Abstract
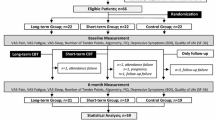
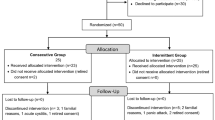
Objective: The aim of the present study is to evaluate the effectiveness of spa therapy in the management of fibromyalgia. Methods: Thirty women with fibromyalgia were randomly assigned to either a spa therapy group or a control group. The spa therapy group (n = 16) had spa treatment for 2 weeks in addition to their medical treatment. The control group (n = 14) continued to have their medical treatment and/or daily exercises. An investigator who was blinded for the intervention assessed all the patients for 9 months. Improvements in Fibromyalgia Impact Questionnaire (FIQ), pain and number of tender points were primary outcomes. Secondary outcome measures were improvement in sleep disturbance, fatigue, gastrointestinal symptoms, anxiety, Beck Depression Inventory and patient’s global evaluation. Results: the spa group was found to be superior to the control group at the end of intervention in terms of FIQ, pain, tender point count, fatigue and patients’ global assessment. This superiority remained for 6 months in FIQ, 1 month in pain and tender point count. Conclusion: It was concluded that the addition of spa therapy to medical therapy has both short- and long-term beneficial effects in female patients with fibromyalgia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fibromyalgia (FM) is characterised by chronic widespread pain, tender points, fatigue, non-refreshing sleep and morning stiffness [1]. Many patients with FM may also have concomitant psychiatric disorders, which could affect the intensity of their symptoms [2]. The American Collage of Rheumatology 1990 Fibromyalgia Classification Criteria are based on a history of chronic widespread musculoskeletal pain for at least 3 months and more than 11 painful tender points with palpation [3]. The prevalence of FM is 3.5% in the women population [4]. The aetiology of FM is unknown and the pathogenesis is not clearly understood.
There is no standard treatment regime for FM; therefore, current therapy modalities are focused on to relieve the symptoms of FM. Analgesics, antidepressants and exercise are widely used to relieve the symptoms. In the last decade, patient education [5, 6], multidisciplinary group programmes [7] and some other non-pharmacologic interventions [8] are becoming more important in the therapy.
Spa therapy is widely used for various rheumatic diseases in Turkey [9–11], in Europe [12–14] and Israel [15]. Balneotherapy is the original form of treatment, which is mainly applied in spa treatment courses.
In most of the spas in Turkey, balneotherapy is the main and sole intervention during the spa stay. Massage is also common in some spas. Certain studies published recently are providing some evidence of the effectiveness of balneotherapy in FM [16–20]. We aimed to compare the effect of spa therapy with that of medical treatment that is commonly prescribed in patients with FM.
Patients and methods
Patients
The patients with FM were recruited from the Musculoskeletal Disorders Outpatient Clinic of Department of Medical Ecology and Hydroclimatology, Istanbul Medical Faculty. The diagnoses of the patients were made according to American Collage of Rheumatology 1990 criteria [3]. The patients were 20–60 years old, and they did not have any other condition that might affect the study results in terms of their clinical and laboratory evaluation. Laboratory tests used for patient evaluation included complete blood count, erythrocyte sedimentation rate, C reactive protein level, glycaemia, hepatic and renal function tests, thyroid stimulant hormone level and X-ray. The patients had not taken balneotherapy in the previous year, and had not had any changes in their pharmacological therapy during the previous 2 months. Current treatment regimes of the patients at the beginning of the study are shown in Table 1. Thirty women with FM were enrolled in the study and their written informed consents were obtained. The patients were randomised using a computer-generated random number list by an independent investigator, and allocated to either the spa therapy or the control arms of the study (16/14). The patients allocated to the control group were assured that they would have a spa course in the following year.
Interventions
The patients in Group I (16) were transported to Balçova Spa Centre, Izmir, and stayed there for 2 weeks. Spa therapy consisted of thermal pool baths (at 36±1°C for 20 min) every day (except Sundays), and pressured shower with thermal water (at 37°C for 15 min) or classical massage (15 min) every other day alternately. The thermal water used in balneotherapy contains primarily sodium, chlorine, bicarbonate and fluoride. The patients also continued with their regular medications for FM during the spa therapy.
The patients in the control group (14) were advised to continue to have their medication “as is”; the researchers made no modification to the treatment regimes.
After randomisation, one patient was withdrawn from the study because of her daughter’s illness.
Assessments
All the patients were assessed before and at the end of the spa therapy course (2nd week), and at the 1st, 3rd, 6th and 9th months after the spa therapy. The same investigator, who was blinded for the study arms, performed all assessments.
Measurements
Pain, total number of tender points and Fibromyalgia Impact Questionnaire (FIQ) were selected as primary outcome measures since tender point count and FIQ are well-documented and widely-used measures in FM therapy studies. Pain is the main symptom of FM, and pain relief is expected as a result of spa therapy.
A 10-cm visual analogue scale (VAS) was used for the evaluation of pain intensity (0 indicates no pain whereas 10 is the worst).
The point pressure threshold was measured with a dolorimeter (Pain, Diagnostic and Thermograph, Inc., Great Neck, NY) by an investigator who was blinded to the intervention groups. Eighteen points were evaluated according to ACR 1990 classification criteria [3].
All patients were required to complete the FIQ. FIQ is a ten-item questionnaire that measures physical functioning, work status, depression, anxiety, sleep, pain, stiffness, fatigue and well-being. Higher scores indicate greater impairment [21]. FIQ is a widely recommended tool in FM research. The Turkish translation of the FIQ was found to be valid [22].
Improvements in certain FM-related symptoms, namely sleep problems, fatigue, gastrointestinal symptoms and anxiety, were considered as secondary outcome measures. The intensity of these symptoms and global assessment of the patient were assessed using the 10-cm VAS. Scale 0 indicates no symptom whereas 10 is the worst.
The patients were also required to complete the Beck Depression Inventory (BDI). BDI is a measure for self-reported depression that consists of 21 items (range 0–63) where higher scores indicate greater depression [23].
Statistical analysis
Age and duration of symptoms were given as mean and standard deviation, whereas study data were represented as median (minimum and maximum). Due to the distribution characteristics, the data were evaluated using non-parametric statistical methods. Comparison of several paired groups (baseline and follow-up measurements) was performed using Friedman’s test. Independent groups were compared using Mann–Whitney U test. All statistical calculations were performed by using a microprocessor and commercially-available statistical software packages. Alpha value was set to 0.05 in all calculations, and calculated p value less than 0.05 was accepted as statistically-significant.
Results
The demographic characteristics and the treatment regimes of the patients are summarised in Table 1. No statistically-significant difference between the groups was observed at the beginning of the study.
Primary outcome measures
Fibromyalgia Impact Questionnaire
The patients in the spa therapy arm showed significant improvements in follow-up evaluations up to the 9th month as compared to the baseline (Table 2). However, no significant improvement during the follow-up period was observed in the control group (Table 3). It was observed that the spa therapy arm was superior at the end of treatment (2nd week), 1st and 6th months, in terms of FIQ score alteration from the baseline (Table 4).
Pain
During the follow-up, pain was significantly less severe up to 9 months in the spa arm as compared to the baseline (Table 2). In the control group, significantly-lower pain measurement as compared to the baseline was found in the assessments at 6 and 9 months (Table 3). VAS-score alterations were also superior in the spa therapy arm at the end of therapy and 1st month measurements (Table 4).
Tender point count
Tender point counts are significantly decreased, as compared to the baseline, and remained low up to the 3rd month measurement in the spa therapy group (Table 2). However, no decrease was observed in the control group in terms of tender point count (Table 3). The decrease in tender point count in the spa therapy group was significantly greater than the control group at the end of the therapy and 1st month measurements (Table 4).
Secondary outcome measures
Patient’s global assessment, fatigue and BDI measurements in the spa therapy group were found to be significantly better than the baseline values during the follow-up period in the spa therapy group. Favourable changes were also observed in sleep disturbance (except at 3rd month) and in anxiety (except at 3rd and 9th months) during the follow-up period. However, no significant improvement could be observed in gastrointestinal symptoms (Table 2).
In the control group significant improvements were observed during the follow-up period in sleep disturbance (except in the 2nd week measurement) and in the patients’ global assessment (except in the 2nd week and 3rd month measurements). There were also a few significant improvements in BDI (3rd and 6th months), fatigue (6th and 9th months) and anxiety (9th month). There was no significant change in the gastrointestinal symptoms (Table 3).
According to the secondary outcome measures, the spa group was superior to the control group in terms of patients’ global evaluation and fatigue in the 2nd week assessment (Table 4).
Discussion
Our study data indicate that the addition of spa treatment to commonly-prescribed medical treatment is beneficial in patients with FM in several aspects, such as improving FIQ, relieving pain and decreasing tender point count. These beneficial effects may persist up to 9 months in most cases and variables. Findings of the present study are in agreement with the other studies published previously. These studies show significant differences in terms of study design and duration.
In another study, Yurtkuran et al. investigated the effect of the addition of balneotherapy to relaxation exercises in patients with FM [16]. The study was conducted in a daily living environment and the study duration was 2 weeks. Pain relief, as measured by VAS-score, was achieved (except at the end of therapy assessment in control group) in both groups at the end of therapy and remained for 6 weeks; however, significant improvements in mean pressure algometrical scores during the follow-up were observed only in the balneotherapy group.
Evcik et al. found that 3-week balneotherapy application in daily living conditions decreased FIQ, pain and number of tender points at the end of therapy and at the 6-month follow-up evaluations in FM patients as compared to controls [19]. The results of this study are comparable with our results; however, improvement in the tender point count lasts longer in their study. Use of different study designs may cause the observed nuances.
Altan et al. reported improvements in FIQ, pain intensity, tender point count and patient’s global evaluation in FM patients receiving balneotherapy three times a week in a thermal pool for 12 weeks [24]. Improvements persisted for 12 weeks when considering FIQ, and 24 weeks when considering pain intensity, tender point count and patient’s global evaluation. The balneotherapy application period in this study is somehow unusual when compared to classical studies; however, end of therapy and 12th week results are comparable with the results of our study and other studies.
In a published study, patients in the control groups were requested to stay in the spa centre as well as the study patients, without having balneotherapy, for 10 days [18]. It was found that disease symptoms were improved in both groups in the 3-month follow-up examination,whereas significant decrease in pain intensity and tender point counts were observed only in the study group.
Although the present study is primarily designed to depict the overall efficacy of spa therapy in patients with FM, it also gives some clues to explain the underlying mechanisms that may produce the intended outcomes of balneotherapy.
Heat and buoyancy effects of the thermal pool help to reduce muscle spasm. The decrease of the muscle tonus may increase the pain threshold in the nerve endings. Gate-control theory in pain perception may provide an explanation of the pain-relieving effect of balneotherapy. Body surface is stimulated by heat and hydrostatic pressure of water in the thermal pool. These stimuli decrease the pain sensation in the affected individual.
During thermomineral water immersion, peripheral vasodilatation occurs through the effects of water temperature and chemical components. Vasodilatation may help to relieve pain by removing algesic metabolites from the environment. It is known that applied heat decreases muscle tonus, increases connective tissue stretching and pain threshold at the free nerve endings.
The observations on the effects of thermomineral baths on beta-endorphin levels are controversial. It has been reported that beta-endorphin levels increase during a thermomineral bath [25], whereas it has also been reported that a 3-week balneotherapy course did not affect plasma beta-endorphin levels in osteoarthritis patients [26].
As Tubergen suggested, certain non-specific variables in the spa environment, such as environmental change, pleasant scenery, being in a non-competitive atmosphere with fellow patients and the absence of work duties, may have beneficial effects in addition to the specific treatment modalities in patients with FM [27].
We consider that the observed beneficial effects in our study are provided through the various mechanisms mentioned above. Individual effects of balneotherapy and non-specific variables of the spa environment may both play a role in the achievement of clinical improvements in our study group.
In conclusion, spa therapy is found to be effective in FM patients. Beneficial effects are observed both in the short and the long term. There is a need for further randomised and controlled studies to verify these results, and to identify whether spa therapy is cost effective in FM.
References
Goldenberg DL (1998) Fibromyalgia and related syndromes. In: Klippel JH, Dieppe PA (eds) Rheumatology, 2nd edn. Mosby, London
Oran Ö, Dönmez A, Erdogan N, Turan M (2002) Psychiatric co-morbidity affects of symptoms of fibromyalgia. Phys Med Rehabil Kuror 12:284–287
Wolfe F, Smyte HA, Yunus MB, Bennett RM, Bombardier C, Goldenberg DL, Tugwell P, Campbell SM, Abeles M, Clark P et al (1990) The American Collage of Rheumatology 1990 criteria for classification of fibromyalgia: report of the multicentre criteria committee. Arthritis Rheum 33:160–172
Wolfe F, Ross K, Anderson J, Russell IJ, Hebert L (1995) The prevalence and characteristics of fibromyalgia in the general population. Arthritis Rheum 38:19–28
Burchardt CS, Bjelle A (1994) Education programmes for fibromyalgia patients: description and evaluation. Baillieres Clin Rheumatol 8:935–956
Brückle W, Bornmann M, Weber H (1997) Patientenschulung bei Fibromyalgie. Akt Rheumatol 22:92–97
Bennet RM (1996) Multidisciplinary group programs to treat fibromyalgia patients. Rheum Dis Clin North Am 22:351–367
Sprott H (2003) What can rehabilitation interventions achieve in patients with primary fibromyalgia? Curr Opin Rheumatol 15:145–150
Karagülle MZ, M Karagülle (2004) Balneotherapie und Kurorttherapie rheumatischer Erkrankungen in der Türkei: Ein systematischer Review. Forsch Komplementärmed Klass Naturheilkd 11:33–41
Dönmez A, Karagülle Z, Turan M (1995) Balneotherapie mit Akratoterme bei Gonartrose. Zeitschrift Naturamed 7:20–23
Odabaşı E, Karagulle MZ, Karagulle M, Turan M, Karagülle O (2002) Comparison of two traditional spa therapy regimens in patients with knee osteoarthritis. Phys Med Rehabil Kuror 12:337–341
Kovacs I, Bender T (2002) The therapeutic effects of Cserkeszölö thermal water in osteoarthritis of knee: a double blind, controlled, follow up study. Rheumatol Int 21:218–221
Bender T, Karagülle Z, Bálint GZ, Gutenbrunner Chr, Bálint PV, Sukenik S (2004) Hydrotherapy, balneotherapy, and spa treatment in pain management. Rheumatol Int 25:220-224
Van Tubergen A, Landewe R, van der Heijde D, Hidding A, Wolter N, Asscher M, Falkenbach A, Genth E, The HG, van der Linden S (2001) Combined spa–exercise therapy is effective in patients with ankylosing spondylitis: a randomized controlled trial. Arthritis Rheum 45:430–438
Sukenik S, Buskila D, Neuman L, Kleiner-Baumgarten A, Zimlichman S, Horowitz J (1990) Sulphur bath and mud pack treatment for rheumatoid arthritis in the Dead Sea area. Ann Rheum Dis 49:99–102
Yurtkuran M, Çeliktaş M (1996) A randomized, controlled trial of balneotherapy in the treatment of patients with primary fibromyalgia syndrome. Phys Rehabil Kur Med 6:109–112
Neuman L, Sukenik S, Bolotin A, Shakra MA, Amir M, Flusser D, Buskila D (2001)The effect of balneotherapy at the Dead Sea on the quality of life of patients with fibromyalgia. Rheumatol Int 20:15–19
Buskila D, Shakra MA, Neumann L, Odes L, Shneider E, Flusser D, Sukenik S (2001) Balneotherapy for fibromyalgia at the Dead Sea. Rheumatol Int 20:105–108
Evcik D, Kızılay B, Gökcen E (2002) The effects of balneotherapy on fibromyalgia patients. Rheumatol Int 22:56–59
Şen U, Karagülle MZ, Karagülle M, Dönmez A, Şen C (2002) Comparison of the efficacy of two different traditional spa regimens in patients with fibromyalgia syndrome. PTT Hastanesi Tıp Dergisi 24:78–81
Burckhardt CS, Clark SR, Bennet RM (1991) The Fibromyalgia Impact Questionnaire: development and validation. J Rheumatol 18:728–733
Sarmer S, Ergin S, Yavuzer G (2000) The validity and reliability of the Turkish version of the Fibromyalgia Impact Questionnaire. Rheumatol Int 20:9–12
Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J (1961) An inventory for measuring depression. Arch Gen Psychiatry 4:561–571
Altan L, Bingöl Ü, Aykaç M, Koç Z, Yurtkuran M (2003) Investigation of the effects of pool-based exercise on fibromyalgia syndrome. Rheumatol Int 24:272-277
Kubota K, Kurabayashi H, Tamura K, Kawada E, Tamura J, Shirakura T (1992) A transient rise in plasma beta-endorphin after a traditional 47 degrees C hot-spring bath in Kusatsu-spa, Japan. Life Sci 51:1877–1880
Yurtkuran M, Ulus H, Irdesel J (1993) The effect of balneotherapy on plasma endorphine level in patient with osteoarthritis. Phys Rehabil Kur Med 3:130–132
van Tubergen A, Hidding A (2002) Spa and exercise treatment in ankylosing spondylitis: fact or fancy? Best Pract Res Clin Rheumatol 16:653–666
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Dönmez, A., Karagülle, M.Z., Tercan, N. et al. SPA therapy in fibromyalgia: a randomised controlled clinic study. Rheumatol Int 26, 168–172 (2005). https://doi.org/10.1007/s00296-005-0623-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00296-005-0623-9