Abstract
Background
To evaluate the changes in visual acuity, metamorphopsia, and thickness of retinal layers after epiretinal membrane (ERM) removal and to investigate factors associated with visual function.
Methods
This prospective study included 52 eyes of 52 patients who underwent surgery for idiopathic ERM. Changes in visual acuity, metamorphopsia score (M-score) using M-chart, and parafoveal thickness of each retinal layer were evaluated preoperatively and at 2-month and 6-month postoperative follow-up visits. Factors associated with visual acuity and M-score were investigated.
Results
Although continuous improvement in visual acuity and decrease in the thickness of parafoveal retinal layers following ERM removal was observed, relatively slow improvement in M-score was noted with values of 0.32 ± 0.27, 0.44 ± 0.46, and 0.23 ± 0.23, respectively at the defined time points. A preoperative increase in the thickness of parafoveal retina was mainly caused by increased thickness of inner retinal layers. Preoperative thickness of inner nuclear layer (INL) were closely associated with preoperative, postoperative visual acuity, and preoperative M-score (p = 0.001, 0.012, and 0.027, respectively).
Conclusions
Compared with the postoperative improvement in visual acuity, the postoperative improvement in metamorphopsia was a rather slow process. Parafoveal INL thickness was found to be a significant structural factor for visual acuity and metamorphopsia in ERM.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Removal of the epiretinal membrane (ERM) is a well-established surgical procedure for restoring visual function [1–6]. Factors including preoperative visual acuity [3–5], duration of symptoms [3, 4], preoperative lens status [3], occurrence of intraoperative complications [3], baseline profile of the internal limiting membrane [5], and the integrity of photoreceptor inner segment/outer segment line [5] may significantly influence postoperative visual acuity outcomes. Improvement in metamorphopsia after ERM removal has also been documented. However, the overall improvement in metamorphopsia was not prominent compared to that of visual acuity [7–11]. Although metamorphopsia is an important factor influencing the quality of life in patients with ERM [9], only a few studies have attempted to identify factors related to metamorphopsia and its temporal changes after surgery [10].
The recent development of spectral domain optical coherence tomography (SD-OCT), which provides faster imaging speed and higher resolution, allows more detailed retinal evaluation [12]. In particular, the resolution of SD-OCT images is high enough to delineate each retinal layer [13]. Recently published studies using SD-OCT have focused primarily on the association between visual acuity and the integrity of the photoreceptor layer [5, 14–17]. Only a few studies have evaluated thickness profiles of each retinal layer, and their possible influence on metamorphopsia [18, 19].
Although the possible association between inner nuclear layer (INL) thickness and visual function was suggested in these studies, the relationship between preoperative retinal thickness profile and postoperative visual outcomes has not yet been elucidated. Thus, metamorphopsia in patients with ERM, including the correlation with the thickness of each retinal layer merits further investigation.
The purpose of this study was to assess temporal changes in metamorphopsia and visual acuity after ERM removal, and to investigate the factors, including changes in the thickness of retinal layers, that might influence visual rehabilitation.
Material and methods
This prospective study was performed at a single center according to the tenets of the Declaration of Helsinki. The study was approved by the institutional review board and written informed consent was obtained from all patients before enrollment.
Patients who were diagnosed with idiopathic ERM and were scheduled for ERM removal between September 2009 and January 2011 were enrolled. If a patient had ERM in both eyes, only one eye with prior surgery was included in this study. Patients with any of the following conditions in the studied eye were excluded: evidence of ocular inflammation, diabetic retinopathy, hypertensive retinopathy and retinal vasculitis, media opacity that would influence visual acuity or preclude acquisition of clear SD-OCT images, presence of cataract judged to affect visual function, −6.0 diopters or more of spherical equivalent, prominent staphyloma, history of intraocular surgery other than uncomplicated cataract surgery, history of retinal detachment, other ocular diseases that may influence the macular microstructure or visual function, immeasurable fovea location on the SD-OCT image due to severe retinal contraction, and indistinct intraretinal structure on SD-OCT images. Additionally, patients who underwent combined ERM removal and cataract extraction less than 6 months follow-up after ERM removal, who had occurrence or progression of cataract after the surgery judged to affect visual function, or who experienced recurrence of ERM during the follow-up period were also excluded from the study. Normal fellow eyes of the subjects who underwent combined ERM removal and cataract extraction were selected as the normal control group for comparison of thickness of each retinal layers.
Each patient underwent a complete preoperative evaluation, including an examination for best-corrected visual acuity (BCVA) using the early treatment diabetic retinopathy study (ETDRS) chart (Lighthouse International, New York, USA), M-chart (Inami Co., Tokyo, Japan) test, anterior segment examination, and dilated fundus examination with a 90-diopter lens. Horizontal and vertical SD-OCT (Spectralis®, Heidelberg Engineering, Vista, USA) scans through the fovea were performed before ERM removal
Metamorphopsia score (M-score) measurement was performed according to a previously described method [9, 20, 21]. After wearing corrective lenses, patients were instructed to view the vertical line on the M-chart which was placed at a distance of 30 cm. The M-chart consists of 19 dotted lines with dot intervals ranging from 0.2° to 2.0° visual angle. When the patient recognized the dotted line on the chart as straight, the visual angle was considered to be the M-score. An increase in M-score means an increase in metamorphopsia severity. After finishing the test using a vertical line, the M-chart was rotated 90° and the same test was performed using a horizontal line. The mean M-score of horizontal and vertical line was used for analysis.
A three-port standard pars plana vitrectomy was performed by a single surgeon (S.W.K.) using a 23-gauge vitrectomy system, either Associate® (Dutch Ophthalmic Research Center. Inc., Zuidland, The Netherlands) or Accurus® (Alcon Laboratories Inc., Fort Worth, TX, USA), with one step scleral tunnel incision. Visualization of the fundus was achieved using a wide-angle viewing system. After core vitrectomy, induction of a posterior vitreous detachment was conducted using a 23-gauge angulated dissecting needle in cases without presence of a posterior vitreous detachment. The peeling of ERM and internal limiting membrane, approximately two disc diameter area centering at the foveal center was conducted in all eyes using vitreoretinal forceps. In most cases, internal limiting membrane was removed without the assistance of staining dye. Indocyanine green (ICG) dye was used to facilitate the removal of internal limiting membrane in some of the cases.
Postoperative measurement of BCVA and M-score and SD-OCT scannings were conducted at 2-month and 6-month follow-up visits.
All SD-OCT images were converted to gray scale for better visualization and then imported to Image J (National Institute of Health, Bethesda, USA) software for analysis. The thickness of each retinal layer was manually measured using calipers provided by the software.
We classified retinal layers for thickness measurement (Fig. 1) as follows: ganglion cell layer (GCL) + inner plexiform layer (IPL), INL, outer plexiform layer (OPL), outer nuclear layer (ONL), and photoreceptor layer (PRL). Because we experienced considerable intra-observer variability when measuring the thickness of the GCL and IPL separately, the thickness of the GCL + IPL was measured as a single unit. The total retinal thickness was defined as the sum of all five layers described above. In our pilot study, the location approximately 500 μm from the foveal center was the point most closest to the fovea in which all retinal layer thicknesses were clearly measurable. Thus, the parafoveal thickness of each retinal layer was measured at 500 μm and 600 μm in the superior, inferior, nasal, and temporal directions, from the foveal center (Fig. 1). Because ONL is usually thick at the fovea, the ONL thickness was used as a primary landmark to determine the location of the fovea. The thickness of each retinal layer was determined by agreement between two observers (J.H.K. and M.G.K.) and the mean of thickness measured at 500 μm and 600 μm was used for analysis. Differences in ETDRS BCVA and M-score between the preoperative visit and postoperative 6-month follow-up were defined as ΔBCVA and ΔM-score, respectively.
Depictions of thickness measurement points (left) and boundary of each retinal layer (right) evaluated in an eye with epiretinal membrane. GCL + IPL ganglion cell layer and inner plexiform layer; INL inner nuclear layer; OPL outer plexiform layer; ONL outer nuclear layer; PRL photoreceptor layer; ELM external limiting membrane
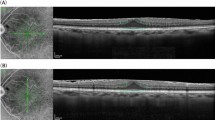
The integrity of the photoreceptor inner segment/outer segment (IS/OS) junction at the fovea was additionally evaluated based on SD-OCT images. A completely invisible or discontinuous IS/OS line was defined as a loss of integrity (Fig. 2).
Analyses were performed according to following categories.
General analysis for BCVA and M-score
Difference in BCVA and M-score were compared among the three time points; preoperative visit, 2-month, and 6-month follow-up. Associations between BCVA and M-score at the preoperative visit and the 6-month postoperative follow-up visit were evaluated. The association between ΔBCVA and ΔM-score was also investigated.
Subgroup analysis of the association between ΔBCVA and ΔM-score
Eyes with ten letters or more improvement in BCVA throughout the follow-up period were divided into two groups: 1) unchanged or increased M-score between the preoperative visit and 6-month postoperatively (except eyes exhibiting zero M-score at both the preoperative visit and the 6-month visit), 2) decreased M-score during the same period. The ΔBCVA of the two groups was compared.
Analysis when divided into four groups
Patients were divided into one of the four groups listed below according to preoperative BCVA and M-score.
-
Group A:
less than 70 letters of BCVA and 0.30 or more of M-score
-
Group B:
less than 70 letters of BCVA and less than 0.30 of M-score
-
Group C:
70 letters or more of BCVA and 0.30 or more of M-score
-
Group D:
70 letters or more of BCVA and less than 0.30 of M-score
The preoperative BCVA, BCVA at 6-month postoperatively, and ΔBCVA were compared among the four groups. The same comparisons were performed for M-score.
Analysis for changes in the parafoveal thickness of each retinal layer
Differences in the parafoveal thickness of each retinal layer were compared over the time points (preoperative visit, 2 months postoperatively, and 6 months postoperatively). In addition, the preoperative thicknesses of the studied eyes were compared with those of the normal eyes.
Analysis for the association between BCVA or M-score and possible influencing factors
The relationship between the integrity of the foveal photoreceptor IS/OS junction and BCVA or M-score were evaluated by dividing the patients into two groups based on the presence or absence of an intact photoreceptor IS/OS junction. Associations between preoperative structural variables and BCVA and M-score preoperatively, after 6 months of follow-up, ΔBCVA, and ΔM-score were analyzed. The following preoperative variables were assessed: central subfoveal thickness, thickness of GCL + IPL, INL, OPL, ONL, and PRL. The integrity of the foveal photoreceptor IS/OS junction was additionally included in multiple linear regression analysis.
Statistical analyses were performed using a commercially available software package (SPSS ver. 18.0 for Windows; SPSS Inc., Chicago, IL, USA). General analyses for BCVA and M-score were performed with repeated measures of analysis of variances (ANOVA) and univariate regression analysis. The influence of the integrity of the foveal photoreceptor IS/OS junction, difference in the thickness of each retinal layer between studied eyes and normal eyes, and subgroup analysis of eyes with ten letters or more improvement in BCVA were performed with independent samples t-test. Analyses of the four groups divided according to preoperative BCVA and M-score were performed using Kruskal Wallis test and Turkey test using ranks. Analysis for changes in the parafoveal thickness of each retinal layer during the follow-up period was performed using repeated measures ANOVA. Analyses of the relationship between possible influencing factors and BCVA or M-score were performed via univariate and stepwise multiple linear regression analyses. The influence of symptom duration on M-score was evaluated with univariate linear regression analysis. Bonferroni’s correction was additionally performed in the cases of multiple comparisons. A P-value less than 0.05 was considered significant.
Results
A total of 75 patients were diagnosed with idiopathic ERM and underwent uncomplicated ERM removal between September 2009 and January 2011. Among them, 52 eyes of 52 patients met the inclusion criteria. Twenty-three patients were excluded for various reasons: cataract progression, less than 6 months of follow-up, ERM recurrence, and inadequate quality of SD-OCT images. ICG dye-assisted internal limiting membrane removal was performed in two eyes (3.8 %).
Table 1 shows the clinical characteristics of the patients. The mean age at the time of the surgery was 62.1 ± 7.5 years (mean ± standard deviation, range 40 to 75 years) and the mean duration of symptoms was 15.8 ± 16.9 months (range, 2 to 60 months) in 37 eyes. The time of onset of visual symptoms could not be accurately estimated in the other 15 eyes. The mean preoperative BCVA and M-score were 68.8 ± 8.5 (range, 52 to 85 letters, Snellen equivalents: 20/40 [22]) and 0.32 ± 0.27 (range, 0.00 to 0.95), respectively. Figure 3 shows the changes in retinal microstructure after the surgery.
The BCVA measured at preoperative visit, 2 months postoperatively, and 6 months postoperatively were 68.8 ± 8.5, 73.9 ± 7.8, and 76.0 ± 7.2 letters, respectively (Fig. 4). The BCVA improved throughout the follow-up period (p < 0.001). The M-score measured preoperatively, and after 2 and 6 months of follow-up were 0.32 ± 0.27, 0.44 ± 0.46, and 0.23 ± 0.23, respectively (Fig. 4). Although the M-score between the preoperative visit and 2 months postoperatively was not significantly different (p = 0.117), the M-score at the 6-month postoperative follow-up visit was decreased compared to the preoperative value (p = 0.048). The association between the BCVA and M-score was not significant preoperatively or at 6 months postoperatively (p = 0.772, p = 0.615, respectively). The association between ΔBCVA and ΔM-score was also not significant (Fig. 5, p = 0.594).
Best-corrected visual acuity (BCVA) and M-score at preoperative visit, at postoperative 2 months follow-up, and at postoperative 6 months follow-up. Asterisks indicate statistically significant difference when tested by repeated measures analysis of variances with Bonferroni’s multiple comparison test
Scatterplot showing difference in best-corrected visual acuity (letters) and M-score between the preoperative visit and postoperative 6 months follow-up (ΔBCVA and ΔM-score). Note unchanged or even increased M-score in some eyes despite marked improvement in visual acuity (positive values indicate improvement in visual acuity or deterioration in metamorphopsia during the follow-up period)
Table 2 shows the results of analyses when patients were divided into four groups according to preoperative BCVA and M-score. Improvements in BCVA in the poor preoperative BCVA groups were +11.5 ± 3.2 and +11.7 ± 4.9 letters, respectively, whereas improvements in the good preoperative BCVA groups were +4.1 ± 5.2 and +2.5 ± 4.6 letters, respectively. Improvement in BCVA was noted in all four groups and more improvement in BCVA was noted in eyes with poor preoperative BCVA (p < 0.001). Improvement in M-score was noted in only in the high preoperative M-score groups. The improvement in M-score in the high preoperative M-score groups were −0.18 ± 0.19 and −0.32 ± 0.25, whereas deterioration in M-score by +0.06 ± 0.17 and +0.15 ± 0.19 were noted in the preoperative low M-score groups. When we analyzed 22 eyes that showed ten letters or more of postoperative improvement in BCVA, the ΔBCVA was significantly greater in eyes with unchanged or deteriorated M-score after surgery (p = 0.029).
In the analysis of 37 eyes in which symptom duration was verified, the associations between symptom duration and preoperative BCVA, BCVA at 6 months postoperatively, and ΔBCVA were not statistically significant (p = 0.163, p = 0.089, and p = 0.052, respectively). The associations between symptom duration and preoperative M-score, M-score at 6 months, and ΔM-score were also not significant (p = 0.175, p = 0.428, and p = 0.084, respectively).
Table 3 summarizes changes in the thickness of the parafoveal retinal layers following surgery. A significant decrease in thickness was noted in GCL + IPL, INL, and OPL after surgery, whereas the thickness of ONL and PRL was stable. Twenty-four eyes were enrolled as the normal control group for comparison of thickness in retinal layers. The age (mean 62.1 vs 64.5 years) and spherical equivalent refractive error (mean +1.46 vs +1.34 diopters) were not different between the studied eyes and normal eyes (p = 0.085 and p = 0.405, respectively). On preoperative examination, parafoveal thicknesses of GCL + IPL, INL, OPL, and ONL were significantly thicker in the studied eyes (Fig. 6, p < 0.01, p < 0.01, p < 0.01, and p = 0.03, respectively). The thicknesses of GCL + IPL, INL, OPL, and ONL in the studied eyes were 95.1 %%, 85.4 %, 43.1 %, and 17.3 % thicker than the thickness of the control eyes, respectively. The thicknesses of GCL + IPL, INL, and ONL at 6 months postoperatively were still significantly greater than those of the control eyes (p < 0.01, p < 0.01, and p < 0.01, respectively). The difference in PRL thickness was not significant at preoperative or postoperative examination (p = 1.000 and p = 1.000, respectively).
A diagram showing thickness of each retinal layer of studied eyes (n = 52) measured at preoperative visit and postoperative 6 months follow-up and thickness of each retinal layer of normal control eyes (n = 24). Asterisks indicate statistically significant difference when tested by independent samples t test with Bonferroni’s correction
The preoperative central subfoveal thickness, integrity of photoreceptor IS/OS junction, thickness of GCL + IPL, and INL were closely associated with preoperative BCVA (Table 4, p = 0.001, p = 0.033, p = 0.003, and p = 0.001, respectively). The central subfoveal thickness was also significantly associated with preoperative BCVA on multiple linear regression analysis (p = 0.001). The preoperative central subfoveal thickness, thickness of GCL + IPL, and INL were significantly associated with BCVA at 6 months on univariate linear regression analysis (Table 4, p = 0.032, p = 0.045, and p = 0.012, respectively). The thinner the respective layer was, the better BCVA was at 6 months postoperatively. The thickness of INL was found to have a significant association with BCVA at 6 months on multiple linear regression analysis (p = 0.012). There were no structural variables that were significantly associated with ΔBCVA. The thickness of GCL + IPL, INL, and the sum of the thicknesses of the six retinal layers were closely associated with preoperative M-score on univariate linear regression analysis (Table 4, p = 0.028, p = 0.027, p = 0.030, respectively). The preoperative INL thickness had the strongest association and was also significantly associated with preoperative M-score on multiple linear regression analysis (p = 0.027). No structural variables were significantly associated with M-score at 6 months postoperatively or ΔM-score.
Discussion
In this study, continuous improvement in visual acuity and continuous decrease in total parafoveal retinal thickness were noted throughout the follow-up period. The changes in these two parameters were more prominent during the first 2 months after the surgery. Results of analyses regarding the visual acuity were relatively comparable to previous studies. The preoperative central retinal thickness [5, 6, 16], and integrity of photoreceptor IS/OS junction [14, 16] was closely associated with preoperative visual acuity. Preoperative visual acuity also showed strong association with postoperative visual acuity outcome [3–5]. However, unlike previous studies [14, 15, 17], preoperative integrity of photoreceptor IS/OS junction was not significantly associated with postoperative visual acuity outcome. This discordant result would be caused by a difference in study design between our study and previous studies.
In this study, we quantified degree of metamorphopsia using M-chart. The M-chart which was introduced in 1999 by Shinoda and colleagues [23] is a simple method to quantify the degree of metamorphopsia. M-chart test is a reliable method with the intraindividual variation of within 0.1 score [20]. Previous studies demonstrated that M-chart is useful in measuring metamorphopsia in patients with ERM [20, 21], and it was well-correlated with severity of membrane proliferation and contraction [20, 21].
It is worthy of note that the mean M-score of our patients slightly deteriorated during the first 2 months. Although the amount of deterioration was not statistically significant compared to preoperative value, this is a notable finding because both improvement in visual acuity and decrease in parafoveal retinal thickness were observed in the same period. The cause of this deterioration of metamorphopsia in early postoperative period is uncertain. One possible explanation is retinal injury caused by peeling of internal limiting membrane. In this study, we performed peeling of internal limiting membrane in all cases. Although there are some debates, removing the internal limiting membrane during the surgery may contribute to regression of retinal fold [24] and prevention of recurrence of ERM [25, 26]. However, possible injuries to the underlying retina [27–29] which may induce poorer postoperative visual function are also documented [27, 30]. A potential negative influence of vitrectomy to the retinal function may be another explanation [31–37]. Elevated intraocular pressure or fluctuation in intraocular pressure [32], temperature [36] and composition [33, 34] of intraocular irrigation solution, phototoxicity by endoillimination [35, 37], and so on were suspected as causative factors.
It is notable that the deterioration of M-score was noted in low preoperative M-score groups (group B and D). However, the improvement in M-score was noted in high preoperative M-score groups (group A and C) and the amount of improvement was greatest in patients with better preoperative visual acuity (group C). This result indicates that the preoperative metamorphopsia is a reliable prognostic factor which predicts the amount of improvement in metamorphopsia following ERM removal. That is, poor M-score despite good vision (group C) merits the surgery for ERM removal. Relatively small amount of improvement in BCVA and great amount of deterioration in M-score in better preoperative visual acuity and M-score group (group D) is another notable finding. This result suggests that eyes with good visual acuities and minimal metamorphopsia should not have had ERM removal, or patients should be warned that their metamorphopsia can be worsened postoperatively.
Although both group A and C exhibited improvement in metamorphopsia, slightly less improvement was noted in poor preoperative BCVA group. It is possible that poor preoperative visual acuity itself indicates more profound impairment of visual function which may be responsible for limited recovery of metamorphopsia. However, according to the subgroup analysis with 22 eyes, eyes with unchanged or increased M-score showed significantly greater improvement in visual acuity. This result suggests that increase in visual acuity itself was partially responsible for postoperative deterioration in metamorphopsia. In spite of possible effect of surgical trauma, prominent postoperative improvement in visual acuity and normalization of thickness of retinal layers strongly indicate that ERM removal procedure do not actually worsens fundamental visual function in many cases. We suspect that many patients came to recognize distortion of lines postoperatively which was unrecognized in preoperative examination because of their poor preoperative visual acuity. In other words, subjective patient’s symptom can be worsened regardless of actual improvement in fundamental visual functions because they can see more clearly after the surgery.
In this study, we found that preoperative parafoveal macular thickening generally originated from thickening of inner retinal layers, including GCL, IPL, and INL. It is notable that preoperative thicknesses of GCL + IPL and INL showed close negative association with both preoperative visual acuity and degree of metamorphopsia. In addition, preoperative parafoveal INL thickness was found to be the strongest prognostic factor of postoperative visual acuity among the structural variables including central subfoveal thickness. All these findings indicate that dysfunction of inner retinal layers is closely related to visual dysfunction in patients with ERM and suggest that abnormalities in these layers, including thickness profile, should be carefully assessed when treating patients with ERM. However, it is possible that changes in thickness may not be responsible for visual acuity recovery. We hope further studies will reveal the association between changes in thickness and visual acuity recovery.
A positive association between preoperative INL thickness and preoperative M-score found in the current study was consistent with the result of a previous study [18, 19]. In addition, we found that the association of INL thickness was stronger than any of the structural variables, including central foveal thickness. The cellular origin of metamorphopsia associated with ERM has not yet been understood. The consistent result of our study and the previous study [19] strongly suggests that dysfunction of the cell bodies and/or disorganization of surrounding tissues in INL may be one of the important etiologies of metamorphopsia.
One of our primary purposes of this study was to reveal possible prognostic factors of postoperative metamorphopsia outcome. Only one factor, the preoperative M-score, was found to be closely associated with ΔM-score. That is, the poorer the preoperative M-score was, the greater the ΔM-score was. Although preoperative INL thickness was closely associated with preoperative M-score, postoperative M-score could not be predicted by any of the preoperative structural variables. Although it is possible that INL has a valid role on metamorphopsia in some aspect, the influence of INL thickness alone may not be as strong to compromise the effect of other factors. We think that development of metamorphopsia is a complicated process which influenced by various factors. In addition to retinal factors, the role of unknown physiology related to the visual construction process in the central nervous system may not be neglected. Thus, the effect of a single factor may not be great enough to show a significant result in statistical analyses. Although results of our study show that postoperative metamorphopsia outcome cannot be predicted by preoperative INL thickness, strong association between preoperative INL thickness and postoperative visual acuity found in our study suggests potential clinical usefulness of classification of ERM based on preoperative INL thickness.
ICG dye-assisted internal limiting membrane removal is a widely used technique. However, one concern is the potential toxicity of ICG dye on the retina [38, 39]. Although only a small proportion of our patients underwent ICG dye-assisted removal of the internal limiting membrane, possible influence of the dye toxicity on the results of the study may not be completely neglected.
One strength of this study is that, unlike previous studies [7–10, 18], we excluded all patients who had undergone combined cataract extraction. By eliminating the influence of preoperative cataract and postoperative pseudophakic macular edema, only the effect of ERM and ERM removal procedure was evaluated in this study. Another strength is that we measured visual acuity using ETDRS chart, assuring good reliability and low test–retest variability [40–43].
There are several limitations for this study. Because of the relatively short follow-up period of our patients, the result of this study may not be valid for patients with more than 6 months of long-term follow-up after ERM removal. In addition, although the onset of symptoms could be accurately estimated in approximately 71 % of the patients, the mean duration of symptoms was relatively long. Thus, some of our results may not be valid for patients with shorter duration of symptoms.
In summary, improvement in visual acuity and decrease in thickness of parafoveal retinal layers were noted throughout the 6 months follow-up after ERM removal. However, the improvement in metamorphopsia was a rather slow process, being detected after postoperative 2 months. The worse the preoperative value was, the larger extent of improvement was noted in the postoperative period in both visual acuity and metamorphopsia. However, eventual postoperative visual acuity was better in eyes with better preoperative visual acuity. This result indicates that both the preoperative visual acuity and preoperative degree of metamorphopsia are useful prognostic factors of postoperative visual outcome. Current study also indicates important role of inner retinal layer thickening on visual dysfunction in eyes with ERM. The preoperative INL thickness showed the strongest association with preoperative and postoperative visual acuity, and with preoperative metamorphosia as well. All these findings may provide useful information for predicting postoperative clinical course of visual rehabilitation and may help to select and monitor the candidate of surgery for ERM.
References
Grewing R, Mester U (1996) Results of surgery for epiretinal membranes and their recurrences. Br J Ophthalmol 80:323–326
Margherio RR, Cox MS Jr, Trese MT, Murphy PL, Johnson J, Minor LA (1985) Removal of epimacular membranes. Ophthalmology 92:1075–1083
Pesin SR, Olk RJ, Grand MG, Boniuk I, Arribas NP, Thomas MA, Williams DF, Burgess D (1991) Vitrectomy for premacular fibroplasia. Prognostic factors, long-term follow-up, and time course of visual improvement. Ophthalmology 98:1109–1114
Rice TA, De Bustros S, Michels RG, Thompson JT, Debanne SM, Rowland DY (1986) Prognostic factors in vitrectomy for epiretinal membranes of the macula. Ophthalmology 93:602–610
Falkner-Radler CI, Glittenberg C, Hagen S, Benesch T, Binder S (2010) Spectral-domain optical coherence tomography for monitoring epiretinal membrane surgery. Ophthalmology 117:798–805
Massin P, Allouch C, Haouchine B, Metge F, Paques M, Tangui L, Erginay A, Gaudric A (2000) Optical coherence tomography of idiopathic macular epiretinal membranes before and after surgery. Am J Ophthalmol 130:732–739
Bouwens MD, Van Meurs JC (2003) Sine Amsler Charts: a new method for the follow-up of metamorphopsia in patients undergoing macular pucker surgery. Graefes Arch Clin Exp Ophthalmol 241:89–93
Arndt C, Rebollo O, Seguinet S, Debruyne P, Caputo G (2007) Quantification of metamorphopsia in patients with epiretinal membranes before and after surgery. Graefes Arch Clin Exp Ophthalmol 245:1123–1129
Okamoto F, Okamoto Y, Hiraoka T, Oshika T (2009) Effect of vitrectomy for epiretinal membrane on visual function and vision-related quality of life. Am J Ophthalmol 147(869–874):874
Bouwens MD, de Jong F, Mulder P, van Meurs JC (2008) Results of macular pucker surgery: 1- and 5-year follow-up. Graefes Arch Clin Exp Ophthalmol 246:1693–1697
Ghazi-Nouri SM, Tranos PG, Rubin GS, Adams ZC, Charteris DG (2006) Visual function and quality of life following vitrectomy and epiretinal membrane peel surgery. Br J Ophthalmol 90:559–562
Nassif N, Cense B, Park BH, Yun SH, Chen TC, Bouma BE, Tearney GJ, de Boer JF (2004) In vivo human retinal imaging by ultrahigh-speed spectral domain optical coherence tomography. Opt Lett 29:480–482
Alam S, Zawadzki RJ, Choi S, Gerth C, Park SS, Morse L, Werner JS (2006) Clinical application of rapid serial fourier-domain optical coherence tomography for macular imaging. Ophthalmology 113:1425–1431
Mitamura Y, Hirano K, Baba T, Yamamoto S (2009) Correlation of visual recovery with presence of photoreceptor inner/outer segment junction in optical coherence images after epiretinal membrane surgery. Br J Ophthalmol 93:171–175
Oster SF, Mojana F, Brar M, Yuson RM, Cheng L, Freeman WR (2010) Disruption of the photoreceptor inner segment/outer segment layer on spectral domain-optical coherence tomography is a predictor of poor visual acuity in patients with epiretinal membranes. Retina 30:713–718
Michalewski J, Michalewska Z, Cisiecki S, Nawrocki J (2007) Morphologically functional correlations of macular pathology connected with epiretinal membrane formation in spectral optical coherence tomography (SOCT). Graefes Arch Clin Exp Ophthalmol 245:1623–1631
Suh MH, Seo JM, Park KH, Yu HG (2009) Associations between macular findings by optical coherence tomography and visual outcomes after epiretinal membrane removal. Am J Ophthalmol 147:473–480
Lim JW (2011) Results of spectral-domain optical coherence tomography by preferential hyperacuity perimeter in patients after idiopathic epiretinal membrane surgery. Curr Eye Res 36:364–369
Watanabe A, Arimoto S, Nishi O (2009) Correlation between metamorphopsia and epiretinal membrane optical coherence tomography findings. Ophthalmology 116:1788–1793
Matsumoto C, Arimura E, Okuyama S, Takada S, Hashimoto S, Shimomura Y (2003) Quantification of metamorphopsia in patients with epiretinal membranes. Investig Ophthalmol Vis Sci 44:4012–4016
Arimura E, Matsumoto C, Okuyama S, Takada S, Hashimoto S, Shimomura Y (2005) Retinal contraction and metamorphopsia scores in eyes with idiopathic epiretinal membrane. Investig Ophthalmol Vis Sci 46:2961–2966
Gregori NZ, Feuer W, Rosenfeld PJ (2010) Novel method for analyzing snellen visual acuity measurements. Retina 30:1046–1050
Shinoda K, Ishida S, Kawashima S, Matsuzaki T, Yamada K, Katsura H (1999) A new method for quantification of metamorphopsia in patients with epiretinal membrane. Nippon Ganka Gakkai Zasshi 103:806–810
Gaudric A, Fardeau C, Goberville M, Cohen D, Paques M, Mikol J (1993) Ablation of the internal limiting membrane, macular unfolding and visual outcome in surgery of idiopathic epimacular membranes. J Fr Ophtalmol 16:571–576
Park DW, Dugel PU, Garda J, Sipperley JO, Thach A, Sneed SR, Blaisdell J (2003) Macular pucker removal with and without internal limiting membrane peeling: pilot study. Ophthalmology 110:62–64
Kwok A, Lai TY, Yuen KS (2005) Epiretinal membrane surgery with or without internal limiting membrane peeling. Clin Exp Ophthalmol 33:379–385
Haritoglou C, Gandorfer A, Gass CA, Schaumberger M, Ulbig MW, Kampik A (2003) The effect of indocyanine-green on functional outcome of macular pucker surgery. Am J Ophthalmol 135:328–337
Konstantinidis L, Uffer S, Bovey EH (2009) Ultrastructural changes of the internal limiting membrane removed during indocyanine green assisted peeling versus conventional surgery for idiopathic macular epiretinal membrane. Retina 29:380–386
Tari SR, Vidne-Hay O, Greenstein VC, Barile GR, Hood DC, Chang S (2007) Functional and structural measurements for the assessment of internal limiting membrane peeling in idiopathic macular pucker. Retina 27:567–572
Uemura A, Kanda S, Sakamoto Y, Kita H (2003) Visual field defects after uneventful vitrectomy for epiretinal membrane with indocyanine green-assisted internal limiting membrane peeling. Am J Ophthalmol 136:252–257
Schatz P, Andreasson S (2010) Recovery of retinal function after recent-onset rhegmatogenous retinal detachment in relation to type of surgery. Retina 30:152–159
Kerrison JB, Haller JA, Elman M, Miller NR (1996) Visual field loss following vitreous surgery. Arch Ophthalmol 114:564–569
Anderson NJ, Edelhauser HF (1999) Toxicity of ocular surgical solutions. Int Ophthalmol Clin 39:91–106
Javaheri M, Fujii GY, Rossi JV, Panzan CQ, Yanai D, Lakhanpal RR, Maia M, Khurana RN, Guven D, De Juan E Jr, Humayun MS (2007) Effect of oxygenated intraocular irrigation solutions on the electroretinogram after vitrectomy. Retina 27:87–94
Miller SA, Landry RJ, Byrnes GA (2004) Endoilluminators: evaluation of potential retinal hazards. Appl Opt 43:1648–1653
Tamai K, Toumoto E, Majima A (1997) Local hypothermia protects the retina from ischaemic injury in vitrectomy. Br J Ophthalmol 81:789–794
van den Biesen PR, Berenschot T, Verdaasdonk RM, van Weelden H, van Norren D (2000) Endoillumination during vitrectomy and phototoxicity thresholds. Br J Ophthalmol 84:1372–1375
Ferencz M, Somfai GM, Farkas A, Kovacs I, Lesch B, Recsan Z, Nemes J, Salacz G (2006) Functional assessment of the possible toxicity of indocyanine green dye in macular hole surgery. Am J Ophthalmol 142:765–770
Engelbrecht NE, Freeman J, Sternberg P Jr, Aaberg TM Sr, Aaberg TM Jr, Martin DF, Sippy BD (2002) Retinal pigment epithelial changes after macular hole surgery with indocyanine green-assisted internal limiting membrane peeling. Am J Ophthalmol 133:89–94
Elliott DB, Sheridan M (1988) The use of accurate visual acuity measurements in clinical anti-cataract formulation trials. Ophthalmic Physiolog Opt 8:397–401
Ferris FL 3rd, Kassoff A, Bresnick GH, Bailey I (1982) New visual acuity charts for clinical research. Am J Ophthalmol 94:91–96
Blackhurst DW, Maguire MG (1989) Reproducibility of refraction and visual acuity measurement under a standard protocol. The Macular Photocoagulation Study Group. Retina 9:163–169
Raasch TW, Bailey IL, Bullimore MA (1998) Repeatability of visual acuity measurement. Optom Vis Sci 75:342–348
Meeting presentation
None.
Financial support
None.
Clinical trial registration ID
NCT01474655
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kim, J.H., Kang, S.W., Kong, M.G. et al. Assessment of retinal layers and visual rehabilitation after epiretinal membrane removal. Graefes Arch Clin Exp Ophthalmol 251, 1055–1064 (2013). https://doi.org/10.1007/s00417-012-2120-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00417-012-2120-7