Abstract
Hepatocellular carcinoma (HCC) is one of the most common types of malignant tumor. It is usually asymptomatic in the early stages and tends to be intravascularly and intrabiliary invasive. Therefore, most patients present with incurable disease at the time of detection and early diagnosis of HCC is critical for a good prognosis.
The imaging-based diagnosis of small tumors is relatively inaccurate, as cirrhotic and dysplastic nodules mimic HCC radiologically. The availability of a suitable serological marker to distinguish between HCC and benign liver lesions would, therefore, be very useful for early diagnosis. The only serological marker currently widely used for the diagnosis of HCC is alphafetoprotein (AFP). However, the sensitivity of this marker is limited (41–65%). Given the high heterogeneity of HCC, it is currently thought that an optimal serological test for HCC will be based on the simultaneous measurement of two or three highly specific serological markers.
Several laboratories have recently reported that glypican-3 (GPC3), a membrane-bound proteoglycan, is expressed by a large proportion of HCCs, but is undetectable in normal hepatocytes and non-malignant liver disease. Furthermore, various studies demonstrated that GPC3 could be used as a serological test for the diagnosis of patients with HCC. Although the specificity of the test was very high in the context of a population with chronic liver disease, the sensitivity was limited (within the same range as AFP). Interestingly, in most cases, elevated GPC3 values did not correlate with elevated AFP values. As a consequence, the serological level of at least one of the two markers was elevated in a large majority of HCC patients. These results suggest that the sensitivity of the diagnostic test can be significantly improved without compromising specificity with the simultaneous measurement of both GPC3 and AFP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
1. Hepatocellular Carcinoma
Hepatocellular carcinoma (HCC) is the fifth most common neoplasm in the world, and the third most common cause of cancer-related death.[1–4] Every year more than 500 000 new cases are diagnosed worldwide.[3,4] Although HCC is more common in Asia and Africa, its incidence has increased substantially in many Western countries during the last twenty years.[3,5,6] A recent study comparing the molecular clock of hepatitis C virus in the US and Japan predicts that the burden of HCC in the US will reach that of Japan in the next two to three decades.[7]
HCC is usually asymptomatic in the early stages and has a tendency for intravascular or intrabiliary invasion, even when the primary tumor is small.[8] Thus, when HCC symptoms appear it is at an advanced stage. Early diagnosis is, therefore, critical for a good prognosis. Historically, only 10–20% of primary HCCs are found to be resectable at the time of diagnosis.[8] More recently, with the advent of HCC screening programs, the proportion of potentially curable tumors has increased, although the percentage is still small.
HCC is associated with chronic liver injury, primarily chronic viral hepatitis and alcoholic liver disease.[3,4,9] The highest incidence of HCC is found in areas where the hepatitis B (HBV) and hepatitis C virus (HCV) are endemic. In the case of HBV, it has been demonstrated that the relative risk of developing HCC is 25- to 35-fold greater in individuals with evidence of chronic infection compared to non-infected individuals.[10] In chronic HCV there are no estimates of relative risk, but the incidence of HCC in cirrhotic carriers of HCV may be as high as 5% per year, compared with 0.5% in HBV carriers.[11] Persistent HCV infection is the cause of 70% of HCC cases in Japan, and the most likely reason for the rising incidence of HCC in North America is the increased spread of HCV infection within the population.[12,13]
2. Diagnosis
Diagnosis of HCC is usually easy in patients with a space-occupying lesion on ultrasonography or computed tomography, and serological alphafetoprotein (AFP) of more than 400 ng/mL.[8] In many cases, however, by the time these conditions are met, the HCC is incurable, as frequently the AFP is not diagnostically elevated.
Diagnosis by the imaging of small lesions is relatively inaccurate, whether by ultrasonography, computed tomography scanning, or MRI.[8,14] In particular, the two benign lesions which may mimic HCC radiologically are cirrhotic and dysplastic nodules. Liver biopsy of small lesions is also insufficiently sensitive or specific.[15] Even with a needle biopsy, a well-differentiated cancer may be difficult to distinguish from a benign lesion due to the limited amount of material usually obtained by this procedure.[8] Thus, despite advances in imaging technology, there is still a need for suitable serological markers to distinguish between HCC and benign liver lesions in difficult cases.
3. Screening
One striking feature of HCC is that most of the risk factors are well known: at least 90% of cases occur in patients with chronic liver disease (CLD), and most also have cirrhosis.[16] Thus, a sensitive and specific serological marker for HCC would also be useful for the screening of patients at risk. For example, the risk for HCC in patients with cirrhosis is estimated to be 1–4% per year. This risk is clearly higher than the 0.2% per year at which the consensus suggest that surveillance is warranted.[17]
Although the screening of patients at risk of HCC is widely applied, as yet there is little data to suggest that it has been effective in reducing disease-specific mortality.[18] The most common screening protocol includes a serological AFP test and ultrasound. One of the reasons why screening has not been shown to be effective is that the serological AFP test currently used has limited sensitivity.[19,20] Thus, we also need better serological tests to improve screening protocols.
4. Molecular Markers
The only serological marker widely used for the screening and diagnosis of HCC is AFP. This protein is synthesized in large quantities during embryonic development by the yolk sac and liver.[21,22] AFP concentration in the serum decreases gradually after birth to <10 ng/mL by the time a child is 12–18 months old; in females, it reappears in maternal serum during pregnancy. Increased circulating AFP has been associated with HCC, gastric carcinoma, lung cancer, pancreatic cancer, biliary tract cancer, and testicular carcinoma.[21]
A recent systematic review of the published literature shows that at a cut-off value of 20 ng/mL AFP displays between 41–65% sensitivity and 80–94% specificity (HCC vs CLD) for the diagnosis of HCC;[23] for small tumors, sensitivity is around 40%.[22,24] AFP can also be moderately elevated in some patients with benign liver disease.[25] If a higher cut-off value is used, the specificity of the test will increase but, obviously, the sensitivity will be reduced.[23] Due to the limited sensitivity, particularly for small tumors, the usefulness of AFP measurement as a diagnostic test and surveillance tool for patients at risk for HCC has been questioned.[26,27] It has been proposed that the only circumstance in which the measurement of AFP is justified is for the confirmation of an initial diagnosis based on an imaging technique.[27]
Given the limitations of the AFP test, the search for more sensitive serological markers for HCC has continued. Other molecules have been investigated as potential markers, including des-gamma carboxy-prothrombin (DGCP, also called protein induced by vitamin K absence or antagonist-II [PIVKA-II]),[28–31] and the AFP variant AFP-L3.[32] None of these markers have been conclusively shown to be more sensitive than AFP.[33] DGCP is currently being used in Japan, but has not been recommended by the European Association for Study of the Liver (EASL).[34]
HCCs are very heterogeneous tumors,[35] therefore the difficulties in finding good tumor markers are not surprising. In fact, as the evidence for HCC heterogeneity accumulates, it is increasingly evident that it is unlikely that a single marker will be found to display both very high sensitivity and specificity. Thus, it is reasonable to propose that an optimal serological test for HCC will be based on the simultaneous measurement of two or three highly specific serological markers.
5. Glypican-3, a Novel Serological and Histochemical Marker for Hepatocellular Carcinoma
The glypicans are a family of heparan sulfate proteoglycans (HSPGs) linked to the exocytoplasmic surface of the plasma membrane by a glycosyl-phosphatidylinositol anchor.[36–39] To date, six glypicans have been identified in mammals (GPC1 to GPC6).[39,40] Genetic and functional studies performed in Drosophila, Xenopus, Zebrafish, and mammals have demonstrated that glypicans can increase the signaling activity of Wnts, hedgehogs, and bone morphogenetic proteins (BMPs).[41–52] In the specific case of Wnts, glypicans have been reported to stimulate both the canonical and non-canonical pathways.[42,47,48] Since Wnts are known to bind to heparan sulfate,[53] it has been proposed that the stimulatory activity of glypicans is based on their ability to act as facilitators of the interaction between Wnts and their receptors.[42] This hypothesis has been supported by the finding that several Wnts can co-immunoprecipitate with glypicans.[48,49,54] In addition to acting as facilitators of ligand-receptor interactions, glypicans may play a role during development in the transport of Wnts, hedgehogs, and BMPs for the purpose of morphogen gradient formation.[52,55]
In 1997 Hsu et al.[56] reported the identification of a transcript that was up-regulated in HCC. This transcript, which had been previously named MXR7,[57] was later called glypican-3 (GPC3).[58] These investigators found that GPC3 messenger RNA (mRNA) was expressed in 143 of 191 (75%) primary and recurrent HCCs, but in only 5 of 154 (3%) normal livers. In addition, no GPC3 expression was detected in three hepatocellular adenomas or in six cholangiosarcomas.[56]
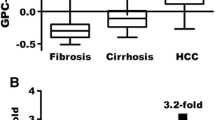
Three other reports confirming the over-expression of GPC3 mRNA in HCC have been published more recently.[59–61] In one of these studies the authors compared the levels of GPC3 mRNA in HCC versus normal liver, focal nodular hyperplasia (a benign lesion), and liver cirrhosis.[59] They found that GPC3 mRNA values in focal nodular hyperplasia and liver cirrhosis were similar to those of normal liver, and that levels of GPC3 in HCCs were above the mean value of the non-malignant groups in 25 of 30 (83%) patients. Based on these results the investigators proposed that GPC3 could be a useful marker to differentiate between benign and malignant liver tissue.[59]
In our laboratory we decided to investigate whether the increase in GPC3 mRNA found in HCC by other investigators was accompanied by an equivalent increase in the levels of the corresponding protein. To this end, we generated monoclonal antibodies against the C-terminus of GPC3 that are able to stain paraffin-embedded tissue sections. Using these antibodies we found that GPC3 was expressed in 21 of 29 (72%) of HCCs, whereas it was not detectable in hepatocytes from normal liver and benign liver diseases[62] (figure 1). These results are clearly consistent with those from the mRNA studies discussed above. Another interesting aspect of the immunohistochemical study was the finding that GPC3 is expressed in small tumors (<3cm), a property that is very important for a tumor marker to be used for diagnostic purposes. Overexpression of GPC3 in HCC tissue sections at the protein level has been also reported by another laboratory.[63]
Immunohistochemical staining of hepatocellular carcinoma sections with the anti-glypican-3 (GPC3) 1G12 monoclonal antibody. (a) Low power picture of a GPC3-positive multinodular hepatocellular carcinoma surrounded by GPC3-negative non-malignant areas, including hepatocytes, blood vessels, and bile ducts; (b) high power picture of the same stained hepatocellular carcinoma section, showing membrane and cytoplasmic staining; and (c) GPC3-negative dysplastic nodule.
Since the immunostaining pattern of GPC3 in HCC tissue sections showed that this glypican can also be seen in the intercellular space, we decided to investigate whether GPC3 could be found in the sera of HCC patients. To this end, we established a sandwich ELISA, using one of our monoclonal antibodies (1G12) and an anti-GPC3 polyclonal antibody.[62] In our initial study, we found that whereas GPC3 was undetectable in the serum of 53 healthy donors and 18 patients with hepatitis, this glypican could be found in the serum of 18 of 34 (53%) of the patients with HCC. In addition, only 1 of 20 patients with hepatitis plus liver cirrhosis displayed elevated levels of GPC3.[62] Thus, the specificity of the serological GPC3 test for the diagnosis of HCC in a population of patients with CLD was very high in this study (97%). On the other hand, sensitivity was limited. In this regard it is important to note that we also measured serological AFP in the same set of HCC patients and found that, at a cut-off level of 20 ng/mL, AFP was elevated in 59% of samples. Interestingly, in most cases elevated GPC3 values did not correlate with elevated AFP values. As a consequence, at the standard cut-off value of 20 ng/mL for AFP, the serological level of at least one of the two markers was elevated in 82% of HCC patients. These results suggest that the sensitivity of the diagnostic test can be significantly improved without compromising specificity by the simultaneous measurement of both GPC3 and AFP.
Two other recent studies have confirmed our results with regard to the potential role of GPC3 as a marker for HCC.[64,65] In addition, both reports confirmed the lack of overlap between GPC3 and AFP values in HCC patients. In the Nakatsura et al.[64] study, the sensitivity of the GPC3 test was somewhat lower than in our study (40%). However, it has to be noted that Nakatsura et al.[64] used for their GPC3 ELISA a commercially available polyclonal antibody which is clearly not very specific, since it detects multiple additional protein bands in Western blots that do not correspond to GPC3 (see figure 2 in Nakatsura et al.[64] ). Moreover, to standardize their assay they used supernatants of GPC3-expressing cells, which contain many other proteins in addition to GPC3.[64] This could increase the background in the ELISA and reduced the sensitivity of the assay.
In the study by Hippo et al.,[65] the sensitivity of the GPC3 test was similar to that of our study. Surprisingly, however, the authors claimed that they could not detect GPC3 in the serum of HCC patients if they used a monoclonal antibody raised against the C-terminus. They proposed, therefore, that in HCC cells GPC3 is released by a protease that leaves the C-terminus of GPC3 bound to the cells. Our results, however, indicate that at least a large proportion of serum GPC3 contains the C-terminus, since by using an antibody against such terminus we could detect GPC3 in 53% of patients by using ELISA. In addition, we can also detect GPC3 in serum by Western blot analysis using the same antibody.[66]
6. Conclusion
Data reported by several laboratories indicate that GPC3 is specifically overexpressed in a majority of patients with HCCs, and that GPC3 could be used as a histological and serological marker for HCC. Furthermore, results published to date suggest that, although the sensitivity of the serological GPC3 test is limited, the combined used of AFP and GPC3 could provide a highly specific and sensitive diagnostic test for HCC. It is also possible that the combined use of GPC3 and AFP would provide an improved test to screen the large number of cirrhotic patients that are at risk of developing HCC. Certainly, further studies are required to test this hypothesis.
References
Parkin DM, Pisani P, Ferlay J. Global cancer statistics. CA Cancer J Clin 1999; 49(1): 33–64
Okuda K, Kojiro M. Neoplasms of the liver. In: Schiff L, Schiff ER, editors. Diseases of the liver. 7th ed. Philadelphia (PA): JB Lippincott Co., 1993
Bruix J, Boix L, Sala M, et al. Focus on hepatocellular carcinoma. Cancer Cell 2004; 5: 215–9
Llovet JM, Burroughs A, Bruix J. Hepatocellular carcinoma. Lancet 2004; 362: 1907–17
Befeler AS, Di Bisceglie AM. Hepatocellular carcinoma: diagnosis and treatment. Gastroenterology 2002; 122: 1609–19
El-Serag HB. Hepatocellular carcinoma: recent trends in the United States. Gastroenterology 2004; 127 (5 Suppl. 1): S27–34
Tanaka Y, Hanada K, Mizokami M, et al. A comparison of the molecular clock of hepatitis C virus in the United States and Japan predicts that hepatocellular carcinoma incidence in the United States will increase over the next two decades. Proc Natl Acad Sci U S A 2002; 99: 15584–9
Fong Y, Kemeny N, Lawrence T. Cancer of the liver and biliary tree. In: DeVita VT, Hellman S, Rosenberg SA, editors. Cancer: principles and practice of oncology. 6th ed. Philadelphia (PA): Lippincott Williams & Wilkins, 2001
Rustgi VK. Epidemiology of hepatocellular carcinoma. Gastroenterol Clin North Am 1987; 16: 545–51
Wands JR. Prevention of hepatocellular carcinoma. N Engl J Med 2004; 351: 1567–70
Di Bisceglie AM. Hepatitis C and hepatocellular carcinoma. Semin Liver Dis 1995; 15: 64–9
Hasan F, Jeffers LJ, De Medina M, et al. Hepatitis C-associated hepatocellular carcinoma. Hepatology 1990; 12: 589–91
El-Serag HB, Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med 1999; 340: 745–50
Murakami T, Kim T, Oi H, et al. Detectability of hypervascular hepatocellular carcinoma by arterial phase images of MR and spiral CT. Acta Radiol 1995; 36: 372–6
Levy I, Greig PD, Gallinger S, et al. Resection of hepatocellular carcinoma without preoperative tumor biopsy. Ann Surg 2001; 34: 206–9
Bosch FX, Ribes J, Diaz M, et al. Primary liver cancer: worldwide incidence and trends. Gastroenterology 2004; 127: S5–S16
Di Bisceglie AM. Issues in screening and surveillance for hepatocellular carcinoma. Gastroenterology 2004; 127: S104–7
Collier J, Sherman M. Screening for hepatocellular carcinoma. Hepatology 1998; 27: 273–8
Collier J, Sherman M. Elevated alphafetoprotein in benign liver diseases. Viral Hepatitis Rev 1998; 4: 31–41
Daniele B, Bencivenga A, Megna AS, et al. α-Fetoprotein and ultrasonography screening for hepatocellular carcinoma. Gastroenterology 2004; 127: S108–12
Chan D, Sell S. Tumor markers. In: Burtis CA, Ashwood A, Tietz NW, editors. Tietz textbook of clinical chemistry. 3rd ed. Philadelphia (PA): WB Saunders, 1999: 722–49
Taketa K. α-Fetoprotein: reevaluation in hepatology. Hepatology 1990; 12: 1420–32
Gupta S, Bent S, Kohlwes J. Test characteristics of α-fetoprotein for detecting hepatocellular carcinoma in patients with hepatitis C. Ann Intern Med 2003; 139: 46–50
Levy I, Greig PD, Gallinger S, et al. Resection of hepatocellular carcinoma without preoperative tumor biopsy. Ann Surg 2001; 234: 206–9
Johnson PJ. The role of serum alpha-fetoprotein estimation in the diagnosis and management of hepatocellular carcinoma. Clin Liver Dis 2001; 5: 145–59
Trevisani F, D’Intino PE, Morselli-Labate AM, et al. Serum alpha-fetoprotein for diagnosis of hepatocellular carcinoma in patients with chronic liver disease: influence of HBsAg and anti-HCV status. J Hepatol 2001; 34: 570–5
Sherman M. Alphafetoprotein: an obituary. J Hepatol 2001; 34: 603–5
Nomura F, Ishijima M, Kuwa K, et al. Serum des-gamma-carboxy prothrombin levels determined by a new generation of sensitive immunoassays in patients with small-sized hepatocellular carcinoma. Am J Gastroenterol 1999; 94: 650–4
Grazi GL, Mazziotti A, Legnani C, et al. The role of tumor markers in the diagnosis of hepatocellular carcinoma, with special reference to the des-gamma-carboxy prothrombin. Liver Transpl Surg 1995; 1: 249–55
Kasahara A, Hayashi N, Fusamoto H, et al. Clinical evaluation of plasma des-gamma-carboxy prothrombin as a marker protein of hepatocellular carcinoma in patients with tumors of various sizes. Dig Dis Sci 1993; 38: 2170–6
Ishii M, Gama H, Chida N, et al. Simultaneous measurements of serum alphafetoprotein and protein induced by vitamin K absence for detecting hepatocellular carcinoma: South Tohoku District Study Group. Am J Gastroenterol 2000; 95: 1036–40
Li D, Mallory T, Satomura S. AFP-L3: a new generation of tumor marker for hepatocellular carcinoma. Clin Chim Acta 2001; 313: 15–9
Marrero JA, Lok ASF. Newer markers for hepatocellular carcinoma. Gastroenterology 2004; 127 (5 Suppl. 1): S1 13–9
Bruix J, Sherman M, Llovet JM, et al. Clinical management of hepatocellular carcinoma: conclusions of the Barcelona-2000 EASL conference. European Association for the Study of the Liver. J Hepatol 2001; 35: 421–30
Thorgeirsson SS, Grisham JW. Molecular pathogenesis of human hepatocellular carcinoma. Nat Genet 2002; 31: 339–46
Lander AD, Stipp CS, Ivins JK. The glypican family of heparan sulfate proteoglycans: major cell-surface proteoglycans: major cell-surface proteoglycans of the developing nervous system. Perspect Dev Neurobiol 1998; 1: 1–7
Veugelers M, David G. The glypicans: a family of GPI-anchored heparan sulfate proteoglycans with a potential role in the control of cell division. Trends Glycosci Glycotechnol 1998; 10: 145–52
Filmus J, Selleck SB. Glypicans: proteoglycans with a surprise. J Clin Invest 2001; 108: 497–501
Filmus J, Song HH. Glypicans. In: Iozzo RV, editor. Proteoglycans. New York: Marcel Dekker, 2000
Veugelers M, De Cat B, Ceulemans H, et al. Glypican-6, a new member of the glypican family of cell surface proteoglycans. J Biol Chem 1999; 274: 26968–77
Jackson SM, Nakato H, Sugiura M, et al. Dally, a Drosophila glypican, controls cellular responses to the TGF-beta-related morphogen Dpp. Development 1997; 124: 4113–20
Baeg GH, Perrimon N. Functional binding of secreted molecules to heparan sulfate proteoglycans in Drosophila. Curr Opin Cell Biol 2000; 12: 575–80
Perrimon N, Bernfield M. Specificities of heparan sulphate proteoglycans in developmental processes. Nature 2000; 404: 725–8
Paine-Saunders S, Viviano BL, Zupicich J, et al. Glypican-3 controls cellular responses to Bmp4 in limb patterning and skeletal development. Dev Biol 2000; 225: 179–87
Lum L, Yao S, Mozer B, et al. Identification of hedgehog pathway components by RNAi in Drosophila cultured cells. Science 2003; 299: 2039–45
Desbordes SC, Sanson B. The glypican dally-like is required for hedgehog signalling in the embryonic epidermis of Drosophila. Development 2003; 130: 6245–55
Topczewsky J, Sepich DS, Myers DC, et al. The zebrafish glypican knypek controls cell polarity during gastrulation movements of convergent extension. Dev Cell 2001; 1: 251–64
Ohkarawa B, Yamamoto TS, Tada M, et al. Role of glypican 4 in the regulation of convergent extension movements during gastrulation in Xenopus laevis. Development 2003; 130: 2129–38
De Cat B, Muyldermans SY, Coomans C, et al. Processing by proprotein convertases is required for glypican-3 modulation of cell survival, Wnt signaling, and gastrulation movements. J Cell Biol 2003; 163: 625–35
Kramer KL, Yost HJ. Heparan sulfate core proteins in cell-cell signaling. Annu Rev Genet 2003; 37: 461–84
Baeg GH, Lin X, Khare N, et al. Heparan sulfate proteoglycans are critical for the organization of the extracellular distribution of Wingless. Development 2001; 128: 87–94
Han C, Belenkaya TY, Wang B, et al. Drosophila glypicans control the cell-to-cell movement of hedgehog by a dynamin-independent process. Development 2004; 131: 601–11
Cumberledge S, Reichsman F. Glycosaminoglycans and WNTs: just a spoonful of sugar helps the signal go down. Trends Genet 1997; 13: 421–3
Ai X, Do AT, Lozynska O, et al. QSulf1 remodels the 6-O sulfation states of cell surface proteoglycans to promote Wnt signaling. J Cell Biol 2003; 162: 341–51
Fujise M, Takeo S, Kamimura K, et al. Dally regulates Dpp morphogen gradient formation in the Drosophila wing. Development 2003; 130: 1515–22
Hsu HC, Cheng W, Lai PL. Cloning and expression of a developmentally regulated transcript MXR7 in hepatocellular carcinoma: biological significance and temporospatial distribution. Cancer Res 1997; 57: 5179–84
Lage H, Dietel M. Cloning and characterization of human cDNAs encoding a protein with high homology to rat intestinal development protein OCI-5. Gene 1997; 188: 151–6
Pilia G, Hughes-Benzie RM, MacKenzie A, et al. Mutations in GPC3, a glypican gene, cause the Simpson-Golabi-Behmel overgrowth syndrome. Nat Genet 1996; 12: 241–7
Zhu ZW, Friess H, Wang L, et al. Enhanced glypican-3 expression differentiates the majority of hepatocellular carcinomas from benign hepatic disorders. Gut 2001; 48: 558–64
Zhou XP, Wang HY, Yang GS, et al. Cloning and expression of MXR7 in human HCC tissue. World J Gastroenterol 2000; 6: 57–60
Huang JS, Chao CC, Su TL, et al. Diverse cellular transformation capability of overexpressed genes in human hepatocellular carcinoma. Biochem Biophys Res Commun 2004; 315: 950–8
Capurro M, Wanless IR, Sherman M, et al. Glypican-3: a novel serum and histochemical marker for hepatocellular carcinoma. Gastroenterology 2003; 125: 81–90
Sung YK, Hwang SY, Park MK, et al. Glypican-3 is overexpressed in human hepatocellular carcinoma. Cancer Sci 2003; 94: 259–62
Nakatsura T, Yoshitake Y, Senju S, et al. Glypican-3, overexpressed specifically in human hepatocellular carcinoma, is a novel tumor marker. Biochem Biophys Res Commun 2003; 306: 16–25
Hippo Y, Watanabe K, Watanabe A, et al. Identification of soluble NH2-terminal fragment of glypican-3 as a serological marker for early-stage hepatocellular carcinoma. Cancer Res 2004; 64: 2418–23
Filmus J, Capurro M. Glypican-3 as a serum marker for hepatocellular carcinoma [letter]. Cancer Res 2005 Jan 1; 65(1): 372
Acknowledgements
We thank Heather Bird for her help in the preparation of this review.
Funding for work described in this review was provided by the NIH. Dr Filmus does consulting work for Biomosaics.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Filmus, J., Capurro, M. Glypican-3 and Alphafetoprotein as Diagnostic Tests for Hepatocellular Carcinoma. CNS Drugs 8, 207–212 (2004). https://doi.org/10.1007/BF03260065
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03260065