Abstract
Background
Our purpose was to assess the performance of ESR iGuide for assisting the selection of the most appropriate imaging tests based on clinical signs and symptoms in patients with hepatocellular carcinoma (HCC) or cholangiocarcinoma (CC).
Methods
We retrospectively reviewed the medical records of 113 patients with a final diagnosis of HCC or CC. Data from a cohort of 40 patients with a reported clinical history suggestive for either disease, who had undergone at least their first imaging test related to their condition at the same Institution, were entered into ESR iGuide. The appropriateness level of the diagnostic tests suggested by ESR iGuide was compared with that of the tests actually performed.
Results
All patients underwent several imaging examinations, ranging from a minimum of 1 to a maximum of 4, for a total of 98 diagnostic procedures. Of these, 79.6% (78/98) were considered “usually appropriate” by ESR iGuide, 11.2% (11/98) were designated as “may be appropriate”, and 9.2% (9/98) were not even suggested. Given a total estimated cost of €14,016 for the 98 examinations performed within the regional (BLINDED) healthcare system, the usage of ESR iGuide would have allowed saving €3033 (21.6%) due to inappropriate testing.
Conclusions
In patients with HCC or CC, ESR iGuide can be effective in guiding the selection of the appropriate imaging examinations and cutting costs due to inappropriate testing.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
In the last decade, the use of medical imaging, and especially of computed tomography (CT) and magnetic resonance imaging (MRI), has increased significantly and continues to grow as a fundamental part of the diagnostic process. Although the benefits gained from the ongoing improvement of imaging techniques are undeniable, it remains unclear whether all the required tests may be justified for medical reasons or whether diagnostic imaging is being overused. Inappropriate imaging requests lead to several issues including longer waiting lists, inflated healthcare costs, and potentially worse patient outcome due to delayed diagnosis and/or improper treatment. In this context, the use of evidence-based medicine and the application of referral guidelines have been suggested as possible remedies [1, 2].
Clinical decision support (CDS) systems refer to “any electronic system designed to directly aid clinical decision-making, in which characteristics of individual patients are used to generate patient-specific assessments or recommendations that are then presented to clinicians for consideration”, and their implementation in clinical practice on a regular basis could improve adherence to guidelines and possibly increase the overall efficiency of the diagnostic workflow [3]. To this purpose, the European Society of Radiology (ESR) and the National Decision Support Company (NDSC) have developed the ESR iGuide CDS, i.e. the CDS system for European imaging referral guidelines, which derive from an adaptation of the American College of Radiologists (ACR) appropriateness criteria to European standards of practice [4,5,6,7]. ESR iGuide is an online web portal that requires patient data as user input and accordingly displays which imaging tests are suggested together with their appropriateness level, estimated cost, and expected radiation exposure. Two consultation options are available: indication-driven (starting with clinical scenarios) or procedure-driven (starting with the diagnostic test that one may want to request) [5].
Some studies have evaluated the effectiveness of CDS systems in improving the diagnostic management of patients with various clinical conditions, showing that compared to CDS-unassisted practice, their usage can result in an increased rate of appropriate examinations and a decreased rate of inappropriate examinations [8,9,10]. However, to the best of our knowledge, there are no published works so far in the literature that have tested the performance of ESR iGuide in assisting diagnostic decision-making and potentially optimising healthcare resources. This would be especially important in an attempt to harmonise and improve disease management with a heavy individual and social impact that require a complex diagnostic and therapeutic approach, such as liver cancer [11, 12].
Our aim was to evaluate how ESR iGuide could impact the diagnostic pathway of patients with hepatocellular carcinoma (HCC) and cholangiocarcinoma (CC).
Methods
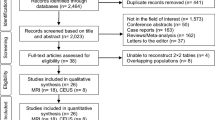
We retrospectively reviewed the medical records of 113 patients with a final diagnosis of HCC or CC (either radiologically or pathologically proven), who had been referred to the Oncology Department of BLINDED from January 2013 to May 2017 at the beginning of their diagnostic pathway. Among them, we analysed a cohort of 40 patients (35.4%) with a reported clinical history of signs, symptoms and laboratory values suggestive for HCC or CC, who had undergone at least their first diagnostic imaging examination specifically related to their disease condition at the same Institution (Table 1).
For each patient, all relevant data (including patient age, gender, and clinical indication) were entered into the ESR iGuide tool without selecting any imaging test (indication-driven mode). As output, the software returns an ordinal value (ranging from 1 to 9) corresponding to the appropriateness score of all potential imaging tests, with scores from 1 to 3 indicating a “usually not appropriate” test, from 4 to 6 a test that “may be appropriate”, and from 7 to 9 a “usually appropriate” test, respectively (Figs. 1 and 2).
Screenshots of the ESR iGuide web interface for the diagnostic workup of a 71-year-old man with jaundice. a The system requires patient’s sex, age, and clinical data as an input and generates a list of selectable potential indications to diagnostic testing. A specific diagnostic modality (“service”) can be also entered as an option. b Upon selection of “jaundice” as clinical indication, a list of candidate diagnostic tests is displayed, each with its appropriateness ranking, estimated cost, and expected radiation exposure (relative radiation level, RRL). By clicking on “Display Evidence…”, the user is directed to a portable document format (PDF) file containing the ACR appropriateness criteria for the diagnostic management of jaundice and a summary of literature review (Supplementary material). c By clicking on the “Select this service” tab (related to “US, abdomen” in this example), a brief report with the appropriateness score of the selected test is generated that can be emailed or converted into a PDF file
ESR iGuide screenshot showing potential examinations for the diagnostic workup of a 25-year-old woman with hepatitis. Diagnostic procedures that are “usually appropriate” are marked by green bars of proportional length to each appropriateness score, whereas those which “may be appropriate” or are “usually not appropriate” are highlighted in yellow or red, respectively
For each imaging modality, the frequency distribution of diagnostic tests suggested by ESR iGuide with an appropriateness score equal to or higher than 7 was compared with that of the tests actually performed using the two-tailed McNemar test. Statistical analysis was carried out using software (GraphPad Prism v. 5, www.graphpad.com). A p value less than 0.05 was set as threshold for statistical significance.
Results
All patients underwent several imaging examinations, ranging from a minimum of 1 to a maximum of 4, for a total of 98 diagnostic procedures (Table 2). Of these, 79.6% (78/98) were considered as “usually appropriate” by ESR iGuide and 11.2% (11/98) were designated as “may be appropriate” (Fig. 3). Of note, 9.2% of tests (9/98) were not even suggested by ESR iGuide.
Of the 11 examinations performed and classified as “may be appropriate” by ESR iGuide, 9 (81.8%) were biopsies, 1 (9.1%) abdominal CT, and 1 (9.1%) barium contrast enema, respectively. On the other hand, of the 9 examinations performed and not suggested by ESR iGuide, 7 (77.8%) were biopsies, 1 (11.1%) colonoscopy, and 1 (11.1%) gastroscopy, respectively.
Ultrasound (US) and CT had been performed in 33 and 31 patients, respectively, and were the most frequently performed diagnostic tests, making up together more than 65% of all imaging examinations. 17 and 13 patients underwent biopsy and MRI, respectively, and only one had abdominal X-ray, contrast enema, gastroscopy or colonoscopy.
US was suggested as “usually appropriate” by ESR iGuide for all patients, but only 33 (82.5%) went ahead with it. Conversely, abdominal CT was recommended as appropriate for 38 patients and correctly performed in 30 of them, with only one patient receiving abdominal CT although this latter had been classified as inappropriate by ESR iGuide.
MRI was suggested as “usually appropriate” in 37 patients and performed in 13 of them, whereas 3 other patients underwent MRI although this latter received an appropriateness score lower than 7. As to radiographic tests, one patient underwent abdominal X-ray (which was suggested as appropriate in 15 cases), and one patient underwent barium contrast enema, a test that would have been considered as “usually not appropriate” by ESR iGuide. Finally, among 17 patients who underwent biopsy, this latter was suggested as “usually appropriate” in one case only, whereas for 9 of them it was designated as “may be appropriate” and for 7 it was not suggested by ESR iGuide.
The proportion of tests suggested by ESR iGuide with an appropriateness score equal to or higher than 7 was significantly different from that of the tests actually performed for all imaging modalities, except endoscopy (i.e. gastroscopy or colonoscopy, p = 0.5) and barium enema (p = 1.0).
According to the established prices within the BLINDED healthcare system, the total cost associated with the 98 imaging tests was €14,016, of which 21.6% (€3033) were related to inappropriate testing as per the guidelines.
Discussion
Diagnostic imaging is growing rapidly and is a major cause of increased costs for healthcare systems. Inappropriate testing leads to longer waiting lists, potential risks for patient health and medico-legal issues due to wrong or delayed diagnosis, and potential unnecessary exposure to ionising radiation. According to some studies, the reason for the increased demand for non-clinically justified tests could be identified in defensive medicine or in the use of medical imaging to reassure patients, despite there being no real suspicion of a disease [13,14,15].
The high costs and limited resources of healthcare systems justify the need for control tools aimed at an appropriate use of imaging. In this context, the ACR developed the first guidelines known as the ACR Appropriateness Criteria in 1993 [6]. In the following years, many alternatives were developed in Europe, such as the Royal College of Radiologists (RCR) iRefer and the French guidelines [16, 17]. Moreover, the Italian National Agency for Regional Health Services produced a text titled “Guidelines for diagnostic imaging” in 2004, which has not been updated since and among other issues, states that the radiologist can choose the best possible procedure for a given case [18]. Although several years have passed from the first guidelines, their use is still debated and not completely accepted. Particularly in Europe, several guidelines have been developed by national radiological societies without reaching international consensus. In this context, the European Society of Radiology introduced ESR iGuide in 2015 (then updated in 2016) and started with pilot implementations in Europe [4, 7].
In this study, we retrospectively evaluated the appropriateness level of imaging examinations performed in the diagnostic workup of 40 patients with HCC or CC, using the ESR iGuide appropriateness criteria as a reference. At the time of this study, no formal CDS system to guide imaging requests was available at our Institution, and using this approach, we observed that a substantial fraction of referrals (79.6%) was appropriate.
Of 20 examinations performed and suggested as “may be appropriate” or not suggested by ESR iGuide, liver biopsy accounted for as much as 81.8% and 77.8% of occurrences, respectively. This is in line with current guidelines, for which the diagnostic algorithm for HCC and CC is mainly based on radiological imaging, whereas pathological confirmation is relegated to cases in which imaging alone cannot establish a diagnosis [19, 20].
MRI was suggested as “usually appropriate” in a higher number of cases than it had actually been performed. This may be related to the particular anatomical area of interest for which MRI is considered the state-of-the-art diagnostic modality. However, MRI has higher costs than CT or US, is more time-consuming, and is usually less readily available than CT or US (resulting in longer waiting lists). This could explain the lower number of MRI examinations requested by referring physicians compared to those deemed as appropriate.
US was performed in 33 patients only, but suggested for all patients by ESR iGuide. This was because the patients’ clinical conditions were suggestive of a neoplastic disease, and/or because patients had reached the emergency room in acute conditions and CT had eventually been considered more appropriate than US. On the other hand, CT was indicated by the ESR iGuide in 38 patients but performed in only 30 of them, since in the remaining 8 cases diagnosis had been reached using MRI before CT.
The examinations that were found to be inappropriate in our study were performed not as first test, but as further steps of the diagnostic pathway. As a matter of fact, currently ESR iGuide does not allow entering data collected after the patient’s diagnostic workup has begun, and in our opinion, this circumstance might deserve further investigation. It could also be hypothesised that the examinations performed as third and fourth diagnostic tests did not play a decisive role for diagnosis, although they were useful for refining it. Despite this, our findings show that the use of ESR iGuide along the diagnostic pathway of HCC and CC patients would have allowed reducing the overall number of examinations and their related costs.
Our study has limitations. Firstly, we based our analysis on the available data, but there may have been some relevant information missing in the medical history that could have better outlined patients’ clinical pathways, partly due to the current absence of a centralised electronic patient record system at our Institution. Thus, we had limited clinical documentation provided by patients on every examination appointment, along with a brief clinical query reported on every request form by the referring physician. Secondly, our patient population was restricted to a relatively small number of patients with HCC or CC, partly due to our choice to only include patients with a definite diagnosis of either disease who had undergone at least their first imaging examination specific to their condition at our Institution. This should, on the one hand, have eliminated any potential bias related to using incomplete and/or not fully controllable data collected elsewhere outside our single-centre study design, but on the other hand, it may have prevented us from gleaning insight into the implications of a more widespread use of ESR iGuide. Therefore, we believe that our findings (although encouraging) should be considered no more than preliminary, and it is our hope that they will serve to pave the way to more extensive research on a multicentre basis, possibly allowing to draw more solid and general conclusions about the actual value of ESR iGuide for assisting diagnosis and optimising healthcare resources. In this setting, future work aimed at extending our evaluation of the ESR iGuide performance to a larger sample of patients with a broader disease spectrum is warranted.
In conclusion, ESR iGuide can be effective in guiding the selection of the appropriate imaging examinations and cutting costs due to inappropriate testing in patients with HCC or CC. Further research on a larger patient sample (possibly at multiple institutions and not limited to a restricted disease spectrum) could contribute to unravel the full potential of ESR iGuide adoption in clinical practice.
References
European Society of Radiology (ESR); American College of Radiology (ACR) (2016) European Society of Radiology (ESR) and American College of Radiology (ACR) report of the 2015 global summit on radiological quality and safety. Insights Imaging 7:481–484
Levy G, Blachar A, Goldstein L et al (2006) Nonradiologist utilization of American College of Radiology appropriateness criteria in a preauthorization center for MRI requests: applicability and effects. AJR Am J Roentgenol 187:855–858
Bright TJ, Wong A, Dhurjati R et al (2012) Effect of clinical decision-support systems: a systematic review. Ann Intern Med 157:29–43
European Society of Radiology (2019) ESR iGuide clinical decision support using European imaging referral guidelines. https://www.myesr.org/esriguide. Accessed 5 Dec 2019
European Society of Radiology (2018) Portal Guide. https://www.nationaldecisionsupport.com/esriguide/assets/portal-guide/ESRiGuidePortal_User_Guide_February_2018.pdf. Accessed 5 Dec 2019
American College of Radiology (2019) https://www.acr.org/Clinical-Resources/ACR-Appropriateness-Criteria. Accessed 5 Dec 2019
European Society of Radiology (2017) Summary of the proceedings of the international forum 2016: “Imaging referral guidelines and clinical decision support-how can radiologists implement imaging referral guidelines in clinical routine?”. Insights Imaging 8:1–9
Blackmore CC, Mecklenburg RS, Kaplan GS (2011) Effectiveness of clinical decision support in controlling inappropriate imaging. J Am Coll Radiol 8:19–25
Sistrom CL, Dang PA, Weilburg JB, Dreyer KJ, Rosenthal DI, Thrall JH (2009) Effect of computerized order entry with integrated decision support on the growth of outpatient procedure volumes: seven-year time series analysis. Radiology 251:147–155
Bookman K, West D, Ginde A et al (2017) Embedded clinical decision support in electronic health record decreases use of high-cost imaging in the emergency department; EmbED study. Acad Emerg Med 24:839–845
Wong MC, Jiang JY, Goggins WB et al (2017) International incidence and mortality trends of liver cancer: a global profile. Sci Rep 7:45846
Global Burden of Disease Liver Cancer Collaboration (2017) The burden of primary liver cancer and underlying etiologies from 1990 to 2015 at the global, regional, and national level: results from the Global Burden of Disease Study 2015. JAMA Oncol 3:1683–1691
Lehnert BE, Bree RL (2010) Analysis of appropriateness of outpatient CT and MRI referred from primary care clinics at an academic medical center: how critical is the need for improved decision support? J Am Coll Radiol 7:192–197
Remedios D, France B, Alexander M (2017) Making the best value of clinical radiology: iRefer Guidelines. Clin Radiol 72:705–707
Vilar-Palop J, Hernandez-Aguado I, Pastor-Valero M, Vilar J, González-Alvarez I, Lumbreras B (2018) Appropriate use of medical imaging in two Spanish public hospitals: a cross-sectional analysis. BMJ Open 8:e019535
The Royal College of Radiologists (2017) RCR iRefer Guidelines: making the best use of clinical radiology, 8e. The Royal College of Radiologists London https://www.irefer.org.uk. Accessed 5 Dec 2019
Société Française de Radiologie (2013). Guide du bon usage des examens d’imagerie médicale. http://gbu.radiologie.fr. Accessed 5 Dec 2019
La diagnostica per immagini-Linee guida nazionali di riferimento (2004) http://www.salute.gov.it/imgs/C_17_pubblicazioni_1164_allegato.pdf. Accessed 5 Dec 2019
European Association for the Study of the Liver (2018) EASL clinical practice guidelines: management of hepatocellular carcinoma. J Hepatol 69:182–236
Cai Y, Cheng N, Ye H, Li F, Song P, Tang W (2016) The current management of cholangiocarcinoma: a comparison of current guidelines. Biosci Trends 10:92–102
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
This article does not contain any studies directly involving human participants or animals performed by any of the authors. (Deidentified data related to patients’ history were retrospectively collected and compared with the ESR iGuide output in a simulation setup).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Gabelloni, M., Di Nasso, M., Morganti, R. et al. Application of the ESR iGuide clinical decision support system to the imaging pathway of patients with hepatocellular carcinoma and cholangiocarcinoma: preliminary findings. Radiol med 125, 531–537 (2020). https://doi.org/10.1007/s11547-020-01142-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11547-020-01142-w