Abstract
This study sought to determine whether adding virtual reality (VR) was superior to standard of care alone in facilitating reduction in pain and anxiety among children who underwent intravenous catheterization in the emergency department (ED). Sixty-six children aged 6–16 years who needed intravenous placement received VR, or standard of care in the ED (videos, television, iPad, child life specialist). Outcome measures included change in pain score, level of anxiety, patient and parent satisfaction (pain and anxiety), number of trials, and procedure time. Compared with controls, the intervention group had similar age, sex, number of trials, and anesthetic use. Time of procedure was shorter in the VR group (median 5 min) but this was not statistically significant compared with 7 min for the control group. Pain in the intervention group was lower, even before the procedure. Difference in pain (before and after) and anxiety (after the procedure) were similar in both groups. Satisfaction from anxiety management was higher for the VR group (p < 0.007) and children rated VR significantly more “fun” (p < 0.024).
Conclusion: VR was an effective distraction tool and increased satisfaction from anxiety management for this common pediatric procedure, and should be incorporated in management of anxiety in children in the ED setting.
Trial registration: clinicaltrials.gov ID NCT03681730, https://clinicaltrials.gov/ct2/show/NCT03681730
What is Known: • Virtual reality is an evolving computer technology that shows some promise in the areas of acute and chronic pain management due to its ability to create effective distraction. | |
What is New: • We report that among children in the emergency setting with intravenous catheterization, satisfaction from the use of VR for anxiety management should support implementation of VR systems for this procedure |
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Inserting a peripheral intravenous (IV) catheter is one of the most common procedures in children in the hospital setting. They are primarily used for therapeutic purposes such as administration of medications, fluids, and blood products as well as blood sampling [1].
Pain is a complex experience comprising sensory, cognitive, behavioral, and psychological components. Painful procedures, such as vaccinations, IV injections, laceration repairs, and dressing changes for burn wounds, are a common part of pediatric medical treatments [2] but pain management for these painful procedures is underused [3]. Recommendations for management of pain and anxiety during emergency department (ED) procedures include pharmacological measures [4] and distraction techniques [5] to help with coping mechanisms.
Virtual reality (VR) is a computer technology that creates an artificial 3-dimensional simulated environment. The system usually includes a head-mounted display and goggles, a computer screen, and sensors that track users’ head movements. These create the illusion of moving around in a virtual space. The technology places patients into a “virtual world” and more recently VR has been considered for medical indications, such as managing pain [6]. Several reports suggest that VR may reduce pain and anxiety among those using it [7, 8].
The aim of this study was to explore the role of VR in facilitating a reduction in pain and anxiety among children 6–16 years of age, during IV catheterization procedure in the ED, compared with standard of care. We also wanted to assess satisfaction of using a VR intervention for reduction of pain and anxiety in the ED.
Materials and methods
This was a prospective randomized controlled trial (ClinicalTrials.gov—NCT03681730) conducted in a tertiary pediatric ED of the BC Children’s Hospital in Vancouver, Canada, during the period May 2018–August 2018. The study was approved by the Institutional Review Board.
Participants
Included were children 6 to 16 years of age if the most responsible physician ordered IV catheterization, and the children were willing to participate. We excluded children that were triaged to the highest acuity category and those that had conditions that excluded them from being able to describe their pain or anxiety, or had trauma to the face, where the VR goggles were to be placed. We also excluded children that already participated in the trial. Parents were asked to sign an informed consent and children 7–16 years old were asked to sign an informed assent.
Randomization
After the research assistant demonstrated to the subject the VR system and how it operates, children were randomized in a 1:1 ratio to an intervention arm—VR goggles use, or comparator arm—standard of care in the ED at the time of recruitment. The control arm may have included heterogeneous group of interventions in order to allow generalizability to other pediatric EDs, and included parental comfort measures, use of distraction tools available in the ED (such as books, DVD movies, a television set, an iPad, bubbles), support by a child life specialist present in the room, or any other activity the child may have requested.
Oral analgesia and topical anesthetics were frequently given in our ED and no restrictions were made for pharmaco-analgesia. Randomization was prepared using computerized randomization table function in blocks of four and achieved using sealed opaque envelopes that were opened sequentially anytime consent and assent were signed. Enrollment and sequential assignment to the intervention group were performed by trained research assistants.
At the initiation of the procedure, children in the intervention arm were provided with the VOX+ Z3 3D Virtual Reality Headset (China). An Asus Zenfone 2 ZE551ML mobile device (Taiwan) pre-loaded with the VR Roller Coaster app [9] was used in the VR system. We used low-cost VR system with a free app in order to offer potential generalizability of the system to other institutions. We used a Roller Coaster app as this type of activity is frequently loved by children and may be attractive to use. Children were able to view the roller coaster artificial environment as riders and could look at 360° around them by moving their head. Sounds of the roller coaster on the track and cheering voices of other riders and spectators on the ground could be heard via the sound system. Children did not need to operate any device using their hands. A trial of up to 1 min was provided prior to the procedure to each child in the intervention arm to ensure appropriate fit and device focus. After the study, all children had a chance to play for 15 min with the VR system. When using the VR system, children wore disposable surgical caps to limit device contact for infection control purposes. Between participants, the VR system was cleaned with isopropyl alcohol wipes with special focus on the front padding, lenses, and head straps. Chlorhexidine cleaning wipes were not used as they were found to leave a residue over the lenses.
Outcome measures
The primary outcome measure was the difference in pain score before and after the procedure, measured using the Faces Pain Scale – Revised (FPS-R), a self-report measure of pain intensity developed for children [10]. Pain was measured immediately before and immediately after the procedure. It was measured by showing the child the faces pain scale and reading a scripted question. The child then selected one of the 6 faces (scored—0, 2, 4, 6, 8, 10).
Secondary measures were the level of anxiety as reported by the patient, measured as a total Venham Situational Anxiety score immediately after IV was secured. This was a validated scoring system that used a series of 8 flash cards, each with a pair of line drawings representing a child in different levels of anxiety and distress [11].
Other outcome measures included patient satisfaction from the procedure. This was determined using an open-ended question “What is your opinion on how the procedure went.” We also documented which medications (orally or topically) were used before IV placement and length of the procedure, defined as time between procedure starting point, when the provider, equipment, and patient were all ready to begin (at which point the intervention arm began using the VR headset) until end time, once there was no further manipulation of the IV placement (at which point the VR headset was removed and the number of attempts recorded). For patients requiring multiple IV attempts, time continued until successful placement or the provider made no further attempts to complete the IV. Time needed to demonstrate how the VR headset operates was not included in the duration of the procedure.
Statistical analysis
Data was collected on a Microsoft Excel spreadsheet and analyzed using SPSS (SPSS version 25; IBM Corporation, Armonk, NY, USA). All probability was two-tailed, and p value of < 0.05 was considered statistically significant. The authors had full access to the data and were responsible for its integrity.
Sample size was calculated with a two-sided α error rate of 5% and B error rate of 20%. Clinical meaningful reduction in pain was determined to be 2 points on the Faces Pain Scale – Revised and a median score was determined to be 5 (scale 0–10). Based on these assumptions, a sample size of 32 subjects per group was required.
Continuous variables were presented as mean and SD and normally distributed variables as median, 25th (Q1) and 75th (Q3) percentiles, and interquartile range (IQR = Q3 − Q1). Categorical variables were presented as frequencies and percentages. Patients were dichotomized into using VR or using standard-of-care measures during IV placement procedures. The difference in primary and secondary outcomes between groups was reported. The Mann-Whitney U test was performed for continuous variables, since the population was found not to have normal distribution. Chi-square and Fisher’s exact tests were used to examine the difference between categorical variables. We did not adjust our findings for multiple comparisons.
To further evaluate the benefit of VR use, we performed an ordinal logistic regression categorizing children into three groups (dependent variable)—those that had improvement in their pain (17 children), those that did not report any change in pain (28 children), and those that reported worsening pain (21 children)—and adjusting the analysis for age and gender.
Results
A total of 136 patients were approached and 70 (51%) consented and completed the study. Four (6%) were excluded because they decided to withdraw participation after consenting and being randomized (Fig. 1).
A total of 66 procedures were analyzed, 30 (45%) females, median age 9.5 year (range 6–16.8). For 45 (68%) children IV was successfully placed after the first trial, 12 (18%) needed 2 trials, 6 (9%) children had three attempts to secure an IV, and one child had 4 attempts.
Majority of children (35, 53%) received oral analgesia before the procedure (24 acetaminophen, 20 ibuprofen, 2 intranasal opioids (one in the VR group, one in the control group)), and almost all (60, 91%) received topical anesthetics before the procedure (51 topical 4% amethocaine gel, 14 vapocoolant (Pain Ease®), 1 lidocaine/prilocaine eutectic mixture (EMLA)).
Twelve (39%) of the children in the control arm used technology-related distraction tools (TV, other mobile screen), and all other non-VR distraction included speaking to caregivers or staff or no distraction at all. All children trialing the system before the study did not have any nausea.
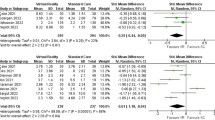
Documentation of pain and anxiety scores, as well as the average difference in pain, is presented in Table 1. We found similar age, sex, number of trials needed to secure the IV, and the rate of use of oral and topical anesthetics between groups. Timing of the procedure was shorter in the VR group (median 5 min), but this was not statistically significant compared with 7 min for the control group.
When the model adjusted for study arm, age, and gender, no significant difference was found among children who had pain improvement and who did not report any change in pain and those that reported worsening pain (Table 2).
Of interest, we noted a significantly lower level of pain as reported by children assigned to the VR arm just before the procedure (and after being aware of their assigned arm) compared with those in the control group (median score 2/10 and 4/10 respectively). In the VR group, pain after the procedure was reported slightly lower than that before the procedure (− 0.51/10), and in the control group, the pain was slightly higher (+ 0.16/10), but this was not statistically significant (p = 0.64).
Level of anxiety, as reported by children immediately after placement of the IV, was similar in both groups, but when satisfaction from anxiety management was rated, it was significantly better in the VR group (median score 9 and 7 in VR and control groups, respectively, p < 0.007). Similarly, children reported much more “fun” with the VR intervention (median score 5/10 and 4/10 in VR and control groups, respectively, p < 0.024).
Discussion
Virtual reality creates artificial stimuli that include visual imagery and spatialized sound that attempt to modify the virtual environment and create a sense of “presence” in the virtual world [12]. The improvement in VR technology, allowing software applications to run on a smartphone, and the low cost of goggles available on the market have brought VR closer to hospitals and medical applications, especially in the area of pain and anxiety [6]. This is the first study to report the effect of a portable VR system on pain and anxiety among children in the ED setting.
A theory explaining the role of VR in reducing pain and anxiety suggests limited attentional capacity and if attention can be diverted, the patient may have a slower response to incoming pain signals [7]. Functional magnetic resonance imaging of healthy individuals showed a greater than 50% reduction in pain-related brain activity in 5 areas of the brain when exposed to VR during a painful stimulus (thermal pain stimulator on the foot) [13].
We report higher satisfaction from anxiety management with VR use among children in the ED during IV placement, more than with other activities aimed at distracting the child’s attention. We found no significant difference in pain reduction as reported by children, almost all of whom received topical analgesia for the procedure and/or oral analgesia in the ED.
The VR group reported significantly less pain before starting the IV procedure, which was further slightly reduced after IV placement. It is possible that despite randomization, we captured a group of children in the VR group with less pain in the initiation of the procedure. However, it is also possible that children that were introduced to the VR system before consenting to participate, and were soon to use the system, were excited about the VR experience and felt or reported less pain. The difference in pain reported was still significant after the IV procedure. The change in pain (before–after) was not statistically different, yet was slightly improved with VR, and slightly worse in the control arm (total mean difference 0.67/10).
It was clear that children liked the VR experience, as they rated it “much more fun” compared with other activities in the control group, even when a child life specialist was involved. The VR was a novelty and our experience recruiting these children clearly reflects this satisfaction. The “fun” aspect of VR was believed to influence VR analgesic effects [14].
Similarly, using VR was associated with more satisfaction from anxiety management compared with other anxiolytic activities, similar to previous reports of VR ability to reduce anxiety, and to induce positive emotions [14]. VR is a very effective distractor as it is able to engage different senses simultaneously, diverting attention from painful stimuli [14], escaping from “the painful real world” [15]. Looking at an interesting scene associated with the thrill of a roller coaster in a virtual world helped with satisfaction from management of anxiety, an experience that is naturally associated with a painful procedure such as IV placement.
There are several possible explanations why children in our VR cohort did not report less pain than those in the control group. Firstly, their level of pain at the beginning of the procedure was low (2/10) especially in relation to the control group. Secondly, our tertiary pediatric ED has been focused on reducing pain and anxiety of children during procedures for years, and implementation of oral and topical analgesia as well as numerous options for distraction has been part of children’s care. It is also possible that the relatively passive interaction with the virtual world, not being active in playing, may have resulted in limited effect of the system, similar to previous reports showing interactive distraction to be more effective [16,17,18,19].
Our ED has been using advanced analgesia and anxiolysis techniques, including the training of staff to support children during procedures, and we are fortunate to have a child life specialist that was involved in many of the procedures in the control arm (as part of our standard of care). These actions likely reduced pain and anxiety to start with, which may account for the relatively low change in pain reported by children. To that effect, the vast majority of children (80% in the VR group, 65% in the control group) wanted the same intervention next time they need an IV.
We were aware that for some children, the motion associated with a roller coaster may produce some nausea, but were glad to find that all children trialing the system before the study did not have any nausea.
Vagnoli et al. reported that a relaxation-guided imagery significantly reduced preoperative anxiety and postoperative pain in children, compared with standard of care in a children’s hospital in Florence, Italy [20]. Gold et al. assessed VR for IV placement, using advanced VR systems that necessitated the use of a computer attached to the VR goggles. Following IV placement in the magnetic resonance imaging or computed tomography suite, they found no increased pain among children using VR compared with fourfold increase in pain without. Likely due to the small sample size, this clinically important difference failed to achieve statistical significance [21]. More recently, Gold et al. assessed VR utility during routine blood draws in children 10 to 21 years of age in Los Angeles. Compared with standard of care that included television playing a cartoon movie at a low volume, those in the VR + standard of care group had significantly less pain and anxiety measured as pain Visual Analogue Scale (VAS), pain Colored Analogue Scale (CAS), and Childhood Anxiety Sensitivity Index [22]. Similarly, Piskorz et al. showed that VR was associated with reduction of pain during IV placement in 38 children 7 to 17 years old using the Visual Analogue Scale [23]. In these studies, compared with ours, advanced (and much more expensive) VR systems were used, which may have enhanced the virtual world experience and ability to capture children’s attention [24]. Furthermore, our study was in the emergency room, a setting that is likely more upsetting for children, since a hospital visit was unexpected and an injury may have taken place and when no advanced preparation of the child could take place. Recently, Dumoulin et al. from Ottawa assessed children visiting the ED and reported reduction in fear of pain but not in pain intensity (Visual Analogue Scale) when VR distraction was used compared with watching television and distraction provided by a child life specialist [25]. In 2 separate RCTs reported in a single paper from Australia, children 4–11 years old in ED and an outpatient laboratory, going through intravenous cannulation or venipuncture procedures, VR was associated with significant reduction in pain compared with standard of care (using Faces Pain Scale – Revised, p = 0.018 in the ED) and significantly less increase in pain with VR for venipuncture (p = 0.034 in the lab) [26]. These encouraging findings using VR may be associated with the younger age group in the study from Australia or the more interactive participation of children with the environment through gaze-based tracking.
This study had several limitations. First, it was in a single hospital, limiting variability in surgeons and procedures. Furthermore, we did not measure level of anxiety before the procedure, limiting the ability to demonstrate potential reduction in anxiety with both study arms. Finally, most children had low level of pain before and after the procedure, suggesting that VR (as well as SOC) had limited ability to reduce further the level of pain.
Future research should differentiate different groups of children by age, as younger children may be more receptive to distraction interventions [27]. It is also important to focus on finding ways to engage children in the VR activity, assess if the novelty of the VR activity itself has any bearings on pain and anxiety perception (the excitement of something new), and assess what VR software and equipment may enhance relief of pain and anxiety in painful procedures. It is also important for future research to address if there is any difference in effect size of analgesia and anxiolysis between different levels of VR systems, and if using low-end (and low resolution) VR system may have contributed to the limited analgesia in this study, compared with other interventions.
In conclusion, the reduction in cost of VR systems and relative ease of using it, as well as the findings in this study related to satisfaction from this tool for anxiety management, are supportive of implementation of VR systems for this procedure.
Abbreviations
- CAS:
-
Colored Analogue Scale
- ED:
-
Emergency department
- EMLA:
-
Eutectic Mixture of Local Anesthetics
- FPS-R:
-
Faces Pain Scale – Revised
- IRB:
-
Institutional Review Board
- IQR:
-
Interquartile range
- IV:
-
Intravenous catheter
- VR:
-
Virtual reality
- VAS:
-
Visual Analogue Scale
References
Catudal JP (1999) Pediatric IV therapy: actual practice. J Assoc Vasc Access 4(1):27–29. https://doi.org/10.2309/108300899775703652
Birnie KA, Noel M, Chambers CT, Uman LS, Parker JA (2018) Psychological interventions for needle-related procedural pain and distress in children and adolescents Cochrane Database Syst Rev 10. https://doi.org/10.1002/14651858.CD005179.pub4
MacLean SBA, Obsipo J, Young KD (2007) The gap between pediatric emergency department procedural pain management treatments available and actual practice. Pediatr Emerg Care 23(2):87–93. https://doi.org/10.1097/PEC.0b013e31803
Olsen K, Weinberg E (2017) Pain-less practice: techniques to reduce procedural pain and anxiety in pediatric acute care. Clin Pediatr Emerg Med 18(1):32–41. https://doi.org/10.1016/j.cpem.2017.01.007
Zempsky WT, Cravero JP (2004) Relief of pain and anxiety in pediatric patients in emergency medical systems. Pediatrics 114(5):1348–1356. https://doi.org/10.1542/peds.2004-1752
Arane K, Behboudi A, Goldman RD (2017) Virtual reality for pain and anxiety management in children. Can Fam Physician 63(12):932–934
Hoffman HG, Chambers GT, Meyer WJ 3rd, Arceneaux LL, Russell WJ, Seibel EJ, Richards TL, Sharar SR, Patterson DR (2011) Virtual reality as an adjunctive non-pharmacologic analgesic for acute burn pain during medical procedures. Ann Behav Med 41(2):183–191. https://doi.org/10.1007/s12160-010-9248-7
Hoffman HG, Richards TL, Coda B, Bills AR, Blough D, Richards AL, Sharar SR (2004) Modulation of thermal pain-related brain activity with virtual reality: evidence from fMRI. Neuroreport 25(7):2013–2014. https://doi.org/10.1097/01.wnr.0000127826.73576.91
Pryszard Android / iOS Gameplay Walkthrough. Short Play #572 VR Roller Coaster Android Gameplay. Youtube. https://www.youtube.com/watch?v=_QnZpNYLqsg. Published January 4th 2015. Accessed 30 July 2020
International Association for the Study of Pain. Faces Pain Scale -Revised Home. International Association for the Study of Pain. http://www.iasp-pain.org/Education/Content.aspx?ItemNumber=1519. Accessed 30 July 2020
Venham LL, Gaulin-Kremer E (1979) A self-report measure of situational anxiety for young children. Pediatr Dent 1(2):93–96
Bowman DA, McMahan PR (2007) Virtual reality: how much immersion is enough? Computer 40:36–43. https://doi.org/10.1109/MC.2007.257
Hoffman HG, Richards TL, Van Oostrom T, Coda BA, Jensen MP, Blough DK, Sharar SR (2007) The analgesic effects of opioids and immersive virtual reality distraction: evidence from subjective and functional brain imaging assessments. Anesth Analg 105(6):1776–1783. https://doi.org/10.1213/01.ane.0000270205.45146.db
Triberti S, Repetto C, Riva G (2014) Psychological factors influencing the effectiveness of virtual reality-based analgesia: a systematic review. Cyberpsychol Behav Soc Netw 17:335–345. https://doi.org/10.1089/cyber.2014.0054
Schneider SM, Workman ML (1999) Effects of virtual reality on symptom distress in children receiving chemotherapy. CyberPsychol Behav 2:125–134. https://doi.org/10.1089/cpb.1999.2.125
Dahlquist LM, McKenna KD, Jones KK, Dillinger L, Weiss KE, Ackerman CS (2007) Active and passive distraction using a head-mounted display helmet: effects on cold pressor pain in children. Health Psychol 26:794–801. https://doi.org/10.1037/0278-6133.26.6.794
Wender R, Hoffman HG, Hunner HH, Seibel EJ, Patterson DR, Sharar SR (2009) Interactivity influences the magnitude of virtual reality analgesia. J Cyber Ther Rehabil 2:27–33
Gutierrez-Maldonado J, Gutierrez-Martinez O, Cabas-Hoyos K (2011) Interactive and passive virtual reality distraction: effects on presence and pain intensity. Stud Health Technol Inform 167:69–73
Law EF, Dahlquist LM, Sil S, Weiss KE, Herbert LJ, Wohlheiter K, Horn SB (2011) Videogame distraction using virtual reality technology for children experiencing cold pressor pain: the role of cognitive processing. J Pediatr Psychol 36:84–94. https://doi.org/10.1093/jpepsy/jsq063
Vagnoli L, Bettini A, Amore E, De Masi S, Messeri A (2019) Relaxation-guided imagery reduces perioperative anxiety and pain in children: a randomized study. Eur J Pediatr 178(6):913–921
Gold JI, Kim SH, Kant AJ, Joseph MH, Rizzo AS (2006) Effectiveness of virtual reality for pediatric pain distraction during I.V. placement. CyberPsychol Behav 9:207–212. https://doi.org/10.1089/cpb.2006.9.207
Gold JI, Mahrer NE (2017) Is virtual reality ready for prime time in the medical space? A randomized control trial of pediatric virtual reality for acute procedural pain management. J Pediatr Psychol 43(3):266–275. https://doi.org/10.1093/jpepsy/jsx129
Piskorz J, Czub M (2018) Effectiveness of a virtual reality intervention to minimize pediatric stress and pain intensity during venipuncture. J Spec Pediatr Nurs 23:e12201. https://doi.org/10.1111/jspn.12201
Hoffman HG, Seibel EJ, Richards TL, Furness TA, Patterson DR, Sharar SR (2006) Virtual reality helmet display quality influences the magnitude of virtual reality analgesia. J Pain 7:843–850. https://doi.org/10.1016/j.jpain.2006.04.006
Dumoulin S, Bouchard S, Ellis J, Lavoie KL, Vézina MP, Charbonneau P, Tardif J, Hajjar A (2019) A randomized controlled trial on the use of virtual reality for needle-related procedures in children and adolescents in the emergency department. Games Health J 8(4):285–293. https://doi.org/10.1089/g4h.2018.0111
Chan E, Hovenden M, Ramage E, Ling N, Pham JH, Rahim A, Lam C, Liu L, Foster S, Sambell R, Jeyachanthiran K, Crock C, Stock A, Hopper SM, Cohen S, Davidson A, Plummer K, Mills E, Craig SS, Deng G, Leong P (2019) Virtual reality for pediatric needle procedural pain: two randomized clinical trials. J Pediatr 209:160–167. https://doi.org/10.1016/j.jpeds.2019.02.034
Sinha M, Christopher NC, Fenn R, Reeves L (2006) Evaluation of nonpharmacologic methods of pain and anxiety management for laceration repair in the pediatric emergency department. Pediatrics 117:1162–1168. https://doi.org/10.1542/peds.2005-1100
Acknowledgements
We are grateful for the patients that participated in this study. A special acknowledgement to Paul Clerc, Charlotte Zwimpfer, Jennifer Ham, Clare Lambert, Isabelle Khalifa, and Nancy Lum who collected data for this study.
Contributors’ contributions
Dr. Goldman and Dr. Behboudi conceptualized and designed the study, submitted to ethics approval, and monitored collection of data. Dr. Goldman and Dr. Behboudi drafted the initial manuscript, and reviewed and revised the manuscript. All authors approved the final manuscript as submitted and agree to be accountable for all aspects of the work.
Funding
Funded by the Peace Arch Hospital, as part of an improvement project. Funds were allocated for a research assistant and all other administrative measures related to presentation and publication of the trial results.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee (University of British Columbia Clinical Research Ethics Board, H17-02711) and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Disclaimer
The funding agency had no influence on the design of the study, its conduct or publication of data from this project.
Additional information
Communicated by Gregorio Paolo Milani
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Goldman, R.D., Behboudi, A. Virtual reality for intravenous placement in the emergency department—a randomized controlled trial. Eur J Pediatr 180, 725–731 (2021). https://doi.org/10.1007/s00431-020-03771-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00431-020-03771-9