Abstract
Human pluripotent stems cells provide an ideal source for the study of hematopoietic differentiation. Natural killer (NK) cells are lymphocytes that play a key role in innate immunity against viral infections as well as malignancies. The development and differentiation of NK cells have been an area of increasing research interest due to their clinical utility in treating multiple types of cancer and potentially infectious disease. Our initial studies to derive NK cells from human embryonic stem cells (hESCs) and induced pluripotent stem cells (iPSCs) used a stromal cell co-culture method with relatively poor-defined conditions. Subsequent studies have utilized a stroma-free embryoid body (EB) method to generate hemato-endothelial precursor cells followed by in vitro NK cell differentiation in defined conditions. Further expansion of these hESC- and iPSC-derived NK cells can be done through the use of interleukin (IL)-21 expressing artificial antigen-presenting cells (aAPCs). Combining these methods, we can efficiently generate enough NK cells required for clinical therapies from a small number of undifferentiated human pluripotent stem cells. These methods enable hESCs and iPSCs to be used to produce an essentially unlimited amount of homogenous NK cells that can be used as a standardized, off-the-shelf immunotherapy for the treatment of refractory cancers and other diseases.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Embryonic stem cells
- Induced pluripotent stem cells
- Embryoid body
- Hematopoietic progenitors
- Natural killer cells
5.1 Introduction
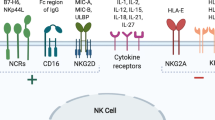
Natural killer (NK) cells represent an important lymphocyte population essential to the innate immune system with a role in protecting the host from both viral infections and malignancies. NK cells isolated from peripheral blood (PB-NK cells) have shown valuable use in the clinic for the treatment of acute myeloid leukemia (AML) as well as other malignancies [1–3]. However, the need for donors and cell processing may limit the use of PB-NK cells. Additionally, PB-NK cells are a heterogeneous cell population, with often less than 50 % NK cells in the product given to patients and will vary from each donor. A method to produce an “off-the-shelf” NK cell product from human pluripotent stem cells could overcome these hurdles. In vitro methods for the differentiation of NK cells from CD34+ cells isolated from human bone marrow or umbilical cord blood (UCB) have previously been established [4–7]. In these studies, NK cells were produced by culture of CD34+ cells with stem cell factor (SCF), IL-7, and Flt3 ligand (Flt3L). These conditions lead to cells that express IL-15 receptor, which has been shown to be critical for the formation of NK cells. Final NK cell differentiation is then driven by the addition of IL-15. Additional studies have aimed to improve the NK cell production from primary CD34+ cells using IL-21 signaling to mediate expansion of NK cells and stimulate expression of CD16 [8, 9], an Fc receptor typically expressed by NK cells and crucial for their ability to mediate antibody-dependent cell-mediated cytotoxicity.
Human pluripotent stem cells represent an ideal starting population for the development of multiple cell types, including NK cells. Human pluripotent stem cells include embryonic stem cells (ESCs) and induced pluripotent stem cells (iPSCs), both of which represent ideal starting populations to further study the development of NK cells in vitro. Furthermore, NK cells from hESC/iPSC provide a standardized cell-based treatment for malignant hematopoietic and solid tumors [10, 11]. However, the advancement of these treatments requires a reliable procedure for the production of large numbers of NK cells from hESC/iPSCs.
This chapter describes a method for the efficient generation of NK cells from hESC/iPSC. As previously described, both hESC- and iPSC-derived NK cells (hESC-NKs, iPSC-NKs) express activating and inhibitory receptors similar to NK cells isolated from adult peripheral blood [12–14]. The hESC-derived NK cells are also highly efficient at direct cell-mediated cytotoxicity and antibody-dependent cell-mediated cytotoxicity, as well as production of cytokines such as interferon-γ. Stromal cell co-culture or stroma-free systems can be used to generate hematopoietic progenitor cells, both of which are capable of developing into functional NK cells. For ease of clinical translation, we have recently adopted a “spin EB” protocol [15, 16] to provide a system for more consistent hematopoietic cell differentiation without the use of xenogeneic stromal cells (Fig. 5.1). Following the formation of the hemato-endothelial precursor cells through the “spin EB” process, NK cells are differentiated from the embryoid bodies (EBs) using procedures similar to those used for CD34+ cells isolated from peripheral blood, or cord blood. Again, this NK cell differentiation step can be done with support from stromal cell co-culture or can be done without the aid of stromal cells for ease of clinical translation.
Schematic diagram of two-step hematopoietic and NK cell differentiation from human embryonic stem cells or induced pluripotent stem cells. In brief, undifferentiated hESC/iPSCs are induced to differentiate into hematopoietic progenitor cells by spin EB formation. The hematopoietic progenitor cells can be characterized based on expression of specific cell surface markers (typically CD34 and CD45). Spin EBs can be directly transferred into NK cell development conditions with defined media plus cytokines. After 3–5 weeks, mature and functional NK cells develop. NK cells can be further expanded using aAPCs and IL-2
5.2 Materials
5.2.1 Cell Lines
-
1.
H1 and H9 line human ES cells (WiCell, Madison, WI). Multiple iPS cell lines have been generated and used in our laboratory for the expression of the four transcription factors Oct4, Sox2, c-Myc, and Klf4 in CD34+ UCB cells, human fibroblasts, or human peripheral blood cells. hESCs/iPSCs are maintained as undifferentiated cells as previously described [17] (Note 1).
-
2.
EL08-1D2 stromal cells (Kindly provided by Dr. Rob Oostendorp, Technical University, Munich, Germany) [18, 19]. These cells are maintained in 50 % Myelocult M5300 (StemCell Technologies, cat. no. 05350), 35 % Alpha Minimum Essential Media (Invitrogen, cat. no. 12571-063), 15 % FBS (StemCell Technologies, cat. no. 06500), 1 % Glutamax 1 (100×, Invitrogen, cat. no. 35050-061), 0.1 mM β-mercaptoethanol, 10−6 M hydrocortisone (StemCell Technologies, cat. no. 07904), and 1 % penicillin/streptomycin.
-
3.
K562 cells expressing membrane-bound IL-21 (Clone 9. mbIL-21) (Kindly provided by Drs. Dean Lee and Lawrence Cooper, MD Anderson Cancer Center, Houston, TX) [20]. These cells are maintained in RPMI-1640 plus L-glutamine, 10 % FBS, and 1 % penicillin/streptomycin.
5.2.2 Hematopoietic Differentiation of hES/iPS Cells by Spin EBs
-
1.
Spin EB differentiation medium (BPEL media) [15]: 43 % Iscove’s Modified Dulbecco’s Medium (IMDM, Thermo, cat. no. SH30228.01), 43 % F-12 Nutrient Mixture w/Glutamax I (Invitrogen, cat. no. 3176503), 0.25 % deionized bovine serum albumin (BSA, Sigma-Aldrich, cat. no. A3311), 0.25 % poly (vinyl alcohol) (Sigma-Aldrich, cat. no. P8136), 0.1 ug/mL linoleic acid (Sigma-Aldrich, cat. no. L1012), 0.1 ug/mL linolenic acid (Sigma-Aldrich, cat. no. L2376), 1:500 Synthechol 500× solution (Sigma-Aldrich, cat. no. S5442), 450 uM α-monothioglycerol (α-MTG) (Sigma-Aldrich, cat. no. M6145), 5 % protein-free hybridoma mix II (Invitrogen, cat. no. 12040077), 50 ug/mL ascorbic acid 2-phosphate (Sigma-Aldrich, cat. no. A8960), 2 mM Glutamax I (Invitrogen, cat. no. 35050061), 1 % Insulin, Transferrin, and Selenium 100× solution (ITS) (Invitrogen, cat. no. 41400-045), 1 % penicillin/streptomycin plus 40 ug/mL recombinant human SCF (PeproTech, cat. no. 300-07), 20 ug/mL BMP4 (R&D systems, cat. no. 314-BP), and 20 ug/mLVEGF (R&D systems, cat. no. 293-VE).
-
2.
TrypLE Select (Gibco/Invitrogen, cat. no. 12563-011).
-
3.
Dulbecco’s phosphate buffer saline (HyClone, cat. No. SH30028.02).
-
4.
96-well round bottom plates (NUNC, cat. no. 262162 with lids cat. no. 264122).
5.2.3 Natural Killer Cell Differentiation from Differentiated Spin EBs
-
1.
NK cell differentiation medium: 56.6 % DMEM-high glucose, 28.3 % HAMS/F12 (Invitrogen, cat. no. 11765-064), 15 % heat-inactivated human AB serum (Valley Biomedical, cat. no. HP1022 HI), 2 mM L-glutamine, 1 uM β-mercaptoethanol, 5 ng/mL sodium selenite (Sigma-Aldrich, cat. no. S5261), 50 uM ethanolamine (MP Biomedicals, cat. no. 194658), 20 mg/L ascorbic acid (Sigma-Aldrich, cat. no. A-5960), 1 % P/S, 5 ng/mL IL-3 (PeproTech, cat. no. 200-03), 20 ng/mL SCF, 20 ng/mL IL-7 (PeproTech, cat. no.), 10 ng/mL IL-15 (PeproTech, cat. no. 200-15), and 10 ng/mL Flt3 ligand (Flt3L) (PeproTech, cat. no. 300-19). Store at 4 °C in the dark.
-
2.
24-well tissue culture plates (NUNC Brand Products, Nalgene Nunc; cat. no. 142475).
5.2.4 Natural Killer Cell Expansion
-
1.
NK cell expansion medium: RPMI-1640, 10 % FBS, 2 mM L-glutamine, 1 % P/S, and 50 U/mL IL-2 added just prior to NK cells.
5.3 Methods
5.3.1 TrypLE Adaptation of hESC/iPSCs
Prior to the generation of spin EB, undifferentiated hESCs/iPSCs must be TrypLE adapted, a method previously described [15, 21]. This process allows for the hESC/iPSC to be made more efficiently into single-cell suspensions. Prior to adaptation, carefully remove differentiated hES/iPS cells and colonies because differentiated cells can easily dominate the cultures. It is very important to make sure your starting population does not contain differentiated cells. Cells can usually be used to set up spin EBs after 12–15 passages in TrypLE.
-
1.
The day prior to passing hESC/iPSCs, seed gelatin-coated 6-well plates with low-density MEFs. Low-density MEFs are plated at ½ the amount of what would be used to support hESC/iPSC cultures. We use 90,000 cells/well of a 6-well plate as low density.
-
2.
After making sure the starting population is free of differentiated colonies, aspirate media and pass hESC/iPSCs by incubating cells for 5 min at 37 °C in pre-warmed TrypLE.
-
3.
Collect cells by gentle pipetting and dilute using equal parts of hESC/iPSC media and DPBS.
-
4.
Centrifuge cells and aspirate media.
-
5.
Wash cells once by resuspending cell pellet in media and DPBS and then centrifuge again.
-
6.
Plate hESC/iPSCs 1:1 onto low-density MEFs plated the day prior to passing.
-
7.
Replace media daily and repeat procedure when cells become confluent. After ~5 passages, split cells 1:2 or 1:3 and eventually cells can be split 1:6 twice a week.
5.3.2 Generation of Hematopoietic Progenitor Cells from hES/iPS Cells by Spin EB Formation
Many studies have investigated hematopoietic differentiation by embryoid body (EB) formation. Advantages of this method compared to stromal cell co-culture include defined culture conditions and higher efficiency of hematopoietic progenitor cell generation. However, the EB system can be compared with the co-culture system [22, 23]. The spin EB approach developed by Elefanty’s group [15, 21] allows for a more consistent generation of hematopoietic progenitors.
-
1.
Two days prior to setting up spin EB differentiation, pass 200,000–250,000 TrypLE-adapted hESC/iPSCs onto fresh MEFs. They should be 70–80 % confluent on the day of spin EBs setup. Generally 2–3 wells of a 6-well plate are sufficient for 5 plates of spin EB.
-
2.
To prepare for Spin EB plating, pipet 150 µL sterile water into the 36 outer wells of each 96-well plate to minimize loss of well volume to evaporation.
-
3.
Aspirate culture media from ES/iPS cells and add 1 ml pre-warmed TrypLE to each well. Place plates in cell culture incubator (5 % CO2, 37 °C) for 4–5 min until hESC/iPSC cells start to come off the plate.
-
4.
Collect dissociated cells in a conical tube and pipet up and down to break up clumps. Dilute TrypLE with 1 volume BPEL media and at least 1 volume DPBS. Centrifuge cells, remove supernatant, and resuspend the cells in 5 ml BPEL media plus 5 ml DPBS. Centrifuge cells again.
-
5.
Remove supernatant and resuspend cells in 5 ml BPEL media. Pass cells through 70-µm filter into a fresh conical tube in order to remove clumps. Count filtered cells and aliquot the appropriate number of cells to be used for plating. Typically, cells are seeded at 3000 cells/well in the 96-well plates, though this density can be varied if desired. Centrifuge and resuspend hESC/iPSCs in BPEL containing cytokines at a concentration of 3 × 104 cells/ml.
-
6.
Pipet 100 µl of the cell suspension into each of the inner 60 wells of the prepared 96-well plates with 150 µl of water in outer wells using a multi-channel pipet. Centrifuge 96-well plates at 480 g, 8 °C for 4 min, and incubate the plates at 37 °C, 5 % CO2 for 8–11 days (Fig. 5.2). We have found with our hESC/iPSCs that 11 days is optimal for the formation of hematopoietic progenitors defined by the presence of CD34+CD45+ cells. It is important not to disturb the plates during the first 3 days of differentiation while the spin EBs are forming (Note 2). Under optimal conditions, the percentage of CD34+ cells can be approximately 40–60 % and percentage of CD34+CD45+ can be up to 20–40 %. While there is variability between different hESC and iPSC lines, some lines can be used up to passage 40–50 after TrypLE adaptation to make spin EBs.
Fig. 5.2 Phase microscope images of developing NK cells from human pluripotent stem cells. a Images taken of spin EBs at day 0 and day 11, immediately before transfer to NK cell differentiation conditions. Spin EBs were made using 3000 cells/well and cultured in SCF, BMP-4, and VEGF. b Images of NK cell differentiation with or without stromal cells. In the enlarged image, non-adherent hematopoietic cells can be seen being produced from the EB population, which is still intact after transfer. In these conditions, the spin EBs also produce adherent endothelial cells and mesenchymal cells. c Images of NK cells being grown in aAPC expansion culture. At this point, the cells are a homogenous NK cell population
5.3.3 Natural Killer Cell Differentiation with or without Stromal Cells
Transfer of spin EBs can be done into 24-well plates with either stromal cells or in a feeder-free method. We have observed that with stromal cells we get slightly higher yields of NK cells, but the feeder-free method is better suited for clinical translation [23].
-
1.
If stromal cell co-culture is desired: The EL08-1D2 (note 3) feeder plates are usually prepared the day before transferring spin EBs. Dissociate cells from flask with 0.05 % trypsin. Collect cells by centrifugation and resuspend in 80 % fresh medium +20 % old medium to 1.2–1.25 × 105/mL. Cell are plated onto 0.1 % gelatin-coated 24-well plates at 1 mL/well and will grow to 85–90 % confluency at 33 °C, 5 % CO2 by the following day. The plates are then X-ray irradiated with 3000 rad, and the feeders are ready for use.
-
2.
Spin EBs (without sorting) are directly transferred into 24-well plates on day 11, with or without stromal cells. Using a multi-channel pipet, carefully remove ½ the volume from the 96-well plates prior to transferring. We transfer 6–8 EBs into each well of the 24-well plate using the multi-channel pipet where two tips fit into each well. Each well then receives 0.5–0.7 mL of NK differentiation medium containing all of the cytokines (note 4).
-
3.
Half-medium changes are done every 5–7 days. Following the first week of the NK cell differentiation, IL-3 is no longer added to the media.
-
4.
Continue half-medium changes for 4–5 weeks to achieve mature NK cells (Fig. 5.2) (note 5). Cells can then be collected by passing them through a 70-μm filter to remove any clumps.
-
5.
Mature CD45+CD56+ NK cells can be phenotyped by flow cytometry. In vitro function of hES/iPS cell-derived NK cells can be analyzed by the measurement of direct cytolytic activity tumor cells (such as K562) by a standard 51Cr-release assay or immunological assays for cytotoxic granule or cytokine release [13, 14]. NK cells developed under feeder-free condition also show a mature NK cell phenotype and cytotoxicity.
5.3.4 Clinical Scale Expansion of hESC-/iPSC-Derived NK Cells for Immunotherapy
From two 24-well plates, we regularly able to produce 3–10 × 106 NK cells. In order to further expand the NK cells, artificial antigen-presenting cells (aAPCs) are used to generate >109 NK cells (Fig. 5.3) [20, 23].
Expansion data for the growth of NK cells using aAPCs. H9 ESC-NK cells grown in EL08-ID2 stromal cells (black line), H9 ESC-NK cells grown in feeder-free conditions (gray line), and iPSC-NK cells grown in feeder-free conditions (black dashed line) were transferred from NK cell differentiation conditions and placed in aAPCs for expansion. Cells were stimulated with aAPCs weekly and expanded for 9 weeks. Cell number was normalized to 1 × 106 cells on D0. Each line represents mean of 2 independent experiments
-
1.
In order to prepare for expansion of NK cells, aAPCs have to be cultured and irradiated. We utilize mbIL-21 K562 s that receive lethal irradiation with 10,000 rads. These can be prepared on the day of expansion or frozen stocks can be made ahead of time.
-
2.
Following NK cell differentiation, the cells are collected by passing them through a 70-μm filter. The cells are then centrifuged and resuspended at a density of 2 × 105 cells/mL in NK expansion medium containing 50 U/mL IL-2 added freshly.
-
3.
The NK cells are then stimulated using aAPCs every 7 days. Initially, we use 2:1 aAPC:NK cells for the first week and thereafter a ratio of 1:1. Media are changed every 3–4 days containing 50 U/mL of freshly added IL-2.
-
4.
NK cells can be expanded for >60 days without a decrease in cell viability or cytolytic activity.
5.4 Notes
-
1.
We have successfully performed NK cell differentiation from multiple iPS cell lines derived from various starting cell populations.
-
2.
EBs should start to form after 24-h incubation, but if hESC/iPSCs have not been well adapted by TrypLE (at least >10 passages), spin EBs may not be formed well. Also, BPEL components should be changed every 3–4 months with the exception of PVA and deionized BSA, which should be made every 4 weeks.
-
3.
EL08-1D2 stromal cells are a temperature-sensitive cell line, which should be maintained at an incubator with 33 °C and 5 % CO2. However, cells can be kept at 37 °C after inactivation. Additionally, other stromas such as OP9, OP9DL1, and OP9DL4 have been compared with EL08-1D2 for NK cell differentiation in our laboratory. OP9DL1 s were found to be just as efficient as EL08-1D2.
-
4.
Poor NK cell differentiation from hematopoietic progenitors on EL08-1D2 stromal cell co-cultures. If these feeder cells have been passed in culture for more than two months (typically more than 10 passages), they may not support NK cell development effectively. The resource and different lots of cytokines also affect NK cell differentiation. Also make sure cytokines are stored at −20 °C long term and no longer than a week at 4 °C. If necessary, use fresh stromal cells every week until mature NK cells development.
-
5.
It usually takes longer (about 5 weeks) to derive NK cells from spin EBs than from enriched progenitors from stromal co-culture. It is likely that hematopoietic progenitor cells in day-11 spin EBs are still in earlier development status compared with those from day 21 M210-B4 co-cultures.
References
Ljunggren HG, Malmberg KJ. Prospects for the use of NK cells in immunotherapy of human cancer. Nat Rev Immunol. 2007;7:329–39.
Miller JS, Soignier Y, Panoskaltsis-Mortari A, et al. Successful adoptive transfer and in vivo expansion of human haploidentical NK cells in patients with cancer. Blood. 2005;105:3051–7.
Geller MA, Cooley S, Judson PL, et al. A phase II study of allogeneic natural killer cell therapy to treat patients with recurrent ovarian and breast cancer. Cytotherapy. 2011;13:98–107.
Miller JS, Alley KA, McGlave P. Differentiation of natural killer (NK) cells from human primitive marrow progenitors in a stroma-based long-term culture system: identification of a CD34 + 7 + NK progenitor. Blood. 1994;83:2594–601.
Miller JS, McCullar V, Verfaillie CM. Ex vivo culture of CD34 +/Lin-/DR- cells in stroma-derived soluble factors, interleukin-3, and macrophage inflammatory protein-1alpha maintains not only myeloid but also lymphoid progenitors in a novel switch culture assay. Blood. 1998;91:4516–22.
Silva MR, Kessler S, Ascensao JL. Hematopoietic origin of human natural killer (NK) cells: generation from immature progenitors. Pathobiology. 1993;61:247–55.
Mrózek E, Anderson P, Caligiuri MA. Role of interleukin-15 in the development of human CD56 + natural killer cells from CD34 + hematopoietic progenitor cells. Blood. 1996;87:2632–40.
Sivori S, Cantoni C, Parolini S, et al. IL-21 induces both rapid maturation of human CD34 + cell precursors towards NK cells and acquisition of surface killer Ig-like receptors. Eur J Immunol. 2003;33:3439–47.
Perez SA, Mahaira LG, Sotiropoulou PA, et al. Effect of IL-21 on NK cells derived from different umbilical cord blood populations. Int Immunol. 2006;18:49–58.
Wilber A, Linehan JL, Tian X, et al. Efficient and stable transgene expression in human embryonic stem cells using transposon-mediated gene transfer. Stem Cells. 2007;25:2919–27.
Giudice A, Trounson A. Genetic modification of human embryonic stem cells for derivation of target cells. Cell Stem Cell. 2008;2:422–33.
Woll PS, Martin CH, Miller JS, Kaufman DS. Human embryonic stem cell-derived NK cells acquire functional receptors and cytolytic activity. J Immunol. 2005;175:5095–103.
Ni Z, Knorr DA, Clouser CL, et al. Human pluripotent stem cells produce natural killer cells that mediate anti-HIV-1 activity by utilizing diverse cellular mechanisms. J Virol. 2011;85:43–50.
Woll PS, Grzywacz B, Tian X, et al. Human embryonic stem cells differentiate into a homogeneous population of natural killer cells with potent in vivo antitumor activity. Blood. 2009;113:6094–101.
Ng ES, Davis R, Stanley EG, Elefanty AG. A protocol describing the use of a recombinant protein-based, animal product-free medium (APEL) for human embryonic stem cell differentiation as spin embryoid bodies. Nat Protoc. 2008;3:768–76.
Ng ES, Davis RP, Azzola L, Stanley EG, Elefanty AG. Forced aggregation of defined numbers of human embryonic stem cells into embryoid bodies fosters robust, reproducible hematopoietic differentiation. Blood. 2005;106:1601–3.
Kaufman DS, Hanson ET, Lewis RL, Auerbach R, Thomson JA. Hematopoietic colony-forming cells derived from human embryonic stem cells. Proc Natl Acad Sci USA. 2001;98:10716–21.
Oostendorp RA, Robin C, Steinhoff C, et al. Long-term maintenance of hematopoietic stem cells does not require contact with embryo-derived stromal cells in cocultures. Stem Cells. 2005;23:842–51.
Ledran MH, Krassowska A, Armstrong L, et al. Efficient hematopoietic differentiation of human embryonic stem cells on stromal cells derived from hematopoietic niches. Cell Stem Cell. 2008;3:85–98.
Denman CJ, Senyukov VV, Somanchi SS, et al. Membrane-bound IL-21 promotes sustained ex vivo proliferation of human natural killer cells. PLoS ONE. 2012;7:e30264.
Ng ES, Davis RP, Hatzistavrou T, Stanley EG, Elefanty AG. Directed differentiation of human embryonic stem cells as spin embryoid bodies and a description of the hematopoietic blast colony forming assay. Curr Protoc Stem Cell Biol Chapter. 2008;1: Unit 1D 3.
Hexum MK, Tian X, Kaufman DS. In vivo evaluation of putative hematopoietic stem cells derived from human pluripotent stem cells. Methods Mol Biol. 2011;767:433–47.
Knorr DA, Ni Z, Hermanson D, et al. Clinical-scale derivation of natural killer cells from human pluripotent stem cells for cancer therapy. Stem Cells Transl Med. 2013;2:274–83.
Acknowledgments
Support for studies of NK cell development have come from National Institutes of Health/NHLBI, the University of Minnesota Masonic Cancer Center, the William Lawrence & Blanche Hughes Foundation, the State of Minnesota Partnership for Biotechnology and Medical Genomics, the Minnesota Ovarian Cancer Alliance, and the International Clinical Research Center.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 The Author(s)
About this chapter
Cite this chapter
Hermanson, D.L., Ni, Z., Kaufman, D.S. (2015). Human Pluripotent Stem Cells as a Renewable Source of Natural Killer Cells. In: Cheng, T. (eds) Hematopoietic Differentiation of Human Pluripotent Stem Cells. SpringerBriefs in Stem Cells, vol 6. Springer, Dordrecht. https://doi.org/10.1007/978-94-017-7312-6_5
Download citation
DOI: https://doi.org/10.1007/978-94-017-7312-6_5
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-017-7311-9
Online ISBN: 978-94-017-7312-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)