Abstract
Melioidosis is a serious infectious tropical disease caused by a soil-dwelling bacterium, Burkholderia pseudomallei, transmitted from contaminated soil or surface water. Although endemic in Southeast Asia, it is considered an emerging disease in Lao PDR where it has only been recognised for 15 years, becoming one of the leading causes of community-acquired septicaemia. A research programme has been developed by the Lao-Oxford-Mahosot Hospital-Wellcome Trust Research Unit in collaboration with the Institut de la Francophonie pour la Médecine Tropicale (IFMT) and the Institut de Recherche pour le Développement (IRD) to investigate the environmental reservoir of B. pseudomallei in Lao PDR. The first study, conducted in 2009, showed that the geographical distribution of B. pseudomallei was very heterogeneous and not limited to the floodplains of the Mekong River. The soil samples collected in the province of Saravane (southern Laos) was proved the most heavily contaminated. The second study, conducted in 2010, aimed to detect B. pseudomallei in surface water using Moore’s swabs. A high proportion of water samples taken from the Sedone River were positive downstream of a heavily contaminated terrestrial site, suggesting contamination by runoff from land reservoirs. Both environmental reservoir studies of B. pseudomallei pave the way for future research in order to clarify the areas at risk of melioidosis to facilitate preventive measures amongst populations at risk and better care for those infected.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Melioidosis
- Burkholderia pseudomallei
- Environmental microbiology
- Soil sampling
- Surface water
- Moore’s swabs
1 Introduction
Melioidosis is a severe tropical bacterial infection that affects man and a range of other animals. It is caused by a Gram-negative bacillus, Burkholderia pseudomallei, an environmental saprophyte that is widespread in Southeast Asia and northern Australia. This facultative intracellular bacterium is infectious to man by inoculation or inhalation. The main modes of exposure are occupational (e.g. agricultural work, especially rice farming) or accidental (e.g. near drowning, typhoons, tsunamis). The disease occurs mostly as an opportunistic infection in individuals with underlying predisposition, particularly diabetes mellitus. The infection can be invasive and rapidly fatal, run a subacute or chronic course or even remain latent for long periods. Even with early and appropriate treatment, the mortality rate remains high at 20–50 %.
Melioidosis is a disease that presents a disconcerting number of paradoxes:
-
It is considered an ‘emerging disease’ even though it was actually first described more than a century ago in Myanmar (Burma). It is actually unclear whether this reflects true emergence of the disease or increasing recognition, thanks to improvements in diagnostic capacity.
-
It is a tropical disease that is usually considered as endemic to Southeast Asia and northern Australia but which is increasingly being identified in other parts of the world.
-
It is a very serious and often fatal infection in its acute form, highly pleomorphic in its subacute form, which can affect any tissue or organ and escape diagnosis, but it can also remain latent and asymptomatic for many years.
-
It is a challenge for researchers to understand how and why this saprophytic environmental bacterium, which is not specifically adapted as a human pathogen, is able to evade the immune defence mechanisms of the host.
In the Lao PDR (Laos), melioidosis was unknown before 1999 even though it had been recognised for several decades in neighbouring countries, most notably Thailand (Leelarasamee 2000). More than 500 cases have been diagnosed in the country over the past 10 years, the majority in Mahosot Hospital in Vientiane (Phetsouvanh et al. 2001), but this apparent emergence really reflects the development of the hospital laboratory to a level that enabled it to grow and identify B. pseudomallei (Phetsouvanh et al. 2006). In addition, the rapid advance of diabetes in Laos, as in all the countries of Southeast Asia (Wild et al. 2004), has probably also contributed to the increase in the incidence of melioidosis, which has now become one of the main causes of community-acquired septicaemia.
This situation justified the establishment of a programme of research initiated by the Lao-Oxford-Mahosot Hospital-Wellcome Trust Research Unit, in collaboration with the Institut de la Francophonie pour la Médecine Tropicale (IFMT) and the Institut de Recherche pour le Développement (IRD).
2 Microbiological and Epidemiological Data
2.1 Burkholderia pseudomallei, a Bacteriological Curiosity
The causative agent of melioidosis is a remarkable pathogen in its capacity for virulence, survival and resistance, at the same time being both an environmental saprophyte and a facultative intracellular parasite. It is experiencing a resurgence of interest since it was classified by the Centers for Disease Control and Prevention as a ‘Category B’ agent of bioterrorism potential (Gilad et al. 2007).
The bacterium was first identified in Rangoon (Burma) in 1912 by Whitmore and Krishnaswami in pus taken from abscesses found at autopsy in morphine addicts. Whitmore’s bacillus was initially named ‘Bacillus pseudomallei’ because of its similarity with the glanders bacillus and has subsequently been known as ‘Pfeifferella whitmori’, ‘Malleomyces pseudomallei’ and ‘Pseudomonas pseudomallei’ until it was finally designated as Burkholderia pseudomallei by Yabuuchi in 1992.
It is a non-sporing Gram-negative bacillus which often exhibits uneven staining, sometimes staining more intensely at the extremities (likened to a shuttle or safety pin), motile via polar flagella. The latter characteristic distinguishes it from the glanders bacillus, Burkholderia mallei, which is nonmotile (Holden et al. 2004). It grows rapidly on most culture media aerobically at 37 °C. After 18 h of incubation, it forms colonies from 1 to 2 mm in diameter, which are usually circular, domed, smooth and grey or whitish in colour. After 48 h, the colonies increase up to 5 mm, become creamy and give off a characteristic smell which has been likened to truffles or wet soil (although since this is a hazard group 3 pathogen, smelling plates should be avoided!). Several different colonial morphotypes have been described and cultures may appear mixed, the commonest forms being smooth and rugose, the latter having a characteristic wrinkled or umbilicated appearance. Some strains are even frankly mucoid. B. pseudomallei is an aerobic organism; it is catalase and oxidase positive and able to use glucose and numerous other sugars oxidatively, but it does not assimilate arabinose. Similar avirulent bacteria isolated from the soil in Southeast Asia, which are able to assimilate arabinose, have been assigned to a separate species Burkholderia thailandensis (Cheng and Currie 2005).
Burkholderia pseudomallei is intrinsically resistant to several different groups of antibiotics: penicillins G and A, first and second generation cephalosporins, aminoglycosides, macrolides, rifampicin and polymyxins. It is usually susceptible to co-trimoxazole, chloramphenicol, tetracyclines, the combination of amoxicillin and clavulanic acid, ureidopenicillins, third-generation cephalosporins and carbapenems. Fluoroquinolones are relatively inactive, reported susceptibility to ciprofloxacin varying between 8.5 and 50 % (Thibault et al. 2004).
The genome of B. pseudomallei has been fully sequenced (Holden et al. 2004). It is large, 7.25 megabase pairs (Mb), and comprises two chromosomes of 4.07 Mb and 3.17 Mb, respectively. The larger chromosome codes for proteins that are essential for growth and survival (e.g. biosynthesis, metabolism, chemotaxis, motility) as well as several virulence determinants. The smaller chromosome codes for accessory functions involved in adaptation to different environmental niches. Phylogenetic analysis shows that B. mallei is really a host-adapted clone of B. pseudomallei (Inglis and Sagripanti 2006).
2.2 Bioecology of Burkholderia pseudomallei
Burkholderia pseudomallei and B. mallei form a unique species on the basis of their genetic homology; the distinction into two species is based on epidemiological and pathogenic differences. While B. mallei is incapable of surviving for long periods outside its mammalian host, B. pseudomallei is a saprophytic bacterium adapted to life in soil and surface water. Its remarkable ability to survive has been well studied in vitro: it can accumulate significant energy reserves in the form of poly-hydroxybutyrate granules, can persist for several years without nutrients in distilled water and can multiply in soil between 4 and 42 °C, with a pH between 5 and 8 and water content from 10 % to 15 %. These types of conditions are found in rice paddy as well as oil palm and rubber tree plantation soil (Inglis and Sagripanti 2006). Organic matter (e.g. manure) found in cultivated land favours its proliferation (Kaestli et al. 2009). Soil contaminated for 3 years still harbours dormant bacilli that maintain their virulence. The survival of these non-sporing bacteria in the environment can be explained by it entering a ‘viable but non cultivable’ state when it encounters hostile environmental conditions. Its genome can be detected in soil samples that are culture negative (Kaestli et al. 2007). When the pH falls below 5, the concentration of sodium chloride goes above 2.5 %, or after desiccation, it is not cultivable by conventional means but it preserves its pathogenic potential (Inglis and Sagripanti 2006; Shams et al. 2007). It can also tolerate the effect of disinfectants and may not always be inactivated by the concentrations of chlorine used to treat drinking water.
The persistence of B. pseudomallei in its natural ecological niches is thought to be related to two properties: (i) the capacity to form biofilms made from capsular polysaccharide in which the bacteria form slowly growing micro-colonies that are protected from disinfectants and antibiotics and (ii) the ability to penetrate into the cytoplasm of free-living amoebae of the genera Acanthamoeba and Hartmannella by a mechanism of ‘coiling phagocytosis’ similar to that previously described in Legionella and Listeria and then to multiply within vacuoles and survive in amoebic cysts (Inglis et al. 2000).
2.3 Epidemiology of Melioidosis
The main endemic areas for melioidosis are Southeast Asia (Cambodia, Indonesia, Laos, Malaysia, Myanmar, the Philippines, Singapore, Thailand, Vietnam) and tropical northern Australia. In the rest of the world, the disease is little known (Aldhous 2005). According to phylogenetic studies of isolates of B. pseudomallei from Australia, Papua New Guinea and Thailand, the common ancestor of these different strains would have arisen in Australia (Currie 2008). Outside the main endemic areas, animal and human cases have been reported in North America (the USA, Mexico), South America (northeast Brazil, Ecuador) and the Caribbean (Puerto Rico, Aruba, Guadeloupe, Martinique). On the other hand, melioidosis has rarely been documented in Africa, more often from environmental or animal sources (Burkina Faso, Niger, Chad, Côte d’Ivoire) than in man (Madagascar, the Gambia) (Currie 2008; Currie et al. 2008).
The endemic areas are hot and humid regions with a minimum temperature of 11 °C. B. pseudomallei is present in various soil types, sediments, stagnant water in ponds and rice fields, but not in estuarine or sea water. Its distribution in the soil is heterogeneous and discontinuous. It can be isolated from 10 % to 50 % of soil samples in northeast Thailand (Vuddhakul et al. 1999). There is a correlation between local rainfall and the incidence of the disease, 50–75 % of cases presenting during the rainy season (Kaestli et al. 2009). Cases are usually sporadic but are sometimes grouped into small outbreaks (Shih et al. 2009), especially during natural disasters such as floods or typhoons (Su et al. 2011), or linked to common sources such as a contaminated water supply.
Human infection can occur by two main routes: cutaneous through contact with soil or water, which is probably the most common and is favoured by walking barefoot or the presence of wounds or superficial abrasions, and inhalation, which was suspected to account for the occurrence of a surplus of cases amongst helicopter crews during the Vietnam War (Aldhous 2005), and also after near drowning in fresh water such as occurred amongst victims of the tsunami of 2004 (Athan et al. 2005). Other routes of infection have been reported less frequently: drinking contaminated water, direct human-human transmission (e.g. mother-infant or sexual transmission), nosocomial infection via inadequately disinfected equipment (e.g. bronchoscopes) and laboratory-acquired infection (Peacock et al. 2008). These remain anecdotal and are not epidemiologically significant. As a general rule, melioidosis is not a contagious disease.
Melioidosis can present at any age, in either sex and in all socio-economic classes. The relative risk is higher in certain subgroups (age >45 years, males, and in Australia, aboriginal ethnicity) which probably partly reflects differences in exposure as opposed to greater susceptibility. Certain occupations involving exposure to soil or surface water also increase the risk of infection: rice farmers, labourers, farmers, potters and other rural activities. Wounds contaminated with soil or water and drowning accidents with aspiration of fresh water are high-risk events. Military activities in natural environments favour different modes of infection (Kronmann et al. 2009). Travellers are less at risk, most cases occurring in people with pre-existing conditions that make them more susceptible to infection. These intrinsic risk factors are underlying conditions that increase both the susceptibility to infection and the severity of the disease. Diabetes is the most significant and increases the risk of infection 5–13-fold: at least half of all patients contracting melioidosis have diabetes. Other predisposing factors include alcoholism; chronic renal disease; chronic lung disease including cystic fibrosis, thalassaemia, malignancy and chronic steroid use. In contrast, HIV infection does not appear to increase susceptibility. In summary, a number of factors appear necessary for the disease to develop: exposure to a sufficient bacterial inoculum, a route of entry and a susceptible host.
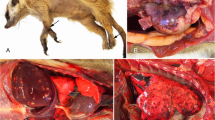
Like glanders, melioidosis can cause epizootics in several animal species. The animals most affected are pigs, sheep, goats and horses, but zoonotic infection can also be seen in camelids, kangaroos, large primates, rodents, birds, captive dolphins and killer whales. Strangely, cattle and animals that live in mud, such as water buffaloes and crocodiles, seem to be relatively resistant to infection (Sprague and Neubauer 2004).
In man, the global incidence of melioidosis is low overall, but it is probably under-diagnosed, both in non-endemic countries where it is frequently overlooked and in endemic countries where diagnostic capabilities are often lacking. The reported incidence rates are 12.7/100,000 in northeast Thailand (Limmathurotsakul et al. 2010) and 19.6/100,000 in northern Australia (Currie et al. 2004). In practice, it is difficult to estimate the true incidence of melioidosis in the absence of reliable diagnostic laboratories accessible to rural communities. This explains the delayed rediscovery of the disease in Cambodia (Wuthiekanun et al. 2008) and its oversight for more than 60 years in Burma where it was first described (Wuthiekanun et al. 2006). In the same way, the emergence of the disease in Brazil (Rolim et al. 2009) and in New Caledonia (Le Hello et al. 2005) can be explained by improved microbiological surveillance.
3 Melioidosis in Laos
In Laos, the first two patients with melioidosis were confirmed in 1999 (Phetsouvanh et al. 2001). Since then the number of patients reported has continued to increase, mainly affecting the rice farming community in the Mekong flood plain. A preliminary study undertaken in 1998 in rice paddies within a radius of 150 km around Vientiane detected B. pseudomallei in 36 % of 110 samples of soil (Wuthiekanun et al. 2005) (Table 7.1). These first data corroborated the conclusions of Thai researchers according to whom there is a correlation between the degree of soil contamination and the incidence of melioidosis in the human population (Vuddhakul et al. 1999). It was decided to try to confirm this through further environmental studies in Laos. The first was undertaken in 2009 to determine the geographic distribution of B. pseudomallei in soil, the second in 2010 to detect the bacterium in surface waters (Rattanavong et al. 2011; Vongphayloth et al. 2012). We summarise these findings.
3.1 Research on B. pseudomallei in Soil in Laos
This work, described in Rattanavong et al. (2011), had the objective of answering a double question: is the area of distribution of melioidosis restricted (i) to the province of Vientiane and (ii) to the Mekong valley?
The sampling plan followed two stages: the first geographic, the second probabilistic. In the first stage, six provinces were selected deliberately following three transects: northwest (Vientiane West, Oudomxay and Luangnamtha), northeast (Vientiane East, Xieng Khouang and Huaphanh) and south (Saravane). Vientiane and Saravane Provinces were divided into two (western and eastern) and three (western, central and eastern) areas of equal width, respectively. In the second stage, three sites were selected randomly on each transect, giving a total of nine sampling areas, using the following criteria: rice fields with an area greater than or equal to 1 ha, ≤100 m from the nearest perennial river, and at least 50 m from a known area of unexploded ordnance and from houses.
The necessary data were obtained from different organisations: Forest Inventory and Planning Division (FIPD) to localise the rice growing areas from 2008 to 2009, National Geographic Department (NGD) to clarify their position in relation to the secondary water courses, Ministry of Communication, Transport and Post to confirm the absence of buildings near the chosen sites and Lao National Unexploded Ordnance Programme (UXO Lao) to be certain of the absence of unexploded ordnance within a radius of 50 m. The coordinates of the sampling sites corresponding to these criteria were determined randomly by computer and identified using a Global Positioning System (GPS). At each site, a grid of 45 × 45 m was defined to dig ten rows of ten holes separated from each other by 5 m.
Samples of soil were collected following a standard methodology adapted from that used previously in Thailand and Laos (Wuthiekanun et al. 2005, 2006). The soil was taken from a depth of 30 cm with a clean shovel which had been washed in fresh water, disinfected with 70 % alcohol and dried between each collection. A sample of 100 g of soil was collected from the bottom of each hole and placed in a numbered plastic bag. Each bag was sealed and placed in a container protected from light at room temperature until its delivery to the laboratory within 48 h. In the laboratory, samples were rehydrated by the addition of 100 ml of sterile distilled water, mixed by agitation and incubated overnight at room temperature. The following day, the supernatant was subcultured onto five plates of Ashdown’s agar: two plates with 10 μl, two plates with 100 μl and one plate with 500 μl. A selective enrichment broth containing colistin (SBCT) was also inoculated with 1 ml of supernatant. The cultures were incubated aerobically at 40 °C for 4 days and inspected daily from the second day. The SBCT broth cultures were subcultured after 48 h incubation onto Ashdown’s agar. Suspect colonies were preliminarily identified by their cultural characteristics on Ashdown’s medium, appearance on Gram stain and oxidase reaction and were counted at the dilution giving the highest countable number of colony-forming units (cfu). The identification was confirmed by a highly specific latex agglutination test which allowed exclusion of B. thailandensis (Wuthiekanun et al. 2002) and by confirming susceptibility to amoxicillin-clavulanic acid and resistance to colistin. API 20 NE tests done subsequently on a subset of isolates identified as B. pseudomallei by these methods confirmed their identity.
Cultures of B. pseudomallei were obtained in four of the nine sites studied (Fig. 7.1): the site in Luangnamtha in the northwest of the country (1 % of samples positive) and the three sites in Saravane in the south (42–94 % of samples positive). The highest geometric mean bacterial concentrations were found in the site in Saravane East (Fig. 7.1). These were the highest concentrations of environmental B. pseudomallei published to date (Rattanavong et al. 2011). The comparison of these results showed that the presence of B. pseudomallei did not correlate with the elevation of the site nor the distance from the Mekong (Fig. 7.2).
Distribution of Burkholderia pseudomallei at nine sampling sites in Laos in 2009 (Data taken from Wuthiekanun et al. 2005)
Presence of B. pseudomallei in relation to elevation and distance from the Mekong River: (a) northeast, (b) northwest and (c) south. (●) positive for B. pseudomallei; (○) negative for B. pseudomallei (Data taken from Rattanavong et al. 2011)
The two sites in Saravane East and West were resampled in 2010 according to the same protocol, at the end of the dry season, whereas they had been sampled at the start of the rainy season in 2009. The rates of contamination with B. pseudomallei were significantly lower with 76 % and 25 % of samples positive, respectively. Similarly, bacterial concentrations were lower with geometric means of 501 cfu/g [95 % CI: 314–797] in Saravane East and 147 cfu/g [95 % CI: 48–452] in Saravane West.
This first study (Rattanavong et al. 2011) suggested three conclusions: (i) the reservoir of melioidosis in Laos has a highly heterogeneous geographical distribution; (ii) it is not restricted to the Mekong basin and to low-lying regions; (iii) there are areas of high-level contamination with B pseudomallei in the province of Saravane.
3.2 Research into B. pseudomallei in Surface Waters
The second study [described in Vongphayloth et al. 2012) aimed to investigate the presence of B. pseudomallei in surface waters in the vicinity of contaminated sites and the use of Moore’s swabs for the detection of the organism in water. The latter is a concentration technique using an immersed gauze swab that acts as a filter to capture and concentrate microorganisms in running or stagnant water. Developed by Moore (1948) more than 60 years ago to detect salmonellas in wastewater in urban settings, this method has proved an effective tool for isolation of enterobacteria, vibrios, mycobacteria and viruses from sewers and provides useful information for epidemiological investigations. It had been used once for the detection of B. pseudomallei in environmental waters, without success (Ketterer et al. 1986).
Based on the results of the study conducted in 2009 (Rattanavong et al. 2011), the sampling was undertaken close to the sites previously sampled in Saravane East and West. Water samples were collected within a radius of 2 km around each reference site. Four types of surface water were collected: (i) water from lakes or ponds, (ii) rice paddy water, (iii) river water and (iv) water from boreholes or domestic water tanks (Table 7.2). Water from the Sedone River, a tributary of the Mekong running within 100 m and 600 m of the sites at Saravane East and Saravane West, respectively, was also collected: 100 Moore’s swabs were immersed every kilometre from 15 km upstream to 33 km downstream of the site at Saravane East and from 38 km upstream to 14 km downstream of the site at Saravane West. The two sites were about 140 km apart following the course of the Sedone River (Vongphayloth et al. 2012).
At each sampling point, Moore’s swab was placed midway between the surface and bottom of the water source. Each swab was attached by two nylon strings, one fixed to a bamboo pole to ensure it was immersed at some distance from the bank and the other attached to a weight to ensure that the device sank. The pH, turbidity and temperature of the water were recorded: the pH and temperature were measured using a combined pH meter and thermometer (pHep-4, Hanna Instruments, Ann Arbor, MI, USA) and turbidity with a pocket turbidimeter (Hach, Loveland, CO, USA) and expressed in Nephelometric Turbidity Units (NTU). Once in place, the swab was left for 24–48 h before being recovered. After cutting the nylon strings aseptically, the swab was placed in 500 ml SBCT broth in a sterile container that was transported to the laboratory within 24 h. After aerobic incubation for 48 h at 40 °C, the broths were subcultured on Ashdown’s agar. The identification of B. pseudomallei was carried out as described above. Note that this method is qualitative and does not permit enumeration of cfu.
Of the 98 samples of water collected around the site in Saravane East, 35 (36 %) were positive for B. pseudomallei. Of the 102 collected around the site in Saravane West, 6 (6 %) were positive (Table 7.2). The samples of water from ponds, lakes and domestic reservoirs were all found to be negative. Only one of the three samples of borehole water collected near Saravane East was positive. At both sites, water samples from the Sedone River were more frequently contaminated (39 % and 11 %, respectively) than rice paddy water (38 % at Saravane East). All the river water samples that were positive for B. pseudomallei were collected between the two reference sites (Figs. 7.3 and 7.4). The 15 swabs placed upstream of Saravane East and the 14 swabs downstream of Saravane West were all negative. The majority of the positive swabs were collected within 33 km downstream of the site in Saravane East (Fig. 7.3).
Sampling points on the Sedone River upstream and downstream from the Saravane East reference site (black square). White circles represent points that were negative for Burkholderia pseudomallei and black circles represent points that were positive for B. pseudomallei. Water flows to the northwest (Data taken from Vongphayloth et al. 2012)
Sampling points on the Sedone River upstream and downstream from the Saravane West reference site (black square). White circles represent points that were negative for Burkholderia pseudomallei and black circles represent points that were positive for B. pseudomallei. Water flows to the south (Data taken from Vongphayloth et al. 2012)
B. pseudomallei was more frequently isolated from water that was more acidic (pH median: 7.62 versus 8.16; p < 0.001) and more turbid (median: 324 NTU versus 236 NTU; p < 0.001), but there was no significant difference in temperature between positive and negative samples. In multivariate analysis, two parameters were independently associated with the presence of B. pseudomallei, a low pH (OR: 0.5 [95 % CI: 0.3–0.8]) and a high turbidity (OR: 1.0039 [95 % CI: 1.0006–1.0072]).
This second study suggested that the use of Moore’s swabs is a simple, inexpensive and effective method of detecting B. pseudomallei in environmental water samples (Vongphayloth et al. 2012). Its main disadvantage is the inability to quantify the number of bacteria present. The high proportion of positive water samples around the highly contaminated site in Saravane East, in particular downstream on the Sedone River, suggests that surface waters are polluted by runoff from land-based reservoirs. A larger study is needed to confirm these results and analyse the relationship between the concentrations of B. pseudomallei in soil and the contamination of waters that drain it during the rainy season. The detection of this bacterium in river water with Moore’s swabs could be good way of identifying the most contaminated watersheds and locating the main environmental reservoirs in areas where melioidosis is endemic.
4 Conclusion
Melioidosis is a common severe community-acquired infection in Laos. Still unknown by the majority of doctors 10 years ago, it is being more frequently recognised, thanks to the strengthening of diagnostic capacity in a few hospital laboratories, but it is probable that its true incidence is still grossly underestimated. Nearly 80 % of the population of Laos live in rural surroundings, the majority undertaking rice farming. This serious illness, frequently fatal, difficult to identify and treat, must be considered an important threat to public health.
Study of the environmental reservoir of B. pseudomallei would assist in defining areas that are melioidosis-free, low risk and high risk. Such stratification would enable health workers in rural areas to gauge the importance of this disease in their differential diagnosis of sepsis, guide empirical therapy and target possible prevention campaigns. Environmental research needs to be undertaken to analyse the physico-chemical parameters of soil that encourage the proliferation of the bacterium and whether any interventions could reduce bacterial density.
References
Aldhous P (2005) Melioidosis? Never heard of it. Nature 434:692–693
Athan E, Allworth AM, Engler C, Bastian I, Cheng AC (2005) Melioidosis in tsunami survivors. Emerg Infect Dis 11:1638–1639
Cheng AC, Currie BJ (2005) Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev 18:383–416
Currie BJ (2008) Advances and remaining uncertainties in the epidemiology of Burkholderia pseudomallei and melioidosis. Trans R Soc Trop Med Hyg 102:225–227
Currie BJ, Jacups SP, Cheng AC, Fisher DA, Anstey NM, Huffam SE, Krause VL (2004) Melioidosis epidemiology and risk factors from a prospective whole-population study in northern Australia. Trop Med Int Health 9:1167–1174
Currie BJ, Dance DAB, Cheng AC (2008) The global distribution of Burkholderia pseudomallei and melioidosis: an update. Trans R Soc Trop Med Hyg 102:S1–S4
Gilad J, Harary I, Dushnitsky T, Schwartz D, Amsalem Y (2007) Burkholderia mallei and Burkholderia pseudomallei as bioterrorism agents: national aspects of emergency preparedness. Isr Med Assoc J 9:499–503
Holden MTG, Titball RW, Peacock SJ, Cerdeño-Tárraga AM, Atkins T, Crossman LC et al (2004) Genomic plasticity of the causative agent of melioidosis, Burkholderia pseudomallei. Proc Natl Acad Sci U S A 101:14240–14245
Inglis TJJ, Sagripanti JL (2006) Environmental factors that affect the survival and persistence of Burkholderia pseudomallei. Appl Environ Microbiol 72:6865–6875
Inglis TJJ, Rigby P, Robertson TA, Dutton NS, Henderson M, Chang BJ (2000) Interaction between Burkholderia pseudomallei and Acanthamoeba species results in coiling phagocytosis, endamebic bacterial survival, and escape. Infect Immun 68:1681–1686
Kaestli M, Mayo M, Harrington G, Watt F, Hill J, Gal D, Currie BJ (2007) Sensitive and specific molecular detection of Burkholderia pseudomallei, the causative agent of melioidosis, in the soil of tropical northern Australia. Appl Environ Microbiol 73:6891–6897
Kaestli M, Mayo M, Harrington G, Ward L, Watt F, Hill J et al (2009) Landscape changes influence the occurrence of the melioidosis bacterium Burkholderia pseudomallei in soil in Northern Australia. PLoS Negl Trop Dis 3:e364
Ketterer PJ, Webster WR, Shield J, Arthur RJ, Blackall PJ, Thomas AD (1986) Melioidosis in intensive piggeries in south eastern Queensland. Aust Vet J 63:146–149
Kronmann KC, Truett AA, Hale BR, Crum-Cianflone NF (2009) Melioidosis after brief exposure: a serologic survey in US marines. Am J Trop Med Hyg 80:182–184
Le Hello S, Currie BJ, Godoy D, Spratt BG, Mikulski M, Lacasin F et al (2005) Melioidosis in New Caledonia. Emerg Infect Dis 11:1607–1609
Leelarasamee A (2000) Melioidosis in Southeast Asia. Acta Trop 74:129–132
Limmathurotsakul D, Wongratanacheewin S, Teerawattanasook N, Wongsuvan G, Chaisuksant S, Chetchotisakd P, Chaowagul W, Day NPJ, Peacock SJ (2010) Increasing incidence of human melioidosis in Northeast Thailand. Am J Trop Med Hyg 82:1113–1117
Moore B (1948) The detection of paratyphoid carriers in towns by means of sewage examination. Mon Bull Minist Health Public Health Lab Serv 7:241–248
Peacock SJ, Schweizer HP, Dance DAB, Smith TL, Gee JE, Wuthiekanun V et al (2008) Management of accidental laboratory exposure to Burkholderia pseudomallei and B mallei. Emerg Infect Dis 14:e2
Phetsouvanh R, Phongmany S, Newton P, Mayxay M, Ramsay A, Wuthiekanun V, White NJ (2001) Melioidosis and Pandora’s box in the Lao People’s Democratic Republic. Clin Infect Dis 32:653–654
Phetsouvanh R, Phongmany S, Soukaloun D, Rasachak B, Soukhaseum V, Soukhaseum S, Frichithavong K et al (2006) Causes of community-acquired bacteremia and patterns of antimicrobial resistance in Vientiane, Laos. Am J Trop Med Hyg 75:978–985
Rattanavong S, Wuthiekanun V, Langla S, Amornchai P, Sirisouk J, Phetsouvanh R, Moore CE, Peacock SJ, Buisson Y, Newton PN (2011) Randomized soil survey of the distribution of Burkholderia pseudomallei in rice fields in Laos. Appl Environ Microbiol 77:532–536
Rolim DB, Rocha MF, Brilhante RS, Cordeiro RA, Leitão NP Jr, Inglis TJ et al (2009) Environmental isolates of Burkholderia pseudomallei in Ceara state, Northeast Brazil. Appl Environ Microbiol 75:1215–1218
Shams AM, Rose LJ, Hodges L, Arduino MJ (2007) Survival of Burkholderia pseudomallei on environmental surfaces. Applied Environ Microbiol 73:8001–8004
Shih HI, Chuang YC, Cheung BM, Yan JJ, Chang CM, Chang K et al (2009) Sporadic and outbreak cases of melioidosis in southern Taiwan: clinical features and antimicrobial susceptibility. Infection 37:9–15
Sprague LD, Neubauer H (2004) Melioidosis in animals: a review on epizootiology, diagnosis and clinical presentation. J Vet Med B Infect Dis Vet Public Health 51:305–320
Su H-P, Chan T-C, Chang C-C (2011) Typhoon-related leptospirosis and melioidosis, Taiwan, 2009. Emerg Infect Dis 17:1322–1324
Thibault FM, Hernandez E, Vidal DR, Girardet M, Cavallo JD (2004) Antibiotic susceptibility of 65 isolates of Burkholderia pseudomallei and Burkholderia mallei to 35 antimicrobial agents. J Antimicrob Chemother 254:1134–1138
Vongphayloth K, Rattanavong S, Moore CE, Phetsouvanh R, Wuthiekanun V, Sengdouangphachanh A, Phouminh P, Newton PN, Buisson Y (2012) Burkholderia pseudomallei detection in surface water in southern Laos using Moore’s swabs. Am J Trop Med Hyg 86:872–877
Vuddhakul V, Tharavichitkul P, Na-Ngam N, Jitsurong S, Kunthawa B, Noimay P, Noimay P, Binla A, Thamlikitkul V (1999) Epidemiology of Burkholderia pseudomallei in Thailand. Am J Trop Med Hyg 60:458–461
Wild S, Roglic G, Green A, Sicree R, King H (2004) Global prevalence of diabetes: estimates for the year 2000 and projections for 2030. Diabetes Care 27:1047–1053
Wuthiekanun V, Anuntagool N, White NJ, Sirisinha S (2002) Short report: a rapid method for the differentiation of Burkholderia pseudomallei and Burkholderia thailandensis. Am J Trop Med Hyg 66:759–761
Wuthiekanun V, Mayxay M, Chierakul W, Phetsouvanh R, Cheng AC, White NJ, Day NPJ, Peacock SJ (2005) Detection of Burkholderia pseudomallei in soil within the Lao People’s Democratic Republic. J Clin Microbiol 43:923–924
Wuthiekanun V, Langa S, Swaddiwudhipong W, Jetsadapanpong W, Kaengnet Y, Chierakul W et al (2006) Melioidosis in Myanmar: forgotten but not gone. Am J Trop Med Hyg 75:945–946
Wuthiekanun V, Pheaktra N, Putchhat H, Sin L, Sen B, Kumar V et al (2008) Burkholderia pseudomallei antibodies in children, Cambodia. Emerg Infect Dis 14:301–303
Acknowledgements
We are grateful to all the staff of the Microbiology Laboratory, Mahosot Hospital, Vientiane, Lao PDR, who assisted with the laboratory studies, and to the Minister of Health and the Director of the Curative Department, Ministry of Health, for their support. This work was undertaken as part of the programme of the Lao-Oxford-Mahosot Hospital-Wellcome Trust Research Unit funded by the Wellcome Trust of Great Britain.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media Singapore
About this chapter
Cite this chapter
Buisson, Y. et al. (2015). Melioidosis in Laos. In: Morand, S., Dujardin, JP., Lefait-Robin, R., Apiwathnasorn, C. (eds) Socio-Ecological Dimensions of Infectious Diseases in Southeast Asia. Springer, Singapore. https://doi.org/10.1007/978-981-287-527-3_7
Download citation
DOI: https://doi.org/10.1007/978-981-287-527-3_7
Publisher Name: Springer, Singapore
Print ISBN: 978-981-287-526-6
Online ISBN: 978-981-287-527-3
eBook Packages: MedicineMedicine (R0)