Abstract
It is important for economic evaluations in healthcare to cover all relevant information. However, many existing evaluations fall short of this goal, as they fail to include all the costs and effects for the relatives of a disabled or sick individual. The objective of this study was to analyse how relatives’ costs and effects could be measured, valued and incorporated into a cost-effectiveness analysis.
In this article, we discuss the theories underlying cost-effectiveness analyses in the healthcare arena; the general conclusion is that it is hard to find theoretical arguments for excluding relatives’ costs and effects if a societal perspective is used. We argue that the cost of informal care should be calculated according to the opportunity cost method. To capture relatives’ effects, we construct a new term, the R-QALY weight, which is defined as the effect on relatives’ QALY weight of being related to a disabled or sick individual. We examine methods for measuring, valuing and incorporating the R-QALY weights. One suggested method is to estimate R-QALYs and incorporate them together with the patient’s QALY in the analysis. However, there is no well established method as yet that can create R-QALY weights. One difficulty with measuring R-QALY weights using existing instruments is that these instruments are rarely focused on relative-related aspects. Even if generic quality-of-life instruments do cover some aspects relevant to relatives and caregivers, they may miss important aspects and potential altruistic preferences. A further development and validation of the existing caregiving instruments used for eliciting utility weights would therefore be beneficial for this area, as would further studies on the use of time trade-off or Standard Gamble methods for valuing R-QALY weights. Another potential method is to use the contingent valuation method to find a monetary value for all the relatives’ costs and effects.
Because cost-effectiveness analyses are used for decision making, and this is often achieved by comparing different cost-effectiveness ratios, we argue that it is important to find ways of incorporating all relatives’ costs and effects into the analysis. This may not be necessary for every analysis of every intervention, but for treatments where relatives’ costs and effects are substantial there may be some associated influence on the cost-effectiveness ratio.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The use of cost-effectiveness analyses in the decision-making process has increased during recent decades, as they provide a way to prioritize among health interventions. It is therefore important that these analyses incorporate all relevant information. However, many fall short of this goal, as they fail to include all the costs and effects for the relatives of a disabled or sick individual. In the case of stroke, schizophrenia or Alzheimer’s disease, for example, a large portion of the costs and effects of the disease is carried by the patient’s relatives.[1–3] Relatives’ costs and effects may also be of special importance in the context of children with serious diseases[4] and in caring for older people.[5] If the costs and effects for a patient’s relatives are not considered in analyses of treatments, the results will be incomplete. It is not always clear whether such costs and effects are excluded on purpose, or simply forgotten; however, most analyses do not discuss them at all, indicating that they have been forgotten. In cases where relatives are considered, there seems to be uncertainty over how these costs and effects should be counted in the analysis. It may also be that the choice of disregarding relatives’ costs and effects is taken in order to, consciously or unconsciously, set a boundary for the costs and effects that are relevant for inclusion in the analysis.
Most guidelines for cost-effectiveness analyses agree that the cost of informal caregiving undertaken by relatives should be included in the analysis when a societal perspective is desired.[6,7] Some also mention the inclusion of relatives’ health effects caused by giving informal care,[8,9] but these effects have hardly ever been included in any analysis. Several studies have shown that providing informal care has effects on the care-givers’ quality of life (QOL),[10–13] and it has also been shown that relatives who give care or support to an elderly person often get a reduced QALY weight because of this.[14] Furthermore, effects for the relatives may occur even if no informal care is given. The members of a family are, for example, often negatively affected by one member’s disease or disability even if none of them are providing informal care. This aspect was mentioned by the Washington Panel,[7] who encouraged analysts to think broadly about the people affected by an intervention. The health economic guidelines used by the UK National Institute for Health and Clinical Excellence (NICE)[15] and by the Dental and Pharmaceutical Benefits Agency in Sweden[16] also state that the analysis should consider the relatives. In addition, it has been shown theoretically that the effects of medical interventions cannot correctly be studied from a societal perspective without considering the life and family situations of the disabled or sick individuals, as there are often spillover effects within family members’ utility functions.[17] Some attempts to include the effects of relatives in cost-effectiveness analyses have been made. For example, Prosser et al.[18] discussed how the effects on parents could be included when analysing interventions for children, and they suggested that the analysis should use the family as the unit of analysis instead of the individual. Another example is a study by NICE that included caregivers’ utilities in a sensitivity analysis when analysing pharmaceutical treatments for Alzheimer’s disease.[19] However, there is still no standard procedure for including all relatives’ costs and effects in a cost-effectiveness analysis, and there are still some methodological issues that remain to be resolved.
The objective of this article was to analyse and discuss how relatives’ costs and effects can be measured, valued and incorporated in a cost-effectiveness analysis. Our main focus is on effects (captured in the denominator), as earlier studies concerning relatives have concentrated on costs (caused by providing informal care; and captured in the numerator).
1. Definitions of Relatives’ Costs and Effects
A relative is defined in this article as a person who is likely to be affected by another person’s disease or disability, but is not necessarily related to the person by blood (the term ‘significant others’ is sometimes used in the literature). Most commonly, this is the person’s family members but it may also include close friends, neighbours and colleagues if they are affected by the person’s disease or disability. The costs are most commonly incurred by providing informal care. The effects are generated by the change in well-being caused by being a relative of an individual with a disease or disability. While this may include effects on relatives’ physical health, more commonly it consists of other aspects such as mental health, worry and anxiety for the patient. It may also be caused by foregone labour market opportunities,[20] an aspect that is generally missed in the cost calculation of informal care. Furthermore, it could also indicate that the relatives have health-related altruistic preferences for the patient. This means that relatives value the patient’s health, even if they themselves are not affected by it. The effects do not have to be negative, as there are also positive aspects of providing informal care, for example the feeling of being appreciated by the cared-for patient, spending time together, and so on.[12,21] Brouwer et al.[11] call this process utility from providing informal care, and argue that it is often high when the care is provided on a voluntary basis.
The most relevant outcome measure to use for relatives’ effects would be their affected utility. However, in practice, the most commonly used outcome measure is the QALY, which combines the value of the health state (QALY weight) with the number of years spent in that health state. It is therefore appropriate to also use QALYs as the outcome measure for relatives’ effects. We use a new term in this article, which we call the R-QALY weight. The R-QALY weight is defined as the effect on relatives’ QALY weight of being a relative of a disabled or sick individual. This measure is intended to capture the effect on relatives’ utility caused by a patient’s disease or disability and is intended to be subtracted from the patient’s QALY. The R-QALY weight is therefore broader than terms such as ‘caregiver burden’.
In order to more precisely define what should be captured in the R-QALY weight, there is a need to examine what is captured in the individual’s QALY weight. If the intention of the analysis is to relate the costs caused by an intervention to the utility generated by it, then it is necessary to define the factors that are assumed to affect the utility, both for patients and for relatives. In general, the utility taken into account in cost-effectiveness analyses is that of the individual who is the target of the medical intervention. Furthermore, only the utility generated by health during a certain time period is generally included; utility that is derived from other aspects will not be captured. If the individual’s own utility is affected by the fact that his or her relatives are influenced by the disease or disability, this indirect effect can be assumed to be incorporated in the individual’s utility. However, any health effects of the disease or disability on the utility of the relatives will not be captured by this utility function. The direct effects on relatives’ utility (the R-QALY weight) must therefore also be included to find the total utility caused by the application of an intervention to an individual. Basu and Meltzer[17] have identified what appears to be the total utility effect of a disease or disability from a societal perspective. They include the direct effect on the individual’s utility, the indirect effect on the individual’s utility through relatives’ utility and the direct effect on relatives’ utility. The latter two effects represent the total spillover effect. We assume that the first two of these effects may be included in the individual’s utility function, and this is what is normally measured as the effects of an intervention. The third, however, is not. When including the direct effect on relatives’ utility, one has to make sure double counting is avoided. If the individual considers relatives’ utility in his or her own QALY weight, an inclusion of the R-QALY weight could lead to double counting. However, as the individual may only include the indirect effect of relatives’ utility on their own utility, we argue that this is not really double counting.
2. Perspective and Theoretical Basis of the Analysis
It is generally recommended that a cost-effectiveness analysis should have a societal perspective,[7,22] indicating that all costs and effects arising from an intervention should be considered, no matter where, when or for whom they appear. One theory that enables the analysis to have this perspective is welfare economics, which assumes that the welfare (or utility) of the society is the sum of all the individuals’ welfare (utilities). By using this theory, it is obvious that relatives’ utilities should also be considered in the analysis if they are affected by the patient’s disease or disability. However, an alternative to welfare economics called extra-welfarism (or the decision-maker’s approach) has often been preferred for use in evaluating medical interventions.[23,24] The extra-welfaristic approach relaxes the assumption that social welfare is a function of all individuals’ utilities and allows factors other than utility to be of importance in finding the social welfare.[25] This approach indicates that an intervention should be evaluated on its capacity to increase the capability of individuals to do certain things. The extra-welfaristic approach, when used within cost-effectiveness analyses, implies that health interventions should be evaluated according to their impact on health. However, using an extra-welfaristic approach does not mean that the analysis cannot have a societal perspective, and it does not mean that relatives’ costs and effects should be omitted. As long as the analysis claims to have a societal perspective, it is thus difficult to find arguments for excluding relatives’ costs and effects. There may nevertheless be theoretical arguments for also incorporating relatives’ costs and effects in other perspectives. The use of a publicly funded healthcare perspective is recommended in, for example, the UK[15] and Canada.[26] Relatives’ effects are considered important within this perspective, as the intention is to maximize the outcome of health from a given budget. However, the cost of informal care may be excluded in this perspective.
Even though an analysis may aim for a societal perspective, based on welfare economics, this aim is often not fulfilled in its empirical application. For example, the use of QALYs as the outcome measure does not fully represent the patient’s utility.[27] Furthermore, none of the accepted methods for eliciting QALY weights explicitly mentions the relatives, and their effects are therefore probably not considered in the patient’s QALY weight. If relatives’ effects can be assumed to be of importance for the treatment being analysed, and the methods used to create the cost-effectiveness analysis do not consider relatives, there are three main alternatives to consider: (i) accept that relatives’ effects are not included, (ii) try to include relatives’ effects or (iii) change to another method for valuing effects (e.g. the contingent valuation method).
The necessity of including relatives’ costs and effects in a cost-effectiveness analysis is illustrated in figure 1. The figure shows a situation where a patient’s disease or disability leads to R-QALY weights. Furthermore, when relatives provide informal care to the patient this leads to increased costs. If relatives are not providing informal care, the values of their negative R-QALY weights are equal to the X on the value axis. If relatives provide informal care, their total costs and effects are illustrated in two steps: the cost of informal care calculated on an hourly basis and their R-QALY weights. If relatives provide 10 hours of informal care per week, the cost of informal care is equal to Y in the figure. The R-QALY weights should be added to this, and the total costs and effects are therefore equal to Z in the figure. If the R-QALY weights are not included, the analysis will be missing a portion of the value (Z — Y). It should be noted that the actual sizes of the costs and effects used in this illustration still need to be tested empirically. Furthermore, the cost of informal care and the value of the R-QALY weight are measured on the same scale in order to graphically present them together, but this is not intended as the recommended approach.
3. Measuring and Valuing Relatives’ Costs and Effects
In order to consider relatives’ costs and effects in the analysis, all costs and effects need to be identified, measured and valued. Methods of valuing the cost of informal care have already been studied (for an overview, see for example van den Berg et al.[28] ) and so are not thoroughly discussed here. However, relatives’ effects have not been widely studied. Most of the calculations of informal care have valued it as the loss of formal production, using the human capital approach. Recently there have been some attempts to calculate the costs of informal care using different methods such as the contingent valuation method,[29–31] the conjoint analysis method[32–35] and the newly developed well-being valuation method.[36,37] These methods of calculating the cost of informal caregiving may also capture (some or all) relatives’ effects. The contingent valuation method aims to find a monetary value for the informal caregiving, often by studying relatives’ willingness to pay (WTP) for a reduction in their own caregiving. The conjoint analysis applied in valuing informal care aims to find the value of informal care by letting individuals choose between situations with different attributes relevant to the caregiving. The well-being valuation method estimates the value of an additional hour of informal care as the compensation the informal caregiver would need in order to maintain the same level of well-being.
Most of the methods used for valuing the cost of informal care do not capture the value of relatives’ effects. How these effects should be measured and valued has not been widely studied, but these effects are sometimes mentioned in studies that examine methods for valuing informal care. Several authors have noticed the importance of relatives’ effects and suggested that relatives’ QOL should be measured,[8,9,38] but not necessarily incorporated into the analysis. It has been suggested that relatives’ effects be measured in terms of well-being, as this measure may include both economic and non-economic factors.[28] However, the use of well-being as the outcome measure may lead to double counting if the cost of informal caregiving is also included. If there is no intention of incorporating the value of relatives’ effects within the analysis, any outcome measure is possible and the research should concentrate on finding the most suitable methods to capture relatives’ effects. However, it is important that relatives’ effects are included within the analysis, as the results of the analysis often guide decision makers.
Earlier in this article, we suggest using R-QALY weights to represent the change in utility for relatives caused by a disabled or sick individual. There are several potential methods to measure and value the R-QALY weights. The methods used to determine the patient’s QALY weights could also be used to determine the R-QALY weights. This could, for example, be studied with direct methods such as the time trade-off (TTO), Standard Gamble (SG) or rating scale (RS). However, the practical use of these methods may be different when determining R-QALY weights, compared with eliciting the patients’ QALY weights. For example, using the TTO and asking the relatives how many life-years they would be willing to trade for the patient’s improved health includes several complicated aspects regarding how the question should be asked and, furthermore, how the answers should be interpreted. Some pioneering work on how the TTO could be used for this purpose has been performed by Mohide et al.[39] and Prosser et al.[40] The RS is probably the easiest direct method to use for estimating the R-QALY weights, as it does not use hypothetical health states or situations with risk. However, this is a theoretical weakness, as the relatives’ preferences will not be revealed when no choice has to be made. If the RS is used for finding the R-QALY weights, the anchoring endpoints cannot be the same as those used when the patient’s QALY weight is measured. The endpoints could, for example, be best imaginable relative-related QOL and worst imaginable relative-related QOL. Transformation of the relative-related QOL to a scale anchored with death at one end and full health at the other is then needed to generate R-QALY weights. All these methods require further research if they are to be used for finding valid R-QALY weights.
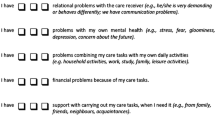
An alternative to the direct methods is to use indirect methods, applying instruments valid for finding R-QALY weights. Several instruments are applicable for measuring relatives’ QOL, but only a few of them are intended to measure relatives’ QALY weights. To our knowledge, there are three such instruments: the Caregiver Quality of Life Instrument,[39] the Caregiver Quality of Life Index[41] and the recently developed CarerQol Instrument.[42] As their titles indicate, they all focus on caregivers rather than relatives. The CarerQol Instrument is probably the most useful. It measures care-related QOL in seven dimensions: fulfilment, relations, mental health, social aspects, financial aspects, support and physical health. It also includes a visual analogue scale with the endpoints ‘completely unhappy’ and ‘completely happy’.
There are also generic instruments that may be suitable for studying R-QALY weights. One example is the EQ-5D, which is one of the most commonly used instruments within cost-effectiveness analyses. This instrument consists of five dimensions, indicating an individual’s health-related QOL, and the utility weights for the health states represent community preferences. Although none of these dimensions include caregiving activities or mention relatives, the instrument has been shown to be able to capture some of the R-QALY weights.[14] However, this may be more of a sign that R-QALY weights are substantial, rather than an indication that the EQ-5D is capable of capturing them. It may also be possible to use other generic indirect methods such as the SF-6D and the Health Utilities Index (HUI).
Other methods of estimating relatives’ effects include the contingent valuation method and the conjoint analysis method. Both of these can be used for valuing both informal care and relatives’ effects, and they are both promising, although they do carry some challenges. It has, for example, been shown that individuals’ WTP estimates often do not reveal their true preferences.[43] The contingent valuation method has not been widely used within health economic analyses, and it is hard to argue that a method that is not accepted (politically) for valuing patients’ effects should be used to value relatives’ effects. Depending on how the question is asked, the WTP value could include both the value of the R-QALY weight and the cost of informal care. One attempt in this direction was made by Mulvaney-Day,[29] who tried to measure relatives’ preferences for a person with mental illness by describing a medication that would significantly improve the person’s situation, and asking how much the relatives were willing to pay for this medication. If relatives’ effects are to be found using the conjoint analysis method, relevant attributes for the relatives’ situation must be chosen. In a study by van den Berg et al.,[34] these attributes were the amount of hours provided for informal care, informal care tasks and monetary compensation.
4. Incorporating Relatives’ Costs and Effects in a Cost-Effectiveness Analysis
In a cost-effectiveness analysis, the costs and effects arising from an intervention can be placed either among the costs in the numerator or among the effects in the denominator. The most obvious solution would be to place relatives’ costs in the numerator and their effects in the denominator. The cost of informal care is also generally placed in the numerator. However, the denominator is generally restricted to the effects of the patient, and it does not clearly enable a combination with relatives’ effects.
Perhaps the least complicated method is to value relatives’ costs and effects in monetary units and then incorporate them in the numerator; this method avoids the need to struggle with the question of how to combine the effects of patients and those of their relatives (QALY weights and R-QALY weights) in the denominator, and it also minimizes the risk of double counting. However, it could be difficult to find a monetary value for all relatives’ effects. Further investigation of this method with the aim of finding the correct value of relatives’ costs and effects would be beneficial.
Some authors have recommended the strategy of presenting relatives’ effects as a separate item in the analysis and excluding them from the cost-effectiveness ratio.[8,9,28,38] The main reason for this is to avoid the risk of double counting, but it also enables comparisons with other analyses. However, this method carries the risk that these effects will lose their impact in the decision-making process; it would be preferable if relatives’ effects could be incorporated within the cost-effectiveness ratio. Furthermore, the common use of a threshold value as an indication of whether a treatment is cost effective or not increases the importance of including relatives’ effects in the cost-effectiveness ratio.
The use of R-QALY weights increases the possibility of combining the patient’s QALY weight with their relatives’ effects. In theory, a QALY is of equal value for everyone, and so the QALYs of individuals can be combined to find the total QALY gain from an intervention; therefore, patients’ QALYs as well as relatives’ R-QALYs can be aggregated to find the total consequences of a medical intervention. However, the situation may not be quite so simple when it comes to empirical application. Several authors[8,9,44] have stressed that the QALY weights of the patients and those of their relatives are not of the same type, and therefore cannot be combined. One is health related and the other is often care related or relative related. When the two kinds of QALY weights are determined using different methods, the direct combination of the weights is problematic, and it is necessary to transform the R-QALY weights before combining them. This transformation could potentially be achieved by asking the relatives to state how much the R-QALY weight (measured in relative-related QOL) affects their general QOL on a cardinal QOL scale (including the health state ‘dead’) and then asking the patients the same question. Studies are needed in order to calibrate these values to permit aggregation, which in practice has been proven to be complicated. Aggregation of utility measures in order to represent societal preferences has been shown to be theoretically troublesome,[45] but is nevertheless commonly used in decision making. Simply focusing on the potential error caused by combining the patient’s and their relatives’ QALY weights is insufficient; it is also necessary to ask what the error would be if these effects were excluded. If the same method is used to elicit QALY weights for both the patient and the relative, then aggregation of these weights is possible. This is mainly the case when indirect methods of valuing the health states are used. If, for example, the EQ-5D instrument is used for both the patient and the relatives, then aggregation of QALY and R-QALY weights is no more complicated than aggregation of QALY weights among patients.
One attempt at considering relatives’ effects was made in NICE’s report for the treatment of Alzheimer’s disease.[19] Since informal caregivers were affected by the patient’s treatment, informal caregivers’ affected QALY weights (utility) were added to the patient’s QALY weight. However, the cost of informal care was not included.
When incorporating relatives’ costs and effects in both the numerator and the denominator of the analysis, one has to be aware of the risk of double counting. In practice, this is not easy. For example, if relatives reduce their hours of paid work to provide informal care, this cost will be captured in the valuation of informal care. If the same income loss furthermore leads to reduced well-being, this may be captured when relatives’ R-QALY weights are measured. The relatives’ income loss will therefore be counted twice if both informal care and R-QALY weights are included in the analysis. One potential solution would be to value lost paid production by the opportunity cost method and to incorporate the value of lost leisure time in the R-QALY weight. Another approach may be to find instruments for valuing R-QALY weights that do not include the effects of lost leisure time or any financial effects; such instruments should rather focus on anxiety, worry and altruistic preferences. Another kind of double counting occurs if the patient has incorporated their relatives’ effects in the valuation of their own health state.
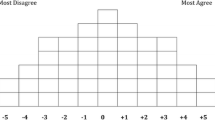
If relatives’ effects are to be incorporated in the analysis, this must be done in a feasible way. It would be rather resource consuming to study relatives’ effects every time a medical technology is being assessed, and it may also be difficult to identify all the relatives. Following the idea of using R-QALYs, one solution may be to use predefined templates in the form of R-QALY weights that can be used in different situations. This could also be used by decision makers when relatives’ effects are of importance but not incorporated in the analysis. An example of how these templates could look is given in figure 2. Depending on the severity of the patient’s disease or disability, and the number of relatives, R-QALY weights will differ. In this example, we suppose that the R-QALY weights are exponentially affected by the severity of the disease or disability. In addition, we assume that the higher the number of relatives, the stronger the R-QALY weight. The true values of these effects are nevertheless not known, and the values in the figure are only meant as examples.
5. Discussion
The relatives of a disabled or sick individual are often affected by the individual’s disease or disability. However, the costs and effects for the relatives are generally omitted from cost-effectiveness analyses. Although there is a consensus that the cost of informal care should be included in order to satisfy a societal perspective, there is still debate over how to measure and value this cost. Furthermore, very few cost-effectiveness analyses performed to date have discussed or included relatives’ effects. In this article, we argue that all the costs and effects of being a relative of a sick or disabled individual should be included in the analysis in order to fulfil a societal perspective. By arguing this, we imply that relatives’ costs can be measured and valued according to earlier recommendations.[28,46] Furthermore, we state that relatives’ effects should be included in the analysis. One possible way of incorporating them in the denominator is to measure the effects for the disabled or sick individual and their relatives on the same scale. As QALYs are currently the most common outcome measure in health economic analyses, we suggest that this measure could also include the relatives’ effects. Therefore, we created the R-QALY weight, defined as the effect on the QALY weight of being a relative of a disabled or sick individual. Another possible method discussed in this article is to use the contingent valuation method to find a monetary value for relatives’ costs and effects. This method has been tested in only a few studies[29,31,40] and there is a need for further research. A short summary of the costs and effects for the disabled or sick individuals and their relatives is given in table I, together with some areas where further research is needed.
The US panel on Cost-Effectiveness in Health and Medicine[7] mentioned in 1996 that the analysis should include effects of ‘significant others’ in order to fulfil a societal approach. The importance of this has also been stressed by, for example, Brouwer.[47] Some studies[8,9,38] have discussed the possibility of including informal caregivers’ health effects in the analysis and recommended presenting them as a separate item rather than including them in the cost-effectiveness ratio. A study of QALY weights measured using the EQ-5D among caregivers of patients with rheumatoid arthritis and a matched reference group did not report any difference in QALY weights.[48] Davidson et al.[14] used a similar approach, based on a sample of relatives giving care or support to an older person. They found small reductions in relatives’ QALY weights (R-QALY weights) due to being a relative of an older person in need of care or support. This reduction was strongest among those whose caregiving situation was described as burdensome.
One difficulty with measuring R-QALY weights using existing instruments is that these instruments are rarely focused on relative-related aspects. Even if generic QOL instruments do cover some aspects relevant for relatives and caregivers, they may miss important aspects and potential altruistic preferences. A further development and validation of the existing caregiving instruments used for eliciting utility weights (especially the CarerQol Instrument[42] ) would therefore be beneficial for this area, as would further studies on the use of TTO, SG or RS for finding R-QALY weights.
If valid methods for estimating relatives’ costs and effects are lacking, it is difficult to study the correct cost effectiveness of both treatments for the patient and treatment or support for the caregiver. It is known that support for the patient often affects the informal caregiver positively.[3] Dixon et al.[49] have shown that improvement of the cared-for individual’s QOL may reduce the need for informal caregiving time and may improve the caregivers’ QOL. There is still uncertainty regarding the types of support for the caregiver that are effective and cost effective. These questions are difficult to study without dealing with the issues of how the cared-for person and caregiver are linked to each other.
The inclusion of relatives’ costs and effects in the cost-effectiveness analysis can cause problems. Some of these problems are methodological or practical, and are covered by the discussion in this article, but others may constitute ethical dilemmas. People with many relatives may receive greater benefit from a medical intervention than people who are alone, all else being equal, and this may affect the priority setting. It would therefore be beneficial if the results of the analysis were presented both with and without relatives’ costs and effects; this would also increase the comparability with results from other cost-effectiveness analyses. On the other hand, health economic analyses do not compare treatments for specific individuals; the comparisons are always between healthcare programmes for patient groups.
6. Conclusions
Because cost-effectiveness analyses are used for decision making, and this is often achieved by comparing different cost-effectiveness ratios, we argue that it is important to find ways of incorporating all relatives’ costs and effects within the analysis. This may not be necessary for every analysis of every intervention, but for treatments where relatives’ costs and effects are substantial they may influence the cost-effectiveness ratio.
References
Donaldson C, Tarrier N, Burns A. Determinants of carer stress in Alzheimer’s disease. Int J Geriatric Psychiatry 1998; 13: 248–56
Han B, Haley WE. Family caregiving for patients with stroke: review and analysis. Stroke 1999; 30: 1478–85
Whitlatch CJ. Distress and burden for family caregivers. In: Wimo A, Jönsson B, Karlsson G, et al., editors. Health economics of dementia. Chichester: John Wiley & Sons, 1998: 123–38
Murphy N, Christian B, Caplin D, et al. The health of caregivers for children with disabilities: caregiver perspectives. Child Care Health Dev 2007; 33(2): 180–7
Stolz P, Udén G, Willman A. Support for family carers who care for an elderly person at home: systematic review. Scand J Caring Sci 2004; 18: 111–9
Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. 3rd ed. Oxford: Oxford University Press, 2005
Gold MR, Siegel JE, Russel LB, et al. Cost-effectiveness in health and medicine. New York: Oxford University Press, 1996
Brouwer WB, van Exel NJA, Koopmanschap MA, et al. The valuation of informal care in economic appraisal: a consideration of individual choice and societal costs of time. Int J Technol Assess Health Care 1999; 15(1): 147–60
Koopmanschap MA, Brouwer WB. Indirect costs and costing informal care. In: Wimo A, Jönsson B, Karlsson G, et al., editors. Health economics of dementia. Chichester: John Wiley & Sons, 1998: 245–56
Aneshensel CS, Pearlin LI, Schuler RH. Stress, role captivity, and the cessation of caregiving. J Health Soc Behav 1993; 34(1): 54–70
Brouwer WB, van Exel NJA, van den Berg B, et al. Process utility from providing informal care: the benefit of caring. Health Pol 2005; 74: 85–99
Nolan MR, Grant G, Keady J. Understanding family care: a multidimensional model of caring and coping. Buckingham: Open University Press, 1996
White CL, Lauzon S, Yaffe MJ, et al. Toward a model of quality of life for family caregivers of stroke survivors. Qual Life Res 2004; 13: 625–38
Davidson T, Krevers B, Levin L-Å. In pursuit of QALY weights for relatives: empirical estimates in relatives caring for older people. Eur J Health Econ 2008; 9: 285–92
National Institute for Health and Clinical Excellence. Updated guide to the methods of technology appraisal. London: NICE, 2008 [online]. Available from URL: http://www.nice.org.uk/media/B52/A7/TAMethodsGuideUpdated June2008.pdf [Accessed 2009 Nov 30]
Läkemedelsförmånsnämnden. General guidelines for economic evaluations from the Pharmaceutical Benefits Board. Stockholm: Pharmaceutical Benefits Board (Läkemedelsförmånsnämnden), 2003 [online]. Available from URL: http://www.tlv.se/Upload/English/ENG-lfnar-2003-2.pdf [Accessed 2009 Nov 30]
Basu A, Meltzer D. Implications of spillover effects within the family for medical cost-effectiveness analysis. J Health Econ 2005; 24: 751–73
Prosser L, Hammitt J, Keren R. Measuring health preferences for use in cost-utility and cost-benefit analyses of interventions in children: theoretical and methodological considerations. Pharmacoeconomics 2007; 25(9): 713–26
National Institute for Health and Clinical Excellence. Donepezil, galantamine, rivastigmine (review) and memantine for the treatment of Alzheimer’s disease (amended). London: NICE, 2007
Bolin K, Lindgren B, Lundborg P. Your next of kin or your own career? Caring and working among the 50+ of Europe. J Health Econ 2008; 27(3): 718–38
Andrén S, Elmståhl S. Family caregivers’ subjective experiences of satisfaction in dementia care: aspects of burden, subjective health and sense of coherence. Scand J Caring Sci 2005; 19: 157–68
Johannesson M. Theory and methods of economic evaluation of health care. Stockholm: Kluwer Academic Publishers, 1996
Culyer AJ. The normative economics of health care finance and provision. In: McGuire A, Fenn P, Mayhew K, editors. Providing health care: the economics of alternative systems of finance and provision. Oxford: Oxford University Press, 1991:65–98
Williams A. Cost-benefit analysis: applied welfare economics or general decision aid. In: Williams A, Giardina E, editors. Efficiency in the public sector. London: Edward Elgar, 1993: 65–79
Birch S, Donaldson C. Valuing the benefits and costs of health care programmes: where’s the ‘extra’ in extra-welfarism? Soc Sci Med 2003; 56: 1121–33
Canadian agency for drugs and technologies in health. Guidelines for the economic evaluation of health technologies. 3rd ed. Ottawa: CADTH, 2006 [online]. Available from URL: http://www.cadth.ca/media/pdf/1 86_EconomicGuidelines_e.pdf [Accessed 2009 Nov 30]
Torrance GW, Feeny DH. Utilities and quality adjusted life years. Int J Technol Assess Health Care 1989; 5: 559–75
van den Berg B, Brouwer WB, Koopmanschap MA. Economic valuation of informal care; an overview of methods and applications. Eur J Health Econ 2004; 5: 36–45
Mulvaney-Day NE. Using willingness to pay to measure family members’ preferences in mental health. J Ment Health Pol Econ 2005; 8: 71–81
van den Berg B, Bleichrodt H, Eeckhoudt L. The economic value of informal care: a study of informal caregivers’ and patients’ willingness to pay and willingness to accept for informal care. Health Econ 2005; 14: 363–76
van den Berg B, Brouwer WB, van Exel NJA, et al. Economic valuation of informal care: the contingent valuation method applied to informal caregiving. Health Econ 2005; 14(2): 169–83
Ryan M. Using conjoint analysis to take account of patient preferences and go beyond health outcomes: an application to in vitro fertilisation. Soc Sci Med 1999; 48: 535–46
Ryan M, Hughes J. Using conjoint analysis to assess women’s preferences for miscarriage management. Health Econ 1997; 6: 261–73
van den Berg B, Al M, van Exel NJA, et al. Economic valuation of informal care: conjoint analysis applied in a heterogeneous population of informal caregivers. Value Health 2008; 11(7): 1041–50
van den Berg B, Maiwenn A, Brouwer W, et al. Economic valuation of informal care: the conjoint measurement method applied to informal caregiving. Soc Sci Med 2005; 61: 1342–55
Ferrer-i-Carbonell A, van Praag BMS. The subjective costs of health losses due to chronic diseases: an alternative model for monetary appraisal. Health Econ 2002; 11: 709–22
van den Berg B, Ferrer-i-Carbonell A. Monetary valuation of informal care: the well-being valuation method. Health Econ 2007; 16(11): 1227–44
Busschbach JJV, Brouwer WB, van der Donk A, et al. An outline for a cost-effectiveness analysis of a drug for patients with Alzheimer’s disease. Pharmacoeconomics 1998; 13(1): 21–34
Mohide EA, Torrance GW, Streiner DL, et al. Measuring the wellbeing of family caregivers using the time trade-off technique. J Clin Epidemiol 1988; 41(5): 475–82
Prosser LA, Bridges CB, Uyeki TM, et al. Values for preventing influenza-related morbidity and vaccine adverse events in children. Health Qual Life Outcomes 2005; 3: 18
McMillan SC, Mahon MM. The impact of hospice services on the quality of life of primary caregivers. Oncol Nurs Forum 1994 Aug; 21(7): 1189–95
Brouwer W, van Exel N, van Gorp B, et al. The CarerQol instrument: a new instrument to measure care-related quality of life of informal caregivers for use in economic evaluations. Qual Life Res 2006; 15: 1005–21
Johannesson M, Liljas B, O’Connor RM. Hypothetical versus real willingness to pay: some experimental results. Appl Econ Lett 1997; 4: 149–51
Karlsson G, Jönsson B, Wimo A, et al. Methodological issues in health economic studies of dementia. In: Wimo A, Jönsson B, Karlsson G, et al., editors. Health economics of dementia. Chichester: John Wiley & Sons, 1998: 161–70
Arrow K. A difficulty in the concept of social welfare. J Pol Econ 1950; 58(4): 328–46
Koopmanschap MA, van Exel NJA, van den Berg B, et al. An overview of methods and applications to value informal care in economic evaluations of healthcare. Pharmacoeconomics 2008; 26(4): 269–80
Brouwer WB. Too important to ignore: informal caregivers and other significant others. Pharmacoeconomics 2006; 24(1): 39–41
Brouwer WB, van Exel NJA, van den Berg B, et al. Burden of caregiving: evidence of objective burden, subjective burden, and quality of life impacts on informal caregivers of patients with rheumatoid arthritis. Arthritis Rheum 2004; 51(4): 570–7
Dixon S, Walker M, Salek S. Incorporating carer effects into economic evaluation. Pharmacoeconomics 2006; 24(1): 43–53
Acknowledgements
Financial support for this study was provided by grants from Apoteket AB’s research fund and from the county council of Östergötland, Sweden. The funding agreement ensured the authors’ independence in writing and publishing this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Davidson, T., Levin, LÅ. Is the societal approach wide enough to include relatives?. Appl Health Econ Health Policy 8, 25–35 (2010). https://doi.org/10.1007/BF03256163
Published:
Issue Date:
DOI: https://doi.org/10.1007/BF03256163