Abstract
Summary
Opportunistic osteoporosis screening using abdominal CT scans obtained for other purposes has the potential to increase detection of those at increased risk for fragility fractures. We sought to combine the tasks of density measurement and vertebral fracture assessment on the sagittal view. We confirm that this represents a robust approach and recommend its implementation in clinical practice.
Introduction
Opportunistic osteoporosis screening at routine abdominal CT has been proposed by measuring axial (transverse) L1 trabecular attenuation and by sagittal reconstruction for vertebral fracture assessment. We sought to combine this dual evaluation on the sagittal reconstruction alone to improve efficiency.
Methods
Routine contrast-enhanced abdominal CT scans performed for any indication on 571 consecutive adults age 60 years or older (mean age 70.7 years) were retrospectively analyzed. These were performed at a single center over a 3-month period. L1 trabecular attenuation was measured using an ovoid region-of-interest on both the transverse and sagittal series. The sagittal reconstruction was also analyzed for moderate-to-severe vertebral compression fractures using the Genant visual semi-quantitative method. Likely osteoporosis was defined by a moderate-to-severe fracture and/or sagittal L1 trabecular attenuation of ≤110 Hounsfield units (HU) (previously found to be >90 % specific for osteoporosis on our calibrated GE CT scanners at 120 kVp). Correlation was made with hip and spine dual X-ray absorptiometry (DXA).
Results
Mean absolute difference in L1 trabecular attenuation between transverse and sagittal reconstructions was 6.7 HU (±5.7) or 6.2 %. The transverse and sagittal HU measurements were in agreement (i.e., both measurements above or below this threshold) in 94.5 % of cases at the 110-HU cutoff. A total of 243 (42.3 %) patients had likely osteoporosis by CT criteria, of which only 48 (19.8 %) had previous DXA screening.
Conclusion
Assessment of the sagittal view alone at routine abdominal CT for both vertebral fractures and trabecular bone mineral density provides a rapid and effective opportunistic screen for detecting individuals at increased risk for fragility fractures.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a common disease, particularly in postmenopausal women [1–3]. In the USA, osteoporosis affects more than 50 million Americans [4] and confers a high fracture risk during a person’s lifetime [3]. Osteoporosis-related fractures affect quality and quantity of life. Indeed, hip fractures in particular are associated with high mortality [5, 6], especially in men [7]. Despite the significant increase in fracture risk and the health implications they carry, osteoporosis remains substantially underdiagnosed and undertreated worldwide [8–10]. There is a need for additional safe and cost-effective screening methods. There is evidence that existing methods such as dual X-ray absorptiometry (DXA) and quantitative computed tomography (QCT) are currently underutilized in clinical practice [4].
Recently, we have shown that CT-derived opportunistic screening for osteoporosis using abdominal CT scans obtained for indications other than osteoporosis can effectively detect low bone mineral density [11–13]. This method uses a simple region-of-interest (ROI) attenuation measurement in the trabecular bone of the L1 vertebra. Because existing CT data are utilized, this opportunistic method can be employed retrospectively and allows for identification of patients potentially at high fracture risk. With over 80 million CT scans performed per year in the USA, this presents a unique opportunity for performing initial osteoporosis screening that does not expose the patient to additional radiation, time, or cost. [14] However, at this point, we have only used the transverse (axial) CT images for the trabecular ROI measurements.
The sagittal reconstructions from an abdominal CT study have been shown to be a valuable tool for identifying vertebral compression fractures that may otherwise be missed if only the axial plane is evaluated [15]. By integrating our simple ROI trabecular measurement onto the sagittal plane, osteoporosis screening can be seamlessly integrated with vertebral fracture assessment, increasing overall efficiency. The purpose of this study was to determine if L1 trabecular bone attenuation measurements on the sagittal reconstructions match well with the axial measurements that are already validated.
Materials and methods
Patient cohort
The University of Wisconsin Health Sciences Institutional Review Board approved this Health Insurance Portability and Accountability Act (HIPAA) compliant retrospective study. The need for obtaining signed informed consent was waived for this retrospective analysis. The main inclusion criteria consisted of adults aged 60 and older who underwent contrast-enhanced CT of the abdomen/pelvis for any indication at our institution over a 3-month time period ending in April 2014. A total of 571 patients met these criteria and were included in the final study cohort (283 men and 288 women, mean age 70.7 years, age range 60–99 years, interquartile range 64–76 years).
Computed tomography
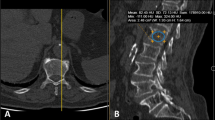
Routine abdominopelvic CT was done using 16–64 row multi-detector CT scanners (GE Healthcare). All scanners are calibrated daily to ensure accuracy of CT attenuation numbers, which correlate well with underlying bone mineral density (BMD) [11]. Transverse (axial) images were acquired with thin collimation at 120 kVp and reconstructed with 5-mm thickness at 3-mm intervals using a standard soft tissue algorithm. Coronal and sagittal reconstructions are routinely obtained with 5-mm thickness at 2.5-mm intervals. The axial and sagittal CT series were retrospectively assessed on a standard radiology picture archiving and communication system (PACS) workstation. Soft tissue and bone windows were used to view the images, which do not influence attenuation or BMD values [12]. Mean CT attenuation was assessed by the primary reader (S.J.L.) placing a single click-and-drag ROI in the anterior trabecular bone space of the L1 vertebral body, as previously described [11, 12] and as shown in Fig. 1. This process was sequentially performed in the axial plane for all patients, followed by the sagittal plane for comparison. Measurements in the sagittal plane were done without knowledge of attenuation values measured in the axial plane to minimize confirmation bias. We avoided placing the ROI over areas of attenuation heterogeneity, such as the posterior venous plexus, spinal hemangiomas, spinal hardware, and compression fractures in order to avoid distortion of attenuation measurements. Attenuation differences between the two views were reported as absolute Hounsfield unit (HU) values to maximize true measurement difference and avoid simple cancellation effects.
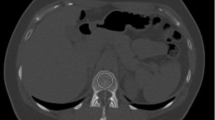
Axial and sagittal L1 trabecular attenuation measurement at abdominal CT in 64-year-old man. Axial (a, b) and sagittal (c, d) CT images in soft tissue (a, d) and bone (c, d) windows show ROI placement in the anterior trabecular space of L1. In addition to low BMD (83 HU axial, 85 HU sagittal) that is likely compatible with osteoporosis, moderate compression fractures are present at T12 and L4 (arrows), indicative of complicated osteoporosis. In retrospect, the patient had a similar L1 attenuation (85 HU sagittal) compatible with osteoporosis at CT 3 years earlier (e) but without complicating fracture
Multi-detector CT represents an ideal non-invasive in vivo method for detection of relevant vertebral fractures, given its cross-sectional/multi-planar nature and level of bone detail. Vertebral compression fracture presence was evaluated using the Genant visual semi-quantitative method [16]; only moderate-to-severe vertebral fractures of the lumbar and lower thoracic spine (i.e., grades 2 or 3 corresponding to at least 25 % height loss) were recorded [11, 12]. This was done by the primary reader (S.J.L.) while viewing the CT images in the sagittal. Experienced radiologists (10 and 15 years, respectively) confirmed the presence of all moderate-to-severe compression fractures. Likely osteoporosis at CT was defined in this study by a mean L1 trabecular bone attenuation value of ≤110 HU in either the sagittal or axial plane or by the presence of a moderate-to-severe compression fracture. This HU threshold value was based on previous work on our calibrated GE CT scanners at 120 kVp, where an L1 attenuation threshold value of ≤110 HU was found to be 90 % specific for diagnosing osteoporosis according to standard DXA (but only about 50 % sensitive), and a threshold of ≤160 HU was found to be 90 % sensitive (but only about 50 % specific) at DXA [11]. These L1 HU measurements at CT are only intended for opportunistic detection of probable low BMD, which should be confirmed by DXA and considered in addition to other clinical fracture risk factors prior to any treatment decisions. As such, the reproducibility and variance of the CT measurement is not as relevant as is the case for DXA.
Dual energy X-ray absorptiometry
Ninety one of the 571 patients in this study had DXA of the proximal femora and lumbar spine performed within 4 years prior to the CT scan used for BMD measurements. DXA was performed using standard techniques on Lunar Prodigy densitometers (GE Healthcare, Waukesha, WI, USA).
Results
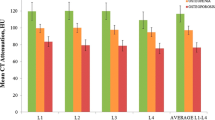
The mean (±standard deviation) axial and sagittal attenuation values for the entire sample were 126.1 ± 45.8 and 122.5 ± 45.9 HU, respectively. The median axial L1 attenuation was 122.1 HU (interquartile range 97.0–150.5) and the median sagittal L1 attenuation was 118 HU (interquartile range 95.0–146.0) (Fig. 2). The mean of the absolute difference between each patient’s axial and sagittal L1 trabecular attenuation measurement was 6.7 ± 5.8 HU, and the mean absolute percentage difference was 6.2 ± 11.3 %. A paired t test of the axial and sagittal attenuation values showed that axial measurements were significantly greater than sagittal measurement, with a mean difference of 3.6 HU (p < 0.01, 95 % CI = 2.9–4.2). A Bland-Altman plot did not reveal any significant dependence or bias of these attenuation differences on the average attenuation (Fig. 3).
Of the 571 patients, 235 (41 %) had a sagittal attenuation value of ≤110 HU (corresponding to 90 % or greater specificity for a CT diagnosis of osteoporosis based on prior DXA correlation). Axial and sagittal measurements agreed on a CT-based HU diagnosis or exclusion of osteoporosis (i.e., both measurements of ≤110 HU or both measurements of >110 HU) in 94.5 % of the cases (540 of 571) at this 90 % specificity threshold. Axial and sagittal measurements were in agreement 96.7 % of the time (552 of 571) at the 160 HU threshold (the 90 % sensitivity threshold for DXA correlation). Of the 243 patients with a sagittal L1 attenuation of ≤110 HU, 48 (20.4 %) had undergone DXA screening within 4 years prior to the CT scan data used for this study.
The average age of women in the cohort was 70.6 ± 8.1 years. Women had mean L1 axial and sagittal attenuation values of 125.4 ± 44.8 and 122.1 ± 45.0 HU, respectively. The mean absolute difference between axial and sagittal L1 attenuation measurements was 6.4 ± 5.5 HU. Of the 283 women in the cohort, 127 (44.9 %) had an L1 sagittal attenuation value of ≤110 HU and/or had a moderate-to-severe vertebral compression fracture. Only 35 of these 127 women (27.6 %) had undergone a DXA study within 4 years prior to the CT scan used for this study. The average age of men in our patient cohort was 70.5 ± 8.1 years. Men had mean L1 axial and sagittal attenuation values of 126.8 ± 46.9 and 122.9 ± 46.8 HU, respectively. The mean absolute difference between axial and sagittal measurements for men was 7.0 ± 6.1 HU. Of the 288 men in the cohort, 116 (40.2 %) of them had an L1 sagittal attenuation value of ≤110 HU and/or had a moderate-to-severe vertebral compression fracture. Of these 116 patients, 13 (11.5 %) had undergone a DXA study within 4 years prior to the CT scan used for this study.
A total of 27 patients had at least one moderate-to-severe vertebral compression fracture present at the time of the CT scan used for this study (13 men, 14 women). The average age of these patients was 73.8 ± 11.1 years, and the average L1 axial and sagittal attenuation values were 87.2 ± 47.2 and 85.5 ± 46.4 HU, respectively. Of these 27 patients, 7 (25.9 %) had undergone a DXA study 4 years prior to the CT scan date used for this study. Of these 7 patients, only 1 was diagnosed with osteoporosis defined by DXA (T-score ≤−2.5 for either femoral neck or L1-L4 average).
Discussion
We have previously demonstrated the ease and utility of assessing lumbar trabecular BMD via simple ROI attenuation measurement (in HU) at routine abdominal CT for the purposes of opportunistic osteoporosis screening [11]. Furthermore, the importance of reviewing the sagittal reconstruction in addition to the standard axial views for unsuspected vertebral compression fractures at abdominal CT has also been shown [15]. To further improve the efficiency of CT-based opportunistic osteoporosis screening, we sought to combine both of these assessments on the sagittal view alone. Because these CT examinations are generally obtained for other indications and typically read by general radiologists or body imagers, this additional opportunistic screen needs to be very simple to apply in order for it to be adopted in actual practice. Before assuming that this approach will work, the main piece of missing information was whether the ROI HU measurement in the sagittal plane could serve as a reasonable replacement for the axial HU measurement.
In this study, the axial (transverse) and sagittal CT trabecular attenuation measurements closely agreed in the great majority of cases, confirming that density measurement and vertebral fracture screening can be combined into one simple assessment on the sagittal view and can be seamlessly integrated into a radiologist’s busy clinical practice pattern. This method is opportunistic and requires no extra radiation, cost, or patient time. By combining attenuation measurement and vertebral fracture assessment into the sagittal view, potentially valuable information is added regardless of the actual CT indication, and a radiologist can potentially identify patients who may be at high risk for developing fragility fractures. Confirmation of low BMD findings with central DXA and estimation of fracture risk with BMD plus clinical fracture risk factor assessment is the current standard of care. Another potential option is a simultaneous DXA-equivalent femoral neck T-score obtained using the same abdominal CT scan [17]. However, a formal baseline DXA and fracture risk assessment would still be needed prior to considering pharmacologic treatment. Regardless, identification of previously undetected low BMD or existing vertebral fracture represents an opportunity to identify those previously unappreciated to be at risk for fragility fracture, thereby allowing appropriate clinical evaluation, assessment of clinical fracture risk factors, and subsequent consideration of therapies with demonstrated efficacy to reduce future fracture risk. This is relevant as osteoporosis is an underdiagnosed condition, and this method provides a simple way to expand initial screening—even if unintended.
Our study findings suggest that opportunistic reporting of vertebral findings at abdominal CT could help to increase overall osteoporosis screening by identifying patients at increased risk for fragility fractures. In particular, only a small fraction of patients (i.e., only about 20 %) with low BMD by L1 CT assessment (≤110 HU) had undergone DXA screening within a 4-year period prior to CT. Furthermore, only about 25 % of patients with a moderate or severe vertebral compression fracture at CT had undergone DXA screening within a 4-year period prior to CT. These findings are not surprising given that screening is not universally performed for those in whom it is indicated and that, at least according to the US Preventative Services Task Force, screening is not indicated in men. In the case we illustrated (Fig. 1), a 64-year-old male was noted to have moderate T12 and L4 vertebral compression fractures at abdominal CT in addition to low BMD suggested by the CT attenuation measurement (83 HU axial, 85 HU sagittal). In retrospect, he also had low BMD (85 HU, sagittal) on a CT scan performed 3 years prior, but at that time had not yet sustained a vertebral fracture. This case provides an example where L1 attenuation measurement might have placed this patient into a high-risk category where preventative measures could have been considered.
One result from our study that may warrant further investigation was the small but statistically significant mean difference in L1 attenuation between the axial and sagittal views of about 3–4 HU measured in the entire cohort. One possible explanation for this systematic difference is the subtle variation in intra-vertebral trabecular architecture. Anecdotally, we have often observed a slightly denser stripe of trabecular bone parallel to the endplates at the mid-vertebral level on the sagittal view at CT. A recent anatomy study has confirmed this observation, showing that BMD was significantly higher at the mid-vertebral region compared with both cranial and caudal regions [18]. If the axial measurements are more often obtained near the mid-vertebral level, this could account for the slight increase in mean attenuation compared to the sagittal measurement, which samples a broader craniocaudal region of the anterior trabecular space. Nonetheless, this small difference is likely of no clinical significance, as this screening method is somewhat forgiving and not meant to be a diagnostic assessment.
Another future area of investigation entails the use of automation for these CT-based assessments, which could allow for large-scale implementation of opportunistic screening. Such automated computer-assisted L1 trabecular HU measurement has been proven feasible [13], but the attenuation measures have not yet been compared with the manual ROI method. Similarly, tools are being developed for computer-assisted detection of vertebral compression fractures. We are currently investigating the use of a combined automatic tool for vertebral BMD and fracture assessment at abdominal CT.
Another interesting finding of our study was the rather similar trabecular L1 HU values between men and women. This is consistent with prior studies documenting that QCT BMD measures are similar between men and women [19]. The reason that DXA areal BMD is higher in men than women is that, generally speaking, male bones are larger than female bones and inclusion of this greater depth in areal BMD measurement leads to a higher value (g/cm2) in men.
We do not intend to imply that the specific HU thresholds used herein should be universally adopted for opportunistic CT screening, but rather demonstrate how HU measures can help inform BMD status in an individual patient at CT. It is important to reiterate that our particular HU thresholds values may not necessarily translate to other practices or CT protocols. As such, CT-scanner-specific thresholds with fixed protocols should be validated against internal DXA results. Furthermore, ongoing CT scanner calibration is required to ensure reproducible and accurate BMD results. Some may wish to consider the use of a lower threshold; for example, an L1 trabecular attenuation of <100 HU (on any CT scanner) should generally lead to DXA confirmation as this level is fairly specific for osteoporosis at DXA [11]. Of course, a low HU measure in conjunction with a moderate or severe vertebral compression fracture should be taken even more seriously and can effectively make the diagnosis of osteoporosis, although confirmatory/baseline DXA is still necessary prior to initiation of pharmacologic therapy. Furthermore, although different CT vendors can deliver somewhat different HU measures—especially as one deviates from water density [20], an L1 trabecular attenuation below 100 HU should generally be considered abnormally low on any scanner at 120 kVp (of note, different HU thresholds would apply at different kVp levels). Of note, a recent independent publication has provided external validation of our simple L1 ROI technique for opportunistic CT-based screening [21]. It should be emphasized that use of a numerical cut point to diagnose osteoporosis and/or to guide pharmacologic therapies is becoming less clinically important. For example, use of fracture risk estimation is increasingly widely recommended [22]. Indeed, a recent position statement of the National Bone Health Alliance recommends that osteoporosis be diagnosed not only by low BMD T-score but also by elevated fracture risk [23]. As such, regardless of the HU criteria selected to define “low,” opportunistic detection of individuals potentially at elevated fracture risk at the time of CT for other indications has great potential to reduce fragility fractures.
We acknowledge limitations to our study. Not all patients in this CT-based study had correlative DXA. However, we had previously explored this issue for the axial HU approach [11], and the axial-sagittal CT comparison was now more relevant. The cost-effectiveness and potential economic implications of this opportunistic screening method have not yet been explored, but given that this is a rapid and “free” add-on, the potential for benefit is substantial. Such information on cost-effectiveness would be useful in terms of adoption by health-care systems and clinicians. Of note, this analysis can be performed either prospectively or retrospectively, as CT scans archived within PACS can be easily retrieved for this analysis.
In summary, we have shown that opportunistic osteoporosis screening with routine abdominal CT by means of trabecular density and vertebral fracture assessment can be combined using the sagittal reconstruction only. Given the volume of body CT scans performed in the USA and the high prevalence and underdiagnosis of osteoporosis, this presents a great opportunity to identify many individuals with elevated fracture risk that is currently unappreciated, including those already complicated by fracture. Following baseline DXA and fracture risk assessment, pharmacologic intervention in some cases may help to reduce the risk of potentially debilitating fragility fractures and the health-care costs associated with them. This approach can be easily integrated into radiologists’ clinical practice pattern and provides further value to abdominal CT regardless of the indication.
References
Raisz LG (2005) Screening for osteoporosis. N Engl J Med 353:164–171
Calonge N, Bibbins-Domingo K, Cantu AG et al (2011) Screening for osteoporosis: U.S. preventive services task force recommendation statement. Ann Intern Med 154:356–U131
Bone Health and Osteoporosis (2004) A report of the surgeon general. Rockville, MD: US Department of Health and Human Services Office of the Surgeon General
King AB, Fiorentino DM (2011) Medicare payment cuts for osteoporosis testing reduced use despite tests’ benefit in reducing fractures. Health Aff 30:2362–2370
Center JR, Nguyen TV, Schneider D, Sambrook PN, Eisman JA (1999) Mortality after all major types of osteoporotic fracture in men and women: an observational study. Lancet 353:878–882
Cauley JA, Thompson DE, Ensrud KC, Scott JC, Black D (2000) Risk of mortality following clinical fractures. Osteop Int : J Estab Res Coop Between Europ Found Osteop Natl Osteop Found USA 11:556–561
Ebeling PR (2008) Osteoporosis in men. N Engl J Med 358:1474–1482
Abraham A (2003) Undertreatment of osteoporosis in men who have had a hip fracture. Arch Intern Med 163:1236, author reply −7
Kiebzak GM, Beinart GA, Perser K, Ambrose CG, Siff SJ, Heggeness MH (2002) Undertreatment of osteoporosis in men with hip fracture. Arch Intern Med 162:2217–2222
Wilkins CH, Goldfeder JS (2004) Osteoporosis screening is unjustifiably low in older African-American women. J Natl Med Assoc 96:461–467
Pickhardt PJ, Pooler BD, Lauder T, del Rio AM, Bruce RJ, Binkley N (2013) Opportunistic screening for osteoporosis using abdominal computed tomography scans obtained for other indications. Ann Intern Med. 2013;158:588--595
Pickhardt PJ, Lee LJ, del Rio AM et al (2011) Simultaneous screening for osteoporosis at CT colonography: bone mineral density assessment using MDCT attenuation techniques compared with the DXA reference standard. J Bone Miner Res 26:2194–2203
Summers RM, Baecher N, Yao J et al (2011) Feasibility of simultaneous computed tomographic colonography and fully automated bone mineral densitometry in a single examination. J Comput Assist Tomogr 35:212–216
IMV (2011) CT market outlook report. IMV Medical Information Division, Des Plaines
Carberry GA, Pooler BD, Binkley N, Lauder TB, Bruce RJ, Pickhardt PJ (2013) Unreported vertebral body compression fractures at abdominal multidetector CT. Radiology 268:120–126
Genant HK, Wu CY, Vankuijk C, Nevitt MC (1993) Vertebral fracture assessment using a semiquantitative technique. J Bone Miner Res 8:1137–1148
Pickhardt P, Bodeen G, Brett A, Brown JK, Binkley N (2014) Comparison of femoral neck BMD evaluation obtained using lunar DXA and QCT with asynchronous calibration from CT colonography. J Clin Densitometr: Off J Int Soc Clin Densitometr. doi:10.1016/j.jocd.2014.03.002
Kennedy OD, Brennan O, Rackard SM, O’Brien FJ, Taylor D, Lee TC (2009) Variation of trabecular microarchitectural parameters in cranial, caudal and mid-vertebral regions of the ovine L3 vertebra. J Anat 214:729–735. doi:10.1111/j.1469-7580.2009.01054.x
Ebbesen EN, Thomsen JS, Beck-Nielsen H, Nepper-Rasmussen HJ, Mosekilde L (1999) Age- and gender-related differences in vertebral bone mass, density, and strength. J Bone Miner Res 14:1394–1403
Lamba R, McGahan JP, Corwin MT (2014) CT Hounsfield numbers of soft tissues on unenhanced abdominal CT scans: variability between two different manufacturers’ MDCT scanners. AJR 203:1013–1020
Buckens CF, Dijkhuis G, de Keizer B, Verhaar HJ, de Jong PA (2015) Opportunistic screening for osteoporosis on routine computed tomography? An external validation study. Eur Radiol 25:2074–2079
Kanis JA, McCloskey EV, Johansson H et al (2013) European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteop Int 24:23–57
Siris E, Adler R, Bilezikian J et al (2014) The clinical diagnosis of osteoporosis: a position statement from the National Bone Health Alliance Working Group. Osteop Int 25:1439–1443
Conflicts of interest
Dr. Pickhardt is co-founder of VirtuoCTC, shareholder in Cellectar Biosciences and consultant for Check-Cap; Scott Lee, Neil Binkley, Meghan Lubner, Richard Bruce, and Timothy Ziemlewicz declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lee, S.J., Binkley, N., Lubner, M.G. et al. Opportunistic screening for osteoporosis using the sagittal reconstruction from routine abdominal CT for combined assessment of vertebral fractures and density. Osteoporos Int 27, 1131–1136 (2016). https://doi.org/10.1007/s00198-015-3318-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-015-3318-4