Abstract
Purpose
The aim of this study was to determine whether a complex surgical procedure such as peri-acetabular osteotomy could be safely learnt by using a programme involving mentoring by a distant expert. To determine this, we examined the incidence of intra-operative complications, the acetabulum correction achieved, the late incidence of re-operation and progressive degenerative arthritis.
Methods
Between 1992 and 2004, peri-acetabular osteotomy was performed in 26 hips in 23 patients. The median follow-up was ten (5–17) years. The median age of the patients at operation was 28 (14–41) years. Clinical outcomes were reported and radiographic results were determined by an independent expert.
Results
There were no intra-articular osteotomies, sciatic nerve injuries, hingeing deformities or vascular injuries. There was one ischial nonunion. The lateral centre-edge angle improved from a median 4° pre-operatively to 25°. One revision osteotomy, one osteectomy and three total hip replacements were required, two for progression of osteoarthritis.
Conclusions
The programme of mentoring was successful in that there was a low incidence of the major intra-operative complications that are often reported during the learning curve period and the acetabular corrections achieved were similar to the originators.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
What little information there is suggests that a programme of mentoring assists senior surgeons in learning new complex surgical procedures, but this mentoring was undertaken in the surgeon’s local environment [3, 6]. For experienced surgeons in practice who are remote from centres with special expertise and who treat relatively uncommon problems requiring complex surgery, the mentoring process might need to be undertaken differently.
Acetabular osteotomy is a complex, but relatively infrequent operation for treating dysplasia of the hip in young adults. One such osteotomy is the Bernese peri-acetabular osteotomy (PAO) which offers several important advantages over other osteotomies used to reorientate the acetabulum [7, 23, 27, 28].
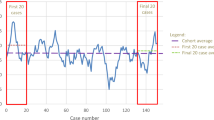
Because the advantages of PAO are increasingly appreciated, surgeons will wish to adopt this relatively new, albeit complex technique, but will often be operating in areas distant from centres with expertise in PAO and without the opportunity to learn the technique under direct supervision. This causes two problems. First, because of the technical difficulties and challenges associated with this technique [7], including using a single anterior approach and performing a so-called blind ischial osteotomy without visualising the ischium, there is a well-reported learning curve period, thought to include the first 20 or so osteotomies, during which complications may be common [1, 2, 4, 5, 7, 12, 18, 19, 28]. Second, because the need for this procedure arises relatively infrequently, it is difficult for a surgeon to maintain the knowledge and surgical expertise necessary to undertake such a procedure with consistently good results. These problems are likely to lead to difficulties and likely contribute to the not infrequent and sometimes major complications reported after PAO, including intra-articular osteotomy, sciatic nerve palsy, femoral artery or nerve damage, inadequate osteotomy and resultant hingeing of the acetabulum rather than rotation, ischial fracture and subsequent nonunion, and under- or overcorrection of the acetabulum.
To reduce the risk of complications during the learning curve, the first author (DWH) began a structured programme of learning from an experienced mentor, the developer of the technique (RG), and was able to learn the surgical technique in a staged manner, discuss cases pre-operatively and review results with the mentor. Because of concerns about undertaking a blind ischial osteotomy without direct supervision, the first author initially used a posterior and anterior double surgical approach [25], the posterior approach allowing direct visualisation of the retro-acetabular surface and protection of the sciatic nerve [13].
The aim of this study was to determine if PAO could be safely learnt by using a structured programme of mentoring. To determine this, we examined the incidence of intraoperative complications, the acetabular correction achieved and the late incidence of re-operation and progressive degenerative arthritis.
Materials and methods
Between August 1992 and December 2004, PAO was performed in 26 hips in 23 patients. There were 11 hips in nine patients in the double approach group and 15 hips in 14 patients in the single approach group. The median age of the patients at surgery was 27 years (14–36) and 28 years (14–41), respectively. There were two men (two hips) and eight women (nine hips) in the double approach group and six men (seven hips) and eight women (eight hips) in the single approach group.
The indication for surgery was hip dysplasia in patients presenting with pain from the hip joint. The degree of dysplasia was classified preoperatively as Severin III in nine hips and Severin IV in 17 hips [22]. In the single approach group one hip had Perthes-like changes of the femoral head with grade IV dysplasia and one hip had grade IV dysplasia due to muscle imbalance from polio. Five cases had undergone previous surgery. In the double approach group, one hip had a previous shelf procedure and another a Salter innominate osteotomy. In the single approach group, one had a femoral osteotomy, one a Salter innominate osteotomy and later a shelf procedure, and one a femoral osteotomy combined with a Sharrad iliopsoas transfer. In the double approach group, three of the hips had concurrent femoral osteotomies at the time of PAO. In the single approach group, six hips had femoral neck osteoplasty undertaken via anterior arthrotomy at the time of PAO and two hips had a combined PAO and transtrochanteric hip dislocation and osteoplasty. All the surgeries were performed by the first author (DWH).
In collaboration with the originator of the procedure, RG, a mentoring programme was developed to learn PAO and to continue monitoring results. This programme included repeated visits to Berne to observe surgeries in the operating room and participation in cadaver surgeries to further develop the double approach. From the first PAO (Fig. 1a, b), cases were discussed pre-operatively, usually by email with the mentor, and post-operative radiographs were forwarded for his review. Further visits to Berne occurred approximately every 2 years and cases were also discussed at international meetings. During the study period the surgeon was tutored by another surgeon from Berne and coauthor (MB) who was working with and trained by the originator of the procedure.
The double approach included first undertaking a small posterolateral approach, with the patient in the lateral decubitus position [11] followed by an anterior approach using the technique described by the originators [7]. Image intensification was not used. Repeat intra-operative plain radiographs of the pelvis were used to confirm the correction. This was defined as a lateral centre-edge (LCE) angle of approximately 25–30° [27], an acetabular index (AI) of 0–5°, but importantly not negative, and medialisation comparable to a normal opposite side or close to the ilioischial line. In the early PAOs, the importance of not retroverting the acetabulum was not appreciated nor was the risk of anterior impingement. Later, care was taken to avoid retroversion and a femoral neck osteochondroplastic trimming was undertaken. The double approach was used to become familiar with the technique for the first 11 cases. A single approach was then used for the remaining 15 cases. An osteotomy of the greater trochanter with intra-articular debridement and trochanteric advancement was undertaken in combination with a PAO in two hips and in these cases the opportunity was taken to undertake an ischial osteotomy under direct vision by exposing the ischium as described above. A capsulotomy was performed routinely after the fourth single approach case and labral and femoral neck pathology was treated if present and accessible. The osteotomies were internally fixed according to the technique of Ganz [7]. Patients were partial weight-bearing for 8 weeks following surgery. No ectopic bone chemoprophylaxis was used.
Radiographic evaluations were undertaken on an anteroposterior (AP) pelvic and a false profile view [14]. Lateral and anterior coverage were measured using the LCE angle [29], the anterior centre-edge (ACE) angle [14] and the AI [26]. Lateralisation of the femoral head was measured and compared to the opposite side of normal and an extrusion score was calculated. A value of greater than 1 indicates a lateralised centre of rotation and a value less than 1 a medialised centre of rotation compared to the contralateral side [10]. The version of the acetabulum was assessed according to Siebenrock et al. [24] and Reynolds et al. [20]. The degree of osteoarthritis pre-operatively and at latest review was graded according to the criteria of Tönnis [26]. All radiographs were independently evaluated by MB, who trained with the originator of the procedure, to eliminate bias and lack of expertise in interpretation of radiographs.
One patient died at one year following surgery but this was unrelated to the surgery. The median duration of follow-up of surviving patients was 13 years (range 10–17) for the double approach group and eight years (range 5–14) for the single approach. Of the surviving hips, 19 were reviewed by clinical examination and two had initial clinical examination, and later telephone interview and questionnaire. Patients were prospectively reviewed clinically and radiographically at regular post-operative intervals. Doctor and patient questionnaires were completed to derive the Harris hip [9] and pain scores.
Results
Complications were few. There were no intra-articular osteotomies, sciatic nerve injuries, vascular injuries or hingeing deformities. There was one ischial nonunion in the single approach group. There was one temporary femoral nerve palsy that fully recovered in a patient who had undergone multiple previous pelvic and femoral operations for a polio affected hip and who had no iliopsoas.
There were five re-operations. Three total hip replacements were undertaken, in one hip with grade 2 osteoarthritis present before PAO, in one hip with grade 1 osteoarthritis and major cartilage damage present before PAO and in one hip replaced elsewhere for impingement, but with no osteoarthritis. One hip underwent repeat osteotomy because poor resolution intra-operative radiographs led to initial undercorrection and another hip underwent resection of part of the ilium adjacent to the site of a previous shelf operation.
For the double approach series the median LCE, ACE and AI angles improved from 5° pre-op (−18 to 22°) to 26° post-op (14 to 50°); −2° pre-op (−45 to 18°) to 25° post-op (−5 to 41°); 26° pre-op (12 to 45°) to 6° post-op (−18 to 19°) and in the single approach from 4° pre-op (−10 to 22°) to 24° post-op (10 to 39°); 2° pre-op (−15 to 18°) to 30° post-op (20 to 54°); 28° pre-op (11 to 35°) to 8° post-op (−3 to 13°). The corrections achieved by using the double and single approach were similar when compared to the initial Berne series [23] with the single approach series showing closer grouping of radiographic measurements around the normal value.
There was an improvement in the lateralisation index of the femoral head to a median of 1.00 (0.62 to 1.21) for the double approach which did not change if the two preoperative moderate osteoarthritis cases were excluded (1.00, 0.62 to 1.06) and 1.11 (0.78 to 1.34) for the single approach.
In the double approach series the version was neutral in four at pre-op and three at post-op, retroverted in three at pre-op and three at post-op and anteverted in four at pre-op and five at post-op. In the single approach series the version was neutral in eight at pre-op and ten at post-op, retroverted in three at pre-op and five at post-op and anteverted in four at pre-op and none at post-op.
At latest radiographic review, the degree of osteoarthritis did not progress in 19 hips, in 15 it remained grade 0 and in three it remained grade 1. Excluding the replaced hips, osteoarthritis progressed from grade 0 to 1 in one hip, from grade 1 to 2 in one hip, from grade 1 to 3 in one hip and from grade 2 to 3 in one hip.
The median Harris hip and pain scores preoperatively were 57 (29–88) and 20 (0–40) and at last follow-up were 80 (41–97) and 40 (10–44).
Discussion
The low incidence of intra-operative complications demonstrates that a complex surgical procedure such as PAO can be learnt and the surgical expertise maintained by using a structured programme of mentoring by an expert, despite the expert being remote and despite the complex procedure being undertaken infrequently.
There is a well-reported learning curve period for PAO, thought to include approximately the first 20 osteotomies [2, 5, 7, 12, 18, 19, 28] during which major surgical complications are not uncommon. The use of the double approach [11, 25] in the initial osteotomies may have contributed to the low incidence of major complications. In particular, complications of joint injury, complete ischial osteotomy, ischial fracture and nerve injury previously reported were avoided [1, 4, 5, 12, 19, 23]. A disadvantage of the double approach is the 1.5 h of extended surgery time [11]. The disadvantage of the extended operative time may adversely affect decision-making because the procedure is physically and mentally demanding on the surgeon.
The PAOs undertaken initially through a double approach and subsequently through a single approach achieved correction of deformity comparable to those of the originator of the procedure [7]. In this study, correction of the dysplasia using the double and single approach, as measured by the different angles, corresponded well with the data of the original authors [7, 23] and others [2, 4, 8, 16, 18, 19, 27]. With experience, increasing awareness of the importance of the correction is mirrored in the finding that in the single approach group the radiographic results for the LCE, ACE and AI angles were more closely grouped around the normal values.
There were three hips that underwent total hip replacement. The surgery for one of these hips was undertaken elsewhere and for symptoms suggestive of impingement, despite there being a well-preserved hip joint. There is now increased awareness of avoiding retroversion [15, 24, 28, 30] and femoroacetabular impingement after PAO [17, 24] and the current surgical approach at PAO often involves an additional femoral neck osteoplasty. The second revised hip pre-operatively had grade 2 osteoarthritis and had an aspheric femoral head that did not permit a congruent joint after the correction, factors now known to be associated with poorer outcomes [2, 16, 21, 23, 27]. The third revised hip pre-operatively had grade 1 osteoarthritis but also had major cartilage damage present before PAO and continued to degenerate.
This study has demonstrated the success of a mentoring technique for senior surgeons remote from centres of expertise. Complications were minimised and the capacity to undertake this surgery infrequently was maintained. Important aspects of the mentoring process need to be encouraged by surgical societies and professional bodies including the importance of society meetings, the ability to visit clinics and attend and scrub in at surgery, opportunities to supplement texts, movies and video clips with anatomical dissection and cadaver surgery and finally, the opportunity and time for the expert to provide advice and monitor progress. Finally, the learning surgeon’s results should be reviewed by an expert and regularly audited.
In summary, a process of mentoring by a distant expert surgeon over more than a decade has allowed a complex surgical procedure to be safely learnt and surgical expertise maintained in a remote centre. Such an approach is an important method of learning complex surgery when prolonged exposure and training under direct supervision is not practicable, a not uncommon situation for senior surgeons faced with the challenge of adopting a new surgical procedure.
References
Biedermann R, Donnan L, Gabriel A, Wachter R, Krismer M, Behensky H (2008) Complications and patient satisfaction after periacetabular pelvic osteotomy. Int Orthop 32:611–617
Clohisy JC, Barrett SE, Gordon JE, Delgado ED, Schoenecker PL (2005) Periacetabular osteotomy in the treatment of severe acetabular dysplasia. J Bone Joint Surg Am 87(2):254–259
Cook A, Khoury A, Bagli D, McLorie GA, El-Ghoneimi A, Farhat WA (2005) The development of laparoscopic surgical skills in pediatric urologists: longterm outcome of a mentorship-training model. Can J Urol 12(5):2824–2828
Crockarell J Jr, Trousdale RT, Cabanela ME, Berry DJ (1999) Early experience and results with the periacetabular osteotomy. The Mayo Clinic experience. Clin Orthop Relat Res 363:45–53
Davey JP, Santore RF (1999) Complications of periacetabular osteotomy. Clin Orthop Relat Res 363:33–37
Farhat W, Khoury A, Bagli D, McLorie G, El-Ghoneimi A (2003) Mentored retroperitoneal laparoscopic renal surgery in children: a safe approach to learning. BJU Int 92(6):617–620
Ganz R, Klaue K, Vinh TS, Mast JW (1988) A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res 232:26–36
Garras DN, Crowder TT, Olson SA (2007) Medium-term results of the Bernese periacetabular osteotomy in the treatment of symptomatic developmental dysplasia of the hip. J Bone Joint Surg Br 89(6):721–724
Harris WH (1969) Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty. An end-result study using a new method of result evaluation. J Bone Joint Surg Am 51(4):737–755
Heyman CH, Herndon CH (1950) Legg-Perthes disease; a method for the measurement of the roentgenographic result. J Bone Joint Surg Am 32(4):767–778
Hussell JG, Mast JW, Mayo KA, Howie DW, Ganz R (1999) A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res 363:64–72
Hussell JG, Rodriguez JA, Ganz R (1999) Technical complications of the Bernese periacetabular osteotomy. Clin Orthop Relat Res 363:81–92
Lazennec JY, Mora Valladares N, Laudet CG, Barabas D, Ramare S, Hansen S, Guerin-Surville H, Saillant G (1998) Anatomic bases of a new technique of juxta-acetabular osteotomy. Technical principles and performance. Surg Radiol Anat 20(3):153–159
Lequesne M, de Sèze S (1961) Le faux profil du bassin. Nouvelle incidence radiographique pour l’étude de la hanche. Son utilité dans les dysplasies et les differentes coxopathies. Rev Rhum Mal Osteoartic 28:643–652
Li PL, Ganz R (2003) Morphologic features of congenital acetabular dysplasia: one in six is retroverted. Clin Orthop Relat Res 416:245–253
Matta JM, Stover MD, Siebenrock K (1999) Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res 363:21–32
Myers SR, Eijer H, Ganz R (1999) Anterior femoroacetabular impingement after periacetabular osteotomy. Clin Orthop Relat Res 363:93–99
Peters CL, Erickson JA, Hines JL (2006) Early results of the Bernese periacetabular osteotomy: the learning curve at an academic medical center. J Bone Joint Surg Am 88(9):1920–1926
Pogliacomi F, Stark A, Wallensten R (2005) Periacetabular osteotomy. Good pain relief in symptomatic hip dysplasia, 32 patients followed for 4 years. Acta Orthop 76(1):67–74
Reynolds D, Lucas J, Klaue K (1999) Retroversion of the acetabulum. A cause of hip pain. J Bone Joint Surg Br 81(2):281–288
Sambandam SN, Hull J, Jiranek WA (2009) Factors predicting the failure of Bernese periacetabular osteotomy: a meta-regression analysis. Int Orthop 33:1483–1488
Severin E (1941) Contribution to the knowledge of congenital dislocation of the hip joint. Late results of closed reduction and arthrographic studies of recent cases. Acta Chir Scand 84(63):1–142
Siebenrock KA, Schöll E, Lottenbach M, Ganz R (1999) Bernese periacetabular osteotomy. Clin Orthop Relat Res 363:9–20
Siebenrock KA, Schoeniger R, Ganz R (2003) Anterior femoro-acetabular impingement due to acetabular retroversion. Treatment with periacetabular osteotomy. J Bone Joint Surg Am 85:278–286
Tönnis D, Behrens K, Tscharani F (1981) A modified technique of the triple pelvic osteotomy: early results. J Pediatr Orthop 1(3):241–249
Tönnis D (1987) Congenital dysplasia and dislocation of the hip in children and adults. Springer, Berlin
Trousdale RT, Ekkernkamp A, Ganz R, Wallrichs SL (1995) Periacetabular and intertrochanteric osteotomy for the treatment of osteoarthrosis in dysplastic hips. J Bone Joint Surg Am 77(1):73–85
Trousdale RT, Cabanela ME (2003) Lessons learned after more than 250 periacetabular osteotomies. Acta Orthop Scand 74(2):119–126
Wiberg G (1939) Studies on dysplastic acetabula and congenital subluxation of the hip joint with special reference to the complication of osteoarthritis. Parts I–IV. Acta Chir Scand 83(58):1–135
Xie J, Naito M, Maeyama A (2010) Evaluation of acetabular versions after a curved periacetabular osteotomy for dysplastic hips. Int Orthop 34:473–477
Acknowledgments
The authors would like to thank Margaret McGee for her critical review of the manuscript. This project was financially supported by the Royal Adelaide Hospital.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Howie, D.W., Beck, M., Costi, K. et al. Mentoring in complex surgery: minimising the learning curve complications from peri-acetabular osteotomy. International Orthopaedics (SICOT) 36, 921–925 (2012). https://doi.org/10.1007/s00264-011-1347-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00264-011-1347-y