Abstract
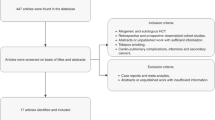
Tobacco use is the leading preventable cause of death in the United States. Recent research in Hematopoietic Stem Cell Transplant (HSCT) populations has begun to examine smoking cigarettes as a risk factor for adverse transplant outcomes. Based on these early studies, estimated prevalence rates vary widely. Lifetime history of smoking among HSCT patients likely approximates that of the general population, while current use appears less than the general population. Smoking has been associated with multiple adverse HSCT outcomes, including shorter duration of disease-free and overall survival; higher treatment related mortality; higher pulmonary infection and respiratory failure rates; higher rates of disease recurrence; increased risk for cardiovascular events; and longer duration of hospitalization. Potential mechanisms are likely many, and include impaired bone marrow hematopoiesis, inflammation, impaired pulmonary function, and also significant associations with other maladaptive health behaviors know to adversely affect general population health outcomes, but understudied in HSCT populations. Future directions for tobacco research in HSCT should focus on use of behavior science methodology to minimize biases common to self-report methodology, and analyzing the effects of both current and lifetime use. Current use is a modifiable risk factor. Cancer diagnosis and HSCT serve as “teachable moments” during which patient motivation to quit tobacco use is increased. Survivor care plans serve as a timely platform for integration of evidence-based tobacco dependence treatment into a comprehensive care plan that targets all known significant risk factors to optimize HSCT outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Hematopoietic Stem Cell Transplant
- Allogeneic Hematopoietic Stem Cell Transplant
- Cigarette Smoke Extract
- Treatment Related Mortality
- Hematopoietic Stem Cell Transplant Recipient
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
Tobacco use is the leading preventable cause of death (ACS 2011). It is responsible for one out of five deaths in US (Mokdad et al. 2004; Steenland et al. 2004) and accounts for at least 30% of all cancer deaths (USDHHS 2010). Recent evidence suggests that tobacco use is linked to worse cancer patient outcomes after hematopoietic stem cell transplantation.
Tobacco and Hematologic Malignancies
A 2004 meta-analysis of smoking and cancer (Levitz et al. 2004) confirmed an etiological link between smoking and increased risk of leukemia, especially among individuals who have acute myeloid leukemia. Hypothesized mechanisms (Cooke and Bitterman 2004; Geyer et al. 2010; Gritz et al. 2008; Sandler et al. 1993; USDHHS 2010) include direct carcinogen impact, activation of other carcinogens through induction of metabolizing enzymes, influence on immunologic functioning (increasing pro-inflammatory cytokines and T-cell function), and impact on the prevalence of the translocation and over expression of bcl-2. (Varadarajan et al. 2010) found decreasing rates in leukemia mortality coincided with declines in population based smoking rates. Smokeless tobacco use has not been studied in relation to hematologic malignancies.
Prevalence of Tobacco Use in Hematopoientic Stem Cell Transplant Populations
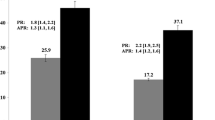
A lifetime history of smoking has been documented in 10–62% of hematopoietic stem cell transplant (HSCT) candidates (Ehlers et al. 2011; Tran et al. 2011), while 0–17% of candidates reported smoking in the year prior to transplant (Chang et al. 2004a, b; Ho et al. 2001; Marks et al. 2009; Miceli et al. 2006; Savani et al. 2005; Sharma et al. 2005; Thompson et al. 2002; Wilczynski et al. 1998). This range of lifetime smoking prevalence rates documented among HSCT candidate studies varies widely, but surrounds the general population prevalence rate. Current use ranges slightly lower than the general population prevalence. The 2009 general population prevalence of smoking is estimated as 19.3 % current use and 57.1% of US adults report smoking more than 100 cigarettes in their lifetime (CDC 2009, 2011).
The prevalence of smoking and smoking relapse in the post-transplant period has been examined by a prospective and a retrospective cohort study, yielding estimates of 0–17%. Chang et al. (2004a) examined smoking prospectively among CML patients undergoing allogeneic HSCT. They documented a 62% lifetime prevalence of smoking with 0% smoking 1 year after transplant. One study has examined smoking prevalence among a retrospective cohort of HSCT survivors, documenting a 17% prevalence 2–22 years post-transplant (Bishop et al. 2010). The similarity to smoking prevalence among HSCT candidates suggests that the prevalence of smoking is stable into the survivorship period. However a cohort bias may be inflating the survivorship estimate, given that current smoking rates have decreased from over 42.4 % in 1965 to 19.3% in 2011 (CDC 2011). Prospective cohort studies are needed to understand the course of smoking across the HSCT care continuum.
Outcomes Associated with Tobacco Use in HSCT Populations
Survival
Recent studies have linked smoking to worse survival after HSCT, focused on allogeneic HSCT recipients treated for acute and chronic myelogenous leukemias (Chang et al. 2004a, b; Ehlers et al. 2011; Marks et al. 2009). Marks et al. (2009) studied sibling allograft recipients treated for CML. They documented that lifetime heavy smoking (>10 pack years, >20 cigarettes per day) was associated with reduced disease free survival and overall survival compared to non-smokers. Five-year survival rates were reduced by 18% (68% among never smokers vs. 50% among high dose smokers). Additionally, treatment related mortality was 50% for heavy smokers versus 28% in non-smokers. The treatment related mortality rate for low-dose smokers was not significantly different (32%). Treatment related mortality for unrelated donor transplants was 68, 50, and 49% for high-dose, low-dose, and never smokers. Similarly, Hoodin et al. (2004) found that lifetime smoking history before transplant was associated with decreased survival rates among a mixed sample of HCST recipients. Savani et al. (2005) also associated a lifetime history of smoking with a fivefold increase in the risk of transplantation-related mortality from pulmonary causes. Ehlers et al. (2011) examined current and lifetime smoking history. They documented that current smoking of any quantity (defined as use during the year prior to transplant) was associated with lower rates of survival post transplant compared to never-smokers, among a HSCT recipients treated for acute leukemias. The effect for lifetime smoking history on survival was not statistically significant in this study of 152 HSCT recipients. Null results are documented by Chang et al. (2004a); smoking behavior was not found to affect 1 year survival rates among patients with CML who underwent HSCT. We could not locate published studies on the impact of tobacco use among other disease-specific HSCT populations. Notably, smoking has been found to negatively impact overall survival rates among Non-Hodgkin’s lymphoma patients (Geyer et al. 2010).
Disease Remission and Recurrence
At least four studies have examined the impact of smoking on recurrence among allogeneic HSCT recipients. Marks et al. (2009) found that smoking 10 or more years (lifetime) was associated with a higher relative risk of CML relapse among allogeneic recipients. Multivariate analysis showed LOWER dose smokers were more at risk for relapse, which the authors attributed to higher mortality rates among high dose smokers. Chang et al. (2004b) also led two studies of recurrence associated with smoking among allogeneic HSCT recipients treated for chronic myelogenous leukemia. She found a 1.7% increased risk of recurrence associated with each lifetime pack-year of smoking after allogeneic HSCT. In a later study, she documented a threefold increased risk of disease recurrence for a person with any lifetime smoking history (Chang et al. 2004b). Tran et al. (2011) documented a higher risk of relapse in a mixed disease sample of allogeneic HSCT recipients related to a twofold increase in lifetime pack-years, however this was not statistically significant in their sample of 845 recipients with 85 smokers. One study reported no difference in disease remission between smokers and non-smokers pre-transplant treated for acute myelogenous leukemia (Chelghoum et al. 2002)
Transplant Complications
Infection is a common complication of HSCT. One study found that pulmonary infections were associated with smoking during the aplastic period following chemotherapy for acute myeloid leukemia pre-transplant (26 smokers vs. 18% non-smokers), (Chelghoum et al. 2002). Miceli et al. (2006) documented that active pre-transplant smoking was also associated with increased risk of pulmonary infection post-transplant, with 37% of tobacco users versus 27% of non-users experiencing infection (60 days post follow-up). Graft versus host disease is also a common complication of allogeneic HSCT. One study (Marks et al. 2009) found no difference in the incidence of acute and chronic GHVD in past or present smokers compared to non-smokers.
Notably, smoking has a dose-dependent effect on bone loss which increases fracture risk (Ward and Klesges 2001). Bone grafts also have a lower success rate among past and current smokers compared to non-smokers (Spear et al. 1999). The association between smoking and bone health deserves further study among HSCT recipients, especially those treated for multiple myeloma who commonly experience bone lesions and fractures.
Comorbidities
A few studies document the pulmonary effects of smoking among HSCT recipients as at least one probable mechanism of increase mortality risk. As above, Savani et al. (2005) associated a lifetime history of smoking with a fivefold increase in the risk of transplantation-related mortality from pulmonary causes. Ehlers et al. (2011) found that pulmonary/respiratory causes of death was higher in previous and current smokers (20, 26%) compared to never smokers (6%). Similarly, Tran et al. (2011) found that each doubling of lifetime pack-years smoked was associated with a 33% increased risk of early respiratory failure, independent of pre-transplant lung function.
Reduced pulmonary function associated with smoking has also been documented among HSCT candidates and recipients pre-transplant. Ehlers et al. (2011) documented reduced FEV1 and DLCO associated with smoking pre-transplant. Post-transplant, smoking has been associated with increased diffuse alveolar damage (Sharma et al. 2005). A study by Ho et al. (2001) resulted in null findings in an examination of severe pulmonary complications limited to the period 60 days post-transplant. Two other studies found null results in examination of a possible association between lifetime smoking and lung function. Notably the prevalence rates of smoking in these samples were much lower than expected based on general population prevalence rates (6.7 and 34%) (Thompson et al. 2002; Wilczynski et al. 1998).
Published examinations of non-pulmonary comorbidities associated with smoking among HSCT recipients are rare, and deserve further exploration as possible contributing mechanisms to explain increased mortality risk. Tichelli et al. (2008) examined the occurrence of cardiovascular events after allogeneic HSCT with a prevalence of 3.6% in the 7 year time period (range from 1 to 13 years). They found that 41% of people who had an arterial event (MI, Chronic coronary heart disease, angina) post-transplant smoked cigarettes currently. Though not studied among HSCT recipients, smoking has also been associated with multiple other comorbidities (Ehlers et al. 2011; Savani et al. 2005; Tran et al. 2011).
Health Care Utilization and Costs
Given the increased risk of HSCT mortality, pulmonary risk, and general smoking related comorbidities, it is reasonable to hypothesize that higher health care utilization and costs are associated with smoking. One study (Ehlers et al. 2011) examined this question, finding that current smokers averaged 21 more days hospitalization in an outpatient-based HSCT program in the 1 year post transplant compared to never smokers. Though not calculated within their study, they cite national average charges for hospitalization with leukemia as primary diagnosis that translated to average hospitalization charges $126,434 greater for a patient smoking pre-transplant within the first year post-HSCT.
Potential Mechanisms
Zhou et al. (2011) hypothesized that cigarette smoking may impair bone marrow hematopoiesis and induce inflammation, documenting that marrow from healthy individuals exposed to cigarette smoke extract had significantly diminished CFU-E, BFU-E and CFU-GM. Cigarette smoke extract inhibited the growth of erythroid and granulocyte-macrophage progenitors. Additionally, health behaviors cluster, such that people who smoke are more likely to engage in other maladaptive health behaviors that may additively (Blanchard et al. 2008; Coups and Ostroff 2005) or synergistically affect outcomes.
Limitations of Studies Cited and Future Directions
The true prevalence of lifetime smoking and smoking prior to hematologic diagnosis among HSCT candidates is likely at least as high as the general population. Many of the studies cited here report lifetime prevalence rates that are much lower, thus the possibility of biases (e.g., self-report, retrospective recall, selection, abstraction methodology) resulting in under-reporting should be considered and addressed in future studies. Additionally, the range of smoking prevalence post-transplant likely reflects a self-report bias, namely under-reporting related to social stigma and a desire to please clinician teams who provided potentially lifesaving treatment. Underestimated prevalence of smoking likely translates to reduced precision and effect sizes in the above literature, thus under-estimating the true effects of smoking on HSCT outcomes. Additionally, several studies are underpowered to detect differences among smokers (i.e., not enough smokers in these studies to detect differences) (Marks et al. 2009), and follow-up may not be of sufficient duration to detect effects (Thompson et al. 2002).
When possible, standardized self-report queries with normative references should be employed in prospective cohorts. Population norms should be referenced when reporting smoking prevalence rates to estimate possible bias and missing data. Within retrospective cohorts, vague or absent tobacco information should be categorized as missing data. Future studies utilizing biochemical validation of self-report (e.g., cotinine as a metabolite of nicotine) could aid in elucidating the true prevalence of active smoking, but cannot estimate history of smoking. This would help address potential self-report biases, such as fear of reporting tobacco use in the context of HSCT candidacy evaluation or follow-up.
Additionally, current smoking should be differentiated from lifetime smoking, as the former is a modifiable risk factor that can be targeted within patient care. Most current studies focus on lifetime smoking. Current smoking should be liberally defined (e.g., within the year prior to transplant) to account for self-report biases that likely increase surrounding the time of evaluation and treatment. Smokeless forms of tobacco use are understudied at least partially due to lower prevalence rates, but deserve further research attention nonetheless.
Smoking Cessation Among HSCT and Cancer Patient Populations
Smoking cessation has not been studied among HSCT patients, beyond above documented change in prevalence rates. The work of Gritz et al. (2006) suggests that cancer diagnosis is a teachable moment; the sooner after diagnosis smoking cessation intervention is delivered, the more personally relevant and potentially effective. Observational studies also link cancer diagnosis to increased quit attempts (Cooley et al. 2011; Hsu et al. 2011). Relapse rates among cancer patients vary, but generally range from 13 to 60% 1 year after treatment (Gritz et al. 2006).
Clinical Practice Guidelines
Evidence based practice guidelines for the general population utilize the “5 As” (Ask, Advise, Assess, Assist, and Arrange) (Fiore et al. 2008). This brief intervention approach focuses on systematically identifying tobacco use, providing professional advice to quit using tobacco, determining motivation/willingness to quit, providing counseling and/or pharmacotherapy, and including as a topic of follow up visits. The guidelines are based on behavioral science, including motivational interviewing principles and problem solving/skills training. The American Cancer Society guidelines support application of this approach to cancer patients (Doyle et al. 2006).
Limitations in Smoking Cessation Trials
Smoking cessation trials among cancer populations focus primarily on head and neck and lung cancer populations, in which the disease is highly correlated with tobacco use. These intervention studies often utilize small sample sizes and thus may be under powered. Additionally, many of the interventions take a general approach and may not be addressing specific needs of patients.
References
American Cancer Society (ACS) (2011) American Cancer Society. Cancer facts and figures 2011. Retrieved from http://www.cancer.org/Research/CancerFactsFigures/CancerFactsFigures/cancer-facts-figures-2011. Accessed 30 June 2011
Bishop MM, Lee SJ, Beaumont JL, Andrykowski MA, Rizzo JD, Sobocinski KA et al (2010) The preventive health behaviors of long-term survivors of cancer and hematopoietic stem cell transplantation compared with matched controls. Biol Blood Marrow Transplant 16:207–214
Blanchard CM, Courneya KS, Stein K (2008) Cancer survivors’ adherence to lifestyle behavior recommendations and associations with health-related quality of life: results from the American Cancer Society’s SCS-II. J Clin Oncol 26:2198–2204
Centers for Disease Control (CDC) (2009) Cigarette smoking among adults and trends in smoking cessation – United States, 2008. MMWR Morb Mortal Wkly Rep 58:1227–1232
Centers for Disease Control (CDC) (2011) Quitting smoking among adults – United States, 2001–2010. MMWR Morb Mortal Wkly Rep 60:1513–1519
Chang G, Orav EJ, McNamara T, Tong MY, Antin JH (2004a) Depression, cigarette smoking, and hematopoietic stem cell transplantation outcome. Cancer 101:782–789
Chang G, Orav EJ, Tong M-Y, Antin JH (2004b) Predictors of 1-year survival assessed at the time of bone marrow transplantation. Psychosomatics 45:378–385
Chelghoum Y, Danaïla C, Belhabri A, Charrin C, Le QH, Michallet M et al (2002) Influence of cigarette smoking on the presentation and course of acute myeloid leukemia. Ann Oncol 13:1621–1627
Cooke J, Bitterman H (2004) Nicotine and angiogenesis: a new paradigm for tobacco-related diseases. Ann Med 36:33–40
Cooley ME, Emmons KM, Haddad R, Wang Q, Posner M, Bueno R et al (2011) Patient-reported receipt of and interest in smoking-cessation interventions after a diagnosis of cancer. Cancer 117:2961–2969
Coups EJ, Ostroff JS (2005) A population-based estimate of the prevalence of behavioral risk factors among adult cancer survivors and noncancer controls. Prev Med 40:702–711
Doyle C, Kushi LH, Byers T, Courneya KS, Demark-Wahnefried W, Grant B et al (2006) Nutrition and physical activity during and after cancer treatment: an American Cancer Society guide for informed choices. CA Cancer J Clin 56:323–353
Ehlers SL, Gastineau DA, Patten CA, Decker PA, Rausch SM, Cerhan JR et al (2011) The impact of smoking on outcomes among patients undergoing hematopoietic SCT for the treatment of acute leukemia. Bone Marrow Transplant 46:285–290
Fiore MC, Jaen CR, Baker TB, Bailey WC, Benowitz N, Curry SJ et al (2008) Treating tobacco use and dependence. Clinical Practice Guideline, p 257
Geyer SM, Morton LM, Habermann TM, Allmer C, Davis S, Cozen W et al (2010) Smoking, alcohol use, obesity, and overall survival from non-Hodgkin lymphoma. Cancer 116:2993–3000
Gritz ER, Fingeret MC, Vidrine DJ, Lazev AB, Mehta NV, Reece GP (2006) Successes and failures of the teachable moment. Cancer 106:17–27
Gritz ER, Lam CY, Vidrine DJ, Cororve MF (2008) Cancer prevention: tobacco dependence and its treatment. In: DeVita V, Lawrence T, Rosenberg S (eds) Cancer: principles and practice of oncology, 8th edn. Lippincott, Williams, and Wilkins, Philadelphia, pp 593–608
Ho VT, Weller E, Lee SJ, Alyea EP, Antin JH, Soiffer RJ (2001) Prognostic factors for early severe pulmonary complications after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 7:223–229
Hoodin F, Kalbfleisch KR, Thornton J, Ratanatharathorn V (2004) Psychosocial influences on 305 adults’ survival after bone marrow transplantation: depression, smoking, and behavioral self-regulation. J Psychosom Res 57:145–154
Hsu CC-T, Kwan GNC, Chawla A, Mitina N, Christie D (2011) Smoking habits of radiotherapy patients: did the diagnosis of cancer make an impact and is there an opportunity to intervene? J Med Imaging Radiat Oncol 55:526–531
Levitz JS, Bradley TP, Golden AL (2004) Overview of smoking and all cancers. Med Clin North Am 88:1655–1675
Marks DI, Ballen K, Logan BR, Wang Z, Sobocinski KA, Bacigalupo A et al (2009) The effect of smoking on allogeneic transplant outcomes. Biol Blood Marrow Transplant 15:1277–1287
Miceli MH, Dong L, Grazziutti ML, Fassas A, Thertulien R, Van Rhee F et al (2006) Iron overload is a major risk factor for severe infection after autologous stem cell transplantation: a study of 367 myeloma patients. Bone Marrow Transplant 37:857–864
Mokdad AH, Marks JS, Stroup DF, Gerberding JL (2004) Actual causes of death in the United States, 2000. JAMA 291:1238–1245
Sandler DP, Shore DL, Anderson JR, Davey FR, Arthur D, Mayer RJ et al (1993) Cigarette smoking and risk of acute leukemia: associations with morphology and cytogenetic abnormalities in bone marrow. J Natl Cancer Inst 85:1994–2003
Savani BN, Montero A, Wu C, Nlonda N, Read E, Dunbar C et al (2005) Prediction and prevention of transplant-related mortality from pulmonary causes after total body irradiation and allogeneic stem cell transplantation. Biol Blood Marrow Transplant 11:223–230
Sharma S, Nadrous HF, Peters SG, Tefferi A, Litzow MR, Aubry M-C et al (2005) Pulmonary complications in adult blood and marrow transplant recipients. Chest 128:1385–1392
Spear MA, Dupuy DE, Park JJ, Halpern EF, Spiro IJ (1999) Tolerance of autologous and allogeneic bone grafts to therapeutic radiation in humans. Int J Radiat Oncol Biol Phys 45:1275–1280
Steenland K, Hu S, Walker J (2004) All-cause and cause-specific mortality by socioeconomic status among employed persons in 27 US States, 1984–1997. Am J Public Health 94:1037–1042
Thompson AM, Couch M, Zahurak ML, Johnson C, Vogelsang GB (2002) Risk factors for post-stem cell transplant sinusitis. Bone Marrow Transplant 29:257–261
Tichelli A, Passweg J, Wojcik D, Rovo A, Harousseau J-L, Masszi T et al (2008) Late cardiovascular events after allogeneic hematopoietic stem cell transplantation: a retrospective multicenter study of the Late Effects Working Party of the European Group for Blood and Marrow Transplantation. Haematologica 93:1203–1210
Tran BT, Halperin A, Chien JW (2011) Cigarette smoking and outcomes after allogeneic hematopoietic stem cell transplantation. Biol Blood Marrow Transplant 17:1004–1011
U. S. Department of Health and Human Services Office of Surgeon General (2010) How tobacco smoke causes disease: the biology and behavioral basis for smoking-attributable disease. Retreived from http://www.surgeongeneral.gov/library/tobaccosmoke/index.html. Accessed 10 July 2011
Varadarajan R, Cummings M, Hyland A, Wang E, Wetzler M (2010) Can decreasing smoking prevalence reduce leukemia mortality? Ann Hematol 89:873–876
Ward K, Klesges R (2001) A meta-analysis of the effects of cigarette smoking on bone mineral density. Calcif Tissue Int 68:259–270
Wilczynski SW, Erasmus JJ, Petros WP, Vredenburgh JJ, Folz RJ (1998) Delayed pulmonary toxicity syndrome following high-dose chemotherapy and bone marrow transplantation for breast cancer. Am J Respir Crit Care Med 157:565–573
Zhou J, Eksioglu EA, Fortenbery NR, Chen X, Wang H, Epling-Burnette PK et al (2011) Bone marrow mononuclear cells up-regulate toll-like receptor expression and produce inflammatory mediators in response to cigarette smoke extract. PLoS One 6:e21173
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer Science+Business Media Dordrecht
About this chapter
Cite this chapter
Ehlers, S., Bronars, C. (2012). Effect of Smoking on the Outcomes of Cancer Patients After Hematopoietic Stem Cell Transplantation. In: Hayat, M. (eds) Stem Cells and Cancer Stem Cells, Volume 8. Stem Cells and Cancer Stem Cells, vol 8. Springer, Dordrecht. https://doi.org/10.1007/978-94-007-4798-2_32
Download citation
DOI: https://doi.org/10.1007/978-94-007-4798-2_32
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-94-007-4797-5
Online ISBN: 978-94-007-4798-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)