Abstract
A large population world over is affected with allergic diseases and asthma. Pharmacotherapy for allergic diseases and asthma is effective in controlling symptoms but on discontinuation of medication, symptoms reoccur. In contrast, immunotherapy modifies and corrects the underlying pathological immune responses in an antigen-specific manner. Immunotherapy shows an increase in IgG (blocking antibody) that competes with IgE for allergen, inhibiting the release of inflammatory mediators. Recent studies suggest that immunotherapy acts by modifying CD4+ T-cell responses either by immune deviation, T-cell anergy and/or both. Current immunological approaches for management of allergies and asthma involve immunization with native allergen, modified allergen, peptides/cDNA of allergen, anti-IgE, adjuvants coupled allergen, including immunostimulatory DNA sequences, cytokines, and bacterial products. These approaches modulate the immune response and are intended to give long-term benefit.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
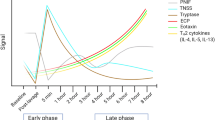
Allergic diseases are immunologic disorders, traditionally referred to as immediate or type I hypersensitivity reactions with IgE playing an important role. Interaction of IgE with allergen on mast cells or basophils leads to allergic reactions causing release of an array of inflammatory mediators resulting in inflammation of airway mucus membrane leading to clinical symptoms in target organ. Allergic reaction has two phases, namely, early and late. In the early phase, IgE sensitizes mast cells and basophils by binding the high-affinity receptor for IgE (FcεRI) at the surface of these cells. On cross-linking of the IgE–FcεRI complexes by allergen, mast cells and basophils degranulate, releasing vaso-active amines (mainly histamine), lipid mediators (prostaglandins and cysteinyl leukotrienes), chemokines and other cytokines [1, 2]. IgE also binds FcεRI at the surface of dendritic cells (DCs) and monocytes, as well as the low-affinity receptor for IgE, FcεRII (also known as CD23), at the surface of B cells. This process increases the uptake of allergen by these antigen presenting cells (APCs) and the subsequent presentation of allergen-derived peptides to specific CD4+ T cells, which in turn activates distinct cytokine pattern leading to the late phase of allergic reaction. The activation of a distinct cytokine pattern in T cells includes increased secretion of certain inflammatory cytokines particularly IL-4, IL-5 and/or IL-13 [3–5].
As per estimates 10–25% of the world population is suffering from rhinitis with increasing prevalence over the last decade [6]. Prevalence of allergic rhinitis has been reported in 7.3% of Indian children [7]. According to the ISAAC study, the prevalence of asthma showed a wide range of 1.6–36.8%, with an eightfold variation seen between the 10th and 90th percentile (3.9–30.6%). Recent reports show prevalence of asthma in the range of 8–15% [7, 8] than reported earlier (<1%) in India [9]. The high incidence of asthma and allergies causes an enormous financial burden and also loss of several working days during the active phase of life. Pharmacotherapy has improved considerably in controlling symptoms, but has many side effects [10]. Tropical country like India is rich in flora and fauna; hence, atmosphere is always laden with various types of pollen allergens that trigger different forms of allergies.
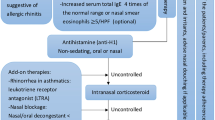
Desensitization (immunotherapy) is the only way of “teaching” the immune system to tolerate allergic triggers. This is a gradual immunizing process in which increasing doses of antigens responsible for causing allergic symptoms are administered to a patient to develop tolerance to the offending allergen when natural exposure occurs. Immunotherapy reduces specific cutaneous, nasal, bronchial and/or ocular reactivity to allergen as assessed by skin provocation and/or in vitro tests. There is an initial transient increase in serum specific IgE followed by gradual decrease over few months of treatment. Then there is a class switch, where IgG1 shows increase initially and IgG4 level increases later as a result of successful immunotherapy. However, these changes may not always correlate with improvement in symptoms.
Allergen avoidance is the best treatment in atopic diseases, wherever possible [11]. Good candidates for immunotherapy are patients whose symptoms are not controlled adequately by medications and allergen avoidance measures. Analysis under a WHO position paper revealed that specific immunotherapy is an effective form of treatment for patients with allergic asthma [12]. Immunotherapy when properly conducted has the potential to reduce symptoms and need for drug significantly. In addition, it is possible to prevent progression into more severe disease by this therapy [13]. Clinical efficacy of immunotherapy in rhinitis and asthma using potent standardized extracts in carefully selected patients has been documented in many double-blind placebo controlled studies. However, only a few studies have demonstrated low degree of clinical efficacy [14]. Meta analysis of clinical trials of allergen immunotherapy has shown benefits for the treatment of allergic conditions/asthma; however, the major risk associated is systemic reactions (anaphylaxis). Immunotherapy is effective and well tolerated in children. Beside, it prevents the development of asthma in children having allergic rhinitis. Immunotherapy with hymenoptera venom allergens has been reported to give almost 100% benefits in patients.
Several clinical trials have been done world over demonstrating beneficial effects of this therapy using clinico-immunologic parameters [15, 16]. Immunotherapy is practiced in India since the last three decades, but only a few systematic studies have been carried out in the country to assess the benefit of this therapy. In a study at Vallabhbhai Patel Chest Institute, Delhi, 50% of the seasonal allergic rhinitis cases showed considerable reduction in their symptom score and drug intake after 2 years of immunotherapy with mixed allergen vaccines [17]. Further, immunotherapy with single allergen preparation of Cocos nucifera pollen showed significant clinical improvement and immunological changes as compared to placebo group [18]. An open comparative trial, taking immunotherapy versus inhaled budenoside showed faster improvement in symptoms with drug therapy. But the decline in benefit after cessation of treatment was more rapid in patients on corticosteroid than patients on immunotherapy [19]. To assess the benefit of immunotherapy, a double-blind placebo controlled trial has been carried out by the authors sponsored by Department of Science and Technology, New Delhi. After 1 year of immunotherapy with single and mixed allergen vaccines, the patients with rhinitis and asthma showed substantial reduction in symptom/drug score, IgE, IL-4 and increase in IgG4 levels than placebo [20, 21].
Types of immunotherapy
Immunotherapy has been classified according to the route of allergen administration.
Subcutaneous immunotherapy (SCIT)
The most effective and frequently used form of immunotherapy is SCIT and it involves repeated subcutaneous injections of increasing doses of allergen extracts until a standard maintenance dose is reached. This dose is then injected subcutaneously on a regular basis (at intervals of approximately 20 days) for not less than 3 years for perennial allergens. The process is specific, in that the treatment is targeted at those allergens recognized by the patient and physician as responsible for symptoms. Treating patients with SCIT on the basis of positive allergy tests alone without relevant clinical symptoms is not justified. The patients receiving immunotherapy should have proven allergy by skin test or in vitro testing that should correlate with their clinical history. Short-term immunotherapy does not affect the cytokine profile and does not have long-term efficacy after discontinuation. The patient needs to be patient, motivated and compliant with treatment.
Studies evaluating the long-term efficacy of subcutaneous immunotherapy with inhalant allergens have been undertaken in patients with rhinitis and asthma. A pollen immunotherapy study of 3 years has confirmed the favorable effects in clinical as well as in immunologic parameters with increased production of specific IgG4 antibodies and decreased IgE-binding affinities in associations with TGF- β and IL-10 [22]. Another 10 year follow-up study investigating the time course changes in specific IgE and IgG4 in serum found that IgE titer decreases with several years of treatment and increase in IgG4 plays a significant contribution to clinical efficacy of immunotherapy [23]. The allergen-specific immunotherapy also prevents onset of new sensitization in allergic patients [24]. Administration of allergens in patients might cause local and/or systemic reactions, such as urticaria, asthmatic attack and/or life-threatening anaphylactic shock. Therefore, attempts have been made to reduce therapy-induced side effects.
Sublingual immunotherapy (SLIT)
Specific immunotherapy (SIT) by the subcutaneous route is effective, but it may be associated with severe or even fatal systemic reactions [25]. Therefore, alternative route of allergen administration has been proposed involving mucosal absorption in allergic patients [26, 27]. The natural mechanism underlying the induction of oral tolerance at mucosal surfaces is considered to be an effective therapeutic strategy for suppression of ongoing pathological immune responses in allergic diseases [25]. A specific form of oral tolerance induction, i.e., sublingual immunotherapy is raising a lot of interest as a noninvasive procedure and demonstrated to be efficacious. SLIT is safe because oral mucosa lacks proinflammatory cells and is rich in Langerhans-like dendritic cells [28]. But it requires high doses of allergen, i.e., 50- to 100-folds more than administered through subcutaneous route. Studies suggest that SLIT is as effective as subcutaneous immunotherapy in reducing allergic symptoms and medication requirement [29–32].
In SLIT, the patients are instructed to hold the extract (drops) under the tongue for 2 min and then swallow. The dose is increased once in every 3–4 weeks or earlier until a maintenance dose is reached, with minimal or no side effects. The contact of the allergen with the oral mucosa is crucial for the success of SLIT. To provide the experimental basis for understanding the relationship between the route of administration and the mechanism of action, allergen labeled with iodine123 has been used for pharmacokinetic studies [33]. In subjects receiving the radiolabelled allergen orally, plasma radioactivity increased rapidly, peaking at about 30 min. However, when given sublingually, plasma radioactivity was undetectable until swallowing. Moreover, a relevant amount of iodine123-labeled allergen persisted in the sublingual region for up to 40 h after administration.
Other possible routes of antigen administration
The extracts are given through mouth (oral) in the form of enteric coated capsules or tablets. Here, the allergen tolerance was reported to improve due to deviation of TH2/TH1 and regulation of IgE production [34]. Studies show clear clinical effectiveness supported by significant symptom improvement and decrease in dosage of drugs required to control the symptoms [35, 36]. However, with high doses of allergen, adverse reactions like intestinal bleeding were seen in this form of immunotherapy [37, 38].
Another route of allergen administration is intranasal (i.n.). Out of 18 studies conducted, 17 reported significant improvement in rhinitis by reduction of nasal sensitivity and local immunological responses [39, 40]. Both, aqueous extracts and dry powders have been tried in nasal immunotherapy. Apparently, nasal immunotherapy exerts its action only on the target organ and the efficacy of the treatment requires preseasonal administration. Here, mild adverse reactions such as rhinitis and itching in the nose have been reported.
Mechanism of immunotherapy
Cooke R.A. (1937) provided the first insight into the mechanisms of SCIT by showing that the transfusion of blood from a patient who had been successfully treated with immunotherapy to an allergic recipient, cured hay fever in the latter [41, 42]. A few years later, the transferable factor was identified as IgG antibodies, which owing to their ability to inhibit immediate skin reactions to allergen provocation were designated as blocking antibodies [43]. Studies on IT have shown modest reduction in allergen-specific IgE levels and induction of allergen-specific IgG subclasses [12, 44–46]. IgG acts as ‘blocking antibody’ and compete with IgE for allergen binding to mast cells, basophils and other IgE receptor-expressing cells. IgE-allergen binds to CD23 on the surfaces of B cells leading to stimulation of allergen-specific T-cell clones. But in patients getting immunotherapy, “blocking” IgG antibodies could inhibit IgE-facilitated allergen binding by B cells and presentation to T cells [47]. Another surface receptor, CD32, is a part of a large population of B-cell co-receptors, which acts to modulate signaling. It has a low-affinity for IgG antibodies and down-regulates antibody production in the presence of IgG. CD32 (FcγII) receptor is involved in the regulation of the B-cell response to antigen [48]. However, the importance of blocking antibodies was questioned, because induction of IgG antibodies is not always associated with clinical improvement after immunotherapy [49].
Studies carried out in defined molecular and cellular systems have rekindled interest in the concept of blocking antibodies [50]. Gradually it has been proved that immunotherapy alters the cytokine profile from a TH2 cytokine dominated response (IL-4 and IL-5) to a TH1-type response with a local accumulation of cells producing IFN-γ [51]. Immunotherapy acts on effector cells inhibiting the release of inflammatory mediators. Early effects of immunotherapy are related to mast cell and basophil desensitization. Intermediate effects are associated with changes in allergen-specific T cells and late effects are on B cells and IgE as well as mast cells, basophils and eosinophils [52].
Control of IgE synthesis is attributed to the actions of mutually antagonistic subsets of CD4+ T cells. Later, activated T cells and their products that play a major role in the pathogenesis of allergic diseases and allergen-specific T cells were considered as the major target for SIT. The concept of T-helper cell heterogeneity with THl and TH2 subsets, which are characterized by a marked variation of their cytokine secretion patterns, has become a common paradigm for description of the immunologic basis of allergic disorders, as well as the mechanism of SIT. The balance between the TH1/TH2 responses is crucial in allergy and atopic asthma. Central paradigm for successful immunotherapy has been to reorient the pattern of allergen-specific T-cell responses in atopic patients from a TH2 to TH1 profile [53]. SIT induces a decrease in IL-4 and IL-5 production by CD4+ TH2 cells and a shift towards increased IFN-γ production by TH1 cells. Activation of TH1 subset is associated with the development of cell mediated immunity, essential for a protective immune response against the development of hypersensitivity/asthma, whereas activation of TH2 subset results in humoral immune response with high IgE production.
IT acts by modifying CD4+ T-cell responses either by immune deviation, T-cell anergy and/or both [54]. Further, a subtype of T cells with immunosuppressive function and cytokine profiles distinct from either TH1 and TH2 cells, termed regulatory/suppressor T cells have been described [54, 55]. Treg cells producing IL-10 and possibly TGF-β, CD4+ CD25+ T cells (possibly TGF-β), and TH3 cells (also TGF- β) play a major role in the inhibition of allergic disorders [56]. It has been reported that IL-10 levels in the bronchoalveolar-lavage fluid of asthmatic patients are lower than in healthy controls, and that T cells from children suffering from asthma also produce less IL-10 mRNA than T cells from control children [57, 58]. There is a growing interest in activating regulatory T cells, capable of down regulating both TH1 and TH2 responses through the production of IL-10 and/or TGF-β (transforming growth factor) [59, 60]. Induction of IL-10 might block B7/CD28 co-stimulation and has a number of documented antiallergic properties that might favur immunotherapy [61, 62]. The properties of T cells producing IL-10 after immunotherapy are contentious, including the immunologic mechanisms that give rise to them. It has yet not been established whether immunotherapy-induced blocking antibodies or T-cell-based down regulation prevent the continuous boosting of IgE production, which otherwise might occur in allergic patients through repeated allergen exposure. Probably, several different mechanisms are responsible for the long-term effects (that is, prolonged clinical remission of symptoms) of immunotherapy. Studies to evaluate the effect of immunotherapy on the T-cell response or cytokine production show conflicting results. While some studies showed decreased IL-4 or IL-5 production, others showed decreased or unaltered IFN-γ production [63].
Sublingual immunotherapy operates through a different route where in the allergen is captured by Langerhans-like dendritic cells in oral mucosa and subsequently, the dendritic cells mature and migrate to proximal draining lymph nodes. The role of these lymph nodes lies in their preferential production of blocking IgG antibodies and the induction of T lymphocytes with suppressive function [64–66]. One explanation for the success of SLIT is the profound difference between oral Langerhans cells and their skin counterparts. Oral Langerhans cells exhibit constitutive high expression of the Fc portion of IgE (FcεRI), major histocompatibility complex (MHC) class I and II, as well as co-stimulatory molecules (CD40, CD80/B7.1, CD86/B7.2), which suggest the specific function of these cells within the regional immune system of the oral mucosa [67, 68]. A recent study has done the comparative analysis of nasal and oral mucosal CD1a+ myeloid dendritic cells of atopic and nonatopic individuals [69]. Both nasal and oral dendritic cell types shared the feature of FcεRI expression, but differed in (1) surface density of FcεRI, (2) lineage specificity, (3) myeloid marker and (4) co-stimulatory and MHC class expression. Furthermore, this study revealed that the lipopolysaccharide receptor CD14, present on both nasal and oral myeloid dendritic cells, was at higher density on oral dendritic cells. Allergen delivery through the sublingual-swallow route appears to be more efficient than either route alone, which suggests an inevitable absorption of allergen through the gastrointestinal tract that potentiates the induction of oral mucosal tolerance [33].
Risks associated with immunotherapy
Local and systemic reactions including severe anaphylaxis leading to death have been reported with subcutaneous injection of allergen immunotherapy [70, 71]. But in most cases it was wrong administration of injection or the overdose of vaccine. Patients with asthma are particularly prone to develop systemic reactions during immunotherapy. This represents the primary argument against the use of IT and secondly use of crude extracts. These untoward reactions can be considerably reduced by using carefully designed protocol depending upon the sensitivity of the patient and the pretreatment. IT must be administered under the supervision of a trained physician to recognize early symptoms and administer emergency treatment wherever necessary. In some cases it may be necessary to administer IT outside the prescribing allergist facility. This decision should be made on individual patient basis weighing the risk versus benefit for the patient. By accepting the responsibility of allergen extract administration, the allergist is agreeing to provide knowledgeable and adequate supervised administration of allergen extract and should have necessary accessories to manage emergencies. Because of the risk of systemic reactions and long duration of treatment, modified allergens and or new routes of administration of vaccines have been explored [30, 31, 40].
Allergens for immunotherapy
Immunotherapy has been effective with pollen, fungi (molds), animal dander, dust mite, cockroach, and in Hymenoptera sensitivity [72]. The current practice of immunotherapy, performed with allergenic products from a wide variety of sources in differing formulations, dilutions and expressed potencies, still has many challenges. Allergen mixture (formulation) requires progress in allergen standardization and information about the efficacy and safety of mixing multiple allergens in a single-vial injection. Knowledge about allergen cross-reactivity, relative compatibility and stability of individual allergens is important in the selection of allergens for immunotherapy, because limiting the number of allergens is necessary to attain optimal therapeutic dose. Phylogenetically related pollens contain cross-reactive allergens, e.g., tree pollen species belonging to same genus/family such as members of family arecaceae (betelnut, fan palm, coconut and date sugar palm), cupressaceae (Japanese cedar, Japanese cypress, mountain cedar) and oleaceae (olive, forsythia, ash, lilac and privet) [73–75]. For substantially cross-reactive pollen allergens, selection of single pollen within the cross-reactive genus or subfamily may suffice the requirement for IT [76]. However, both unique and shared antigens have been reported in phylogenetically related or unrelated insect species [77]. For mixed allergen vaccine, the following factors must be considered; (1) the cross-reactivity of the allergens, (2) the optimal dose of each constituent, and (3) enzymatic degradation of the allergens. Allergenic extracts containing high concentration of proteolytic enzymes have been implicated in reducing the potency of allergen mixture and, thus interfere with their clinical utility [78]. With the discovery of cross-reactive allergens, it is now possible to form a panel of allergens for predicting the sensitization profile and to make right choice of allergens for use in therapy [79].
Native allergen extracts are heterogeneous mixture of proteins and lose potency on storage. The loss in potency affects the results of allergy diagnosis and immunotherapy. Hence, the extracts are recommended to be stored in a refrigerator between 2 and 8°C (35.6–46.4°F), because at higher temperature allergenic proteins degrade rapidly. The inherent proteolytic enzymes can expedite the degradation of self and other allergen extracts in vaccines [80]. Concentrated aqueous extracts (1:10 w/v) in 50% glycerin are stable for about 3 years, if stored in a refrigerator at 4°C (39.2°F), but without glycerin, they may lose half their original strength within 6 months [81]. A study on stability of Periplaneta americana extract shows, EACA (0.05 M) and sucrose (0.25 M) in combination maintain shelf life of extract for 1 year at 4°C [82]. Specific immunotherapy requires extracts with consistent allergenic activity and composition. Standardized extracts are therefore required with a defined potency for vaccines and are labeled with a common unit of measure. However, the commercial extracts vary widely in biologic activity and allergen constituents [83]. The coordinated efforts of scientists at Institute of Genomics and Integrative Biology and clinicians at V. P. Chest Institute, Delhi, have resulted in characterization of many pollen, fungi and/or insect allergens relevant to type I respiratory allergy [84–88]. Besides, few more Indian labs have contributed towards identification of allergenic proteins from pollens. In recent years, allergens from food sources such as chick pea, black gram, rice, peanut and soybean have been evaluated for allergenicity [89–94]. This knowledge can be applied in quality control of extracts for diagnosis and/or therapy of allergic disorders.
The current practice of immunotherapy has many other challenges. To minimize the risk associated with immunotherapy, various approaches given below have been adopted to reduce the allergenicity and retain immunogenicity of antigens.
Allergoids
Allergoids are allergen extracts, polymerized into larger aggregates by a chemical reaction resulting in reduced allergenicity and maintained immunogenicity. Formaldehyde is used to cross-link the proteins and produce toxoids (allergoids). Allergoids (modified proteins) can be given in high doses without much risk as they have reduced capacity to trigger degranulation of mast cells, yet capable of inducing IFN-γ production by T cells [95, 96]. The major advantage of allergoids is that they produce immune response with least risk of systemic reactions. Such preparations are available as depot allergens in some European countries. However, they were not able to completely eliminate the systemic reactions or decrease the initial rise in IgE.
Commercial (glutaraldehyde) polymerized allergens are used in a few European countries for treatment of rhinitis, but they are still not accepted everywhere. Mono methoxy polyethylene glycol conjugated derivatives of allergens have been tried in humans and proved useful in regulating IgE synthesis and preventing systemic reactions [97]. The tolerance was shown to be associated with the induction of non cytotoxic CD8+ suppressor T cells. Glutaraldehyde polymerized allergens could down regulate IgE antibody by inducing the IFN-γ production [98]. The major problem in use of chemically modified allergens in clinical practice has been the difficulty in defining or in standardizing such preparations, and therefore, these could not get clearance from FDA, USA.
Adjuvant/carrier
The occurrence of severe anaphylactic side effects caused by the injection of aqueous allergen extracts and the necessity to administer a great number of injections over long periods prompted the development of safe and efficacious allergen formulations.
Alum
Out of many adjuvants tried to improve the response of allergen vaccines, alum-adsorbed allergen found some applications in immunotherapy. Alum is also used as an adjuvant for tetanus toxoid vaccine and can produce high titer of IgG antibodies. Aqueous and formaldehyde polymerized allergenic (extracts) components adsorbed on calcium phosphate or aluminum hydroxide are currently available in some countries commercially. However, alum together with small quantity of allergen can induce vigorous IgE response, and hence, its utility remains limited [99].
Liposomes
Liposomes made from naturally occurring lipids in the body have been proposed as a carrier of allergens for immunotherapy. Studies with liposomes-entrapped allergen have shown immune response modulating ability in mice [100–102]. Here, we do not require modification of proteins because allergens can be incorporated into liposomes in natural form. Liposome preparations are proved safe to administer, which may be due to the slow release of antigens. Specially designed lipid vesicles like elastic vesicle transfersomes, non-ionic surfactant vesicles (niosomes) are attracting intense attention and can be used for non-invasive antigen delivery. Niosomes and liposomes also have potential in topical delivery of bioactives, but niosomes reflect better immune response than liposomes. Transfersomes are the recent development in vesicle design for transdermal bioactive delivery which differs from conventional niosomes and liposomes by their characteristic fluid membrane with high elasticity. This feature enables transfersomes to squeeze themselves through intercellular regions of the stratum corneum under the influence of transdermal water gradient [103]. In vitro skin permeation experiment revealed that transfersomal formulation has maximum permeation profile, whereas niosomes and liposomes showed relatively low permeation characteristics, because cholesterol affects profoundly their membrane properties. However, these formulations need further investigations.
Recombinant allergens
With the advent of molecular biology methods, several new approaches to immunotherapy became possible including cloning and sequencing of allergen and knowledge of proteins involved in IgE pathways. This has enabled to generate purified homogeneous allergen preparation with consistent potency. The knowledge has also showed the way to block the pathway(s) involved in IgE synthesis. The protein of defined structure and/or patient’s specific therapeutic molecule can be prepared in an appropriate vector. High-level expression systems have been developed to produce recombinant allergens in bacteria, yeast or insect cells. Chapman et al. (2000) [104] have listed 19 recombinant allergens from cat, mite, cockroach, grass, ragweed, birch and peanut that show allergenic activity appropriate for their use in diagnostics. Studies suggest that recombinant allergens show comparable IgE binding to their natural counterparts [105, 106]. Several studies with recombinant allergens have been performed to improve the efficacy and safety of immunotherapy [107]. Modified derivatives of major birch pollen allergen, Bet v 1 have been tried successfully in two studies on immunotherapy [108, 109]. Recombinant allergens also offer the possibility of developing hypo-allergens with reduced IgE reactivity but intact immunogenicity.
Peptides
Peptides are small fragments of protein which are too small to be recognized by IgE for cross-linking on mast cells. Preclinical studies in mice have shown downregulation of both T cell and antibody responses, an increase in allergen-specific IgG2a and clinical protection against anaphylaxis [110]. It has been reported that human lymphocyte cultures, synthetic peptides representing T cell epitopes, if presented without co-stimulation, can induce anergy to subsequent challenges with the peptide or full-length protein [111, 112]. Peptides are not expected to strengthen TH1-mediated immunity, but rather induce a state of tolerance specific to allergen. Peptides for treatment are selected on the basis of their ability to induce proliferation in lymphocyte lines from a panel of patients with a specific allergy. Peptide allergen immunotherapy has been studied extensively with cat major allergen Fel d 1 [113] and with hymenoptera venom major allergen phospholipase A2 [114]. Investigators have examined a collection of overlapping peptides of Fel d 1, each with 12 amino acids in length that covers the whole protein [115, 116]. Because of the peptides overlap, they affect many T cells in a wide variety of individuals. The induction of allergen-specific peripheral T cell tolerance represents an essential step for successful therapy [117]. Complete allergens with the full T cell repertoire are apparently necessary, because multiple T cell epitopes are recognized individually by different patients as a result of the large diversity of MHC and T-cell receptors.
Humanized monoclonal antibodies
Advances in our knowledge of the mechanism of allergic reactions and inflammatory mediators have lead to approaches aimed at selective inhibition of IgE antibody. IgE sensitizes the target cells by binding to the receptor, but does not activate target cell degranulation until the legend is aggregated by the antigen. Methods to competitively inhibit the binding of IgE to mast cells have been explored. It was reported that Fcε fragments derived from human myeloma IgE by cleavage with papain can competitively inhibit passive cutaneous anaphylaxis [118]. This has led to the development of smaller Fcε-derived peptides as potential therapeutic blocking agents. However, this approach has failed due to the development of auto-antibodies to the FcεRI portion of the chimeric molecule, which could continuously trigger mast cell degranulation. Another approach has been neutralization of IgE by monoclonal antibodies directed against a region of IgE involved in the interaction with IgE receptors. The peculiar binding specificity of the antibody has the inherent ability to inhibit effector function by blocking IgE binding to FcεRI receptors on mast cells or basophils and prevent cross-linking by activation of IgE sensitized mast cells.
The humanized monoclonal anti-IgE antibody available is called omalizumab (Xolair: a recombinant humanized monoclonal antibody). It binds to circulating IgE, inhibiting interaction with FcεRI receptors and decreasing the number of FcεRI receptors on basophils. Omalizumab administration decreases inflammatory mediators and also down-regulates dendritic cell FcεRI expression [119]. Anti-IgE therapy reduces leukotriene release of peripheral leukocytes stimulated with allergen in children with allergic rhinitis undergoing allergen immunotherapy. It induces changes in interleukin levels and does not decrease all TH2 related interleukins [120]. It was observed that the mean percentage sputum eosinophil count decreased significantly (P < 0.001) in the omalizumab group, and this was associated with a significant reduction in tissue eosinophils, FcεRI+ cells, CD3+, CD4+, CD8+ T lymphocytes, B lymphocytes and cells staining for IL-4+, but no improvement in airway hyperresponsiveness to methacholine challenge [121]. A recent evaluation by the Cochrane group found that omalizumab led to a significant reduction in inhaled steroid consumption compared to placebo [122].
Omalizumab has a low incidence of side effects, but it is quite expensive and requires administration at frequent intervals. Study in ragweed allergy has demonstrated the potential utility of omalizumab treatment along with allergen-specific immunotherapy [123]. The omalizumab pretreatment provided substantial protection against acute allergic reactions, including anaphylaxis. The combined effect of SIT and omalizumab is associated with prevention of increase in nasal eosinophilic cationic protein increase and decreased tryptase levels in nasal secretions [124]. Administration of omalizumab before and during allergen-specific immunotherapy would lead to a decrease in serum free IgE levels and reduced FcεR1 expression on mast cells and basophils, resulting in increased safety and efficacy. A previous study in children showed that concomitant treatment with omalizumab and allergen-specific (tree or grass) immunotherapy was more effective than allergen immunotherapy alone [125, 126].
Experimental approaches
Anti-cytokine
IL-4 antibodies/soluble IL-4 receptor α chain
IL-4 is a cytokine that is required for B-cell IgE responses and is therefore crucial to type I hypersensitivity responses. IL-4 is the primary TH2 differentiation factor and can be neutralized with anti-IL-4 mAb [127]. Allergen immunotherapy performed in the presence of anti-IL-4 is likely to be more effective in inducing protective immunity. IL-4 has also been targeted by a soluble form of the IL-4 receptor α chain (sIL-4R α), which binds to and inactivates IL-4. A study reported partial efficacy of IL-4 inhibition by sIL-4R α in adult asthmatics, where treated group showed improvement in comparison to the placebo group [128]. Administration of sIL-4Rα seems safe, but further clinical studies are required with this agent [129].
IL-5 antibodies
IL-5, a TH2 cytokine, is involved in pathophysiology of both atopic and non-atopic asthma and allergy. Eosinophils release potentially toxic products that potentiate airway obstruction in asthma. Patients with mild or severe asthma treated with two closely related neutralizing anti-IL-5 antibodies showed no clinical improvement, despite marked suppression of blood eosinophilia [130, 131]. These findings were initially interpreted that the eosinophil is not pathogenic in human asthma [132]. However, subsequent studies have shown that anti-IL-5 treatment during established disease state does not ablate tissue eosinophils, nor does it diminish sputum eosinophils, [133] thereby, reinvigorating the concept that at least lung eosinophils might be pathogenic. In future, anti-IL-5 can be combined with other agents and investigated for inhibition of multiple inflammatory pathways.
Inhibition of signaling pathways
IL-4 and IL-13 are important cytokines of TH2 response and signaling initiated by these leads to enhanced expression of MHC II, CD23, IL-4Rα chain and Ig class switching to IgE and IgG4. Both the cytokines use Janus kinases to initiate signaling, activate signal transduction and transcription-6 (STAT 6) which is a transcription factor suppressor of cytokine signaling-1 (SOCS-1). Its family of proteins acts as inhibitors of cytokine signaling by inhibiting the activity of JAK family members. Some of the target genes induced by STAT-6 can be repressed by BCL-6 (B-cell lymphoma gene-6). The signals required for IL-4/IL-13 induced proliferation are more complex. Inhibition of any steps in this pathway is expected to suppress allergy.
Allergen conjugates
These are allergens chemically linked to oligodeoxynucleotides with immunomodulatory capacity. These conjugates activate the immune system and enhance immunogenicity. The adjuvants include IL-12, IL-18, CpG DNA (consisting of cytidine and guanosine dinucleotide sequences within DNA) and heat killed Listeria monocytogenes. The adjuvants in general, stimulate the innate immune system and antigen presenting cells, and induce a protective type of immunity which blocks the development of TH2 responses and the effects of eosinophils. The fusion protein is formed by combining allergen with some adjuvant or two major allergens. The chemical conjugation reduces the IgE-binding capacity of the allergen conjugates. In the fusion protein, IgE-binding B-cell epitopes are almost totally disrupted, whereas the T-cell epitopes remain intact. So, the fusion protein offer advantages over T-cell peptide-based immunotherapy because it is composed of the complete repertoire of T-cell epitopes. Safe administration of the fusion protein may increase the efficacy of SIT directing the allergic immune response towards a tolerized and balanced/healthy immune response [134]. By providing decreased allergenicity with preserved T-cell tolerance capacity, the fusion protein represents a novel vaccine prototype for allergen-specific immunotherapy.
IL-12
Subcutaneous administration of IL-12 in soluble form shows minimal effects on allergen-specific cells, whereas IL-12 linked with an allergen demonstrate focused effects on antigen-specific cells. IL-12 consists of two chains, joined by a disulfide bond that can be linked to an allergen by linking one of the chains, i.e., IL-12p40 subunit. Using IL-12 allergen conjugate in immunotherapy, the effects of IL-12 can be focused on allergen-specific cells. In a mice study, IL-12 fused with the OVA allergen (fusion protein) has proved effective in reversing TH2 biased immune responses. However, these recombinant constructs are very difficult to produce. Also, IL-12 administration reduced eosinophils but did not reduce airway hyperreactivity, a cardinal feature of asthma [135]. Recombinant human IL-12 was observed to lower numbers of blood and sputum eosinophils, without any significant effects on airway hyperresponsiveness or the late asthmatic reaction. [136].
IL-18
IL-18 is a potent inducer of IFN-γ in T cells, NK cells and B cells. In activated T cells, IL-18 induces up to 100-fold stimulation of IFN-γ than IL-12 alone, and in combination with IL-12 it inhibits IgE synthesis [99]. IL-18 administration in mice could potently inhibit allergen induced airway hyperresponsiveness (AHR). Mice sensitized and challenged with free allergen develop severe AHR as demonstrated by exposure of mice with increasing concentrations of methacholine [137]. But the mice administered with IL-18 during immunization phase showed significant reduction in AHR and airway inflammation in the lungs. Like IL-12, it can also be fused with allergens using recombinant DNA technology. This DNA fusion construct is effective in reversing AHR in sensitized mice.
TLR’s
Toll-like receptor (TLR) ligands offer an exciting prospect for immunotherapeutic strategies to counter allergic disorders. TLR controls innate and adaptive immune responses by inducing synthesis of pro- as well as anti-inflammatory cytokines and activation of effector as well as regulatory lymphocytes. Individual TLR7, TLR8 and TLR9 agonists have already been used successfully as adjuvants to boost CD4+ and CD8+ T-cell responses to candidate microbial vaccine antigens. These agonists seem to be effective when they are covalently conjugated to the immunogens [138]. TLR4 ligands induce DC maturation resulting in the up-regulation of major histocompatibility complex (MHC) and co-stimulatory molecules and in the production of cytokines, which govern the polarization of the CD4+ T-cell responses. Several mechanisms contribute to the protective action of TLR2 ligands against allergic responses. First, TLR2 ligands are able to inhibit the production of TH2 cytokines by allergen-specific T cells [139]. TLR7 and TLR9 are intracellular endosomal receptors for nucleic acids. The effects of TLR7 ligation are similar to those elicited by TLR9 ligation, including the stimulation of plasmacytoid DC to produce high levels of type 1 IFN [140]. Humans TLR9 is expressed on B cells and plasmacytoid DC, the latter cells represent a major source of type 1 IFN, which acts on many cell types and promotes directly and indirectly TH1 polarization of CD4+ T-cell responses [141]. Oligodeoxynucleotides containing unmethylated cytosine-guanine motifs (CpG) are potent TLR9 activators, which induce type 1 interferon and stimulate TH1 responses in vivo [142, 143].
CpG DNA
CpG motifs contain central unmethylated CpG dinucleotide flanked by two 5′ purines and two 3′ pyrimidines and present in bacterial and viral DNA. The sequences mimic infection and are recognized by the innate immune system through specific receptors, called TLR9, on macrophages, dendritic cells (DCs), NK cells and B cells. TLR9 receptors on DCs recognize CpG DNA and results in the production of IL-12, IL-18, IFN-α, IFN-γ and IL-10. This combination of cytokines makes CpG DNA more efficient than any of the cytokines alone. In mammalian DNA, CpG motifs occur but the cytidines are methylated, which prevents recognition by TLR9. The biology of CpG motifs had been reviewed by Krieg and Wagner [143], followed by a review of Toll-like receptor by Zuany-Amorin et al. [144].
The potential use of CpG in the treatment of allergic rhinitis [145] and asthma has been suggested [143, 144]. Synthetic CpG motifs are either mixed with an allergen vaccine or covalently conjugated to an allergen. In the first trial of this concept, a conjugated product was developed by Dynavax Technologies Corporation that has an average ratio of six CpG residues per ragweed Amb a 1 molecule. In vivo administrations of conjugates promoted allergen-specific IgG2a antibody production, a marker for TH1 responses in mice [146]. Such responses occur not only in naive animals, but also in animals previously sensitized with allergen. The conjugate was stimulatory for TH1 responses in rabbits and monkeys as well [147]. Tulic et al. [148] reported clinical and immunologic results comparing CpG-allergen conjugate group (n = 28) with placebo (n = 29) in patients with ragweed-induced hay fever. Symptom reporting was not different between treated patients and placebo in the first post-immunotherapy ragweed season started 3 weeks after the last injection. However, after the end of the season, biopsy specimens after challenge in treated patients showed a significant reduction in eosinophils and IL-4 mRNA-positive cells and an increase of IFN-γ mRNA-positive cells compared to placebo patients. The next ragweed season saw a significant decrease in chest symptoms and a trend toward reduced nasal symptoms without any treatment. These results provide evidence for long-lasting effects from a single short course of allergen–DNA conjugate. CpG motifs present on the vector backbone enhance immunogenicity [111] and effectively induce IL-12, IL-18, IFN-γ production, and antigen-specific CD8 cells [110]. Studies in murine models have demonstrated that DNA immunization strategies prevent the development of antigen-specific IgE synthesis, airway hyperresponsiveness, or food induced anaphylaxis and induce inhibitory CD8 cells [112–114].
Future therapies
Transgenic oral vaccine
The treatment of choice for IgE-mediated food allergy is avoidance of the incriminated food by elimination diet. But avoiding some basic foods such as cow’s milk, etc., becomes difficult because of their widespread use in processed food. Specific immunotherapy in food anaphylaxis is an interesting option, but not always applicable easily [149]. There are reports encouraging oral route of allergen therapy, where the patients developed tolerance on antigen administration orally [150–152]. Techniques to produce transgenic plants are in practice and can be good prospect for food immunotherapy. Therefore, it may not be long to develop allergen vaccines incorporated in certain fruits or foods. But extreme care is required in selection of native material (non-allergenic source) for developing the transgenic vaccine.
Immunization early in life
Recent advances in knowledge related to the maturation of infant immune system suggest new approaches that may enable to deviate the immune response to TH1 type. It is known that normal pregnancy in human is accompanied by TH2 environment around the fetus as IFN-γ a TH1 cytokine would be harmful during pregnancy. As a consequence, the immune system of the new born baby is also skewed toward TH2 type of immunity. During postnatal maturation, there is a shift of the immune response from TH2 to TH1 and a balanced TH1/TH2 immunity is developed in normal children. This shift may have a genetic basis depending on the ability to synthesize IL-12. It seems that environmental exposure to antigens in early life has a considerable effect on this shift. During the postnatal period, the immune system is not fully developed to produce the desired immunoglobulin isotypes due to inefficient TH1 inducing capacity [153]. The postnatal maturation of T cell functions may be particularly slow in atopic children and in majority of children the adult levels are not reached until 3–5 years after birth. It has been reported that certain transient infections during this period actually divert the immune system towards TH1 type.
Early life allergen exposure may increase the risk of childhood allergy, but the protective effect of reduction in allergen exposure remains uncertain. In infants genetically predisposed to atopy, allergen exposure in infancy plays a critical role in the development of phenotypic manifestations, and allergen avoidance in this period may lead to a reduction in the development of allergic diseases with the benefit continuing beyond the actual period of avoidance [154]. The prevention effects of isolated dietary interventions have also been a source of constant study. An apparent decline in microbial exposure during early childhood is suggested to be one of the most plausible causes of the escalating rate of allergic diseases. Today providing probiotics for microbial exposure is considered more active modality to possibly reduce atopic diseases [155]. Most of the studies exploring the role of probiotics in the treatment of allergic disease have focused on the early manifestations of allergy, namely, food allergy and atopic dermatitis. Studies in older individuals with established respiratory disease have failed to show any improvement in asthma [156] or allergic rhinitis [157], although one larger study reported improved quality of life in patients with allergic rhinitis [158]. The lack of any effect of these products in older individuals (with asthma and allergic rhinitis) [156–158] suggests that beneficial effects could be limited to early life before allergic disease is established. Despite a sound theoretical basis for anticipating benefits of probiotic supplementation in allergic disease, there is currently insufficient data to recommend this as a part of standard therapy.
Reports from China on the beneficial effects of BCG immunization in children [159] resulting in TH1 response and further prevention of sensitization are interesting. Studies indicate an increased risk for allergy on exposure to environmental allergens early in life may lead to allergic sensitization later [160]. Thus, inducing a TH1 response to an antigen early in life could prevent a subsequent TH2 response to the same antigen. Also creating a pervasive TH1 dominated environment could influence the response occurring to the exposure of other allergenic proteins. Using the various allergen-specific methods with adjuvants or DNA based immunizations at an early age to high-risk children may give a long lasting protective TH1 response [161]. Here, the major problem is to reliably identify children at high risk. With the developments in human genome project, it may be possible to identify genes responsible for allergy/asthma which serve as markers for identifying children at high risk. These children can be benefited by proper immunotherapy at an early age before their immune responses get locked up in TH2 immunity.
References
Akdis M, Verhagen J, Taylor A, et al. Immune responses in healthy and allergic individuals are characterized by a fine balance between allergen-specific T regulatory 1 and T helper 2 cells. J Exp Med. 2004;199:1567–75.
Galli SJ, Tsai M, Piliponsky AM. The development of allergic inflammation. Nature. 2008;454:445–54.
Lund R, Ahlfors H, Kainonen E, Lahesmaa AM, Dixon C, Lahesmaa R. Identification of genes involved in the initiation of human Th1 or Th2 cell commitment. Eur J Immunol. 2005;35:3307–19.
Dong C, Flavell RA. TH1 and TH2 cells. Curr Opin Hematol. 2001;8:47–51.
Tavakkol Afshari J, Farid Hosseini R, Hosseini Farahabadi S, et al. Association of the expression of IL-4 and IL-13 genes, IL-4 and IgE serum levels with allergic asthma. Iran J Allergy Asthma Immunol. 2007;6:67–72.
Salib RJ, Drake-Lee A, Howarth PH. Allergic rhinitis: past, present and the future. Clin Otolaryngol Allied Sci. 2003;28:291–303.
Gaur SN, Rajpal S, Rohatgi A. Prevalence of bronchial asthma and allergic rhinitis among school children in Delhi. Intern Med J Thai. 2004;20:8–13.
Chhabra SK, Gupta CK, Chhabra P, Rajpal S. Prevalence of bronchial asthma in schoolchildren in Delhi. J Asthma. 1998;35:291–6.
Vishwanathan R. Definition, incidence, etiology and natural history of asthma. Ind J Chest Dis. 1964;6:108–24.
Ariano R, Berto P, Tracci D, Incorvaia C, Frati F. Pharmacoeconomics of allergen immunotherapy compared with symptomatic drug treatment in patients with allergic rhinitis and asthma. Allergy Asthma Proc. 2006;27:159–63.
Chan-Yeung M, Dimich-Ward H, Becker A. Atopy in early life and effect of a primary prevention program for asthma in a high-risk cohort. J Allergy Clin Immunol. 2007;120:1221–3.
Tonnel AB. Specific immunotherapy and therapeutic strategies in allergic diseases. What’s new? Bull Acad Natl Med. 2005;189:1475–87.
Moller C, Dreborg S, Ferdousi HA, et al. Pollen immunotherapy reduces the development of asthma in children with seasonal rhinoconjunctivitis. J Allergy Clin Immunol. 2002;109:251–6.
Adkinson NF Jr, Eggleston PA, Eney D, et al. A controlled trial of immunotherapy for asthma in allergic children. N Engl J Med. 1997;336:324–31.
Dam Petersen K, Gyrd-Hansen D, Kjaergaard S, Dahl R. Clinical and patient based evaluation of immunotherapy for grass pollen and mite allergy. Allergol Immunopathol (Madr). 2005;33:264–9.
Casimir G, Cuvelier P, Allard S, Duchateau J. Life-threatening fish allergy successfully treated with immunotherapy. Pediatr Allergy Immunol. 1997;8:103–5.
Gaur SN, Gupta S. Clinical response of immunotherapy in cases of nasobronchial allergy. Indian J Allergy Appl Immunol. 1996;10:65–8.
Karmakar PR, Das A, Chatterjee BP. Placebo-controlled immunotherapy with Cocos nucifera pollen extract. Int Arch Allergy Immunol. 1994;103:194–201.
Sheikh WA. Immunotherapy vs. inhaled budesonide in bronchial asthma: an open, parallel, comparative trial. Clin Exp Allergy. 1997;27:1279–84.
Srivastava D, Singh BP, Sudha VT, Arora N, Gaur SN. Immunotherapy with mosquito (Culex quinquefasciatus) extract: a double-blind, placebo-controlled study. Ann Allergy Asthma Immunol. 2007;99:273–80.
Anonymus (2007) Clinico-immunologic studies on allergen specific immunotherapy in patients of respiratory allergy (2004–2007). Project report Department of Science and Technology, New Delhi.
Young-Min Y, Soo-Keol L, Seung-Hyun K, Dong-Ho N, Chang-Hee S, Hae-Sim P. Changes of serum cytokines after the long-term immunotherapy with Japanese Hop pollen extracts. J Korean Med Sci. 2006;21:805–10.
Ohashi Y, Nakai Y, Tanaka A, et al. Ten-year follow-up study of allergen-specific immunoglobulin E and immunoglobulin G4, soluble interleukin-2 receptor, interleukin-4, soluble intercellular adhesion molecule-1 and soluble vascular cell adhesion molecule-1 in serum of patients on immunotherapy for perennial allergic rhinitis. Scand J Immunol. 1998;47:167–78.
Pajno GB, Barberio G, De Luca F, Morabito L, Parmiani S. Prevention of new sensitizations in asthmatic children monosensitized to house dust mite by specific immunotherapy. A six-year follow-up study. Clin Exp Allergy. 2001;31:1392–7.
Marcucci F, Sensi L, Allocca G, et al. Sublingual immunotherapy: from safety to mechanism of action. Eur Ann Allergy Clin Immunol. 2007;39:101–3.
Di Gioacchino M, Perrone A, Petrarca C, et al. Early cytokine modulation after the rapid induction phase of sublingual immunotherapy with mite monomeric allergoids. Int J Immunopathol Pharmacol. 2008;21:969–76.
Savolainen J, Jacobsen L, Valovirta E. Sublingual immunotherapy in children modulates allergen-induced in vitro expression of cytokine mRNA in PBMC. Allergy. 2006;61:1184–90.
Akdis CA, Barlan IB, Bahceciler N, Akdis M. Immunological mechanisms of sublingual immunotherapy. Allergy. 2006;S 81:11–4.
Antunez C, Mayorga C, Corzo JL, Jurado A, Torres MJ. Two year follow-up of immunological response in mite-allergic children treated with sublingual immunotherapy. Comparison with subcutaneous administration. Pediatr Allergy Immunol. 2008;19:210–8.
Silvestri M, Spallarosa D, Battistini E, et al. Changes in inflammatory and clinical parameters and in bronchial hyperreactivity asthmatic children sensitized to house dust mites following sublingual immunotherapy. J Investig Allergol Clin Immunol. 2002;12:52–9.
Mortemousque B, Bertel F, De Casamayor J, Verin P, Colin J. House dust mite sublingual swallow immunotherapy in perennial conjunctivitis: a double blind placebo controlled study. Clin Exp Allergy. 2003;33:464–9.
Sun JB, Cuburu N, Blomquist M, Li BL, Czerkinsky C, Holmgren J. Sublingual tolerance induction with antigen conjugated to cholera toxin B subunit induces Foxp3+ CD25+ CD4+ regulatory T cells and suppresses delayed-type hypersensitivity reactions. Scand J Immunol. 2006;64:251–9.
Bagnasco M, Mariani G, Passalacqua G, et al. Absorption and distribution kinetics of the major Parietaria judaica allergen (Par j 1) administered by noninjectable routes in healthy human beings. J Allergy Clin Immunol. 1997;100:122–9.
Moller C, Dreborg S, Lanner A, Bjorksten B. Oral immunotherapy of children with rhinoconjuctivitis due to birch pollen allergy. Allergy. 1986;41:271–7.
Giovane A, Bardare M, Passalacqua G. A three year double blind placebo controlled study with oral immunotherapy to pediatric patients. Clin Exp Allergy. 1994;24:53–9.
Miller A, Lider O, Roberts AB, Sporn MB, Weiner HL. Suppressor T cells generated by oral tolerance to myelin basic protein suppress both in vitro and in vivo immune response by release of TGF β following antigen specific triggering. Proc Nal Acad Sci USA. 1992;89:421–5.
Mosbech H, Dreberg S, Madsenn F. High dose grass pollen tablets used for hyposensitization in hay fever patients. A 1 year double blind placebo controlled study. Allergy. 1987;42:451–5.
Litwin A, Flanazan M, Eritis G. Oral immunotherapy with short ragweed in a novel encapsulated preparation: a double blind study. J Allergy Clin Immunol. 1997;100:30–8.
Tari MG, Mancino M, Monti G. Immunotherapy by inhalation of allergen in powder in house dust allergic asthma: a double blind study. J Invest Allergol Clin Immunol. 1992;2:59–67.
Schumacher MJ, Pain MC. Intranasal immunotherapy with polymerized grass pollen allergens. Allergy. 1982;37:241–8.
Loveless MH. Immunological studies of pollinosis: I. The presence of two antibodies related to the same pollen antigen in the serum of treated hay-fever patients. J Immunol. 1940;38:25–50.
Pilette C, Nouri-Aria KT, Jacobson MR, et al. Grass pollen immunotherapy induces an allergen-specific IgA2 antibody response associated with mucosal TGF-β expression. J Immunol. 2007;178:4658–66.
Flicker S, Steinberger P, Norderhaug L, et al. Conversion of grass pollen allergen specific human IgE into a protective IgG1 antibody. Eur J Immunol. 2002;32:2156–62.
Kawakami A, Koketsu R, Suzukawa M, et al. Blocking antibody is generated in allergic rhinitis patients during specific immunotherapy using standardized Japanese cedar pollen extract. Int Arch Allergy Immunol. 2008;146(S1):54–60.
Rabinovitch N, Gelfand EW. Expression of functional activating and inhibitory Fcgamma receptors on human B cells. Int Arch Allergy Immunol. 2004;133:285–94.
Larche M, Akdis CA, Valenta R. Immunological mechanisms of allergen-specific immunotherapy. Nat Rev Immunol. 2006;6:761–71.
Wachholz PA, Soni NK, Till SJ, Durham SR. Inhibition of allergen-IgE binding to B cells by IgG antibodies after grass pollen immunotherapy. J Allergy Clin Immunol. 2003;112:915–22.
Zhuang Q, Bisotto S, Fixman ED, Mazer B. Suppression of IL-4- and CD40-induced B-lymphocyte activation by intravenous immunoglobulin is not mediated through the inhibitory IgG receptor FcgammaRIIb. J Allergy Clin Immunol. 2002;110:480–3.
Jeannin P, Delneste Y, Tillie-Leblond I, et al. Abnormal IgG4 antibody response to aeroallergens in allergic patients. Int Arch Allergy Immunol. 1994;104:191–8.
Ball T, Sperr WR, Valent P, et al. Induction of antibody responses to new B-cell epitopes indicates vaccination character of allergen immunotherapy. Eur J Immunol. 1999;29:2026–36.
Durham SR, Walker SM, Varga EM, et al. Long-term clinical efficacy of grass pollen immunotherapy. N Engl J Med. 1999;341:468–75.
Akdis M, Akdis CA. Mechanisms of allergen-specific immunotherapy. J Allergy Clin Immunol. 2007;119:780–9.
Van Neerven RJ, Wikborg T, Lund G, et al. Blocking antibodies induced by specific allergy vaccination prevents the activation of CD4+ T cells by inhibiting serum-IgE-facilitated allergen presentation. J Immunol. 1999;163:2944–52.
McHugh SM, Deighton J, Stewart AG, Lachmann PJ, Ewan PW. Bee venom immunotherapy induces a shift in cytokine response from a TH2 to a TH1 dominant pattern: comparison of rush and conventional immunotherapy. Clin Exp Allergy. 1995;25:828–33.
Gardner LM, Thien FC, Douglass JA, Rolland JM, O’Hehir RE. Induction of T regulatory cells by standardized house dust mite immunotherapy: an increase in CD4+ CD25+ interleukin-10+ T cells expressing peripheral tissue trafficking markers. Clin Exp Allergy. 2004;34:1209–19.
Presser K, Schwinge D, Wegmann M, et al. Coexpression of TGF-beta1 and IL-10 enables regulatory T cells to completely suppress airway hyperreactivity. J Immunol. 2008;181:7751–8.
Borish L, Aarons A, Rumbyrt J, Cvietusa P, Negri J, Wenzel S. Interleukin-10 regulation in normal subjects and patients with asthma. J Allergy Clin Immunol. 1996;97:1288–96.
Koning H, Neijens HJ, Baert MR, Oranje AP, Savelkoul HF. T cells subsets and cytokines in allergic and non-allergic children. II. Analysis and IL-5 and IL-10 mRNA expression and protein production. Cytokine. 1997;9:427–36.
Jutel M, Akdis M, Budak F, et al. IL-10 and TGF-β cooperate in the regulatory T cell response to mucosal allergens in normal immunity and specific immunotherapy. Eur J Immunol. 2003;33:1205–14.
Francis JN, Till SJ, Durham SR. Induction of IL-10 CD4+ CD25+ T cells by grass pollen immunotherapy. J Allergy Clin Immunol. 2003;111:1255–61.
Schandene L, Alonso-Vega C, Willems F, et al. B7/CD28-dependent IL-5 production by human resting T cells is inhibited by IL-10. J Immunol. 1994;152:4368–74.
Akdis CA, Joss A, Akdis M, Faith A, Blaser K. A molecular basis for T cell suppression by IL-10: CD28-associated IL-10 receptor inhibits CD28 tyrosine phosphorylation and phosphatidylinositol. 3-kinase binding. FASEB J. 2000;14:1666–8.
Abramson MJ, Puy RM, Weiner JM. Allergen immunotherapy for asthma. Cochrane Database Syst Rev. 2003;4:CD001186.
Tseng SH, Fu LS, Nong BR, Weng JD, Shyur SD. Changes in serum specific IgG4 and IgG4/IgE ratio in mite-sensitized Taiwanese children with allergic rhinitis receiving short-term sublingual-swallow immunotherapy: a multicenter, randomized, placebo-controlled trial. Asian Pac J Allergy Immunol. 2008;26:105–12.
Moingeon P, Batard T, Fadel R, Frati F, Sieber J, Van Overtvelt L. Immune mechanisms of allergen-specific sublingual immunotherapy. Allergy. 2006;61:151–65.
Bohle B, Kinaciyan T, Gerstmayr M, Radakovics A, Jahn-Schmid B, Ebner C. Sublingual immunotherapy induces IL-10-producing T regulatory cells, allergen-specific T-cell tolerance, and immune deviation. J Allergy Clin Immunol. 2007;120:707–13.
Cosmi L, Santarlasci V, Angeli R, et al. Sublingual immunotherapy with Dermatophagoides monomeric allergoid down-regulates allergen-specific immunoglobulin E and increases both interferon-gamma- and interleukin-10-production. Clin Exp Allergy. 2006;36:261–72.
Allam JP, Novak N, Fuchs C, et al. Characterization of dendritic cells from human oral mucosa: a new Langerhans cell type with high constitutive FcepsilonRI expression. J Allergy Clin Immunol. 2003;112:141–8.
Allam JP, Niederhagen B, Bücheler M, et al. Comparative analysis of nasal and oral mucosa dendritic cells. Allergy. 2006;61:166–72.
Rank MA, Oslie CL, Krogman JL, Park MA, Li JT. Allergen immunotherapy safety: characterizing systemic reactions and identifying risk factors. Allergy Asthma Proc. 2008;29:400–5.
Karaayvaz M, Erel F, Caliskaner Z, Ozanguc N. Systemic reactions due to allergen immunotherapy. J Investig Allergol Clin Immunol. 1999;9:39–44.
Martin Munoz MF. Efficacy of immunotherapy in the treatment of asthma. Allergol Immunopathol. 2004;32:133–41.
Gonzalez EM, Villalba M, Rodriguez R. Allergenic cross-reactivity of Olive pollen. Allergy. 2000;55:658–63.
Di Felice G, Barletta B, Tingho R, Pini C. Cupressaceae pollinosis: identification, purification and cloning of relevant allergens. Int Arch Allergy Immunol. 2001;125:280–9.
Chakraborty P, Gupta-Bhattacharya S, Roy I, Chanda S. Identification of shared allergenic components from four common and dominant pollen taxa of Arecaceae. Curr Science. 2004;86:1539–43.
Moingeon P, Hrabina M, Bergmann KC, et al. Specific immunotherapy for common grass pollen allergies: pertinence of a five grass pollen vaccine. Int Arch Allergy Immunol. 2008;146:338–42.
Chaudhry S, Jhamb S, Chauhan UP, Gaur SN, Agarwal HC, Agarwal MK. Shared and specific allergenic and antigenic components in the two sexes of American cockroach Periplaneta americana. Clin Exp Allergy. 1990;20:59–65.
Grier TJ, LeFevre DM, Duncan EA, Esch RE. Stability of standardized grass, dust mite, cat, and short ragweed allergens after mixing with mold or cockroach extracts. Ann Allergy Asthma Immunol. 2007;99:151–60.
Pauli G. Evolution in the understanding of cross-reactivities of respiratory allergens: the role of recombinant allergens. Int Arch Allergy Immunol. 2000;123:183–95.
Van der Veen MJ, Mulder M, Witteman AM, Van Ree R, Aalberse RC, Jansen HM. False-positive skin prick test responses to commercially available dog dander extracts caused by contamination with house dust mite (Dermatophagoides pteronyssinus) allergens. J Allergy Clin Immunol. 1996;98:1028–34.
Singh BP, Gangal SV. Defined allergen extracts; need for efficient diagnosis of allergy and immunotherapy. Indian J Allergy Asthma Immunol. 2001;15:67–74.
Sudha VT, Srivastava D, Arora N, Gaur SN, Singh BP. Stability of protease rich Periplaneta americana allergen extracts during storage: formulating preservatives to enhance shelf life. J Clin Immunol. 2007;27:294–301.
Ruiz Reyes H, Rodriguez Orozco AR. Allergic fungi: importance of the standardization of fungal extracts and their application on clinical practice. Rev Alerg Mex. 2006;53:144–9.
Bijli KM, Singh BP, Sridhara S, Gaur SN, Arora N. Standardizing Imperata cylindrica source material for quality allergen preparations. Immunol Methods. 2002;260:91–6.
Kurup VP. Fungal allergens. Curr Allergy Asthma Rep. 2003;3:416–23.
Bisht V, Arora N, Singh BP, Gaur SN, Sridhara S. Purification and characterization of a major cross-reactive allergen from Epicoccum purpurascens. Int Arch Allergy Immunol. 2004;133:217–24.
Dhyani A, Arora N, Gaur SN, Jain VK, Sridhara S, Singh BP. Analysis of IgE binding proteins of mesquite (Prosopis juliflora) pollen and cross-reactivity with predominant tree pollens. Immunobiology. 2006;211:733–40.
Sudha VT, Arora N, Sridhara S, Gaur SN, Singh BP. Biopotency and identification of allergenic proteins in Periplaneta americana extract for clinical applications. Biologicals. 2006;35:131–7.
Patil SP, Niphadkar PV, Bapat MM. Chickpea: a major food allergen in the Indian subcontinent and its clinical and immunochemical correlation. Ann Allergy Asthma Immunol. 2001;87:140–5.
Kumari D, Kumar R, Sridhara S, Arora N, Gaur SN, Singh BP. Sensitization to black gram in patients with bronchial asthma and rhinitis: clinical evaluation and characterization of allergens. Allergy. 2006;61:104–10.
Kumar R, Srivastava P, Kumari D, et al. Rice (Oryza sativa) allergy in rhinitis and asthma patients: a clinico-immunological study. Immunobiology. 2007;212:141–7.
Ito M, Kato T, Matsuda T. Rice allergenic proteins, 14–16 kDa albumin and alpha-globulin, remain insoluble in rice grains recovered from rice miso (rice-containing fermented soybean paste). Biosci Biotechnol Biochem. 2005;69:1137–44.
Scurlock AM, Burks AW. Peanut allergenicity. Ann Allergy Asthma Immunol. 2004;93:S12–8.
Lin J, Shewry PR, Archer DB, et al. Potential allergenicity of two 2S albumins from soybean (Glycine max): a protein microarray approach. Int Arch Allergy Immunol. 2006;141:91–102.
Secrist H, DeKruyff RH, Umetsu DT. Interleukin 4 production by CD4+ cells from allergic individuals is modulated by allergen concentration and antigen-presenting cell type. J Exp Med. 1995;181:1081–90.
HayGlass KT, Stefura BP. Anti-interferon gamma treatment blocks the ability of glutaraldehyde-polymerized allergens to inhibit specific IgE responses. J Exp Med. 1991;173:279–85.
Ohman S, Bjorkander J, Dreborg S, Lanner A, Malling HJ, Weeke B. A preliminary study of immunotherapy with a monomethoxy polyethylene glycol modified honey bee venom preparation. Allergy. 1986;41:81–8.
Malet A, Lluch M, Valero AL, Casanovas M. Clinical and immunological effects of immunotherapy with glutaraldehyde modified house dust mite extract. Allergol Immunopathol (Madr). 1994;22:226–32.
Pollock KG, Conacher M, Wei XQ, Alexander J, Brewer JM. Interleukin-18 plays a role in both the alum-induced T helper 2 response and the T helper 1 response induced by alum-adsorbed interleukin-12. Immunology. 2003;108:137–43.
Arora N, Gangal SV. Efficacy of liposome entrapped allergen in regulation of IgE response in mice. Clin Exp Allergy. 1992;22:35–42.
Gangal SV, Arora N, Chugh L, Sehra S, Singh B, Malik BK (1999) Immunomodulation and immunotherapy using liposome entrapped allergens. Arb Paul Ehrlich Inst Bundesamt Sera Impfstoffe Frankf A M 93: 267–73
Sehra S, Chug L, Gangal SV. Polarized TH1 responses by liposome entrapped allergen and its potential in immunotherapy of allergic disorders. Clin Exp Allergy. 1998;28:1530–7.
Cevc G, Gebauer D, Stieber J, Schaltzein A, Blume G. Ultraflexible vesicles, transfersomes, have an extremely pore penetration resistant and transport therapeutic amount of insulin across the intact mammalian skin. Biochim Biophys Acta. 1998;1368:201–15.
Chapman MD, Smith AM, Vailes LD, Arruda LK, Dhanaraj V, Pomes A. Recombinant allergens for diagnosis and therapy of allergic diseases. J Allergy Clin Immunol. 2000;106:409–18.
Shankar J, Singh BP, Gaur SN, Arora N. Recombinant glutathione-S-transferase, a major allergen from Alternaria alternata for clinical use in allergy patients. Mol Immunol. 2006;43:1927–32.
Tresch S, Holzmann D, Baumann S, et al. In vitro and in vivo allergenicity of recombinant Bet v 1 compared to the reactivity of natural birch pollen extract. Clin Exp Allergy. 2003;33:1153–8.
Jutel M, Jaeger L, Suck R, Meyer H, Fiebig H, Cromwell O. Allergen-specific immunotherapy with recombinant grass pollen allergens. J Allergy Clin Immunol. 2005;116:608–13.
Pauli G, Larsen TH, Rak S, et al. Efficacy of recombinant birch pollen vaccine for the treatment of birch-allergic rhinoconjunctivitis. J Allergy Clin Immunol. 2008;122:951–60.
Niederberger V, Horak F, Vrtala S, et al. Vaccination with genetically engineered allergens prevents progression of allergic disease. Proc Natl Acad Sci USA. 2004;101:14677–82.
Von Garnier C, Astori M, Kettner A, et al. Allergen-derived long peptide immunotherapy down-regulates specific IgE response and protects from anaphylaxis. Eur J Immunol. 2000;30:1638–45.
Kammerer R, Chvatchko Y, Kettner A, Dufour N, Corradin G, Spertini F. Modulation of T-cell response to phospholipase A2 and phospholipase A2-derived peptides by conventional bee venom immunotherapy. J Allergy Clin Immunol. 1997;100:96–103.
Fellrath JM, Kettner A, Dufour N, et al. Allergen-specific T-cell tolerance induction with allergen-derived long synthetic peptides: results of a phase I trial. J Allergy Clin Immunol. 2003;111:854–61.
Pene J, Desroches A, Paradis L, et al. Immunotherapy with Fel d 1 peptides decreases IL-4 release by peripheral blood T cells of patients allergic to cats. J Allergy Clin Immunol. 1998;102:571–8.
Muller U, Akdis CA, Fricker M, et al. Successful immunotherapy with T-cell epitope peptides of bee venom phospholipase A 2 induces specific T-cell anergy in patients allergic to bee venom. J Allergy Clin Immunol. 1998;101:747–54.
Oldfield W, Larche M, Kay A. Effect of T cell peptides derived from Fel d 1 on allergic reactions and cytokine production in patients sensitive to cats: a randomized controlled trial. Lancet. 2002;360:47–53.
Maguire P, Nicodemus C, Aaronson D, Robinson D, Umetsu DT. The safety and efficacy of ALLERVAX CAT in cat allergic patients. Clin Immunol. 1999;93:222–31.
Akdis CA, Akdis M, Blesken T, et al. Epitope-specific T cell tolerance to phospholipase A2 in bee venom immunotherapy and recovery by IL-2 and IL-15 in vitro. J Clin Invest. 1996;98:1676–83.
Helm BA, Spivey AC, Padlan EA. Peptide blocking of IgE/receptors interaction: possibilities and pitfalls. Allergy. 1997;52:1155–69.
Prussin C, Griffith DT, Boesel KM, Lin H, Foster B, Casale TB. Omalizumab treatment down regulates dendritic cell FcepsilonRI expression. J Allergy Clin Immunol. 2003;112:1147–54.
Kopp MV, Brauburger J, Riedinger F, et al. The effect of anti-IgE treatment on in vitro leukotriene release in children with seasonal allergic rhinitis. J Allergy Clin Immunol. 2002;110:728–35.
Djukanovi R, Wilson SJ, Kraft M, Jarjour NN, Steel M, Chung KF et al. Effects of treatment with anti-immunoglobulin E antibody omalizumab on airway inflammation in allergic asthma. Am J Respir Crit Care Med. (2004); 170: 583–93.
Walker S, Monteil M, Phelan K, Lasserson TJ, Walters EH. Anti-IgE for chronic asthma in adults and children. Cochrane Database Syst Rev. 2006;19(2):CD003559.
Casale TB, Busse WW, Kline JN, et al. Omalizumab pretreatment decreases acute reactions after rush immunotherapy for ragweed-induced seasonal allergic rhinitis. J. Allergy Clin Immunol. 2006;117:134–40.
Bez C, Schubert R, Kopp M, et al. Effect of anti-immunoglobulin E on nasal inflammation in patients with seasonal allergic rhino conjunctivitis. Clin Exp Allergy. 2004;34:1079–85.
Rolinck-Werninghaus C, Hamelmann E, Keil T, et al. The co-seasonal application of anti-IgE after preseasonal specific immunotherapy decreases ocular and nasal symptom scores and rescue medication use in grass pollen allergic children. Allergy. 2004;59:973–9.
Kuehr J, Brauburger J, Zielen S, et al. Efficacy of combination treatment with anti-IgE plus specific immunotherapy in polysensitized children and adolescents with seasonal allergic rhinitis. J Allergy Clin Immunol. 2002;109:274–80.
Tournoy KG, Kips JC, Pauwels RA. The allergen-induced airway hyperresponsiveness in a human-mouse chimera model of asthma is T cell and IL-4 and IL-5 dependent. J Immunol. 2001;166:6982–91.
Borish LC, Nelson HS, Corren J, et al. Efficacy of soluble IL-4 receptor for the treatment of adults with asthma. J Allergy Clin Immunol. 2001;107:963–70.
Borish LC, Nelson HS, Lanz MJ, et al. Interleukin-4 receptor in moderate atopic asthma. A phase I/II randomized, placebo-controlled trial. Am J Respir Crit Care Med. 1999;160:1816–23.
Kips JC, O’Connor BJ, Langley SJ, et al. Effect of SCH55700, a humanized anti-human interleukin-5 antibody, in severe persistent asthma: a pilot study. Am J Respir Crit Care Med. 2003;167:1655–9.
Leckie MJ, ten Brinke A, Khan J, et al. Effects of an interleukin-5 blocking monoclonal antibody on eosinophils, airway hyper-responsiveness, and the late asthmatic response. Lancet. 2000;356:2144–8.
Boushey HA, Fahy JV. Targeting cytokines in asthma therapy: round one. Lancet. 2000;356:2114–6.
Flood-Page PT, Menzies-Gow AN, Kay AB, Robinson DS. Eosinophil’s role remains uncertain as anti-interleukin-5 only partially depletes numbers in asthmatic airway. Am J Respir Crit Care Med. 2003;167:199–204.
Terada T, Zhang K, Belperio J, Londhe V, Saxon A. A chimeric human-cat Fcgamma-Fel d 1 fusion protein inhibits systemic, pulmonary and cutaneous allergic reactivity to intratracheal challenge in mice sensitized to Fel d 1, the major cat allergen. Clin Immunol. 2006;120:45–56.
Bryan SA, O’Connor BJ, Matti S, et al. Effects of recombinant human interleukin-12 on eosinophils, airway hyper-responsiveness, and the late asthmatic response. Lancet. 2000;356:2149–53.
Kim TS, DeKruyff RH, Rupper R, Maecker HT, Levy S, Umetsu DT. An ova-IL-12 fusion protein is more effective than OVA plus rIL-12 in inducing a Th1-dominated immune response and inhibiting antigen-specific IgE production. J Immunol. 1997;158:4137–44.
Walter DM, Wong CP, DeKruyff RH, Berry GJ, Levy S, Umetsu DT. IL-18 gene transfer by adenovirus prevents the development of and reverses established allergen induced airway hyper reactivity. J Immunol. 2001;166:6392–8.
Revets H, Pynaert G, Grooten J, De Baetselier P. Lipoprotein I, a TLR2/4 ligand modulates TH2-driven allergic immune responses. J Immunol. 2005;174:1097–103.
Taylor RC, Richmond P, Upham JW. Toll-like receptor 2 ligands inhibit TH2 responses to mite allergen. J Allergy Clin Immunol. 2006;117:1148–54.
Takeda K, Akira S. Toll-like receptors in innate immunity. Int Immunol. 2005;17:1–14.
Krieg AM. Therapeutic potential of Toll-like receptor 9 activation. Nat Rev Drug Discov. 2006;5:471–84.
Klinman DM. Immunotherapeutic uses of CpG oligodeoxynucleotides. Nat Rev Immunol. 2004;4:249–58.
Krieg AM, Wagner H. Causing a commotion in the blood: immunotherapy progresses from bacteria to bacterial DNA. Immunol Today. 2000;21:521–6.
Zuany-Amorim C, Hastewell J, Walker C. Toll-like receptors as potential therapeutic targets for multiple diseases. Nat Rev Drug Discov. 2002;1:797–807.
Creticos PS, Schroeder JT, Hamilton RG, et al. Immunotherapy with a ragweed-toll-like receptor 9 agonist vaccine for allergic rhinitis. N Engl J Med. 2006;355:1445–55.
Shirota H, Sano K, Kikuchi T, Tamura G, Shirato K. Regulation of murine airway eosinophilia and TH2 cells by antigen-conjugated CpG oligodeoxynucleotides as a novel antigen-specific immunomodulator. J Immunol. 2000;164:5575–82.
Tighe H, Takabayashi K, Schwartz D, et al. Conjugation of immunostimulatory DNA to the short ragweed allergen Amb a 1 enhances its immunogenicity and reduces its allergenicity. J Allergy Clin Immunol. 2000;106:124–34.
Tulic MK, Fiset PO, Christodoulopoulos P, et al. Amb a 1-immunostimulatory oligodeoxynucleotide conjugate immunotherapy decreases the nasal inflammatory response. J Allergy Clin Immunol. 2004;113:235–41.
Kerzl R, Mempel M, Ring J. Allergen-specific immunotherapy in food anaphylaxis. WAO J. (2008); 1:47–50.
Mansfield L. Successful oral desensitization for systemic peanut allergy. Ann Allergy Asthma Immunol. 2006;97:266–7.
Oppenheimer JJ, Nelson HS, Bock SA, Christensen F, Leung DY. Treatment of peanut allergy with rush immunotherapy. J Allergy Clin Immunol. 1992;90:256–62.
Patriarca G, Nucera E, Pollastrini E, et al. Oral rush desensitization in peanut allergy: a case report. Dig Dis Sci. 2006;51:471–3.
Bjorksten B. The intrauterine and post natal environments. J Allergy Clin Immunol. 1999;104:1119–27.
Arshad SH, Bateman B, Sadeghnejad A, Gant C, Matthews SM. Prevention of allergic disease during childhood by allergen avoidance: the Isle of Wight prevention study. J Allergy Clin Immunol. 2007;119:307–13.
Sicherer SH, Leung DY. Advances in allergic skin disease, anaphylaxis, and hypersensitivity reactions to foods, drugs, and insects in 2007. J Allergy Clin Immunol. 2008;121:1351–8.
Wheeler JG, Shema SJ, Bogle ML, et al. Immune and clinical impact of Lactobacillus acidophilus on asthma. Ann Allergy Asthma Immunol. 1997;79:229–33.
Helin T, Haahtela S, Haahtela T. No effect of oral treatment with an intestinal bacterial strain, Lactobacillus rhamnosus (ATCC 53103), on birch-pollen allergy: a placebo-controlled double-blind study. Allergy. 2002;57:243–6.
Wang MF, Lin HC, Wang YY, Hsu CH. Treatment of perennial allergic rhinitis with lactic acid bacteria. Pediatr Allergy Immunol. 2004;15:152–8.
Guo YJ, Wu D, Wang KY, Sun SH. Adjuvant effects of Bacillus Calmette-Guerin DNA or CpG-oligonucleotide in the immune response to Taenia solium cysticercosis vaccine in porcine. Scand J Immunol. 2007;66:619–27.
Stelmach I, Smejda K, Jerzynska J, et al. Decreased markers of atopy in children with presumed early exposure to allergens, unhygienic conditions, and infections. Ann Allergy Asthma Immunol. 2007;99:170–7.
Holt PG. A potential vaccine strategy for asthma and allied atopic diseases during early childhood. The Lancet. 1994;344:456–8.
Author information
Authors and Affiliations
Corresponding author
Additional information
Responsible Editor: M. J. Parnham.
Rights and permissions
About this article
Cite this article
Srivastava, D., Arora, N. & Singh, B.P. Current immunological approaches for management of allergic rhinitis and bronchial asthma. Inflamm. Res. 58, 523–536 (2009). https://doi.org/10.1007/s00011-009-0033-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00011-009-0033-7