Abstract
Background: A fixed-dose combination (FDC) of four compounds, hydrochlorothiazide 12.5 mg, triamterene 12.5 mg, dihydralazine 12.5 mg and reserpine 0.1 mg (HTDR), is widely used as an antihypertensive treatment in China. Although HTDR has been used in China for more than 30 years, there have been few comprehensive evaluations of this treatment.
Objective: The aim of this study was to investigate the long-term efficacy and tolerability of HTDR in Chinese patients with essential hypertension.
Methods: This was a 36-month, community-based, open-label surveillance study, conducted in the Huangpu District (Shanghai, China). The study was based in local primary healthcare settings. Subjects were recruited if they had essential hypertension, were aged ≥35 years at the time of enrolment, were expected to remain in the area for 3 years, and were able to provide informed consent. Patients who had secondary hypertension, myocardial infarction or stroke within 6 months of screening, impaired renal or hepatic function, history of cardiomyopathy or chronic heart failure, or were pregnant or lactating were excluded. HTDR was administered as one or two tablets per day in the morning. If necessary, additional hydrochlorothiazide was added. Blood pressure (BP) was measured at baseline and throughout the 36-month surveillance period every 3 months. Biochemical indicators (e.g. fasting blood glucose, plasma lipid parameters, plasma sodium and potassium, plasma uric acid and serum creatinine) were also measured, and adverse events were noted. BP reductions and the rate at which patients achieved BP targets (systolic BP [SBP] <140 mmHg and diastolic BP [DBP] <90 mmHg) throughout the period were determined. Subgroup analyses by sex and age were also conducted.
Results: A total of 1529 patients (550 male, 979 female; mean age 65.7 years) entered the study. After the 36-month treatment period, 93.1% of patients had achieved the SBP target, 97.9% had achieved the DBP target, and 92.1% had achieved both. The mean decreases in SBP and DBP were 15.3 mmHg and 9.9 mmHg, respectively. Overall, 127 adverse events in 119 patients (7.8%) occurred during the follow-up period, most of which were mild to moderate. Plasma lipid profiles were improved after 24 months of treatment. In addition, a significant increase in plasma potassium and a significant reduction in plasma uric acid were seen.
Results: A total of 1529 patients (550 male, 979 female; mean age 65.7 years) entered the study. After the 36-month treatment period, 93.1% of patients had achieved the SBP target, 97.9% had achieved the DBP target, and 92.1% had achieved both. The mean decreases in SBP and DBP were 15.3 mmHg and 9.9 mmHg, respectively. Overall, 127 adverse events in 119 patients (7.8%) occurred during the follow-up period, most of which were mild to moderate. Plasma lipid profiles were improved after 24 months of treatment. In addition, a significant increase in plasma potassium and a significant reduction in plasma uric acid were seen.
Conclusion: HTDR was found to have good long-term efficacy and tolerability in Chinese patients with essential hypertension.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Evidence from several clinical studies suggests that the majority of hypertensive patients require more than one antihypertensive medication to reach an acceptable blood pressure (BP) goal[1–4] and most treatment guidelines for hypertension now advocate the use of a combination of two or more drugs in fixed doses to achieve better BP control.[5,6] The advantages of fixed-dose combinations (FDCs) include greater BP-lowering effects, lower doses of component drugs, a lower incidence of clinical and metabolic adverse effects, a longer duration of action, decreased costs and improved patient compliance.[7–9] Many effective and well tolerated FDCs are now available, and their use is increasingly favoured by primary-care physicians and hypertensive patients.
In China the most widely used FDC for hypertension is a compound with four components: hydrochlorothiazide 12.5 mg, triamterene 12.5 mg, dihydralazine 12.5 mg and reserpine 0.1 mg (HTDR). This compound is known in China as ‘Compound Hypotensive Tablets No. 0’ but is here referred to by its acronym, HTDR. The Ministry of Health of China ratified clinical application of this compound in 1977. Compared with other commonly used double or triple FDCs, each component of this FDC has a relatively low dose and therefore less potential for adverse affects.[10] Currently, HTDR is the most widely used quadruple FDC for hypertension in China with more than 15 million Chinese hypertensive patients (>10% of market share) taking this compound.[11–13] However, although HTDR has been used for more than 30 years, its long-term effectiveness and tolerability have not been systematically studied. The widespread use of this combination without evidence of its effects has now become a public health concern. Thus, the aim of this surveillance study was to evaluate the long-term efficacy and tolerability of HTDR in Chinese patients with essential hypertension.
Methods
Study Design
This community-based, open-label surveillance study was conducted in the Huangpu District in Shanghai, China over a period of 36 months. It was designed and organized by the School of Public Health, Peking University, as one of the key tasks of the Community-Based Prevention and Control of Cardiocerebrovascular Disease (CPCC) Project of the China National Tenth Five-Year-Plan Funding Program (2002–7). The protocol was approved by the ethics review boards of the Peking University Health Science Center and all participating subjects gave written informed consent.
Study Population
Subjects were recruited from local primary healthcare clinics in the Huangpu District. Subjects were patients with essential hypertension, aged ≥35 years at the time of enrolment, expected to remain in the area for 3 years, and able to provide informed consent. Initial baseline BP was measured in the morning three times using standardized sphygmomanometers and the mean values calculated. Hypertension was defined as mean diastolic BP (DBP) ≥90 mmHg or mean systolic BP (SBP) ≥140 mmHg, or current use of antihypertensive medication. Exclusion criteria included: secondary hypertension; myocardial infarction or stroke within 6 months of screening; impaired renal or hepatic function; history of cardiomyopathy or chronic heart failure; or being pregnant or lactating.
Treatment
HTDR was administered to all participants with the objective of achieving control of BP (<140/90 mmHg). The initial daily dosage was one HTDR tablet. Another tablet was added if the target BP level had not been reached within 2 months. For those who still did not reach the BP target level at two tablets a day, additional hydrochlorothiazide was commenced. If BP was still not controlled with hydrochlorothiazide after 2 months, patients could be started on other therapeutic regimens, at which point they were excluded from the study. During the 36-month follow-up period, all patients were expected to discontinue all antihypertensive medications except HTDR and hydrochlorothiazide.
All patients were also counselled regarding non-pharmacological methods of BP control, including limiting salt intake, increasing fresh fruit and vegetable intake, weight loss (where appropriate), and the importance of aerobic exercise.
Follow-Up and Data Collection
The study was conducted in the local primary healthcare setting in the communities. The general physicians who participated in this study were well trained and qualified and had considerable research experience.
Routine follow-up visits were scheduled once a month during the first 6 months, then every 3 months thereafter, with additional visits if necessary. At each visit, BP and heart rate were measured for all patients in the same way as at baseline, as described in the Study Population section. Patients were advised to take their regular non-hypertensive medications as usual.
Investigators recorded the severity, time of occurrence, duration and prognosis of adverse events (AEs). AEs were defined as any untoward medical occurrences in a participant that may, or may not, have been caused by HTDR treatment. AEs were classified as mild, moderate or severe in accordance with US FDA practice. Mild AEs were those of a minor irritant type requiring no medication or medical evaluation. Moderate AEs were those interfering with daily activities, but which usually improved with simple therapeutic measures. Severe AEs were events that interrupted the participant’s normal daily activities and generally required systemic treatment, or may have resulted in death, hospitalization or significant disability.
Fasting blood samples were collected at study entry and 24 months thereafter to determine concentrations of plasma sodium and potassium, serum creatinine, plasma uric acid, fasting blood glucose and plasma lipid profiles.
Statistical Analysis
Baseline demographic characteristics are shown as means (and standard deviations) for continuous variables and as numbers (and percentages) for categorical measures. BP parameters after 36 months were calculated for all patients and for different sex and age subgroups (≤60 years, 61–70 years, >70 years). Results in patients who withdrew prematurely were also calculated.
All of the analyses were carried out using Statistical Analysis System software, version 8.2 (SAS Institute, Cary, NC, USA). Only either t- or chi-squared (χ2) tests are reported. All p-values are two sided. p-Values less than 0.05 were considered statistically significant.
Results
Baseline Characteristics
In total 1529 subjects met the inclusion criteria and agreed to take part in the study. Baseline characteristics of the 1529 patients are shown in table I by sex. There were significant differences between men and women in all variables (i.e. age, body weight, height, blood pressure and history of stroke and coronary heart disease) except body mass index and heart rate. Of all the participants, 96.5% were initially taking antihypertensive therapy, but only 21.3% of these patients had their BP under control. Of those who were taking therapy at baseline, 85.3% (n = 1257) were taking antihypertensive monotherapy or an FDC alone, while the remainder were taking two or more separately prescribed antihypertensive agents. The most commonly used agents were FDCs (n = 627; 33.8%), calcium channel antagonists (n = 368; 19.9%), ACE inhibitors (n = 259; 14.0%), diuretics (n = 227; 12.2%) and β-adrenergic antagonists (n = 79; 4.3%).
Treatment and Withdrawal
During the 36-month follow-up, 1421 patients (92.9%) took HTDR exclusively. The other 108 patients (7.1%) took HTDR in combination with additional hydrochlorothiazide, with about 50% of these patients taking the additional treatment for one-third of the follow-up period. In those who took HTDR alone, the majority (1410; 99.3%) took only one tablet a day.
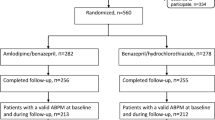
During the study, 376 patients (24.6%) discontinued therapy. The reasons for discontinuation are described in table II. The median time to discontinuation was 7 months, with 172 (45.7%) of the withdrawals occurring within the first 6 months and 281 (74.7%) within the first 12 months. A comparison of the baseline characteristics of patients who withdrew prematurely and patients who remained in the study showed that the sex distribution was similar, i.e. 145 males (38.6%) versus 405 males (35.1%; p = 0.224), respectively. Patients who withdrew were older than patients who remained in the study (mean ± SD age 66.9 ± 10.1 years vs 65.3 ± 9.5 years; p = 0.007) and baseline BP levels were similar between these two groups (mean ± SD SBP 146.8 ± 9.5 vs 146.0 ± 9.6 mmHg, p = 0.146, respectively; mean ± SD DBP 88.5 ± 7.5 vs 88.0 ± 7.6 mmHg, p = 0.361, respectively).
Efficacy
Rate of Achieving Target Blood Pressure (BP)
As indicated in table III, after 36 months of treatment, 1051 (93.1%) of the 1129 patients who remained in the study had achieved only target SBP, 1105 (97.9%) had achieved only target DBP, and 1040 (92.1%) had achieved both targets. When analysed by sex and age (table IV), achievement of target BPs was similar, except for DBP differences by age (96.4% for patients aged ≤60 years, 97.5% for patients aged 61–70 years, and 99.7% for patients aged >70 years; p = 0.008).
Change in Mean BP
After 36 months of treatment, the mean ± SD decrease in SBP in patients who remained in the study was 15.3 ± 11.1 mmHg and the mean ± SD decrease in DBP was 9.9 ± 8.5 mmHg. Subgroup analysis showed that the mean DBP reduction in men was higher than in women (p = 0.009). As indicated in table III, mean SBP and DBP tended to decrease over time with the greatest decrease occurring within the first 12 months of treatment. As shown in table IV, at 36 months, mean DBP had decreased with age and SBP was lower in women than in men.
BP of Patients Who Discontinued Treatment
Table V shows the final BP levels for patients who discontinued treatment (n = 376). 318 (84.6%) of these patients achieved target BP reductions in both SBP and DBP, while 324 (86.2%) achieved only target SBP, and 348 (92.6%) achieved only target DBP. From baseline to withdrawal, the mean ± SD change in SBP was 13.6 ± 11.7 mmHg and the mean ± SD change in DBP was 8.5 ± 9.2 mmHg. Patients who withdrew from the study were divided into four groups, i.e. patients who discontinued treatment: within the first 3 months, from 3–6 months, from 6–9 months, and after 9 months. Baseline SBP and DBP measurements were similar among the four groups, but the final SBP and DBP measurements differed (SBP: F = 2.950, p = 0.033; DBP: F = 7.290, p < 0.001), as did the proportion of patients who achieved target BP (SBP: χ2 = 12.045, p = 0.007; DBP: χ2 = 13.709, p = 0.003; total BP: χ2 = 14.410, p = 0.002).
Adverse Events
Overall, 127 AEs in 119 participants (7.8%) were reported. Of the 127 adverse events, 38 (29.9%) were mild, 66 (52.0%) were moderate and 23 (18.1%) were severe. Seventy-three percent of the AEs occurred within 6 months. The most common AEs were dizziness (26.0%), death (18.1%), abdominal discomfort (11.8%), palpitation (11.8%), sleepiness (9.4%), chest distress (4.7%), headache (4.7%), fatigue (3.9%) and nausea (3.1%). The 23 severe AEs occurring in the study were all deaths unrelated to treatment. Fifty-three patients discontinued from the study because of AEs, including death (n = 23), dizziness (n = 9), abdominal discomfort (n = 8), fatigue (n = 4), palpitations (n =2), arthralgia (n = 2), depression status (n = 2), diarrhoea (n = 1), chest distress (n = 1) and bradycardia (n = 1). The symptoms of AEs in the other 66 patients who continued in the study were successfully mitigated with treatment where necessary.
Biochemical Analyses
Changes in biochemical parameters over 24 months’ treatment are shown in table VI. Total cholesterol, low-density lipoprotein cholesterol, alanine aminotransferase, uric acid and creatinine all decreased, while the remaining parameters, i.e. high-density lipoprotein cholesterol, triglycerides, glucose, sodium and potassium, increased. Some of the differences were statistically significant, although clinically unimportant.
Discussion
We have presented the results of a follow-up investigation of 1529 patients treated for hypertension with HTDR, a compound that consists of hydrochlorothiazide, triamterene, dihydralazine and reserpine. The results have shown that, after treatment for 36 months, mean SBP decreased by 15.3 mmHg, mean DBP decreased by 9.9 mmHg, and the proportion of patients whose BP was under control was 92.1%.
The observed mean BP reductions in the study were substantial. The 15.3/9.9 mmHg SBP/DBP reductions are consistent with results for thiazide combinations reported in a meta-analysis.[14] The reductions occurred in all age groups and both sexes. Previous studies have shown that a prolonged 10–14 mmHg lower level of usual SBP or 5–6 mmHg lower level of DBP is associated with about a 40% lower risk of stroke, a 17% lower risk of coronary heart disease, and a 33% lower risk of all cardiovascular events.[15] The SBP and DBP levels of the study patients steadily decreased over time, with the greatest decline occurring within the first 12 months. After 36 months’ treatment, older patients had lower SBP and DBP levels and higher BP control rates, but the differences among age groups showed no statistical significance.
A total of 127 AEs occurred in 119 participants (7.8%). Reported adverse events that exceeded 3% incidence were dizziness, death, abdominal discomfort, palpitation, sleepiness, chest distress, headache, fatigue and nausea. All adverse events other than 23 deaths were of mild to moderate severity. None of the deaths could be attributed to the HTDR treatment. Hypokalaemia and hyperuricaemia are the most specific adverse events of hydrochlorothiazide,[16,17] but the biochemical analyses showed an apparent increase in plasma potassium and an apparent reduction in plasma uric acid, although these changes were not clinically significant. Previous studies have shown that hydrochlorothiazide in high doses (25 mg/day) may cause unfavourable changes in carbohydrate metabolism and in the plasma lipid profile.[18–20] These changes may limit the response to antihypertensive therapy.[21] However, in our study, biochemical analyses showed that plasma lipid profiles improved slightly, and fasting glucose did not change. Use of a combination of drugs in low doses may partially explain the different results observed in our study.[22] In addition, because we did not restrict the use of cardiovascular drugs (such as statins) other than other antihypertensive agents, the true effect of HTDR may have been confounded.
Although there has been some concern that reserpine, one of the compounds included in HTDR, may cause depression,[23] only two cases of depression were observed in our study. However, we did not use a mood scale (such as the Center for Epidemiologic Studies Depression Scale) to actively observe depression; it was reported only as an adverse event by the physicians and mild depression status may have gone unnoticed.
There are some potential limitations to this study. Firstly, as participants in the study were recruited from only one community and were not randomly selected, the generalizability of our findings may be limited. Secondly, the study had a relatively high dropout rate of 24.6%. Withdrawers were older than patients who remained in the study, which may have biased the results. Thirdly, as all patients in this study were also advised about non-pharmaceutical interventions, the pure effect of HTDR may have been confounded. Fourthly, there was no initial washout period for the study, although this is not a major concern given the long follow-up period of this study. Finally, this was an observational surveillance study and did not include a parallel control group.
Conclusion
Although this study had limitations, it is the first study with a sufficiently large sample to evaluate a widely used Chinese antihypertensive compound. As it is a surveillance study, the study provides a profile of the typical antihypertensive effects of HTDR. The major conclusion of this study is that HTDR is well tolerated and offers prolonged, stable efficacy in lowering BP.
References
Dahlöf B, Sever PS, Poulter NR, et al. Prevention of cardiovascular events with an antihypertensive regimen of amlodipine adding perindopril as required versus atenolol adding bendroflumethiazide as required, in the Anglo-Scandinavian Cardiac Outcomes Trial-Blood Pressure Lowering Arm (ASCOT-BPLA): a multicentre randomised controlled trial. Lancet 2005 Sep; 366(9489): 895–906
Julius S, Kjeldsen SE, Weber M, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet 2004 Jun; 363(9426): 2022–31
Jamerson K, Weber MA, Bakris GL, et al. Benazepril plus amlodipine or hydrochlorothiazide for hypertension in high-risk patients. N Engl J Med 2008 Dec; 359(23): 2417–28
Destro M, Cagnoni F, D’Ospina A, et al. New strategies and drugs in the treatment of hypertension: monotherapy or combination? Recent Pat Cardiovasc Drug Discov 2010 Jan; 5(1): 69–81
Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the management of arterial hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Eur Heart J 2007 Jun; 28(1): 1462–536
Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003 Dec; 42(6): 1206–52
Gerbino PP, Shoheiber O. Adherence patterns among patients treated with fixed-dose combination versus separate antihypertensive agents. Am J Health Syst Pharm 2007 Jun; 64(12): 1279–83
Schroeder K, Fahey T, Ebrahim S. How can we improve adherence to blood pressure-lowering medication in ambulatory care? Systematic review of randomized controlled trials. Arch Intern Med 2004 Apr; 164(7): 722–32
Gupta AK, Arshad S, Poulter NR. Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension 2010 Feb; 55(2): 399–407
Guglietta A, Guerrero M. Issues to consider in the pharmaceutical development of a cardiovascular polypill. Nat Clin Pract Cardiovasc Med 2009 Feb; 6(2): 112–9
Beijing Double-Crane Pharmaceutical Business Co. Ltd. Compound hypotensive tablets no. 0: summary of product characteristics [online]. Available from URL: http://www.dcpb.com.cn/product/ArticleShow.asp?ArticleID=12. [Accessed 2010 Sep 10]
Kang S, Hu X, Xi X. The strategy Research on Domestic Brand Antihypertensive Drugs in Beijing Market [in Chinese]. Chin J Pharmaceut Technol Economics Management 2009 Mar; 3(3): 32–42
IMS Market Research Consulting (Shanghai) Co., Ltd. Antihypertensive agents: the older the better [in Chinese]. China Drug Store 2010 Jan; 2: 12
Wald DS, Law M, Morris JK, et al. Combination therapy versus monotherapy in reducing blood pressure: meta-analysis on 11,000 participants from 42 trials. Am J Med 2009 Mar; 122(3): 290–300
Whitworth JA. World Health Organization, International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens 2003 Nov; 21(11): 1983–92
Helgeland A, Strommen R, Hagelund CH, et al. Enalapril, atenolol, and hydrochlorothiazide in mild to moderate hypertension: a comparative multicentre study in general practice in Norway. Lancet 1986 Apr; 1(8486): 872–5
Frishman WH, Zawada Jr ET, Smith LK, et al. Comparison of hydrochlorothiazide and sustained-release diltiazem for mild-to-moderate systemic hypertension. Am J Cardiol 1987 Mar; 59(6): 615–23
Fogari R, Zoppi A, Malamani GD, et al. Effects of different antihypertensive drugs on plasma fibrinogen in hypertensive patients. Br J Clin Pharmacol 1995 May; 39(5): 471–6
Krum H, Skiba M, Gilbert RE. Comparative metabolic effects of hydrochlorothiazide and indapamide in hypertensive diabetic patients receiving ACE inhibitor therapy. Diabet Med 2003 Sep; 20(9): 708–12
Lindholm LH, Persson M, Alaupovic P, et al. Metabolic outcome during 1 year in newly detected hypertensives: results of the Antihypertensive Treatment and Lipid Profile in a North of Sweden Efficacy Evaluation (ALPINE study). J Hypertens 2003 Aug; 21(8): 1563–74
Reyes AJ. Diuretics in the therapy of hypertension. J Hum Hypertens 2002 Mar; 16Suppl. 1: 78–83
Padilla MC, Armas-Hernández MJ, Hernández RH, et al. Update of diuretics in the treatment of hypertension. Am J Ther 2007 Mar–Apr; 14(2): 154–60
Quetsch RM, Achor RW, Litin EM, et al. Depressi reactions in hypertensive patients; a comparison of tho treated with Rauwolfia and those receiving no specific antihypertensive treatment. Circulation 1959 Mar; 19(3): 366–75
Acknowledgements
We would like to thank the participating study physicians, nurses, practices and patients for their contribution.
This study was supported by Chinese Science & Technology (S&T) Ministry grant 2001BAF03B02 ‘Community-Based Prevention and Control of Cardiocerebrovascular Disease’, and Chinese Science & Technology (S&T) Ministry grant 2006BAI01A03-(16) ‘Community-Based Comprehensive Prevention and Control for Cardiovascular and Cerebrovascular Diseases’.
The authors have no conflicts of interest that are relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wu, Y., Hu, Y., Tang, X. et al. Long-Term Efficacy and Tolerability of a Fixed-Dose Combination of Antihypertensive Agents. Clin. Drug Investig. 31, 769–777 (2011). https://doi.org/10.1007/BF03256917
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256917