Abstract
Objective and design
Laticifer proteins (LP) of Calotropis procera were fractionated by ion-exchange chromatography, and the influence of a sub-fraction (LPPI) on the inflammatory response of Swiss mice challenged by Salmonella enterica Ser. Typhimurium was investigated.
Methods
Mice (n = 10) received LPPI (30 or 60 mg/kg) in a single inoculum by the intraperitoneal route 24 h before infection. To investigate the relevance of the proteolytic activity, three additional groups were included: the first one received heat-treated LP (30 mg/kg—30 min at 100 °C), the second received LP (30 mg/kg) inactivated by iodoacetamide, and a control group received only phosphate-buffered saline (PBS).
Results
The survival rate reached 100 % in mice treated with LPPI and was also observed with the other treatment, whereas the PBS group died 1–3 days after infection. The neutrophil infiltration into the peritoneal cavity of pretreated mice was enhanced and accompanied by high bacterial clearance from the bloodstream. Tumor necrosis factor-alpha mRNA transcripts, but not interferon-gamma, were detected early in spleen cells of pretreated mice after infection; however, the nitric oxide contents in the bloodstream were decreased in comparison to the PBS group.
Conclusions
The inflammatory stimulus of C. procera proteins increased phagocytosis and balanced the nitric oxide release in the bloodstream, preventing septic shock induced by Salmonella infection.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Natural plant products with anti-inflammatory properties are prospective sources of new drugs against infections and chronic inflammatory diseases [1]. For example, aqueous extracts of the stem bark of Mangifera indica and glucosylxanthone mangiferin were shown to suppress inflammatory cytokines, such as tumor necrosis factor-alpha (TNF-α), and inhibit nitric oxide (NO) production by activated macrophages [2]. Catechins derived from green tea down-regulated the inducible gene expression and enzyme activity of nitric oxide synthase (iNOS) [3]. In the present study, we investigated the shrub Calotropis procera (Ait.) R. Br. (Asclepiadaceae), a widespread plant in Brazil and India commonly used in folk medicine. The plant’s laticifer fluid is described as having healing, analgesic, antipyretic, anticancer, toxicological, inflammatory and anti-inflammatory properties [4–9]. Antibacterial activity against Staphylococcus aureus, S. epidermidis, Pseudomonas aeruginosa, Klebsiella pneumoniae, Salmonella serovar Paratyphi A and S. Typhi was also reported [10].
Although most of the medicinal properties reported for the latex of C. procera were obtained through use of aqueous and organic-solvent extracts, it is also rich in numerous proteins that can be separated by dialysis [11]. Non-dialyzable proteins (LP) have anti-cancer properties and can decrease neutrophil infiltration induced by carrageenan in the paw edema model [12, 13]. Freitas et al. [14] described proteins with molecular masses ranging from 5 to 95 kDa and at least four cysteine proteinases in the latex of C. procera. Proteinases have emerged as therapeutics against many medical disorders, including sepsis [15]. Furthermore, plant proteinases have been shown to influence immunity by acting to reverse the effects of circulating α2-macroglobulin and α1-protease inhibitor and also by interfering with the binding of cytokines such as transforming growth factor-beta and interleukin (IL)-1 beta [16].
The influence of the laticifer proteins (LP) of C. procera on the protection of Swiss mice against S. Typhimurium infection, the murine model of typhoid fever, was recently shown [17]. However, the immune mechanisms by which C. procera proteins prevented the bacterial septic shock are unclear. While these LP have been fractionated by ion-exchange chromatography and biochemically characterized, the aim of the present study was to investigate the effect of one sub-fraction, named LPPI, on the protection rates and inflammatory response of Swiss mice infected by S. Typhimurium. This fraction was chosen because its administration was highly anti-inflammatory, decreasing the number of rolling and adherent leukocytes in the mesenteric microvasculature of animal models [18]. The influence of LPPI on NO release, cytokine mRNA expression and neutrophil recruitment are discussed in light of previous biological activities reported for C. procera proteins.
Materials and methods
Plant collection and identification
Samples of C. procera (Ait.) R. Br. (Asclepiadaceae) latex were collected in the city of Fortaleza, in the state of Ceará in northeast Brazil. The voucher (sample specimen no. 32663) was deposited at the Prisco Bezerra Herbarium of the Ceará Federal University, and the plant was authenticated by a taxonomist from the school’s biology department.
Procera proteins
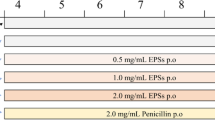
Calotropis procera proteins were obtained as described by Alencar et al. [11]. Briefly, fresh C. procera latex was collected from healthy plants through small incisions directly into tubes containing distilled water to obtain a mixture (v/v). The samples were centrifuged (5,000×g) at 10 °C for 10 min. The precipitated material, showing a rubbery aspect, was discarded, while the suspended phase was submitted to exhaustive dialysis (cut-off 8,000 Da) against distilled water at 8 °C for 60 h and then centrifuged as previously mentioned. The new precipitate material was discarded, and the soluble phase devoid of rubber was freeze-dried. This fraction, containing almost all of the latex’s soluble proteins, has been named laticifer proteins (LP). These proteins were fractionated by ion-exchange chromatography, as previously reported [12], through a CM-Sepharose fast-flow column (Amersham Biosciences, Brazil) previously equilibrated with 50 mM acetate buffer, pH 5.0. After washing the column with acetate buffer, the sample was sequentially eluted with buffer containing 0.2 and 0.3 M sodium chloride (NaCl). Fractions (4 ml) were collected at a flow rate of 1 ml/min, and the absorbance was read at a wavelength of 280 nm. Three distinct protein peaks—PI, PII and PIII (LPPI, LPPII and LPPIII)—were obtained (Fig. 1). The fractions corresponding to these peaks were dialyzed against distilled water and lyophilized. In the present study, LPPI was used because previous data have shown that this fraction is highly anti-inflammatory [18].
Microorganisms
Salmonella enterica Subsp. enterica serovar Typhimurium was isolated from a human clinical case at the Ezequiel Dias Foundation (FUNED, Belo Horizonte, MG, Brazil), donated by Dr. Jacques Robert Nicoli (Minas Gerais Federal University). The bacteria were maintained at −18 °C in brain heart infusion (BHI) medium containing 50 % glycerol. During the experiments, bacteria were activated after culture in BHI broth at 37 °C for 24 h.
Animals
Adult male Swiss mice (30–35 g) and Wistar rats (180–200 g) were obtained from the Biotery of Ceará Federal University and were kept in an animal house with free access to water and a commercial feed (Purina, Paulínia, SP, Brazil). The animals were handled according to the standards set forth in the ‘Guide for the Care and Use of Laboratory Animals’ of the National Research Council, after approval by the university’s animal ethics committee (protocol number 24/09).
Study design
Mice in the experimental groups were given a single inoculum of two doses of LPPI (30 and 60 mg/kg) in 0.2 ml of sterile phosphate-buffered saline (PBS), pH 7.2, by the intraperitoneal (i.p.) route. The protein dosages were based on previous data obtained with treatments with LP, which were protective against Salmonella infection. The control group received 0.2 ml of PBS devoid of C. procera proteins. Three additional experimental groups received LP, heat-treated LP (30 min at 100 °C) or LP submitted to inactivation by iodoacetamide (IAA). The experimental infection with S. Typhimurium was conducted following Lima-Filho et al. [19]. Salmonella Typhimurium was activated in BHI broth at 37 °C for 6 h and then cultured in MacConkey agar for another 24 h at 37 °C. Five to seven colony-forming units (CFU) were diluted in sterile PBS, pH 7.2, to attain a bacterial suspension containing 108 CFU/ml (according to the 0.5 tube of the MacFarland scale). The bacterial suspension was diluted 100-fold, and 0.2 ml (106 CFU) was administered to Swiss mice by the i.p. route 24 h after the inoculums of C. procera proteins.
Survival evaluation and bacterial clearance
Mice from all animal groups (n = 10) were observed for clinical signs and for mortality every day until 7 days post-infection. Additionally, mice treated with LPPI or LP (n = 5) and the PBS group were sacrificed under anesthesia with halothane (Halocarbon Laboratories, USA) at 4 h and 24 h after infection. The liver, spleen and blood samples were aseptically extracted and submitted to serial decimal dilutions in PBS, and 0.1-ml aliquots were plated onto MacConkey agar (Oxoide). The enumeration of CFUs was carried out after incubation at 37 °C for 24 h, and the results were expressed as CFUs/g of organ or ml of blood.
Histological examination
The liver and spleen tissue samples were fixed in 10 % formaldehyde and submitted to histopathological examination. The samples were embedded in paraffin, and 5-µm sections were stained with hematoxylin-eosin (H&E). The slides were coded and examined by a single pathologist who was unaware of the experimental conditions. Histological examination was also conducted on the organs of survivors treated with LPPI and LP at the end of the experiment, 7 days post-infection.
Influence of C. procera proteins on neutrophil infiltration into the peritoneal cavity
Initially, uninfected mice (n = 5) were given C. procera proteins by the i.p. route and neutrophil recruitment was evaluated at 4 h, 24 h and 7 days after the inoculums. The peritoneal cavity was washed with 3 ml of sterile saline (0.15 M NaCl) containing heparin (5 IU/ml). Leukocytes were counted in the recovered peritoneal fluid, following the method of Souza and Ferreira [20]. From these results, an additional animal group was composed to evaluate the influence of the administration route of LP and LPPI on neutrophil infiltration into the peritoneal cavity. In this case, uninfected Wistar rats (n = 5) were treated by the endovenous (e.v.) or the i.p. route with LP (30 mg/kg), LPPI (5 mg/kg) or PBS (control) 30 min before an i.p. injection of carrageenan (800 μg/cavity). An additional control group received PBS that was not injected with carrageenan. Four hours later, the peritoneal cavities of the rats were washed with 10 ml sterile saline containing 5 IU/ml heparin. The leukocyte count was determined as described above. Neutrophil migration to the peritoneal cavity was also evaluated in LP- and LPPI-treated mice (n = 5) and the PBS group (n = 5) at 4 h, 24 h and 7 days post-infection, as described for the uninfected mice.
Analyses of cytokine mRNA expression in spleen cells
The spleens from the animals were removed aseptically and homogenized in 1 ml RNAzol solution (4 M guanidine isothiocyanate phenol + v/v) for extraction of total RNA. The homogenate was left on ice for 40 min–1 h. The samples were then submitted to chloroform–isopropanol extraction, as described in other studies [21], and quantified through spectrophotometer reading at 260 nm. The integrity of the extracted RNA was confirmed by electrophoresis in 1.5 % agarose gel. Reverse transcription was carried out with the use of murine leukemia virus reverse transcriptase at 37 °C for 60 min. Cytokines were amplified through polymerase chain reaction with the following primers: interferon-gamma (IFN-γ) (forward 5′ GGTGACATGAAAATCCTGCAGAGC 3′, reverse 5′ CGCTGGACCTGTGGGTTGTTGACC 3′); tumor necrosis factor-alpha (TNF-α) (forward 5′ GATCTCAAA GACAACCAACTAGTG 3′, reverse 5′ CTCCAGCTGGAAGACTCCTCCCAG 3′). The enzyme hypoxanthine ribosyltransferase was used as an internal control: forward 5′ GTTGGATACAGGC CAAGACTTTGTTG 3′, reverse 5′ GATTCAACTTGCG CTCATCTTAGGC 3′. Amplification was performed by 40 cycles consisting of denaturation at 94 °C for 90 s, primer annealing at 55 °C for 30 s, and primer extension at 72 °C for 60 s (Thermocycler PTC-100, MJ Research).
Nitric oxide measurement
Blood aliquots (0.7–1.0 ml) were obtained through cardiac puncture at 4 h and 24 h post-infection and left to coagulate in sterile tubes at room temperature. Serum levels of NO (NO3/NO2) were measured following the method reported by Chen et al. [22]. A 0.1-ml aliquot of Griess reagent (1 % sulfanilamide and 0.1 % naphthalene diamine dihydrochloride in 1 % orthophosphoric acid) was added to 0.1 ml serum and incubated at room temperature for 10 min. Serum nitrite concentrations were then determined through reading the optical densities at 540 nm and comparison with a standard curve made from sodium nitrite.
Determination of adenosine deaminase activity (ADA)
The assay was carried out as described by Guisti [23]; the mice were pretreated with LP (30 mg/kg i.p.) or PI (5 mg/g i.p.) and were challenged with Salmonella 24 h later. Peritoneal fluids of healthy or infected mice were collected at 4 h and 24 h post-infection. After centrifugation, the supernatant (20 μl) was used as the enzyme source and incubated with 200 μl (22 mM) of adenosine at 37 °C for 1 h in 50 mM phosphate buffer, pH 7.2. The ammonium concentration after deamination of adenosine by the enzyme adenosine deaminase was measured by indophenol production (Berthelot reaction) and analyzed through spectrometry at 628 nm.
Enzymatic activities of transaminases and lactate dehydrogenase in serum
The glutamic oxaloacetic transaminase (TGO), glutamic pyruvic transaminase (TGP) and lactate dehydrogenase (LDH) enzyme levels were measured using commercial kits (Labtest). These methods were based on evaluating the enzymatic kinetics. The results are expressed in international units/ml.
Statistical analyses
The survival curves of the mice after bacterial inoculums represent two independent experiments and are expressed as percentages (%) of survival. The data were statistically evaluated by the Mantel–Cox log rank test (p < 0.05). The remaining data are reported as the mean ± SEM. Statistical significance was assessed by ANOVA followed by Bonferroni’s test or the Student’s t test. The level of significance was determined as p < 0.05.
Results
Intraperitoneal preinoculation with LPPI latex fraction from C. procera induces protection against Salmonella infection, as previously shown for the entire LP fraction. Survival was measured 7 days post-infection and was 100 % in the mice treated with LPPI, whereas the animals in the PBS group died 1–3 days after infection (Fig. 2a). The bacterial load in the bloodstream of the LP- and LPPI-treated mice was reduced approximately 100-fold at 4 h and 24 h after infection (p < 0.05) (Fig. 2b). However, there was no significant difference between counts recorded in the spleen and the liver compared to controls at these time points (data not shown). Survival was still evident with proteins submitted to heat treatment at 100 °C for 30 min or treated with IAA, and was at least 70 % by 7 days post-infection (Fig. 2c). Histological examination of liver in the PBS group revealed inflammatory filtrates other than apoptotic cells, as well as hypertrophy and congestion of the reticulum endothelial system 24 h after infection, while no significant alterations were seen in liver of mice submitted to pretreatment with LP or LPPI during this interval (Fig. 3). However, there were moderate cell infiltrates, vacuolization and a few necrosis foci in the liver of these survivor mice 7 days after infection (Fig. 3). The presence of a few giant cells and inflammatory infiltrates was seen in the spleen of all animal groups 24 h post-infection regardless of the treatment.
The protective effect of LPPI in Swiss mice subjected to lethal infection by S. Typhimurium. Mice were treated with 30 or 60 mg/kg of LPPI (a). The S. Typhimurium CFU in the bloodstream at 4 h and 24 h after infection are shown (b). Survival was still observed in mice inoculated with heat-treated LP (30 mg/kg) or LP (30 mg/kg) submitted to proteolysis with IAA (c). Proteins were given by the i.p. route 24 h before bacterial challenge, and survival was monitored for 7 days. Survival rates of animals from all experimental groups were significantly different from the PBS group (untreated mice) at all tested doses (n = 10, p < 0.05; Mantel–Cox log rank test). *p < 0.05 indicates a significant difference between the CFU counts in the bloodstream compared to uninfected mice (PBS group) (n = 5; ANOVA–Bonferroni test)
Effect of LP (LP and LPPI) from C. procera on the histopathological pattern of the liver in animals infected by S. Typhimurium. The figures show photomicrographs of histological sections from the liver of uninfected mice stained by the H&E method (a); PBS group—24 h (b); LP (30 mg/kg)—24 h (c); LPPI (5 mg/kg)—24 h (D); LP (30 mg/kg)—7 days (e) and PI (5 mg/kg)—7 days (F). Magnification ×100. The thin arrow indicates inflammatory infiltrates, while wide arrows indicate necrosis foci
The LP and LPPI pre-inoculums delivered via the i.p. route induce strong neutrophil infiltration into the peritoneal cavity of uninfected mice stimulated by carrageenan (p < 0.05) (Fig. 4c, d). Conversely, the neutrophil migration into the peritoneal cavity was impaired when LP or LPPI treatments were delivered by the e.v. route (Fig. 4). Significant recruitment of neutrophils into the peritoneal cavity was also observed in Salmonella-infected animals after i.p. inoculums with LP or LPPI and remained strong 7 days post-infection (Fig. 5). Conversely, neutrophils failed to migrate into the peritoneal cavity in mice that were not treated with C. procera proteins (PBS group) (Fig. 5). The hematological profiles of healthy and infected mice confirm that treatment with LP or LPPI did not hamper neutrophil migration into the peritoneal cavity and prevented the reduction of lymphocytes in the bloodstream commonly observed in septic animals (Table 1). No significant differences were observed among monocyte, eosinophil and basophil counts, regardless of the treatment (Table 1).
Effect of LP of C. procera on neutrophil migration into the peritoneal cavity of healthy Swiss mice and Wistar rats. Mice were treated with LP (10, 30 or 60 mg/kg i.p.) (a) or LPPI (5, 10 or 30 mg/kg i.p.) (b). Neutrophil migration was evaluated at 4 h, 24 h and 7 days after protein inoculums. To evaluate the influence of the administration route, rats were treated with LP (30 mg/kg) (c) or LPPI (5 mg/kg) (d) by the e.v. or i.p routes 30 min before an i.p. injection of carrageenan (Cg–800 μg/cavity), whereas control mice received PBS. Neutrophil migration was evaluated 4 h later. The results are expressed as the mean ± SEM of neutrophils per cavity. *p < 0.05 indicates a significant difference compared to the PBS group, and # p < 0.05 indicates a significant difference compared to the carrageenan group (PBS + Cg) (n = 10, ANOVA–Bonferroni test)
Effect of LP from C. procera on neutrophil migration into the peritoneal cavity of mice challenged with S. Typhimurium. Swiss mice were treated with single inoculums of LP (10, 30 and 60 mg/kg) or LPPI (5, 10 and 30 mg/kg) by the i.p. route 24 h before bacterial challenge. Neutrophil migration to the peritoneal cavity was evaluated at 4 h, 24 h and 7 days post-infection. The results are expressed as the mean ± SEM of neutrophils per cavity. + indicates that all mice from the PBS group died. *p < 0.05 indicates a significant difference compared to uninfected mice, and # p < 0.05 indicates a significant difference compared to the PBS group (n = 10, ANOVA–Bonferroni test)
The level of NO in serum showed almost a three-fold increase in non-treated infected animals when compared to LP or LPPI groups 24 h post-infection (p < 0.05) (Fig. 6a). Conversely, ADA activity was increased in the treated groups 24 h after infection (p < 0.05) (Fig. 6b). In addition, early TNF-α mRNA expression was observed at 4 h post-infection in the LP and LPPI animal groups, but IFN-γ was not observed at this early time point (Fig. 6c). The TGO, TGP and LDH enzymatic levels were similar among all animal groups (data not shown).
NO concentrations, adenosine deaminase activity and TNF-α mRNA expression in mice treated with LP from C. procera. Swiss mice were treated with LP (30 mg/kg i.p.) or LPPI (5 mg/kg i.p.) 24 h before bacterial challenge. NO was titrated as nitrite and serum concentrations were determined by the Griess reaction (a), whereas adenosine deaminase activity was determined in the peritoneal fluid (b) of animals 4 h and 24 h after infection. The extraction of RNA by reverse transcription-polymerase chain reaction was conducted from spleen cells at the same intervals (c). The results are expressed as the mean ± SEM of the nitrite concentration in μM. *p < 0.05 indicates a significant difference compared to uninfected mice, and #p < 0.05 indicates a significant difference compared to infected animals of the PBS group (n = 10, ANOVA–Bonferroni test). Hypoxanthine ribosyltransferase was used as an internal control of gene expression
Discussion
The laticifer fluid of C. procera encompasses a large amount of proteins with anti-inflammatory properties and prospective pharmacological uses [11, 18]. We have shown that the enhanced protection by LP or LPPI inoculums against Salmonella infection was not related to protease activity. However, although mice submitted to protein treatments did not show clinical symptoms of the infection, the bacterium was not cleared from the spleen and liver of the surviving animals 7 days after infection, causing moderate histological damage to these target organs. Furthermore, survival was accompanied by early bacterial clearance in the bloodstream, supporting the hypothesis that phagocytic activity stimulated by the protein inoculums facilitated bacterial removal. Afterwards, this hypothesis was confirmed because the protein inoculums caused a high local inflammatory stimulus after the bacterial challenge. Interestingly, the i.p. inoculum of C. procera proteins into uninfected rats also prompted inflammation, whereas an e.v. inoculum provoked anti-inflammation. The occurrence of antagonistic activities due to the inoculum routes of C. procera proteins remains to be elucidated.
Salmonella Typhimurium causes a strong inflammatory response in susceptible mice that results in sepsis and septic shock [24]. In contrast, resistance to disseminated infection results from the activation of CD4 + T cells as part of the adaptive immune response [24]. In the early stages of the disease, macrophage-derived IL-12 is important in stimulating IFN-γ release by natural killer cells, which in turn enhance the microbicidal capacity of macrophages through the production of NO and its derivatives from the nicotinamide adenine dinucleotide phosphate-oxidase cascade [25, 26]. However, the cytokine IFN-γ played a minor role in the protective effect induced by C. procera proteins because mRNA transcripts were not clearly evidenced after infection. Additionally, protection was enhanced during innate immunity due to a non-specific inflammatory stimulus by the C. procera proteins. The activation of the inflammatory cascade by LP and LPPI before infection reduced the bacterial load in the bloodstream after infection, preventing extensive inflammation. TNF-α-derived macrophages are major mediators of acute inflammation against Salmonella circulating bacterial antigens [27]. Therefore, stimulation of TNF-α through pretreatment with LP of C. procera was shown to be highly beneficial by recruiting macrophages and neutrophils to the peritoneal cavity before Salmonella infection.
Large amounts of IL-1β or TNF-α are known to be involved in bacterial sepsis, but blocking these cytokines as therapy for septic patients has failed in clinical trials and can lead to immunocompromisation and infections [28]. Accordingly, high amounts of macrophage-derived NO in the bloodstream are related to hypotension, cardiodepression, vascular hyporeactivity and septic shock [29, 30]. It was clear that the NO levels in the serum of untreated mice were substantially higher and remarkably increased the inflammatory response, producing premature death. Previous studies have shown that immunosuppression following infection with S. Typhimurium is related to high serum NO content released by activated macrophages [31]. Paradoxically, inoculation of mice with an attenuated Salmonella strain decreased the NO levels in serum and evoked a high protection against challenge with virulent Salmonella [32]. Likewise, the inflammatory stimulus of LPPI or LP balanced the NO content in serum after Salmonella inoculums, preventing immunosuppression and septic shock. This finding was corroborated by increased ADA activity, which is reported as a down-regulator of several pro-inflammatory cytokines involved in NO release [33, 34].
The enhancement of immunological function has been described for medicinal plants in the prevention and treatment of infectious diseases [35]. Additionally, the use of proteins as vaccines or immunological adjuvants represents an interesting tool because amino acid sequences could be reproduced by genetic engineering [36]. While C. procera proteins have been purified and biochemically characterized, their role in counterbalancing the effects of NO in the host’s defense against Salmonella is of prospective interest in the management of infections caused by Gram-negative bacteria.
References
Seo CS, Lee YK, Kim YJ, Jung JS, Jahng Y, Chang HW, Song DK, Son JK. Protective effect of lignans against sepsis from the roots of Saururus chinensis. Biol Pharm Bull. 2008;31:523–6.
Garrido G, Delgado R, Lemus Y, Rodríguez J, García D, Núñez-Sellés AJ. Protection against septic shock and suppression of tumor necrosis factor alpha and nitric oxide production on macrophages and microglia by a standard aqueous extract of Mangifera indica L. (VIMANG®) Role of mangiferin isolated from the extract. Pharmacol Res. 2004;50:165–72.
Chan MM, Fong D, Ho C, Huang H. Inhibition of inducible nitric oxide synthase gene expression and enzyme activity by epigallocatechin gallate, a natural product from green tea. Biochem Pharmacol. 1997;54:1281–6.
Rasik AM, Raghubir R, Gupta A, Shukla A, Dubey MP, Srivastava S, Jain HK, Kulshrestha DK. Healing potential of Calotropis procera on dermal wounds in Guinea pigs. J Ethnopharmacol. 1999;68:261–6.
Dewan S, Kumar S, Kumar VL. Antipyretic effect of latex of Calotropis procera. Ind J Pharmacol. 2000;32:247–52.
Arya S, Kumar VL. Anti-inflammatory efficacy of extracts of latex of Calotropis procera against different mediators of inflammation. Mediators Inflamm. 2008;4:228–32.
Choedon T, Mathan G, Arya S, Kumar VL, Kumar V. Anticancer and cytotoxic properties of the latex of Calotropis procera in a transgenic mouse model of hepatocellular carcinoma. World J Gastroenterol. 2006;12:2517–22.
El Badwi SMA, Bakhiet AO. Toxicity of Calotropis procera latex in pregnant and non-pregnant goats. Sci Res Essays. 2010;5:2404–8.
Kumar VL, Chaudhary P, Ramos MV, Mohan M, Matos MPV. Protective effect of proteins derived from the latex of Calotropis procera against inflammatory hyperalgesia in monoarthritic rats. Phytother Res. 2011. doi:10.1002/ptr.3428.
Parabia FM, Kothari IL, Parabia MH. Antibacterial activity of solvent fractions of crude water decoction of apical twigs and latex of Calotropis procera (Ait.) R. Br. Nat Prod Radiance. 2008;7:30–4.
Alencar NMN, Oliveira JS, Mesquita RO, Lima MW, Vale MR, Etchells JP, Freitas CDT, Ramos MV. Pro- and antiinflammatory activities of the latex from Calotropis procera (Ait.) R.Br. are trigged by compounds fractionated by dialysis. Inflamm Res. 2006;55:559–64.
Alencar NMN, Figueredo IST, Vale MR, Bitencurt FS, Oliveira JS, Ribeiro RA, Ramos MV. Anti-inflammatory effect of the latex from Calotropis procera in: three different experimental models: peritonitis, paw edema and hemorrhagic cystitis. Planta Med. 2004;7:1144–9.
Oliveira JS, Freitas CDT, Moraes MO, Pessoa C, Costa-Lotufo LV, Ramos MV. In vitro cytotoxicity against different human cancer cell lines of laticifer proteins of Calotropis procera (Ait.) R.Br. Toxicol In Vitro. 2007;21:1563–73.
Freitas CDT, Oliveira JS, Miranda MRA, Macedo NMR, Sales MP, Villas-Boas LA, Ramos MV. Enzymatic activities and protein profile of latex from Calotropis procera. Plant Physiol Biochem. 2007;45:781–9.
Craik CS, Page MJ, Madison EL. Proteases as therapeutics. Biochem J. 2011;1435:1–16.
Salas CE, Gomes MTR, Hernandez M, Lopes MTP. Plant cysteine proteinases: evaluation of the pharmacological activity. Phytochemistry. 2008;69:2263–9.
Lima-Filho JV, Patriota JM, Silva AFB, Pontes-Filho NT, Oliveira RSB, Alencar NMN, Ramos MV. Proteins from latex of Calotropis procera prevent septic shock due to lethal infection by Salmonella enterica serovar Typhimurium. J Ethnopharmacol. 2010;129:327–34.
Ramos MV, Oliveira JS, Figueiredo JG, Figueiredo IST, Kumar VL, Bitencurt FS, Cunha FQ, Oliveira RSB, Bomfim LR, Lima-Filho JV, Ramos MV. Involvement of NO in the inhibitory effect of Calotropis procera latex protein fractions on leukocyte rolling, adhesion and infiltration in rat peritonitis model. J Ethnopharmacol. 2009;125:1–10.
Lima-Filho JVM, Vieira LQ, Arantes RME, Nicoli JR. Effect of the Escherichia coli EMO strain on experimental infection by Salmonella enterica serovar Typhimurium in gnotobiotic mice. Braz J Med Biol Res. 2004;37:1005–13.
Souza GEP, Ferreira SH. Blockade by anti-macrophages serum of the migration of PMN neutrophilis into the inflamed peritoneal cavity. Agent Actions. 1985;17:97–103.
Gilliland G, Perrin S, Blanchard K, Bunn HF. Genetics analysis of cytokine mRNA and DNA: detection and quantitation by competitive polymerase chain reaction. Proc Natl Acad Sci USA. 1990;87:2725–9.
Chen CC, Lin YC, Chen SA, Luk HN, Ding PY, Chang MS, Chiang CE. Shortening of cardiac action potentials in endotoxic shock in guinea pigs is caused by an increase in nitric oxide activity and activation of the adenosine triphosphate-sensitive potassium channel. Crit Care Med. 2000;28:1713–20.
Guisti G. Adenosine deaminase. In: Ulrich Hans, editor. Methods of enzymatic analyses. New York: Bergmeyer, Academic Press; 1974.
Portillo FG. Salmonella intracellular proliferation: where, when and how? Microb Infect. 2001;3:1305–11.
John B, Rajagopal D, Pashine A, Rath S, George A, Bal V. Role of IL-12-independent and IL-12-dependent pathways in regulating generation of the IFN-gamma component of T cell responses to Salmonella typhimurium. J Immunol. 2002;169:2545–52.
Withanage GSK, Wigley P, Kaiser P, Mastroeni P, Brooks H, Powers C, Beal R, Barrow P, Maskell DM. Cytokine and chemokine responses associated with clearance of a primary Salmonella enterica Serovar Typhimurium infection in the chicken and in protective immunity to rechallenge. Infect Immun. 2005;73:456–60.
Mastroeni P. Immunity to systemic Salmonella infections. Curr Mol Med. 2002;2:393–406.
Pérez-Sola MJ, Torre-Cisneros J, Pérez-Zafrilla P, Carmona L, Descalzo MA, Gómez-Reino JJ. Infections in patients treated with tumor necrosis factor antagonists: incidence, etiology and mortality in the BIOBADASER registry. Med Clin (Barc). 2011;137(12):533–40.
Kirkebøen KA, Strand ØA. The role of nitric oxide in sepsis—an overview. Acta Anaesthesiol Scand. 1999;43:275–88.
Guzik TJ, Korbut R, Adamak-Guzik T. Nitric oxide and superoxide in inflammation and immune regulation. J Physiol Pharmacol. 2003;54:469–87.
Schwacha MG, Meissler JJ Jr, Eisenstein TK. Salmonella typhimurium infection in mice induces nitric oxide-mediated immunosuppression through a natural killer cell-dependent pathway. Infect Immun. 1998;66:5862–6.
Al-Ramadi BK, Brodkin MA, Mosser DM, Eisenstein TK. Immunosuppression induced by attenuated Salmonella: evidence for mediation by macrophage precursors. J Immunol. 1991;146:2737–46.
Link AA, Kino T, Worth JA, McGuire JL, Crane ML, Chrousos GP, Wilder RL, Elenkov IJ. Ligand-activation of the adenosine A2a receptors inhibits IL-12 production by human monocytes. J Immunol. 2000;164:436–42.
Kreckler LM, Wan TC, Ge ZD, Auchampach JA. Adenosine inhibits tumor necrosis factor-α release from mouse peritoneal macrophages via A2A and A2B but not the A3 adenosine receptor. J Pharmacol Exp Ther. 2006;317:172–80.
Rishi P, Rampuria A, Tewari R, Koul A. Phytomodulatory potentials of Aloe vera against Salmonella OmpR-mediated inflammation. Phytother Res. 2008;22:1075–82.
Adamou JE, Heinrichs JH, Erwin A, Walsh H, Gayle T, Dormitzer M, Dagan R, Brewah YA, Barren P, Lathigra R, Langermann S, Koenig S, Johnson S. Identification and characterization of a novel family of pneumococcal proteins that are protective against sepsis. Infect Immun. 2001;69:949–58.
Acknowledgments
The biochemical, functional and applied studies of the latex proteins from Calotropis procera were supported by grants from FUNCAP and CNPq (Universal, RENORBIO and Brazil/India cooperation). We also thank the Educational Tutorial Program (MEC/SESu) for scholarship support.
Conflict of interest
The authors declare that there is no conflict of interests.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Responsible Editor: Artur Bauhofer.
Rights and permissions
About this article
Cite this article
Oliveira, R.S.B., Figueiredo, I.S.T., Freitas, L.B.N. et al. Inflammation induced by phytomodulatory proteins from the latex of Calotropis procera (Asclepiadaceae) protects against Salmonella infection in a murine model of typhoid fever. Inflamm. Res. 61, 689–698 (2012). https://doi.org/10.1007/s00011-012-0460-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-012-0460-8