Abstract
Background and objective
Optimisation of hydrocortisone replacement therapy in children is challenging as there is currently no licensed formulation and dose in Europe for children under 6 years of age. In addition, hydrocortisone has non-linear pharmacokinetics caused by saturable plasma protein binding. A paediatric hydrocortisone formulation, Infacort® oral hydrocortisone granules with taste masking, has therefore been developed. The objective of this study was to establish a population pharmacokinetic model based on studies in healthy adult volunteers to predict hydrocortisone exposure in paediatric patients with adrenal insufficiency.
Methods
Cortisol and binding protein concentrations were evaluated in the absence and presence of dexamethasone in healthy volunteers (n = 30). Dexamethasone was used to suppress endogenous cortisol concentrations prior to and after single doses of 0.5, 2, 5 and 10 mg of Infacort® or 20 mg of Infacort®/hydrocortisone tablet/hydrocortisone intravenously. A plasma protein binding model was established using unbound and total cortisol concentrations, and sequentially integrated into the pharmacokinetic model.
Results
Both specific (non-linear) and non-specific (linear) protein binding were included in the cortisol binding model. A two-compartment disposition model with saturable absorption and constant endogenous cortisol baseline (Baseline cort,15.5 nmol/L) described the data accurately. The predicted cortisol exposure for a given dose varied considerably within a small body weight range in individuals weighing <20 kg.
Conclusions
Our semi-mechanistic population pharmacokinetic model for hydrocortisone captures the complex pharmacokinetics of hydrocortisone in a simplified but comprehensive framework. The predicted cortisol exposure indicated the importance of defining an accurate hydrocortisone dose to mimic physiological concentrations for neonates and infants weighing <20 kg.
EudraCT number: 2013-000260-28, 2013-000259-42.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Therapy optimisation of hydrocortisone replacement therapy is challenging due to no licensed paediatric formulation, non-linear pharmacokinetics and lack of a validated pharmacokinetic target. |
We pooled data from two clinical studies in healthy adult participants to establish a semi-mechanistic pharmacokinetic model to describe the non-linear pharmacokinetics for hydrocortisone in a large dose range (0.5–20 mg) of Infacort® (paediatric granules with taste masking). |
The predicted cortisol exposure varied considerable within a small body weight (BW) range, and indicated the need to define an accurate hydrocortisone dose especially for paediatric patients with low BW (<20 kg). |
1 Introduction
Hydrocortisone is equivalent to endogenous cortisol, and is the recommended glucocorticoid for paediatric patients with adrenal insufficiency, which is lethal if untreated [1]. The goal of therapy is to obtain as close to physiological cortisol concentrations as possible [2]. The recommended daily dose for growing children is hydrocortisone 8 mg/m2, divided in three or four doses [1] as hydrocortisone has a short half-life (mean: 1.3–1.8 h [3, 4]). However, there is currently no licensed hydrocortisone formulation for patients less than 6 years in Europe or the USA. These patients are commonly administered low doses (0.5–5 mg) as crushed tablets suspended in water [5, 6]. The accuracy associated with dividing a licensed tablet (e.g. 10 mg in Europe) to generate a low dose is poor and may impact treatment outcomes [6]. Indeed, a large variability in dose was observed in a study on extemporaneously compounded hydrocortisone capsules undertaken in community pharmacies in Germany [7]. Administering a hydrocortisone suspension is also a common option, but has been associated with inadequate disease control due to inhomogeneous distribution of hydrocortisone in the suspension and a short shelf-life [8]. To overcome these limitations and to provide a suitable paediatric hydrocortisone formulation from birth, Infacort® (Diurnal Ltd, Cardiff, UK), oral hydrocortisone granules with taste masking, is currently under development [6].
Optimising hormone replacement is challenging as most hormones have distinct secretory patterns and are frequently bound to circulating binding proteins. Hydrocortisone has complex pharmacokinetics caused by several factors: cortisol is mainly bound with high affinity to corticosteroid-binding globulin (CBG), which can be saturated within the therapeutic range [9]; cortisol is to a lesser extent also transported by albumin and erythrocytes with low affinity but high capacity [10]; and the area under the concentration–time curve (AUC) profile of hydrocortisone is dose-dependent, potentially due to a dose-dependent bioavailability or concentration-dependent clearance (CL) [3, 11]. Despite these known non-linear processes, the pharmacokinetics of hydrocortisone have mostly been described with linear pharmacokinetic models, probably due to the limited dose range studied or the lack of integrated approaches to simultaneously analyse the different dose levels [4, 12, 13]. 11β-Hydroxysteroid dehydrogenase type 2 (11β-HSD2) is responsible for converting cortisol to cortisone in the kidney, which can be converted to cortisol by 11β-hydroxysteroid dehydrogenase type 1 (11β-HSD1) (in liver and adipose tissue). In addition, cortisol can be metabolised in sequential steps by 5α-reductase, 5β-reductase and 3α-hydroxysteroid dehydrogenase to allo-tetrahydrocortisol, tetrahydrocortisol and tetrahydrocortisone, which are all renally excreted. 6β-hydroxylase (cytochrome P450 [CYP] 3A4) metabolises a small fraction of cortisol (~1%) to 6β-hydroxycortisol, which is also renally excreted [14]. Furthermore, the fast absorption of hydrocortisone is slightly delayed by food [12], and hydrocortisone cannot be bioanalytically separated from endogenous cortisol.
The pharmacokinetics of Infacort® have been evaluated in a healthy adult population by non-compartmental analysis (NCA), in which a dose dependency in both AUC and maximum concentration (C max), explained by the plasma protein binding, was suggested [6]. However, NCA assumes linear pharmacokinetics and therefore does not allow for a quantitative description of the known non-linear processes, thus limiting extrapolation to a paediatric population. The objective of the current analysis was to provide a quantitative and mechanistic understanding of the complex pharmacokinetics of hydrocortisone after administration of Infacort® in healthy adult participants using a population approach, and to use the established model to predict hydrocortisone exposure in paediatric patients.
2 Methods
2.1 Study Design
Data from two independent crossover studies (ClinialTrials.gov identifiers: NCT02777268, NCT01960530 [6, 15]), with four and five study periods, respectively, were used for model development. Both studies were approved by the South East Wales Research Ethics committee and performed according to European and international guidelines [16,17,18]. Written informed consent was obtained from all participants. Healthy males between 18 and 60 years not working shifts, with no clinically significant infection or known sensitivity to hydrocortisone and/or dexamethasone were included.
Participants in study 1 received single morning oral doses of 0.5, 2, 5 and 10 mg Infacort® (n = 16 [6]) in a random order with at least 1 week washout between periods. Total plasma cortisol concentrations (C tot) were sampled at pre-dose and 0.5, 1, 1.5, 2.5, 3, 3.5, 4, 4.5, 5, 5.5, 6, 6.5, 7, 7.5, 8, 9, 10, 11 and 12 h post-dose in study 1. Dexamethasone (1 mg) was administered in each study period, according to Fig. 1 (top), to suppress the endogenous cortisol synthesis.
Schematic representation of the hydrocortisone (HC) and dexamethasone (DEX) administration and sampling schedule for the two crossover studies: study 1 (upper panel) and study 2 (lower panel). Study 1 consisted of four sampling periods of 12 h, in which total cortisol concentrations (C tot : light blue arrows) were measured after DEX suppression and administration of single doses of 0.5, 2, 5 and 10 mg of Infacort® with a washout period of at least 1 week between periods. In study 2, C tot, corticosteroid-binding globulin (CBG), i.e. CBG + C tot (dark-blue arrows) and unbound cortisol concentrations (C u), i.e. CBG + C tot + C u (red arrows) were measured first over 24 h in the absence of DEX, followed by 12 h sampling periods (n = 4) with DEX suppression and no HC, 20 mg of Infacort®, 20 mg licensed HC tablet and HC intravenously (iv). The washout period between study periods was at least 1 week. Asterisks randomised study periods
Study 2 included an additional evaluation of the endogenous cortisol synthesis without treatment over 24 h at the beginning of the study, in which C tot and CBG were determined once every hour for 24 h (15:00–15:00; Fig. 1, bottom). Subsequently, the participants (n = 14 [15]) received only dexamethasone (1 mg), dexamethasone and single doses of Infacort® 20 mg or licensed oral hydrocortisone 20 mg tablet (Auden Mckenzie Ltd, Ruislip, UK) in a random order followed by intravenous bolus hydrocortisone administration (hydrocortisone succinate) with a washout period of at least 1 week. In these periods C tot and CBG were sampled pre-dose, and 0.25, 0.5, 0.75, 1, 1.25, 1.5, 2, 2.5, 3, 4, 5, 6, 8, 10 and 12 h post hydrocortisone dose/period start. In addition, unbound concentrations (C u) were obtained for samples at 22:00, 07:00 and 09:00 in absence of dexamethasone and pre-dose and 2 h post-dose after administration of dexamethasone with/without hydrocortisone (Fig. 1).
Participants in both studies received standardised meals after administration of hydrocortisone (08:00 and 13:00) to not interfere with the absorption process. In both studies, body weight (BW), height and age were recorded, and participants with insufficient suppression, as judged by elevated adrenocorticotropic hormone, were excluded from the analysis. Samples for C tot, C u and CBG were immediately frozen and stored at −20 °C or below prior to analysis. C tot was quantified by a cortisol liquid chromatography–tandem mass spectrometry (LC-MS/MS) assay with a lower limit of quantification (LLOQ) of 1.4 nmol/L. Intra-assay variability (coefficient of variation [CV]) was <15% at LLOQ and <10% for 22–552 nmol/L [6]. C u was quantified using temperature-controlled ultrafiltration at 37 ºC followed by a cortisol LC/MS-MS assay (LLOQ = 0.8 nmol/L, intra- and interassay variability <8 and <9.5%, respectively) [15]. The sample volume was not corrected after ultrafiltration as collection of ultrafiltrate was kept to a minimum, i.e. 10–20% of the total plasma volume. Adsorption to the ultrafiltration device was assessed and was found to be negligible. CBG was quantified using ELISA (Biovendor, Brno, Czech Republic; LLOQ = 3.13 ng/mL, intra- and inter-assay variability of <3 and <8%, respectively) [19].
2.2 Population Pharmacokinetic Analysis
The semi-mechanistic population pharmacokinetic model was developed in three sequential steps: (i) binding model, (ii) CBG model, and (iii) semi-mechanistic pharmacokinetic model, using NONMEM® 7.3 [20] and Perl speaks NONMEM (PsN 4.4.0) [21]. For pharmacokinetic parameter estimation the first-order conditional estimation with interaction was used for the binding and CBG model, whereas stochastic estimation algorithms (Stochastic Approximation Expectation Maximisation [SAEM] method with interaction followed by Monte-Carlo Importance Sampling Expectation Maximisation method) were used for the semi-mechanistic model. Only 4% of the post-dose C u in the hydrocortisone periods were less than the LLOQ and were therefore disregarded. No CBG or C tot concentrations were less than the LLOQ.
2.2.1 Plasma Protein Binding and Corticosteroid-Binding Globulin (CBG) Model
The plasma protein binding model of cortisol was established using log-transformed C tot observations for which the corresponding C u was available. Linear, non-linear and combined linear and non-linear binding models were assessed. The combined model (exemplified in Eq. 1), derived the bound concentration (C b) by estimating the equilibrium dissociation constant (K d), the linear non-specific binding parameter (NS) and the maximum binding capacity (B max). Using CBG as a covariate for B max was evaluated. Constant CBG concentrations were observed after dexamethasone administration (Fig. S1, Electronic Supplementary Material [ESM] Online Resource 1); thus, a CBG model with a constant CBG baseline (BaselineCBG) and interindividual variability (IIV) was estimated using untransformed data from periods with dexamethasone.
2.2.2 Semi-Mechanistic Pharmacokinetic Model
The pharmacokinetic model was developed on log-transformed C tot after administration of Infacort® or intravenous hydrocortisone from both studies. Measured C tot before and after treatment were similar, hence a constant cortisol baseline (Baselinecort) was estimated [22], and included in the model according to Eq. 2, in which C tot was derived from the amount in central compartment (A c), the central volume of distribution (V c) and the Baselinecort. Different disposition models (one, two and three compartments) were evaluated and allometric scaling with exponents of 0.75 and 1 was implemented for CL and distribution parameters, respectively. Absorption was assessed as first-, zero-, sequential zero- and first-order absorption and saturable absorption. The latter is exemplified in Eq. 3, for which the maximum absorption rate (V max) and amount in the depot compartment (A depot) resulting in half V max (K m) were estimated. The binding model was included in the pharmacokinetic model by fixing the binding parameters.
IIV was implemented as an exponential model, thereby assuming a log-normal distribution of structural pharmacokinetic parameters. IIV parameters not being estimated were fixed to a CV of 15%, to allow for the SAEM algorithm to converge efficiently. Residual variability (RUV) was modelled as an additive error on the log scale, except for the CBG model, for which a proportional error model on linear scale was used. Assessment of available covariates was pursued if relations were observed between covariates and parameter estimates.
2.2.3 Model Evaluation
Model performance was assessed by goodness-of-fit plots, parameter plausibility and precision, model stability and objective function value (OFV). Nested models were compared using the likelihood ratio test, and a reduction in the OFV of 3.84 points was considered statistically significant (corresponding to a p value of 0.05 for large samples). The Akaike Information Criterion (AIC) was used for non-nested models. Precision of parameter estimates was assessed using parameteric bootstraps in PsN (n = 1000) [21]. Predictive performance was evaluated by visual predictive checks (VPCs) in which the percentiles (5th, 50th and 95th) of observed and simulated data (n = 1000) were compared (R package: VPC [23]). In addition, an external model evaluation (VPC, n = 1000) for the developed binding model was performed using plasma protein binding data from Lentjes and Romijn [10].
2.3 Simulations
The different concentrations of cortisol (unbound, specific binding, non-specific binding) were simulated in R 3.3.0 [24] using the developed binding model and the typical CBG baseline over a range of C tot from 23.7 (corresponding to C u of 0.5 nmol/L) to 492 nmol/L (the 75th percentile of observed C max from Knutsson et al. [25]; see paragraph below).
To explore the dose–exposure relationship of Infacort® (0.5–20 mg), C max and AUC in individuals with different BW (5–100 kg) and the typical CBG concentration were simulated without variability using the semi-mechanistic pharmacokinetic model in NONMEM®. The simulated C max and AUC were compared to C max and AUC values extracted from Knutsson et al. [25] from healthy paediatric volunteers (2.2–18.5 years): the C max comparison range, consisting of the 25th–75th percentiles of the C max for the morning peak in children was extracted digitally using WebPlotDigitizer [26]. The AUC comparison range (95% confidence interval) was derived as one-third of the 24 h AUC for children, assuming a recommended three times daily dosing regimen with equal doses.
3 Results
3.1 Data Analysis
The median BW and height were similar between study 1 and 2, whereas the median age was slightly higher in study 1 (43.5 years) than in study 2 (28.5 years), but still in the same range. The distributions of all demographic factors were similar between the two studies; hence, no differences in pharmacokinetic parameters based on demographic factors were expected (Table 1). Due to insufficient cortisol suppression, one and three study periods for two participants in study 1 were excluded from the analysis (4.3% of all periods).
The concentration–time profiles showed a bi-phasic decline of hydrocortisone after intravenous and oral administration with all profiles approaching and stabilising at approximately 10–20 nmol/L (Fig. 2a). The highest Infacort® dose had a more pronounced mono-phasic decline than the lower doses, indicating non-linear distribution, elimination and/or absorption processes. In addition, the dose-normalised concentration–time profiles (Fig. 2b) were not superimposable, the lower doses had higher dose-normalised C max values, and time to C max (t max) was slightly delayed for higher doses.
Absolute total cortisol concentration–time profiles (a) and dose-normalised cortisol concentration–time profiles (b) after oral administration of Infacort® 0.5 mg (n = 15), 2 mg (n = 16), 5 mg (n = 15), 10 mg (n = 14) and 20 mg (n = 14) and intravenous administration of hydrocortisone succinate (n = 14)
3.2 Population Pharmacokinetic Analysis
3.2.1 Plasma Protein Binding and CBG Model
The binding model was established using 61 C u values and the respective C tot from 11 participants in study 2. A linear relation was observed between total versus unbound cortisol concentration in their lower and a non-linear relation in their higher concentration range (Fig. S2, ESM Online Resource 2). A combined linear and non-linear binding model described the data best, judged by reduction in OFV and performance of the VPC (Fig. 3a). Initially, B max and its associated IIV were estimated (B max: 495 nmol/L, ωB max: 17% CV). To provide a more mechanistic interpretation, B max was derived based on the measured CBG and a parameter reflecting the number of CBG binding sites (N CBG, Eq. 4). This approach explained more than half of the IIV, and considerably reduced OFV (∆OFV: –16.2). The estimated N CBG was very close to 1 and hence fixed (Table 2). The derived B max [median (range)] was very plausible [414 (312–632) nmol/L]. Moreover, the developed binding model adequately predicted the published binding data reported in Lentjes and Romijn [10], which was not used for model building (Fig. 3b). The 895 CBG concentrations in study 2 were accurately described by a constant baseline of 22.4 µg/mL (Fig. S3, ESM Online Resource 3), which was used to impute the missing CBG concentrations for study 1. The associated IIV was low (12.9% CV).
Visual predictive check (n = 1000) for the binding model including both a non-linear and linear component, and a substituted maximum binging capacity (B max) (a). External model evaluation using observed total and unbound cortisol concentrations from Lentjes and Romijn [10] (b). Lines 5th, 50th and 95th percentile of observed (red) and simulated (blue) data; corresponding areas 95% confidence intervals around the simulated percentiles; red circles observations
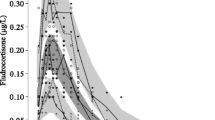
The binding model was used to simulate the unbound and bound cortisol concentrations (with specific or non-specific binding) for concentrations including the target C max in children from Knutsson et al. [25], and the respective fractions were derived. The specific binding (i.e. binding to CBG, dark-blue area) was higher for lower (89%) than for higher (70%) concentrations (Fig. 4). The fraction of cortisol bound with non-specific binding (i.e. albumin and erythrocytes, blue area) increased from 8.7% at low concentrations to 24% at higher concentrations. In the evaluated C tot range (23.7–492 nmol/L), the fraction of unbound cortisol (light-blue area) increased considerably from 2.1 to 6.4%, translating to C u ranging from 0.5 to 31.5 nmol/L.
Simulated cortisol fractions (%) as unbound, with non-specific binding (linear) or specific binding (non-linear) based on the final binding model. The total cortisol concentration range corresponds to the predicted concentration range if considering the maximum concentrations (75th percentile) in children observed from Knutsson et al. [25]
3.2.2 The Semi-Mechanistic Pharmacokinetic Model
The semi-mechanistic pharmacokinetic model was developed using 1705 C tot values from 30 patients from both studies. A two-compartmental model estimating CL, V c, intercompartmental CL (Q) and peripheral volume of distribution (V p), described the hydrocortisone profiles better than a one-compartmental model (∆OFV: −96.9). Addition of a third compartment did not change OFV. As expected, use of linear pharmacokinetics to describe the hydrocortisone pharmacokinetics resulted in large discrepancies between observed and predicted concentrations. Inclusion of a saturable absorption improved the description of the absorption phase across doses, allowing also for a slightly delayed t max for higher doses. Subsequently, the binding model was incorporated to account for the non-linear disposition and elimination (Eqs. 5–7). Equation 5 derived the unbound amount (A u) in the central compartment from A c, assuming parallel linear and non-linear binding in rapid equilibrium. The non-linear binding parameters K and A max corresponded to K d and B max, but expressed in amounts instead of concentrations. Inclusion of the binding model improved model performance, especially for higher doses. The semi-mechanistic model was finally described by Eqs. 2–7, in which only A u can be distributed or eliminated, similar to a previous publication [27]. Alternative approaches to consider the non-linear pharmacokinetics included, for example, (i) implementing plasma protein binding using the Wagner equation [28]; and (ii) estimating a dose-dependent bioavailability. These approaches resulted in unstable models with less precise estimates and/or higher OFV than the selected model approach and were, thus, not supported by the data and not further considered.
IIV was supported for CL, V c and Baselinecort, which were moderate (25.6–30.8% CV). A positive correlation between CL and V c was identified, and RUV was minor (14.3% CV). Allometric scaling was applied for CL and volume parameters, but addition of further covariates was not supported by the data. The final parameter estimates and a schematic representation are available in Table 2 and Fig. 5, respectively. Although a slight underprediction was observed for the initial phase in the VPC for the highest Infacort® dose, the developed model described the overall central tendency and variability very accurately in all doses and via different administration routes (Fig. 6).
Schematic representation of the final semi-mechanistic hydrocortisone model considering the endogenous cortisol baseline (Baselinecort) after suppression with dexamethasone, and plasma protein binding. A b amount bound, A b :Alb amount bound to albumin, A b :CBG amount bound to corticosteroid-binding globulin, A depot amount in depot compartment, A p amount in peripheral compartment, A u unbound amount, B max maximum binding capacity, CL clearance, K d equilibrium dissociation constant, K m amount in depot compartment resulting in half of V max, NS linear non-specific binding parameter, Q intercompartmental clearance, V c central volume of distribution, V max maximum absorption rate, V p peripheral volume of distribution
3.3 Predicting Cortisol Exposure in Paediatric Patients
Simulations were performed to illustrate the impact of the non-linearities in the semi-mechanistic model on cortisol exposure, and to evaluate the predicted exposure after the administration of different doses to virtual patients with different BW (5–100 kg). As expected, dose-normalised C max and AUC was higher and varied more for low than for high doses (Fig. 7a, b). Both C max and AUC decreased with increasing BW in the virtual population (Fig. 7c, d). The exposure varied considerably for a given BW for patients with low BW (<20 kg), and stabilised at adult BW (>55 kg). As paediatric comparison ranges, AUC and C max from physiological cortisol concentrations in healthy paediatric volunteers were extracted from Knutsson et al. [25]. Large discrepancies in the dose selected for each BW range was observed for the AUC and C max comparison ranges, and C max overall suggested lower doses than the AUC range. The largest difference in appropriate dose selection was observed for lower BW of, for example, 20 kg, for which a three- to fourfold difference in doses was observed (C max: 1 mg; AUC: 3–4 mg).
Simulated maximum concentration (C max) (a, c) and area under the total cortisol concentration–time curve (AUC) (b, d) for administration of Infacort® 0.5–20 mg to a virtual population with body weights ranging from 5 to 100 kg. a, b Display the dose-normalised C max and AUC versus dose for each body weight. c, d Display the C max and AUC versus body weight, for which solid and dashed lines correspond to the doses included and not included in the study protocol, respectively. The blue area for C max in c corresponds the 25th–75th percentiles of the peak cortisol concentration in healthy paediatric volunteers in absence of dexamethasone from Knutsson et al. [25]. The blue area for AUC in d corresponds to a third of the observed AUC from time zero to 24 h (AUC24) in healthy paediatric volunteers in absence of dexamethasone from Knutsson et al. [25]
4 Discussion
We developed a population pharmacokinetic model to describe the complex pharmacokinetics of hydrocortisone with a semi-mechanistic approach. Model complexity could be supported, since oral data from a large dose range (0.5–20 mg), with additional information after intravenous administration (20 mg), were available from two clinical trials in adults. The semi-mechanistic model formed the basis for extrapolation to paediatric patients, and demonstrated the need to optimise dosing especially in paediatric patients <20 kg.
Clinical trials performed in healthy volunteers need to demonstrate that they reflect the situation in the target population. In the current study, this would mean that the healthy adults should reflect the low/no endogenous cortisol synthesis and sequentially diminished negative feedback of the hypothalamus–pituitary–adrenal (HPA) axis observed in patients with adrenal insufficiency. Participants in both studies received dexamethasone prior to hydrocortisone treatment to suppress endogenous cortisol synthesis (to mimic the disease) and improve quantification of the exogenous hydrocortisone. After administration of Infacort®, cortisol concentrations in all dose groups decreased relatively fast from C max until approaching concentrations similar to pre-dose concentrations (Fig. 2). A constant baseline was therefore estimated (15.5 nmol/L) to consider the endogenous cortisol. This approach allowed for appropriate parameter estimation and thereby supports the potential extrapolation to patients. Extrapolating this constant Baselinecort of 15.5 nmol/L to the paediatric patients is a strong assumption. Undetectable morning and evening baseline cortisol concentrations (LLOQ: 28 nmol/L) were, however, reported in paediatric patients on treatment [29]. This indicates little endogenous synthesis of cortisol in this patient population, and supports that this baseline value could be appropriate. Further studies in paediatric patients with adrenal insufficiency are necessary to elucidate whether a constant Baselinecort can also be applied to patient data.
Previous pharmacokinetic analyses of hydrocortisone used one- or two-compartmental disposition models, depending on administration route and study design [4, 13]. Our data were most accurately described by a two-compartmental model, although a trend of a mono-phasic decline was observed for higher doses, potentially due to the slight time delay in absorption masking the first disposition phase. The absorption process was successfully described by saturable absorption model (Michaelis–Menten kinetics). The K m was 2100 nmol, indicating a saturated absorption for doses >5 mg (5 mg: 5090 nmol in the depot compartment). The non-linear absorption process could be due to poor solubility at higher doses, which has previously been described in experiments in vitro [30].The lowest doses were below K m, for which a first-order absorption rate constant (V max /K m) of 4.53 h−1 can be assumed, indicating a rapid absorption with absorption half-life (t ½,absorption) = ~10 min.
In addition to C tot, multiple C u measurements were available from 11 participants. This allowed for establishing a binding model that was integrated into the pharmacokinetic model. Both non-linear (specific) and linear (non-specific) processes were identified (Fig. S2, ESM Online Resource 2), plausibly corresponding to binding to CBG (high affinity, limited capacity) and albumin/erythrocytes (low affinity, high capacity), respectively. To provide a more physiological interpretation, B max was substituted by the measured CBG concentration and a parameter (N CBG) representing the number of binding sites of CBG to cortisol. Consequently, >50% of the IIV of B max was explained by the individual CBG concentration. The IIV of N CBG can therefore rather be regarded as RUV for the CBG measurements, with 7% CV potentially corresponding to imprecision of the bioanalytical assay. Fixing N CBG to 1 (estimate = 1.09), i.e. one binding site for cortisol per CBG molecule, was in line with previous findings [31]. Furthermore, the derived B max using CBG concentrations was well in agreement with Toothaker et al. [3], suggesting a saturable binding at C tot >550 nmol/L. The K d (11.8 nmol/L) and NS (3.12) were in similar ranges as previous estimates (K d: 33 nmol/L [32], NS: 1.75 [33]). Additionally, an external model evaluation was performed to increase model reliability. The binding model adequately predicted the observed data from Lentjes and Romijn [10], with C tot ranging between 300 and 850 nmol/L. A slight overprediction was, however, observed, potentially due to the use of another assay in Lentjes and Romijn [10]. Furthermore, the impact of the specific and non-specific binding processes of cortisol were simulated using C tot in a 20-fold range (23.7–492 nmol/L, Fig. 4), illustrating the importance of the specific and non-specific binding for lower and higher concentrations, respectively. A three-fold increase was observed in fraction unbound, which together with C tot translated to a large range (~60-fold) in C u (0.5–31.5 nmol/L).
B max was derived using CBG, which was not quantified in study 1. A CBG model was therefore established to enable imputation of CBG in study 1. The CBG measured in our study was in the lower end of reported reference ranges, which are rather large, indicating a large variability between individuals and/or high variability in analytical assays, e.g. reference range given as [mean (standard deviation)]: 31.7 (12.6) mg/L [19]. Previous studies have indicated that CBG displays a circadian rhythm [15, 34], whereas other studies have contradicted this [35]. CBG concentrations were approximately constant from 07:00 to 19:00 (Fig. S1, ESM Online Resource 1), thus a constant CBG baseline with associated variability was sufficient to describe the CBG concentrations during this time span. It remains to be elucidated whether the circadian rhythm of CBG needs to be considered if applying the model at timepoints outside the studied daytime interval.
Few previous pharmacokinetic models have considered the plasma protein binding of cortisol. We acknowledge that changes in plasma protein binding are rarely clinically relevant after oral administration and may have little impact of unbound exposure. The plasma protein binding may, however, have an impact on the pharmacokinetic parameter estimates and sequentially the description of the total concentrations [36]. In our model, the inclusion of the binding model significantly improved model performance, especially for higher doses (10 and 20 mg), which also had most C tot concentrations above B max. When including the binding model, CL, Q, V p and F were stated with respect to C u values, preventing a direct comparison with previous parameters. The previous NCA indicated a dose-dependency in AUC [6], which could be explained either by decreasing F or increasing CL with higher doses. The latter scenario is compatible with our semi-mechanistic model, in which the fraction unbound increases with increasing doses, resulting in an increased CL after saturation of CBG.
In summary, we applied a non-linear mixed-effects modelling approach to evaluate the pharmacokinetics after rich sampling in healthy adult participants. Rich data allowed for the development of a semi-mechanistic model that incorporated known aspects of hydrocortisone pharmacokinetics, such as its saturable binding to plasma proteins. Each of the features implemented was supported by an improvement in the model predictions, considerable reduction in the OFV/AIC and acceptable precision of parameters. The semi-mechanistic model was developed on a wide range of doses, including doses used in the paediatric population, and mechanistic understanding, which supports its potential use in paediatrics and for various age groups.
One powerful application of the validated population model is to explore new scenarios and guide dose selection. The aim of the current model presented was to extrapolate knowledge to a paediatric population and evaluate the resulting exposure. We explored how C max and AUC vary with different BW (including BW expected in a paediatric population). There is currently no validated pharmacokinetic target for the hydrocortisone therapy in this population, but one plausible option would be to mimic the physiological cortisol concentration. One important aspect to be monitored is the morning cortisol concentrations, which is why the average C max and AUC of cortisol in healthy paediatric volunteers were derived from Knutsson et al. [25] and used as reference. By using deterministic simulations, we visualised how the C max and AUC differ with different BW and compared them with proposed pharmacokinetic targets derived from Knutsson et al. [25]. The model predicted a much larger variation in C max and AUC within a small BW range in individuals <20 kg. This implies that defining an accurate dose to replicate physiological concentrations becomes very important for children <20 kg. These simulations represent an extrapolation of the semi-mechanistic model to a special population with different BW range. It should be noted that the simulations did not consider age-relevant factors, such as maturation of CBG for neonates [37] or the slightly lower and higher 5α-reductase activity in neonates and infants [38], respectively. Clinical interpretation of the results should therefore be made with caution for patients below 2 years of age (BW ≤15 kg [39]) before these results have been verified with prospective clinical trials.
As next step, further analyses should assess the capability of the model to extrapolate pharmacokinetic knowledge in particular to paediatric populations, and whether additional model refinements, such as inclusion of maturation processes, are needed. The developed semi-mechanistic model represents a first step towards a better understanding of hydrocortisone pharmacokinetics, extrapolation to paediatric patients, and can potentially be used to evaluate Infacort® therapy in this population.
5 Conclusions
By using rich data from adult healthy participants, we established a semi-mechanistic population pharmacokinetic model for hydrocortisone accounting for (i) constant Baselinecort after dexamethasone suppression; (ii) non-linear plasma protein binding to CBG and linear binding (e.g. to albumin/erythrocytes); and (iii) a saturable absorption process. In addition, we assessed the predicted exposure in a wide range of doses and for a wide range of BW to illustrate the usefulness of the model using two pharmacokinetic comparison targets (C max and AUC). The developed model captures the complex pharmacokinetics of hydrocortisone in a comprehensive framework and can potentially be used to extrapolate information to paediatric populations. Our simulations imply the need to define an exact dose to replicate physiological cortisol concentrations for paediatric individuals <20 kg.
References
Bornstein SR, Allolio B, Arlt W, Barthel A, Don-Wauchope A, Hammer GD, et al. Diagnosis and treatment of primary adrenal insufficiency: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2016;101:364–89.
Porter J, Blair J, Ross RJ. Is physiological glucocorticoid replacement important in children? Arch Dis Child. 2017;102:199–205.
Toothaker RD, Sundaresan GM, Hunt JP, Goehl TJ, Rotenberg KS, Prasad VK, et al. Oral hydrocortisone pharmacokinetics: a comparison of fluorescence and ultraviolet high-pressure liquid. J Pharm Sci. 1982;71:573–6.
Derendorf H, Mollmann H, Barth J, Mollmann C, Tunn S, Krieg M. Pharmacokinetics and oral bioavailability of hydrocortisone. J Clin Pharm. 1991;31:473–6.
Speiser PW, Azziz R, Baskin LS, Ghizzoni L, Hensle TW, Merke DP, et al. Congenital adrenal hyperplasia due to steroid 21-hydroxylase deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2010;95:4133–60.
Whitaker MJ, Spielmann S, Digweed D, Huatan H, Eckland D, Johnson TN, et al. Development and testing in healthy adults of oral hydrocortisone granules with taste masking for the treatment of neonates and infants with adrenal insufficiency. J Clin Endocrinol Metab. 2015;100:1681–8.
Kauzor D, Spielmann S, Brosig H, Ross R, Blankenstein O, Kloft C. Medication safety study investigating hydrocortisone individually and extemporaneously compounded capsules for paediatric use in CAH [abstract no. P825]. 16th European Congress of Endocrinology, 2014. http://www.endocrine-abstracts.org/ea/0035/ea0035P825.htm. Accessed 25 Jun 2017.
Merke DP, Cho D, Calis KA, Keil MF, Chrousos GP. Hydrocortisone suspension and hydrocortisone tablets are not bioequivalent in the treatment of children with congenital adrenal hyperplasia. J Clin Endocrinol Metab. 2001;86:441–5.
Toothaker RD, Welling PG. Effect of dose size on the pharmacokinetics of intravenous hydrocortisone during endogenous hydrocortisone suppression. J Pharmacokinet Biopharm. 1982;10:147–56.
Lentjes EGWM. Romijn FHTPM. Temperature-dependent cortisol distribution among the blood compartments in man. J Clin Endocrinol Metab. 1999;84:682–7.
Toothaker RD, Craig WA, Welling PG. Effect of dose size on the pharmacokinetics of oral hydrocortisone suspension. J Pharm Sci. 1982;71:1182–5.
Mah PM, Jenkins RC, Rostami-Hodjegan A, Newell-Price J, Doane A, Ibbotson V, et al. Weight-related dosing, timing and monitoring hydrocortisone replacement therapy in patients with adrenal insufficiency. Clin Endocrinol. 2004;61:367–75.
Simon N, Castinetti F, Ouliac F, Lesavre N, Brue T, Oliver C. Pharmacokinetic evidence for suboptimal treatment of adrenal insufficiency with currently available hydrocortisone tablets. Clin Pharmacokinet. 2010;49:455–63.
Hoshiro M, Ohno Y, Masaki H, Iwase H, Aoki N. Comprehensive study of urinary cortisol metabolites in hyperthyroid and hypothyroid patients. Clin Endocrinol. 2006;64:37–45.
Debono M, Harrison RF, Whitaker MJ, Eckland D, Arlt W, Keevil BG, et al. Salivary cortisone reflects cortisol exposure under physiological conditions and after hydrocortisone. J Clin Endocrinol Metab. 2016;101:1469–77.
World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–4.
Association of the British Pharmaceutical Industry. Guidelines for phase 1 clinical trials (2012 edition). http://www.abpi.org.uk/our-work/library/guidelines/Pages/phase-1-trials-2012.aspx. Accessed 18 Nov 2016.
International Council for Harmonisation of Technical Requirements for Human Use. Guideline for good clinical practice E6(R1). http://www.ich.org/products/guidelines/efficacy/efficacy-single/article/good-clinical-practice.html. Accessed 18 Nov 2016.
Lewis JG, Lewis MG, Elder PA. An enzyme-linked immunosorbent assay for corticosteroid-binding globulin using monoclonal and polyclonal antibodies: decline in CBG following synthetic ACTH. Clin Chim Acta. 2003;328:121–8.
Beal S, Sheiner LB, Boeckmann A, Bauer RJ. NONMEM user’s guides (1989–2009). Ellicott City: Icon Development Solutions; 2009.
Lindbom L, Pihlgren P, Jonsson EN, Jonsson N. PsN-Toolkit–a collection of computer intensive statistical methods for non-linear mixed effect modeling using NONMEM. Comput Methods Programs Biomed. 2005;79:241–57.
Dansirikul C, Silber HE, Karlsson MO. Approaches to handling pharmacodynamic baseline responses. J Pharmacokinet Pharmacodyn. 2008;35:269–83.
Keizer R, Pastoor D, Savic R. New open source R libraries for simulation and visualization: “PKPDsim” and “vpc” 2015. http://www.page-meeting.eu/pdf_assets/1215-Page_Keizer_2015_pkpdsim_vpc.pdf. Accessed 5 Oct 2016.
R Development Core Team. R: a language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2016. ISBN 3-900051-07-0. http://www.R-project.org. Accessed 15 June 2016.
Knutsson U, Dahlgren J, Marcus C, Rosberg S, Brönnegård M, Stierna P, et al. Circadian cortisol rhythms in healthy boys and girls: relationship with age, growth, body composition, and pubertal development. J Clin Endocrinol Metab. 1997;82:536–40.
Rohatgi A. WebPlotDigitizer. http://arohatgi.info/WebPlotDigitizer. Accessed 5 Oct 2016.
Wright DH, Stone JA, Crumley TM, Wenning L, Zheng W, Yan K, et al. Pharmacokinetic-pharmacodynamic studies of the 11β-hydroxysteroid dehydrogenase type 1 inhibitor MK-0916 in healthy subjects. Br J Clin Pharmacol. 2013;76:917–31.
Picard-Hagen N, Gayrard V, Alvinerie M, Smeyers H, Ricou R, Bousquet-Melou A, et al. A nonlabeled method to evaluate cortisol production rate by modeling plasma CBG-free cortisol disposition. Am J Physiol Endocrinol Metab. 2001;281:E946–56.
Charmandari E, Johnston A, Brook CG, Hindmarsh PC. Bioavailability of oral hydrocortisone in patients with congenital adrenal hyperplasia due to 21-hydroxylase deficiency. J Endocrinol. 2001;169:65–70.
Lennernäs H, Skrtic S, Johannsson G. Replacement therapy of oral hydrocortisone in adrenal insufficiency: the influence of gastrointestinal factors. Expert Opin Drug Metab Toxicol. 2008;4:749–58.
Westphal U. Steroid-protein interactions. In: Gross F, Labhart A, Mann T, Samuels L (eds.) 1st edn. New York: Springer; 1971.
Westphal U. Steroid-protein interactions XIII. Concentrations and binding affinities of corticosteroid-binding globulins in sera of man, monkey, rat, rabbit and guinea pig. Arch Biochem Biophys. 1967;118:556–67.
Coolens J-L, Baelen HVAN, Heyns W. Clinical use of unbound plasma cortisol as calculated from total cortisol and corticosteroid-binding globulin. J Steroid Biochem. 1987;26:197–202.
Lewis JG, Möpert B, Shand BI, Doogue MP, Soule SG, Frampton CM, et al. Plasma variation of corticosteroid-binding globulin and sex hormone-binding globulin. Horm Metab Res. 2006;38:241–5.
Chung TT, Gunganah K, Monson JP, Drake WM. Circadian variation in serum cortisol during hydrocortisone replacement is not attributable to changes in cortisol-binding globulin concentrations. Clin Endocrinol. 2016;84:496–500.
Benet LZ, Hoener B. Changes in plasma protein binding have little clinical relevance. Clin Pharmacol Ther. 2002;71:115–21.
Hadjian AJ, Chedin M, Cochet C, Chambaz EM. Cortisol binding to proteins in plasma in the human neonate and infant. Pediatr Res. 1975;9:40–5.
Rogers SL, Hughes BA, Jones CA, Freedman L, Smart K, Taylor N, et al. Diminished 11β-hydroxysteroid dehydrogenase type 2 activity is associated with decreased weight and weight gain across the first year of life. J Clin Endocrinol Metab. 2014;99:E821–31.
World Health Organisation. WHO child growth standards. 2006. http://www.who.int/childgrowth/standards/Technical_report.pdf. Accessed 19 Apr 2017.
Acknowledgements
The authors would like to thank the high-performance computing service of ZEDAT, Freie Universitaet Berlin, for computing time. In addition, the authors would like to thank Trevor Johnson and Dena Digweed for valuable support. Parts of the results were presented as a poster at the 2016 Population Approach Group Europe (PAGE) meeting.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The work was carried out under a Cooperation Agreement between Freie Universitaet and Diurnal funded by the European Commission FP7 Grant (No. 281654 TAIN).
Conflict of interest
Johanna Melin, Zinnia P. Parra Guillen and Niklas Hartung have no conflicts of interest. Richard Ross is a director of Diurnal Ltd and has stock options. Martin Whitaker is an employee and director of Diurnal Ltd and has stock options. Charlotte Kloft reports a research grant to Freie Universitaet Berlin from Diurnal funded by the European Commission FP7 Grant (No. 281654 TAIN) and grants from the Innovative Medicines Initiative-Joint Undertaking (‘DDMoRe’). Charlotte Kloft and Wilhelm Huisinga report grants from an industry consortium (AbbVie Deutschland GmbH & Co. KG, Boehringer Ingelheim Pharma GmbH & Co. KG, Grünenthal GmbH, F. Hoffmann-La Roche Ltd, Merck KGaA and SANOFI).
Ethical approval
Data from two studies (Registered EudraCT numbers: 2013-000260-28 and 2013-000259-42) were used for this analysis. Both studies were approved by the South East Wales Research Ethics committee and performed according to the 1964 Helsinki Declaration and International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use (ICH) guidelines.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Melin, J., Parra-Guillen, Z.P., Hartung, N. et al. Predicting Cortisol Exposure from Paediatric Hydrocortisone Formulation Using a Semi-Mechanistic Pharmacokinetic Model Established in Healthy Adults. Clin Pharmacokinet 57, 515–527 (2018). https://doi.org/10.1007/s40262-017-0575-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-017-0575-8