Abstract
Risk communication is central to the risk management strategy of a pharmaceutical company. Pharmaceutical companies primarily communicate risk through labelling tools such as the Summary of Product Characteristics (SmPC), package insert, patient information leaflet (PIL) and the carton, which are currently regulated based on templates such as those of the EU. Recent research raises concern about how effective the SmPC is alone in communicating risk. There is some evidence that carton design can influence risk comprehension. Processes to check new trade names cannot be confused with existing names is a simple measure to mitigate one form of risk. Given the central role and the vast amount of resource that is consumed, it is surprising there has not been extensive original research to see whether product information such as the SmPC is a good tool for communicating risk. Recently, EU agencies have assessed the communication value of the PIL and revised the template and guidelines. However, no evaluation of user testing has been conducted at European level since the introduction of these new requirements. As regards ‘Dear Healthcare Professional Communications’, there is inconsistent evidence about their ability to change patient and physician behaviour. There is a dearth of evidence about what sort of communications materials are the most effective under which circumstances.
The use of templates restricts the flexibility of companies to adapt their risk messages to their targets. Effective communication requires understanding how different audiences perceive the message and what the funda-mental drivers are for altering patient and prescriber behaviour to be safer. This requires careful consideration of the relationship between risk communication, perception and management. However, the focus of a company’s risk communication plan is normally on the International Conference on Harmonisation (ICH) regions and their regulations. Although the same regulatory tools are used globally, we are not aware of any research into their effectiveness outside the ICH regions.
What listed companies can communicate about benefits and risks is strongly influenced by the obligations of companies to the market and investors. There needs to be internal coordination for simultaneous release. Internal communications about significant issues should be restricted to those who know how to manage the risk of insider dealing from internal communications that may later be made public.
Unfortunately, there is evidence that some companies do not have a cohesive strategy for communicating risk which should take into account all forms of promotional material and company-sponsored information sources on the Internet.
A pharmaceutical company is not the only stakeholder responsible for communicating risks on their products. However, the relative roles and responsibilities of all relevant stakeholders are not defined and are often un-clear. This means it is difficult to evaluate whether a company’s actions might be duplicative or inefficient. We recommend that companies have a dedicated communications group whose role is to coordinate the company’s communications strategy mapped to objectives that have been agreed with key stakeholders apart from just regulatory agencies. This same group can assess effectiveness of the communications, monitor audience reaction and adjust the communication strategy accordingly.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
1. Introduction: The Risk Communication of Marketed Products
Pharmaceutical companies rely on risk communication as one of the main ways to manage their risks of their products. Since the start of modern regulatory systems in the 1960s, the pharmaceutical industry has primarily communicated ‘risk’ through product labelling (such as the Summary of Product Characteristics [SmPC] and patient information leaflet [PIL] in the EU, package insert in the US and the product carton) and the occasional letter to healthcare professionals (the Dear Doctor Letter, Direct Healthcare Professional Communication). In addition, for EU centralized products, the European Medicines Agency (EMA) summarizes regulatory benefit-risk assessment about a product in the European Public Assessment Reports (EPARs).
What evidence do we have that such labelling effectively manages risk? This is not solely the responsibility of a pharmaceutical company, but a joint effort between the various stakeholders as the public expects the pharmaceutical companies and its regulators to do their best to cooperate to reduce drug risks.[1] This leads us to think more broadly as to whether or not there should be concern about how well the industry manages the risks of their medicines. The answer is definitely ‘yes’ for certain groups of medicines and this may relate partially to inadequate risk communication although a thorough root cause analysis has not been performed. For example, the disastrous cases of blindness resulting from the ophthalmic misuse of Avastin® (bevacizumab) approved for oncology, reported in August 2011, serve as a wake-up call that all is not well with the pharmaceutical safety system.[2]
In the last century, communicating risk was traditionally focused on physical harm, that is, suspected adverse drug reactions (ADRs). Over the last 10 years, as pharmaceutical risk management has developed, the science of risk communication has evolved considerably. We now understand that public reception and processing of risk communications are influenced by perceptions of risk. Perceptions of risk are not strictly derived from the raw statistics of the actual probability of a risk occurring but rather involve additional factors not included in expert assessments of risk. One example of such a factor is that of dread potential or the severity assigned by the public to a risk based on personal feelings of how catastrophic the outcomes of that particular risk might be in a certain sociopolitical context. Thus the best intentions for ‘communicating’ risk are highly dependent on and influenced by the level of uncertainty regarding understanding of actual risk. So how has the industry adapted its own risk communication techniques globally in the light of the science of risk communication?
We can begin to address this issue by illustrating the size of the public health problem from continuing harm from certain medicines through three examples. In the US, for those aged 45 years and older there has been a growth in hospitalization for medication-induced delirium; ‘poisoning’ or overdose by codeine, meperidine and other opiate-based pain medicines; and withdrawal from narcotic or non-narcotic drugs. Admissions for all medication and drug-related conditions grew by 117% from 30 100 to 65 400 for 45- to 64-year-olds between 1997 and 2008. The rate of admissions for people aged 65–84 years closely followed, growing by 96%, and for people aged 85 years and older, the rate grew by 87%.[3]
In the second example, also from the US, twice in the past 5 years the FDA have issued nationwide alerts about medically significant and sometimes fatal ADRs when antipsychotics are taken by people with dementia. This topic has also been the subject of a recent editorial.[4,5]
The third example concerns the added complexity of communicating pharmaceutical risk given a different regulatory system for devices. This is particularly problematic when the risks of a medicine are strongly influenced by safe use of a device. For example, in the US about 375 000 adults with type 1 diabetes mellitus used insulin pumps in 2007, with nearly 17 000 reports of health problems over the 3 years ended in 2009. The FDA found that manufacturers had not been investigating many of the reports, leaving the causes of failures unknown and unevaluated. This is linked to 18 recalls of pumps over 5 years because of hardware and software problems.[6]
Safety concerns surrounding marketed products are the focus of this article. We should not forget that risk communication is equally important when developing and researching medicines. This is reflected in the dissemination of safety information during clinical trials and effective medical monitoring.[7] As a result, a sponsor of a clinical trial should ensure that there is full disclosure to subjects about benefits and risks to ensure informed consent as well as timely reporting to regulatory agencies of newly discovered safety information according to the requirements of those agencies. Risk communication is an important part of investigator training, ongoing clinical monitoring and prompt reporting to a Data Safety Monitoring Board. There have been some significant breakdowns in ethical conduct often relating to communication about benefits and risks of participating in a clinical trial.[8] Also, there has been an underreporting of clinical trials on external registries despite being a regulatory requirement with significant consequences for assessing benefits and risks.[9] Exploring risk communication within drug development exceeds the scope of this article although it is worthy of further analysis.
Concerning the current article, given the concerns about certain types of marketed products as illustrated by the examples above and because the science of risk communication has advanced, this article focuses on how effective the pharmaceutical industry is at communicating risk about prescription-only medicines in the EU. Firstly, it is important to summarize how risk management has evolved since the year 2000.
2. The Emergence of Risk Management Planning to Take Centre Stage
Around the year 2000, the pharmaceutical industry, EU and US regulators began exploring the concept of risk management as a way of better managing relevant risks to reassure society about the safety of pharmaceuticals and ultimately patient safety. There were some interesting discussions within the industry and academia concerning voluntary risk management which culminated in ICH E2E pharmacovigilance planning.[10–12] This led to the development of the current EU Risk Management template in 2006 for all new marketing authorizations or older products with safety issues.[13,14] This obliged marketing authorization holders (MAH) to take a more active approach to managing risk communication seriously as one of the fundamental tools for mitigating risk. Although the FDA was part of the International Conference on Harmonisation (ICH) process, it took a different regulatory approach through risk evaluation and mitigation strategies (REMS) and MedGuides, which, unlike the EU, were not mandatory for all new drug applications.[15] The third main stakeholder in ICH, the Pharmaceutical and Medical Devices Agency in Japan, has issued their own risk management template and plan to implement this in 2013.[16]
3. Current EU Requirements for Risk Communication
The requirement to produce educational material as part of an EU Risk Management Plan (RMP) [more than just relying on the SmPC] depends on individual risk assessment. Of course, MAHs may produce material to inform and educate healthcare professionals and patients outside of the RMP as part of their marketing programme.
If educational materials are submitted with a RMP (Annex 8 of the EMA template[13]) there needs to be clear objectives with key principles and messages concerning enhancing the understanding of specific risk(s) and methods to reduce either the frequency or severity, especially if there is a need for additional precautions. There are critical questions physicians want answered if the risk to medicine is to be adequately managed, which would also apply to a US medication guide.[15] These include the following:
-
• How serious is this risk in the sense is it life threatening or bothersome?
-
• How concerned should I be or how likely is this risk going to occur?
-
• What is suggested I do about this issue?
-
Do I need to monitor something?
-
Do I need to warn patients?
-
Do I need to avoid prescribing to specific patients?
-
Do I need to limit or stop prescribing?
-
Examples of the type of risk that might have to be communicated are as follows:
-
how to administer the medicine with certain types of devices;
-
specific ADRs such as those that require monitoring or early detection;
-
specific contraindications or increased risk by interactions with certain medicines or procedures;
-
advice about drug titration matched to symptoms and signs or laboratory tests;
-
how to avoid certain medication errors.
The type of educational material will depend on the specific safety concern. This must be in line with the SmPC and PIL, and include examples such as the following:
-
guide to prescribing or dispensing;
-
checklist for actions for prescribing or dispensing;
-
patient information brochure (as well as the PIL);
-
patient alert card/patient monitoring card.
Although MAHs are advised to consult patient groups/healthcare professionals and risk communication experts to ensure good comprehension and acceptance of the educational material, it is uncertain how often that actually happens. There is a particular regulatory concern about such materials being ‘too promotional’.[17] As there is no common understanding about what being too promotional means, this means it is even more important to seek opinions of other stakeholders to check messages are balanced. MAHs are expected to describe how they will assess the effectiveness of their communication plan in the RMP. Methods of evaluation are appropriate to the specific risk and the risk minimization activity, and may include surveys of comprehension and behaviour change, drug utilization studies and other database studies. Although these assessment activities may be mentioned in the EPARs, generally there are too few details to fully evaluate what MAHs are actually doing let alone perform benchmarking to improve practice.
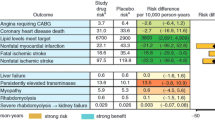
Once a risk communication plan is agreed, then a variety of different potential communication channels could be utilised (see table I); the marketing departments of companies are often well experienced in harnessing these sources.
4. Risk Communication Tools
4.1 The Summary of Product Characteristics
The SmPC has other functions apart from being the main tool a company relies upon to communicate risk. These functions of a SmPC include being:
-
the agreed position between the MAH and regulatory agencies following assessment;
-
the basis of information for healthcare professionals on how to use the product safely and effectively;
-
the basis for how the PIL must be drawn up in accordance with the SmPC.
Unlike the PIL, there is no requirement for user testing of the SmPC. Such user testing was performed by Luto Research in collaboration with Roche for the two SmPCs for Lariam® (mefloquine) and CellCept® (mycophenolate mofetil).[18] Fifteen points relevant to safe and effective use were selected, and ten doctors were recruited to identify each piece of information and explain what it means. Of these 15 points for the Lariam SmPC, nine were not found or found with difficulty and five were not understood by two or more doctors. Comments included that the SmPC was muddled so that information was not where it was expected and there was considerable repetition with the sections on interactions, pregnancy and driving. Revising wording using the original layout led to a modest improvement in finding the information and understanding. Testing of the CellCept SmPC with specialist hospital doctors revealed low ability of doctors to navigate the SmPC, with 11 of 15 points not found or found with difficulty. This form of user testing identified issues around doctors finding relevant information where it would be expected. Because MAHs must follow a standard template, it is not possible to design a bespoke version for healthcare professionals dependent on the product or healthcare professional.
Despite its limitations, the SmPC is taken into account by hospital and national formulary committees (such as the British National Formulary and Vidal in France) and reimbursement authorities. However, we are not aware of evidence describing how these other bodies, which have major influences on prescribing, adopt the SmPC. UK versions of the SmPC are available internationally through the electronic medicines compendium.
4.2 Assessing the Patient Information Leaflet
The method most frequently employed by MAHs to meet the requirements of article 59(3) for assessing the PIL is that cited in national and EU guidance documents — namely the ‘Australian’ method.[19] This involves the following steps:
-
optimizing the leaflet for content and design elements;
-
identification of key messages for safe and effective use of the medicine;
-
preparation of a questionnaire that contains open questions based on the key messages, and some general questions on overall perception of the document.
Typically, face-to-face interviews with participants in groups of ten are preceded by a pilot test of around three participants. The purpose of the pilot test is to ensure the questions are appropriate and are not included in the results. The responses are collated and, if necessary, revision of the PIL is followed by re-testing. Two rounds of ten participants are involved in testing the final version of the leaflet. Success criteria of 90% of participants being able to find the information required and, of these, 90% being able to understand the information (overall 81% but in practice 80%). Each question must pass the success criteria for the PIL to be considered to have passed the test. This performance-based method provides evidence of how the PIL performs when participants search for information contained in the document. It is not a content-based test that would provide any information on whether or not the leaflet could be understood.
Within the UK, the legislative requirement was for all companies without PILs to submit an application by 30 June 2008. The Medicines and Healthcare products Regulatory Agency (MHRA) then conducted an assessment of all applications and approvals that were granted after that deadline. The MHRA conducted a survey on behalf of the Commission on Human Medicines Expert Advisory Group on Patient Information of user test houses.[20] The survey identified issues with regards to the methodology used by companies and user testing houses, and highlighted deficiencies on the presentation of the content, design and layout of current leaflets.[16] Subsequently, additional guidance was issued by the MHRA to address some of the deficiencies identified in the report.[21] At a European level, as a result of these findings, the Quality Review of Documents (QRD) template for PILs was updated in 2011 in line with comments received from user testing houses.[22] In addition, in February 2011 the Co-ordination Group for Mutual Recognition and Decentralised Procedures — Human (CMDh) issued a position paper discussing other methods acceptable for conducting user testing.[23] No other evaluation of user testing has been conducted at European level since the introduction of this requirement.
4.3 The Importance of the Carton and Packaging in Communicating Risk
The pharmaceutical packaging and carton play an important role in communicating risk. In the EU, there are statutory statements such as ‘Keep Out of the Reach of Children’ which is a prime example.[24] Wording has been clarified for 32 revised cautionary and advisory labels in the UK although it is unknown how uniform such a practice is across the world.[25]
Before a medicine is authorized in the EU and US there are regulatory checks of a medical product name to see if a new product may be confused with an existing product. The criteria for these checks have been most clearly laid out in the centralized procedure in the EU.[26]
One of the best resources on medication errors and mix-ups is the Institute for Safe Medication Practices’ website where one can find look-alike/sound-alike drugs, lists of dangerous abbreviations, and high-risk medications.[27] In addition, under Patient Safety Solutions on the Joint Commission website there is a wealth of resources covering look-alike sound-alike medication names, including translation into Arabic.[28] This is a resource that industry can use to anticipate confusion, although the extent to which it is referred to is unknown.
To illustrate how packaging can influence risk perception, a study was performed evaluating two package designs, one of which had indication-specific signal colours, signal text/administration and pictograms. The latter produced better comprehension results compared to the conventional design. Also, the results indicated that older people, those with physical problems, people not in a receptive mood and those with a poor doctor-patient relationship or a lack of trust in medicines in general, answered the questions with a significantly higher number of errors, and/or required significantly more time to do so, than the remainder of the sample. A good patient-doctor relationship was associated with better results. The authors concluded that the design of packaging should be given more attention as a risk mitigation tool.[29] In addition, from the analysis performed by Shrank et al.[30] the authors concluded that specific content and format of the labels facilitate communication and comprehension by patients and provided guidelines for future labelling.
4.4 Dear Healthcare Professional Communication and Safety Advisory Notices
It has been expressed that alerting healthcare professionals by a Dear Healthcare Professional Communication (DHPC) alone is unlikely to change behaviour in the intended direction, but rather that a letter should be part of a broader communication package and education programme.[31,32] One of the most detailed analyses of the impact of DHPCs concluded that impact assessment needs to be subtle and thorough as there can often be a beneficial impact on some aspects of prescribing behaviour, although such behavioural change needs to be coupled with publicity and other direct interventions by the regulatory agency and manufacturer.[33]
One study looked at whether content, organization and formatting of DHPCs influences physicians’ responses to the letters. For the years 2000 and 2001 in the US, 124 drugs were identified as having had changes to the warning section of the label. Of these, DHPCs were sent in 32 (25.8%) instances. Letters varied in terms of the placement of key information, use of formatting and length. Physicians’ ratings suggested 25% of the letters were deficient in clarity, 28% in readability, 36% in the ratio of relevant information to supporting information, 36% in key information easily discernable, and 28% in overall effectiveness of communication. Letters with formatting highlighting key information were preferred. Letter length and placement of key information were not correlated with physicians’ ratings. The authors concluded that many DHPCs do not communicate labelling changes clearly and effectively.[34]
The most recent assessment of FDA safety advisory notices between 1990 and 2010 identified 49 studies assessing the impact of such notices. These studies covered 16 medicines or therapeutic classes; one-third examined communications regarding antidepressants. Most used medical or pharmacy claims with a few examining patient-provider communication, decision making or risk perceptions. Advisories recommending increased clinical or laboratory monitoring generally led to decreased drug use, but only modest, short-term increases in monitoring. Communications targeting specific subpopulations often spilled over to other groups. Repeated or sequential advisories tended to have larger but delayed effects and decreased incident more than prevalent use. Drug-specific warnings were associated with particularly large decreases in utilization, although the magnitude of substitution within therapeutic classes varied across clinical contexts. Overall, these authors concluded that although some notices have a significant impact, others have delayed or no impact.[35]
We are not aware of any prospective studies looking at different formats of DHPCs to see what works and what does not, as well as looking at different types of assessment and when they should be performed. These were looked for in a systematic search for articles published between January 1996 and January 2010 evaluating the impact of DHPCs, Black-Box Warnings and Public Health Advisories. The authors of this review concluded that safety-related regulatory action can have some impact on clinical practice but could not reach firm conclusions because the evidence is primarily based on only three drugs and drug groups, about half of the studies had inadequate before/after designs, and the heterogeneity in analyses and outcome measures hampered the reporting of overall effect sizes. Furthermore, this review shows the relevance of looking for the unintended effects of safety warnings.[36]
5. Alternative Ways to Communicate Risk: Impact of the Internet
If a physician or patient needs further information or if they are looking for very specific information related to the specific safety issue, it is increasingly likely that they will search the Internet and access sources in addition to the corporate site of a licence holder.[37] Such sources include those that a company can have no direct influence over, such as other colleagues or family friends, social media, published prescribing information (for example, Physician Desk Reference in the US and British National Formulary in the UK), medical websites (for example, WebMD, Medscape, uptodate.com) and regulatory sites (for example, those of the FDA, MHRA and EMA).[38] Then there are pharmaceutical product sites that may or may not receive industry sponsorship, such as Wikipedia and search engines, which can generate all sorts of product information. So do we know whether a company typically checks whether all these sources have correct information? How can a company ensure all the messages are aligned? For company-sponsored sites, a company should ensure consistency (even this can be a major challenge for a global company with affiliates setting up local websites). For non-company websites and other sources, there is a major regulatory disincentive to do so in the sense that if any information such as adverse events is identified they need to be reported as recommended in published guidance for industry.[39]
So who should be concerned about information provided on the Internet? A study of 44 pharmaceutical websites of leading direct-to-consumer (DTC) advertised drugs was performed to determine the extent to which risk information was completely communicated. Three operational definitions of ‘completeness’ were used: communication of the single highest incidence adverse effect, communication of the top three highest incidence adverse effects, and communication of adverse effects with an incidence of ≥10% (all measured in terms of absolute percentage). Results indicated that regardless of the measures used, pharmaceutical websites at that time were unlikely to completely communicate risk information. About two-thirds of all sites communicated the single highest incidence adverse effect or all top three adverse effects. For drugs with adverse effects at ≥10% incidence, only about half of their websites fully reported all effects at this level of incidence.[40]
In a further study, a simulated customer search using the Google search engine identified sites offering statins for sale without prescription. These sites were evaluated using a Website Quality Analysis tool based on previous website assessment tools and a Statin Information Quality Analysis tool searching for specific statin-related information based on PIL headings. Quality (Q) scoring was created so that the higher the score, the better the website. Between November and December 2010, 184 sites from 17 countries were analysed: atorvastatin, pravastatin, rosuvastatin and simvastatin (40 each), and fluvastatin (24). Most sites scored less than half the maximum Q score (26; range 5–17). There were no statistically significant differences between statins. General contraindications were absent in 92.4% of sites and contraindicated medicines in 47.3%. Key warnings on the appearance of symptoms associated with myopathy, liver disease, hypersensitivity and pancreatitis were absent in 37, 48.4, 91.3, and 96.2% of sites, respectively. Most websites presented a chaotic and incomplete list of known adverse effects; just 13 (7.1%) presented a list compatible with current prescribing information. Only two-thirds (65.8%) attempted to describe risks in lay language.[41]
6. Impact of Promotional Material on Risk Communication
Ideally, MAHs should aim to have a joined-up approach to their communications which should all be consistent with a regulatory RMP. The negative impact of industry communication is reflected in a study that assessed the main causes of warning letters issued by the FDA for promotional claims related to medications.[42] This study found evidence of poor risk communication practice (of course many of these letters predated regulatory risk management planning). Between May 1995 and June 2007, a total of 8692 warning letters were issued, of which 25% were related to drugs. Of these, 206 warning letters focused on drug promotion and were included in the analysis. In total, 47% of the warning letters were issued because of false or misleading unapproved doses and uses, 27% failed to disclose risks, 15% cited misleading promotion, 8% related to misleading labelling and 3% promoted false effectiveness claims.[41] This includes one product under intense regulatory scrutiny with a high profile risk management programme — oxycontin.[43]
There have been assessments of how promotional material affects risk perception and understanding by the public. Most evidence for this concerns impact of DTC advertising in the US. In an assessment in 2005, 60% of people surveyed thought advertisements did not provide enough information about risks, whereas 44% stated advertisements lacked sufficient information about benefit.[44] A study of university students looked at how recall and recognition of risk disclosures in prescription drug television commercials were affected by how that information is presented. The results showed that risk disclosures presented either visually or visually and auditory increased the likelihood of recall and recognition compared with no presentation. Risk disclosures presented concurrently in visual and auditory modalities produced the highest recall and recognition. The results suggest visual risk disclosures produce better recall and recognition than auditory risk disclosures.[45] To obtain a more up-to-date position in the US, the FDA convened a panel of TV advert experts to study how much people are influenced during DTC prescription drug ads by such factors as ‘images, scene changes, words on the screen and music that occur at the same time as an audio presentation of risk information.’ According to a June 2011 report, the panel found evidence that adverts with the most positive visuals gave viewers positive feelings about the drugs, but ‘because of a flaw in the experiment’, the group said it could draw no conclusions on a key question: whether the tone of visuals affected comprehension of risks.[46]
It is evident from the studies described and other existing research that effective communication requires understanding how different audiences perceive the message and what the fundamental drivers are for altering patient and prescriber behaviour. As we know, this is largely attributed to the effects of teamwork, tasks, equipment, workspace, culture and organization on human performance.[47]
7. Legal Obligations for Companies: The Emphasis on Commercial Transparency
The ability of listed pharmaceutical companies to communicate risk is made more complex by the tension between drug regulatory obligations, product liability and requirements of the stock markets. A company listed on the markets must disclose ‘inside information’ that concerns it as soon as possible in a way that avoids creation or continuance of false markets or else a company risks accusations of trying to mislead investors. In particular, if information is not disclosed, insider trading will be suspected. ‘Inside information’ is information that is:
-
of a precise nature that is not generally available;
-
directly or indirectly related to an issuer of securities or investment;
-
likely to have a significant effect on price in the sense that would an investor base their decision on this information.
Thus, it is easy to see how information about both benefit and risk could constitute ‘inside information’. Failure to report to the markets or financial regulator (especially the Securities and Exchange Commission in the US) can result in heavy financial penalties for the company, its officers or other connected persons. The financial authorities may delist or suspend trading, and certain offences such as insider dealing and market abuses carry heavy criminal penalties (UK: unlimited fines and/or up to 7 years imprisonment; US: fines up to $5 million and/or up to 20 years plus civil penalties up to three times trading gains or losses avoided and shareholder litigation which may result in substantial damages). The Wyeth versus Levine case was a landmark case in the US as it means companies are potentially liable for failure to make appropriate label changes without FDA action.[48] Thus, a license holder is required to maintain the product label in accordance with FDA laws and regulations irrespective of the FDA’s explicit instructions or approval, which is similar to the EU.
The penalties of delays and likelihood of enforcement in financial disclosure may exceed that of pharmaceutical regulation.[49] As described by the UK Financial Services Authority, “If a company is faced with an unexpected and significant event, a short delay may be acceptable if it is necessary to clarify the situation. In such circumstances a holding announcement should be used when there is a danger of inside information leaking out before the facts and their impact can be confirmed.” When assessing a new risk, a company can delay disclosure if such a delay would not be deemed as misleading the investment community. An example of how this can go seriously wrong was the censure the company British Biotech received from the UK Stock Exchange because it misled investors and broke rules over directors’ share dealings. This related to continuing press releases about the future launch of a product called Zacutex® (lexipafant) despite being informed by the EU Committee for Proprietary Medicinal Products that the product was unapprovable.[50]
This regulatory complexity of pharmaceutical and financial regulation is illustrated by problems that embroiled Allergan’s product Botox®. The FDA imposed a REMS relating to Botox® requiring dissemination of safety information to healthcare professionals (HCPs) relating to both approved indications and off-label uses. Although from the outset this could result in potential Office of Inspector General compliance violations, failure to comply with REMS provisions may lead the FDA to render a drug ‘misbranded’ by violating statutory marketing requirements. However, Allergan had previously determined that information on appropriate patient selection, injection sites and dosage, even if regarding off-label uses that were reported in the medical literature, would benefit HCPs, increase patient safety and potentially assist in product liability. Allergan filed a suit against the FDA in 2009 challenging its policies regarding dissemination of truthful, accurate and non-misleading information, even if off-label. In the interim, the Department of Justice had filed a suit against Allergan for off-label promotion and marketing of Botox®, citing violations of the Federal Food, Drug, and Cosmetic Act and the False Claims Act. Settlement in 2010 resulted in fines/forfeiture of $US375 million, additional payments of $US225 million, resolution of several qui tam actions, and imposition of a 5-year Corporate Integrity Agreement. The Department of Justice also required dismissal by Allergan of its action against the FDA.[51]
Thus, the legal system in the US can perversely impair risk communication by making companies confusingly try and comply with conflicting sets of regulations. The role of the legal system must be examined in relation to the regulatory system in its capacity as supporting deterrence or compliance to improved risk communication.
8. The Risk Communications Environment for the Pharmaceutical Industry
The communications environment for the industry is polluted with allegations and rumour, is legalistic and riddled with blame culture.[52] The recent controversy concerning rosiglitazone (Avandia®) was based on the muddle around communicating risk with mixed messages from different regulators and allegations of data suppression, misrepresentation and statistical skullduggery.[53] Trust is essential for effective risk communication, but trust in the pharmaceutical industry has been severely tarnished by the shortages that have occurred of potentially lifesaving drugs and suspicions of price gouging aggravated by cases of investigation of alleged healthcare fraud and accusation of conflicts of interest.[54,55]
On top of this, the industry has to operate in a global environment with differing regulatory expectations and a 24-hour news culture. The number of information sources for patients has never been greater, particularly with the rise of social media. As for patients, unsolicited direct communication from the industry, even to incentivize safe practice, is strongly discouraged and even ‘illegal’ in many countries.[56] The sad paradox is that consumers prefer detailed, readily accessible risk information and yet risk communication is currently driven by regulatory requirements rather than by best presentation of the evidence for the product concerned and best use of communication science. Such patient preferences are a major departure from current pharmaceutical communication practices and from what current and proposed regulations require.[57,58] As of 2010, the Affordable Care Act in the US recognized in legislation the importance of communicating basic health information to help patients make appropriate health decisions, which includes ‘benefit-risk’ communication about medicines. In addition the US Plain Writing Act of 2010, requires all new publications, forms and publicly distributed documents from the federal government to be written in a ‘clear, concise, well organized’ manner.[59] Although there is the REMS programme, the authors are not aware of any recent industry initiatives to improve actual content of communication materials to meet health literacy needs. Confining risk communication to templates (such as for the SmPC and PIL) has the potential to restrict flexibility and the way a company can adapt to different stakeholders.[60] A study that illustrates the need to be flexible with the patient leaflet templates looked at how a plain language, pictogram-based intervention could be used as part of medication counselling. The results suggested decreased medication dosing errors and improved adherence among multi-ethnic, low socioeconomic status caregivers whose children were treated at an urban paediatric emergency department.[61]
9. Global Risk Communication Difficulties Despite the International Conference on Harmonisation
The differential implementation of ICH E2E guidelines is similar to the experience with other ICH guidelines as they too have been variably implemented into regulation. Thus, although each ICH region signed up to ICH E2E, the way this has been translated into law at different speeds has been fundamentally different as has attitudes to enforcement. In addition, significant regions in the world have had no direct input into the ICH process (Australia, Canada) and some of the emerging markets (that is, Brazil, Russia, India, China) have no obligation to adopt ICH guidelines.
The industry itself is very heterogeneous with no unifying global industry association with compulsory membership. The operation of some parts of the industry is not at all transparent, particularly with respect to the supply chain. Thus, because of human factors and sociopolitical factors there is variable understanding about what ‘safety’ is and what is ‘risk’ between companies and with their stakeholders.[62] Not all parts of the heterogeneous pharmaceutical sector are equally committed to communicating risk beyond labelling. All the published evidence primarily refers to ICH regions. As a result there is no common understanding between industry and regulators about what we are trying to achieve with risk communication. Is it to:
-
Inform only?
-
Inform and help understand/interpret?
-
Inform, help understand/interpret and change behaviour temporarily for that course of therapy?
-
Or inform, help understand and change behaviour permanently?
10. Conclusions
Ideally, quantifying a risk is best referring to a multiplicity of aids and tools for presenting the numbers although it will always be difficult to overcome uncertainty and to move from population to individuals, which is why a team effort is needed involving doctors/nurses/carers to help perform this extrapolation.[63] Given the central role that the industry gives to product information such as the SmPC, it is surprising that there has not been extensive original research to see whether the SmPC is a good tool for communicating risk. There is need to evaluate the impact of user testing at the European level since the introduction of a revised template.
Communicating risk for listed companies is made more complicated because they must consider their obligations to the market and investors when communicating safety and efficacy issues. There needs to be internal coordination for simultaneous release. Internal communications about significant issues should be restricted to those who need to know how to manage risk of insider dealing and internal communication which may later be disseminated after careful considerations. In reality, how much influence can the industry have over the behaviour of significant stakeholders, i.e. doctors and patients, in the safe use of medicines? In the EU doctors can only be mandated to follow a certain course of action with a medicine if this is instructed in the SmPC. If patients buy medicines from Internet suppliers, how can they be sure that not only will they get the information but that it is accurate? The industry should more actively sponsor efforts to align safety cultures between the pharmaceutical and healthcare sector. However, a company needs to look at its entire communication strategy if it wants to convincingly communicate risk. There needs to be an impartial safety review step of promotional material to ensure the messages are entirely consistent with those agreed for the risk communication programme.
Building trust is critical for effective communication. The reality is that the end user is in receipt of many other sources of information, some of which may be more trusted than a pharmaceutical company. This means physicians learn of safety warnings and alerts from a variety of sources such as mainstream and online media, online healthcare sites, colleagues or patients. Risk communication, with or without an RMP, is part of routine pharmacovigilance and so should be adapted taking into account all the scientific evidence for communicating risk not just relying on regulatory templates.
As already in place in some companies, we advise that all companies think of the most efficient way to establish a communications group dedicated to understanding the sensitivity and nuance of the psychological and social factors that influence the way doctors prescribe and the way patients take their medicines.
References
Slovic P, Peters E, Grana J, et al. Risk perception of prescription drugs: results of a national survey. Drug Inf J 2007; 41(1): 81–100
US FDA. FDA alerts health care professionals of infection risk from repackaged Avastin intravitreal injections [online]. Available from URL: http://www.fda.gov/Drugs/DrugSafety/ucm270296.htm [Accessed 2012 Mar 30]
Fierce Healthcare. Hospitalizations for medication and illicit drug-related conditions on the rise among Americans ages 45 and older [online]. Available from URL: http://www.fiercehealthcare.com/press-releases/hospitalizations-medication-and-illicit-drug-related-conditions-rise-among-americans-?utm_medium=nl&utm_source=internal [Accessed 2012 Mar 25]
Lazar K. Nursing home drug use puts many at risk [online]. Available from URL: http://www.boston.com/news/health/articles/2010/03/08/antipsychotic_drug_use_for_dementia_patients_is_questioned/ [Accessed 2012 Mar 25]
McCleery J. Antipsychotic prescribing in nursing homes. BMJ 2012; 344: 7
White JA. FDA finds problems with insulin pumps ‘across manufacturers’ [online]. Available from URL: http://blogs.wsj.com/health/2010/03/03/fda-finds-problems-with-insulin-pumps-across-manufacturers/tab/print/ [Accessed 2012 Mar 11]
Management of safety information from clinical trials. Report of CIOMS Working Group VI [online]. Available from URL: http://www.cioms.ch/publications/blurbs/management_of_safety_information.htm [Accessed 2012 Jun 3]
SOMO briefing paper on ethics in clinical trials #1: examples of unethical trials February 2008 (updated) [online]. Available from URL: http://somo.nl/html/paginas/pdf/Examples_of_unethical_trials_nov_2006_NL.pdf [Accessed 2012 Mar 12]
Lehman R, Loder E. Missing clinical trial data. BMJ 2012; 314: 1–2
Perfetto EM, Ellison R, Ackermann S, et al. Evidence based risk management: how can we succeed? Deliberations from a Risk Management Advisory Council. Drug Inf J 2003; 37: 127–34
International Conference on Harmonisation of Technical Requirements for Registration of Pharmaceuticals for Human Use. ICH harmonized tripartite guideline: pharmacovigilance planning E2E [online]. Available from URL: http://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E2E/Step4/E2E_Guideline.pdf [Accessed 2012 Mar 25]
Waller PC, Evans SJ. A model for the future conduct of pharmacovigilance. Pharmacoepidemiol Drug Saf 2003; 12(1): 17–29
European Medicines Agency. Annex C: template for EU risk management plan (EU — RMP). Doc. Ref. EMEA/192632/2006 [online]. Available from URL: http://eudravigilance.ema.europa.eu/human/docs/19263206en.pdf [Accessed 2012 Mar 25]
Volume 9A of the rules governing medicinal products in the European Union guidelines on pharmacovigilance for medicinal products for human use [online]. Available from URL: http://ec.europa.eu/health/files/eudralex/vol-9/pdf/vol9a_09-2008_en.pdf [Accessed 2012 Jun 3]
US Department of Health and Human Services, FDA. Guidance medication guides: distribution requirements and inclusion in risk evaluation and mitigation strategies (REMS). November 2011 [online]. Available from URL: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM244570.pdf [Accessed 2012 Aug 23]
Pharmaceutical and Food Safety Bureau, Ministry of Health, Labour and Welfare. Risk Management Plan (RMP) guidance (Draft). August 2011 [online]. Available from URL: http://www.pmda.go.jp/english/service/pdf/mhlw/20110802_RMP.pdf [Accessed 2012 Aug 23]
Medicines and Healthcare products Regulatory Agency. Good pharmacovigilance practice guide. London: Pharmaceutical Press, 2009; 7: 89
Rayner DK. What is wrong with current SmPCs? DIA Product Information Forum. 2011 Jun 8; London
Raynor DK Testing, testing … user testing and how it will revolutionise how we think about patient information leaflets. Pipeline April 2005; 86: 4–5
MHRA. Report of the findings of the survey of user test houses undertaken on behalf of the Commission on Human Medicines Expert Advisory Group on Patient Information (CHMEAGPI) [online]. Available from URL: http://www.mhra.gov.uk/home/groups/pl-a/documents/websiteresources/con2030408.pdf [Accessed 2012 Aug 23]
MHRA. Further guidance on designing patient information leaflets and how to achieve success in user testing. March 2007 [online]. Available from URL: http://www.mhra.gov.uk/home/groups/pl-a/documents/websiteresources/con2030572.pdf [Accessed 2012 Aug 23]
Annex I: summary of product characteristics, and annex III: labelling and package leaflet. Version 8, 07/2011 Rev. 1, 10/2011 [online]. Available from URL: http://www.emea.europa.eu/docs/en_GB/document_library/Template_or_form/2009/10/WC500004368.pdf [Accessed 2012 Mar 30]
CMDh. Position paper on user testing of package leaflet: consultation with target patient groups (compliance with article 59(3) of council directive 2001/83/EC). Doc. Ref: CMDh/234/2011, February 2011 [online]. Available form URL: http://www.hma.eu/fileadmin/dateien/Human_Medicines/CMD_h_/procedural_guidance/Consulation_PatientsGroups/CMDh_234_2011.pdf [Accessed 2012 Mar 11]
The Helen Hamlyn Research Centre. A guide to the graphic design of medication packaging. Second edition [online]. Available from URL: http://www.hhc.rca.ac.uk/cms/files/npsa-design-for-patient-safety-.pdf [Accessed 2012 Mar 11]
Harris E, Enright D. New words for cautionary and advisory labels make them easily understood. Pharm J 2011 Mar; 286: 278–9
EMA. Committee for Human Medicinal Products (CHMP). Guideline on the acceptability of names for human medicinal products processed through the centralised procedure CPMP/328/98 [online]. Available from URL: www.ema.europa.eu/pdfs/human/regaffair/032898en.pdf [Accessed 2012 Aug 23]
Institute for Safe Medication Practices. ISMP’s list of confused drug names [online]. Available from URL: http://www.ismp.org/tools/confuseddrugnames.pdf [Accessed 2012 Aug 23]
WHO, The Joint Commission. Look-alike, sound-alike medication names [online]. Available from URL: http://www.ccforpatientsafety.org/common/pdfs/fpdf/Presskit/PS-Solution1.pdf [Accessed 2012 Aug 23]
Wilke T, Mueller S, Kai N, et al. Does package design matter for patients? The association between package design and patients’ drug knowledge Pharm Med 2011; 25(5): 307–17
Shrank W, Avorn J, Rolon C, et al. Effect of content and format of prescription drug labels on readability, understanding, and medication use: a systematic review. Ann Pharmacother 2007; 41(5): 783–801
van Grootheest ACK, Edwards IR. Labeling and ‘Dear Doctor’ letters: are they noncommittal? Drug Saf 2002; 25(15): 1051–5
Campbell WH, Califf RM. Improving communications of drug risks to prevent patient harm: proceedings of a workshop. Pharmacoepidemiol Drug Saf 2003; 12: 183–94
Goldman SA. Communication of medical product risk: how effective is effective enough? Drug Saf 2004; 27(8): 519–34
Mazor KM, Andrade SE, Auger J, et al. Communicating safety information to physicians: an examination of Dear Doctor letters. Pharmacoepidemiol Drug Saf 2005; 14:869–75
Dusetzina S, Higashi A, Dorsey ER, et al. Impact of FDA drug risk communications on health care utilization and health behaviors: a systematic review Med Care 2012; 50(6): 466–78
Piening S, Haaijer-Ruskamp FM, de Vries JTN, et al. Impact of safety-related regulatory action on clinical practice: a systematic review. Drug Saf 2012; 35(5): 373–85
Harris Interactive. The growing influence and use of health care information obtained online [online]. Available from URL: http://www.harrisinteractive.com/NewsRoom/HarrisPolls/tabid/447/ctl/ReadCustom%20Default/mid/1508/ArticleId/863/Default.aspx [Accessed 2012 Mar 26]
Acharya N, Hochstetler H. Healthcare provider focused communications. 9th Annual DIA Conference on Contemporary Pharmacovigilance and Risk Management Strategies. 2010 Jan 11–13; Washington, DC
ABPI. Pharmacovigilance and the internet: a call for change. A white paper from the ABPI Pharmacovigilance Expert Network, 13 June 2011 [online]. Available from URL: http://www.abpi.org.uk/our-work/library/industry/Pages/pharmacovigilance-the-internet.aspx [Accessed 2012 Aug 23]
Davis JJ, Cross E, Crowley J. Pharmaceutical websites and the communication of risk information. J Health Commun 2007; 12(1): 29–39
Williams B, Brown D. Direct to consumer internet advertising of statins: an assessment of safety. Pharmacoepidemiol Drug Saf 2012; 21: 352–65
Salas M, Martin M, Pisu M, et al. Analysis of US Food and Drug Administration warning letters false promotional claims relating to prescription and over-the-counter medications. Pharm Med 2008; 22(2): 119–25
NDA 20-553, OxyContin© (oxycodone HCl controlled-release) tablets, MACMIS ID# 11400. Released by FDA: 1/17/03. Posted by FDA: 1/22/03 [online]. Available from URL: http://www.pharmcast.com/WarningLetters/Yr2003/Jan2003/PurduePharma0103.htm [Accessed 2012 Mar 11]
Gellad ZF, Lyles KW. Direct-to-Consumer Advertising of Pharmaceuticals. Am J Med 2007; 120: 475–80
Kalshera MJ, Wogalterb MS. Influence of presentation modality on communication of pharmaceutical risk information in direct-to-consumer (DTC) television commercials [online]. Available from URL: http://www.safetyhumanfactors.org/wp-content/uploads/2011/12/284KalsherWogalter2006.pdf [Accessed 2012 Mar 11]
Division of Drug Marketing, Advertising, and Communications, Office of Medical Policy, Center for Drug Evaluation and Research, Food and Drug Administration and Office of Planning, Office of the Commissioner, Food and Drug Administration and Office of the Assistant Secretary for Planning and Evaluation, Department of Health and Human Services. A supplementary test of distraction in DTC advertising using an implicit measure, the affect misattribution procedure. June, 2011 [online]. Available from URL: http://www.fda.gov/downloads/AboutFDA/CentersOffices/OfficeofMedicalProductsandTobacco/CDER/UCM285379.pdf [Accessed 2012 Mar 30]
Clinical Human Factors Group [online]. Available from URL: http://www.chfg.org [Accessed 2012 Jun 3]
Supreme Court of the United States. Wyeth v. Levine. No. 06-1249. Argued November 3, 2008 — Decided March 4, 2009 [online]. Available from URL: http://www.law.cornell.edu/supct/html/06-1249.ZS.html [Accessed 2012 Mar 25]
Curtin T, Relkin E Preamble preemption and the challenged role of failure to warn and defective design pharmaceutical cases in revealing scientific fraud, marketing mischief, and conflicts of interest [online]. Available from URL: http://lawarchive.hofstra.edu/pdf/Academics/Journals/LawReview/lrv_issues_v35n04_CC4_CurtinRelkin_35_4_final.pdf [Ac-cessed 2012 Mar 30]
Exchange censures British Biotech [online]. Available from URL: http://www.execreview.com/1999/06/exchange-censures-british-biotech/ [Accessed 2012 Mar 11]
The United States Department of Justice, Office of Public Affairs. Allergan agrees to plead guilty and pay $600 million to resolve allegations of off-label promotion of Botox®. Wednesday, September 1, 2010 [online]. Available from URL: http://www.justice.gov/opa/pr/2010/September/10-civ-988.html [Accessed 2012 Mar 11]
Newman M. Bitter pills for pharma. BMJ 2010; 341: 632–3
Cohen D. Rosiglitazone: what went wrong. BMJ 2010; 341: 530–5
Largen S. Spartanburg judge upholds $327M verdict against pharmaceutical company [online]. Available from URL: http://www.goupstate.com/article/20111221/ARTICLES/111229952/1051/news?Title=Spartanburg-judge-upholds-327M-verdict-against-pharmaceutical-company [Accessed 2012 Mar 11]
Brian D, Feder N. Joint advisory committee meeting on Yaz and Yasmin: industry ties. January 11,2012 [online]. Available from URL: http://www.pogo.org/pogo-files/letters/public-health/ph-fda-20120111-pogo-letter-fda-advisors.html [Accessed 2012 Mar 11]
European Public Health Alliance Direct-to-consumer communication by pharmaceutical companies? Europeans deserve better [online]. Available from URL: http://www.epha.org/a/3925 [Accessed 2012 Mar 11]
Davis JJ. Consumers’ preferences for the communication of risk information in drug advertising. Health Aff (Millwood) 2007; 26(3): 863–70
Lipkus IM. Numeric, Verbal and visual formats of conveying health risks: suggested best practices and future recommendations. Med Decis Making 2007; 27: 696–713
Berkman ND, Sheridan SL, Donahue KE, et al. Low health literacy and health outcomes: an updated systematic review. Ann Intern Med 2011; 155(2): 97–107
van der Waarde K. Enabling users or readability? Graphic-Design Research May 2005; 1–12
Yin HS, Dreyer BP, van Schaick L, et al. Randomized controlled trial of a pictogram-based intervention to reduce liquid medication dosing errors and improve adherence among caregivers of young children. Arch Pediatr Adolesc Med 2008; 162(9): 814–22
Edwards B, Olsen AK, Whalen MW, et al. Guiding principles of safety. Curr Drug Saf 2007; 2: 135–9
Hugman B. Healthcare Communication. London: Pharmaceutical Press, 2009 Apr
Acknowledgements
The authors would like to thank Professor D.K. Theo Raynor, Professor of Pharmacy Practice, University of Leeds, UK, and LUTO Research Ltd, Dr Bart Cobert, Pharmacovigilance Consultant, for providing useful references and Rosa Chinchilla of NDA Regulatory Science Ltd for providing information about PIL testing. Material has been used from the presentation of Grant Castle, Covington & Burling, at the International Society for Pharmacoepidemiology meeting in Bordeaux, 25 August 2004. No sources of funding were used to prepare this manuscript. Dr Edwards is a consultant for NDA Regulatory Science Ltd who advise pharmaceutical companies on patient leaflets and risk communication. Dr Chakraborty has no conflicts of interest to declare.
This article is part of a theme issue co-edited by Priya Bahri, European Medicines Agency, UK, and Mira Harrison-Woolrych, New Zealand Pharmacovigilance Centre, New Zealand. No external funding was used to support the publication of this theme issue.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Edwards, B., Chakraborty, S. Risk Communication and the Pharmaceutical Industry. Drug Saf 35, 1027–1040 (2012). https://doi.org/10.1007/BF03261989
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03261989