Abstract
Pain catastrophizing is a maladaptive mechanism associated with the exaggerated experience of pain, increased rumination and feelings of helplessness. The main objective of this study was to explore whether increased pain catastrophizing is independently associated with a lower proportion of low disease activity (LDA) in rheumatoid arthritis (RA), psoriatic arthritis (PsA) and axial spondylarthritis (axSpA). Demographics, comorbidities, treatment, disease activity measures and patient-reported outcome data were recorded in RA, PsA and axSpA patients. Pain catastrophizing score (PCS) was assessed using a standardised questionnaire. For each diagnosis, composite disease activity scores with distinct cut-off values for LDA, i.e. DAS28-CRP (RA), DAPSA (PsA) and ASDAS-CRP (axSpA) were calculated and used as the dependent variable in logistic regression reflecting LDA achieved. A total of one thousand two hundred and twenty nine patients were included: 580 with RA, 394 with PsA and 255 with axSpA. In the multivariable analysis, pain catastrophizing was independently associated with LDA rates in axSpA (OR 0.33, 95% CI [0.12, 0.88]) amongst tested groups. In RA (OR 0.90, 95% CI [0.64, 1.28]) and PsA (OR 0.77, 95% CI [0.55, 1.07]), a statistically significant association was not observed. Higher PCS was independently associated with not achieving LDA in axSpA. Our data, however, indicate that pain catastrophizing, which also reflects a patient’s personality traits and coping abilities, plays a less important role for the patient than general pain perception.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The group of inflammatory joint disorders, which includes rheumatoid arthritis (RA), psoriatic arthritis (PsA), and axial spondyloarthritis (axSpA), carries a substantial burden for affected individuals and healthcare systems worldwide [1,2,3,4,5]. Our understanding of pathogenesis and the ongoing implementation of modern disease-modifying antirheumatic drugs (DMARDs) can decrease inflammation and disease activity and improve patient-related outcomes and quality of life [6,7,8]. Still, despite years of progress, some patients cannot achieve remission defined by cut-offs of composite disease activity scores e.g. DAS28 (Disease Activity Score 28) for RA, DAPSA (Disease Activity in PSoriatic Arthritis) for PsA or ASDAS (Ankylosing Spondylitis Disease Activity Score) for axSpA. These cohorts are often characterised by low inflammatory status [9].
From the patient’s perspective, pain seems to be a hallmark variable reflecting the burden of inflammatory joint disorders [10, 11]. Increasing evidence favours a multidimensional, biopsychosocial model of pain pathophysiology and underlines the contribution of emotional and cognitive processes to inter-individual differences in its experience and overall influence [12,13,14].
An essential factor in this consideration might be pain catastrophizing. Pain catastrophizing, a maladaptive trait, can be described as an individual’s tendency to define a pain experience in more excessive terms, associated with increased helplessness and rumination [15].
Its association with subjective disease burden e.g. pain characteristics but not with markers of inflammation that could be objectively measured was proven [16]. The current status of knowledge and previous analyses confirms the association of pain catastrophizing with pain severity, pain sensitivity, depression and disability [17,18,19]. Many pathways affecting different mechanisms that are not yet fully understood are considered as mediators of these effects [20,21,22,23].
Pain catastrophizing might be considered as a candidate trait to investigate factors associated with not achieving LDA or remission despite adequate pharmacological interventions targeting inflammation. Furthermore, it has been shown that an individual’s perception of disease and psychological status might reduce the probability of remission achieved in RA and PsA [24].
Our previous analysis of pain catastrophizing in rheumatic disorders revealed the prevalence of high pain catastrophizers ranging from 10.5 to 15.3% amongst RA, PsA and axSpA. This pattern is best explained by biological subjective measures and is associated with worse HRQoL [25]. To our knowledge, an extensive analysis of pain catastrophizing, in addition to demographic, treatment response and quality of life (QoL) variables, in relation to LDA or remission, has yet to be done to date. To better understand the current situation, we analysed whether increased pain catastrophizing is independently associated with not achieving LDA in patients with chronic inflammatory joint disorders.
Patients and methods
Materials and part of the methodology overlap with our previous publication concerning pain catastrophizing, based on the same study population. Thus, for detailed information regarding methodology, please refer to our last analysis [25].
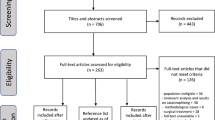
Patient recruitment was performed during routine evaluation at a Norwegian outpatient clinic in the period between 8 August 2018 (from this time point, a pain catastrophizing questionnaire was included in the database) and 25 February 2020 (date of data extraction).
In this cross-sectional study, included were RA patients who fulfilled the EULAR/ACR classification criteria [26], PsA patients fulfilling the CASPAR classification criteria [27] and axSpA patients fulfilling the ASAS classification criteria [28]. PsA patients with predominant axial manifestation were included in the PsA group (53 out of a total 394 PsA patients, 13.5%). Computer software GoTreatIT® Rheuma was used to facilitate gathering patient data and other clinically essential measures as a part of standard clinical care. In RA patients, a 28-joint count was performed as a routine assessment. PsA patients' joint assessment was done with a 66/68 joint count. At the clinical visits of axSpA patients, no routine joint assessment was performed. Data from the last visit were selected if multiple visits during the recruitment period occurred. When extracting data files from the clinical database, predefined queries were used and data were anonymised before analysis.
Data collection comprised a range of clinically significant variables, according to real-world evidence rules [29]. We evaluated markers of inflammation, such as erythrocyte sedimentation rate (ESR), C-reactive protein (CRP) serum level and clinical examination of the peripheral joint for RA (28 tender and swollen joint count) and PsA (28 tender and swollen joints and 68 tender and 66 swollen joint count).
Patient-reported outcome instruments (PROs) with global pain and fatigue were evaluated on a visual analogue scale (VAS, 0–100 mm) and a multidimensional health assessment questionnaire (MDHAQ) divided into functional and psychological parts. To analyse different aspects of HRQoL, we used a modified health assessment questionnaire (MHAQ). General patients' perception of disease burden was described using a patient global assessment (PGA). The evaluation of pain catastrophizing score remained the same as previously [25].
To describe achieved treatment goals, we applied universally used composite clinical activity measures of LDA with distinct cut-off values: DAS28 (CRP) ≤ 3.2 for RA, DAPSA ≤ 14.0 for PsA and ASDAS (CRP) < 2.1 for ax-SpA. All these measures were routinely calculated at outpatient visits.
The regional ethical committee approved this study (Regional etisk komite Midt-Norge 2010/3078) to analyse anonymised data from outpatient clinics in Norway. No patient consent was required, as all the data described above were gathered as part of clinical care to facilitate treatment decisions.
Statistical analysis
The data were processed using IBM SPSS 26 statistical software. Categorical variables were summarised using numbers and percentages. Continuous variables were presented as means with 95% confidence intervals (95% CI). Data density was displayed by presenting percentages of missing data regarding each variable in different diagnoses.
The distribution of our data, assessed using the Kolmogorov–Smirnov test and graphical methods, was non-homogenous; thus, we used non-parametric tests. When comparing between two groups, we utilised the Mann–Whitney statistics. Comparison between several groups was conducted using Kruskal–Wallis ANOVA with a post hoc test. To determine the associations between categorical variables, a chi-squared test was performed.
For each explored disease group, we sought to determine if PCS was independently associated with LDA rates using multivariable logistic regression and assessed model fit with Nagelkerke’s R-squared. Relying on clinical experience, we selected a set of variables to be used in the analysis, which included age, gender, BMI, years of education, ESR, working a paid job, reported fatigue VAS, reported global pain VAS, MHAQ, MDHAQ psychological domain and PCS. We wanted to diversify variables included in models emphasising patient-reported outcome measures and those related to psychological aspects of illness. LDA was calculated as described in the patients and methods section and was used as the dependent variable. We also confirmed our results using multivariable logistic regression with backwards elimination (remove at p value < 0.2; results not included in the main manuscript).
Also, the variation inflation factor (VIF) was calculated for variables in each model to exclude the presence of possible confounding variables or multicollinearity. We used VIF ≥ 4 as a cut-off value [30]. All VIFs in mentioned models did not exceed 4, thus excluding the existence of confounding variables.
A p value < 0.05 was considered to be statistically significant.
Results
A total of one thousand two hundred and twenty nine patients were included: 580 with RA, 394 with PsA and 255 with axSpA. The percentages of women were 66.7, 47.0 and 38.4%, in the RA, PsA and axSpA, respectively. The mean age of the study participants was 61.5, 54.4 and 47.5 years, respectively. Most axSpA patients were occupationally active or studying (paid job group), significantly more than in RA and PsA groups. Detailed information regarding demographics and treatment is presented in our previous publication.
Table 1 comprises characteristics of the study population including disease activity variables, patient-reported outcomes and comorbidity data with results of statistics comparing for significant differences. Amongst inflammatory parameters, ESR was significantly higher in RA than in other groups, but differences in CRP level were not unequivocal. The prevalence of LDA was obtained in 80.5% of the RA group, 67.7% in the PsA group and 50.6% in the axSpA group. These differences were all statistically significant when comparing diagnoses to each other.
When assessing patient-reported outcomes, a tendency to report higher global pain, worse patient global assessment, more fatigue and worse results of the psychological part of the MDHAQ questionnaire than in other diagnoses was observed in axSpA. There weren’t significant differences when comparing MDHAQ assessment of functional capacities and reported MHAQ across diagnoses. The mean (95% CI) score for pain catastrophizing was for RA 1.9 (1.8, 2.0), PsA 2.1 (1.9, 2.2) and axSpA 2.3 (2.1, 2.4). In a detailed analysis, there were statistically significant differences between axSpA and RA (p < 0.01) and between axSpA and PsA (p = 0.04). The difference was insignificant when comparing mean PCS in RA and PsA patients (p = 0.07).
The results of the multivariable logistic regression analysis, with LDA achieved as the dependent variable, are presented in Table 2. Higher global pain was shown to be a significant, independent obstacle in achieving LDA across all diagnoses. The obtained models revealed that other essential variables in that consideration reflected the quality of life measures, fatigue and inflammation, with a non-specific marker, ESR. A significant association between higher PCS and LDA rates was found only in axSpA (OR 0.33, 95% CI [0.12, 0.88]). In RA (OR 0.90, 95% CI [0.64, 1.28]) and PsA (OR 0.77, 95% CI [0.55, 1.07]), the results were not statistically significant. The R2 value of the obtained model was the highest in axSpA (R2 0.86).
Discussion
Our study demonstrates that pain catastrophizing, a subjective variable reflecting pain perception, was independently associated with not achieving LDA in axSpA patients, but not in RA and PsA cohorts. We argue that a maladaptive-related psychological factor such as pain catastrophizing might be responsible for not achieving low disease activity in axial SpA. This finding emphasises the significance of the multidimensional remission theory, incorporating the impact of non-inflammatory factors, as reported previously [31, 32].
Pain is a hallmark variable reflecting disease activity and burden in chronic inflammatory rheumatic disorders [33]. Its perception depends on an individual’s psychological traits and a wide variety of other factors, such as biological and social aspects. It derives from inflammatory or non-inflammatory causes and could be modulated in multiple ways, including neuropsychological. Different signalling pathways and molecules involved in pain perception reflect its complexity; thus, it is still difficult to clearly define its pathophysiology. Our results highlight the role of higher pain catastrophizing as one of the candidate factors for determining falsely increased axSpA activity when utilising composite measurements, which include patients’ assessment of pain. Our study shows that higher PCS is becoming an obstacle in achieving remission or low disease activity, especially in axSpA.
In the axSpA cohort, we found statistically higher reported global pain compared to RA and the highest mean pain catastrophizing score amongst the three diseases. This may indicate that pain perception between patients with axial and peripheral joint disorders might carry substantial differences. In our previous analysis of pain catastrophizing in rheumatic diseases, distinctive endotypes of patients with RA, PsA and axSpA who are prone to be high pain catastrophizers were suggested, with an emphasis on variables that were uniform in all three diseases, including younger age, fewer years of education, unemployment and more global pain [25]. This combination of traits is an unfavourable configuration in the context of the biopsychosocial hypothesis of pain genesis. A similar phenotype-based approach was explored previously in patients with common musculoskeletal disorders [34].
The prevalence of LDA was the lowest in axSpA in our analysis. Difficulties in achieving treat-to-target goals could be explained by more prominent psychological traits related to catastrophizing and interfering with disease activity. The reason why patients still feel inadequate or suffer from pain, despite low inflammation is an exciting field for further studies. EULAR recommendations, published by Nagy et al., focus on the definition of difficult-to-treat RA, underlining the specific phenotype of patients whose disease activity score is hampered by non-inflammatory conditions. This process leads to a high clinical burden not explained by objective signs of inflammation [35]. Also, Buch et al. introduced the term non-inflammatory refractory RA (NIRRA) and persistent inflammatory refractory RA (PIRRA) [36]. Our results are in line with these theories, trying to answer the question as to why some patients cannot achieve remission. These patients were treated adequately in our group, with the prevalence of biologics being 65.9% in axSpA, so other factors, unrelated to DMARD use, most probably interfered. To our knowledge, studies analysing difficult-to-treat axSpA and its causes have not been conducted so far.
Our results support the concept of non-inflammatory factors hindering remission in chronic inflammatory rheumatic diseases. Nevertheless, we did not find a significant association between PCS and LDA in the RA group. Overall, the priority of assessing psychological status in patients with inflammatory joint disorders, especially axSpA, needs to be underlined to develop better treatment options for refractory disease, considering the biopsychosocial model of pain and including the need for separate, non-anti-inflammatory treatments. In a recent study by Diab et al., web-based cognitive behavioural therapy was found to reduce reported pain intensity in musculoskeletal pain [37].
One more conclusion is evident despite the association between PCS and LDA in axSpA shown in this study. Amongst all diagnoses, reported global pain was independently associated with LDA. This indicates that a patient’s personality traits and coping abilities are less critical in the patient assessment than general pain perception. Each individual’s pain experience might also be modified by factors other than catastrophizing [38].
The strength of our study is its novelty, discovering that pain catastrophizing is a possible independent obstacle in achieving remission. So far, there have not been in-depth analyses of difficult-to-treat axSpA, and we hope our results could lead to a better understanding of this matter. The high density of data, variety of variables included and real-world evidence setting strengthen the results and conclusions achieved. Combining these features indicates high internal validity and advocates that the study population might reflect the ordinary outpatient clinic population. Also, because there are no indications that the study centre differs substantially from other outpatient clinics in Norway, the possible external validity for Norway is fairly good. Nevertheless, external validity may be limited due to population, lifestyle, healthcare and cultural differences in other countries. In a previous systematic review of studies comparing catastrophizing and pain beliefs amongst adults with chronic pain from 16 different countries, in the majority of cases, mean scores of catastrophizing were significantly different [39]. These results may indicate that cultural discrepancy and possibly other factors may affect the perception of disease burden and pain.
The systematic approach to the statistical methodology with multivariable logistic regression analyses, including the backwards-elimination procedure should be considered reliable in illuminating associations. Comparison of several inflammatory diseases in analyses is another strength and elucidates possible correlations and differences. Also, testing each model for possible multicollinearity and confounding variables augment obtained results. The logistic regression model obtained for axSpA, confirming the independent role of PCS, is highly valid, with a Nagelkerke’s R-squared value of 0.86.
A study limitation is a cross-sectional design, which allowed for exploring associations and not causality. Also, it seems that overall pain perception, which might be influenced by various factors, not only catastrophizing, plays a crucial role in general. Using patient-reported outcomes might have also posed a risk of bias. Still, we intended to analyse real-life data, and we argue that, due to the size of the analysed groups and the methodology of our study, we were able to provide reliable results. Also, the main subject was evaluated with a non-validated scale consisting of two questions. We intended to simplify data recording in large populations of patients in a real-life setting. Using a complete and validated scale would have provided more reliable information, but we are aware of various researches or clinical circumstances requiring the briefest possible assessment. The possible pitfall of our results is that disease refractory due to non-psychological reasons may cause higher catastrophizing.
In conclusion, higher pain catastrophizing was independently associated with LDA rates in axSpA, but not in the peripheral arthritis disorders, i.e. RA and PsA, suggesting differences in the impact of pain catastrophizing between axial and peripheral arthritis patients.
Availability of data and materials
The data underlying this article will be shared on reasonable request to the corresponding author and following ethical or other needed approval.
References
Mease PJ, Liu M, Rebello S et al (2019) Comparative disease burden in patients with rheumatoid arthritis, psoriatic arthritis, or axial spondyloarthritis: data from two corona registries. Rheumatol Ther 6:529–542. https://doi.org/10.1007/S40744-019-00172-9/FIGURES/2
Hsieh PH, Wu O, Geue C et al (2020) Economic burden of rheumatoid arthritis: a systematic review of literature in biologic era. Ann Rheum Dis 79:771–777. https://doi.org/10.1136/ANNRHEUMDIS-2019-216243
Krüger K, Burmester GR, Wassenberg S et al (2019) Patient-reported outcomes with golimumab in patients with rheumatoid arthritis, psoriatic arthritis, and ankylosing spondylitis: non-interventional study GO-NICE in Germany. Rheumatol Int 39:131–140. https://doi.org/10.1007/S00296-018-4180-4/FIGURES/6
Pilgaard T, Hagelund L, Stallknecht SE et al (2019) Severity of fatigue in people with rheumatoid arthritis, psoriatic arthritis and spondyloarthritis - results of a cross-sectional study. PLoS ONE 14:e021883. https://doi.org/10.1371/JOURNAL.PONE.0218831
Kerola AM, Kazemi A, Rollefstad S et al (2022) All-cause and cause-specific mortality in rheumatoid arthritis, psoriatic arthritis and axial spondyloarthritis: a nationwide registry study. Rheumatology (Oxford) 61:4656–4666. https://doi.org/10.1093/RHEUMATOLOGY/KEAC210
Chimenti MS, D’antonio A, Conigliaro P et al (2020) An update for the clinician on biologics for the treatment of psoriatic arthritis. Biologics 14:53–75. https://doi.org/10.2147/BTT.S260754
Janke K, Biester K, Krause D et al (2020) Comparative effectiveness of biological medicines in rheumatoid arthritis: systematic review and network meta-analysis including aggregate results from reanalysed individual patient data. BMJ 370:m2288. https://doi.org/10.1136/BMJ.M2288
Ho A, Younis I, Le QA (2022) Impact of biologics on health-related quality of life in patients with ankylosing spondylitis: a systematic review and meta-analysis of randomized controlled trials. Semin Arthritis Rheum 54:151996. https://doi.org/10.1016/J.SEMARTHRIT.2022.151996
Roodenrijs NMT, van der Goes MC, Welsing PMJ et al (2021) Difficult-to-treat rheumatoid arthritis: contributing factors and burden of disease. Rheumatology 60:3778–3788. https://doi.org/10.1093/RHEUMATOLOGY/KEAA860
Garrido-Cumbrera M, Hillmann O, Mahapatra R et al (2017) Improving the management of psoriatic arthritis and axial spondyloarthritis: roundtable discussions with healthcare professionals and patients. Rheumatol Ther 4:219. https://doi.org/10.1007/S40744-017-0066-2
Vergne-Salle P, Pouplin S, Trouvin AP et al (2020) The burden of pain in rheumatoid arthritis: Impact of disease activity and psychological factors. Eur J Pain 24:1979. https://doi.org/10.1002/EJP.1651
Bar-Shalita T, Cermak SA (2020) Multi-sensory responsiveness and personality traits predict daily pain sensitivity. Front Integr Neurosci 13:77. https://doi.org/10.3389/FNINT.2019.00077/BIBTEX
Bruce TO (2008) Comorbid depression in rheumatoid arthritis: pathophysiology and clinical implications. Curr Psychiatry Rep 10:258–264. https://doi.org/10.1007/S11920-008-0042-1
Sturgeon JA, Finan PH, Zautra AJ (2016) Affective disturbance in rheumatoid arthritis: psychological and disease-related pathways. Nat Rev Rheumatol 12:532. https://doi.org/10.1038/NRRHEUM.2016.112
Leung L (2012) Pain catastrophizing: an updated review. Indian J Psychol Med 34:204–217. https://doi.org/10.4103/0253-7176.106012
Hammer HB, Uhlig T, Kvien TK, Lampa J (2018) Pain catastrophizing, subjective outcomes, and inflammatory assessments including ultrasound: results from a longitudinal study of rheumatoid arthritis patients. Arthritis Care Res (Hoboken) 70:703–712. https://doi.org/10.1002/ACR.23339
Zhaoyang R, Martire LM, Darnall BD (2020) Daily pain catastrophizing predicts less physical activity and more sedentary behavior in older adults with osteoarthritis. Pain 161:2603–2610. https://doi.org/10.1097/J.PAIN.0000000000001959
Shim EJ, Hahm BJ, Go DJ et al (2018) Modeling quality of life in patients with rheumatic diseases: the role of pain catastrophizing, fear-avoidance beliefs, physical disability, and depression. Disabil Rehabil 40:1509–1516. https://doi.org/10.1080/09638288.2017.1300691
Galvez-Sánchez CM, Montoro CI, Duschek S, del Paso GAR (2020) Pain catastrophizing mediates the negative influence of pain and trait-anxiety on health-related quality of life in fibromyalgia. Qual Life Res 29:1871–1881. https://doi.org/10.1007/S11136-020-02457-X
Weissman-Fogel I, Sprecher E, Pud D (2008) Effects of catastrophizing on pain perception and pain modulation. Exp Brain Res 186:79–85. https://doi.org/10.1007/S00221-007-1206-7
Toledo TA, Kuhn BL, Payne MF et al (2020) The effect of pain catastrophizing on endogenous inhibition of pain and spinal nociception in Native Americans: results from the Oklahoma study of Native American pain risk. Ann Behav Med 54:575–594. https://doi.org/10.1093/ABM/KAAA004
Ferdek MA, Adamczyk AK, van Rijn CM et al (2019) Pain catastrophizing is associated with altered EEG effective connectivity during pain-related mental imagery. Acta Neurobiol Exp (Wars) 79:53–72. https://doi.org/10.21307/ane-2019-005
Ellingson LD, Stegner AJ, Schwabacher IJ et al (2018) Catastrophizing interferes with cognitive modulation of pain in women with fibromyalgia. Pain Med 19:2408–2422. https://doi.org/10.1093/PM/PNY008
Michelsen B, Kristianslund EK, Sexton J et al (2017) Do depression and anxiety reduce the likelihood of remission in rheumatoid arthritis and psoriatic arthritis? Data from the prospective multicentre NOR-DMARD study. Ann Rheum Dis 76:1906–1910. https://doi.org/10.1136/ANNRHEUMDIS-2017-211284
Wilk M, Łosińska K, Pripp AH et al (2022) Pain catastrophizing in rheumatoid arthritis, psoriatic arthritis and axial spondyloarthritis: biopsychosocial perspective and impact on health-related quality of life. Rheumatol Int 42:669–682. https://doi.org/10.1007/S00296-021-05070-4
Aletaha D, Neogi T, Silman AJ et al (2010) 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European league against rheumatism collaborative initiative. Ann Rheum Dis 69:1580–1588. https://doi.org/10.1136/ARD.2010.138461
Taylor W, Gladman D, Helliwell P et al (2006) Classification criteria for psoriatic arthritis: development of new criteria from a large international study. Arthritis Rheum 54:2665–2673. https://doi.org/10.1002/ART.21972
Rudwaleit M, van der Heijde D, Landewé R et al (2009) The development of assessment of spondyloarthritis international Society classification criteria for axial spondyloarthritis (part II): validation and final selection. Ann Rheum Dis 68:777–783. https://doi.org/10.1136/ARD.2009.108233
de Lusignan S, Crawford L, Munro N (2015) Creating and using real-world evidence to answer questions about clinical effectiveness. BMJ Health Care Inform 22:368–373. https://doi.org/10.14236/JHI.V22I3.177
Hair JF et al (2010) Multivariate data analysis: international version. Pearson, New Jersey
Brkic A, Łosińska K, Pripp AH et al (2022) Remission or not remission, that’s the question: shedding light on remission and the impact of objective and subjective measures reflecting disease activity in rheumatoid arthritis. Rheumatol Ther 2022:1–17. https://doi.org/10.1007/S40744-022-00490-5
Paulshus Sundlisæter N, Sundin U, Aga AB et al (2022) Inflammation and biologic therapy in patients with rheumatoid arthritis achieving versus not achieving ACR/EULAR Boolean remission in a treat-to-target study. RMD Open 8:e002013. https://doi.org/10.1136/RMDOPEN-2021-002013
Nowell WB, Gavigan K, Kannowski CL et al (2021) Which patient-reported outcomes do rheumatology patients find important to track digitally? A real-world longitudinal study in ArthritisPower. Arthritis Res Ther 23:53. https://doi.org/10.1186/S13075-021-02430-0
Meisingset I, Vasseljen O, Vøllestad NK et al (2020) Novel approach towards musculoskeletal phenotypes. Eur J Pain 24:921–932. https://doi.org/10.1002/EJP.1541
Nagy G, Roodenrijs NMT, Welsing PMJ et al (2021) EULAR definition of difficult-to-treat rheumatoid arthritis. Ann Rheum Dis 80:31–35. https://doi.org/10.1136/ANNRHEUMDIS-2020-217344
Buch MH, Eyre S, McGonagle D (2021) Persistent inflammatory and non-inflammatory mechanisms in refractory rheumatoid arthritis. Nat Rev Rheumatol 17:17–33. https://doi.org/10.1038/S41584-020-00541-7
Diab R, Bomar R, Slaven J et al (2022) Nurse-supported web-based cognitive behavioral therapy for chronic musculoskeletal pain: a randomized controlled trial. Pain Physician 25:E959–E968
Park SJ, Yoon DM, Yoon KB et al (2016) Factors associated with higher reported pain levels in patients with chronic musculoskeletal pain: a cross-sectional, correlational analysis. PLoS ONE 11:e0163132. https://doi.org/10.1371/JOURNAL.PONE.0163132
Sharma S, Ferreira-Valente A, Williams ACDC et al (2020) Group differences between countries and between languages in pain-related beliefs, coping, and catastrophizing in chronic pain: a systematic review. Pain Med 21:1847–1862. https://doi.org/10.1093/PM/PNZ373
Acknowledgements
Preliminary results of this study were reported at Annual European Congress of Rheumatology EULAR 2021 as oral abstract presentation in “The origins of pain in RMDs” session (02 June 2021) (http://dx.doi.org/10.1136/annrheumdis-2021-eular.3715). Manuscript proofreading was performed by Proof-Reading-Service.com Ltd, Devonshire Business Centre, Works Road, Letchworth Garden City, Hertfordshire, SG6 1GJ, United Kingdom.
Funding
No specific funding was received from any bodies in the public, commercial or not-for-profit sectors to carry out the work described in this article.
Author information
Authors and Affiliations
Contributions
MW, AHP, MK, GH: conceptualization, study design; GH: patients enrolment, data acquisition; MW, AHP, MK, GH: data analysis and interpretation; MW, AHP: statistical analyses; MW: drafting manuscript; AHP, MK, GH: revision of the manuscript. All authors have read and approved the final submitted version of the manuscript. All authors agreed to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Corresponding author
Ethics declarations
Conflict of interest
Mateusz Wilk: none declared; Are Hugo Pripp: none declared; Mariusz Korkosz: none declared; Glenn Haugeberg: Previous founder and shareholder in the company DiaGraphIT AS; manufacturing the GoTreatIT Rheuma computer tool used to collect data in this study.
Ethical approval
The approval for this study was given by the regional ethical committee (Regional etisk komite Midt-Norge 2010/3078) to analyse anonymised data from outpatient clinics in Norway. No consent from patients was needed according to the ethical committee, as all the data described above were collected as part of clinical care to facilitate treatment decisions.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Wilk, M., Pripp, A.H., Korkosz, M. et al. Exploring pain catastrophizing and its associations with low disease activity in rheumatic inflammatory disorders. Rheumatol Int 43, 687–694 (2023). https://doi.org/10.1007/s00296-023-05271-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-023-05271-z