT-3′ (for Y293A). The upstream and downstream PCR products were phosphorylated and ligated before a PCR with CX3CR1 sense and antisense primers was performed. The cDNA was then inserted into pcDNA3.1 (+) (Invitrogen, Karlsruhe, Germany) using EcoRI and XhoI. An expression vector for the fusion protein of human CX3CL1 and human IgG1-Fc-fragment (hFc) was generated by insertion of cDNA coding for hFc into pcDNA3.1 using EcoRI and XhoI. Subsequently, a cDNA fragment for the ectodomain of human CX3CL1 was generated by PCR using 5′-GAATTCCACCATGGATCAGTTCCCTG-3′ (sense primer) and 5′-GAATTCTTCCTGGGAAGAA-3′ (antisense primer) and then inserted into pcDNA3.1-Fc using HindIII and EcoRI. All sequences were confirmed by sequencing (MWG Biotech, Germany).
The lentiviral expression vector pLVTHM was used to generate lentiviral particles for the expression of short hairpin RNA (shRNA) targeting ADAM10 and ADAM17 as described previously [22].
Cell preparation, culture, and transfection
Primary umbilical vein endothelial cells (HUVEC) were freshly isolated from human umbilical veins by filling the vein with collagenase type II solution (40 μg/ml in PBS, Sigma, Munich, Germany) and incubating for 15 min at 37°C. After washing with 50 ml PBS, cells were resuspended in supplemented HUVEC growth medium and seeded on collagen G-coated (Biochrom, Berlin, Germany) cell culture dishes. HUVEC were subcultured before reaching confluence for maximal four passages. HUVEC were stimulated with IFN-γ and TNF-α (10 ng/ml each) for 16 h to induce CX3CL1 expression. Human PBMC were isolated from citrated (0.38%) venous blood of healthy volunteers by 1:1 dilution in PBS and subsequent density gradient centrifugation on a Ficoll Hypaque layer (Pan Biotech, Aidenbach, Germany) for 40 min at RT. After twofold washing with PBS, PBMC were used for transmigration or adhesion assays as described below. The presence of CX3CR1 on monocytes and T cell subsets was confirmed by flow cytometry. Human embryonic kidney cells (HEK293) were grown in DMEM medium supplemented with 10% FCS and antibiotics. Transfection was carried out with Lipofectamine (Invitrogen, Karlsruhe, Germany) according to the manufacturer’s instructions. The murine pre-B cell line L1.2 (Massachusetts Association of Technology Transfer, Tufts University, Boston, MA, USA) was grown in RPMI1640 medium supplemented with 10% FCS, 1% pyruvate, 1% HEPES, β-mercaptoethanol and gentamycin. Transfection was carried out using AMAXA kit V (program P16; AMAXA, Cologne, Germany) according to the manufacturer’s instructions. Stably transfected cells were selected with 1 mg/ml G418 and single clones were established by limited dilution. The adherent human bladder carcinoma cell line ECV304 (derivative of epithelial bladder carcinoma cell line T-24, DSMZ, Braunschweig, Germany) [23] was stably transfected with CX3CL1 (CX3CL1–ECV304) as previously described and cultured in M199 medium supplemented with 10% FCS [9].
Recombinant lentiviral particles were produced by transient transfection of 293T packaging cells according to standard protocols. ECV304 cells were transduced using virus particle-containing 293T cell supernatant as described [22].
CX3CL1 cleavage assays
Wild-type (WT-) or CX3CL1-expressing ECV304 cells (CX3CL1-ECV304) were grown to confluence in 24-well cell culture dishes and incubated in the absence or presence of PBMC or L1.2 cells (200,000 cells per well) for 3 h. Surface expression of CX3CL1 on ECV304 cells was determined by flow cytometry. Conditioned media and cell lysates were analyzed for the presence of soluble and transmembrane CX3CL1, respectively. Quantification was carried out by enzyme-linked immunosorbent assay (ELISA) as described previously [9].
Flow cytometric analysis
Cells were analyzed for CX3CR1 expression by staining with a PE-conjugated anti-hCX3CR1 rat monoclonal antibody. ADAM10 and ADAM17 surface expression was examined using mouse monoclonal antibodies (1 and 5 μg/ml, respectively) and a PE-conjugated anti-mouse antibody (5 μg/ml). Binding assays were performed using soluble CX3CL1-Fc-construct (see above), which was then detected with a PE-conjugated anti-Fc-antibody (5 μg/ml). The fluorescence signal was analyzed by flow cytometry (FACSCalibur or FACSCanto, Becton-Dickinson, Heidelberg, Germany).
Ligand uptake
For ligand-uptake experiments, HEK293 cells expressing the indicated receptor variants were harvested and resuspended in PBS at 5 × 106 cells/ml. Prior to CX3CL1-treatment, cells were left on ice for 30 min with or without 0.2% NaN3. Cells were then incubated with 10 nM AlexaFluor647-labeled CX3CL1 chemokine domain at 4°C or 30 min. Cells were washed with ice-cold PBS or PBS containing 0.2% NaN3 and the fluorescence signal was measured by flow cytometry.
Intracellular calcium transients
HEK293 cells were resuspended in PBS to 5 × 106 cells/ml and loaded with 4 μg/ml of the calcium-indicator Fluo-3-AM for 30 min at 37°C. After twofold washing, cells were kept in calcium assay buffer (138 mM NaCl, 6 mM KCl, 1 mM MgCl2, 5.5 mM d-Glucose, 20 mM HEPES, 1.6 mM CaCl2, pH 7.4) supplemented with 1% FCS. Before measurement, 2.5 × 106 cells were resuspended in 1.5 ml assay buffer containing no calcium but 0.3 mM EDTA. Cells were incubated in a plastic cuvette at 37°C under constant stirring and Fluo-3-AM fluorescence was continuously monitored at excitation and emission wavelengths of 490 and 526 nm, respectively, using a Cary Eclipse fluorescence spectrophotometer (Varian, Palo Alto, CA, USA). After 1 min, cells were stimulated with 10 nM CX3CL1-chemokine domain. Finally, calcium (1.6 mM) and digitonin (125 μg/ml) were added leading to maximal loading of Fluo-3-AM, followed by addition of EGTA (15 mM) for dissolving the complex.
Adhesion
Static cell adhesion via CX3CL1 was measured as described previously [9]. For adhesion under flow conditions, ECV304 cells or HUVEC were seeded onto a flow adhesion chamber (μ-slide VI, IBIDi, Munich, Germany) and cultured to full confluence. HEK293 cells expressing the indicated receptor variants or freshly isolated PBMC were stained with CalceinAM, washed with PBS, and resuspended in flow adhesion buffer (10% HBSS, 1% HEPES, 1% BSA, pH 7.4) to 5 × 105 cells/ml. The flow adhesion chamber containing the ECV304 or HUVEC cell layer was then connected to a syringe pump (Landgraf Laborsysteme, Langenhagen, Germany) and inserted into a temperature-controlled incubation chamber on the stage of an inverted microscope (Leica DM-IRB, Leica, Wetzlar, Germany). After washing with warm flow adhesion buffer for 3 min, the cell layer was perfused by a suspension of calcein-labeled cells with a shear stress rate of 2 or 5 dyne/cm2 for 1 min. Thereafter, eight subsequent photographs (each depicting an area of 3.2 mm2) were taken and the number of adherent cells was determined. The results were expressed as adhesion index, which was calculated by expressing the number of adherent cells in relation to the control (adhesion in the absence of stimulus, which was about 5–20 cells per 10 μm2 depending on the donor).
Chemotaxis
Stably transfected L1.2 cells expressing the indicated receptor variants or freshly isolated PBMC were washed with PBS and resuspended at 2 × 106 cells/ml in RPMI1640 with 0.2% BSA. The lower wells of a modified 48-well Boyden chamber (Neuroprobe, Gaithersburg, MD, USA) were filled with 29.5 μl RPMI1640/0.2% BSA with or without the indicated concentrations of CX3CL1 chemokine domain, covered with a polycarbonate membrane (Neuroprobe, Gaithersburg, MD, USA) with 8-μm pores, and 30 μl of cell suspension was added to the upper wells. After incubation for 2 h at 37°C, migrated cells were counted using a hemocytometer. The results were expressed as chemotaxis index calculated as the number of migrated cells in the presence of stimulus in relation to the number of migrated cells in the absence of stimulus, which was typically between 3,000 and 10,000 cells per well depending on the donor.
Transmigration
Wt- or CX3CL1-ECV304 cells or HUVEC were seeded on transwell filters (8-μm pores, Costar Corning, Schiphol-Rijk, Netherlands) and grown to confluence. Lower wells were filled with 600 μl/well RPMI1640/0.2% BSA with or without the indicated concentrations of CX3CL1 chemokine domain. Transwell inserts containing the ECV304 cell or HUVEC layer were then placed into the wells and filled with 100 μl of L1.2 or PBMC cell suspension (2 × 106 cells/ml in RPMI1640/0.2% BSA). After incubation for 2 h at 37°C, the migrated cells were counted using a hemocytometer. The results were presented as transmigration index representing the number of migrated cells in the presence of stimulus in relation to the number of migrated cells in the absence of stimulus which was typically between 3,000 and 10,000 cells per well depending on the donor.
Before the transmigration assays, permeability of the cell layer was controlled using fluorescein isothiocyanate (FITC)-labeled dextran (MW 40,000, Sigma, Munich, Germany) that was added to the upper chamber at a concentration of 0.1 mg/ml. After 2 h, FITC-dextran in the lower chamber was quantified by measuring fluorescence intensity at 485-nm excitation and 535-nm emission wavelength (Tecan, Crailsheim, GER). In transmigration experiments, permeability was below 20% for HUVEC and below 12% for ECV304 cells compared to the maximal diffusion of FITC-dextran in the absence of any cell layer.
Statistics
Data were statistically analyzed using the one-way analysis of variance with posthoc Bonferroni’s multiple comparison t tests using GraphPad Prism software (GraphPad Prism 5.01, GraphPad Software, San Diego, CA, USA). In case of heteroscedasticity (Bartlett test), data were log-transformed prior to analysis. Data were statistically analyzed using one-way analysis of variance followed by two-sided t tests (GraphPad Prism). The data in Fig. 3b and the data in Fig. 4b were analyzed by the Mixed Model procedure in SAS 9.1 (SAS Institute, Cary, NC, USA). Multiple comparisons were corrected by the Bonferroni–Holm procedure. In the figures, only those comparisons with interest to the main hypotheses are indicated.
Results
Transmembrane CX3CL1 mediates PBMC transmigration through cultured bladder carcinoma epithelial cells
Previous work has demonstrated that the soluble ectodomain of human CX3CL1 induces migration of freshly isolated PBMC [7, 24], whereas transmembrane CX3CL1 when expressed on a confluent layer of ECV304 cells (derivative of the epithelial bladder carcinoma cell line T-24, [23]) promotes PBMC adhesion [9, 12]. We thought to determine whether transmembrane CX3CL1 would also mediate PBMC transmigration through the cell monolayers. To this end, PBMC were seeded onto wt- or CX3CL1-ECV304 cells, which were grown to confluence on transwell filters. For removal of free soluble CX3CL1, cells were washed and transferred into fresh medium. Transmigration was then studied in the absence or presence of recombinant soluble CX3CL1 that was added to the lower compartment. As expected, transmigration of PBMC was increased when soluble CX3CL1 was used as a chemoattractant (Fig. 1a). The magnitude of this response was comparable to that induced by CCL2, which was used as a positive control (transmigration index of 2–3, data not shown). Interestingly, transmigration was also increased when transmembrane CX3CL1 was expressed on the ECV304 cell layer, even when the free soluble CX3CL1 had been removed (Fig. 1a). Simultaneous presence of transmembrane and soluble CX3CL1 did not further enhance transmigration.
Transmembrane CX3CL1 promotes transmigration. a Wt- or CX3CL1-ECV304 cells were grown in transwell inserts and washed to remove free CX3CL1. As a control, recombinant soluble CX3CL1 was again added to the lower transwell compartment. Subsequently, cells were assayed for transmigration of freshly prepared PBMC that were added to the upper transwell compartment. PBMC that transmigrated into the lower compartment were counted and results were expressed as transmigration index representing the fold increase over random migration. b Wt- or CX3CL1-ECV304 cells were pretreated with recombinant soluble CX3CL1 (10 nM) that was added to the upper transwell compartment. After 1 h, cells were washed and assayed for transmigration of PBMC in the absence or presence of recombinant soluble CX3CL1 in the lower compartment. c HUVEC were left unstimulated or stimulated with IFN-γ and TNF-α (both 10 ng/ml) for 16 h and subsequently treated with neutralizing antibodies against CX3CL1 and ICAM-1 or isotype control (10 μg/ml each) for 1 h. After washing to remove free antibody, HUVEC were transferred into fresh medium and assayed for PBMC transmigration. Data are shown as mean plus SD of three independent experiments. The asterisks indicate statistically significant differences versus the controls (untransfected, unstimulated or isotype, respectively, p < 0.05)
Since soluble chemokines can bind to surface-expressed proteoglycans and are thereby presented to leukocytes [25], we examined whether soluble CX3CL1 was immobilized to regulate the transmigratory response. ECV304 cells were pretreated with soluble CX3CL1 and subsequently washed to remove free chemokine. For the pretreatment, a dosage of 10 nM CX3CL1 was chosen, which would yield an optimal migratory response when added as soluble chemoattractant to the lower compartment. However, this pretreatment neither led to immobilization of the chemokine on the cell surface according to immunofluorescence staining of fixed and permeabilized cells (data not shown) nor did it increase transmigration of PBMC through the ECV304 cell layer (Fig. 1b). Again, expression of transmembrane CX3CL1 on the ECV304 cells clearly enhanced transmigration and this response was not influenced by pretreatment with soluble CX3CL1. Finally, soluble CX3CL1 consisting of only the extracellular part of the chemokine was expressed and investigated for PBMC transmigration in parallel with transmembrane CX3CL1 as described above. Although both forms of CX3CL1 were expressed at a similar protein level and followed the predicted trafficking routes as shown by flow cytometry and ELISA [20], PBMC transmigration was not induced when only soluble CX3CL1 was expressed (data not shown). Therefore, enhanced transmigration through cells expressing transmembrane CX3CL1 cannot be explained by the release of free soluble CX3CL1 acting as a chemoattractant.
Transmembrane CX3CL1 mediates PBMC transmigration through HUVEC
The experiments described above were generated using an epithelial cell layer and indicate that the presence of transmembrane CX3CL1 is a trigger for transcellular migration. To analyze transendothelial migration, we next used HUVEC as a cell layer. These cells were stimulated with IFN-γ and TNF-α to express endogenous CX3CL1 [24] or left unstimulated. Immunocytochemistry demonstrated intracellular as well as surface expression of endogenous CX3CL1 on stimulated HUVEC. Additional binding of exogenous free CX3CL1 to HUVEC was not detected, suggesting that surface staining resulted from the expression of transmembrane CX3CL1 (supplemental Fig. 1). To specifically investigate the role of surface-expressed CX3CL1, cells were then incubated in the presence and absence of a neutralizing antibody to CX3CL1. Free antibody was removed and the cells were transferred to fresh medium before PBMC were added. Transmigration of PBMC was considerably increased when cells were stimulated with IFN-γ and TNF-α (Fig. 1c). This transmigration was almost completely suppressed by pretreatment of HUVEC with the neutralizing antibody to CX3CL1. The inhibition was as efficient as that obtained with a neutralizing antibody to ICAM-1. Although these experiments suggest a role of surface-expressed CX3CL1, it seemed possible that soluble CX3CL1, which was generated during the transmigration assay, could influence the migratory response. Quantitative analysis of conditioned medium from HUVEC using a CX3CL1-specific ELISA, however, revealed that only a minimal amount of CX3CL1 is shed during this time period (0.01 nM), which was far below the minimal dosage required to induce a migratory response. Since preoccupation of surface-expressed CX3CL1 by the neutralizing antibody was sufficient to block transmigration and soluble chemokines were removed by washing, we conclude that surface expression of transmembrane CX3CL1 is sufficient to induce leukocyte migration through cytokine-activated endothelial cells.
CX3CR1 mediates transmigration
For a more detailed mutational analysis of how the interaction of surface-expressed CX3CL1 with its receptor CX3CR1 induces transmigration, we used the embryonic kidney cell line HEK293 and the murine pre B cell line L1.2 that do not produce endogenous CX3CR1. Both cell lines were transfected to express CX3CR1. Chemotaxis experiments confirmed that CX3CR1 promotes migration of L1.2 cells towards recombinant soluble CX3CL1. Moreover, the receptor mediated efficient CX3CL1-dependent adhesion of HEK293 cells and L1.2 cells (data not shown). These studies are well in line with our observations made with primary leukocytes and suggest that the transfected L1.2 cell lines may be used to investigate chemokine-mediated cell recruitment in more detail [12, 18]. Next, L1.2 cells expressing CX3CR1 were assayed for transmigration across cultured wt- or CX3CL1-ECV304 cells in the absence or presence of soluble CX3CL1 in the lower compartment of the transwell chamber. Soluble and cell-expressed CX3CL1, both induced migration of CX3CR1-L1.2, but not of wt-L1.2 cells (Fig. 2a). Simultaneous presence of transmembrane and soluble CX3CL1 did not further enhance transmigration. Pretreatment of CX3CL1-ECV304 cells with a neutralizing antibody against CX3CL1 that was added to the upper compartment of the transwell system for 15 min and removed directly before the migration assay reduced cell migration, whereas addition of the antibody to the lower compartment did not suppress cell migration (Fig. 2b). These results indicate that apically expressed CX3CL1 is the relevant trigger for transmigration.
CX3CR1 mediates transmigration. a Wt- and CX3CR1-L1.2 were investigated for transmigration across wt- or CX3CL1-ECV304 cells cultured in transwell inserts. b Neutralizing monoclonal antibody to CX3CL1 or isotype control (10 μg/ml each) was added to the lower or upper compartment of transwells containing wt- or CX3CL1-ECV304 cells. After 15 min, the antibody was removed and the cells were investigated for transmigration of CX3CR1-L1.2 cells. c HUVEC were stimulated with IFN-γ and TNF-α (both 10 ng/ml) for 16 h or left untreated. Subsequently, wt- and CX3CR1-L1.2 cells were assayed for transmigration across the HUVEC layer. d Wt- and CX3CR1-L1.2 cells were pretreated for 30 min with soluble CX3CL1 (10 nM) or 2 h with PTX (100 ng/ml) and subsequently assayed for transmigration across wt- or CX3CL1-ECV304 cells. Data are shown as mean plus SD of three independent experiments. The asterisks indicate statistically significant differences versus the controls (untransfected, unstimulated or isotype, respectively, p < 0.05)
We then used HUVEC as a cell layer for transmigration of L1.2 cells. When these cells were stimulated with IFN-γ and TNF-α to express endogenous CX3CL1, CX3CR1-L1.2 cells but not wt-L1.2 cells transmigrated through the HUVEC layer (Fig. 2c). Collectively, the data demonstrate that transmembrane CX3CL1 expressed on the cell surface of endothelial cells not only functions as an adhesion molecule, but can also mediate transmigration through CX3CL1-expressing endothelial cells.
It has been previously demonstrated, that pretreatment of PBMC with soluble CX3CL1 blocks chemotaxis as well as cell adhesion via transmembrane CX3CL1 whereas pretreatment with the Gi protein inhibitor pertussis toxin (PTX) selectively blocks chemotaxis but not adhesion [12]. In a first step to characterize transmigration in response to transmembrane CX3CL1, we pretreated CX3CR1-L1.2 cells with soluble CX3CL1 or with PTX before transmigration through CX3CL1-expressing ECV304 cells was assayed. Pretreatment with soluble CX3CL1 or with PTX efficiently suppressed transmigration of CX3CR1-L1.2 cells (Fig. 2d). These data suggest that transmigration is mediated by the interaction of CX3CR1 and transmembrane CX3CL1 and requires Gi Protein-mediated signaling of the receptor.
Distinct requirements for ligand binding, ligand uptake and calcium signaling via CX3CR1
To further investigate the requirements for CX3CR1-mediated transmigration, we introduced several mutations into CX3CR1 that potentially affect signaling of the receptor. From other reports on murine CX3CR1 and related GPCR it can be concluded that the NPX(2-3)Y motif in the seventh transmembrane region, the DRY motif in the second intracellular loop and the intracellular C-terminus play a role in CX3CR1-induced signaling [15, 19, 26]. We sought to investigate whether these motifs are required for the transmigratory response towards transmembrane CX3CL1. Four different variants of CX3CR1 were constructed: R127N in the DRY sequence, N289A and Y293A in the NPX(2-3)Y motif and truncation of the intracellular C-terminus before serine 319 (S319X) (Fig. 3a).
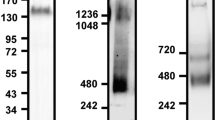
Design and expression of CX3CR1 mutants. a CX3CR1 carries a number of conserved sequences including a DRY motif in the second intracellular loop, a NPX2-3Y motif in the seventh transmembrane domain and several serine residues at the C-terminus. To disrupt these motifs, CX3CR1 was mutated at the indicated sites. R127 in the second intracellular loop was mutated to N (R127N), N289 and Y293 in the seventh transmembrane domain were changed into A (N289A and Y293A, respectively), and the intracellular C-terminus was truncated before S319 (S319X). b Expression of the receptor variants was controlled by flow cytometry using PE-conjugated rat anti-CX3CR1. Ligand binding was analyzed by flow cytometry using a recombinant CX3CL1-Fc construct as a ligand. Receptor expression and ligand binding were measured as the mean fluorescence intensity increase compared to control. After logarithmic transformation, the data were summarized as means plus SD from five independent experiments. Expression in mock cells was used as a covariate. The asterisks indicate statistically significant differences (p < 0.05) in receptor expression and ligand binding between CX3CR1 and its variants. c CX3CR1 and its R127N and S319X variants were then stably expressed in HEK293 cells and selected for comparable surface expression by flow cytometry using PE-conjugated rat anti-CX3CR1. Cells were constantly controlled for stable receptor expression. Data are shown as a representative histogram
We first determined whether introducing these mutations would still allow receptor expression and ligand binding. The receptor variants were transiently transfected into HEK293 cells and analyzed for their expression by flow cytometry using an anti-CX3CR1 antibody. We found that all variants could be detected on the cell surface (Fig. 3b). To examine whether the transfected receptor variants bind CX3CL1, cells were incubated with CX3CL1 fused to the Fc-part of human IgG1. This construct was then detected by flow cytometry using an anti-Fc-antibody (Fig. 3b). Binding of this ligand was still detectable for the R127N and S319X variants, but absent in the N289A and Y293A variants. Therefore, only the R127N and S319X mutations were further characterized in functional assays. For this purpose, both receptor variants were stably transfected in HEK293 cells that were then selected for receptor expression matching that of CX3CR1-HEK293 cells (Fig. 3c).
Since most GPCR rapidly internalize upon ligand-binding, we tested whether the introduced mutations altered ligand uptake by the receptor. When incubated with AlexaFluor647-labeled CX3CL1 (AF-CX3CL1), CX3CR1-HEK293 cells showed a time dependent increase in fluorescence as measured by flow cytometry. This increase was almost completely abolished when cells were treated with NaN3 to prevent ligand uptake (Fig. 4a, b) suggesting that most of the fluorescence increase was due to ligand uptake rather than surface binding of AF-CX3CL1. No specific fluorescence uptake was seen with wt-HEK293 cells. Expression of CX3CR1 or the R127N mutation led to a time dependent fluorescence increase (Fig. 4b). This increase in fluorescence was clearly reduced when the S319X variant was expressed indicating that the receptor’s C-terminus contributes to receptor-mediated ligand uptake.
Ligand uptake and calcium signaling via CX3CR1 mutants. a HEK293 cells expressing the different receptor variants were incubated with AlexaFluor647-labeled CX3CL1 (AF-CX3CL1) at 37°C in the absence or presence of NaN3 (0.2%). Subsequently, cells were analyzed for binding and uptake of fluorescent CX3CL1 by flow cytometry. A representative histogram of the fluorescence signal for CX3CR1-HEK293 cells is shown. b HEK293 cells expressing the different receptor variants were incubated with AF-CX3CL1 at 37°C for the time periods indicated. The fluorescence intensity for the different HEK293 mutants was expressed in relation to that of the control receiving no AF-CX3CL1 and is presented as mean plus SD from three independent experiments. The asterisks indicate statistically significant differences versus the untransfected control. The crosses indicate statistically significant differences versus CX3CR1-HEK293 cells (p < 0.05). c HEK293 cells expressing the indicated receptor variants were loaded with calcium indicator Fluo-3-AM and changes in fluorescence intensity upon treatment with soluble CX3CL1 (10 nM at 100 s) were recorded. The arrow indicates an increase of 0.5 mM Ca2+. Results shown are representative for three independent experiments
The concentration of intracellular free calcium rapidly increases upon activation of most chemokine receptors including CX3CR1 [10]. To investigate whether the mutated CX3CR1 variants were still able to mediate intracellular calcium transients, transfected HEK293 cells were stained with the calcium indicator Fluo-3-AM and treated with 10 nM CX3CL1 (Fig. 4c). We found that HEK293 cells expressing CX3CR1 or its truncated variant S319X responded to the chemokine by intracellular calcium signals whereas wt-HEK293 or HEK293 expressing the R127N mutant were not responsive. These data indicate that the induction of intracellular calcium transients by CX3CR1 requires the integrity of the receptor’s DRY motif, but is independent of its C-terminus.
Chemotaxis and transmigration but not adhesion depend on the DRY motif and the C-terminus of CX3CR1
To explore the functional relevance of the R127N and S319X mutations for cell recruitment, stably transfected HEK293 cells were tested for their ability to adhere to CX3CL1-expressing ECV304 cells and HUVEC under static and flow conditions. Compared to the wild-type receptor, both receptor mutations did not show any differences in static adhesion to CX3CL1-ECV304 (Fig. 5a). These experiments were confirmed in flow adhesion assays using HUVEC that were stimulated with IFN-γ and TNF-α to express endogenous transmembrane CX3CL1 [24]. A shear stress of 2 dyne/cm2 was chosen for initial experiments since adhesion to immobilized CX3CL1 was found to be maximal at these flow rates [27]. Under these conditions, adhesion to stimulated HUVEC was similar for all tested receptor variants including the wild-type receptor (Fig. 5b). Further adhesion experiments at 5 dyne/cm2 indicated that there was no difference between the tested receptor variants at higher flow rates (data not shown).
Role of the DRY motif and the C-terminus for CX3CR1-mediated adhesion and transmigration. The ability of the receptor variants to mediate adhesion to CX3CL1 was tested under static (a) and flow (b) conditions. a For static adhesion assays, calcein-labeled HEK293 cells expressing the indicated receptor variants were seeded onto wt- or CX3CL1-ECV304 cells. After washing, the fluorescence signal of the adhering cells was measured. The adhesion index was determined by calculating the ratio of the fluorescence signal from adherent HEK293 cells bound to CX3CL1-ECV304 and from that bound to wt-ECV304 cells. b For flow adhesion experiments, labeled HEK293 cells expressing the indicated receptor variants were perfused over a layer of cytokine-stimulated HUVEC for 1 min. c L1.2 cells expressing the indicated receptor variants were tested for their chemotactic response towards increasing concentrations of soluble CX3CL1 (0.1–100 nM) in a modified Boyden chamber assay. d L1.2 cells expressing the indicated receptor variants were studied for transmigration through CX3CL1-ECV304 cells. e HUVEC were stimulated with IFN-γ and TNF-α (both 10 ng/ml) for 16 h and subsequently probed for transmigration of L1.2 cells in response to CX3CR1 or its R127N variant. Three independent experiments were performed and data are shown as mean plus SD. The asterisks indicate statistically significant differences versus the untransfected control (p < 0.05)
Chemotaxis experiments were performed to investigate whether the R127N and S319X mutations would allow migration in response to soluble CX3CL1. For this purpose, the receptor variants were stably transfected in L1.2 cells. Similar expression levels and comparable adhesive activity of all receptor variants was confirmed by flow cytometry and adhesion assays with CX3CL1-ECV304 cells (data not shown). In a modified Boyden chamber chemotaxis assay, only the CX3CR1-expressing cells, but not the cells with mutated receptors (R127N or S319X) migrated towards increasing concentrations of CX3CL1 (Fig. 5c). We then examined the ability of CX3CR1 variants to induce transmigration through the ECV304 cell layer (Fig. 5d). When CX3CR1-L1.2 cells were seeded onto CX3CL1-ECV304 cells transmigration was increased. By contrast, transmigration was even below baseline when L1.2 cells expressed the R127N or S319X-mutant.
To confirm these data under more physiologic settings, we used cytokine-stimulated HUVEC instead of ECV304 cells for transmigration assays. Again, CX3CR1 increased transmigration of L1.2 cells whereas R127N-CX3CR1 (Fig. 5e) suppressed transmigration (S319X-CX3CR1 was not investigated). These results suggest that receptor function via the DRY motif and the C-terminus are required for transmigration. In the absence of these motifs, however, transmigration is blocked which could be explained by the increased adhesion of leukocytes to transmembrane CX3CL1 on the ECV304 cells and a failure to induce transmigratory signals in the adherent leukocytes.
ADAM10 and 17 activity is required for CX3CL1-mediated transmigration
ADAM10 and ADAM17 have been found to shed transmembrane CX3CL1 [8, 9] and thereby facilitate detachment of leukocytes bound to CX3CL1 [21]. We therefore decided to investigate the role of the two metalloproteinases in the transmigration process. We pretreated the ECV304 cell layer with GW280264X [28], an inhibitor of the metalloproteinases ADAM10 and ADAM17. To selectively address the role of the proteases on the ECV304 cell layer, the inhibitor was removed prior to starting the transmigration assay by the addition of L1.2 cells. The inhibitor did not affect L1.2 recruitment via soluble CX3CL1, but clearly blocked transmigration in response to transmembrane CX3CL1 (Fig. 6a). Moreover, this inhibition of transmembrane CX3CL1 activity could not be overcome by addition of soluble CX3CL1 as a chemoattractant. Residual migration in the absence of CX3CL1 was not affected by GW280264X indicating that there was no general effect on the integrity of the cell layer. These results indicate that the activity of ADAMs is required for transmigration in response to transmembrane CX3CL1, but not to soluble CX3CL1.
Effect of the metalloproteinase inhibitor GW280264X on CX3CL1-mediated transmigration. a Wt- or CX3CL1-ECV304 cells were grown on transwell inserts and pretreated with GW280264X (10 μM) or DMSO control for 1 h. After removal of the inhibitor, the lower compartments of the transwell systems received soluble CX3CL1 (10 nM) or were left without stimulus. Subsequently, cells were assayed for transmigration of wt- and CX3CR1-L1.2 cells. b CX3CL1-ECV304 cells were pretreated with GW280264X (10 μM) or DMSO for 1 h, washed and co-incubated with freshly prepared PBMC for 3 h. Cells were harvested and analyzed for CX3CL1 surface expression by flow cytometry. Surface expression was expressed in relation to that of CX3CL1-ECV304 cells receiving no inhibitor and no PBMC. c Wt- or CX3CL1-ECV304 cells were incubated for 3 h in the presence or absence of L1.2 cells expressing the indicated CX3CR1 variants and subsequently conditioned media were analyzed for the presence of shed soluble CX3CL1 by ELISA. Results are expressed in relation to the control receiving no L1.2 cells. d Wt- or CX3CL1-ECV304 cells were pretreated with DMSO control or GW280264X (10 μM) for 1 h, washed and subsequently analyzed for adhesion of PBMC under flow. e Wt- or CX3CL1-ECV304 cells were grown on transwell inserts, pretreated with DMSO control or GW280264X (10 μM) for 1 h, and subsequently probed for transmigration of PBMC. f HUVEC were stimulated with IFN-γ and TNF-α (both 10 ng/ml) or left unstimulated for 16 h. Subsequently, cells were pretreated with DMSO control or GW280264X (10 μM) for 1 h and then analyzed for flow-resistant adhesion of PBMC. g Unstimulated and IFN-γ/TNF-α-stimulated HUVEC were pretreated with DMSO control or GW280264X and subsequently probed for transmigration of PBMC. Data are shown as mean plus SD obtained from three independent experiments. Statistically significant differences between inhibitor-treated and DMSO-treated cells are indicated by asterisks (p < 0.05)
The following experiments were performed to investigate whether CX3CL1 shedding on ECV304 cells would be altered in the presence of leukocytes. The surface expression level of CX3CL1 on ECV304 cells was diminished when these cells were exposed to PBMC (Fig. 6b). Pretreatment of CX3CL1-ECV304 cells with GW280264X considerably increased CX3CL1 surface expression. This effect of the inhibitor was not altered when the CX3CL1-ECV304 cell layer was exposed to PBMC. These findings suggest that ADAM10 or ADAM17 are the relevant sheddases of CX3CL1 in the absence and in the presence of PBMC. To determine whether interaction of CX3CL1 with its receptor CX3CR1 would affect the shedding of CX3CL1, we co-incubated L1.2 cells expressing CX3CR1 variants with CX3CL1-ECV304 cells and determined the amount of shed CX3CL1 by ELISA. We could confirm that CX3CL1 shedding is enhanced in the presence of leukocytes (Fig. 6c). However, we did not observe that expression of CX3CR1 (wild-type or any mutant) on L1.2 cells has an effect on the shedding of CX3CL1 suggesting that binding and activation of CX3CR1 does not affect shedding of the chemokine.
To examine whether inhibition of CX3CL1 shedding and the increased surface expression of the chemokine would affect cell recruitment, adhesion assays with PBMC were performed. CX3CL1-mediated adhesion to ECV304 cells was considerably increased when the cells were pretreated with the inhibitor (Fig. 6d). However, despite increased CX3CL1 surface expression and increased adhesion, CX3CL1-mediated transmigration of PBMC through the ECV304 cell layer was completely suppressed by GW280264X (Fig. 6e). Residual migration in the absence of CX3CL1 was not affected by the inhibitor. Experiments were repeated with HUVEC (Fig. 6f, g), demonstrating that PBMC adhesion to cytokine-stimulated HUVEC is profoundly increased whereas transmigration is completely suppressed by the inhibitor.
The importance of ADAM10 and ADAM17 in CX3CL1-dependent transmigration was further investigated by shRNA-mediated silencing of these proteases. A lentiviral expression vector for the shRNA was used for efficient and sustained downregulation of ADAM10 and ADAM17 surface expression on CX3CL1-ECV304 cells (Fig. 7a). By ELISA, we confirmed that silencing of ADAM10 led to accumulation of CX3CL1 in the cell lysates (Fig. 7b). Silencing of ADAM17 had no comparable effect on the constitutive release of CX3CL1, which is consistent with our previous observation that this protease is implicated in the PMA-stimulated release of CX3CL1, but not in the constitutive shedding of the chemokine [9]. CX3CR1-mediated transmigration through CX3CL1-expressing ECV304 cells was almost completely suppressed when ADAM10 expression was silenced and moderately reduced when ADAM17 expression was downregulated (Fig. 7c). Combined targeting of both proteases did not further decrease transmigration (data not shown).
Role of ADAM10 and ADAM17 for CX3CL1-induced transmigration. Wt- and CX3CL1-ECV304 cells were stably transduced with lentivirus carrying shRNA for knockdown of ADAM10 and ADAM17 (A10shRNA or A17shRNA) or scrambled shRNA control, respectively. a Efficient and sustained downregulation of ADAM10 and ADAM17 surface expression was controlled by flow cytometry and is shown as representative histograms. b Stably transduced CX3CL1-ECV304 cells were incubated for 2 h, and subsequently released CX3CL1 in the supernatants and cell-associated CX3CL1 in the lysates were quantified by ELISA. The amount of residual cell-expressed CX3CL1 was calculated in relation to the total content of CX3CL1 in both the lysates and supernatants. c Stably transduced CX3CL1-ECV304 cells were investigated for transmigration by wt- and CX3CR1-L1.2 cells. d HUVEC were transduced with A10shRNA, A17shRNA or scramble shRNA control. Cells were stimulated with IFN-γ and TNF-α (both 10 ng/ml) or left unstimulated for 16 h and subsequently investigated for transmigration by wt- and CX3CR1-L1.2 cells. Data are shown as mean plus SD obtained from three independent experiments. Statistically significant differences versus the controls receiving scrambled shRNA are indicated by asterisks (p < 0.05)
Finally, silencing experiments were performed with HUVEC. Again, CX3CR1/CX3CL1-dependent transmigration was completely suppressed when ADAM10 was downregulated. These results indicate that ADAM10 and to a lesser degree ADAM17 decrease CX3CL1 surface expression as well as CX3CL1-mediated adhesion and are required for transmigration in response to CX3CL1.
Discussion
Fractalkine/CX3CL1 is an unusual chemokine that is expressed as a transmembrane molecule on the surface of physiologic interfaces such as endothelial or epithelial cells [6]. Transmembrane CX3CL1 is known to promote flow resistant adhesion of leukocytes to endothelial or epithelial interfaces, which is mediated by physical interaction with its receptor CX3CR1 independently of signaling via Gi proteins [7, 12]. Here we extend these findings by showing that leukocytes employ the CX3CR1 receptor not only to bind to CX3CL1 expressed by the epithelial cell line ECV304 or by endothelial cells but also for Gi-dependent signaling leading to transmigration of adherent leukocytes. The latter activity is mediated by apically expressed transmembrane CX3CL1, which is consistent with the fact that immobilized chemokines can induce haptotactic migration of responsive leukocytes and that a concentration gradient of soluble chemokine is not required for this activity [25]. CX3CL1-induced transmigration critically depends on the receptor’s DRY motif and C-terminus and requires the proteolytic activity predominantly of the sheddase ADAM10 and to some degree of ADAM17. In the absence of CX3CR1 signaling, leukocytes attach to CX3CL1 but do not transmigrate. In the absence of ADAM10/17 shedding activity, CX3CL1-mediated adhesion is even further enhanced whereas transmigration is completely blocked. This was observed with ECV304 cells as well as with HUVEC and suggests that the proteases are required to set the leukocytes free for transmigration in both cell types. These data support the model that CX3CL1 induces cell recruitment by a sequence of events including cell adhesion, signaling via CX3CR1, which initiates the transmigration process, and proteolytic shedding via ADAMs, which allows the leukocyte to continue transmigration. Since very similar observations were made with CX3CL1-expressing ECV304 cells as well as with HUVEC it appears that transmembrane CX3CL1 has a broader activity to trigger transmigration through different types of cell layers. This activity of CX3CL1 would not only induce transendothelial migration but could also be relevant in the gut where the molecule is expressed on epithelial cells and has been made responsible to mediate access of dendritic cells to the intestinal lumen [29].
CX3CR1 carries a number of motifs typical for several other Gi protein-coupled receptors including a NPX(2-3)Y motif in the seventh transmembrane region, a DRY sequence in the second intracellular loop, and a number of serine residues within the C-terminus [12]. Our mutational analysis of these motifs revealed that they are not required for surface expression, but for ligand binding, calcium signaling and trafficking of the receptor, respectively. The NPX(2-3)Y motif is required for ligand binding as has been reported for other GPCR [15, 16]. The DRY motif is critical for the activation of calcium signals, but not for receptor trafficking as assessed by ligand uptake. And finally, the C-terminus contributes to trafficking, but not to induction of calcium transients. These data are consistent with the established knowledge for other GPCR that the calcium response depends on the DRY motif and its interaction with Gi proteins [13, 30]. Apparently, this rapid calcium response occurs independently of slower processes such as receptor internalization. Most chemoattractant receptors including CXCR2 and CCR5 carry a number of serine residues that become phosphorylated upon ligand engagement and may trigger the interaction with β-arrestin, which in turn mediates receptor desensitization and internalization [26, 31]. In line with this, deletion of the serine-rich C-terminal part of CX3CR1 attenuates ligand uptake by internalization, but not calcium signaling, whereas disruption of the DRY motif only abolishes calcium signaling, but not internalization indicating that each motif contributes to a different CX3CR1 function.
Although the DRY sequence as well as the C-terminus of CX3CR1 differentially contribute to signaling and trafficking, they are both required for the induction of chemotaxis and transmigration. The importance of the DRY motif may be explained by the fact that it represents a critical motif for Gi protein activation, which triggers phospholipase C activation followed by diacylglycerol formation and calcium mobilization. This signaling pathway is involved in the control of actin polymerization being critical for cell migration [32, 33]. In murine CX3CR1, the DRY motif appears to hold a similar function as indicated by the finding that its mutation into DNY blocks chemotaxis towards soluble CX3CL1 [19]. The importance of the receptor’s C-terminus may be explained by the fact that its integrity is required for receptor desensitization. This is a critical regulatory mechanism for receptor adaptation towards increasing dosages of chemokines and a prerequisite for the sensing of chemotactic gradients as shown for other chemokine receptors such as CXCR2 [34]. This may explain why both Gi protein activation by the DRY motif as well as receptor regulation at the C-terminus are critical for induction of chemotaxis by soluble CX3CL1. Our data furthermore demonstrate that both motifs are also required for transmigration in response to transmembrane CX3CL1, suggesting that they may fulfill very similar functions in chemotaxis and transmigration. By contrast, adhesion is neither affected by mutating the DRY motif nor by truncation of the C-terminus. The molecular explanation for this activity is provided by other reports showing that adhesion to transmembrane CX3CL1 is predominantly mediated by the physical interaction with the receptor [18, 19] and by our finding that the physical properties of the human receptor in terms of surface expression and ligand binding are independent of the DRY motif and the C-terminus.
Transmembrane CX3CL1 can be cleaved proximal to the cell membrane resulting in the release of its soluble ectodomain and the downregulation of CX3CL1 from the cell surface [8, 9]. We show that this cleavage can be enhanced by cell stimulation or by the presence of leukocytes, but the underlying mechanism of this regulation remains to be further investigated. On the one hand, shedding leads to reduced adhesiveness for CX3CR1-expressing leukocytes via transmembrane CX3CL1. On the other hand, leukocytes bound to transmembrane CX3CL1 may become released upon cleavage of the transmembrane chemokine [21]. Such a process could be relevant for transmigration when adherent leukocytes move from the apical site of the endothelium towards the lateral junction for transmigration between two substrate cells. This process would require the detachment from the apical side including the interruption of the initial contacts between leukocytes and endothelial cells. Since the binding of CX3CL1 to its receptor is extremely tight due to a low dissociation rate from the receptor [35], cleavage of CX3CL1 might be the only way to disrupt the cell–cell contact and thereby allow transmigration. This model is corroborated by our observation that pharmacological or transcriptional inhibition of ADAM10/17 proteases efficiently blocked shedding of CX3CL1 leading to enhanced surface expression and adhesive activity of the chemokine, whereas transmigration in response to CX3CL1 was completely blocked. In our shRNA experiments, downregulation of ADAM10 had the most prominent effect on CX3CL1-induced transmigration. However, in vivo other proteases such as ADAM17, MMPs and cathepsins that are capable of CX3CL1 cleavage [8] may contribute to this process depending on the tissue environment and the stimulatory conditions.
Extravasation of leukocytes out of the bloodstream is thought to take place in a multi-step process that starts with rolling onto endothelial cells via selectins, turns into chemokine-mediated firm adhesion to adhesion molecules such as integrins, and ends with the migration of leukocytes towards chemotactic factors through the endothelial barrier [1]. These events are mediated by the coordinated activity of selectins, chemokines, and integrins. Interestingly, CX3CL1 has the capacity to mediate capture under flow, tight adhesion and directional transmigration, and can therefore contribute to all steps of the recruitment process. From our present study, we would like to propose that the process of CX3CL1-mediated cell recruitment involves a sequence of events starting with physical binding of the receptor, activation of the receptor initiating the transmigration process, and finally cleavage by ADAM10 and 17 allowing the cells to proceed in diapedesis. The last step of transmigration may involve the cleavage of several surface molecules that contribute to the transmigration process such as VCAM-1, JAM-A, and VE-cadherin [36], and very likely also includes the shedding of transmembrane CX3CL1. Our data provide a molecular explanation for the proinflammatory activity of the CX3CR1/CX3CL1 axis in vascular diseases such as atherosclerosis, which is well documented by a number of genetic studies on human CX3CR1 polymorphisms and by animal experiments using CX3CR1- or CX3CL1-deficient mice [2–5]. Finally, when considering the CX3CR1/CX3CL1 axis as a therapeutic target in order to block leukocyte recruitment in atherosclerosis, it seems preferable to interfere with the initial step of adhesion using a receptor antagonist rather than blocking CX3CR1 signaling or CX3CL1 shedding, which would both lead to the accumulation of adherent leukocytes at the vascular surface [36].
Abbreviations
- AM:
-
Acetoxymethylester
- ADAM:
-
A disintegrin and a metalloproteinase
- CCL2:
-
CC-chemokine ligand 2
- CX3CL1:
-
CX3C-chemokine ligand 1
- CX3CR1:
-
CX3C-chemokine receptor 1
- ELISA:
-
Enzyme-linked immunosorbent assay
- FCS:
-
Fetal calf serum
- FITC:
-
Fluorescein isothiocyanate
- Gi protein:
-
Inhibitory G protein
- GPCR:
-
G protein-coupled receptor
- hFc:
-
Human IgG1-Fc-fragment
- HUVEC:
-
Human umbilical vein endothelial cells
- ICAM:
-
Intercellular adhesion molecule
- IFN:
-
Interferon
- MMP:
-
Matrix metalloproteinase
- PBMC:
-
Peripheral blood mononuclear cells
- PBS:
-
Phosphate-buffered saline
- PE:
-
Phycoerythrin
- TNF:
-
Tumor necrosis factor
- shRNA:
-
Short hairpin RNA
- wt:
-
Wild-type
References
Springer TA (1994) Traffic signals for lymphocyte recirculation and leukocyte emigration: the multistep paradigm. Cell 76:301–314
Combadiere C, Potteaux S, Gao JL, Esposito B, Casanova S, Lee EJ, Debre P, Tedgui A, Murphy PM, Mallat Z (2003) Decreased atherosclerotic lesion formation in CX3CR1/apolipoprotein E double knockout mice. Circulation 107:1009–1016
Lesnik P, Haskell CA, Charo IF (2003) Decreased atherosclerosis in CX3CR1−/− mice reveals a role for fractalkine in atherogenesis. J Clin Invest 111:333–340
Teupser D, Pavlides S, Tan M, Gutierrez-Ramos JC, Kolbeck R, Breslow JL (2004) Major reduction of atherosclerosis in fractalkine (CX3CL1)-deficient mice is at the brachiocephalic artery, not the aortic root. Proc Natl Acad Sci USA 101:17795–17800
McDermott DH, Fong AM, Yang Q, Sechler JM, Cupples LA, Merrell MN, Wilson PW, D’Agostino RB, O’Donnell CJ, Patel DD, Murphy PM (2003) Chemokine receptor mutant CX3CR1–M280 has impaired adhesive function and correlates with protection from cardiovascular disease in humans. J Clin Invest 111:1241–1250
Ludwig A, Weber C (2007) Transmembrane chemokines: versatile ‘special agents’ in vascular inflammation. Thromb Haemost 97:694–703
Bazan JF, Bacon KB, Hardiman G, Wang W, Soo K, Rossi D, Greaves DR, Zlotnik A, Schall TJ (1997) A new class of membrane-bound chemokine with a CX3C motif. Nature 385:640–644
Garton KJ, Gough PJ, Blobel CP, Murphy G, Greaves DR, Dempsey PJ, Raines EW (2001) Tumor necrosis factor-alpha-converting enzyme (ADAM17) mediates the cleavage and shedding of fractalkine (CX3CL1). J Biol Chem 276:37993–38001
Hundhausen C, Misztela D, Berkhout TA, Broadway N, Saftig P, Reiss K, Hartmann D, Fahrenholz F, Postina R, Matthews V, Kallen KJ, Rose-John S, Ludwig A (2003) The disintegrin-like metalloproteinase ADAM10 is involved in constitutive cleavage of CX3CL1 (fractalkine) and regulates CX3CL1-mediated cell–cell adhesion. Blood 102:1186–1195
Harrison JK, Jiang Y, Chen S, Xia Y, Maciejewski D, McNamara RK, Streit WJ, Salafranca MN, Adhikari S, Thompson DA, Botti P, Bacon KB, Feng L (1998) Role for neuronally derived fractalkine in mediating interactions between neurons and CX3CR1-expressing microglia. Proc Natl Acad Sci USA 95:10896–10901
Combadiere C, Salzwedel K, Smith ED, Tiffany HL, Berger EA, Murphy PM (1998) Identification of CX3CR1. A chemotactic receptor for the human CX3C chemokine fractalkine and a fusion coreceptor for HIV-1. J Biol Chem 273:23799–23804
Imai T, Hieshima K, Haskell C, Baba M, Nagira M, Nishimura M, Kakizaki M, Takagi S, Nomiyama H, Schall TJ, Yoshie O (1997) Identification and molecular characterization of fractalkine receptor CX3CR1, which mediates both leukocyte migration and adhesion. Cell 91:521–530
Lagane B, Ballet S, Planchenault T, Balabanian K, Le Poul E, Blanpain C, Percherancier Y, Staropoli I, Vassart G, Oppermann M, Parmentier M, Bachelerie F (2005) Mutation of the DRY motif reveals different structural requirements for the CC chemokine receptor 5-mediated signaling and receptor endocytosis. Mol Pharmacol 67:1966–1976
Berchiche YA, Chow KY, Lagane B, Leduc M, Percherancier Y, Fujii N, Tamamura H, Bachelerie F, Heveker N (2007) Direct assessment of CXCR4 mutant conformations reveals complex link between receptor structure and G(alpha)(i) activation. J Biol Chem 282:5111–5115
Slice LW, Wong HC, Sternini C, Grady EF, Bunnett NW, Walsh JH (1994) The conserved NPXnY motif present in the gastrin-releasing peptide receptor is not a general sequestration sequence. J Biol Chem 269:21755–21761
Barak LS, Tiberi M, Freedman NJ, Kwatra MM, Lefkowitz RJ, Caron MG (1994) A highly conserved tyrosine residue in G protein-coupled receptors is required for agonist-mediated beta 2-adrenergic receptor sequestration. J Biol Chem 269:2790–2795
Ribas C, Penela P, Murga C, Salcedo A, García-Hoz C, Jurado-Pueyo M, Aymerich I, Mayor F (2007) The G protein-coupled receptor kinase (GRK) interactome: role of GRKs in GPCR regulation and signaling. Biochim Biophys Acta 1768:913–922
Fong AM, Robinson LA, Steeber DA, Tedder TF, Yoshie O, Imai T, Patel DD (1998) Fractalkine and CX3CR1 mediate a novel mechanism of leukocyte capture, firm adhesion, and activation under physiologic flow. J Exp Med 188:1413–1419
Haskell CA, Cleary MD, Charo IF (1999) Molecular uncoupling of fractalkine-mediated cell adhesion and signal transduction. Rapid flow arrest of CX3CR1-expressing cells is independent of G-protein activation. J Biol Chem 274:10053–10058
Andrzejewski MG, Koelsch A, Kogel T, Dreymueller D, Schwarz N, Ludwig A (2010) Distinct role of the intracellular C-terminus for subcellular expression, shedding and function of the murine transmembrane chemokine CX3CL1. Biochem Biophys Res Commun 395:178–184
Hundhausen C, Schulte A, Schulz B, Andrzejewski MG, Schwarz N, von Hundelshausen P, Winter U, Paliga K, Reiss K, Saftig P, Weber C, Ludwig A (2007) Regulated shedding of transmembrane chemokines by the disintegrin and metalloproteinase 10 facilitates detachment of adherent leukocytes. J Immunol 178:8064–8072
Pruessmeyer J, Martin C, Hess FM, Schwarz N, Schmidt S, Kogel T, Hoettecke N, Schmidt B, Sechi A, Uhlig S, Ludwig A (2010) A disintegrin and metalloproteinase 17 (ADAM17) mediates inflammation-induced shedding of syndecan-1 and-4 by lung epithelial cells. J Biol Chem 285:555–564
Dirks WG, MacLeod RA, Drexler HG (1999) ECV304 (endothelial) is really T24 (bladder carcinoma): cell line cross-contamination at source. In Vitro Cell Dev Biol Anim 35:558–559
Ludwig A, Berkhout T, Moores K, Groot P, Chapman G (2002) Fractalkine is expressed by smooth muscle cells in response to IFN-gamma and TNF-alpha and is modulated by metalloproteinase activity. J Immunol 168:604–612
Rot A, von Andrian UH (2004) Chemokines in innate and adaptive host defense: basic chemokinese grammar for immune cells. Annu Rev Immunol 22:891–928
Ben Baruch A, Bengali KM, Biragyn A, Johnston JJ, Wang JM, Kim J, Chuntharapai A, Michiel DF, Oppenheim JJ, Kelvin DJ (1995) Interleukin-8 receptor beta. The role of the carboxyl terminus in signal transduction. J Biol Chem 270:9121–9128
Kerfoot SM, Lord SE, Bell RB, Gill V, Robbins SM, Kubes P (2003) Human fractalkine mediates leukocyte adhesion but not capture under physiological shear conditions; a mechanism for selective monocyte recruitment. Eur J Immunol 33:729–739
Ludwig A, Hundhausen C, Lambert MH, Broadway N, Andrews RC, Bickett DM, Leesnitzer MA, Becherer JD (2005) Metalloproteinase inhibitors for the disintegrin-like metalloproteinases ADAM10 and ADAM17 that differentially block constitutive and phorbol ester-inducible shedding of cell surface molecules. Comb Chem High Throughput Screen 8:161–171
Niess JH, Brand S, Gu X, Landsman L, Jung S, McCormick BA, Vyas JM, Boes M, Ploegh HL, Fox JG, Littman DR, Reinecker HC (2005) CX3CR1-mediated dendritic cell access to the intestinal lumen and bacterial clearance. Science 307:254–258
Roland J, Murphy BJ, Ahr B, Robert-Hebmann V, Delauzun V, Nye KE, Devaux C, Biard-Piechaczyk M (2003) Role of the intracellular domains of CXCR4 in SDF-1-mediated signaling. Blood 101:399–406
Kraft K, Olbrich H, Majoul I, Mack M, Proudfoot A, Oppermann M (2001) Characterization of sequence determinants within the carboxyl-terminal domain of chemokine receptor CCR5 that regulate signaling and receptor internalization. J Biol Chem 276:34408–34418
Murdoch C, Finn A (2000) Chemokine receptors and their role in inflammation and infectious diseases. Blood 95:3032–3043
Samstag Y, Eibert SM, Klemke M, Wabnitz GH (2003) Actin cytoskeletal dynamics in T lymphocyte activation and migration. J Leukoc Biol 73:30–48
Ludwig A, Petersen F, Zahn S, Gotze O, Schroder JM, Flad HD, Brandt E (1997) The CXC-chemokine neutrophil-activating peptide-2 induces two distinct optima of neutrophil chemotaxis by differential interaction with interleukin-8 receptors CXCR-1 and CXCR-2. Blood 90:4588–4597
Haskell CA, Cleary MD, Charo IF (2000) Unique role of the chemokine domain of fractalkine in cell capture. Kinetics of receptor dissociation correlate with cell adhesion. J Biol Chem 275:34183–34189
Pruessmeyer J, Ludwig A (2009) The good, the bad and the ugly substrates for ADAM10 and ADAM17 in brain pathology, inflammation and cancer. Semin Cell Dev Biol 20:164–174
Acknowledgments
We thank Tanja Kogel and Melanie Esser for expert technical assistance. This work was supported in part by the IZKF Aachen, and by the Deutsche Forschungsgemeinschaft (SFB542, A12, and FOR809, P5).
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
SUPPLEMENTAL FIGURE 1:
HUVEC were stimulated with IFN-γ and TNF-α (both 10 ng/ml) to induce endogenous CX3CL1 expression or left unstimulated for 16 h. Subsequently, cells were incubated in the absence or presence of exogenous soluble CX3CL1 (10 nM) for 1 h to investigate potential surface binding of the chemokine. Subsequently, cells were fixed, permeabilized, and stained for CX3CL1 (red) as described [20]. Nuclei were stained in blue. Scale bars represent 20 µm (PPT 3790 kb)
Rights and permissions
About this article
Cite this article
Schwarz, N., Pruessmeyer, J., Hess, F.M. et al. Requirements for leukocyte transmigration via the transmembrane chemokine CX3CL1. Cell. Mol. Life Sci. 67, 4233–4248 (2010). https://doi.org/10.1007/s00018-010-0433-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00018-010-0433-4