Abstract
Objective
To elucidate if TLR4-mediated MyD88 and TRIF signalling by the clinically applicable Lipopolysaccharide (LPS)-derivative monophosphoryl lipid A (MPLA) in primary human dendritic cells requires LPS cofactors LPS-binding protein (LBP) and CD14.
Methods
Cytokine production by monocyte-derived DCs stimulated with MPLA or LPS was determined using ELISA. To investigate involvement of CD14 for action of LPS or MPLA, CD14 was inhibited using blocking antibodies or down-modulated using specific siRNA. To assess involvement of LBP monocyte-derived DCs were stimulated in serum-free culture medium in absence or presence of purified LBP.
Results
LBP and CD14 are not required for and do not enhance the capacity of MPLA to induce MyD88- and TRIF-dependent pro-inflammatory IL-6 and TNF-α. Interestingly, although CD14 is required for TRIF-dependent downstream events in mice, we show that in human CD14 is redundant for MPLA-induced TRIF-dependent chemokine production.
Conclusions
These findings provide novel insight in the modes of action of MPLA in human and show that, compared to LPS, MyD88 and TRIF signalling in dendritic cells by MPLA is not mediated nor amplified by TLR4 cofactors. This gives insight why MPLA induces immune activation without provoking toxicity in human and clarifies why MPLA can be used as activating compound for clinically applicable immuno-activatory cellular products grown in serum-free regimens.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monophosphoryl lipid A (MPLA) is a detoxified LPS-variant that still acts as a potent Toll-like receptor 4 (TLR4) ligand to activate antigen-presenting cells. Therefore, MPLA is a popular vaccine adjuvant and there is increasing interest for the use of MPLA in clinical immunostimulatory cellular products [1, 2]. Whereas lipopolysaccharide (LPS) consists of a hydrophilic repeating polysaccharide chain (O-antigen), core oligosaccharide and an amphipathic biphosphorylated lipid A component, MPLA is only comprised of a monophosphate-linked lipid A. Compared to LPS or lipid A this structure has a low-toxicity profile [3–5]. Both LPS and MPLA are immunostimulatory components, capable of inducing a Th1 response [6, 7]. The toxicity mediated by LPS prevents its use in a clinical setting, while in several vaccines MPLA is successfully being used as a clinical adjuvant [1, 2].
When ligated at the cell membrane TLR4 signals via the MyD88-dependent signalling pathway, while after endocytosis TLR4 signals via the TRIF-dependent pathway [8–11]. Classically, only signalling via the MyD88-dependent pathway has been linked to production of pro-inflammatory cytokines [8], but TRIF-dependent signalling is equally important for induction of pro-inflammatory cytokines [12, 13]. Signalling via the TRIF-dependent pathway has been linked to production of type I interferons, chemokines IP-10 and RANTES and upregulation of co-stimulatory molecules on the cell membrane [12–14]. In human monocyte-derived DCs (moDCs) production of chemokine RANTES is dependent exclusively on the TRIF-dependent pathway, while production of pro-inflammatory cytokines is dependent on both the TRIF- and MyD88-dependent pathways [13].
By itself LPS is a poor activator of TLR4. The cofactors LPS-binding protein (LBP) and CD14 are required to deliver LPS to the TLR4/MD-2 complex [15–17] that acts as the LPS receptor [18, 19]. Because of its hydrophobic nature, LPS is mostly present in micelles when in an aqueous environment. LBP, present in serum at average levels of 7.5 μg/ml, is required to extract single molecules of LPS from bacterial membranes or micelles and to transfer it to CD14 [20–24]. CD14, which can be present both in soluble form and as a membrane-bound receptor on the target cell, subsequently transfers LPS to the TLR4/MD2 complex. There it chaperones the process of dimerization of TLR4/MD2 complexes which is followed by activation of intracellular signalling cascades [19, 25–28].
During ligation, the lipid A portion of LPS partially binds to the co-receptor MD2. Both lipid A and MD-2 show direct interaction with TLR4. Five of the six acyl chains of lipid A are buried in the hydrophobic pocket of MD-2, while one acyl chain is exposed on its surface. This acyl chain is important for dimerization of the TLR4/MD2 complex. In addition, hydrophilic interactions between the phosphate groups of lipid A and the positively charged residues in TLR4 are important in dimerization [27, 29]. Dimerization of TLR4/MD2 complexes is required for strong activation of MyD88 and TRIF. In addition, in mice CD14 has been shown to be important for induction of TLR4 endocytosis [30–32] and thereby for activation of the TRIF-dependent pathway by LPS [30, 31, 33–36]. In this manner CD14 promotes MyD88- and TRIF-dependent signal transduction.
The toxic profile of LPS is linked to the induction of the pro-inflammatory cytokines via MyD88 and TRIF. Signalling via TRIF and induction of the TRIF-dominated cytokines is not toxic and still allows induction of adaptive immunity in mice [31, 37, 38]. One of the two phosphate groups present on LPS is absent on MPLA. Since these phosphate groups interact with the dimerization interface of TLR4, the lack of a phosphate group on MPLA may cause decreased dimerization of TLR4 complexes [39]. In mice this dimerization is required for MyD88-dependent signalling, but not for TRIF-dependent signalling [36]. Still, CD14 dependency for TRIF signalling by MPLA has been reported in mice as well [31]. We have observed that in human MPLA, like LPS, uses both TRIF- and MyD88-dependent signal transduction routes [13]. It remains to be elucidated, however, whether the MyD88 and TRIF signalling cascades upon activation of TLR4 by MPLA are under the control of the LBP/CD14 axis in human. Insight in this question may provide a rationale for the efficacy and safety of MPLA as a clinical adjuvant.
Materials and methods
Generation of monocyte-derived DCs
Monocytes were isolated from fresh aphaeresis material of healthy volunteers (Sanquin Blood Supply, Amsterdam, The Netherlands) upon informed consent using the Elutra™ cell separation system (Gambro, Lakewood, US), as described previously [6, 40]. Monocytes were cultured in Cellgro DC serum-free culture medium supplemented with GM-CSF (1000 IU/ml), IL-4 (800 IU/ml) (Cellgenix, Freiburg, Germany), penicillin (100 U/ml) and streptomycin (100 μg/ml) (Invitrogen Breda, The Netherlands). After 6 days of culture immature DCs (iDCs) were harvested for further experiments.
Maturation of DCs
iDCs were seeded at 100.000 cells/well in a 96-wells plate (Nunc, Roskilde, Denmark) in Cellgro culture medium (Cellgenix, Freiburg, Germany), penicillin (100 U/ml) and streptomycin (100 μg/ml) (Invitrogen Breda, The Netherlands), supplemented with 1 % fetal calf serum (FCS) (Bodinco, Alkmaar, The Netherlands) in case of LPS stimulation. Cells were stimulated with indicated concentrations of LPS from S. typhimurium (LPSs) (Sigma Aldrich, Steinheim, Germany), ultrapure LPS from E. coli O111B4 (LPSe) (Invivogen, San Diego, US), MPLA from S. minnesota re595 (MPLAs) (Sigma) or synthetic MPLA from E. coli r515 (MPLAe, contains six 14C acyl chains) (Invivogen).
CD14 inhibition
iDCs were matured as described above in absence or presence of monoclonal anti-CD14 blocking antibody (mouse anti-human CD14.22 was obtained from Prof. dr. van der Schoot, Sanquin Blood Supply) or irrelevant IgG1 control antibody directed to cat allergen FelD1 (Sanquin Reagents, Amsterdam, The Netherlands). Culture supernatants were harvested 24 h after addition of stimuli. Production of IL-6 and TNF-α was determined using PeliKine-compact ELISA kits (Sanquin Reagents). For detection of RANTES a DuoSet ELISA kit (R&D systems, Minneapolis, US) was used.
siRNA-mediated down-regulation of CD14, MyD88 or TRIF
Specific CD14-targeting siRNA (Thermo Scientific, Lafayette, US) was used for down-regulation of CD14. MyD88 or TRIF was down-regulated as described previously [13] using ON-TARGET plus SMARTpool siRNA. Three days after monocyte isolation 5 × 106 cells were electroporated with 3 μg siRNA/1 × 106 cells in 200 µl Cellgro culture medium in 4 mm cuvettes (BioRad, Carlsbad, US) using the BioRad Gene Pulser Xcell (BioRad) (250 V, 150 μF). After electroporation DCs were resuspended in culture supernatant and cultured for an additional 3 days before stimulation with LPS or MPLA.
LBP assay
iDCs were seeded at 100.000 cells/well in Iscove’s modified Dulbecco’s medium (IMDM) (Bio Whittaker, Verviers, Belgium) containing penicillin/streptomycin in a 96-wells plate. iDCs were stimulated with indicated concentrations of LPS and MPLA in absence or presence of 12.5 ng/ml purified human LBP (Hycult Biotech, Uden, The Netherlands). Culture supernatants were harvested 24 h after addition of stimuli.
Signal transduction
After stimulation with 50 ng/ml LPSe +1000 IU/ml IFNγ in presence of 1 % FCS or 2.5 μg/ml MPLAs +1000 IU/ml IFNγ, DCs were fixated with 4 % paraformaldehyde and subsequently permeabilized with 90 % methanol. For determination of nuclear translocation of NFκB DCs were stained with nuclear dye DRAQ5 (Cell Signaling Technology, Danvers, US) and rabbit anti-NFκB p65 polyclonal antibody E498 (Cell Signaling Technology). Approximately 20,000 cells per sample were imaged using ImageStream X (Amnis, Seattle, US), nuclear translocation of NFκB was quantified using Ideas software using the nuclear localization wizard and is depicted as similarity score (Amnis). Nuclear translocation was quantified as the ‘mean similarity’ between NFκB staining and nuclear DRAQ5 staining, a method recommended by the manufacturer of the ImageStream X. A high mean similarity (+1, +2) indicates overlap in NFκB and nuclear staining, or nuclear translocation of NFκB, whereas low or negative mean similarity (−1, 0) indicates little or no overlap and thus no NFκB nuclear translocation.
Statistical analysis
Data are shown as mean ± SEM. To compare the relative ability of LPS to stimulate DCs in presence or absence of monoclonal CD14-blocking antibodies, the amount of LPS required to induce 20 % of the maximum of TNF-α or IL-6 production in control antibody-treated DCs was determined from each dose–response curve (EC20 CTRL). This concentration was divided upon the LPS concentration required to induce the same amount of cytokine production in anti-CD14 blocking antibody-treated DCs (EC20 aCD14). A paired t test was used for statistical analysis, for normalized cytokine production a one sample t test was performed. Cytokine production by LPS-treated DCs in the LBP assays was not normally distributed, as tested by D’Agostino and Pearson omnibus normality test, therefore a Wilcoxon signed rank test was used for statistical analysis. All statistical analyses have been performed using PRISM 5.01 software (GraphPad, La Jolla, US).
Results
LBP is required for LPS-mediated cytokine production, but dispensable for MPLA
Under serum-free conditions, LPS stimulation of DCs required LBP in a concentration-dependent manner, in line with previous publications (Fig. 1a, c–e, S1A) [22, 41]. In contrast, LBP did not affect MPLA-mediated stimulation of TLR4 (Fig. 1b, f–h, S1B). Addition of 12.5 ng/ml LBP to the serum-free culture medium did not increase production of TNF-α and IL-6 [which, in moDCs, is dependent on both MyD88 and TRIF-dependent signalling ([13]; Fig. S2A, B)] or production of RANTES [which is exclusively dependent on TRIF-dependent signalling ([13]; Fig. S2C)] by DCs matured by synthetic MPLAe (Fig. 1f–h) or highly purified MPLAs (Fig. S1C, D).
MPLAe can induce cytokine production in absence of LBP. a, b TNF-α production by DCs stimulated in presence of a titration of LBP in serum-free IMDM with a 10 ng/ml LPSe, a representative experiment (n = 6), or b 10 μg/ml MPLAe, a representative experiment (n = 7). c–e TNF-α (c), IL-6 (d) and RANTES (e) production induced in absence or presence of 12.5 ng/ml LBP by DCs stimulated with indicated concentrations of LPSe, n = 8. e RANTES production is shown normalized to RANTES production at 2.5 ng/ml LPS. RANTES production in ng/ml mean ± SEM: 0.6 ng/ml LPS 0.7 ± 0.6; 0.6 ng/ml LPS + LBP 0.7 ± 0.9; 2.5 ng/ml LPS 1.7 ± 0.6; 2.5 ng/ml LPS + LBP 2.5 ± 0.9; 10 ng/ml LPS 2.8 ± 1.6; 10 ng/ml LPS + LBP 3.0 ± 1.11 f–h TNF-α (f), IL-6 (g) and RANTES (h) production in presence or absence of 12.5 ng/ml LBP by DCs stimulated with indicated concentrations of MPLAe, n = 7. Grey bars only medium, black bars LBP. Data are shown as mean + SEM. Cytokine production by unstimulated DCs: TNF-α 0.02 ± 0.01 ng/ml, IL-6 0.06 ± 0.02 ng/ml, RANTES was below detection limit (50 ng/ml). For statistical analysis a Wilcoxon signed rank test was performed. *p < 0.05, **p < 0.01
Thus, while LBP is required for LPS-mediated stimulation of TLR4, MPLA-mediated TLR4 stimulation and activation of the MyD88 and TRIF pathways does not require, nor is enhanced, by LBP.
MPLA-mediated TRIF-dependent cytokine production is CD14-independent
To investigate possible CD14 dependency of MPLA for TLR4 stimulation, production of pro-inflammatory cytokines TNF-α and IL-6, as well as production of TRIF-dependent chemokine RANTES (CCL5) was analysed in presence of CD14-blocking antibodies in human monocyte-derived DCs. Blockage of CD14 significantly decreased the potency of LPS derived from S. typhimurium (LPSs) (Fig. 2a–d) or E. coli O111B4 (LPSe) (Fig. S3A–C) to induce TNF-α, IL-6, or RANTES in DCs. This is in accordance with previous studies [41, 42]. In contrast, presence of CD14-blocking antibodies showed no inhibitory effect on the potency of MPLA derived from S. minnesota re595 (MPLAs) to induce production of pro-inflammatory cytokines IL-6 and TNF-α, while production of TRIF-dependent chemokine RANTES was even slightly enhanced (Fig. 2e–j). Similar results were obtained when DCs were stimulated with MPLA derived from E. coli r515 (MPLAe) (Fig. S3D–G).
CD14 is dispensable for MPLAs-mediated cytokine production. Cytokine production by DCs stimulated with LPSs (a–d) or MPLAs (e–j) in the presence of control antibodies (CTRL) (grey lines) or CD14-blocking antibodies (α-CD14) (black lines). LPSs stimulated production of TNF-α (a), IL-6 (b), or RANTES (c), a representative experiment (n = 4). d LPSs responsiveness to α-CD14 treatment is quantified as described in materials and methods, n = 4, a paired t test was performed for statistical analysis, ***p < 0.001. MPLAs-stimulated production of TNF-α (e), IL-6 (f), or RANTES (g), a representative experiment (n = 6). MPLAs-stimulated production of TNF-α (h), IL-6 (i), or RANTES (j), as a % of CTRL condition n = 6. A one sample t test was performed for statistical analysis. *p < 0.05, **p < 0.01
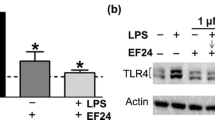
Some antibodies targeting CD14 can induce endocytosis of CD14 and TLR4 [43]. To verify that the apparent CD14 independency of MPLA activity was not caused by increased TLR4 internalization by the anti-CD14 antibodies, CD14 was also down-regulated in moDCs using siRNA (Fig. 3a–c). This resulted in similar findings; when compared to CTRL siRNA-treated DCs (Fig. 3d–f); the potency of LPSs for induction of TNF-α or RANTES production was decreased in CD14 siRNA-treated DCs, whereas CD14 down-regulation showed no inhibitory effect on MPLAs-induced TNF-α or RANTES production (Fig. 3g–j). Thus, interestingly, while CD14 is required for optimal LPS-mediated cytokine production, CD14 does not contribute to MPLA-mediated MyD88- and TRIF-dependent cytokine production by DCs.
CD14 down modulation indicates that CD14 is dispensable for MPLAs-mediated cytokine production. Three days after the start of the differentiation, imDC were electroporated with siRNA targeting CD14 (siCD14) or control siRNA (siCTRL). Three days after electroporation iDCs were harvested and stimulated with LPSs or MPLAs. a, b Expression of CD14 (a) and CD40 (b) determined by flow cytometry upon iDC harvesting, a representative experiment, n = 3. c Relative expression of CD14 and CD40 after siCD14 treatment, n = 3. d, e LPSs-mediated TNF-α production (d) or RANTES production (e) in DCs treated with CTRL siRNA (grey lines) or CD14-targeting siRNA (black lines), a representative experiment, n = 3. f LPSs responsiveness by siCD14 treatment is quantified as described in materials and methods, n = 3. g, h MPLAs-mediated TNF-α production (g) or RANTES production (h) in DCs treated with CTRL siRNA (grey lines) or CD14-targeting siRNA (black lines) a representative experiment out of three experiments. i, j MPLAs-stimulated production of TNF-α (i), RANTES (j), as a % of CTRL condition, mean + SEM, n = 3
Serum factors are not required for MPLA-mediated signal transduction, but do increase speed of signalling
The above experiments show that LBP and CD14 are required for TLR4 stimulation by LPS, but not by MPLA. To investigate if the differences in requirement of MPLA and LPS for LBP and CD14 were related to the efficiency of TLR-4-induced signal transduction, nuclear translocation of NFκB p65 in response to TLR4 stimulation by MPLA or LPS in presence of interferon gamma was analysed. Figure 4a and b illustrate the method of quantification of NFκB nuclear translocation. Presence of LBP-containing FCS was obligatory to induce LPS-mediated nuclear translocation of NFκB p65, while MPLA-induced nuclear translocation of NFκB p65 did not require FCS (Fig. 4c, d). Although serum factors did not affect optimal production of cytokines (Figs. 1, 2, 3) or maximal activation of NFκB by MPLA (Fig. 4c), MPLA-mediated NFκB nuclear translocation occurred faster in presence of FCS (Fig. 4c, d). Altogether these data indicate that addition of serum factors enhances the rate of MPLA-mediated TLR4 signalling, but that this is not necessary for optimal NFκB activation or cytokine production.
MPLA-induced signal transduction occurs faster in presence of serum factors. In absence or presence of FCS DCs were stimulated with MPLA (2.5 μg/ml) + IFNγ (1000 U/ml) or LPSe (50 ng/ml) + IFNγ (1000 U/ml). At different time points after stimulation DCs were fixed and stained for NFκB. Nuclear translocation of NFκB (similarity score, a calculation of overlap between NFκB and nuclear staining) was determined using ImageStream. a Representative example of nuclear (top row) and NFκB staining (middle row) and overlay of nuclear staining (red) and NFκB (green) of LPS-stimulated cells. Representative cells displaying no nuclear translocation (mean similarity 0), little nuclear translocation (mean similarity 0 and 1) or a high level of nuclear translocation (mean similarity 2) are shown. b Histogram showing NFκB nuclear translocation (similarity score) of immature DCs stimulated with LPSe for 0′, 5′, 15′, or 30′. c Nuclear translocation of NFκB (similarity score) after stimulation with LPSe or MPLAs in time, n = 2. d A two-way ANOVA was used for statistical analysis, *p < 0.05, **p < 0.01, ***p < 0.001
Discussion
Detoxified LPS-variant MPLA provides potent TLR4 activation, but has low toxicity when compared to LPS. Recently, the induction of type I IFN by TLR4 agonists and the subsequent autocrine effects of type I IFN have been indicated to contribute to the bias that TLR4 exhibits for signalling via TRIF. This bias induces an immunostimulatory response with decreased toxicity, while at the same time only weakly activating the toxic MyD88-dependent pro-inflammatory responses [44]. Here, we investigated whether MPLA-mediated TLR4 stimulation can be enhanced by cofactors LBP and CD14, as has been described for LPS, and whether differences in dependence on these cofactors may also contribute to the difference in mediation of toxic effects between LPS and MPLA. Our results show that MPLA-induced MyD88- and TRIF-dependent pro-inflammatory cytokine and TRIF-dominated chemokine production is not amplified by either CD14 or LBP. A constant potency of MPLA to activate the TRIF pathway is important for the adjuvant action of MPLA, as this pathway is needed to confer immune responses [38]. The independency of the LBP/CD14 axis explains the ability of MPLA to efficiently induce maturation of pro-inflammatory DCs under serum-free conditions [6, 13, 40]. The lack of LBP/CD14-mediated amplification of the signalling pathways that induce pro-inflammatory cytokines is in line with the nontoxic profile of MPLA, as for LPS these pro-inflammatory cytokines were linked to its toxicity [38].
Even though TLR4 signalling is very similar in mice and human, it is not identical. For example there are species-dependent differences in response to TLR4 ligands, e.g. lipid A analogue lipid IVa functions as a TLR4-antagonist in human, but as a TLR4-agonist in mice [45]. These differences are probably caused by subtle differences between human and mouse TLR4 and MD2 [46]. The essential role of LBP in LPS and lipid A stimulation of TLR4 has been well described in human and mouse [21, 22], and LBP has recently been shown to be required for MPLA-induced TNF-α production in mouse DCs [36]. In contrast to these recent findings in mice, we show that, while LBP is necessary for LPS-mediated cytokine and chemokine production, it is dispensable for MPLA-mediated cytokine and chemokine production. LBP binds mostly to the hydrophobic portion of LPS [47, 48], which suggests that LBP might be capable of binding to MPLA and be as efficient in removing MPLA from micelles as it is in removing LPS. In absence of CD14 LBP is incapable of transferring LPS to TLR4 [28] and of enhancing LPS-mediated stimulation of SW620 cells [15]. Since absence or blockage of CD14 does not impair MPLA-induced cytokine production by DCs, the inability of LBP to improve MPLA-induced TLR4-mediated cytokine production is probably caused by an inability of CD14 to acquire MPLA from LBP and subsequently deliver it to TLR4.
Confirming previous research showing that CD14 plays an important role in presenting and orienting LPS to TLR4 [19, 26, 49], LPS-induced production of MyD88-dependent pro-inflammatory cytokines TNF-α and IL-6 is decreased when CD14 is blocked or down-regulated. However, similar to research using biphosphorylated lipid A [33, 36, 41, 43, 50], MPLA-mediated stimulation of TLR4 is CD14-independent since pro-inflammatory cytokine production is not affected by blocking or down-regulation of CD14, which is in line with the results of Tanimura and colleagues [36] in mice. Gangloff and colleagues suggest that CD14 discriminates structural differences between LPS variants such that CD14 increases responsiveness to complete LPS, while CD14-negative cells are more responsive to lipid A than to LPS [41, 51].
Since structural differences between MPLA and LPS exist, it is possible that MPLA can bind with decreased efficiency to CD14, which in turn may be a reason for the inability of CD14 to enhance MPLA-mediated TLR4 stimulation. Several observations suggest that LPS-carbohydrate chains are important for CD14 binding: CD14 has been shown to bind to the carbohydrate chains of LPS [52] and deacylated LPS (consisting only of carbohydrate chains, but lacking acyl chains) is still capable of binding to CD14 as well [53]. The crystal structure of human CD14 shows that, in addition to the hydrophobic pocket which is instrumental in ligand binding, two other sites on CD14 might be significant for ligand binding. One of those sites is hydrophilic and might be important for orienting or binding LPS [49]. MPLA contains very few hydrophilic residues which suggests that MPLA may have a decreased ability to bind to CD14 and thereby cannot use CD14 to enhance presentation to TLR4.
Consistent with dependency of LPS on serum-factors CD14 and LBP for production of cytokines, we observed minimal NFκB nuclear localization upon LPS stimulation in absence of FCS. The significant NFκB nuclear translocation induced by MPLA in absence of serum compared to LPS confirmed that MPLA is not dependent on serum factors to induce TLR signalling. Interestingly, even though LBP and CD14 are not required for cytokine and chemokine production, MPLA-induced nuclear translocation of NFκB occurs faster in presence of LBP and CD14-containing serum. TLR4 heterotetramerization has been described to be important for ligand-induced signalling and decreased heterotetramerization of TLR4/MD2 and slower activation of NFκB have been reported for TLR4 activation in absence of CD14 or LBP [18, 28]. In this light, our data suggest that, also for MPLA, heterotetramerization of TLR4/MD2 is more efficient in presence of cofactors, but that this increase in speed of translocation does not correlate with induction of higher cytokine production. The latter may be more related to the total efficiency of NFκB nuclear translocation by MPLA, a parameter that was not affected by serum.
CD14 has been shown to play an important role in endocytosis of TLR4 [30, 31, 33–35], a process required for induction of TLR4-mediated TRIF signalling [37]. Therefore, membrane CD14 is considered to be even more indispensable for TRIF-dependent signalling upon LPS stimulation than for MyD88-dependent TLR4 signalling [25, 35, 54]. Interestingly, we observed that in presence of CD14-blocking antibodies MPLA could still induce RANTES production. In previous studies we demonstrated that MPLA-induced RANTES production by human moDCs is TRIF dependent [13]. Since some antibodies targeting CD14 can induce endocytosis of CD14 and TLR4 [43], such antibodies might potentially influence TRIF-mediated cytokine production. To ensure that absence of effect of the blocking anti-CD14 antibodies on MPLA-induced RANTES in our study is not caused by an increased TLR4 internalization, CD14 was down-regulated using siRNA. Reassuringly this yielded results similar to the results obtained by anti-CD14 blocking antibodies. Thus, although data in mice are still conflicting on the requirement of CD14 for TLR4-mediated TRIF signalling [36, 55], our data clearly show that CD14 in human is not only dispensable for MPLA-mediated MyD88 signalling, but also dispensable for TRIF signalling. Watanabe and colleagues [55] showed that intracellular delivery of LPS by liposomes can initiate the TRIF-dependent signalling pathway independent of CD14. This suggests that CD14 is necessary for internalization of LPS and consequently needed for TLR4-mediated signalling of LPS via TRIF. This might implicate that, in contrast to LPS, MPLA does not require CD14 for TLR4-endocytosis. Alternatively, MPLA ligation of TLR4 allows signalling via TRIF from the plasma membrane.
These data show that immunological activation of DCs by MPLA is effective independent of the presence of the serum cofactor LBP and the CD14 helper function. The lack of amplification of the potential toxic pro-inflammatory cytokines in a serum-proficient environment supports the safe use of MPLA as a clinical adjuvant, while the effective action of MPLA in absence of LBP and CD14 endorses its application to generate immuno-activatory cellular products under serum-free conditions of Good Manufacturing Practice.
Abbreviations
- LPS:
-
Lipopolysaccharide
- MPLA:
-
Monophosphoryl lipid A
- LBP:
-
LPS-binding protein
- MPLAs:
-
MPLA derived from S. minnesota re595
- LPSs:
-
LPS derived from S. typhimurium
- MPLAe:
-
MPLA derived from E. coli r515
- LPSe:
-
LPS derived from E. coli O111B4
- RANTES:
-
Chemokine CCL5
References
Kundi M. New hepatitis B vaccine formulated with an improved adjuvant system. Expert Rev Vaccines. 2007;6:133–40.
Schwarz TF. Clinical update of the AS04-adjuvanted human papillomavirus-16/18 cervical cancer vaccine. Cervarix Adv Ther. 2009;26:983–98.
Casella CR, Mitchell TC. Putting endotoxin to work for us: monophosphoryl lipid A as a safe and effective vaccine adjuvant. Cell Mol Life Sci. 2008;65:3231–40.
Garcon N, Wettendorff M, van Mechelen M. Role of AS04 in human papillomavirus vaccine: mode of action and clinical profile. Expert Opin Biol Ther. 2011;11:667–77.
Martin M, Michalek SM, Katz J. Role of innate immune factors in the adjuvant activity of monophosphoryl lipid A. Infect Immun. 2003;71:2498–507.
ten Brinke A, Karsten ML, Dieker MC, Zwaginga JJ, van Ham SM. The clinical grade maturation cocktail monophosphoryl lipid A plus IFNgamma generates monocyte-derived dendritic cells with the capacity to migrate and induce Th1 polarization. Vaccine. 2007;25:7145–52.
McAleer JP, Vella AT. Educating CD4 T cells with vaccine adjuvants: lessons from lipopolysaccharide. Trends Immunol. 2010;31:429–35.
Kawai T, Akira S. The role of pattern-recognition receptors in innate immunity: update on Toll-like receptors. Nat Immunol. 2010;11:373–84.
Kagan JC, Medzhitov R. Phosphoinositide-mediated adaptor recruitment controls Toll-like receptor signaling. Cell. 2006;125:943–55.
Hoebe K, Janssen EM, Kim SO, Alexopoulou L, Flavell RA, Han J, Beutler B. Upregulation of costimulatory molecules induced by lipopolysaccharide and double-stranded RNA occurs by Trif-dependent and Trif-independent pathways. Nat Immunol. 2003;4:1223–9.
Hoebe K, Du X, Goode J, Mann N, Beutler B. Lps2: a new locus required for responses to lipopolysaccharide, revealed by germline mutagenesis and phenotypic screening. J Endotoxin Res. 2003;9:250–5.
Yamamoto M, Sato S, Hemmi H, Hoshino K, Kaisho T, Sanjo H, Takeuchi O, Sugiyama M, Okabe M, Takeda K, Akira S. Role of adaptor TRIF in the MyD88-independent Toll-like receptor signaling pathway. Science. 2003;301:640–3.
Kolanowski ST, Dieker MC, Lissenberg-Thunnissen SN, van Schijndel GM, van Ham SM, ten Brinke A. TLR4-mediated pro-inflammatory dendritic cell differentiation in humans requires the combined action of MyD88 and TRIF. Innate Immun. 2013;20:423–30.
Sasai M, Yamamoto M. Pathogen recognition receptors: ligands and signaling pathways by Toll-like receptors. Int Rev Immunol. 2013;32:116–33.
Pugin J, Schurer-Maly CC, Leturcq D, Moriarty A, Ulevitch RJ, Tobias PS. Lipopolysaccharide activation of human endothelial and epithelial cells is mediated by lipopolysaccharide-binding protein and soluble CD14. Proc Natl Acad Sci USA. 1993;90:2744–8.
Wright SD, Ramos RA, Tobias PS, Ulevitch RJ, Mathison JC. CD14, a receptor for complexes of lipopolysaccharide (LPS) and LPS binding protein. Science. 1990;249:1431–3.
Ulevitch RJ. Recognition of bacterial endotoxins by receptor-dependent mechanisms. Adv Immunol. 1993;53:267–89.
Viriyakosol S, Tobias PS, Kitchens RL, Kirkland TN. MD-2 binds to bacterial lipopolysaccharide. J Biol Chem. 2001;276:38044–51.
Shimazu R, Akashi S, Ogata H, Nagai Y, Fukudome K, Miyake K, Kimoto M. MD-2, a molecule that confers lipopolysaccharide responsiveness on Toll-like receptor 4. J Exp Med. 1999;189:1777–82.
Bingle CD, Craven CJ. Meet the relatives: a family of BPI- and LBP-related proteins. Trends Immunol. 2004;25:53–5.
Schumann RR. Old and new findings on lipopolysaccharide-binding protein: a soluble pattern-recognition molecule. Biochem Soc Trans. 2011;39:989–93.
Miyake K. Roles for accessory molecules in microbial recognition by Toll-like receptors. J Endotoxin Res. 2006;12:195–204.
Tobias PS, Soldau K, Gegner JA, Mintz D, Ulevitch RJ. Lipopolysaccharide binding protein-mediated complexation of lipopolysaccharide with soluble CD14. J Biol Chem. 1995;270:10482–8.
Tobias PS, Soldau K, Kline L, Lee JD, Kato K, Martin TP, Ulevitch RJ. Cross-linking of lipopolysaccharide (LPS) to CD14 on THP-1 cells mediated by LPS-binding protein. J Immunol. 1993;150:3011–21.
Akira S, Uematsu S, Takeuchi O. Pathogen recognition and innate immunity. Cell. 2006;124:783–801.
Casella CR, Mitchell TC. Inefficient TLR4/MD-2 Heterotetramerization by Monophosphoryl Lipid A. PLoS One. 2013;8:e62622.
Maeshima N, Fernandez RC. Recognition of lipid A variants by the TLR4-MD-2 receptor complex. Front Cell Infect Microbiol. 2013;3:3.
Tsukamoto H, Fukudome K, Takao S, Tsuneyoshi N, Kimoto M. Lipopolysaccharide-binding protein-mediated Toll-like receptor 4 dimerization enables rapid signal transduction against lipopolysaccharide stimulation on membrane-associated CD14-expressing cells. Int Immunol. 2010;22:271–80.
Park BS, Song DH, Kim HM, Choi BS, Lee H, Lee JO. The structural basis of lipopolysaccharide recognition by the TLR4-MD-2 complex. Nature. 2009;458:1191–5.
Tanimura N, Saitoh S, Matsumoto F, Akashi-Takamura S, Miyake K. Roles for LPS-dependent interaction and relocation of TLR4 and TRAM in TRIF-signaling. Biochem Biophys Res Commun. 2008;368:94–9.
Zanoni I, Ostuni R, Marek LR, Barresi S, Barbalat R, Barton GM, Granucci F, Kagan JC. CD14 controls the LPS-induced endocytosis of Toll-like receptor 4. Cell. 2011;147:868–80.
Roy S, Karmakar M, Pearlman E. CD14 mediates Toll-like receptor 4 (TLR4) endocytosis and spleen tyrosine kinase (Syk) and interferon regulatory transcription factor 3 (IRF3) activation in epithelial cells and impairs neutrophil infiltration and Pseudomonas aeruginosa killing in vivo. J Biol Chem. 2014;289:1174–82.
Jiang Z, Georgel P, Du X, Shamel L, Sovath S, Mudd S, Huber M, Kalis C, Keck S, Galanos C, Freudenberg M, Beutler B. CD14 is required for MyD88-independent LPS signaling. Nat Immunol. 2005;6:565–70.
Lloyd-Jones KL, Kelly MM, Kubes P. Varying importance of soluble and membrane CD14 in endothelial detection of lipopolysaccharide. J Immunol. 2008;181:1446–53.
Gangloff M. Different dimerisation mode for TLR4 upon endosomal acidification? Trends Biochem Sci. 2012;37:92–8.
Tanimura N, Saitoh SI, Ohto U, Akashi-Takamura S, Fujimoto Y, Fukase K, Shimizu T, Miyake K. The attenuated inflammation of MPL is due to the lack of CD14-dependent tight dimerization of the TLR4/MD2 complex at the plasma membrane. Int Immunol. 2014;16:307–14.
Kagan JC, Su T, Horng T, Chow A, Akira S, Medzhitov R. TRAM couples endocytosis of Toll-like receptor 4 to the induction of interferon-beta. Nat Immunol. 2008;9:361–8.
Mata-Haro V, Cekic C, Martin M, Chilton PM, Casella CR, Mitchell TC. The vaccine adjuvant monophosphoryl lipid A as a TRIF-biased agonist of TLR4. Science. 2007;316:1628–32.
Ohto U, Fukase K, Miyake K, Satow Y. Crystal structures of human MD-2 and its complex with antiendotoxic lipid IVa. Science. 2007;316:1632–4.
ten Brinke A, van Schijndel G, Visser R, de Gruijl TD, Zwaginga JJ, van Ham SM. Monophosphoryl lipid A plus IFNgamma maturation of dendritic cells induces antigen-specific CD8 + cytotoxic T cells with high cytolytic potential. Cancer Immunol Immunother. 2010;59:1185–95.
Gangloff SC, Zahringer U, Blondin C, Guenounou M, Silver J, Goyert SM. Influence of CD14 on ligand interactions between lipopolysaccharide and its receptor complex. J Immunol. 2005;175:3940–5.
Wright SD. CD14 and innate recognition of bacteria. J Immunol. 1995;155:6–8.
Kim D, Kim JY. Anti-CD14 antibody reduces LPS responsiveness via TLR4 internalization in human monocytes. Mol Immunol. 2013;57:210–5.
Kolb JP, Casella CR, SenGupta S, Chilton PM, Mitchell TC. Type I interferon signaling contributes to the bias that Toll-like receptor 4 exhibits for signaling mediated by the adaptor protein TRIF. Sci Signal. 2014;7:ra108.
Triantafilou M, Lepper PM, Olden R, Dias IS, Triantafilou K. Location, location, location: is membrane partitioning everything when it comes to innate immune activation? Mediat Inflamm. 2011;2011:186093.
Resman N, Oblak A, Gioannini TL, Weiss JP, Jerala R. Tetraacylated lipid A and paclitaxel-selective activation of TLR4/MD-2 conferred through hydrophobic interactions. J Immunol. 2014;192:1887–95.
Beamer LJ, Carroll SF, Eisenberg D. The BPI/LBP family of proteins: a structural analysis of conserved regions. Protein Sci. 1998;7:906–14.
Beamer LJ, Carroll SF, Eisenberg D. The three-dimensional structure of human bactericidal/permeability-increasing protein: implications for understanding protein-lipopolysaccharide interactions. Biochem Pharmacol. 1999;57:225–9.
Kelley SL, Lukk T, Nair SK, Tapping RI. The crystal structure of human soluble CD14 reveals a bent solenoid with a hydrophobic amino-terminal pocket. J Immunol. 2013;190:1304–11.
Jahr TG, Sundan A, Lichenstein HS, Espevik T. Influence of CD14, LBP and BPI in the monocyte response to LPS of different polysaccharide chain length. Scand J Immunol. 1995;42:119–27.
Anas AA, Hovius JWR, van’t Veer C, van der Poll T, de Vos AF. Role of CD14 in a mouse model of acute lung inflammation induced by different lipopolysaccharide chemotypes. PLoS One. 2010;5:e10183.
Jerala R. Structural biology of the LPS recognition. Int J Med Microbiol. 2007;297:353–63.
Kitchens RL, Munford RS. Enzymatically deacylated lipopolysaccharide (LPS) can antagonize LPS at multiple sites in the LPS recognition pathway. J Biol Chem. 1995;270:9904–10.
Evans JT, Cluff CW, Johnson DA, Lacy MJ, Persing DH, Baldridge JR. Enhancement of antigen-specific immunity via the TLR4 ligands MPL adjuvant and Ribi. 529. Expert Rev Vaccines. 2003;2:219–29.
Watanabe S, Kumazawa Y, Inoue J. Liposomal lipopolysaccharide initiates TRIF-dependent signaling pathway independent of CD14. PLoS One. 2013;8:e60078_1–7.
Acknowledgments
We thank Gijs van Schijndel and Miranda Dieker for technical assistance. We thank Prof. dr. van der Schoot, Sanquin Blood Supply for provision of mouse anti-human CD14.22 antibodies.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This work was supported by a grant from the Joghem van Loghem foundation.
Conflict of interest
The authors declare that there is no conflict of interest.
Additional information
Responsible Editor: John Di Battista.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Fig. S1
MPLA does not require LBP to induce cytokine production. (A,B) IL-6 production by DCs stimulated with a titration of LBP in serum-free IMDM in presence of (A) 10 ng/ml LPSe, one representative experiment out of 6 is shown, or (B) 10 μg/ml MPLAe, a representative experiment (n = 7). (C,D) TNF-α (C) and IL-6 (D) production by DCs stimulated with indicated concentrations of MPLAs in presence or absence of LBP. Cytokine production is shown relative to stimulation with comparable amounts of MPLAs in absence of LBP, n = 8. For statistical analysis a paired t test was performed (EPS 92 kb)
Fig. S2
RANTES production is solely TRIF dependent in human moDCs. To verify that production of chemokine RANTES was TRIF dependent, MyD88 or TRIF was down-regulated using siRNA prior to stimulation of iDCs with MPLAe. To down-regulate MyD88 of TRIF iDCs were electroporated with control siRNA (siC) or specific siRNA targeting MyD88 (siM) or TRIF (siT). Two days after electroporation iDCs were stimulated with MPLAe. Production of TNF-α and IL-6 was lower in MyD88- and TRIF down-regulated DCs compared to control siRNA-treated DCs (A, B) while production of RANTES was only decreased in TRIF down-regulated DCs, but not MyD88 down-regulated DCs (C). Concentration of cytokines TNF-α (A), IL-6 (B) or chemokine RANTES (C) was determined in supernatant harvested 24 h after stimulation with MPLA, siMyD88, n = 17, siTRIF n = 8, a paired t test was performed for statistical analysis, values were compared to siC condition *: p < 0.05 (EPS 117 kb)
Fig. S3
CD14 is not required for MPLAe-mediated cytokine production. (A-C) Cytokine production by DCs stimulated with LPSe in the presence of control antibodies (CTRL, grey lines) or CD14-blocking antibodies (a-CD14, black lines). LPSe-stimulated production of TNF-α (A), IL-6 (B), a representative experiment (n = 7). (C) LPSe responsiveness by a-CD14 treatment is quantified as described in materials & methods, n = 4. (D,E) MPLAe-stimulated production of TNF-α (D) or IL-6 (E), one representative experiment out of 9 is shown. (F,G) MPLAe-stimulated production of TNF-α (F), IL-6 (G), as a % of CTRL condition n = 6. (C, F, G) A one sample t test was performed for statistical analysis. *: p < 0.05, **: p < 0.01 (EPS 145 kb)
Rights and permissions
About this article
Cite this article
Kolanowski, S.T.H.M., Lissenberg-Thunnissen, S.N., Emal, D. et al. Monophosphoryl lipid A-induced pro-inflammatory cytokine expression does not require CD14 in primary human dendritic cells. Inflamm. Res. 65, 449–458 (2016). https://doi.org/10.1007/s00011-016-0927-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-016-0927-0