Abstract
The number of lymph nodes retrieved from colorectal cancer (CRC) resection specimens is crucial for adequate diagnosis and therapy. Previous studies indicate that in addition to the extent of surgical resection and the quality of pathological lymph node examination, non-modifiable tumour parameters like microsatellite instability (MSI) are associated with higher lymph node count. In order to study the potential influence of MSI on lymph node count, we analysed a previously MSI-typed population of CRC patients (n = 1196) to determine the relationship between MSI and the frequency with which at least 12 lymph nodes were retrieved, as well as the mean and median number of retrieved lymph nodes. MSI was associated with an increased frequency of 12-node retrieval, as well as a higher mean and median lymph node count in the overall analysis (p 0.004 and 0.001 for 12-node retrieval and lymph node count, respectively). However, when the analysis was restricted to cancers of the proximal colon, the main location of microsatellite unstable tumours (84% in our study), no association between MSI and 12-node retrieval was found. Subcategorisation by UICC stage of proximally located cancers showed a statistically significant increase in the lymph node count only in microsatellite unstable stage I tumours (p 0.010). In conclusion, our data shows that previously reported associations between MSI and higher lymph node count are mainly a consequence of the increased incidence of microsatellite unstable cancer in the proximal colon. Our finding that MSI is related to a significantly higher mean lymph node count in proximal stage I cancers may indicate that the immunogenicity of this molecular tumour type induces earlier lymph node activation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Although contemporary management of colorectal cancer (CRC) is multimodal, surgical resection remains the mainstay of curative treatment [1]. In addition to the degree of tumour invasion, the number of involved lymph nodes also defines the UICC stage, which is a crucial prognostic indicator and guides the use of adjuvant chemotherapy [2]. Hence, adequate lymph node retrieval is essential for the pathological evaluation of resected specimens. Since the introduction of the AJCC/UICC staging manuals in 1997 [3], which require a minimum of 12 lymph nodes for the adequate staging of CRC, various studies have addressed the impact of different factors on the lymph node count.
Independent of other factors, the depth of colonic wall penetration, reflected in the T category, directly correlates to the number of nodes retrieved [4]. Tumours that are larger or that have a higher T category are thought to provoke a greater antigenic immune and inflammatory response within regional lymph nodes leading to increased prominence and easier retrieval. It also seems probable that macroscopically aggressive tumours are resected and examined with greater diligence [5].
Furthermore, the site of the disease is related to the number of retrieved lymph nodes. Several studies have demonstrated that more lymph nodes are retrieved from right-sided than from left-sided cancers [5,6,7,8]. Although the reasons for this discrepancy are not entirely clear, differences in the anatomy of the blood and lymphatic drainage are hypothesised to be responsible [9]. Other possible explanations are location-specific molecular mechanisms: proximal carcinomas are more commonly microsatellite unstable, BRAF-mutated and express the CIMP phenotype, whilst chromosomal instability is more common in distal tumours [10]. Although the association between tumour location and the underlying molecular pathways is well established, various studies reported that adequate lymph node count (a minimum of 12 lymph nodes) is independently associated with microsatellite instability (MSI) [11,12,13].
In order to investigate the association between MSI and the lymph node count as well as the frequency with which it was adequate in resected specimens, we examined data from 1196 patients with CRC enrolled in a population-based case-control study.
Materials and methods
Study population
The patients investigated were participating in the DACHS study (DACHS: Darmkrebs, Chancen der Verhütung durch Screening), a population-based case-control study of CRC with patient follow-up, which has already been described in detail in previous publications [14, 15]. Patients were recruited from all 22 hospitals of the study region (the Rhine-Neckar region in southwest Germany), were 30 years or older with a histologically confirmed first diagnosis of primary colorectal cancer between 2003 and 2007, were physically as well as mentally fit to take part and able to communicate in German. Of this population, 1196 patients (those with available data on lymph node count, CRC category and microsatellite status) were included in our analysis. The characteristics of the study population are illustrated in Table 1.
Data collection
Patient information was acquired in standardised personal interviews after surgery, during hospitalisation or at home after discharge. Clinical data (discharge letters, pathology reports of the cases and endoscopy reports) was also collected.
Definition of proximal and distal colorectal cancer
Tumours oral to the left (splenic) colic flexure were defined as being proximal, those aboral as distal. This well-established cut-off was chosen based on the differing embryological origins of the proximal and distal segments of the colon and since it is the boundary between regions supplied by the superior and inferior mesenteric arteries.
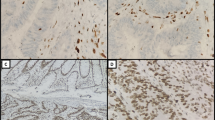
Collection and processing of tumour samples
Formalin-fixed paraffin-embedded (FFPE) colorectal tumour samples were collected from the pathology departments of participating institutions and transferred to the tissue bank of the National Center for Tumour Diseases (NCT) in Heidelberg.
After microscopic identification of areas with the highest tumour cell concentration (comprised of at least 70% tumour cells), DNA was isolated from the tumour tissue blocks. DNA isolation was performed using a commercial DNA Extraction Kit (DNeasy; Qiagen) following the manufacturer’s protocols. Microsatellite instability was identified in 1196 cases using a mononucleotide marker panel (BAT25, BAT26 and CAT25). The marker panel used is able to differentiate MSI-high from non-MSI-high tumours with a sensitivity of 98.2%, a specificity of 100% and in 100% agreement on MSI-high tumours with the National Cancer Institute/International Collaborative Group on HNPCC (NCI/ICG-HNPCC) marker panel (BAT25, BAT26, D17S250, D2S123 and D5S346) for the evaluation of microsatellite instability in colorectal cancer [16, 17].
Lymph node examination
The number of retrieved lymph nodes was taken from pathology reports and discharge letters which were available from all participating institutions. Tumour processing (gross room dissection and histopathological evaluation) was performed by five different pathological institutes, which were not aware of the specimens’ inclusion in a study at the time of assessment, reflecting performance in routine practice in the study region. Following the, at that time contemporary, UICC TNM Classification Guidelines 6th edition [18], when fewer than 12 lymph nodes were histologically assessable after primary grossing, mesenteric fat was routinely re-examined. No fat clearance techniques were routinely used during lymph node assessment.
Statistical analysis
Descriptive analyses were carried out on the clinical and pathological characteristics of patients enrolled in the study. MSI/MSS subgroups were defined by differing clinicopathological characteristics of the tumours and tested for heterogeneity with respect to whether lymph node retrieval was adequate (≥12 assessable nodes retrieved) (I) and the total number of lymph nodes (II).
P values were determined using either (I) chi-square test (if one cell had <5 observations in the 2 × 2 table, Fisher’s exact test was used) or (II) non-parametric two-sample median test (Wilcoxon rank-sum test, two-sided p value).
All analyses were performed with SAS, software version 9.2 (SAS Institute, Cary, NC). Tests for statistical significance were two-sided and defined by p < 0.05.
Overview of studies reporting an association between MSI status and lymph node count
Studies reporting on the association of MSI status and lymph node count in CRC were identified by PubMed search up until Jan. 15, 2017 using “lymph node yield/count/harvest/number,” “MSI,” “colon cancer” and “colorectal cancer” as keywords. Manuscripts providing data concerning MSI status, the median lymph node count, mean lymph node count and/or the frequency of adequate (≥12) lymph node count were chosen for comparison.
Results
Lymph node count and MSI/MSS status
In the complete cohort of 1196 CRCs, a median of 16 and a mean of 17 lymph nodes were found. An adequate retrieval of at least 12 lymph nodes was seen in 81% of cases (Table 2).
The study cohort comprised 113 MSI and 1083 MSS tumours. Adequate lymph node count was reported for 91% of the MSI and 80% of the MSS cancers, respectively (p = 0.004). However, after stratification according to UICC stage, an association between adequate lymph node count and MSI status was only observed for UICC stage I (pT1/pT2, pN0, pM0) cancers (p 0.004).
When restricted to the proximal colon, no statistically significant difference in the frequency of adequate lymph node retrieval was observed between MSI and MSS cancers (89 versus 87%, p = 0.576). Further subclassification of proximal colon cancers by UICC stage showed a higher frequency of adequate (≥12) lymph node retrieval in MSI tumours only among stage I CRCs (p: 0.010).
Moreover, significant differences in the median and mean lymph node counts between MSI and MSS were restricted to UICC stages I-II and to T categories I-III. Within the proximal colon, MSI was, in general, associated with higher lymph node count (p 0.009). Subclassification based on UICC stage showed this association to be limited to stage I tumours.
Overview of studies reporting an association between MSI status and lymph node count
Our PubMed search found five manuscripts meeting the stated requirements (Table 3). Two publications by Ogino et al. [19, 20] were not used for comparison, in spite of giving data on lymph node number and MSI status, since the association with lymph node count was not directly addressed. The included investigations originated from four different countries and were published between 2009 and 2013, representing geographical diversity and scientific discourse. Except for the manuscript by Eveno et al. [13], a prospective study, the investigations were retrospective. However, one study population included a prospective patient series enrolled in a sentinel node project.
Our study cohort was comprised of 1196 patients including 113 with microsatellite unstable CRC (9.4%). The largest previous study, conducted by Belt et al. [12], included more than 300 cases of CRCs. While Eveno et al. [13] and MacQuarrie et al. [21] detected MSI in 12–13% of their cohorts, the ratio of MSI cases reported by Belt et al. (19.6%), Søreide et al. [22] (27%) and Berg et al. [11] (33%) were much higher.
The minimum adequate lymph node count of 12, as required by the current AJCC/UICC staging manuals [23], was achieved in over 80% of our study cohort. Since the first publication by Søreide et al. [22] in 2009, the frequency of adequate (≥12) lymph node retrieval has risen from 36 to 67% in the 2013 publication by Berg et al. [11]. In the Dutch study by Belt et al. [12], a minimum lymph node count of more than 10 was achieved in 40% of cases. The other studies did not give data on minimum lymph node count compliance.
Discussion
A series of studies have shown that more lymph nodes are obtained in resected CRC specimens from the proximal than from the distal colon [5, 7, 24, 25]. Although the association between proximal tumour location and underlying MSI is well known [26, 27], some authors still argue against an explanation for differing lymph node count based strictly on anatomy. These reports link an adequate lymph node count to the influence of microsatellite instability [11,12,13].
In order to study the role of MSI on adequate as well as total lymph node count, we examined data from 1196 CRC patients (UICC stages I-IV), who were diagnosed between 2003 and 2007, following current standards for lymph node retrieval and assessment in pathology. A 12 lymph node minimum was used as the cut-off for the distinction between cancers with adequate and inadequate lymph node retrieval.
As in previous reports, our data showed a statistically significant difference (p = 0.004) in the number of lymph nodes retrieved in CRC with MSI versus MSS tumours, with an adequate lymph node retrieval of 91 and 80% for MSI and MSS cancers, respectively. However, a location-specific analysis of lymph node count in the proximal colon, where most MSI tumours (84% in this study) are found, showed no statistically significant difference (p = 0.576) in adequate lymph node count between MSI and MSS colon carcinoma. A further comparison of lymph node count in the distal colon and rectum lacked statistical significance due to low prevalence of MSI tumours in those locations.
In a detailed assessment, an association between MSI and adequate lymph node count was found for stage I cancers (p = 0.004). In a further subclassification of proximal colon cancers by UICC stage, this association was also restricted to stage I cancers (p 0.010). The frequency of adequate lymph node count was similar in MSI and MSS cancers of the proximal colon among UICC stages II-IV. Thus, in contrast to previous reports, we saw a significant association between MSI and adequate (AJCC/UICC minimum of 12 assessable lymph nodes) lymph node count only in UICC stage I, proximal cancers.
In order to study the association between MSI and total lymph node count, independently from whether the total was adequate, we also compared median and mean lymph node retrieval of MSI/MSS colorectal cancers. Here, we found a significantly higher lymph node count in MSI cancers of UICC stages I-II as well as T categories I-III. The difference in lymph node count, however, was again restricted to UICC stage I (pT1/T2, pN0) when analysis was restricted to the proximal colon.
The influence of MSI on higher lymph node count in the early stage of colorectal tumour development suggests underlying mechanisms of tumour biology. It is possible that tumour immunogenicity of early-stage MSI-H cancers leads to an increased immune reaction and enlargement of the lymph nodes, facilitating detection. This concept of tumour immunogenicity seems consistent with the characteristic “Crohn’s-like” lymphoid reaction accompanying CRC with microsatellite instability. The generation of frame shift mutations in coding microsatellites (coding MSI) leads to the production of neo-peptides in MSI-H cancers which are presented at the cell surface via MHC molecules [28]. This is believed to stimulate the immune system and is a possible explanation for the remarkably strong lymphocytic infiltration which is a characteristic feature of this cancer type [29].
The absence of an association between MSI and higher lymph node count in UICC stages II-IV could indicate a decreasing relevance of this MSI-related, immunogenic effect on the number of retrieved lymph nodes. In higher UICC stages, tumour-induced tissue destruction may cause a greater inflammatory response. This would also explain the higher number of lymph nodes found in UICC stages II-IV compared to stage I and indicate that the influence of MSI on lymph node count is overshadowed in more deeply invasive cancers.
Our results are in line with the findings in stage III CRC reported by MacQuarrie et al., which indicated no significant relationship between MSI-H status and a higher number of retrieved lymph nodes [21]. The study was restricted to stage III CRC and thus could not assess the influence of MSI-H on earlier stages, where we have identified an association. Moreover, a recent publication by Rössler et al., which investigated the relationship between lymph node size and lymph node involvement, supports our findings. Similar to the results of our study, the mean size of lymph nodes in MSI cancers was reported as being significantly larger than in MSS cancers. However, when the analysis was restricted to proximal tumours, microsatellite instability was not associated with lymph node size [30].
Søreide et al. and Berg et al. found, in their studies [11, 22], MSI-H to be associated with a higher frequency of adequate lymph node retrieval [11, 22]. However, in the whole study population, this was achieved only in 36% [22] and in 67% [11] of cases, respectively, which does not comply with current quality standards. Moreover, both Norwegian studies report a very high percentage of MSI in CRC (27% [22] and 33% [11]): more than double the average reported frequency of MSI in CRC [31]. While geographical/epidemiological differences in molecular biology seem unlikely to be responsible, a sample selection bias due to the ex vivo sentinel lymph node mapping performed in this prospective sentinel lymph node study seems possible.
Another investigation by Eveno et al. also found an association between MSI and lymph node count in the examination of 135 patients with CRC stage I and II [13]. However, the strength of this conclusion is limited by the small number of MSI tumours in this prospective study (n = 11). More CRC patients (n = 332) with a higher number of microsatellite unstable tumours (n = 65) were included in the study conducted by Belt et al., which also saw an association between MSI phenotype and a greater frequency of “high” (defined in the study as >10 retrieved nodes) lymph node count [12]. Interestingly, this relationship was strongest in stage III tumours, contrasting to previous studies. However, the results are limited by the generally low lymph node counts in the investigation. In only 40.1% of the cases was a “high” lymph node count reported.
Reviewing the presented data, we found no significant association between MSI and adequate lymph node count (minimum of 12 assessable lymph nodes retrieved) in CRC, in contrast to previous reports by different groups. However, MSI seems to lead to a higher mean and median lymph node count in early UICC stages. The discrepancy between our results and previous studies is possibly due to higher lymph node counts. In comparison to the aforementioned studies, the 12 lymph node minimum for adequacy was achieved in over 80% of the total study cohort while in previous analyses, this ranged from 36 to 67%. This is also represented by a significantly higher median and mean number of retrieved lymph nodes.
In conclusion, our data refutes the claim that MSI-driven molecular mechanisms are the determining factor in lymph node retrieval in CRC. Based on improved lymph node retrieval, we saw differences in lymph node count between the proximal and distal colon, while the impact of MSI on the median and mean lymph node count was restricted to early UICC stages. Moreover, a location-specific analysis detected higher mean lymph node count only in stage I (pT1, pT2) microsatellite unstable CRC of the proximal colon. Thus, our data shows that the observed associations between MSI-H cancers and lymph node count are predominantly attributable to their preferential location in the proximal colon, where the number of lymph nodes is generally higher than in the distal colon and the rectum. Our results further suggest that the immunogenicity of MSI-H has an impact on the median and mean number of retrievable lymph nodes in early-stage CRC, where the immunologic response due to tissue destruction is low enough to not overshadow this effect.
References
Schmoll HJ, Van Cutsem E, Stein A, Valentini V, Glimelius B, Haustermans K, Nordlinger B, van de Velde CJ, Balmana J, Regula J, Nagtegaal ID, Beets-Tan RG, Arnold D, Ciardiello F, Hoff P, Kerr D, Kohne CH, Labianca R, Price T, Scheithauer W, Sobrero A, Tabernero J, Aderka D, Barroso S, Bodoky G, Douillard JY, El Ghazaly H, Gallardo J, Garin A, Glynne-Jones R, Jordan K, Meshcheryakov A, Papamichail D, Pfeiffer P, Souglakos I, Turhal S, Cervantes A (2012) ESMO consensus guidelines for management of patients with colon and rectal cancer. A personalized approach to clinical decision making. Ann Oncol 23(10):2479–2516. doi:10.1093/annonc/mds236
Benson AB 3rd, Venook AP, Cederquist L, Chan E, Chen YJ, Cooper HS, Deming D, Engstrom PF, Enzinger PC, Fichera A, Grem JL, Grothey A, Hochster HS, Hoffe S, Hunt S, Kamel A, Kirilcuk N, Krishnamurthi S, Messersmith WA, Mulcahy MF, Murphy JD, Nurkin S, Saltz L, Sharma S, Shibata D, Skibber JM, Sofocleous CT, Stoffel EM, Stotsky-Himelfarb E, Willett CG, Wu CS, Gregory KM, Freedman-Cass D (2017) Colon cancer, version 1.2017, NCCN clinical practice guidelines in oncology. J Natl Compr Cancer Netw 15(3):370–398
Sobin LH, Fleming ID (1997) TNM classification of malignant tumors, fifth edition (1997). Union Internationale Contre le cancer and the American Joint Committee on Cancer. Cancer 80(9):1803–1804
Gonsalves WI, Kanuri S, Tashi T, Aldoss I, Sama A, Al-Howaidi I, Ganta A, Kalaiah M, Thota R, Krishnamurthy J, Fang X, Townley P, Ganti AK, Subbiah S, Silberstein PT (2011) Clinicopathologic factors associated with lymph node retrieval in resectable colon cancer: a veterans’ affairs central cancer registry (VACCR) database analysis. J Surg Oncol 104(6):667–671. doi:10.1002/jso.21886
Baxter NN, Virnig DJ, Rothenberger DA, Morris AM, Jessurun J, Virnig BA (2005) Lymph node evaluation in colorectal cancer patients: a population-based study. J Natl Cancer Inst 97(3):219–225. doi:10.1093/jnci/dji020
Wright FC, Law CH, Last L, Khalifa M, Arnaout A, Naseer Z, Klar N, Gallinger S, Smith AJ (2003) Lymph node retrieval and assessment in stage II colorectal cancer: a population-based study. Ann Surg Oncol 10(8):903–909
Chou JF, Row D, Gonen M, Liu YH, Schrag D, Weiser MR (2010) Clinical and pathologic factors that predict lymph node yield from surgical specimens in colorectal cancer: a population-based study. Cancer 116(11):2560–2570. doi:10.1002/cncr.25032
Vather R, Sammour T, Kahokehr A, Connolly AB, Hill AG (2009) Lymph node evaluation and long-term survival in stage II and stage III colon cancer: a national study. Ann Surg Oncol 16(3):585–593. doi:10.1245/s10434-008-0265-8
Yada H, Sawai K, Taniguchi H, Hoshima M, Katoh M, Takahashi T (1997) Analysis of vascular anatomy and lymph node metastases warrants radical segmental bowel resection for colon cancer. World J Surg 21(1):109–115
Missiaglia E, Jacobs B, D’Ario G, Di Narzo AF, Soneson C, Budinska E, Popovici V, Vecchione L, Gerster S, Yan P, Roth AD, Klingbiel D, Bosman FT, Delorenzi M, Tejpar S (2014) Distal and proximal colon cancers differ in terms of molecular, pathological, and clinical features. Ann Oncol 25(10):1995–2001. doi:10.1093/annonc/mdu275
Berg M, Guriby M, Nordgard O, Nedrebo BS, Ahlquist TC, Smaaland R, Oltedal S, Soreide JA, Korner H, Lothe RA, Soreide K (2013) Influence of microsatellite instability and KRAS and BRAF mutations on lymph node harvest in stage I-III colon cancers. Mol Med 19:286–293. doi:10.2119/molmed.2013.00049
Belt EJT, te Velde EA, Krijgsman O, Brosens RPM, Tijssen M, van Essen HF, Stockmann HBAC, Bril H, Carvalho B, Ylstra B, Bonjer HJ, Meijer GA (2012) High lymph node yield is related to microsatellite instability in colon cancer. Ann Surg Oncol 19(4):1222–1230. doi:10.1245/s10434-011-2091-7
Eveno C, Nemeth J, Soliman H, Praz F, de The H, Valleur P, Talbot IC, Pocard M (2010) Association between a high number of isolated lymph nodes in T1 to T4 N0M0 colorectal cancer and the microsatellite instability phenotype. Arch Surg (Chicago, Ill: 1960) 145(1):12–17. doi:10.1001/archsurg.2009.224
Brenner H, Chang-Claude J, Seiler CM, Rickert A, Hoffmeister M (2011) Protection from colorectal cancer after colonoscopy: a population-based, case–control study. Ann Intern Med 154(1):22–30. doi:10.7326/0003-4819-154-1-201101040-00004
Bläker H, Hildebrandt B, Riess H, von Winterfeld M, Ingold-Heppner B, Roth W, Kloor M, Schirmacher P, Dietel M, Tao S, Jansen L, Chang-Claude J, Ulrich A, Brenner H, Hoffmeister M (2015) Lymph node count and prognosis in colorectal cancer: the influence of examination quality. Int J Cancer 136(8):1957–1966. doi:10.1002/ijc.29221
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, Meltzer SJ, Rodriguez-Bigas MA, Fodde R, Ranzani GN, Srivastava S (1998) A National Cancer Institute workshop on microsatellite instability for cancer detection and familial predisposition: development of international criteria for the determination of microsatellite instability in colorectal cancer. Cancer Res 58(22):5248–5257
Findeisen P, Kloor M, Merx S, Sutter C, Woerner SM, Dostmann N, Benner A, Dondog B, Pawlita M, Dippold W, Wagner R, Gebert J, von Knebel DM (2005) T25 repeat in the 3′ untranslated region of the CASP2 gene: a sensitive and specific marker for microsatellite instability in colorectal cancer. Cancer Res 65(18):8072–8078. doi:10.1158/0008-5472.can-04-4146
Sobin L, Wittekind C (2002) International Union Against Cancer: TNM: classification of malignant tumours, 6th edn. Wiley-Liss, New York
Ogino S, Nosho K, Irahara N, Meyerhardt JA, Baba Y, Shima K, Glickman JN, Ferrone CR, Mino-Kenudson M, Tanaka N, Dranoff G, Giovannucci EL, Fuchs CS (2009) Lymphocytic reaction to colorectal cancer is associated with longer survival, independent of lymph node count, microsatellite instability, and CpG island methylator phenotype. Clin Cancer Res 15(20):6412–6420. doi:10.1158/1078-0432.ccr-09-1438
Ogino S, Nosho K, Irahara N, Shima K, Baba Y, Kirkner GJ, Mino-Kenudson M, Giovannucci EL, Meyerhardt JA, Fuchs CS (2010) Negative lymph node count is associated with survival of colorectal cancer patients, independent of tumoral molecular alterations and lymphocytic reaction. Am J Gastroenterol 105(2):420–433. doi:10.1038/ajg.2009.578
MacQuarrie E, Arnason T, Gruchy J, Yan S, Drucker A, Huang WY (2012) Microsatellite instability status does not predict total lymph node or negative lymph node retrieval in stage III colon cancer. Hum Pathol 43(8):1258–1264. doi:10.1016/j.humpath.2011.10.002
Soreide K, Nedrebo BS, Soreide JA, Slewa A, Korner H (2009) Lymph node harvest in colon cancer: influence of microsatellite instability and proximal tumor location. World J Surg 33(12):2695–2703. doi:10.1007/s00268-009-0255-4
Brierley JD, Gospodarowicz MK, Wittekind C (2016) TNM classification of malignant tumours. Wiley
Merok MA, Ahlquist T, Royrvik EC, Tufteland KF, Hektoen M, Sjo OH, Mala T, Svindland A, Lothe RA, Nesbakken A (2013) Microsatellite instability has a positive prognostic impact on stage II colorectal cancer after complete resection: results from a large, consecutive Norwegian series. Ann Oncol 24(5):1274–1282. doi:10.1093/annonc/mds614
Morikawa T, Tanaka N, Kuchiba A, Nosho K, Yamauchi M, Hornick JL, Swanson RS, Chan AT, Meyerhardt JA, Huttenhower C, Schrag D, Fuchs CS, Ogino S (2012) Predictors of lymph node count in colorectal cancer resections: data from US nationwide prospective cohort studies. Arch Surg (Chicago, Ill: 1960) 147(8):715–723. doi:10.1001/archsurg.2012.353
Sanz-Pamplona R, Cordero D, Berenguer A, Lejbkowicz F, Rennert H, Salazar R, Biondo S, Sanjuan X, Pujana MA, Rozek L, Giordano TJ, Ben-Izhak O, Cohen HI, Trougouboff P, Bejhar J, Sova Y, Rennert G, Gruber SB, Moreno V (2011) Gene expression differences between colon and rectum tumors. Clin Cancer Res 17(23):7303–7312. doi:10.1158/1078-0432.ccr-11-1570
Vilar E, Gruber SB (2010) Microsatellite instability in colorectal cancer-the stable evidence. Nat Rev Clin Oncol 7(3):153–162. doi:10.1038/nrclinonc.2009.237
Schwitalle Y, Kloor M, Eiermann S, Linnebacher M, Kienle P, Knaebel HP, Tariverdian M, Benner A, von Knebel DM (2008) Immune response against frameshift-induced neopeptides in HNPCC patients and healthy HNPCC mutation carriers. Gastroenterology 134(4):988–997. doi:10.1053/j.gastro.2008.01.015
Dolcetti R, Viel A, Doglioni C, Russo A, Guidoboni M, Capozzi E, Vecchiato N, Macri E, Fornasarig M, Boiocchi M (1999) High prevalence of activated intraepithelial cytotoxic T lymphocytes and increased neoplastic cell apoptosis in colorectal carcinomas with microsatellite instability. Am J Pathol 154(6):1805–1813. doi:10.1016/s0002-9440(10)65436-3
Rossler O, Betge J, Harbaum L, Mrak K, Tschmelitsch J, Langner C (2017) Tumor size, tumor location, and antitumor inflammatory response are associated with lymph node size in colorectal cancer patients. Mod Pathol. doi:10.1038/modpathol.2016.227
Chen W, Swanson BJ, Frankel WL (2017) Molecular genetics of microsatellite-unstable colorectal cancer for pathologists. Diagn Pathol 12:24. doi:10.1186/s13000-017-0613-8
Acknowledgements
We kindly thank Jack Eaton, Institute of Pathology, Charité University Medicine Berlin for his editorial support, in the form of language editing.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Research involving human participants
All patients provided written informed consent prior to participation in the study. The study was approved by the responsible ethics committee of the University of Heidelberg and the medical boards of Baden–Wuerttemberg and Rhineland–Palatinate.
Funding
This was funded by the following:
- German Research Council. Grant Numbers: BR 1704/6-1, BR 1704/6-3, BR 1704/6-4 and CH 117/1-1
- German Federal Ministry of Education and Research. Grant Number: 01KH0404 and 01ER0814
- National Center for Tumour Diseases (NCT, Heidelberg, Germany; Interdisciplinary Research Program)
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Michael Hoffmeister and Hendrik Bläker shared senior authorship
Rights and permissions
About this article
Cite this article
Arnold, A., Kloor, M., Jansen, L. et al. The association between microsatellite instability and lymph node count in colorectal cancer. Virchows Arch 471, 57–64 (2017). https://doi.org/10.1007/s00428-017-2150-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00428-017-2150-y