Abstract
Objective and design
Resistin and neutrophil gelatinase-associated lipocalin (NGAL) are upregulated in circulating leucocytes in sepsis, but the significance of this is uncertain. We evaluated associations between Resistin and NGAL with endothelial cell activation and clinical outcomes in a prospective observational study in the Emergency Department (ED).
Methods
Serum levels of Resistin, NGAL, inflammatory cytokines (IL-6, IL-10) and soluble endothelial adhesion molecules (VCAM-1, ICAM-1) were measured at defined time points up to 24 h. Patterns and relationships between markers were investigated using linear mixed regression models. Predictive values for clinical outcomes for markers at enrollment were assessed by logistic regression and receiver operator characteristic (ROC) curves.
Results
186 participants (89 septic-shock, 69 sepsis, 28 uncomplicated infection) were compared with 29 healthy controls. Median Resistin and NGAL were higher in uncomplicated infection compared to controls, and in septic shock compared to non-shock sepsis. Resistin and NGAL correlated with IL-6 and IL-10, with VCAM-1 and ICAM-1, and with organ failure. Resistin and NGAL were associated with septic shock but had limited predictive utility for mortality.
Conclusion
Resistin and NGAL correlate with expression of endothelial cell adhesion molecules in sepsis. Further evaluation of the role of Resistin and NGAL in sepsis pathogenesis is warranted.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Sepsis is defined as life-threatening organ dysfunction caused by a dysregulated host response to infection [1], involving pro- and anti- inflammatory components of the host innate immune system [2]. The vascular endothelium plays a central role in the pathogenesis of sepsis; endothelial cells are activated by circulating microbial or host-derived agonists, resulting in recruitment and transmigration of leucocytes, micro-thrombus formation, fluid extravasation and vasomotor changes, all of which can adversely affect organ function in the setting of critical illness [3, 4]. Markers of endothelial cell activation measured on admission are associated with illness severity and mortality in sepsis [5].
The pro-inflammatory adipokine resistin has been observed to be elevated during sepsis in the ICU [6, 7], and has been studied as a potential indicator of sepsis in neonates [8]. Resistin was first identified in mouse adipocytes, and is implicated in the pathogenesis of diabetes [9, 10]. In humans, resistin is principally produced by macrophages and neutrophils [11], and its ability to activate endothelial cells is thought to play a role in the pathogenesis of atherosclerosis [12, 13], likely mediated via toll-like receptor signaling pathways [4].
In a previous study we demonstrated that resistin and NGAL are upregulated in circulating leucocytes in ED patients with sepsis [14]. Importantly there was corresponding sustained correlation of serum levels with illness severity over the subsequent 24 h, making these molecules of potential clinical interest. NGAL has been most extensively studied as an early marker of acute kidney injury in a range of critical illnesses, including sepsis [15]. We postulate that Resistin and NGAL play a role in sepsis pathogenesis by promoting neutrophil-endothelial cell adhesion. Previous investigators have demonstrated Resistin-induced expression of the leucocyte adhesion molecules ICAM-1 and VCAM-1 in endothelial cells in vitro [16]. In vivo, these receptors are cleaved and released into the circulation in a soluble form that may be assayed as an indirect measure of endothelial activation [17]. The role of Resistin and NGAL as possible mediators of endothelial activation in clinical sepsis has not previously been studied.
The aims of the present investigation were to validate our previous findings of correlations between Resistin and NGAL and illness severity in sepsis; to explore relationships between resistin and NGAL, and biomarkers of systemic inflammatory responses and endothelial cell activation, specifically VCAM-1 and ICAM-1; and to investigate the relationship with clinical outcome including mortality.
Materials and methods
Design and setting
The Critical Illness and Shock Study (CISS) is an observational dataset of ED patients with a range of acute critical illnesses recruited at Royal Perth and Armadale-Kelmscott Hospitals, Perth, Australia. Details of the CISS methodology have previously been described [18]. In brief, patients meeting physiologic criteria for shock or organ failure undergo real-time data collection and serial research blood sampling over the initial 24 h, and are then followed for clinical outcomes. Recruitment is restricted to research nurse duty hours (0700–2100, up to 7 days of the week) necessitating convenience sampling.
Ethical approval and consent
Full ethical approval was obtained from the relevant institutional research committees. Written informed consent was obtained from participants or from next-of kin. Where prospective consent could not be obtained, provision for initial waiver of consent was granted under the terms of paragraph 2.3.6 of the Australian National Health and Medical Research Council guidelines for ethical conduct of research. All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research ethics committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Participants
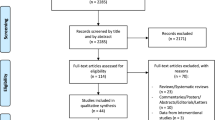
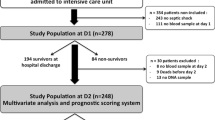
Patients recruited into CISS between March 2010 and July 2013, and who met criteria for sepsis according to the Surviving Sepsis campaign definitions [19] when in the ED were enrolled. We excluded patients transferred from other hospitals and for whom there were inadequate research blood samples for analysis. Sepsis cases were further classified as uncomplicated sepsis (SOFA score < 2 and no requirement for organ support), severe sepsis (SOFA score ≥ 2 and/or elevated serum lactate) and septic shock (persistent hypotension despite fluid resuscitation), according to SSC definitions. These three categories broadly correspond to the recently revised sepsis definitions as infection, sepsis and septic shock [1]. Therefore, the updated terminology will be utilized henceforth. This classification was undertaken without knowledge of the results of biomarker assays. A cohort of healthy subjects stratified for age and sex and with blood sampled at a single time point, served as a control group.
Clinical data collection
Data were collected on admission for baseline demographics, vital signs, investigations, interventions and suspected source of sepsis. Illness severity was estimated using the SOFA score [20], and comorbid disease burden by the CCS [21]. Follow-up data included results of microbial cultures, disposition from ED, ICU/hospital duration of stay and discharge diagnosis.
Blood sampling and sample storage
Blood samples (serum and plasma) were collected upon enrolment in the ED when inclusion criteria were met (T0) and at 1–2 h (T1), 3–6 h (T3) and 12–24 h (T24) subsequently. These were immediately centrifuged and the supernatant divided into 0.25 ml aliquots prior to storage at −80 °C for subsequent batch analysis.
Laboratory methods
Serum concentrations of Resistin and NGAL were measured using commercial ELISA kits (R&D Systems, Minneapolis, MN, USA). We measured two inflammatory cytokines, IL-6 and IL-10, and two soluble markers of endothelial cell activation, VCAM-1 and ICAM-1 by Cytometric Bead Array Flex Sets as described previously [22].
Outcomes and statistical methods
The clinical outcomes of interest were septic shock diagnosis, and mortality within 30 days of enrolment. We also compared levels of biomarkers between sepsis severity groups, and relationships with inflammatory cytokines and endothelial activation at baseline and over time. Continuous data are presented as median and interquartile range or as mean ± SD. Comparisons between groups (including the control group) at T0 were analysed using the Kruskal–Wallis test and where significant, pairwise comparisons were performed using Wilcoxon rank-sum (Mann–Whitney) test.
Relationships between markers over time in the sepsis groups were explored using an interaction of time and group in linear mixed models and, when values were censored due to assay limits, random effects Tobit regression. These regression techniques employ maximum likelihood estimation, which retains patients with incomplete data in the analysis, therefore producing unbiased estimates when missing data are missing at random. Biomarker outcomes were log-transformed and where distributions remained slightly skewed, bootstrapping was employed to obtain robust standard errors and p values. Relationships between Resistin and NGAL and the inflammatory and endothelial cell markers over the subsequent 24 h were examined using the interaction Resistin/NGAL and time in the model. Potential non-linearity was investigated using scatter plots with linear and LOWESS fits at each time point. There were a small number of patients with missing data due to death prior to 24 h post presentation. A sensitivity analysis was performed excluding these patients from the sample to assess their influence on the results.
The relationships between biomarker value at presentation and the outcomes of septic shock diagnosis and mortality were evaluated by logistic regression models incorporating biomarker results along with age, sex and CCS as predictor variables using a backward stepwise approach, and by the ROC AUC. Goodness of fit was assessed using the Hosmer–Lemeshow test and the optimal model selected using Akaike’s Information Criterion. To account for any bias associated with clinical decisions to limit goals of care, the mortality analysis was repeated for the subgroup admitted to ICU.
All analyses were performed using Stata 14 (College Station, TX, USA) and significance was concluded if p < 0.05. Given the exploratory nature of the study, no corrections were applied for multiple testing.
Results
Clinical outcomes
During the study period, 240 patients met enrolment criteria. We excluded 27 who were participants in a previously reported study [14] and for a further 27, blood samples were either missing or unsuitable for analysis giving a total of 186 participants. Of these, 28 had uncomplicated infection, 69 had sepsis and 89 met criteria for septic shock. In total 35 (19%) died within 30 days. Baseline participant characteristics are shown in Table 1. The most frequent clinical source of infection was respiratory tract, followed by urinary tract and skin/soft tissue. Causative organisms were isolated in 98 (41 with positive blood cultures) with approximately equal numbers of gram-positive and gram-negative organisms. Finally we analysed blood samples from 29 healthy controls.
Biomarker measurements
Figure 1 shows boxplots for the various biomarkers across the three patient groups at T0 compared to controls. Table 2 contains between group comparisons within each time point, as well as the results of the interaction of group and time derived from the random effects models (see below). At T0, median serum levels of Resistin were significantly higher in uncomplicated infection compared to controls (45 vs 11 ng/ml, p < 0.001) and in septic shock compared to non-shock sepsis (121 vs. 67 ng/ml, p < 0.001). Median NGAL concentration was also significantly higher in infection compared to controls (173 vs. 49 ng/ml, p < 0.001) and in septic shock compared to sepsis (552 vs. 289 ng/ml, p < 0.001). Both IL-6 and IL-10 were significantly higher in infection than controls (p < 0.001 for both), and higher in septic shock than in sepsis or infection. In contrast there was no significant difference in VCAM-1 or ICAM-1 level between infection and controls; however, both these markers were significantly higher in septic shock compared to sepsis and infection at T0. No significant differences were seen at T0 for IL-6, IL-10, VCAM-1 or ICAM-1 between sepsis and uncomplicated infection.
Boxplots for biomarkers at T0 by patient subgroup, and healthy controls. IL-6 and IL-10 log-transformed variable. See also Table 2 and text
Patterns of biomarkers over time
Figure 2 depicts the pattern of each marker over time across the three patient groups derived from the random effects models summarized in Table 2. For both Resistin and NGAL, there was no significant change over time in the sepsis and septic shock groups. In the uncomplicated infection group there was a significant increase between T3 and T24, such that there was no difference between infection and sepsis at 24 h.
IL-6 showed a significant decline from T0 to T24 in all three patient groups, but with no significant difference in the rate of this decline in the sepsis and septic shock groups compared to infection (p = 0.55 and 0.88, respectively). For IL-10, there were also significant declines between T0 and T24; again this did not differ significantly between the groups. At 24 h IL-10 remained higher in the septic shock group, but for IL-6 there was no difference between the groups. ICAM-1 and VCAM-1 did not vary significantly over time in any of the patient groups. A sensitivity analysis excluding 13 patients who died before 24 h, 12 of which were in the septic shock category, did not yield any substantial change in the results.
Relationships between markers
The relationships between Resistin and NGAL and the other biomarkers at each of the four sampling time points were investigated using random effects models (See Online Resource 1, Supplementary Figs. 1 and 2.pdf and Online Resource 2, Supplementary Tables 1 and 2.pdf). There was a significant positive association between Resistin and both IL-6 and at T0 (p < 0.001 for both), which did not significantly differ at T1 and T3, but declined significantly by T24. For the endothelial adhesion molecules, Resistin was significantly associated with VCAM-1 at T0 (p = 0.007), and this did not vary over time, while an association with ICAM-1 (p = 0.011 at T0) was significantly closer to zero at T3, but otherwise did not vary over time. NGAL showed significant relationships with IL-6 and IL-10 at T0 (p = 0.046 and 0.001, respectively), which did not change over time. There was also a significant association between NGAL and VCAM-1 at T0 (p = 0.011), which did not vary over time. The association between NGAL and ICAM-1 at T0 did not reach statistical significance (p = 0.065), and similarly this did not significantly alter over time.
Relationships between biomarkers and clinical outcomes
Table 3 shows the association between each of the six biomarkers measured on admission (T0) and lactate as predictors of septic shock and 30 day mortality. Both Resistin and NGAL showed significant correlation with SOFA score (Spearman’s rho 0.41, p < 0.001 and 0.51, p < 0.001, respectively). SOFA score was included in the analysis for mortality as a comparison measure but not for septic shock, to avoid incorporation bias. None of the biomarkers alone showed good predictive characteristics when assessed by ROC AUC. NGAL was superior to lactate for diagnosis of septic shock (AUC 0.74 vs. 0.63, p = 0.035). In contrast lactate was superior to Resistin for predicting mortality among the subgroup of patients admitted to ICU only (AUC 0.87 vs. 0.73, p = 0.034). For Septic Shock, Resistin, VCAM-1 and lactate provided the optimal model with AUC 0.76 (0.69–0.82), while for mortality this comprised NGAL, lactate, CCS and age, with AUC 0.80 (0.73–0.85). Models containing both Resistin and NGAL were not superior to models with these markers alone due to co-linearity. Details of these models are shown (Online Resource 3, Supplementary Appendix.pdf).
Discussion
In this exploratory observational study we confirmed previous findings that Resistin and NGAL are associated with illness severity and clinical outcome in sepsis. In addition both are significantly elevated in septic shock compared to uncomplicated infection at 24 h from admission. The reason for a rise in both Resistin and NGAL by 24 h in the uncomplicated infection group is not clear, and is not explained by missing data. In contrast, the inflammatory markers IL-6 and IL-10, while showing similar associations on presentation, were significantly attenuated by 24 h. Our hypothesis about a relationship between Resistin and NGAL with expression of the endothelial cell adhesion molecules VCAM-1 and ICAM-1 is supported by our data; however, neither of these molecules was found to have a strong association with outcome in this study.
The role of NGAL as a marker of acute kidney injury, and as a prognostic indicator in sepsis has been the subject of significant previous research [15]. Our results are similar to Shapiro et al. who found NGAL to have a ROC AUC of 0.75 (0.68–0.82) for in-hospital mortality in sepsis [23]. Resistin, an adipokine hormone with possible pathogenic roles in diabetes and obesity has been the subject of only limited study in sepsis [11–13]. Our previous finding of increased expression of Resistin and NGAL, by circulating leucocytes in sepsis [14], coupled with evidence for interaction between Resistin and endothelial cells in the pathogenesis of vascular disease [9], led us to postulate that both these molecules mediate leucocyte-endothelial cell signaling and therefore play a pathogenic role in the development of septic shock.
Resistin and NGAL both significantly correlated with inflammation. IL-6 and IL-10 are cytokine markers of severity of the inflammatory response. Our results confirm significantly higher levels of both IL-6 and IL-10 in patients with infection compared to healthy controls; however, there was limited association with sepsis severity and prognosis. While median values of both cytokines at presentation were higher in the septic shock group, there was large variability, and levels attenuated significantly within 24 h. Other investigators have shown limited utility for both IL-6 and IL-10 to predict mortality in sepsis [24, 25].
We found associations between Resistin/NGAL and the endothelial markers ICAM-1 and VCAM-1. While these soluble endothelial adhesion molecules were associated with severity of illness, they had no relationship with mortality. Previous investigators have shown relationships between increased expression of these markers and illness severity/outcome in sepsis; however, the results of these studies have been variable [26]. This may be due to different patient cohorts (post-operative versus community-acquired sepsis) or clinical settings (ICU vs. ED). Shapiro et al. found only moderate associations between ICAM-1/VCAM-1 with illness severity and mortality in ED patients [17]. Others have suggested a potential protective role for shedding of endothelial adhesion molecules during sepsis [27], with elevated ICAM -1 levels being associated with better outcome in septic children [28]. Thus our findings are not inconsistent with an effect of Resistin and/or NGAL on the endothelium. Of note, while this work focused on two specific leucocyte adhesion molecules, there are multiple markers of endothelial cell activation in sepsis, reflecting the vast array of biological functions undertaken by these cells [5, 26]. Analysis of alternative activation markers may yield different associations with clinical outcome.
The design of this study encompassed pragmatic, clinically relevant enrollment criteria, data and sample collection during the early phase of treatment in the ED, and standardized outcome definitions. Biomarker analyses were performed blinded to clinical data. However, non-consecutive recruitment and incomplete blood sampling on all subjects were limiting factors. To mitigate their influence, we employed statistical techniques robust to data missing at random, and undertook a sensitivity analysis to exclude deaths within the first 24 h, which did not alter the results.
These findings have implications at both a basic science and clinical level, confirming the role of the vascular endothelium in sepsis pathogenesis [2, 3]. Further investigation into the cellular mechanisms by which Resistin acts is important for potential future therapeutic advances. Resistin along with NGAL is also consistently associated with sepsis severity and outcomes. Although, based upon our results, neither is sufficiently accurate alone for diagnosis or prognosis in sepsis, the fact that the signal appears time-insensitive in the dynamic setting of acute sepsis increases the attraction as potential tools for risk-stratification, perhaps in combination with other biomarkers or clinical parameters.
Conclusion
Resistin and NGAL are associated with illness severity in sepsis and correlate with inflammatory response, and expression of endothelial cell adhesion molecules VCAM-1 and ICAM-1 Further evaluation of the role of Resistin and NGAL in the pathogenesis of septic shock is warranted.
Abbreviations
- AUC:
-
Area under the curve
- CCS:
-
Charlson comorbidity score
- CISS:
-
Critical illness and shock study
- ED:
-
Emergency department
- ICU:
-
Intensive care unit
- ICAM-1:
-
Inter-cellular adhesion molecule-1
- IL-6:
-
Interleukin-6
- IL-10:
-
Interleukin-10
- LOWESS:
-
Locally weighted scatterplot smoothing
- NGAL:
-
Neutrophil gelatinase-associated lipocalin
- ROC:
-
Receiver operator characteristic
- SOFA:
-
Sequential organ failure assessment
- VCAM-1:
-
Vascular cell adhesion molecule-1
References
Singer M, Deutschman CS, Seymour CW, Shankar-Hari M, Annane D, Bauer M, et al. The third international consensus definitions for sepsis and septic shock (sepsis-3). JAMA. 2016;315:801–10.
Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369:840–51.
van Ierssel SH, Jorens PG, Van Craenenbroeck EM, Conraads VM. The endothelium, a protagonist in the pathophysiology of critical illness: focus on cellular markers. Biomed Res Int. 2014;2014:985813.
Khakpour S, Wilhelmsen K, Hellman J. Vascular endothelial cell toll-like receptor pathways in sepsis. Innate Immun. 2015;21:827–46.
Skibsted S, Jones AE, Puskarich MA, Arnold R, Sherwin R, Trzeciak S, et al. Biomarkers of endothelial cell activation in early sepsis. Shock. 2013;39:427–32.
Sundén-Cullberg J, Nyström T, Lee ML, Mullins GE, Tokics L, Andersson J, et al. Pronounced elevation of resistin correlates with severity of disease in severe sepsis and septic shock. Crit Care Med. 2007;35(6):1536–42.
Vassiliadi DA, Tzanela M, Kotanidou A, Orfanos SE, Nikitas N, Armaganidis A, et al. Serial changes in adiponectin and resistin in critically ill patients with sepsis: associations with sepsis phase, severity, and circulating cytokine levels. J Crit Care. 2012;27:400–9.
Aliefendioglu D, Gürsoy T, Çağlayan O, Aktaş A, Ovalı F. Can resistin be a new indicator of neonatal sepsis? Pediatr Neonatol. 2014;55:53–7.
Steppan CM, Bailey ST, Bhat S, Brown EJ, Banerjee RR, Wright CM, et al. The hormone resistin links obesity to diabetes. Nature. 2001;409:307–12.
Park HK, Ahima RS. Resistin in rodents and humans. Diabetes Metab J. 2013;37:404–14.
Johansson L, Linnér A, Sundén-Cullberg J, Haggar A, Herwald H, Loré K, et al. Neutrophil-derived hyperresistinemia in severe acute streptococcal infections. J Immunol. 2009;183:4047–54.
Verma S, Li S-H, Wang C-H, Fedak PWM, Li R-K, Weisel RD, Mickle DAG. Resistin promotes endothelial cell activation: further evidence of adipokine-endothelial interaction. Circulation. 2003;108:736–40.
Jamaluddin MS, Weakley SM, Yao Q, Chen C. Resistin: functional roles and therapeutic considerations for cardiovascular disease. Br J Pharmacol. 2012;165:622–32.
Macdonald SPJ, Stone SF, Neil CL, van Eeden PE, Fatovich DM, Arendts G, Brown SGA. Sustained elevation of resistin, NGAL and IL-8 are associated with severe sepsis/septic shock in the emergency department. PLoS ONE. 2014;9:e110678.
Zhang A, Cai Y, Wang P-F, Qu J-N, Luo Z-C, Chen X-D, et al. Diagnosis and prognosis of neutrophil gelatinase-associated lipocalin for acute kidney injury with sepsis: a systematic review and meta-analysis. Crit Care. 2016;20:41.
Hsu W-Y, Chao Y-W, Tsai Y-L, Lien C-C, Chang C-F, Deng M-C, et al. Resistin induces monocyte-endothelial cell adhesion by increasing ICAM-1 and VCAM-1 expression in endothelial cells via p38MAPK-dependent pathway. J Cell Physiol. 2011;226:2181–8.
Shapiro NI, Schuetz P, Yano K, Sorasaki M, Parikh SM, Jones AE, et al. The association of endothelial cell signaling, severity of illness, and organ dysfunction in sepsis. Crit Care. 2010;14:R182.
Arendts G, Stone SF, Fatovich DM, van Eeden P, MacDonald E, Brown SG. Critical illness in the emergency department: lessons learnt from the first 12 months of enrolments in the critical illness and shock study. Emergency Med Australas. 2012;24:31–6.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, et al. Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock: 2012. Crit Care Med. 2013;41:580–637.
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. Intensive Care Med. 1996;22:707–10.
Charlson ME, Pompei P, Ales K, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chron Dis. 1987;40:373–83.
Stone SF, Cotterell C, Isbister GK, Holdgate A, Brown SGA. Elevated serum cytokines during human anaphylaxis: identification of potential mediators of acute allergic reactions. J Allergy Clin Immunol. 2009;124(786–92):e4.
Shapiro NI, Trzeciak S, Hollander JE, Birkhahn R, Otero R, Osborn T, et al. The diagnostic accuracy of plasma neutrophil gelatinase-associated Lipocalin in the prediction of acute kidney injury in emergency department patients with suspected sepsis. Ann Emerg Med. 2010;56(52–59):e1.
Wunder C, Eichelbronner O, Roewer N. Are IL-6, IL-10 and PCT plasma concentrations reliable for outcome prediction in severe sepsis? A comparison with APACHE II and SAPS II. Inflamm Res. 2004;53:158–63.
Marecaux G, Pinsky MR, Dupont E, Kahn RJ, Vincent JL. Blood lactate levels are better prognostic indicators than TNF and IL-6 levels in patients with septic shock. Int Care Med. 1996;22:404–8.
Xing K, Murthy S, Liles WC, Singh JM. Clinical utility of biomarkers of endothelial activation in sepsis: a systematic review. Crit Care. 2012;16:R7.
Zonneveld R, Martinelli R, Shapiro NI, Kuipers TW, Plotz FB, Carman CV. Soluble adhesion molecules as markers for sepsis and the potential pathophysiological discrepancy in neonates, children and adults. Crit Care. 2014;18:204.
Briassoulis G, Papassotiriou I, Mavrikiou M, Lazaropoulou C, Margeli A. Longitudinal course and clinical significance of TGF-β1, sL- and sE-Selectins and sICAM-1 levels during severe acute stress in children. Clin Biochem. 2007;40:299–304.
Acknowledgements
Dr Shelley Stone undertook preparatory work towards this project. We also acknowledge the contributions of Ellen Macdonald, Sophie Damianopoulos and the research nurses at the participating hospitals.
Funding
The Australasian College for Emergency Medicine (ACEM) Foundation New Investigator award, and the Royal Perth Hospital Medical Research Foundation funded this research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no other conflicts of interest.
Additional information
Responsible Editor: Bernhard Gibbs.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Macdonald, S.P.J., Bosio, E., Neil, C. et al. Resistin and NGAL are associated with inflammatory response, endothelial activation and clinical outcomes in sepsis. Inflamm. Res. 66, 611–619 (2017). https://doi.org/10.1007/s00011-017-1043-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-017-1043-5