Abstract
Objectives
The primary endpoint in trials of perioperative systemic therapy for urothelial carcinoma is 5-year overall survival (OS). A shorter-term endpoint could significantly speed the translation of advances into practice. We hypothesized that disease-free survival (DFS) could be a surrogate endpoint for OS in upper tract urothelial carcinoma (UTUC) patients treated with radical nephroureterectomy (RNU).
Patients and methods
The study included 2,492 patients treated with RNU with curative intent for UTUC.
Results
2/3-year DFS estimates were 78/73 %, and the 5-year OS estimate was 64 %. The overall agreements between 2- and 3-year DFS with 5-year OS were 85 and 87 %, respectively. Agreements were similar when analyzed in subgroups stratified by pathological stages, lymph node status, and adjuvant chemotherapy. The kappa statistic was 0.59 (95 % CI 0.55–0.63) for 2-year DFS/5-year OS and 0.64 (95 % CI 0.61–0.68) for 3-year DFS/5-year OS, indicating moderate reliability. The hazard ratio for DFS as a time-dependent variable for predicting OS was 11.5 (95 % CI 9.1–14.4), indicating a strong relationship between DFS and OS.
Conclusions
In patients treated with RNU for UTUC, DFS and OS are highly correlated, regardless of tumor stage and adjuvant chemotherapy. While significant differences in DFS, assessed at 2 and 3 years, are highly likely to persist in OS at 5 years, marginal DFS advantages may not translate into OS benefit. External validation is necessary before accepting DFS as an appropriate surrogate endpoint for clinical trials investigating advanced UTUC patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Radical nephroureterectomy (RNU) with excision of bladder cuff is the standard of care for patients with high-risk non-muscle-invasive and those with muscle-invasive upper tract urothelial carcinoma (UTUC) [1, 2]. Despite its durable long-term disease control in early-stage patients, the 5-year overall survival (OS) of patients with non-organ-confined UTUC is <50 %, and for those with nodal metastasis, it is only 35 % [3–5]. In patients whose disease is detected at a point where surgical cure is possible but risk of disease recurrence remains high (≥pT3 and/or positive lymph node metastasis), adjuvant therapy could reduce the likelihood of disease recurrence and lead to long-term improvements in OS [6]. One of the obstacles to trial accrual is the length of time it takes to reach 5-year OS, the typical endpoint for trials in urothelial carcinoma. Based on an analysis of individual patient data from 10 international centers, we previously established that the endpoint of disease-free survival (DFS), assessed after 2- or 3-year median follow-up, is a valid surrogate endpoint for 5-year OS in urothelial carcinoma of the bladder [7]. The goal of the current study, using data from 2492 patients treated with RNU for UTUC at 23 international centers, was to evaluate whether DFS with 2- or 3-year median follow-up is an appropriate surrogate endpoint for OS at 5 years. Moreover, we assessed whether the association between hazard ratios (HRs) based on DFS and OS was different in pathologic subgroups.
Materials and methods
Patient selection and data collection
This was an institutional review board (IRB)-approved study with all participating sites providing the necessary institutional data sharing agreements prior to initiation of the study. A total of 23 international centers provided data, which was submitted to a computerized databank. After combining the data sets, reports were generated for each variable to identify data inconsistencies and other data integrity problems. Through regular communication, resolution of all identified anomalies was achieved before analysis. Prior to final analysis, the database was frozen, and the final data set was produced.
The study population comprised 2,492 patients with UTUC who underwent RNU between 1987 and 2007. We excluded patients with a history of muscle-invasive urothelial carcinoma (UC) of the urinary bladder. Surgery was performed by surgeons according to the standard criteria for RNU, that is, extrafascial dissection of the kidney with the entire length of ureter and adjacent segment of the bladder cuff. The hilar and regional lymph nodes adjacent to the ipsilateral great vessel were generally resected if palpable intraoperatively or enlarged on preoperative axial imaging. The extent of lymphadenectomy performed was at the discretion of individual surgeons. No patient had neoadjuvant chemotherapy or radiotherapy. No patient had distant metastatic disease at the time of RNU.
Pathologic evaluation
All surgical specimens were processed according to standard pathologic procedures at each institution. Tumors were staged according to the 2002 American Joint Committee on Cancer–Union Internationale Contre le Cancer (AJCC/UICC) TNM classification [8]. Tumor grade was assessed according to the 1998 WHO/International Society of Urologic Pathology (ISUP) consensus classification [9].
Follow-up regimen
Patients were followed as previously described [10], generally every 3–4 months for the first year following RNU, every 6 months from the second through the fifth year, and annually thereafter. Follow-up consisted of a history, physical examination, routine blood work, urinary cytology, chest radiography, cystoscopic evaluation of the urinary bladder, and radiographic evaluation of the contralateral upper urinary tract. Elective bone scans, chest computerized tomography, or magnetic resonance imaging were performed when clinically indicated.
Disease recurrence was defined as tumor relapse in the operative field, regional lymph nodes, and/or distant metastasis. Occurrences of UC in the bladder or contralateral upper tract were not coded as disease recurrence. Cause of death was determined by treating physicians, by chart review corroborated by death certificates, or by death certificates alone [11]. To reduce bias in attribution of cause of death, only patients who had UC listed in the death certificate were considered to have died of UTUC for this study. All patients who were coded as dead of cancer had previous disease recurrence. Patients who died in the perioperative period (i.e., within 30 days of surgery) were censored at the time of death for UTUC-specific survival analyses.
Statistical analysis
Disease-free survival (DFS) and overall survival (OS) rates were calculated using the Kaplan–Meier method. DFS was defined as the duration from RNU to disease recurrence or death from any cause or loss of follow-up. Recurrence and survival were analyzed to investigate the individual levels of association between DFS at 2 years (DFS2) or 3 years (DFS3) with OS at 5 years (OS5) using Cox proportional hazards modeling [3, 7, 12]. The kappa statistic was calculated to determine agreement above that expected by chance. All tests were two-sided with a significance level set at 0.05. We performed an internal validation by the leave-one-out method for the three centers contributing the greatest number of patients (modified jackknife method). Statistical tests were performed using SAS version 9.2.
Results
Patient characteristics
Median patient age was 69.2 years (range 27–97). There were 1,681 men (67.5 %) and 811 women (32.5 %). Overall, 1618 (64.9 %) patients had pT2 or less disease [pT0 = 17 (0.7 %), pTa = 527 (21.2 %), pTis = 48 (1.9 %), pT1 = 553 (22.2 %), or pT2 = 473 (19.0 %)], 754 (30.3 %) with pT3 disease, and 120 (4.8 %) with pT4 disease. Of these patients, 597 (24.0 %) were lymph node negative, 222 (8.9 %) had positive lymph nodes, and 1673 (67.1 %) did not have a lymphadenectomy performed. Adjuvant chemotherapy was administered to 247 (9.9 %) of patients.
Outcomes after radical nephroureterectomy
Within a median follow-up of 46 months (interquartile range 24–79), 659 (26.4 %) patients experienced disease recurrence, 541 (21.7 %) died of disease, and 884 (35.5 %) died of all causes. Of the 659 patients who experienced disease recurrence, 541 (82.1 %) died of disease and 7 (1.1 %) died of other causes.
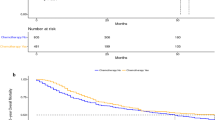
Two- and 3-year disease-free survival (DFS2/DFS3) rates were 78/73 % for all patients, 90/87 % for those with pT2 or less disease, and 55/49 % for those with pT3 or higher disease (Table 1). Of all disease recurrences, 79 % were within 2 years and 89 % within 3 years of RNU. Median time to disease recurrence was 55.8 months for pT2 or less and 30.8 months for pT3 or higher disease. Of patients with pT2 or less disease who experienced disease recurrence, 63.8 % experienced disease recurrence within the first 2 years versus 85.4 % of those with pT3 or higher-stage disease (p < 0.0001). Of patients with pT2 or less disease who experienced recurrence, 81.7 % recurred within the first 3 years versus 92.8 % of those with pT3 or higher disease (p < 0.0001). Of patients with pT3 or higher disease, 43 % experienced disease recurrence within the first year. Of patients with lymph node-positive disease who experienced disease recurrence, 93.3 % had disease recurrence within 2 years and 98.0 % within 3 years. The 5-year OS rate was 64 % for all patients, 76 % for those with pT2 or less, and 42 % for those with pT3 or higher disease (Fig. 1).
Association of 2- or 3-year DFS with 5-year OS
Within the first 36 months after RNU, DFS and OS curves had the same pattern (Fig. 1a). Median time from disease recurrence to death was 5.9 months (IQR 12). The overall agreement of DFS2 and DFS3 with OS5 was 85 % (IQR 82–88 %) and 87 % (IQR 85–90 %), respectively. Agreements were similar when analyzed in patients with pT2 or less disease [87 % (IQR 82–91 %) for DFS2/OS5 and 89 % (IQR 85–93 %) for DFS3/OS5] (Fig. 1b), and in those with pT3 or higher disease [80 % (IQR 76–85 %) for DFS2/OS5 and 83 % (IQR 78–86 %) for DFS3/OS5] (Fig. 1c). When examining only node-positive disease, the agreement of DFS2 and DFS3 with OS5 was 88 % (IQR 75–100 %) and 89 % (IQR 78–100 %), respectively. Categorizing patients by tumor stage revealed that patients with pT3 or higher disease were much more likely to experience disease recurrence (Fig. 2). Given the earlier recurrence and relatively high proportion of disease recurrence within the first year in pT3 or higher disease, we also examined the agreement of DFS within the first year (DFS1) with OS5 for this subgroup, which was 77 % (IQR 73–81 %).
There was no difference in the overall agreement rate when patients were categorized into those who received adjuvant chemotherapy [DFS2/OS5 87 % (IQR 80–94 %) and DFS3/OS5 87 % (IQR 79–100 %)] and those who did not [DFS2/OS5 85 % (IQR 81–89 %) and DFS3/OS5 86 % (IQR 83–90 %)]. The agreement was generally observed for DFS2 and DFS3 with OS5 at most of the contributing institutions as shown in Fig. 3. The kappa statistic was 0.59 (95 % CI 0.55–0.63) for DFS2/OS5 and 0.64 (95 % CI 0.61–0.68) for DFS3/OS5, indicating moderate agreement. The hazard ratio for DFS as a time-dependent variable for prediction of OS was 11.5 (95 % CI 9.13–14.42), indicating a strong relationship between DFS and OS.
We performed an internal validation by the leave-one-out method for the three centers contributing the greatest number of patients (modified jackknife method), which also supported the strong relationship between DFS and OS. These three centers were omitted from the analyses one at a time. The HRs for DFS as a time-dependent variable for prediction of OS for the three analyses were 13.0 (95 % CI 10.2–16.6), 10.8 (95 % CI 8.51–13.7), and 11.5 (95 % CI 9.03–14.7).
Discussion
UTUC is an uncommon and aggressive malignancy. RNU alone is often insufficient to assure long-term disease control in patients with UTUC. Multimodal therapy integrating systemic therapy may improve overall survival and quality of life of patients who have aggressive UTUC [6, 14]. Unfortunately, prospective clinical trials evaluating novel perioperative therapies require long-term follow-up in order to demonstrate improvement in OS, the standard primary endpoint for UC. This endpoint is problematic as it requires large resources (i.e., trial length) and failure to allow patients who fail therapy the opportunity to enroll into sequential trials. Identifying a surrogate endpoint that can be achieved more quickly than OS could improve trial design and accrual, leading to a higher rate of and faster completion of clinical trials [13]. This in turn would allow more rapid regulatory approval of agents and ultimately allow effective treatments to reach patients more quickly. In both colon and bladder cancers, 2- or 3-year DFS have been shown to be valid surrogate endpoints for 5-year OS [7, 12].
In an international cohort of 2,493 patients treated with RNU for UTUC, we found that DFS within a median of 2 or 3 years after surgery was a valid surrogate for OS at 5 years. Since most patients succumb to their disease recurrence, it has been suggested that extended follow-up could improve the association of DFS2 and DFS3 with OS. Moreover, establishing cancer-specific endpoints is important in UTUC patients as it is a disease of the elderly in whom competing causes of death take on a greater role as follow-up duration increases [15].
DFS at 2 and 3 years is the key endpoint regardless of stage and LN status. Exclusion of adjuvant chemotherapy did not affect the strength of the association between DFS2 and DFS3 with OS5. This overall agreement was confirmed with subgroup analysis reporting similar agreements comparing pT1-2–pT3-4 disease, and pN0 to pN+ disease.
Our study is limited by its retrospective and multicenter nature. An important limitation of this analysis is that it is based on only 2,492 patients. Analyses of surrogate endpoints with a limited number of patients are known to suffer from large variability in estimation. This was not the case in our study, and this cohort represents the largest cohort of UTUC patients and as such provides the best available evidence. To control for the impact of single high-volume center on the results, we performed an internal validation by the leave-one-out method for the three centers contributing more than 10 % of the total patients. Another limitation could lie in the application of our findings. For example, a trial where the agent being tested may have such a mechanism of action (delay as opposed to prevent recurrence), the use of short-term endpoints such as DFS must be carefully considered. Uncertainty in the impact of a therapy argues for a longer-term DFS endpoint, such as 3-year or even 4-year DFS as opposed to 2-year DFS. In addition, the endpoint must allow adequate time past the completion of a therapy to assess the delay versus prevention of recurrence hypothesis.
Conclusions
In this analysis of 2,492 international UTUC patients treated with RNU, we found that DFS assessed after 2- or 3-year median follow-up is a valid and appropriate primary endpoint. Indeed, 2- or 3-year median follow-up results accurately predicted OS results at 5 years. Interestingly, this correlation was independent of tumor stage, lymph node status, and adjuvant chemotherapy. However, while significant differences in DFS, assessed after 2 or 3 years, were highly likely to persist in OS after 5 years of follow-up, marginal DFS advantages may not translate into OS benefit. These findings together with those in bladder cancer [6], as well as the lengthy required follow-up and possible associated confounding for OS, support DFS as a potentially appropriate endpoint for adjuvant clinical trials in patients with UTUC treated with RNU. Nevertheless, external validation is necessary before integration of DFS as endpoint in clinical trials.
References
Margulis V, Shariat SF, Matin SF et al (2009) Outcomes of radical nephroureterectomy: a series from the Upper Tract Urothelial Carcinoma Collaboration. Cancer 15(115):1224–1233
Xylinas E, Rink M, Cha EK et al (2012) Impact of distal ureter management on oncologic outcomes following radical nephroureterectomy for upper tract urothelial carcinoma. Eur Urol (in press)
Abouassaly R, Alibhai SM, Shah N, Timilshina N, Fleshner N, Finelli A (2010) Troubling outcomes from population-level analysis of surgery for upper tract urothelial carcinoma. Urology 76:895–901
Jeldres C, Sun M, Isbarn H et al (2010) A population-based assessment of perioperative mortality after nephroureterectomy for upper-tract urothelial carcinoma. Urology 75:315–320
Roscigno M, Shariat SF, Margulis V et al (2009) Impact of lymph node dissection on cancer specific survival in patients with upper tract urothelial carcinoma treated with radical nephroureterectomy. J Urol 181:2482–2489
Hellenthal NJ, Shariat SF, Margulis V et al (2009) Adjuvant chemotherapy for high risk upper tract urothelial carcinoma: results from the Upper Tract Urothelial Carcinoma Collaboration. J Urol 182:900–906
Sonpavde G, Khan MM, Lerner SP et al (2011) Disease-free survival at 2 or 3 years correlates with 5-year overall survival of patients undergoing radical cystectomy for muscle invasive bladder cancer. J Urol 185:456–461
Greene FL (2002) American Joint Committee on Cancer, American Cancer Society. AJCC cancer staging manual, 6th edn. Springer, New York
Epstein JI, Amin MB, Reuter VR, Mostofi FK (1998) The World Health Organization/International Society of Urological Pathology consensus classification of urothelial (transitional cell) neoplasms of the urinary bladder. Bladder Consensus Conference Committee. Am J Surg Pathol 22:1435–1448
Cha EK, Shariat SF, Kormaksson M et al (2012) Predicting clinical outcomes after radical nephroureterectomy for upper tract urothelial carcinoma. Eur Urol 61(4):818–825
Rink M, Fajkovic H, Cha EK et al (2012) Death certificates are valid for the determination of cause of death in patients with upper and lower tract urothelial carcinoma. Eur Urol 61(4):854–855
Sargent DJ, Patiyil S, Yothers G et al (2007) End points for colon cancer adjuvant trials: observations and recommendations based on individual patient data from 20,898 patients enrolled onto 18 randomized trials from the ACCENT Group. J Clin Oncol 10(25):4569–4574
Green E, Yothers G, Sargent DJ (2008) Surrogate endpoint validation: statistical elegance versus clinical relevance. Stat Methods Med Res 17:477–486
Matin SF, Margulis V, Kamat A et al (2010) Incidence of downstaging and complete remission after neoadjuvant chemotherapy for high-risk upper tract transitional cell carcinoma. Cancer 1(116):3127–3134
Verhoest G, Shariat SF, Chromecki TF et al (2011) Predictive factors of recurrence and survival of upper tract urothelial carcinomas. World J Urol 29:495–501
Acknowledgments
We thank all members of the Upper Tract Urothelial Carcinoma Collaboration (UTUCC): Patrick J. Bastian, Thomas F. Chromecki, Mario Fernández, Vincenzo Ficarra, Wareef Kabbani, Eiji Kikuchi, Theresa M. Koppie, Casey K. Ng, Mototsuga Oya, Jean-Jacques Patard, Mesut Remzi, Marco Roscigno, Arthur I. Sagalowsky, Stefan Tritschler, Alon Weizer, Christopher G. Wood, Jean-Jacques Patard, Jeffrey Wheat, Matthias Waldert, Charles C. Guo, and Philipp Ströbel.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fajkovic, H., Cha, E.K., Xylinas, E. et al. Disease-free survival as a surrogate for overall survival in upper tract urothelial carcinoma. World J Urol 31, 5–11 (2013). https://doi.org/10.1007/s00345-012-0939-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00345-012-0939-5