Abstract
Emotional, psychological or environmental stress (e.g., heat or nanoparticles) influences brain function. However, the detailed mechanisms of stress induced brain dysfunction are not well known. Research carried out in our laboratory since last 20 years show that various kinds of stressors depending on their magnitude and durations alter the blood-brain barrier (BBB) permeability to proteins leading to brain pathology. These stressed animals also show marked behavioral and cognitive deficits at the time of the BBB leakage. Entry of several restricted elements from the blood to the brain compartment after breakdown of the BBB results in immunological, biochemical and pathological reaction causing brain edema formation and cell injury. Blockade of several neurochemical receptors, e.g., serotonin, prostaglandin or opioids as well as neutralization of key neurodestructive elements, i.e., neuronal nitric oxide synthase (nNOS), Tumor necrosis factor-alpha (TNF-α), dynorphin A or hemeoxygenase-2 (HO-2) using specific drugs or antibodies against these factors reduces BBB disturbances, cognitive and behavioral dysfunction, and brain pathology. Based on these new evidences, it appears that the BBB is the gateway to neuropsychiatric diseases. Thus, efforts should be made to maintain a healthy BBB in various brain diseases to achieve neuroprotection. The possible mechanisns of BBB breakdown and brain pathology in stress in relation to altered cognitive and sensory-motor functions is discussed in this review.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Blood-brain barrier
- Stress
- Brain pathology
- Serotonin
- Prostaglandin
- Cytokines
- Cognitive dysfunction
- Sensory motor abnormalities
- Brain edema
- Neuropsychiatry diseases
1 Introduction
Blood-brain barrier (BBB) was first recognized by Paul Ehrlich in Germany about 125 years ago [1]. However, its role in various neurological and psychiatric diseases is still not well known. About 30 years ago, our laboratory was the first to demonstrate that the BBB is compromised to protein tracers under different stressful situations [2–4]. This opening of the BBB under stressful situations is somehow related with neurochemical metabolism and appears to be mediated via specific neurotransmitter receptors for serotonin [5, 6], prostaglandin [7], histamine [8, 9] and opioids [4, 10–14].
However, our knowledge regarding the functional significance of BBB breakdown in stressful situations is still unclear (see [13]). Thus, we still do not know how this information is useful in interpreting neurological or neurodegenerative diseases? Whether the BBB breakdown is crucial for cognitive or sensory-motor impairment? Is brain pathology always associated with BBB breakdown? Or, increased BBB permeability in disease situations reflects some kind of compensatory mechanisms? This review is focused on these pertinent questions that are largely based on our own investigations and in the light of the recently available new data in the field. In addition, the new results obtained in other stressful situations caused by psychostimulants or nanoparticles on BBB functions are also discussed. Furthermore, the functional significance of BBB breakdown in relation to brain pathologies and its modulation by various neuroprotective agents to enhance neurorepair are presented.
2 Blood-Brain Barrier: A Dynamic Anatomical Barrier
BBB is a physiologically dynamic barrier whose permeability properties are very similar to that of an extended plasma membrane [4, 14, 15]. Anatomically, the BBB mainly resides within the endothelial cells of the cerebral microvessels, which are connected with tight junctions [16], a feature that is not found in non-cerebral capillaries (Fig. 9.1). The other important feature of cerebral capillaries includes a very low level or almost absence of vesicular transport, a phenomena that is very common in other vascular beds [4, 11, 17]. Furthermore, endothelial cells of the cerebral capillaries are almost covered with glial end-feet that encircle the microvessels (about 85–90%) at the one end and the other end is connected to the nerve cells or to the dendrites [18]. It is still uncertain whether glial end-feet contribute to the BBB phenomena; however, it has been established that their presence is needed to induce BBB properties within the endothelial cells during development [15, 19]. The basal lamina, which is also known as basement membrane, is quite thick in cerebral microvessels; however, its role in BBB function is still not well known. Available evidences mainly points out that the basal lamina, per se, has no role in restricting tracer transport from vascular compartment to the neural compartment when the endothelial cell barrier is compromised (see [11, 12]).
Anatomical site of the blood-brain barrier (BBB). Schematic drawing of the ultratstructural aspects of one brain capillary (a) and one general capillary (b). The endothelial cells (EC) of cerebral capillaries are connected with tight junctions and normally do not contain microvesicles for vesicular transport as compared to the non cerebral capillary. The endothelial cells of the cerebral capillaries are also covered with a thick layer of basement membrane (BM) compared to the general capillary. Modified after [11–14]
2.1 BBB: A Physiological Regulatory Barrier
The BBB strictly regulates the composition of the extracellular fluid microenvironment of the brain in which neurons bath. Thus, the BBB works as exchange medium for essential nutrients from blood to brain as well as excretory medium for metabolic products from brain to blood [12, 13]. Many substances are transported actively from blood to brain via active transport (Fig. 9.2). Recently, presence of several transporter genes has been found for many essential substrates or neurochemicals [13–15]. Among which glucose transporter, 5-HT transporters are widely examined. Although, the role of transporters are still not clear, there are evidences that these transporters alter in several neurological diseases, indicating that altered transport properties of the BBB either reflect disease processes or in disease conditions, abnormalities in the BBB transport occurs [4, 9, 12, 13–15].
Blood-brain barrier (BBB) is a physiological dynamic barrier. The BBB effectively regulates exchange of substances between brain fluid microenvironment and the vascular system. Thus, nutrients and waste products are easily exchanged between the neuronal and microvascular endothelial cell membrane interface through the extracellular space. Modified after [12]
2.2 BBB: A Chemical Barrier System
The endothelial cells of the cerebral microvessels possess several enzymes, which are capable to degrade various neurotransmitters while their passage from blood to brain [12–15] (Table 9.1). Thus many neurotransmitters substances, that as such cannot pass the endothelial cell barrier are eliminated due to degradation within the endothelial cells [12, 15, 21]. On the other hand, precursor of most of the neurotransmitters gain easy access within the brain compared to their prototypes. Blockade of endothelia cell enzymes using pharmacological agent is thus one suitable approach to increase the concentration of the neurotransmitters, if needed. This aspect is used to enhance the penetration of L-DOPA in the brain after inhibiting the carbonic anhydrase enzyme using methyl-DOPA [12–15, 20, 21].
Apart from neurotransmitter metabolizing enzymes, several other enzymes are found in the cerebral endothelial cells whose functional significance is yet to be established [12, 13, 20]. Thus recently described nitric oxide synthase enzyme responsible for generation of nitric oxide is present in cerebral endothelial cells (see [22, 23]). Likewise, hemeoxygenase enzyme, responsible for carbon monoxide production in vivo is also found to be present in endothelial cells [21, 24]. These observations suggest an active role of endothelial cells in maintaining the fluid microenvironment of the brain in a very strict fashion.
3 The Brain-Blood Barrier (bbb)
Very little is known about the barrier between brain and blood [12, 20, 24, 26]. It is believed, that brain-blood barrier (bbb) is also very tight as blood-brain barrier [27, 28] (Fig. 9.3). The assumption for this comes from the idea that in brain several neurotransmitters are released due to altered demand or stimulation of particular pathways and/or due to altered chemical sensation in different neuronal pathways responsible for pain or stress [21, 22, 25, 26]. In such circumstances, the brain could produce large quantity of neurochemicals that are released in the brain or in spinal cord for functional purposes. In most of the cases, the release of neurochemicals will be prolonged and reabsorption will occur very slowly. If these neurochemicals can gain access into the systemic circulation due to a defect in the brain-blood barrier, then rebound phenomena may amplify the effects of these vasoactive neurochemicals by many folds into the brain [12, 24–28]. However, in normal circumstances this does not occur and the peripheral circulation is kept largely aloof from changes in the neurochemical transmission in the brain and vice versa (see [23–28]). The main reason behind these regulatory phenomena is a strong brain-blood barrier function.
The brain-blood barrier (bbb) is equally effective as the Blood-Brain Barrier (BBB). A. Schematic diagram showing bbb (B) and BBB (A). The endothelial cells (E) in the brain microvessels are connected with tight junction and are surrounded by a thick basement membrane. The glial cells (G) and nerve cells (N) around the cerebral endothelial cell are clearly seen. Intravascular tracer is normally stopped at the tight junction and donot penetrate the luminal endothelial cell membrane to reach extracellular space indicating a very tight BBB (A). Likewise, intrathecal tracer does not normally pass the abluminal endothelial cell membrane and/or the tight junctions to reach the vascular compartment (B) suggesting that the bbb like the BBB also effectively regulates exchange of substances between brain microenvironment and the vascular system (B). It is still not known whether BBB leakage is also accompanied with bbb disruption in stress or in brain diseases. Modified after [11–14]
However, there are reasons to believe that under stressful conditions or following brain diseases the brain-blood barrier (bbb) is also altered [12, 27, 28]. Although, information about breakdown of the bbb in disease conditions are still lacking, it remains to be seen whether drugs influencing various neurochemical receptors could also modified the bbb [28].
4 BBB and Brain Pathology
An increased permeability of the BBB is quite common in almost all the diseases afflicting the brain or spinal cord in which marked alterations in the neural, glial and endothelial cells are seen (see [11–13, 20]). This suggests BBB dysfunction is crucial for brain diseases. However, the functional significance of BBB opening in these pathological conditions is still not well understood. Thus, it is not yet clear whether increased BBB permeability is the result of the pathological alterations in the brain or a breakdown of the BBB permeability has resulted in all the pathological changes seen under these clinical and experimental brain disease situations.
4.1 BBB “Opening”, “Leakage”, “Dysfunction”, “Breakdown” or “Increased Permeability”?
The BBB opening or breakdown under brain disease conditions is quite common- [12–15, 21]. In the literature, the term “opening”, “leakage” and “breakdown” are used most often interchangeably. However, some caution must be made while using these terms. The opening of the BBB can be a physiological demand for increased transfer of some molecules across the cerebral endothelium. It seems reasonable to assume that this opening is most likely a temporary one. Thus, the term “breakdown” should be reserved for long-term opening associated with often-irreversible phenomena, which cannot be controlled any longer [12–16]. However, in the literature, these terms are often used interchangeably in almost all experimental or disease states. Moreover, in a clinical situation, it is hard to find whether the “leakage” of the BBB is reversible or irreversible [20]. Thus, both terms are misleading. Further understanding on the mechanisms of BBB permeability will probably determine the real nature of the leakage that can fall in the category of BBB breakdown or opening [11–13]. In this review, both terms are used to identify leakage of tracers across the BBB as opening and breakdown. However, the term “breakdown” is used quite sparingly in this review to denote pathology of the endothelial cells as we believe that “dysfunction”, “leakage” or “increased permeability” of the BBB is more appropriate to describe acute disturbances in the BBB function that can be restored or repaired eventually over time or by drugs [11–13, 21].
5 BBB in Hypertension
One of the earliest literature describing a comprise of the BBB in clinical condition is hypertension [14, 15, 29]. This subject is mainly developed by the pioneer works or Johansson from Sweden [30–33]. Her results clearly show that hypertension associated with chemical means, or by clipping of renal arteries are associated with focal leakage of protein tracers in the brain [34]. These early findings show that cerebrovascular diseases associated with hypertension, or encephalopathy following long-term hypertensive crisis are somehow associated with the damage of the BBB [30–34]. Later works from her group clearly show that hypertensive opening of the BBB plays major role in brain dysfunction leading to long-term consequences and brain pathology (see [34]).
Using hypertension as a model, it was seen further that it is the magnitude and degree of abrupt hypertensive insult to the cerebral vessels that will produce a mechanical disruption of the BBB, probably by increasing intramural pressure of the vascular wall [12–15, 30–34]. Under such circumstances, mechanical widening of the tight junctions is possible [14, 15]. These works are further supported from the laboratory of several workers (see [12–15]). It was found that a slow development of hypertension is not associated with the breakdown of the BBB function [11–16, 20–25, 30–34]. This was evident from the fact that cerebral vessels have the capacity to autoregulate and thus could sustain any increase in the intramural pressure if applied within 90–120 sec [14, 15]. However, if an abrupt increase in the transmural pressure occurs within 90 sec, the BBB disruption occurs [14, 30–33]. However, increase in arterial pressure beyond that time limit will allow the cerebral microvessels to resist the hypertension induced BBB leakage [14, 15, 30–33].
5.1 Widening of the Tight Junctions Vs. Increased Vesicular Transport
The probable mechanisms of increased BBB permeability under hypertension are still controversial. Previously, it was believed that widening of the tight junctions could be largely responsible for BBB disruption in hypertension [14, 15]. However, further research revealed that apart from a widening of the tight junctions in hypertension there also occurs an increase in vesicular transport [30–33]. Although, the magnitude of tracer transport by vesicular transport across the BBB in hypertension is still controversial [11–13]. This aspect was addressed in details by researchers from Lund, Sweden. Thus, Larsson and his co-workers for the first time administered Vinca alkaloids [4–8, 23, 29, 33, 35, 36], Vincristine as a pretreatment before chemical induced hypertension in rats [35, 36]. Their results demonstrated that vincristine pretreatment, which is mainly an inhibitor of vesicular transport, attenuated the tracer transport across the BBB [36]. Since the BBB opening was not prevented, these authors concluded that vesicular transport plays major role in arterial hypertension induced breakdown of the BBB permeability [35, 36].
Additional studies to demonstrate tracer transport using lanthanum across the cerebral microvessels in hypertension were carried out by Nag et al. [37–42]. The studies of Nag and her co-workers demonstrated that exudation of the electron dense tracer takes place in different regions of the brain across the microvessels following hypertensive insults to the brain [40–42]. Thus, the lanthanum was found within the endothelial cell cytoplasm as well as in the vesicular profiles of large vessels. The lanthanum was also seen within the tight junctions demonstrating that, the ion can pass the junctional barrier probably due to widening of the gaps between the endothelial tight junctions [40–42].
Apart from simple widening of the tight junction, it appears that several other factors are also operating in hypertension induced increased BBB permeability. This is evident with the fact that pretreatment with hydrocortisone attenuated the BBB permeability in hypertension without reducing the intensity of arterial pressure increase [14, 15, 30–34, 37–42]. Thus, pressure induced triggering of secondary injury mechanisms seems to play important role. However, this is a new subject in hypertension and requires further study.
6 BBB in Disease Conditions
The BBB permeability is compromised in almost all neurological and psychiatric diseases as mentioned above [4, 11–15, 20–23] (Table 9.2). It may be that leakage of BBB to endogenous serum proteins in neurological diseases could lead to abnormal mental functions precipitating neuropsychiatric diseases [11–15, 20, 21]. This idea is supported by the fact that extravasation of serum proteins can be found in the brain extracellular space and in some cases in the intracellular space in several psychiatric diseases [12, 14, 15, 21, 29]. The CSF protein concentration also increased markedly in these psychiatric diseases, as normal protein concentration in the CSF is almost negligible [14, 21, 43–45]. These observations clearly indicate that the permeability properties of the BBB are different in neurological disease conditions. Recent research show that breakdown of the BBB also occurs in Alzheimer’s diseases [21], Parkinson’s disease as well as in Huntingdon’s Chorea [12, 13–15]. The other psychiatric diseases, which reflect an increased BBB permeability to wide variety of tracers, include dementia, autism and depression [21, 29]. Although, demonstration of increased BBB permeability or disturbed barrier function is known in such neurological or psychiatric diseases several decades ago, the function significance of such findings are still obscure.
Pathological studies and case reports from such diseases suggest that in wide variety of neurological and psychiatric diseases, marked pathological alteration in the nerve cells, glial cells and axons are found [14, 15, 29]. Probably an increased BBB permeability to several tracers ranging from 9 to 80 Å wide may results in contamination of the CNS structures with peripheral agents [43–45]. These phenomena seem to be one of the major factors in inducing abnormal cell reaction in the CNS leading to brain pathology. It is likely that the day to day stressful situations affecting mental function for long time may also induce BBB disturbances and could be instrumental in precipitating brain pathology leading to neurodegenerative diseases [2, 6–9, 11–15]. In addition, peripheral alterations in neurochemical metabolites or their receptor activation or down regulation could also influence the BBB function [21, 29]. However, further studies regarding role of cellular and molecular stress on the BBB function are needed to clarify these points.
Since, the areas of abnormal brain function in relation to BBB damage are still not well investigated in details, new insight and novel impetus are needed to expand our knowledge in this field of research.
7 Neurobiology of Stress
The term “Stress” denotes any external or internal stimuli that could perturb the physiological and/or psychological homeostasis of the organisms [11–13, 24–27, 46–49]. Thus, stress-related disorders include anxiety to post-traumatic experiences [50, 51] all could impair the cognitive functions [52, 53]. However, so, far it is unclear whether alterations in the cognitive functions in stress are related to the stress-induced BBB dysfunction [11–13, 20, 21, 25–27].
Stress could activate or inhibit a select group of neurons or influence the functioning of selective organs, e.g., hippocampus within the brain [5–7, 11–13, 54]. Since stress is able to release several hormones and neurotransmitters that could impair the neuronal activity [4–13, 55, 56] there are reasons to believe that long-term exposure to stress will induce CNS disorders [50].
Thus, prolonged excitation/inhibition of nerve cells leads to brain dysfunction and results in brain pathology and/or neurodegeneration [7–12, 54, 55]. This idea is supported by the fact that abnormal regulation of stress response culminates in chronic systemic diseases including hypertension and several affective disorders, e.g., depression, post-traumatic stress symptoms and Alzheimer’s disease [57–61].
7.1 Information-Processing System and Brain Dysfunction in Stress
Nerve cells are equipped with a stimulus-response information processing system (IPS) [2–13, 20–27] (Fig. 9.4). Depending on the magnitude and severity of the stress response, the nerve cells may induce short- or long-lasting changes in its phenotype [11–13]. The early stress responses lasting from milliseconds to minutes are normally induced by various neurotransmitters and growth factors (the first messengers) acting on the cell surface receptors to activate the second messenger systems [212, 25–27]. The second messenger systems then by acting through specific protein kinases leads to phosphorylation of specific neuronal proteins resulting in alteration of the structure and function of the nerve cells [62–64].
Influence of stress on BBB dysfunction. (a) Stress depending on its magnitude and severity can induce CNS dysfunction. The information processing system (IPS) of the CNS can handle certain level of stress without showing symptoms (optimal information). Inadequate handling of stress due to information overload (psychological, environmental, physical exercise or hyperactivity, etc.) may impair IPS and the BBB permeability. Likewise, stressors causing an information underload (hypoactivity, peripheral nerve transection, suturing of one eye-lid, etc.) will also perturb IPS and the BBB function. (b) Three stages of stress response. Effects of stress on the organisms can be divided into 3 stages. The initial reaction of an information overload induces alarm reaction showing profound symptoms. When the stress is further continued with same intensity, the symptoms disappear after some time leading to stage of adaptation. Further continuation of stress may finally lead to stage of exhaustion in which the symptoms of alarm reaction may re-appear and results in death of the organism. (c) Stages of stress response in clinical situations. Mild stress induces short-term alterations in the arousal and emotional response that can affect learning and memory processes. When the magnitude, severity and/or duration of stress increases, several transient and/or permanent changes (synaptic plasticity, changes in neuronal structure and circuitry as well as neurotoxicity) will occur in the CNS. BBB dysfunction can be seen after moderate level of stress overload and may be crucial for short-term or permanent structural changes in the CNS. Modified after [11–14]. For details see [12]
It appears that disruption of the BBB is one of the most important factors in stress-induced alterations in the IPS leading to subsequent brain dysfunctions [4–13] (Fig. 9.4). This idea is well supported by the fact that an overload on the IPS caused by foot-electroshock, electrical or chemical induced seizures or training in water maze results in BBB leakage in selective parts of the brain within a very short exposure periods [4, 11–13, 14, 15]. Likewise, an underload on the IPS caused by restriction of movement, e.g., restraint or immobilization, peripheral nerve lesion or denucleation of one eye could also results in BBB disruption after considerably long periods of time [4, 11–13, 15, 29]. Similarly, degeneration of noradrenergic neurons (information underload), or stimulation of locus coeruleus (information overload) also results with an increased permeability of water into the brain [12, 13, 21, 27]. Taken together, these observations suggest that stress-induced alterations in the IPS may results in brain dysfunction that is probably mediated through the BBB disruption.
7.2 Three Stages of Stress Response in the CNS
The effect of “acute” stress on the organism is often entirely different and sometimes results in opposite symptoms following “chronic” exposure of the same stressor [50]. This led Selye to categorize the whole stress response into three stages (Fig. 9.4) [12, 25, 26, 50]. Some effects like adrenal enlargement, gastrointestinal ulcers and thymicolymphatic involution invariably occur in response to any stressor and classified as “general adaptation syndrome (GAS)” (see [2, 4, 50]).
Thus, the initial stress response that results in immediate reaction within the organisms is characterized as (i) Alarm reaction. When stress is continued further to such an extent that these alarm reactions are disappeared and it seems that organism is not showing any apparent reactions to the continued stress, the stage of (ii) Adaptation ensues. However, continuation of stress further may result in precipitation of alarm reaction type symptoms again after certain period of time and denotes the (iii) Exhaustion stage of the organism precipitated by causing death [46, 50] (Fig. 9.4). The duration and appearance of these stages of stress-responses in the organism mainly depend on the magnitude and intensity of the primary stimulus and environmental (external) and genetic or metabolic (internal) factors of the organisms [11–15].
Experiments carried out in our laboratory suggest that these three stages of stress-responses are also applicable on stress-induced brain dysfunction [2–13, 20–28]. This is evident from the fact that the intensity and duration of stress closely corresponds to the magnitude and severity of the BBB leakage and brain pathology [2–13, 11–15, 20–28, 65] (Fig. 9.4). Thus, it appears that major brain diseases, e.g., Alzheimer Diseases, depression, psychosis, and other neuropsychiatric illnesses may represent life time stress exposure resulting in sever brain dysfunction over time [46, 50, 56, 65].
7.3 “Specific” Vs. “Non-specific” Effects of Stress on the CNS
Although, stress is part of our daily life that includes numerous dissimilar events like fear, frustration, sorrow, joy, fatigue, pain, mental or physical efforts and related events [46, 50] the body responds to all these diverse stressors in almost identical manner [2, 4, 11–13, 25–27]. Thus, the effects of pleasant (eustress) or unpleasant (distress) stressors on the body function are mainly identical in nature [50]. According to Selye [46, 50] there cannot be different types of stress. Thus, the terms “emotional stress”, “heat stress”; “cold stress”, “swimming stress”, “immobilization stress”, “surgical stress”, “sleep deprivation stress” and other kind of stimuli denote the stress produced by these stressors [21, 27, 46, 50, 65].
The effect of stress on the organism largely depends on the (i) non-specific effects, as well as (ii) the specific effects of these stressors [11–13, 25–27, 46, 50, 65]. In addition, the stress-induced effects are finally influenced by several conditioning factors such as age, sex, genetic predisposition (endogenous factors) or diet, drugs, environment or hormones (exogenous factors) [13, 27, 46, 50]. Under the influence of these external or internal factors, any stressor or adverse conditions can induce pathogenesis and produce disease of adaptation that affects the specific parts of the body according to sensitivity of the specific stressors or to the above conditioning factors [2–13, 25–27, 50]. Molecular mapping of genes and proteins that are activated by stress in different regions of the CNS are in good agreement with this hypothesis [12]. Our investigation suggests that a selective and specific opening of the BBB under different kinds of stress stimuli could also denotes the specificity of each stressors at the level of CNS response, a feature not described before.
7.4 Improper Handling of Stress Leads to “CNS Diseases”
It is widely believed that improper handling of stress by the organisms could lead to CSN diseases [11–13, 25–27, 46, 50]. Thus, any stressor on the organism will first induce a non-specific response (the first mediator): either a nervous stimuli from the cerebral cortex, reticular formation or limbic system particularly the hippocampus and amygdala; or a chemical substance, the exact nature of which has not established yet [46, 50]. The incoming nervous stimuli act on neuroendocrine cells in the median eminence (transducer) where these signals are transformed into a humoral messenger “corticotropin releasing factor (CRF)” that causes discharge of adrenocorticotropic hormone (ACTH) from the adenohypophysis into general circulation [46, 50]. The ACTH then acts on the adrenal cortex to release glucocorticoids that provide energy to cope with the increased necessary demands of the organism resulted in response to the stressor [4–13, 22–27, 29, 46, 50]. This release of ACTH from the pituitary is controlled by the level of excess ACTH in the blood (ACTH short-loop feed back mechanism), as well as the high level of the corticoid levels (corticoid long-loop feedback mechanism) [4, 11–13, 23–27].
In addition, the stress response is mediated by the catecholamines released from the autonomic nerve endings (noradrenaline) under the influence of acetylcholine, and from the adrenal medulla (mainly adrenaline) [4, 50]. Infusion of noradrenaline and adrenaline in the similar amount released in stress induces a short-term disruption of the BBB function [4, 11, 13, 66]. This indicates that stress-induced release of neurochemicals is capable to influence CNS microenvironment.
Taken together, it is obvious that insufficient, excessive or faulty response of the organism to the stressors either in terms of inappropriate nervous or hormonal responses could leads to “stress diseases” including the CNS disorders [11–13, 22–27, 46, 50].
7.5 Stress Pathways in the CNS
Hypothalamus, prefrontal cortex, cingulate cortex, hippocampus, amygdala and the bed nucleus of the stria terminalis are the most sensitive structures that are affected by stress [11–13, 61]. In addition, brain stem could also influences stress-induced activation of the hypothalamic-pituitary-adrenal (HPA) axis and the limbic system through the ascending serotonergic and noradrenergic nerve fibers emanating from the raphé nucleus and locus coeruleus, respectively (Fig. 9.5 ) [61, 66–69].
Stress can influence information processing system (IPS) of the CNS. Sensory information is relayed to the hypothalamus through spinal cord. Hypothalamic information is further transmitted to the limbic and thalamocortical systems and hypophysis. Alterations in internal milieu and feedback from the thalamocortical and limbic systems to hypothalamus are the integral part of the CNS to maintain homeostasis. However, an overload or dysfunction of this feedback may lead to alterations in the brain fluid microenvironment and BBB permeability. Modified after [12]
Stress caused by several neuropsychiatric diseases, psychostimulants, substance abuse and other neurovascular anomalies results in very selective and specific hippocampal damage resulting in profound memory impairment [23–28]. Stress induced specific cell damages in the hippocampus are seen in the CA 3 and CA4 subfields along with atrophy of dendrites particularly in the CA3 area [11–13, 23–27, 54, 70–74]. Animal experiments show that repeated stress induces reversible synaptogenesis in the CA1 region [75] besides the atrophy of dendrites in the CA3 subfield [76] (for details see [12]). These observations suggest that stress could activate selective and specific pathways in the brain leading to selective brain damage.
7.6 Beneficial Vs. Harmful Effects of Stress
Whether stress is beneficial or harmful to the organisms with special references to the CNS structure and function is still unclear. Available evidences suggest that mild to moderate stress could results in enhancement of adaptive response whereas, excessive stress for sufficient duration leads to brain damage [11–13, 54]. Administration of corticosterone in doses simulating the stress conditions induces loss of nerve cells in the pyramidal cell layer in the CA3 subfield of the rat hippocampus [11, 54]. Glucocorticoid administration normally does not affect nerve cells in the dentate gyrus and in CA1 sector of the hippocampus [77, 78]. On the other hand, stress downregulates the expression or function of neurotrophic factors that may induce slowly developing neurodegeneration.
The neurotrophic factors are intracellular messengers capable to induce gene expression in the target neurons [79]. An increase in the BDNF mRNA in the hippocampus and in cortex is seen following seizures, ischemia and hypoglycemia [80]. This indicates that mild stress could be beneficial for the CNS function [11–13, 81].
On the other hand, 2 h immobilization decreased the BDNF mRNA in the hippocampus of adult rats [15, 82] that is most pronounced in the dentate gyrus followed by CA3 and CA1 hippocampal pyramidal neurons [11–13, 22–26, 82]. A reduction in BDNF expression in hippocampus is also seen 24 h after maternal separation in the rats on the postnatal day 12–20 (see [81]). This stress-induced reduction in the BDNF expression leads to atrophy but is not sufficient to induce cell death [83]. Thus, stress-induced downregulation of BDNF expression will have profound consequences on neuronal communication and the signal transduction mechanisms in the brain [11–13, 20–28].
Long-term treatment with antidepressants or electroconvulsive seizures prevents the stress-induced decrease in the BDNF expression [84]. Interestingly, an increased expression of BDNF mRNA following stress is also seen in the pituitary and in the hypothalamus [85]. The BDNF is often co-localized with corticotropin-releasing factor (CRF) in the hypothalamus and thyrotropin-releasing hormones (TRH) in the paraventricular nucleus (PVN) neurons [81–84]. An increase in BDNF expression could be seen in the PVN following adrenalectomy or thyroidectomy [11–13]. This suggests that neurotrophic factors could exert trophic effects on the pituitary to regulate the local peptide or hormone secretion into the general circulation [81]. This indicates that stress effects on the brain functions are still unclear and requires further investigations.
7.6.1 Stress Releases Neurosteroids: An Antistress Hormone
Although, elevated levels of stress and corticosterone impair memory function in several animal models [11–13, 86–88], highly arousing but sub-threshold levels of stress could enhance memory functions as well [89]. This effect of stress is mediated through a new category of steroids termed, as “neurosteroids” [13, 87]. The neurosteroids are produced endogenously in the periphery as well as in the brain. One type of neurosteroids, dehydroepiandrosterone sulfate (DHEAS) is the most abundant adrenal neurosteroids in humans [90]. The DHEAS antagonizes the functions of corticosterone and thus is often known as an antiglucocorticoid hormone [90]. The DHEAS enhances hippocampal-dependent learning in rats [91] and enhance electrophysiological and cognitive measures of hippocampal function [92]. The complex effects of stress on brain function or behavioural alterations are mainly due to a competitive interaction between corticosterone and DHEAS [87, 88, 91, 92]. These observations suggest that endogenous neurosteroids could act as an antistress hormone and may possibly protect brain dysfunction in stress up to certain extent.
7.6.2 Stress Enhances Virus Penetration into the Brain
A variety of stressors exacerbate the effects of several viruses, e.g., herpes simplex [93], influenza [94, 95]; and encephalitic viruses [96, 97] leading to significantly higher increase in the morbidity and mortality [98–102].
Thus, inoculation with attenuated variant of West-Nile virus (WN-25) or neuroadapted noninvasive Sindbis strain (SVN) to mice subjected to stressors like cold, isolation or administration of corticosterone enhanced their mortality by 50–80% as compared to the non-stressed animals [9]). This effect was most pronounced during isolation stress (mortality 80%) followed by cold (about 60%) and corticosterone administration (50%). Moreover, these stressors resulted in fatal encephalitis when avirulent strain of Semliki Forest virus (SFV-A7) was administered as compared to no death seen in normal mice. Laboratory investigations showed that the brain titters of viruses in the stressed mice are 3- to 4-fold higher in comparison to the normal unstressed group [11–13, 96, 97]. This suggests that stress is able to enhance brain penetration of viruses causing lethality.
It is believed that stress-induced immunosupression could enhance the proliferation of the viruses into the CNS leading to exacerbation of the infection and pathogenesis [11–13, 20–27, 96, 97]. However, an increased permeability of the BBB following stress could be another factor in exacerbation of viruses-induced mortality.
8 BBB in Stressful Situation
Although, stress is known to influence brain function, alterations in the BBB permeability following stressful situation is still not well characterized. About 41 years ago, Angel [103] demonstrated an increased uptake of 14C-cocaine in the brain following starvation, training in the water maze or adrenalectomy. This was the first report suggesting that mental abnormalities will result following long-term stressful situation probably due to an increase in BBB permeability. However, the molecular mechanisms of BBB opening following stressful situations were not examined in this investigation.
Since adrenalectomy will induce disturbances in endocrine system, it was speculated that neuroendocrine imbalance seems to be the endogenous factor responsible for BBB dysfunction.
Taking clue from these observations, our laboratory has initiated a series of experiments to study the effects of different stressors on the BBB function [2–9]. Thus, we developed different models of stressors that are known to represent emotional disturbances akin to depression and helplessness [2–13, 20–28, 104]. In addition, we also evaluated effects of unpleasant environmental situations, e.g., heat stress [2–13] and/or effects of microfine particles in the ambient environments, i.e., nanoparticles exposure [13, 27, 105, 106] on the BBB function in relation to brain pathology [107–110]. Results from our laboratory revealed that stress of immobilization, swimming, environmental heat stress or exposure to nanoparticles resulted in an increase in the permeability of the BBB to several protein tracers and induced brain pathology [2–13, 20–27, 107, 111]. Our observations further show that these stressors also alter cognitive and sensory motor functions at the time of the BBB disruption [13, 105–111]. A brief summary of our investigations in the past together with recent observations on stress and brain pathology and their pharmacological manipulations for neuroprotection is summarized below.
9 Our Observations on BBB Dysfunction and Brain Pathology in Stress
Studies carried out in our laboratory since last 30 years revealed that several stressful situations are able to disrupt the BBB function [3–13, 112], a feature that was confirmed now by several independent studies [2–13, 20–27, 104–112]. This BBB dysfunction in stress is dependent on the magnitude and intensity of stressors and is primarily responsible for brain pathology. Thus, breakdown of the BBB in stress may be regarded as “a gateway” to neurological diseases and neurodegeneration. This aspect is critically evaluated below based on our own investigations.
9.1 Animal Models of Depression and the BBB Dysfunction
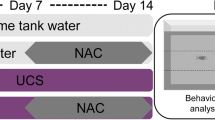
Animal models of depression are induced by hypoactivity that is also used as models for post-traumatic disorders [113–115]. Since immobilization and swim stressors are well known animal models for immobility [116, 117], we employed these animal models of stress to understand the state of BBB function of depression and post-traumatic stress disorders [118, 119].
9.1.1 BBB in Immobilization Stress
Different animal models of immobilization stress show disruption of the BBB function to various tracers at different time points [4, 6, 7, 112, 120–123]. Thus, mild changes in the BBB function in few brain regions were observed after 5 to 15 min of immobilization [124, 125]. Whereas, 2 and 6 h immobilization results in an increase tracer transport into several brain regions [120, 121]. Our observations show that long-term immobilization stress (7–9 h) is needed to induce leakage of protein tracers across the BBB in many brain regions [4, 6, 7]. These observations suggest that the magnitude and intensity of the BBB breakdown depend on the severity of immobilization stress.
Visual inspection of Evans blue dye in the brain of immobilized rats revealed Evans blue dye extravasation in the cingulate, occipital, parietal and frontal cortex. The cerebellum was also stained (Fig. 9.6). The choroid plexus and other non-barrier regions took deep blue stain. A mild to moderate blue staining is seen in the walls of lateral and in the 4th cerebral ventricles indicating disruption of the blood-CSF barrier by immobilization. The dorsal surface of the hippocampus and caudate nucleus stained mildly. The massa intermedia, hypothalamus and regions surrounding third ventricle showed mild to moderate blue staining (Fig. 9.6). Coronal section of the brain passing through basal ganglia, hippocampus, brain stem and cerebellum showed mild to moderate staining of the deeper tissues across the dorsal, lateral and ventral surfaces of the brain (Figs. 9.6 and 9.8). These observations suggest that immobilization induces selective disruption of the BBB.
Stress induced leakage of Evans blue albumin indicates disruption of the BBB. Diagrammatic representation of Evans blue albumin (EBA) extravasation in the brain following 4 h heat stress (HS, A), 30 min forced swimming (FS, B) and 8 h immobilization (IMZ, C) stress. The mapping of EBA extravasation in the brain is based on 6 to 8 individual experiments in each category. Heat stress appears to induce most extensive EBA extravasation in the dorsal (A.a) and ventral (A.b) surfaces of the brain. In forced swimming (FS) the most prominent extravasation of EBA is seen in the cerebellum (FS, B.a). Immobilization stress (IMZ) induces most frequent EBA staining in the anterior and posterior cingulate cortices (C.a). EBA staining on the ventral surfaces of the brain also varied according to the stressors used. However, the piriform cortex and pons regions always exhibited EBA staining in stress. (D) Diagrammatic representation of mid-sagittal section of the rat brain showing extravasation of Evans blue albumin (EBA) following heat stress (HS, a), forced swimming (FS, b), immobilization (IMZ, c) and sleep deprivation (SD, d). Differences in the pattern of EBA extravasation are prominent in the cingulate cortex, cerebellum, thalamus and in the brain stem. Staining of cerebroventricular walls of the lateral ventricles, 4th ventricle and median eminence is a frequent finding in all stress experiments. Bar = 5 mm. Modified after [12, 13]
Quantitative studies using measurement of Evans blue leakage and radioiodine ([131] Iodine) extravasation showed profound BBB disruption (EBA, +670%; radioiodine tracers +1061%) in the whole brain [2, 4–6]. Whereas, only a slight increase in BBB permeability to Evans blue (135%) and radioiodine (100%) is seen at 4 h immobilization [6, 7]. The permeability changes at 1 h stress are negligible (Fig. 9.7). Since every brain regions are different with regard to stress pathways, we examined the regional BBB dysfunction in 12 brain areas after 8 h immobilization stress using radioiodine tracer [4, 6, 7, 12]. The most marked increase in radioiodine was seen in the occipital cortex (1018%) followed by parietal cortex (622%), hippocampus (563%), inferior colliculi (268%), cerebellum (255%), superior colliculus (225%), hypothalamus (102%), thalamus (94%), caudate nucleus (85%), cingulate cortex (61%), temporal cortex (55.5%) and frontal cortex (25%). The pons and medulla did not show extravasation of radioiodine [3, 6]. The regional extravasation of radiotracer at 4 h immobilization is not significant in any region. At 1 h immobilization stress, a mild extravasation of radiotracer (14–33%) is seen in the mid-brain regions including cerebellum [12, 25, 26]. These observations suggest that immobilization stress increases the permeability of the BBB in selective and specific brain areas.
Regional BBB permeability changes in Stress. Left Panel: Changes in regional blood-brain barrier (rBBB) permeability following heat stress (A), forced swimming (B) and immobilization stress (C). The rBBB permeability showed significant increase to radiotracer in the all 14 brain regions after 4 h heat stress (A), only in 9 brain regions (b, c, e–i, k, l) following 30 min forced swimming (B), and in 12 brain regions (a–j) at 8 h immobilization stress (C). Brain regions (A, C) : a = frontal cortex, b = parietal cortex, c = occipital cortex, d = temporal cortex, e = cingulate cortex, f = hippocampus, g = caudate nucleus, h = thalamus, i = hypothalamus, j = sup. colliculus, k = inf. colliculus, l = cerebellum, m = pons, n = medulla. Brain regions (B): a = frontal cortex, b = parietal cortex, c = occipital cortex, d = ant. cingulate cortex, e = post. cingulate cortex, f = cerebellum vermis, g = cerebellar cortex, h = caudate nucleus, i = hippocampus, j = colliculi, k = thalamus, l = hypothalamus, m = medulla, n = brain stem. Values are mean±SD of 10 to 12 rats. Data modified after [12, 13]. Right Panel: Representative examples of coronal sections of rat brain from 6 different levels (a–f) showing Evans blue albumin (EBA) extravasation following immobilization heat stress (HS, A), forced swimming (FS, B) and immobilization stress (IMZ, C). The pattern and intensity of EBA showed selective variations in different levels according to the stressors used. Most extensive staining of various brain regions are observed after heat stress (B) followed by forced swimming (C) and immobilization (A). Staining of cingulate (a–c), frontal (a), parietal (b, c), temporal (c), occipital (d), and piriform (b–c) cortices are clearly evident (A.a–c; B.a–d; C.a–c). Different pattern and intensity of EBA staining in immobilization (C), heat stress (A) and forced swimming (A) are apparent in deep brain structures, e.g., caudate putamen (a), hippocampus (b–c), thalamus (b–d), hypothalamus (b–d), amygdala (b–c), brain stem (d–e) and cerebellum (f). (Co-ordinates for coronal sections: a = + 0.10 to +0.45; b –3.25 to –3.90; c = –4.20 to –4.60; d = .5.25 to –6.65; e = –7.10–7.60; f = –10. 60 to –11.90 from Bregma). Bar = 5 mm. Modified after [12]
Structural changes in the brain at the time of BBB disruption in stress. Representative examples of light microscopic changes in different brain regions following 4 h heat stress (HS), 8 h immobilization (IMZ) or 30 min forced swimming (FS). Marked degeneration (arrow heads) in dentate gyrus and CA-4 region (*) of the hippocampus is seen following HS (A.b) compared to control (A.a). Many damaged and distorted nerve cells in the brain stem regions following HS is apparent (A.d, arrows) compared to control (A.c). Mild to moderate cell damage in the hippocampus CA-4 region is seen following IMZ (A.e, arrows) or FS (A.f, arrow heads). IMZ (B.a) and FS (B.b) induces specific and selective cell damage (arrow heads) in the cerebral cortex. Cell damage in ependymal cells (arrows) in the median eminence following IMZ (B.c) and FS (B.d) is clearly evident. Degeneration (arrows) of choroid plexus epithelial cells and ependymal cells in the lateral cerebral ventricle by IMZ (B.f) and FS (B.g) is apparent compared to control (B.e). In the cerebellar Purkinje cells and granule cells show marked degenerative changes following FS (B.i, arrows) compared to control (B.h). A. a-d Nissl stain; others H & E stain on 3 μm thick paraffin sections. Bars: A. a–b 50 μm; c–d, g–h 25 μm, e–f 30 μm; B: a–i 40 μm. Reproduced with permission after [12]
9.1.2 Immobilization Stress and Structural Changes in the Brain
Profound neuronal damages are seen in the brains of immobilized rats at the time of the BBB leakage. Most of the nerve cell damage is seen in the areas showing leakage of Evans blue or radioiodine extravasation [12]. Thus, specific nerve cell damage following 8 h immobilization is seen in the cerebral cortex, hippocampus, cerebellum and in brain stem. Many dark and distorted nerve cells are present in the superficial layers of the cerebral cortex especially in the cingulate, parietal, temporal and in occipital cortex (Fig. 9.8). The hippocampal dentate gyrus, CA4 and CA3 sectors as well as CA1 subfield contain several damaged nerve cells (Fig. 9.8). Dark neurons are frequent in the brain stem reticular formation. Degenerative changes in cerebellar Purkinje cells and granule cells are also quite common (Fig. 9.8).
The choroid plexuses and the ependymal cells around the lateral and third ventricles show degenerative changes. In these regions, sponginess and edema is frequent (Fig. 9.8). These observations indicate disruption of the blood-CSF barrier in immobilization stress [4, 6, 7, 12, 43].
At the ultratstructural level, areas showing BBB disruption reveals membrane damage, vacuolation and distortion of nerve cells (Fig. 9.13). This indicates that stress induced BBB disruption is associated with structural changes in the neuropil.
9.1.3 BBB in Forced Swimming
Forced swimming is frequently used as an animal model of depression. When rats are forced to swim in a restricted pool, they quickly acquire an immobility response [127]. The hypoactivity caused by swim stress is associated with selective neurochemical metabolism in the brain. Our laboratory was the first to show that rats subjected to forced swimming exhibit selective disruption of the BBB [104, 126, 128] that is reversible in nature [12, 104].
Thus, extravasation of Evans blue albumin was noted in 5 brain regions following 30 min forced swimming. These regions are cingulate cortex, parietal cortex, occipital cortex, cerebellum and the dorsal surface of the hippocampus the brain is evident (Figs. 9.6 and 9.7). In most cases, the cerebellar vermis took moderate blue staining compared to the lateral cerebellar cortex (Fig. 9.7). The deep cerebellar nuclei were mainly unstained (Figs. 9.6 and 9.7). The walls of lateral ventricle took mild stain, whereas the 4th ventricle exhibited deep blue staining (Fig. 9.6). The areas around the third ventricle were also stained mildly indicating a disruption of the blood-CSF barrier by forced swimming (Fig. 9.7). On the other hand, extravasation of radioiodine after 30 min swimming was observed in 8 brain regions. Thus, besides 5 blue stained regions, the radiotracer is present in another 3 brain areas viz., caudate nucleus, thalamus and hypothalamus (Figs. 9.6 and 9.7) [12, 104].
Subjection of animals to short duration of swimming, e.g., 5 or 15 min did not show extravasation of protein tracers in the brain (Fig. 9.7) [12, 104]. This BBB disruption following forced swimming in young rats is reversible in nature. Thus, the BBB permeability is no longer observed in rats subjected to 2 h rest after 30 min swimming (Fig. 9.7) [12, 104, 128].
9.1.4 Swimming Induced Structural Changes in the Brain
Structural changes in the brain were seen in the rats after 30 min swimming in the areas exhibiting BBB disruption [12]. Thus, light microscopy revealed specific changes in the neuropil, and damage of selective nerve cells in the cerebral cortex, hippocampus and in cerebellum in rats subjected to 30 min forced swimming (Fig. 9.8). This selective nerve cell damage is seen largely in the layer III to V in the cerebral cortex that is most pronounced in the cingulate, occipital and piriform cortices (Fig. 9.8). This indicates that BBB disruption contributes to cellular injury.
Degenerative changes in few nerve cells are visible in the brain stem and granule cells of the cerebellum after 30 min swimming (Fig. 9.8). The presence of damaged nerve cells is common in the dentate gyrus, CA 3 and CA 4 sectors of hippocampus.
Mild to moderate degree of ependymal cell damage around the lateral and third ventricle and degenerative changes in the choroid plexuses are also seen at this time (Fig. 9.8) confirming the BCSFB disruption by forced swimming.
At the ultrastructural level, vacuolation and damage to neuropil is present in the cortex and in brain stem in rats after forced swimming (Fig. 9.9). These observations are in line of the idea that BBB disruption in swim stress is associated with selective nerve cell damage. Whether these cell changes in such a short duration of 30 min reflect acute nerve cell death or permanent neurodegenerative changes are unclear. To further confirm this point, morphological investigations in rats following several days or weeks after 30 min swimming are needed [2, 12, 13].
Ultratstructural changes in the brain at the time of BBB opening in stress. Representative examples of ultrastructural changes in the rats brain following 4 h heat stress (HS), 30 min forced swimming (FS) or 8 h immobilization (IMZ) stress. In the cerebral cortex, one nerve cell with dark and electron dense cytoplasm (arrows) is seen following HS (A.a) Many degenerative changes can be seen in the neuropil (A.a). High power electron micrograph from the parietal cerebral cortex cellular layer III showing damaged synapses (arrows), vesiculation of myelin and membrane damage following HS (A.b). A completely collapsed microvessel (arrow heads) and distorted granule cells in the cerebellum are seen following HS (A–c). Perivascular edema (*), membrane damage and leakage of lanthanum across the microvessels (A–d) are quite frequent in HS. Vacuolation, membrane damage (arrows) and perivascular edema (*) are frequent following FS (B.a,c) or IMZ (B.b,d). Myelin vesiculation (B.e) and nerve cell damage (B.f) is very common in hippocampus and in thalamus following HS. Bars: A.a = 0.6 μm; A.c,d = 1 μm; A.b = 0.4 μm nm; B.a–e = 1 μm; B.f = 0. 5 μm. Reproduced with permission after [12]
9.2 Learned Helplessness and the BBB Dysfunction
Learned helplessness induced by sleep deprivation is an experimental model of depression and/or anxiety [129–132]. Sleep structure is a sensitive marker of human affective disorder in depression [133, 134] as well as in anxiety [135]. Thus, sleep deprivation for certain periods could mimic learned helplessness and induce signs of depression (see [12, 13, 136]).
9.2.1 Sleep Deprivation and the BBB Disruption
Sleep deprivation for 4 days induces profound cellular and molecular changes in the brain reticular activating system [136, 137] along with expression of c-fos and Fos proteins. In addition, alterations in GABergic and serotonergic neurons could also be seen in the brain stem reticular formation in these sleep-deprived rats [136]. However, alterations in the BBB function following sleep deprivation are still not investigated in details [12, 13].
We examined BBB function in rats following 1–4 days of sleep deprivation using an inverted flower pot model [136–138] that induces a selective deprivation of paradoxical sleep (PS) [138]. Each rat is placed on an inverted flower pot (6.5 cm in diameter) surrounded by water filled in a Plexiglas box up to 1 cm of the surface with free access to food and water [136–138]. The water temperature is maintained at 30±1°C [104, 128].
The animals in this model can undergo to slow wave sleep (SWS) but not the PS [136]. Thus, the loss of muscle tonus with the onset of PS causes animals to fall into the water and awaken them [136–138]. The PS is significantly attenuated 48 h after the sleep deprivation in this model. For BBB experiments, the animals were kept maximum for 96 h under these conditions [12, 13, 136].
Our observations show that sleep deprivation of 48 h induces mild blue staining of the frontal, temporal and cingulate cortices [12, 13]. The cerebellar cortex took faint staining. This increase in Evans blue extravasation was further intensified at 96 h after sleep deprivation. Thus, moderate Evans blue staining in the cingulate, frontal, parietal and temporal cortices is observed (Sharma HS unpublished observations). The walls of lateral cerebral ventricles, dorsal surface of the hippocampus and massa intermedia showed mild blue staining (Fig. 9.5). Some areas in the brain stem reticular system took mild to moderate staining (Fig. 9.5).
Extravasation of HRP and endogenous albumin immunohistochemistry showed a good relationship with the exogenous Evans blue extravasation in the brain (results not shown). Thus, the albumin immunoreactivity was mainly seen around the microvessels in the cerebral cortex, hippocampus, brain stem and thalamus. In 96 h sleep-deprived rats, the albumin immunoreactivity was also seen around few nerve cells in the cortex, hippocampus, brainstem, cerebellum and thalamus (Sharma HS unpublished observation). These observations are the first to show that the sleep deprivation stress depending on its duration is able to induce BBB disruption in specific regions.
9.2.2 Structural Changes in the Brain Following Sleep Deprivation
Light and electron microscopy showed profound neuronal, glial and endothelial cell changes in the areas associated with Evans blue leakage in rats following 48 h and 96 h after sleep deprivation (results not shown). Several neurons in the hippocampus CA-3 regions, dentate gyrus and subiculum were dark in appearance and perineuronal edema was most prominent (Sharma HS unpublished observations). Sporadic changes in cerebellar granule cells and purkinje cells were also seen in the vermis region. Most profound alterations in neuronal structures were seen in the brainstem reticular formation. These observations suggest that BBB disruption in sleep deprivation is associated with marked neuronal damages.
9.3 Environmental Heat as Stressor and the BBB Dysfunction
Around 60% of the World populations live in the temperate climate where high environmental temperatures during summer seasons could induce serious health problems. Thus, about 10,000–12,000 deaths are recorded during heat waves when the ambient air temperature reaches between 32 and 34°C [139–142]. High incidence of heat-related mortality occurs in cities with high levels of urbanization [12, 27, 105, 110, 142–144]. However, the exact causes of heat deaths are still not well known.
The first scientific report on heat-related death was published in 1743 describing death of 11,000 persons in China during a hot weather in July. Another incidence of heat death was seen in Liverpool in 1841, in which 33 British soldiers died in one hot day in a ship while coming from Muscat to Bushier [105, 110, 143–145]. Similarly, during 1873 in the “Black Hole of Calcutta”, 123 out of 186 British prisoners collapsed in one night [21, 27, 49, 105, 145]. More than 700 persons died in 1995 due to hot weather conditions in Chicago during summer [21, 27, 49, 146]. About 1000 deaths in 1996 occurred in nursing homes of Rotterdam, the Netherlands that were related to hot weather conditions [147, 148]. These reports suggest that high environmental heat is a serious life-threatening event probably due to heat-induced severe brain damage [21, 27, 28, 49, 105, 106].
Rise in core body temperatures above 40°C is associated with heat-stroke [105, 106, 149]. More than 50% of heat stroke victims die within short period despite lowering of the body temperature and/or therapeutic interventions. Those who survive show permanent neurological deficits [21, 27, 28, 49, 105, 106, 150]. This indicates that the brain is a highly vulnerable organ in heat-related illnesses [4, 9, 11–13, 21, 28, 105, 150].
Our laboratory was the first to show that experimental or environmental heat stress induces BBB disruption to protein tracers [2–13, 22–27, 150]. This suggests that environmental heat exposure during summer months could lead to brain damage due to BBB dysfunction [12, 13, 150].
9.3.1 Heat Stress Induced BBB Dysfunction
Using an animal model of heat stress we exposed rats at 38° C in an environmental chamber (wind velocity 2.6 cm/sec; Relative humidity 45–47%) for 1–4 h and examined the BBB function using Evans blue and radioiodine [2–13]. Marked increase in the BBB to Evans blue albumin and radioiodine tracer are apparent in animals after 4 h heat exposure (Figs. 9.6 and 9.7). The blue staining is seen in 8 brain regions, viz., cingulate cortex, occipital cortex, parietal cortex, cerebellum, temporal cortex, frontal cortex, hypothalamus and thalamus (Fig. 9.7). Mild to moderate staining of the ventricular walls were observed. The fourth ventricle showed deep blue staining and the structures around the third ventricles were moderately stained (Fig. 9.7). Occasionally the dorsal surface of the hippocampus also took mild stain (Figs. 9.6 and 9.8). indicating disruption of the blood-CSF barrier function as well [43].
On the other hand, extravasation of radioiodine occurred in 14 brain regions examined. Thus, besides the 8 blue stained regions, another 6 region viz., hippocampus, caudate nucleus, superior and inferior colliculi, pons and medulla also showed an increase in radioactivity (Fig. 9.6) [2, 6, 12, 13].
Subjection of rats to shorter periods of heat stress, i.e., 1 or 2 h did not induce BBB disruption [6]. Furthermore, animals subjected to 2 h rest at room temperature after 4 h heat exposure still show a mild leakage of Evans blue and radiotracers extravasation in brain (Fig. 9.7). These animals are still lethargic, however their body temperature returned to normal level (Sharma HS unpublished observations). This suggests that the BBB changes in heat stress are long lasting and can be seen even when the body temperature returned to normal [12, 13, 150].
9.3.2 Structural Changes in the Brain Following Heat Stress
Disruption of BBB in heat stress is associated with brain damage [12–14, 24, 151]. Thus, profound nerve cell changes are seen in those brain areas exhibiting leakage of Evans blue and radioiodine after 4 h heat exposure. Neuronal cell injury, edematous expansion and sponginess of the neuropil are common in several brain areas e.g., such as cerebral cortex, brain stem, cerebellum, thalamus and hypothalamus (Figs. 9.8 and 9.9). A selective nerve cell damage in the hippocampus is most pronounced within the CA-4 subfield compared to other regions (Fig. 9.8), although edematous swelling and general sponginess are present throughout this region. This indicates that BBB leakage is associated with brain damage in heat stress.
Damage to ependymal cells around the lateral and third ventricle is quite prominent in heat stress (Fig. 9.12). The choroid plexus from the lateral ventricle, third ventricle and fourth ventricles exhibited degenerative changes (Fig. 9.8) indicating heat stress induced disruption of the blood-CSF barrier [43, 44, 105, 106].
At the ultrastructural level, damaged nerve cells, degenerated nuclei accompanied with eccentric nucleolus are frequent in the cerebral cortex, hippocampus, cerebellum, thalamus, hypothalamus, and brain stem (Fig. 9.9). The nerve cells are dark in appearance and contain vacuolated cytoplasm. The nuclear membrane contains many irregular foldings and the nucleolus often showed signs of degeneration (Fig. 9.9). Interestingly, damage of the one nerve cell is often seen in a region where the adjacent neuron is almost normal in appearance suggesting a selective vulnerability of nerve cells in heat exposure [2–14, 22–28, 49, 105, 106, 150, 151].
Swollen synapses with damage to both pre-and post-synaptic membranes are common in thalamus, brain stem, hypothalamus, cerebellum, hippocampus and in cerebral cortex (Fig. 9.9). In some of these regions damage to post-synaptic dendrites and disruption of synaptic membrane is also common.
Widespread axonal damage, demyelination and vesiculation are most pronounced in the brain stem reticular formation, pons, medulla and the spinal cord (Fig. 9.9). Many unmyelinated axons are also swollen. These observations are in line with the idea that breakdown of the BBB is an important factor in heat induced brain damage.
9.3.3 Ultratstructural Changes in the Cerebral Endothelium
Disruption of the BBB at ultrastructural level is clearly seen in heat stress. Using lanthanum as electron dense tracer, we observed several microvessels that exhibit leakage of lanthanum across the cerebral endothelium in a very selective manner (Fig. 9.10). The leakage of lanthanum is often evident in one endothelial cell, whereas the rest of the vessel or the adjacent endothelial cells are completely normal (see Fig. 9.10). This indicates a highly selective nature of the endothelial cell membrane permeability in heat stress [11–13]. Activation of specific endothelial cell transporters, permeability factors, neurochemical receptors or ions channels located on the selected area of the endothelial cell membrane many be responsible for such a selective increase in the lanthanum permeability [13].
Ultrastructural changes in the cerebral endothelial cells and the adjacent neuropil at the time of the BBB disruption in stress. Ultratstructural studies on the cerebral endothelial cells from various brain regions in heat stress showing lanthanum extravasation and damage to adjacent neuropil. (A) Lanthanum, an electron dense tracer (seen as dark black particles) is seen across the endothelial cell membrane containing tight junctions (A.a blank arrows). Infiltration of lanthanum across the endothelial cell membrane is clearly seen (solid arrows, A.b,c). In some cases lanthanum is seen diffusely infiltrated within the cell membranes of tight junction complex and endothelial cell cytoplasm covering the apposed plasma membranes connected with the tight junctions (A.a). However in these cases the tight junctions are not found opened because lanthanum within the intercellular cleft is stopped at the tight junction (blank arrows, A.a). In some cases only one endothelial cell membrane covering tight junction is found diffusely infiltrated with lanthanum (filled and blank arrows) leaving its counterpart completely intact (A.c) One endothelial cell showed infiltration of lanthanum in a certain segment of the cerebral endothelium (A.d, arrow heads). Damage to neuropil (*) and myelin vesiculation are prominent (A.e) in the adjacent area. (B) Lanthanum is present in endothelial cell and in the basement membrane (B.a, b) without widening of the tight junction (B.a). In several microvascular profiles, lanthanum is stopped at the tight junctions (B.c,d, arrow heads). Damage to synaptic membrane (arrows, B.e), vacuolation, edema and myelin vesiculation (B.f) is frequent around microvessels showing BBB disruption to lanthanum (B.e, f). (C) Many cerebral endothelium show presence of lanthanum in the microvesicular (*) profiles within the cell cytoplasm (C.b, d). Normally, the tight junction in these microvessels appears to be closed (C.a, c, d). Complete collapse of microvessels with perivascular edema and damage to neuropil (C.e) is common in many brain regions during heat stress. Bars: A = 0.3 μm; B = 0.2 μm; C = 0.2 μm. Reproduced with permission after [12]
In many other vascular profiles, lanthanum is stopped at the luminal side of the tight junctions (Fig. 9.10). Whereas, several microvessels showed infiltration of lanthanum across the endothelial cells membranes including the tight junctions without widening them (Fig. 9.10). These observations support the idea of specific receptor mediated increase in microvascular permeability [12, 13, 23, 24, 105]. Since receptors can also be present on the membranes apposing tight junctions, increased microvascular permeability around the junctions is possible via activation of such receptors [12, 13, 150].
Taken together our morphological studies clearly points out an intimate role of BBB breakdown in brain pathology following heat stress.
9.3.4 Cognitive and Sensory-Motor Dysfunction in Heat Stress
Whether BBB disturbances in heat stress contribute to cognitive and sensory motor dysfunction is still a matter of speculation [12–14, 23, 24, 28, 105, 106, 143, 144, 150]. Available evidences show that alterations in fluid microenvironment of the brain in specific regions, e.g., hippocampus, cerebellum, amygdala, visual, sensory-motor cortex, hypothalamus, caudate nucleus, colliculi and cerebellum could be responsible for cognitive and sensory motor dysfunctions. Thus, it is quite likely that in heat stress cognitive and sensory-motor functions are affected at the time of the increased BBB permeability [11–14, 105, 106, 150].
Keeping these views in mind, we examined cognitive and sensory-motor functions in animals subjected to heat stress using standard procedures [105, 106, 143, 144, 150].
We used Rota-Rod treadmill (at 16 rpm) to assess motor co-ordination and fatigue in rats. Rats not falling off the Rota-Rod for 2 min were considered normal during a 3 min session [144]. Subjection of rats to 3 h heat stress showed a significant decline in Rota-Rod performance that was progressive in nature up to 4 h period (Fig. 9.11). In these rats, changes in locomotor behaviour, gait and overall walking skill was examined using a grid-walking test in which an elevated level (30°) of stainless steel grid was used with a mesh size of 30 mm [144]. The animals were placed on the grid for 1 min and the total number of paired steps, i.e., placement of both forelimbs was counted. During this period, the number of misplaced limbs error, viz., the forelimbs fell through the grid was recorded. The total number of errors for each forelimb was also counted manually [12, 13, 144, 150].
Sensory-motor and cognitive dysfunction at the of the BBB disruption in heat stress and their prevention with Naloxone treatment. A significant decrease in the angle of inclined plane test reflecting alterations in motor functions was noted in rats after 3 h after heat exposure that was progressive up to 4 h (A). Marked decline in cognitive function was also seen in heat stressed animals when they are subjected to Rota-Rod performance (B). At 3 h heat stress, rats could not stand on Rota-Rod for more than 75 sec that was subsequently reduced to 60 sec at 4 h (B). Measurement of gait and walking pattern revealed deficit in the placement of legs (c) and the stride length (D) from 3 h and onwards. Heat stressed rats also showed significant deficit in grid walking and placement errors compared to controls (E, F). Decrease in the number of steps taken in a grid walking test for 60 sec was evident in rats subjected to 4 h heat stress (E). However, placement errors of hind feet can be seen as early as 3 h after heat exposure (F). Pretreatment with naloxone in high doses improved the motor and cognitive functions in rats after 4 h heat stress (A–F). However, low doses of naloxone (1 and 5 mg) did not alter these deficits significantly. Data at each column represent mean±SD of 5 to 6 rats. * P <0.05; ** P <0.01, ANOVA followed by Dunnet’s test for multiple group comparison from one control group. DD = P<0.01, chi-square test from the control group. Reproduced after permission from [144]
Rats subjected to 4 h heat exposure were unable to walk normally during a grid walking session. The number of steps taken during a 60 sec grid-walking session was significantly reduced in heat stressed rats at 4 h (Fig. 9.11). These animals exhibited greater placement errors of hind legs on the grid following 3 and 4 h after heat exposure (Fig. 9.11). These observations suggest that BBB disruption following heat stress leads to significant deficits in cognitive and sensory function.
The motor disturbances in the rat after heat stress was determined using the inclined plane test. The angle of inclined plane was set in such a way (60°) that the normal animal could stay on the plane for 5 sec without falling. In this test, a significant motor deficit in heat stressed animals is seen that was most pronounced after 3–4 h exposure (Fig. 9.11). Another good measure of gait and motor disturbances can be judged using footprint analysis [12, 13, 144]. For this purpose, the hind paws were wetted and the animals were allowed to walk on a paper coated with bromophenol blue dissolved in acetone. The imprints of hind paws were used to determine motor function behaviour by measuring the distance (mm) between hind paws from the base of the central pads [12, 13, 21, 23, 24, 28, 105, 106, 150]. In addition, the stride length (mm) was also determined by measuring the distance between hind paws in two consecutive steps.
Animals subjected to heat stress exhibited pronounced motor disturbances at the time of the BBB disruption. Thus, the transverse distance between the hind feet, a measure of disturbed gait was increased significantly at 4 h (Fig. 9.11). On the other hand, the stride length calculated as longitudinal distance between hind feet during stepping showed a significant decrease from 2 h heat exposure and was progressive in nature (Fig. 9.11). Taken together, these observations clearly indicate that cognitive sensory-motor functions are definitely altered at the time of the BBB dysfunction in heat stress [12–14, 144]. This suggests that persons exposed to long time period in hot environments, e.g., solders in the Middle East may be highly prone to cognitive and sensory motor disturbances over time even without any external injuries to their CNS.
9.4 Nanoparticles as Stressors and the BBB Dysfunction
Several nanoparticles from various sources are present in the environment that could influence human health functions [107, 108, 152]. However, the potential effects on environmental nanoparticles on human brain functions with regard to BBB dysfunction are still not well known [107, 108, 152–155]. Persons exposed to environments around the industrial waste, battlefield, or silica dust in deserts could inhale lots of nanoparticles e.g., SiO2, Cu, S, Al, C, Ag and Mn etc. that could reach to their CNS easily through translocation [107, 108, 152–156]. Once these nanoparticles reach into circulation that may be deposited in different areas of the body in various organ system leading to alterations in respiratory, cardiac, renal, hepatic or even brain and spinal cord functions [13, 107, 108, 152, 153].
There are reasons to believe that nanoparticles once entered into the body fluid system will induce oxidative stress and production of free radicals and could be thus responsible for cell membrane damage [107]. Thus, nanoparticles, from Cobalt, carbon tubes, quantum dots, and ultrafine particles (20–80 nm) induce production of reactive oxygen species (ROS), especially following concomitant exposure to light, ultraviolet, or transition metals [157–165]. Since oxidative stress alone is capable to induce brain pathology [166–168], it is likely that nanoparticles induce ROS activation may play crucial roles in inducing BBB disruption and neurotoxicity. However, the effects of nanoparticles exposure per se on the BBB function are still not well investigated in details [152–156].
9.4.1 Nanoparticles Administration Induces BBB Disruption
Using engineered nanoparticles from metals, i.e., Ag, Al and Cu (50–60 nm) we examined BBB permeability to proteins in rodents after their administration through systemic or cerebral routes. Our observations are the first to show that nanoparticles when administered systemically or in to the brain ventricles, significantly increased the BBB permeability to Evans blue and radioiodine in rats and mice [154]. This effect was most pronounced with Ag and Cu nanoparticles as compared to Al in mice compared to rats (Table 9.3). Intraperitoneal administration of nanoparticles (50 mg/kg) was the least affective in inducing BBB disruption caused by any nanoparticles used these studies (Table 9.3).
On the other hand, intravenous administration of nanaoparticles (30 mg/kg) resulted in pronounced disruption of the BBB 24 h after administration as compared to 4 h period (Table 9.3) and was most marked in mice (Table 9.3). Ag and Cu nanoparticles exerted most powerful disruption of the BBB as compared to Al treatment (Table 9.3).
When nanaoparticles (2.5 mg/kg) were administered into the cerebral circulation through right internal carotid artery (ica) Evans blue or radioiodine leakage was seen in the ipsilateral side of the brains only (Table 9.3). This effect was most prominent with Ag and Cu nanoparticles after 24 h injection (Table 9.3) [154].
Direct injection of nanoparticles (20 μg in 10 μl) into right lateral ventricle resulted in extravasation of Evans blue and radioiodine into the infused side of cerebral hemisphere significantly that was most prominent at 24 h after nanoparticles administration (Table 9.3). Ag and Cu nanoparticles exerted most powerful BBB disruption in rats and mice as compared to Al infusion (Table 9.3) [154].
In most cases, cerebellum, hypothalamus, piriform cortex, brain stem and ventral surface of the brain served by major cerebral arteries showed quite pronounced leakage of Evans blue in nanoparticle treated groups (Fig. 9.12). Blue staining was also seen on the dorsal and ventral surfaces of the brain and spinal cord in nanoparticles treated rats and mice (Fig. 9.12). The leakage of Evans blue was also seen in deeper structures of the brains as coronal sections showing profound blue staining of the deeper areas of the cortex, hippocampus, thalamus and hypothalamus (Fig. 9.12 arrows).
These observations clearly suggest that nanoparticles depending on their type, dosage and route of administration induces BBB disruption. Thus, Ag and Cu are mot effective in opening of the BBB as compared to Al in identical doses. This effect of nanaoparticles appears to be species specific as mice are more sensitive to rats in BBB disruption [154].
Effects of engineered nanoparticles from metals on the BBB disruption and concomitant structural changes in the brain. (A) Shows extravasation of Evans blue on the dorsal (a) and ventral (b) surfaces of rat brain after Ag nanoparticle treatment. The Ag nanoparticle was administered intravenously (35 mg/kg) and the rat is allowed to survive 24 h after injection. Coronal sections of the brain passing through hippocampus (c) and caudate nucleus (d) are also shown. Leakage of Evans blue dye can be seen in various brain regions (arrows). The deeper parts of the brain, e.g., hippocampus, caudate nucleus, thalamus, hypothalamus, cortical layers including pyriform, cingulate, parietal and temporal cortices showed moderate blue staining. This indicates widespread leakage of Evans blue albumin within the brains after Ag treatment. Bar = 3 mm. (B) Shows albumin immunoreactivity (a, b) and glial fibrillary acidic protein (GFAP) expression (c, d) in the cerebral cortex rats receiving Cu (a, c) or Ag (b, d) treatment. These nanoparticles were administered separately (35 mg/kg) intravenously in rats and the animals allowed to survived 24 after the administration. Paraffin (3 μm thick) sections showed massive uptake of albumin (a, b, arrows) by the nerve cells and along with its extravasation in the neuropil. Damage to nerve cell and leakage of albumin in the neuropil is more conspicuous by Ag treatment (b) compared to Cu nanoparticles administration (a). Overexpression of astrocytes, as seen by GFAP immunoreactivity is present in the neuropil of both Ag (d) and Cu (c) treated animals. Star shaped astrocytes are more frequent in the neuropil of Ag treated rats compared to Cu treatment. Bar: 50 μm. (C) Transmission electronmicrograph of myelin (a, b), nerve cell (c) and one microvessel (d) following Ag or Cu nanoparticles treatment. Low power light micrograph showing immunostaining of heat shock protein (HSP, e, f) and glial fibrillary acidic protein (GFAP, g, h) in the spinal cord following Ag or Cu nanoparticle treatment. Ag (a) or Cu (b) nanoparticles selectively induce damage to myelinated fibers (arrowheads) in rats after 24 h administration. However, normal myelinated fibers (arrows) are also seen in the neuropil. Bar a, b = 600 nm. Degeneration of one nerve cell and disintegration of nucleolus (arrows) is clearly seen in the cerebral cortex by Cu treatment (c). Damage to myelinated fibers and vacuolation of the neuropil are also seen (c). A completely collapsed microvessel (arrow) with perivascular edema and myelin damage (arrow) is seen in Cu treated rat (d). Bars c, d = 1 μm. (D) Expression of stress protein seen using heat shock protein expression (HSP 72 kD) is evident in the spinal cord after Ag (e) or Cu (f) treatment. HSP expression is seen within the neurons (arrows) as well as in glial cells. Bars e, f = 40 μm. Expression of GFAP, marker of astrocytes is seen in the longitudinal section of spinal cord (arrows) of Ag (g) or Cu (h) treated rats. Bars g, h = 50 μm. Modified after [13, 154]
9.4.2 Structural Changes in the Brain After Nanoparticles Administration
Light and electron microscopy revealed profound brain pathology in nanoparticles treated animals. These structural changes were present in those areas showing BBB leakage [108, 154]. Thus, profound alterations in nerve cells were seen in the cerebral cortex, hippocampus, cerebellum, thalamus, hypothalamus and brain stem in
nanoparticles treated rats or mice at light microscopy (Table 9.3, Fig. 9.13). These neuronal changes were most marked when Ag or Cu nanoparticles were administered through intravenous, intracarotid or intracerebroventricular routes (Fig. 9.13) [154]. In terms of loss of neurons or nerve cell damage by nanaoparticles, hippocampus (Fig. 9.13) was the most adversely affected organ followed by cerebellum, cerebral cortex, brain stem, thalamus and hypothalamus [154]. These observations demonstrate that nanoparticles are capable to induce brain pathology probably though BBB disruption [107, 108, 154].
9.4.3 Cognitive and Sensory-Motor Dysfunctions by Nanoparticles Exposure
At the time of BBB dysfunction, nanoparticles treated rats showed mild to moderate deficits in the cognitive and sensory-motor functions. This was evident by their poor performances seen on Rota Rod, grid walking, inclined plane angle and footprint analysis tests. These sensory motor deficits were most pronounced by Ag and Cu treated group as compared to Al treatment. Moreover, administration of nanoparticles through intravenous, intracarotid or intracerebroventricular routes resulted in most massive deficits in the above behavioral functions as compared to their intraperitoneal administration (Sharma HS unpublished observations). These observations indicate that nanoparticles induced BBB dysfunction and subsequent brain pathology could be responsible for sensory motor dysfunction (Sharma HS unpublished observations).
10 A Combination of Nanoparticles and Heat Stress Exacerbate BBB Disruption and Brain Pathology
Recently, magnetic nanoparticles are used to enhance tumor temperatures [169]. This “Thermotherapy” for tumor treatment is based on controlled heating of intra-tumoral administered magnetic nanoparticles [170]. Thus, local administration of magnetic nanoparticles within the tumor sites resulted in a 3–4°C higher temperature compared to tumors without the nanoparticles administration. This observation suggests that magnetic nanoparticles could enhance the tumor temperature effectively to kill the cancer cells. Interestingly, this thermotherapy with nanoparticles also limits proliferation by inducing localized necrosis around the peritumoral zones [107, 170]. This suggests that heating in presence of magnetic nanoparticles enhances tumor temperature that could kill more cells as compared to heating without these nanoparticles. However, this is still uncertain whether exposure of nanoparticles may alter the sensitivities of the whole body hypertehrmia (WBH) [150]. Accordingly, this is not known whether soldiers in Middle East that are exposed to silica dust or Cu nanoparticles routinely could be more sensitive to environmental heat induced exacerbation of brain pathology as compared to normal populations [156].
To further clarify these points, we initiated animal experiments in our laboratory in which nanaoparticles exposed rats or mice are subjected to heat stress and BBB permeability and brain pathology was examined. Our novel investigations show that rats exposed to nanaoparticles prior to heat stress exhibited an exacerbation of BBB dysfunction and brain pathology [107, 108, 156].
10.1 Exacerbation of BBB Disruption Heat Stress by Nanoparticles
We examined the effects of chronic exposure of three different nanoparticles derived from metals e.g., Al, Ag, and Cu (50–60 nm sizes) on brain function subjected to WBH. The results are compared with heat-stressed rats without receiving any nanoparticles. The metal nanoparticles (Cu, Al and Ag, ≈50–60 nm in size) were suspended in Tween 80 and administered separately in 3 different groups of rats through intraperitoneally route in a dose of 50 mg/kg (weight by volume) once daily for 7 days. On the 8th day, these animals were subjected to 4 h heat stress at 38°C and barrier permeability and brain pathology were examined [107].
Rats treated with nanoparticles exhibited about 3–30% increase the BBB and about 16–75% increase in blood-spinal cord barrier (BSCB) permeability to protein tracers after WBH as compared to saline treated heat stressed animals (Table 9.4). This effect was most pronounced in Cu treated nanoparticles followed by Ag and Al treatment (Table 9.4). The magnitude of BBB disruption after WBH in nanoparticles treated animals was most marked in the spinal cord. This suggests that nanoparticles are likely to produce severe damage to the spinal cord resulting in more profound sensory-motor dysfunction. The mechanisms behind a selective vulnerability of the spinal cord in nanoparticles treated heat stressed rats compared to brain is still unclear.
Using radioiodine, the tracer extravasation following WBH was most pronounced in different brain regions by Ag treatment followed by Cu and Al treatments (Table 9.4). The highest increase in regional BBB to radioiodine was seen in brain stem (≈400%) followed by hippocampus and cerebellum (≈300%), cerebral cortex (200%) and thalamus and hypothalamus (≈150%, See Table 9.4). These observations indicate that nanoparticles are able to influence regional BBB function in a selective manner depending on their chemistry [107, 153].
10.2 Exacerbation of Structural Changes in Brain in Heat Stress by Nanoparticles
Nanoparticles treated animals when subjected to 4 h heat stress; they exhibited an exacerbation of neuronal, glial, axonal and endothelial cell damages (see Table 9.5). The most marked effects of WBH-induced aggravation of cellular injuries are seen in Ag nanoparticles followed by Cu and Al treatment [107]. These brain cell damages are mostly seen in the regions exhibiting BBB leakage.
Thus, large number of distorted neurons is seen in the brainstem, hippocampus, cerebellum, cerebral cortex, thalamus, hypothalamus and spinal cord [107, 156]. The neuronal damage includes chromatolysis, degeneration, distortion of cell nucleus and/or nucleolus that are most marked in Ag and Cu treated stressed animals (Fig. 9.14). A greater expansion, sponginess and edema are common finding in these nanoparticles treated rats after WBH as compared to saline treated animals (Fig. 9.13).
Exacerbation of neuronal damage in heat stress by prior exposure to nanoparticles. Neuronal damage in heat stress (a) and its exacerbation with Cu nanoparticles (b). Many nerve cells (arrows) are dark and distorted in heat stressed rat (a) and sign of sponginess and edema are clearly seen. These cell changes appears to be more prominent in rat that received Cu nanoparticles treatment (for 1 week) before heat stress (b). The number of dark and distorted nerve cells (arrow heads) is much more pronounced in Cu nanoparticle treated rats after heat exposure (b) and saline treat rat (a). Bar = 100 μm. Reproduced with permission after [107]
Exacerbation of BBB leakage to lanthanum at the ultrastructural level in heat stress by prior exposure to nanoparticles. Blood-spinal cord barrier (BSCB) to electron dense tracer lanthanum after 4 h heat stress in saline treated (a) and in Ag nanoparticle treated (1 week) rat (b). High power electron micrograph showing presence of lanthanum in the basal lamina (arrows) of one spinal cord microvessel from the ventral horn of the T9 segment (a). Deposit of lanthanum within the basal lamina and in extracellular space is clearly seen in the neuropil (a). In Ag nanoparticle treated stressed rat, the magnitude and intensity of lanthanum extravasation across the BSCB and in the neuropil is much more pronounced (b) Thus, the endothelial cell cytoplasm is heavily infiltrated in nanoparticle treated heat stressed rat (b). The extent of penetration of the tracer in the extracellular compartment of the spinal cord neuropil is much deeper within 4 h (b) compared to the same period in saline treated stressed rat (a). Perivascular edema and myelin degeneration are prominent in the neuropil of heat stressed rats (a, b). However, the tight junctions are intact to lanthanum (b). Bar = a, b = 600 nm. Reproduced with permission after [107]
At the ultrastructural level, the endothelial cells of cerebral microvessels showed widespread exudation of lanthanum in Ag and Cu nanoparticles treated rats after WBH as compared to saline treated animals (Fig. 9.14). Diffusion of lanthanum in the adjacent neuropil is quite common in nanoparticles treated rats after WBH. Whereas, in saline treated group, the electron dense tracer is largely confined to the basal lamina (Fig. 9.14). These observations suggest that the magnitude and intensity of endothelial cell membrane dysfunction to Lanthanum (Mol. Diam. 12 Å) is significantly increased in nanoparticles treated group after WBH as compared to saline treatment [107].
10.3 Exacerbation of Cognitive and Sensory-Motor Dysfunctions in Heat Stress by Nanoparticles
We observed most pronounced disturbances in cognitive and motor functions in nanoparticles treated heat stressed rats as compared to saline treated group (Table 9.6). Cu treatment resulted in most marked decline in rota-rod performance after WBH followed by Ag and Al treatment. On the other hand, Ag nanoparticles treated rats showed most severe decrease in the number of steps taken during a grid-walking session after WBH than Cu and Al treatment (Table 9.6). However, no significant difference in placement error was seen in saline or nanoparticles treated animals after heat stress (Table 9.6).
A marked reduction in the angle of inclined plane in Ag treated rats was seen after WBH (Table 9.6). The distance between hind feet is also decreased in Ag treated stressed rats. However, no difference in stride length is seen in Ag or saline treated animals after WBH (Table 9.6). Interestingly, inclined plane test or foot print analysis did not show any significant differences from saline or Cu or Al treated rats after WBH (Table 9.6). These observations suggest that disturbances in the cognitive and motor functions caused by WBH in animals is markedly influence by nanoparticles depending on their chemistry [107].
10.4 Possible Mechanisms of Nanoparticles Induced Exacerbation of Brain Damage
The possible mechanisms behind exacerbation of hyperthermia-induced brain damage in nanoparticles treated rats are still unclear. However, it appears that profound oxidative stress induced by nanoparticles will further enhance hyperthermia induced free radical formation and release of oxygen radicals leading to exacerbation of brain damage [107, 153]. This is supported by previous studies showing carbon nanoparticles depending on their sizes could aggravate lung inflammation induced by bacterial endotoxins [171]. This exacerbation of inflammatory changes by nanoparticles is mediated through enhanced local expression of proinflammatory cytokines and induction of oxidative stress [13, 107, 171].
In our studies, nanoparticles in normal animals induced mild brain damage that could also probably by induction of oxidative stress by them. Since heat exposure alone induces profound oxidative stress [12, 13, 166–168, 172], additional exposure of nanoparticles treated rats to WBH could reflect the synergistic effects of two inflammatory agents (heat stress and nanoparticles) resulting in potentiation of oxidative tress and the pathological outcome [107, 153].
Alternatively, BBB damage in WBH will result in transport of nanoparticles into the brain fluid microenvironment that could further generate local oxidative stress [173] resulting in higher brain inflammation and cellular damage.
Moreover, nanoparticles within the body or brain fluid microenvironment could induce a higher increase in local cell and tissue temperatures leading to exacerbation of brain damage [107, 153].
Taken together, our novel study demonstrates that nanoparticles could exacerbate BBB disruption and brain pathology following WBH. These findings have immense strategic significance with regard to defense planning and military exercise, particularly in hot environments at various places in the World. It is likely that both military and non-military personals when exposed to nanoparticles from the ambient air at home or abroad are more vulnerable to additional environmental heat load. However, to understand the basic mechanisms of nanoparticles induced exacerbation of brain pathology in stressful situations, additional studies are needed.
11 Pharmacological Manipulation of BBB and Brain Pathology in Stress
Based on the above observations, it is clear that disruption of the BBB in diverse stressful conditions or nanoparticles treatment is associated with brain pathology, cognitive and sensory-motor dysfunction and cell or tissue injuries (see Table 9.6). To further confirm this idea, we examined the effects of several pharmacological agents, neurotrophic factors and antibodies directed against neurochemicals and enzymes on the BBB dysfunction in relation to brain pathology in the above animal models of stress [2–14, 22–28, 49, 105–108, 111, 152–156, 166–168].
11.1 Antibodies Against Injury Factors Attenuate BBB Dysfunction and Brain Pathology
Use of antibodies therapy to neutralize the endogenous effects of their antigens in various disease conditions has been emphasized recently [174–176]. The antibodies are considered much more effective in neutralizing the effects of the neurochemicals in vivo than pharmacological blockade of their receptors [12, 13, 25, 26, 174–176]. Our laboratory took one of the earliest initiatives to study the in vivo effects of antibodies directed against several potential injury factors e.g., neuropeptide dynorphin A 1-17 (Dyn A) [174]; neuronal nitric oxide synthase (nNOS) [175]; serotonin (5-HT) [177, 178] and the tumor necrosis factor-alpha [179] to induce neuroprotective effects or in CNS injuries or in stress conditions [12–14, 24–26, 111].
The antibodies directed against Dyn A, nNOS or 5-HT (1:20 dilution) when administered intracerebroventricularly 30 min before or 30 min after immobilization, forced swimming or heat exposure resulted in marked reductions in the BBB disruption and brain damage (results not shown). On the other hand, when these antibodies were administered either 60 or 90 min after onset of stressful conditions, no reductions in BBB permeability or cell injury were noted (Sharma HS unpublished observations). These observations suggest that antibodies to Dyn A, nNOS and 5-HT if effectively neutralize the harmful effects of their endogenous antigens, i.e., dynorphin, nitric oxide and serotonin within minutes after stress results in neuroprotection (see Table 9.6). Whereas, delayed neutralization of these injury factors with antibodies is ineffective. These findings support the idea that the antibodies could be potential neurotherapeutic agents in minimizing BBB dysfunction in stress to achieve neuroprotection [111].
On the other hand TNF-a antibodies when applied 10–30 min after immobilization, forced swimming or heat exposure are quite effective in reducing the BBB disruption and brain pathology [111, 179]. Whereas, TNF-α antibodies if given 10–30 min before stress, they exacerbated the BBB dysfunction and brain pathology (Sharma HS unpublished observations). These observations are the first to suggest that early neutralization of TNF-α is injurious to the brain [111, 179]. This indicates that the TNF-α has a dual role in inducing BBB disruption and brain pathology (results not shown). Taken together it appears that a reduction in the BBB or BSCB disruptions induced by antibodies appears to be largely responsible for neuroprotection following stress induced brain damage.
11.2 Neurochemical Synthesis Inhibitors Reduce BBB Permeability and Brain Pathology
The neurochemical mediators such as serotonin or prostaglandins are known to induce BBB disruption and brain damage [10, 12, 13, 23, 25, 26, 73, 74, 151, 180–182]. Thus, it is likely that inhibition of prostaglandin or serotonin synthesis prior to CNS insults in stress is neuroprotective (Fig. 9.15). Weused p-chlorophenylalanine (p-CPA) and indomethacin to inhibit serotonin and prostaglandin synthesis, respectively in separate groups of rats [2–14, 22–28, 150, 151, 181–190] and then subjected them to different stressful situations (see Table 9.6). In these animals, the BBB permeability in relation to neural injuries was determined [12, 13, 25, 26, 185].
Ultrastructural changes in the brain at the time of the BBB permeability in stress and neuroprotection by various agents. Ultratstructural changes in stress and their modification with drugs. (A) Pretreatment with p-CPA markedly attenuated cell damage following 8 h immobilization (IMZ) stress (A.a). However, treatment with 5,7-DHT (i.c.v., A.b) or 6-OHDA (i.c.v.; A.c) did not prevent IMZ induced cell changes. Perivascular edema (arrowheads), membrane damage (arrows) and vacuolation (*) are quite common in these drug treated rats. Administration of aminophylline (A.d) or 5-HT (A.e) following 4 h IMZ also induced profound membrane damage and edema. (B) Pretreatment with indomethacin (B.a), p-CPA (B.d), naltrexone (B.e) or nimodipine (B.f) significantly attenuated 4 h heat stress (HS) induced cell damage at the ultrastructural levels compared to the untreated group (B.c). Pretreatment with 6-OHDA (i.c.v., B.b) did not reduce cell damage following HS. On the other hand, heat adapted (HA) rats either reared at high environmental temperature (B. g, h) or chronically exposed to heat stress for 7 days (B. i, j) when subjected to HS did not show any cell damage. (C) Pretreatment with indomethacin (C.b) or p-CPA (C.c) markedly attenuated 30 min forced swimming (FS) induced cell damage (C.a) at the ultrastructural level. Bars: A.a–c = 1 μm; d,e = 0.6 μm; B. a–f = 1 μm; g–h = 0.6 μm; i, j = 0.8 μm; C. a–c = 0. 6 μm. Reproduced with permission after [12]
Pretreatment with p-CPA or indomethacin significantly attenuated BBB disruption in rats subjected to 8 h immobilization, 4 h heat stress or 30 min forced swimming [2–14, 22–28]. Brain edema formation and cell injury were also considerably reduced in these drug treated stressed animals (Table 9.6). These observations suggest that serotonin and prostaglandin participate in BBB disturbances and brain edema formation in stress. Furthermore, a reduction in BBB function with p-CPA or indomethacin is largely responsible for reduction in brain pathology caused by stress.
11.3 Neurochemical Receptor Modulation Influence BBB and Brain Pathology
Several neurochemicals released in stress could influence the BBB function and contribute to brain injury through specific receptor mediated mechanisms [2–14, 22–28, 43–45, 56, 65, 73, 74, 104–112, 150–156, 174–179, 181–192]. Thus, using pharmacological approaches we examined the effects of serotonin, histamine, and opioids receptor blockers on the BBB function in relation to brain damage in stress [2–14, 22–28, 43–45, 56, 65, 73, 74, 150].
Blockade of serotonin 2 (5-HT2) receptors with ketanserin or ritanserin [12, 13, 24–26]; histamine 2 (H2) receptors with cimetidine or ranitidine [12, 13, 24–26, 191, 192]; or multiple opioid receptor blockers with naloxone [12, 13, 144] significantly attenuated heat stress induced BBB disturbances and CNS pathology. However, blockade of histamine 1 (H1) receptor with mepyramine [12, 13, 181–192] or a combination of H1 and 5-HT2 receptor blockers cyproheptadine [2–14, 22–28] did not reduce BBB or cell injury in stressful situations (See Table 9.6; Fig. 9.15). Interestingly, cyproheptadine and mepyramine treatment exacerbated BBB dysfunction and brain injury in stress [12, 24–26]. These observations indicate that blockade of 5-HT2, H2, and multiple opioid receptors before CNS insults are neuroprotective in nature. Whereas, antagonism of H1 or a combination of H1 and 5-HT2 receptor before stress may have neurodestructive effects. Taken together our results show that the BBB disruption is instrumental in inducing in cell and tissue injuries in the brain [13].
11.4 Antioxidants Attenuate BBB Breakdown and Brain Pathology
Stress caused by various environmental or mental factors, nanoparticles, trauma and psychostimulant abuse induce oxidative stress and formation of free radicals and lipid peroxidation in the CNS [13, 166–168]. Generation of free radicals and lipid peroxidation causes neuronal, glial and endothelial cell membrane damages [12, 13, 24, 25, 166–168]. Disruption of endothelial cell membrane will induce BBB breakdown leading to brain edema formation and cell injury. Thus, antioxidants either capable to inhibit lipid peroxidation or are scavengers of free radicals would induce neuroprotection caused by wide variety of CNS insults [12, 13, 166–168, 185, 193]. However the role of antioxidants in BBB disruption in CNS injuries is still not well known. Our laboratory was the first to examine the effects of antioxidants on BBB dysfunction in a wide variety of stressful situation as well as against nanoparticles exposure [2–14, 22–28, 43–45, 56, 65, 73, 74, 104–112, 150–156, 174–179, 181–192].
Using potent inhibitor of lipid peroxidation (H-290/51) [12, 13]; or scavengers of free radicals (EGB-761 and BN 22023) [24–26, 194, 195] we found that antioxidants are capable to attenuate BBB disruption and brain pathology in various stress models (see Table 9.6) [105–107, 153]. Thus, pretreatment with H-290/51 significantly attenuated BBB permeability, edema formation and cell damage in heat stress when administered 30 min before heat exposure [12, 13, 25, 26, 185]. Interestingly, the compound was also effective in reducing BBB disruption and brain pathology in nanoparticles (Ag, Cu or Al) treated rats (Table 9.6) [107, 153]. These observations suggest that inhibition of lipid peroxidation in stress or nanoparticle administration prevents BBB disruption and cell injury.
Similarly, daily treatment with EGB-761 or BN22123 separately in rats for 5 days reduced the BBB disruption and brain pathology in heat stress [12, 13]. However, the magnitude and intensity of BBB disruption and brain pathology were much less pronounced than the H-290/51 treatment [166–168]. This indicates that the compounds able to inhibit lipid peroxidation have superior neuroprotective ability than those drugs that are capable to scavenge the free radicals after their generation [153]. These observations strongly indicate a close correlation between BBB disruption and pathological outcome in various kinds of CNS insults.
11.5 Biogenic Amine Neurotoxins Exacerbate BCNSB Breakdown and CNS Pathology
The microvessels of the brain and spinal cord are innervated with serotoninergic, histaminergic, and catecholaminergic nerve fibers [14, 21, 35]. These nerve fibers control the vascular reactivity of neurochemicals and thus may influence the BBB function [35]. We examined the influence of serotoninergic and catecholaminergic nerve terminal degeneration on the BBB disruption in stress in relation to brain pathology.
Our observations show that destruction of central 5-HT neurons with 5,7-dihydroxytryptamine (5,7-DHT) significantly enhanced the BBB disruption to Evans blue albumin and radioiodine in the rat brains following immobilization, forced swimming or heat stress [2–24, 22–28]. These observations suggest that destruction of central serotoninergic nerve terminals enhances the BBB leakage and thus exacerbate brain pathology [2–14, 22–28].
Interestingly, exacerbation of BBB permeability, brain edema and brain pathology was also observed in rats subjected heat stress after destruction of either central or peripheral catecholaminergic nerve terminals with 6-hydroxydopamine (6-OHDA) [2–14] (Sharma HS, unpublished observation).
Taken together it appears that serotoninergic and catecholaminergic nerve terminals regulate BBB function in stress. Thus, chemical degeneration of serotoninergic or catecholaminergic nerve terminals aggravate BBB dysfunction causing enhanced brain pathology and support the hypothesis that the BBB disruption is instrumental in cell and tissue injury following diverse kinds of CSN insults.
12 Possible Mechanisms of Stress Induced BBB Dysfunction and Brain Pathology
Based on our neuropharmacological investigations, it appears that alterations in neurochemicals following stress or nanoparticle administration are responsible for the BBB breakdown. Depending on the magnitude and intensity of stressors, several neurochemicals, i.e., serotonin, prostaglandin, histamine, opioids, amino acid neurotransmitters and other injury factors are released in the CNS as well as in the periphery [2–14, 22–28, 166–168]. These neurochemicals then will act on the luminal and abluminal sides of the cerebrovascular endothelium [14, 21, 35] inducing a cascade of effects leading to alteration in the cell membrane permeability [21, 25, 26]. These neurochemicals could also induce oxidative stress, lipid peroxidation, and generation of free radicals in the CNS that could directly or indirectly affects BBB dysfunction leading to cell damage. Reduction in BBB disruption by blockade of serotonin, prostaglandin, histamine and opioid effects in various kinds of stressors are in line with this hypothesis [12, 21, 24–26, 28, 105, 107, 111, 150, 152–156, 185].
These neurochemicals after binding to their receptors located on microvessels in both the luminal and the abluminal surfaces could induce intracellular signaling, e.g., stimulation of prostaglandins, nitric oxide synthase (NOS), cAMP or cGMP synthesis and/or release [12, 13, 22, 25, 26, 196]. The CNS capillaries contain all necessary enzymes for synthesis and catabolism of prostaglandins, NOS as well as cAMP [13, 22]. Local accumulation of prostaglandins, cGMP or cAMP in cerebral capillaries induces marked vasodilatation and an increases vesicular transport [14, 21, 22, 150]. Obviously, various pharmacological agents could influence this mode of tracer transport. Alteration in the cell membrane transport caused by cAMP and cGMP could also account for increased tracer transfer across the BBB [13, 21, 197–200]. Taken together, our observations suggest that the BBB function strictly regulates the cell and tissue injury in various CNS insults or diseases.
13 General Conclusion
In conclusion, our studies demonstrate that the BBB is an important regulator of the brain function in physiological and pathological conditions. Thus, a normal BBB is always responsible for physiological regulation of fluid environment of the brain and spinal in order to maintain their good health. However, leaky BBB caused by a variety of endogenous (neurochemical, alterations, diseases) or exogenous (heat, nanoparticles, forced stressful situations) agents could lead to brain pathology. Damage to specific brain or spinal cord areas in such disease or stressful situations are primarily responsible for deteriorating cognitive, sensory and motor functions. Thus, maintenance of a healthy BBB is the key to maintain good health of the CNS. Neuropharmacological agents including neurochemical synthesis inhibitors, receptor modulators or antibodies directed against neurodestructive elements are able to attenuate BBB dysfunction in a variety of stress situations. A reduction in BBB disruption clearly leads to brain protection in such situations and improve cognitive and sensory motor functions. Taken together, these observations clearly support the idea that the BBB is the gateway to neurodegeneration and neuroprotection.
14 Future Perspectives
With advent of nanotechnologies and development of nanomedicine, it remains to be seen how nano-drug delivery could enhance neuroprotection in stress induced brain diseases. Since nanoparticles by itself induce neurotoxicity and exacerbation of brain pathology, further research is needed to see whether nanoparticles could also influence the neuroprotective efficacy of drugs in brain diseases. It is utmost importance for pharmacotherapeutic agents to reduce nanoparticles induced enhanced brain damage in stressful situations. Thus, exploration of suitable therapeutic strategies using nano-drug delivery of various antibodies, receptors blockers or synthesis inhibitors are needed to reduce nanoparticles induces exacerbation of brain pathology and the BBB dysfunction. Our laboratory is currently engaged to identify novel therapeutic agents that can attenuate nanoparticles induced enhanced brain damage in a variety of traumatic and stressful situation in different animals models.
Abbreviations
- BBB:
-
Blood-brain barrier
- bbb:
-
brain-blood-barrier
- nNOS:
-
neuronal nitric oxide synthase
- TNF-α:
-
Tumor necrosis factor alpha
- HO-2:
-
Hemeoxygenase-2
- IPS:
-
Information processing system
- GAS:
-
General adaptation syndrome
- CRF:
-
Corticotrophin releasing factor
- ACTH:
-
Adrenocorticotrophic hormone
- HPA:
-
Hypothalamus pituitary adrenal axis
- TRH:
-
Thyrotrophin releasing hormone
- PVN:
-
Para ventricular nucleaus
- DHEAS:
-
dehydroepiandrosterone sulfate
- WN-25:
-
West Nile virus
- SFV-A7:
-
Semliki Forest virus
- EBA:
-
Evans blue albumin
- PS:
-
Paradoxical sleep
- SWS:
-
Slow wave sleep
- ROS:
-
Reactive oxygen species
- WBH:
-
whole body hyperthermia
- BSCB:
-
Blood-spinal cord barrier
- Dyn:
-
Dynorphin A
- 5-HT:
-
5-hydroxytryptamine
- CNS:
-
Central nervous system
- p-CPA:
-
para-Cholorophenylalanine
- H1:
-
Histamine H1 receptor
- H2:
-
Histamine H2 receptor
- 5,7-DHT:
-
5,7-dihydroxytryptamine
- 6-OHDA:
-
6-hydroxydopamine
References
Ehrlich P. Das Sauerstoff-Bedürfniss des Organismus: eine farbenanalytische Studie. Hirschwald, Berlin; 1885
Sharma HS, Dey PK. Impairment of blood-brain barrier (BBB) in rat by immobilization stress: role of serotonin (5-HT). Indian J Physiol Pharmacol 1981 Apr–Jun; 25(2):111–122
Sharma HS, Dey PK. Role of 5-HT on increased permeability of blood-brain barrier under heat stress. Indian J Physiol Pharmacol 1984 Oct–Dec; 28(4):259–267
Sharma HS. Blood-Brain Barrier in Stress, Ph D Thesis, Banaras Hindu University, Varanasi, India, 1982; pp. 1–85
Sharma HS, Dey PK. Influence of long-term immobilization stress on regional blood-brain barrier permeability, cerebral blood flow and 5-HT level in conscious normotensive young rats. J Neurol Sci 1986; 72:61–76
Sharma HS, Dey PK. Influence of long-term acute heat exposure on regional blood-brain barrier permeability, cerebral blood flow and 5-HT level in conscious normotensive young rats. Brain Res 1987; 424:153–162
Sharma HS, Dey PK. EEG changes following increased blood-brain barrier permeability under long-term immobilization stress in young rats. Neurosci Res 1988; 5:224–239
Sharma HS, Cervós-Navarro J, Dey PK Acute heat exposure causes cellular alteration in cerebral cortex of young rats. NeuroReport 1991; 2:155–158
Sharma HS, Nyberg F, Cervós-Navarro J, Dey PK Histamine modulates heat stress induced changes in blood-brain barrier permeability, cerebral blood flow, brain oedema and serotonin levels: an experimental study in conscious young rats. Neuroscience 1992; 50:445–454
Sharma HS, Westman J, Cervós-Navarro J, Dey PK, Nyberg F Opioid receptor antagonists attenuate heat stress-induced reduction in cerebral blood flow, increased blood-brain barrier permeability, vasogenic brain edema and cell changes in the rat. Ann NY Acad Sci 1997; 813:559–571
Sharma HS. Pathophysiology of blood-brain barrier, brain edema and cell injury following hyperthermia: New role of heat shock protein, nitric oxide and carbon monoxide. an experimental study in the rat using light and electron microscopy, Acta Universitatis Upsaliensis 1999; 830:1–94
Sharma HS. Blood-brain and spinal cord barriers in stress. In: Sharma HS, Westman J (eds) The Blood-Spinal Cord and Brain Barriers in Health and Disease, Elsevier Academic Press, San Diego, 2004; pp. 231–298
Sharma HS. Blood-central nervous system barriers. A gateway to neurodegeneration, neuroprotection and neuroregeneration. Hand Book of Neurochem Mol Neurobiol, Vol. 24, Ch. 11, Springer, Berlin, New York, 2009; pp. 163–209
Rapoprt SI. Blood-Brain Barrier in Physiology and Medicine. Raven Press, New York; 1976
Bradbury MW. The Concept of a Blood Brain Barrier. Chicester, UK; 1979
Brightman MW, Reese TS. Junctions between intimately apposed cell membranes in the vertebrate brain. J Cell Biol 1969; 4:648–677
Majno G, Palade GE. Studies on inflammation. 1. The effect of histamine and serotonin on vascular permeability: an electron microscopic study. J Biophys Biochem Cytol. 1961 Dec; 11:571–605
Brightman MW. Morphology of blood-brain interfaces. Exp Eye Res. 1977; 25(Suppl):1–25. Review
Brightman MW. The brain’s interstitial clefts and their glial walls. J Neurocytol. 2002 Sep–Nov; 31(8–9):595–603. Review
Sharma HS. New perspectives for the treatment options in spinal cord injury. Expert Opin Pharmacother 2008 Nov; 9(16):2773–2800. Review
Sharma H S, Westman J. The Blood-Spinal Cord and Brain Barriers in Health and Disease, Academic Press, San Diego, USA, 2004; pp. 1–617 (Release date: Nov. 9, 2003)
Sharma H S, Alm P. Role of nitric oxide on the blood-brain and the spinal cord barriers. In: Sharma HS, Westman J (eds) The Blood-Spinal Cord and Brain Barriers in Health and Disease, Elsevier Academic Press, San Diego, 2004; pp. 191–230
Sharma HS, Westman J, Nyberg F. Pathophysiology of brain edema and cell changes following hyperthermic brain injury. In: Sharma HS, Westman J (eds) Brain Functions in Hot Environment, Progress in Brain Research, 1998; 115:351–412
Sharma HS, Westman J, Cervós-Navarro J, Dey PK, Nyberg F. Blood-brain barrier in stress: a gateway to various brain diseases. In: Levy A, Grauer E, Ben-Nathan D, de Kloet ER (eds) New Frontiers of Stress Research: Modulation of Brain Function, Harwood Academic Publishers Inc., Amsterdam, 1998; pp. 259–276
Sharma HS. Influence of serotonin on the blood-brain and blood-spinal cord barriers. In: Sharma HS, Westman J (eds) The Blood-Spinal Cord and Brain Barriers in Health and Disease, Elsevier Academic Press, San Diego, 2004; pp. 117–158
Sharma HS. Histamine influences the blood-spinal cord and brain barriers following injuries to the central nervous system. In: Sharma HS, Westman J (eds) The Blood-Spinal Cord and Brain Barriers in Health and Disease, Elsevier Academic Press, San Diego, 2004; pp. 159–190
Sharma HS. Selective neuronal vulnerability, blood-brain barrier disruption and heat shock protein expression in stress induced neurodegeneration. Invited Review: In: Sarbadhikari SN (ed) Depression and Dementia: Progress in Brain Research, Clinical Applications and Future Trends , Nova Science Publishers Inc., New York, 2005; pp. 97–152
Sharma HS. Neurotrophic factors in combination: a possible new therapeutic strategy to influence pathophysiology of spinal cord injury and repair mechanisms. Curr Pharm Des 2007; 13(18):1841–1874. Review
Bradbury MWB. Physiology and pharmacology of the blood-brain barrier. Handbook Exp Pharmacol 1990; 103: 1–450, Springer, Heidelberg
Johansson BB, Auer LM. Neurogenic modification of the vulnerability of the blood-brain barrier during acute hypertension in conscious rats. Acta Physiol Scand 1983 Apr; 117(4):507–511
Johansson BB. The blood-brain barrier and cerebral blood flow in acute hypertension. Acta Med Scand Suppl 1983; 678:107–112
Johansson BB, Auer LM, Linder LE. Phenothiazine-mediated protection of the blood-brain barrier during acute hypertension. Stroke 1982 Mar–Apr; 13(2):220–225
Johansson BB. Cerebral vascular bed in hypertension and consequences for the brain. Hypertension. 1984 Nov–Dec; 6(6 Pt 2):III81–III86
Johansson BB. Hypertension mechanisms causing stroke. Clin Exp Pharmacol Physiol 1999 Jul; 26(7):563–565. Review
Edvinsson L, Johansson BB, Larsson B, MacKenzie ET, Skärby T, Young AR. Calcium antagonists: effects on cerebral blood flow and blood-brain barrier permeability in the rat. Br J Pharmacol 1983 May; 79(1):141–148
Larsson B, Skärby T, Edvinsson L, Hardebo JE, Owman C. Vincristine reduces damage of the blood-brain barrier induced by high intravascular pressure. Neurosci Lett 1980 Apr; 17(1–2):155–159
Nag S, Harik SI. Cerebrovascular permeability to horseradish peroxidase in hypertensive rats: effects of unilateral locus ceruleus lesion. Acta Neuropathol 1987; 73(3):247–253
Nag S. Cerebral endothelial plasma membrane alterations in acute hypertension. Acta Neuropathol 1986; 70(1):38–43
Nag S. Cerebral changes in chronic hypertension: combined permeability and immunohistochemical studies. Acta Neuropathol 1984; 62(3):178–184
Nag S. Cerebral endothelial surface charge in hypertension. Acta Neuropathol 1984; 63(4):276–281
Nag S, Robertson DM, Dinsdale HB. Intracerebral arteriolar permeability to lanthanum. Am J Pathol 1982 Jun; 107(3):336–341
Nag S, Robertson DM, Dinsdale HB. Quantitative estimate of pinocytosis in experimental acute hypertension. Acta Neuropathol 1979 Apr 12; 46(1–2):107–116
Sharma HS, Johanson CE. Blood-cerebrospinal fluid barrier in hyperthermia.Prog Brain Res 2007; 162:459–478. Review
Sharma HS, Johanson CE. Intracerebroventricularly administered neurotrophins attenuate blood cerebrospinal fluid barrier breakdown and brain pathology following whole-body hyperthermia: an experimental study in the rat using biochemical and morphological approaches. Ann NY Acad Sci. 2007 Dec; 1122:112–129
Sharma HS, Duncan JA, Johanson CE. Whole-body hyperthermia in the rat disrupts the blood-cerebrospinal fluid barrier and induces brain edema. Acta Neurochir Suppl 2006; 96:426–431
Selye H. A syndrome produced by diverse noccuous agents. Nature (Lond) 1936; 138:32
Chrousos GP, Gold PW. The concept of stress and stress system disorders: Overview of physical and behavioral homeostasis. JAMA 1992; 267:1244–1252
Friedman MJ, Charbey DS, Deutch AY. Neurobiological and Clinical Consequences of Stress, Lipincott-Raven, Philadelphia; 1995
Sharma HS, Westman J. Brain Functions in Hot Environment, Progress in Brain Research, 115, Elsevier, Amsterdam, 1998; pp. 1–516
Selye H. Stress in Health and Disease. Butterworths, London; 1976
Foa EB, Zinbarg R, Olasov-Rothbaum B. Uncontrollability and unpredictability in post-traumatic stress disorder: an animal model. Psychol Bull 1992; 112:218–238
Gazzaniga MS. The Cognitive Neurosciences. MIT Press, Cambridge, MA; 1995
McEwen BS, Sapolsky RM. Stress and cognitive function. Curr Opin Neurobiol 1995; 5:205–217
Sapolsky RM. Stress, the aging brain, and the mechanisms of neuronal death. MIT Press, Cambridge, MA; 1992
Sapolsky RM. Why stress is bad for your brain. Science 1996; 273:749–750
Sharma HS, Westman J. Pathophysiology of hyperthermic brain injury. Current concepts, molecular mechanisms and pharmacological strategies. Research in Legal Medicine Vol. 21 Hyperthermia, Burning and Carbon Monoxide, Oehmichen M (ed) Lübeck Medical University Publications, Schmidt-Römhild Verlag, Lübeck, Germany, 2000; pp. 79–120
McEwen BS, Stellar E. Stress and the individual. Mechanisms leading to disease. Arch Intern Med 1993; 153:2093–2101
Kathol RG, Jaeckle RS, Lopez JF, Meller WH. Consistent reduction of ACTH responses to stimulation with CRH, vasopressin and hypoglycaemia in patients with major depression. Br J Psychiatry 1989; 155:468–478
Charney DS, Deutch AY, Krystal JH, Southwick SM, Davis M. Psychobiologic mechanisms of posttraumatic stress disorder. Arch Gen Psychiatry 1993; 50:295–305
Landfield PW, Eldridge JC. The glucocorticoid hypothesis of brain aging and neurodegeneration: recent modifications. Acta Endocrinol (Copenh) 1991; 125(Suppl 1):54–64
Herman JP, Cullinan WE. Neurocircuitry of stress: central control of the hypothalamo-pituitary-adrenocortical axis. Trends Neurosci 1997; 20:78–84
Garthwaite J. Glutamate, nitric oxide and cell-cell signalling in the nervous system. Trends Neurosci 1991; 14:60–67
Bronstein JM, Farber DB, Wasterlain CG. Regulation of type-II calmodulin kinase: functional implications. Brain Res Rev 1993; 18(1):135–147
Hughes P, Dragunow M. Induction of immediate-early genes and the control of neurotransmitter-regulated gene expression within the nervous system. Pharmacol Rev 1995; 47(1):133–178
Sharma HS, Westman J. The heat shock proteins and hemeoxygenase response in central nervous system injuries. In: Sharma HS, Westman J (eds) The Blood-Spinal Cord and Brain Barriers in Health and Disease, Elsevier Academic Press, San Diego, 2004; pp. 329–360
Abdul-Rahman A, Dahlgren N, Johansson BB, Siesjö BK. Increase in local cerebral blood flow induced by circulating adrenaline: involvement of blood-brain barrier dysfunction. Acta Physiol Scand 1979; 107:227–232
Abercrombie ED, Jacobs BL. Single-unit response of noradrenergic neurons in the locus coeruleus of freely moving cats. II. Adaptation to chronically presented stressful stimuli. J Neurosci 1987; 7(9):2844–2848
Cullinan WE, Herman JP, Battaglia DF, Akil H, Watson SJ. Pattern and time course of immediate early gene expression in rat brain following acute stress. Neuroscience 1995; 64(2):477–505
Smith MA, Brady LS, Glowa J, Gold PW, Herkenham M. Effects of stress and adrenalectomy on tyrosine hydroxylase mRNA levels in the locus coeruleus by in situ hybridization. Brain Res 1991; 544(1):26–32
Uno H, Tarara R, Else JG, Suleman MA, Sapolsky RM. Hippocampal damage associated with prolonged and fatal stress in primates. J Neurosci 1989; 9:1705–1711
McEwen BS. Stress and hippocampal plasticity. Annu Rev Neurosci 1999; 22:105–122
Magarinos AM, McEwen BS, Flugge G, Fuchs E. Chronic psychological stress causes apical dendritic atrophy of hippocampal CA3 pyramidal neurons in subordinate tree shrews. J Neurosci 1996; 16:3534–3540
Sharma HS, Westman J, Nyberg F, Cervós-Navarro J, Dey PK. Role of serotonin and prostaglandins in brain edema induced by heat stress. An experimental study in the rat. Acta Neurochirurgica (Suppl) 1994; 60:65–70
Sharma HS, Nyberg F, Olsson Y. Topical application of dynorphin antibodies reduces edema and cell changes in traumatised rat spinal cord. Regulatory Peptide (Supplement) 1994; 1:S91–S92
Gazzaley AH, Weiland NG, McEwen BS, Morrison JH. Differential regulation of NMDAR1 mRNA and protein by estradiol in the rat hippocampus. J Neurosci 1996; 16:6830–6838
Popov VI, Bocharova LS, Bragin AG. Repeated changes of dendritic morphology in the hippocampus of ground squirrels in the course of hibernation. Neuroscience 1992; 48:45–51
Wooley CS, Gould E, McEwen BS. Exposure to excess glucocorticoids alters dendritic morphology of adult hippocampal pyramidal neurons. Brain Res 1990; 531:225–231
Watanabe Y, Gould E, McEwen BS. Stress induces atrophy of apical dendrites of hippocampal CA3 pyramidal neurons. Brain Res 1992; 588:341–345
Lindvall O, Kokaia Z, Bengzon J, Elmer E, Kokaia M. Neurotrophins and brain insults. Trends Neurosci 1994; 17:490–496
Zafra F, Lindholm D, Castren E, Hartikka J, Thoenen H. Regulation of brain-derived neurotrophic factor and nerve growth factor mRNA in primary cultures of hippocampal neurones and astrocytes. J Neurosci 1992; 12:4793–4799
Smith MA. The role of brain-derived neurotrophic factor in the central effects of stress. In: Levy A, Grauer E, Ben-Nathan D, de Kloet E R (eds) New frontiers in Stress Research. Modulation of Brain Function, Harwood Academic Publishers, The Netherlands, 1998; pp. 53–57
Smith MA, Makino S, Kvetnansky R, Post RM. Stress and glucocorticoid affect the expression of brain-derived neurotrophic factor and neurotrophin-3 mRNA levels in the hippocampus. J Neurosci 1995; 15:1768–1777
Sofroniew MV, Cooper JD, Svendsen CN, Crossman P, Ip NY, Lindsay RM, Zafra F, Lindholm D. Atrophy but not death of adult septal cholinergic neurones after ablation of target capacity to produce mRNAs for NGF, BDNF and NT3. J Neurosci 1993; 13:5263–5276
Nibuya M, Morinobu S, Duman RS. Regulation of BDNF and trkB in rat brain by chronic electroconvulsive seizures and antidepressant drug treatments. J Neurosci 1995; 15:7539–7547
Smith MA, Makino S, Kim S-Y, Kvetnansky R. Stress increases brain-derived neurotrophic factor mRNA in the hypothalamus and pituitary. Endocrinology 1995; 136:3743–3750
Bremner JD, Scott TM, Delancy RC, Southwick SM, Mason JW, Johnson DR, Innis RB, McCarthy G, Charney DS. Deficits in short-term memory in posttraumatic stress disorder. Am J Psychiat 1993; 150:1015–1019
Diamond DM, Fleshner M, Ingersoll N, Rose GM. Psychological stress impairs spatial memory: relevance to electrophysiological studies of hippocampal function. Behav Neurosci 1996; 110:661–672
Diamond DM, Ingersoll N, Branch BJ, Mesches MH, Coleman-Mesches K, Fleshner M. Stress impairs cognitive and electrophysiological measures of hippocampal function. In: Levy A, Grauer E, Ben-Nathan D, de Kloet ER (eds) New frontiers in Stress Research. Modulation of Brain Function, Harwood Academic Publishers, The Netherlands, 1998; pp. 117–126
Cahill L, Prins B, Weber M, McHaugh JL. b-adrenergic activation and memory for emotional events. Nature 1994; 371:702–704
Kalimi M, Shafagoj Y, Loria R, Padgett D, Regelson W. Anti-glucocorticoid effects of dehydroepiandrosterone (DHEA). Mol Cell Biochem 1994; 131:99–104
Diamond DM, Branch BJ, Coleman-Mesches K, Mesches HM, Fleshner M. DHEAS enhances spatial memory and hippocampal primed burst potentiation. Soc Neurosci Abstr 1996; 22:140
Diamond DM, Branch BJ, Fleshner M. The neurosteroid dehydroepiandrosterone sulfate (DHEAS) enhances hippocampal primed burst, but not long-term potentiation. Neurosci Lett 1996; 202:204–208
Rasmussen AF, March JT, Brill NQ. Increased susceptibility to herpes simplex in mice subjected to avoidance-learning stress or restrain. Proc Soc Exp Biol Med 1957; 96:183–189
Feng N, Pagniano R, Tovar CA, Bonneaue RH, Glasser R, Sheridan JF. The effect of restraint stress on the kinetics, magnitude, and isotype of the humoral immune response to influenza virus infection. Brain Behav Immun 1991; 5:370–382
Herman JP, Adams D, Prewitt C. Regulatory changes in neuroendocrine stress-integrative circuitry produced by a variable stress paradigm. Neuroendocrinology 1995; 61(2):180–190
Ben-Nathan D, Lustig S, Daneberg H. Stress-induced neuroinvasiveness of a neurovirulent non invasive Sindbis virus in cold or isolation subjected mice. Life Sci 1991; 48:1493–1500
Ben-Nathan D, Kobiler D, Loria RM, Lustig S. Stress-induced central nervous system penetration by non-invasive attenuated encephalitis viruses. In: Levy A, Grauer E, Ben-Nathan D, de Kloet ER (eds) New frontiers in Stress Research. Modulation of Brain Function, Harwood Academic Publishers, The Netherlands, 1998; pp. 277–2283
Friedman SB, Glasgow LA, Ader R. Differential susceptibility to viral agent in mice housed alone or in group. Psychosom Med 1970; 32:285–299
Sheridan JF, Dobbs C, Brown D, Swilling B. Psychoneuroimmunology: Stress effects on pathogenesis and immunity during infection. Clin Microbiol Rev 1994; 7:202–212
Sharp FR, Sagar SM, Hicks K, Lowenstein D, Hisanaga K. c-fos mRNA, Fos, and Fos-related antigen induction by hypertonic saline and stress. J Neurosci 1991; 11(8):2321–2331
Cohen S, Williamson GM. Stress and infectious disease in human. Psychol Bull 1991; 109:5–24
Dantzer R, Kelley KW. Stress and immunity: An integrated view of the relationships between the brain and immune system. Life Sci 1989; 44:1995–2008
Angel C. Starvation, stress and the blood-brain barrier. Dis Nerv Syst 1969; 30:94–97
Sharma HS, Westman J, Navarro JC, Dey PK, Nyberg F. Probable involvement of serotonin in the increased permeability of the blood-brain barrier by forced swimming. An experimental study using Evans blue and 131I-sodium tracers in the rat. Behav Brain Res 1995 Dec 14; 72(1–2):189–196
Sharma HS. Methods to produce hyperthermia-induced brain dysfunction. Prog Brain Res 2007; 162:173–199. Review
Sharma HS. Interaction between amino acid neurotransmitters and opioid receptors in hyperthermia-induced brain pathology. Prog Brain Res 2007; 162:295–317. Review
Sharma HS, Sharma A. Nanoparticles aggravate heat stress induced cognitive deficits, blood-brain barrier disruption, edema formation and brain pathology. Prog Brain Res 2007; 162:245–273. Review
Sharma HS. Nanoneuroscience: emerging concepts on nanoneurotoxicity and nanoneuroprotection. Nanomedicine 2007 Dec; 2(6):753–758. Review
Sharma HS. Post-traumatic application of brain-derived neurotrophic factor and glia-derived neurotrophic factor on the rat spinal cord enhances neuroprotection and improves motor function. Acta Neurochir Suppl 2006; 96:329–334
Sharma HS. Neurobiology of hyperthermia. Prog Brain Res 2007; 162:1–523, Elsevier, Amsterdam
Sharma HS, Sharma A. Antibodies As Promising Novel Neuroprotective Agents in the Central Nervous System Injuries. Central Nervous System Agents in Medicinal Chemistry (Formerly Current Medicinal, Vol. 8, No. 3, Sept 2008, pp. 143–169(27). DOI: 10.2174/187152408785699640
Sharma HS, Dey PK. Influence of heat and immobilization stressors on the permeability of blood-brain and blood-CSF barriers. Indian J Physiol Pharmacol 22, Supplement II, 1978; 59–60
Sapolsky RM, Zola-Morgan S, Squire LR. Inhibition of glucocorticoid secretion by the hippocampal formation in the primate. J Neurosci 1991; 11(12):3695–3704
Karst H, Wadman WJ, Joëls M. Corticosteroid receptor-dependent modulation of calcium currents in rat hippocampal CA1 neurons. Brain Res 1994; 649:234–242
Chaouloff F. Physiopharmacological interactions between stress hormones and central serotonergic systems. Brain Res Rev 1993; 18(1):1–32
Porsolt RD, Bertin A, Jalfre M. Behavioral despair in mice: a primary screening test for antidepressants. Arch Int Pharmacodyn Ther 1977; 229(2):327–336
Porsolt RD, Bertin A, Blavet N, Deniel M, Jalfre M. Immobility induced by forced swimming in rats: effects of agents which modify central catecholamine and serotonin activity. Eur J Pharmacol 1979; 57(2–3):201–210
Kofman O, Levin U, Alpert C. Lithium attenuates hypokinesia induced by immobilization stress in rats. Prog Neuropsychopharmacol Biol Psychiatry 1995; 19(6):1081–1090
Miyazato H, Skinner RD, Garcia-Rill E. Locus coeruleus involvement in the effects of immobilization stress on the p13 midlatency auditory evoked potential in the rat. Prog Neuropsychopharmacol Biol Psychiatry 2000; 24(7):1177–1201
Belova TI, Jonsson G. Blood-brain barrier permeability and immobilization stress. Acta Physiol Scand 1982; 116:21–29
Dvorská I, Brust P, Hrbas P, Rühle HJ, Barth T, Ermisch A. On the blood-brain barrier to peptides: effects of immobilization stress on regional blood supply and accumulation of labelled peptides in the rat brain. Endocr Regul 1992; 26(2):77–82
Esposito P, Gheorghe D, Kandere K, Pang X, Conally R, Jacobson S, Theoharides TC. Acute stress increase permeability of the blood-brain barrier through activation of mast cells. Brain Res 2001; 888:117–127
Esposito P, Chandler N, Kandere K, Basu S, Jacobson S, Connolly R, Tutor D, Theoharides TC. Corticotropin-releasing hormone and brain mast cells regulate blood-brain barrier permeability by acute stress. J Pharmacol Exp Thera 2002; 303:1061–1066
Ohata M, Fredericks WR, Sundaram U, Rapoport SI. Effects of immobilization stress on regional cerebral blood flow in the conscious rat. J Cereb Blood Flow Metab 1981; 1(2):187–194
Ohata M, Takei H, Fredericks WR, Rapoport SI. Effects of immobilization stress on cerebral blood flow and cerebrovascular permeability in spontaneously hypertensive rats. J Cereb Blood Flow Metab 1982; 2(3):373–379
Sharma HS, Dey PK. Increased permeability of blood-brain barrier (BBB) in stress: Blockade by p-CPA pretreatment. Indian J Physiol Pharmacol 1980; 24(Suppl I): 423–424
Lalonde R. Acquired immobility response in weaver mutant mice. Exp Neurol 1986; 94(3):808–811
Sharma HS, Cervós-Navarro J, Dey PK. Increased blood-brain barrier permeability following acute short-term forced-swimming exercise in conscious normotensive young rats. Neurosci Res 1991; 10:211–221
Miller WR, Seligman EP. Learned helplessness, depression and the perception of reinforcement. Behav Res Ther 1976; 14:7–17
Maier SF, Watkins LR, Fleshner M. Psychoneuroimmunology: the interface between behaviour, brain and immunity. Amer Psych 1994; 49:1001–1018
Van de Kar LD, Piechowski RA, Rittenhouse PA, Gray TS. Amygdaloid lesions: differential effect on conditioned stress and immobilization-induced increases in corticosterone and renin secretion. Neuroendocrinology 1991; 54(2):89–95
Petty F, Kramer G, Wilson L, Jordan S. In vivo serotonin release and learned helplessness. Psychiatry Res 1994; 52:285–293
Kupfer DJ. REM latency: a psychobiological marker for primary depressive disease. Biol Psychiatry 1976; 11: 159–174
Kupfer DJ, Spiker DG, Coble PA, Shaw DH. Electroencephalographic sleep recordings and depression in the elderly. J Am Geriatr Soc 1978 Feb; 26(2):53–57
Rotenberg VS, Boucsein W Adaptive versus maladaptive emotional tension. Genetic, Social and General Psychology Monographs 1993; 119:209–232
Maloney KJ, Mainville L, Jones BE. Differential c-Fos expression in cholinergic, monoaminergic, and GABAergic cell groups of the pontomesencephalic tegmentum after paradoxical sleep deprivation and recovery. J Neurosci 1999; 19(8):3057–3072
Maloney KJ, Mainville L, Jones BE. c-Fos expression in GABAergic, serotonergic, and other neurons of the pontomedullary reticular formation and raphe after paradoxical sleep deprivation and recovery. J Neurosci 2000; 20(12):4669–4679
Mendelson WB. The flower pot technique of rapid eye movement (REM) sleep deprivation. Pharmacol Biochem Behav 1974; 2:553–556
Centers for Disease Control and Prevention (CDC). Heat-related deaths – United States, 1999–2003. MMWR Morb Mortal Wkly Rep. 2006 Jul 28; 55(29):796–798
Department of Health. Heatwave—plan for England—protecting health and reducing harm from extreme heat and heatwaves. London: DoH, 2004. http://www.dh.gov.uk/PublicationsAndStatistics/Publications/PublicationsPolicyAndGuidance/PublicationsPolicyAndGuidanceArticle/fs/en?CONTENT_ID=4086874&chk=opuHhJ (published 2004, superseded by 2005 edition; last accessed 10 Aug 2006)
Keatinge WR, Donaldson GC. The impact of global warming on health and mortality. South Med J 2004 Nov; 97(11):1093–1099. Review
Smoyer KE, Rainham DG, Hewko JN. Heat-stress-related mortality in five cities in Southern Ontario: 1980–1996. Int J Biometeorol 2000 Nov; 44(4):190–197
Sharma HS. Heat-related deaths are largely due to brain damage. Indian J Med Res 2005 May; 121(5):621–623
Sharma HS. Hyperthermia influences excitatory and inhibitory amino acid neurotransmitters in the central nervous system. An experimental study in the rat using behavioural, biochemical, pharmacological, and morphological approaches. J Neural Transm 2006 Apr; 113(4):497–519
Knochel JP. Environmental heat illness. An eclectic review. Arch Intern Med 1974 May; 133(5):841–864
Centers for Disease Control and Prevention (CDC). Heat-related deaths – Los Angeles County, California, 1999–2000, and United States, 1979–1998. MMWR Morb Mortal Wkly Rep. 2001 Jul 27; 50(29):623–626
Garssen J, Harmsen C, de Beer J. The effect of the Summer 2003 heat wave on mortality in the Netherlands. Euro Surveill 2005 Jul; 10(7):165–168
Kunst AE, Looman CW, Mackenbach JP. Outdoor air temperature and mortality in The Netherlands: a time-series analysis. Am J Epidemiol 1993 Feb 1; 137(3):331–341
Bouchama A, Knochel JP. Heat stroke. N Engl J Med. 2002 Jun 20; 346(25):1978–1988. Review
Sharma HS, Hoopes PJ. Hyperthermia induced pathophysiology of the central nervous system. Int J Hypertherm 2003; 19:325–354
Sharma HS, Cervos-Navarro J. Brain oedema and cellular changes induced by acute heat stress in young rats. Acta Neurochir Suppl (Wien) 1990; 51:383–386
Sharma HS. Nanoneuroscience: nanoneurotoxicity and nanoneuroprotection. J Nanosci Nanotechnol 2009; 9:4992–4995
Sharma HS, Ali SF, Tian ZR, Hussain SM, Schlager JJ, Sjöquist P-O, Sharma A, Muresanu DF. Chronic treatment with nanoparticles exacerbate hyperthermia induced blood-brain barrier breakdown, cognitive dysfunction and brain pathology in the rat. Neuroprotective Effects of Nanowired-Antioxidant Compound H-290/51. J Nanosci Nanotechnol 2009; 9:5073–5090
Sharma S, Ali SF, Hussain SM, Schlager JJ, Sharma A. Influence of engineered nanoparticles from metals on the blood-brain barrier permeability, cerebral blood flow, brain edema and neurotoxicity. An experimental study in the rat and mice using biochemical and morphological approaches. J Nanosci Nanotechnol 2009; 9:5055–5072
Sharma HS, Ali S, Tian ZR, Patnaik R, Patnaik S, Lek P, Sharma A, Lundstedt T. Nano-drug delivery and neuroprotection in spinal cord injury. J Nanosci Nanotechnol 2009; 9:5014–5037. Review
Sharma HS, Patnaik R, Sharma A, Sjöquist P-O, Lafuente, LV. Silicon Dioxide Nanoparticles (SiO2, 40–50 nm) Exacerbate pathophysiology of traumatic spinal cord injury and deteriorate functional outcome in the rat. An experimental study using pharmacological and morphological approaches. J Nanosci Nanotechnol 2009; 9:4970–4980
Brown DM, Stone V, Findlay P, MacNee W, Donaldson K. Increased inflammation and intracellular calcium caused by ultrafine carbon black is independent of transition metals or other soluble components. Occup Environ Med 2000; 57:685–691. [PubMed]
Brown DM, Wilson MR, MacNee W, Stone V, Donaldson K. Size-dependent proinflammatory effects of ultrafine polystyrene particles: a role for surface area and oxidative stress in the enhanced activity of ultrafines. Toxicol Appl Pharmacol 2001; 175:191–199
Derfus AM, Chan WCW, Bhatia SN. Probing the cytotoxicity of semiconductor quantum dots. Nano Lett 2004; 4(1):11–18
Joo SH, Feitz AJ, Waite TD. Oxidative degradation of the carbothioate herbicide, molinate, using nanoscale zerovalent iron. Environ Sci Technol 2004; 38:2242–2247
Li N, Sioutas C, Cho A, Schmitz D, Misra C, Sempf J, et al. Ultrafine particulate pollutants induce oxidative stress and mitochondrial damage. Environ Health Perspect 2003; 111:455–460
Oberdörster E. Manufactured nanomaterials (fullerenes, C60) induce oxidative stress in brain of juvenile largemouth bass. Environ Health Perspect 2004; 112:1058–1062
Sayes C, Fortner J, Guo W, Lyon D, Boyd AM, Ausman KD, et al. The differential cytotoxicity of water-soluble fullerenes. Nano Lett 2004; 4:1881–1887
Shvedova AA, Kisin ER, Murray A, Kommineni C, Vallyathan V, Castranova V. Pro/antioxidant status in murine skin following topical exposure to cumene hydroperoxide throughout the ontogeny of skin cancer. Biochemistry (Mosc) 2004 Jan; 69(1):23–31
Shvedova AA, Kisin ER, Mercer R, Murray AR, Johnson VJ, Potapovich AI, Tyurina YY, Gorelik O, Arepalli S, Schwegler-Berry D, Hubbs AF, Antonini J, Evans DE, Ku BK, Ramsey D, Maynard A, Kagan VE, Castranova V, Baron P. Unusual inflammatory and fibrogenic pulmonary responses to single-walled carbon nanotubes in mice. Am J Physiol Lung Cell Mol Physiol 2005 Nov; 289(5):L698–L708
Sharma HS, Sjöquist PO, Ali SF. Drugs of abuse-induced hyperthermia, blood-brain barrier dysfunction and neurotoxicity: neuroprotective effects of a new antioxidant compound H-290/51. Curr Pharm Des 2007; 13(18):1903–1923. Review
Sharma HS, Sjoquist PO, Alm P. A new antioxidant compound H-290151 attenuates spinal cord injury induced expression of constitutive and inducible isoforms of nitric oxide synthase and edema formation in the rat. Acta Neurochir Suppl 2003; 86:415–420
Sharma HS, Gordh T, Wiklund L, Mohanty S, Sjoquist PO. Spinal cord injury induced heat shock protein expression is reduced by an antioxidant compound H-290/51. An experimental study using light and electron microscopy in the rat. J Neural Transm 2006 Apr; 113(4):521–536
Jordan A, Scholz R, Maier-Hauff K, van Landeghem FK, Waldoefner N, Teichgraeber U, Pinkernelle J, Bruhn H, Neumann F, Thiesen B, von Deimling A, Felix R. The effect of thermotherapy using magnetic nanoparticles on rat malignant glioma. J Neurooncol 2006 May; 78(1):7–14
Plotkin M, Gneveckow U, Meier-Hauff K, Amthauer H, Feussner A, Denecke T, Gutberlet M, Jordan A, Felix R, Wust P. 18F-FET PET for planning of thermotherapy using magnetic nanoparticles in recurrent glioblastoma. Int J Hyperthermia 2006 Jun; 22(4):319–325
Inoue K, Takano H, Yanagisawa R, Hirano S, Sakurai M, Shimada A, Yoshikawa T. Effects of airway exposure to nanoparticles on lung inflammation induced by bacterial endotoxin in mice. Environ Health Perspect 2006 Sep; 114(9):1325–1330
Sharma H S, Sjöquist P-O, Westman J. Pathophysiology of the blood-spinal cord barrier in spinal cord injury. Influence of a new antioxidant compound H-290/51. In: Kobiler D, Lustig S, Shapra S (eds) Blood-Brain Barrier. Drug Delivery and Brain Pathology, Kluwer Academic/Plenum Publishers, New York, 2001; pp. 401–416
MacNee W, Donaldson K. How can ultrafine particles be responsible for increased mortality? Monaldi Arch Chest Dis 2000 Apr; 55(2):135–139. Review
Sharma HS, Olsson Y, Nyberg F. Influence of dynorphin A antibodies on the formation of edema and cell changes in spinal cord trauma. Prog Brain Res 1995; 104:401–416. Review
Sharma HS, Westman J, Olsson Y, Alm P. Involvement of nitric oxide in acute spinal cord injury: an immunocytochemical study using light and electron microscopy in the rat. Neurosci Res 1996 Mar; 24(4):373–384
Faden AI. Opioid and nonopioid mechanisms may contribute to dynorphin’s pathophysiological actions in spinal cord injury. Ann Neurol 1990 Jan; 27(1):67–74
Sharma HS, Westman J, Nyberg F. Topical application of 5-HT antibodies reduces edema and cell changes following trauma of the rat spinal cord. Acta Neurochir Suppl 1997; 70:155–158
Sharma HS, Patnaik R, Patnaik S, Mohanty S, Sharma A, Vannemreddy P. Antibodies to serotonin attenuate closed head injury induced blood brain barrier disruption and brain pathology. Ann NY Acad Sci 2007 Dec; 1122:295–312
Sharma HS, Winkler T, Stålberg E, Gordh T, Alm P, Westman J. Topical application of TNF-alpha antiserum attenuates spinal cord trauma induced edema formation, microvascular permeability disturbances and cell injury in the rat. Acta Neurochir Suppl 2003; 86:407–413
Wahl M, Unterberg A, Baethmann A, Schilling L. Mediators of blood-brain barrier dysfunction and formation of vasogenic brain edema. J Cereb Blood Flow Metab 1988 Oct; 8(5):621–634. Review
Olsson Y, Sharma HS, Pettersson CA. Effects of p-chlorophenylalanine on microvascular permeability changes in spinal cord trauma. An experimental study in the rat using 131I-sodium and lanthanum tracers. Acta Neuropathol 1990; 79(6):595–603
Sharma HS, Westman J, Olsson Y, Johansson O, Dey PK. Increased 5-hydroxytryptamine immunoreactivity in traumatized spinal cord. An experimental study in the rat. Acta Neuropathol 1990; 80(1):12–17
Sharma HS, Olsson Y. Edema formation and cellular alterations following spinal cord injury in the rat and their modification with p-chlorophenylalanine. Acta Neuropathol 1990; 79(6):604–610
Sharma HS, Olsson Y, Cervós-Navarro J. p-Chlorophenylalanine, a serotonin synthesis inhibitor, reduces the response of glial fibrillary acidic protein induced by trauma to the spinal cord. An immunohistochemical investigation in the rat. Acta Neuropathol 1993; 86(5):422–427
Sharma HS Pathophysiology of the blood-spinal cord barrier in traumatic injury. In: Sharma HS, Westman J (eds) The Blood-Spinal Cord and Brain Barriers in Health and Disease, Elsevier Academic Press, San Diego, 2004; pp. 437–518
Sharma HS, Alm P, Westman J. Nitric oxide and carbon monoxide in the brain pathology of heat stress. Prog Brain Res 1998; 115:297–333. Review
Sharma HS, Nyberg F, Thörnwall M, Olsson Y. Met-enkephalin-Arg6-Phe7 in spinal cord and brain following traumatic injury to the spinal cord: influence of p-chlorophenylalanine. An experimental study in the rat using radioimmunoassay technique. Neuropharmacology 1993 Jul; 32(7):711–717
Sharma HS, Olsson Y, Westman J. A serotonin synthesis inhibitor, p-chlorophenylalanine reduces the heat shock protein response following trauma to the spinal cord: an immunohistochemical and ultrastructural study in the rat. Neurosci Res 1995 Jan; 21(3):241–249
Sharma HS, Olsson Y, Nyberg F, Dey PK. Prostaglandins modulate alterations of microvascular permeability, blood flow, edema and serotonin levels following spinal cord injury: an experimental study in the rat. Neuroscience 1993 Nov; 57(2):443–449
Winkler T, Sharma HS, Stålberg E, Olsson Y. Indomethacin, an inhibitor of prostaglandin synthesis attenuates alteration in spinal cord evoked potentials and edema formation after trauma to the spinal cord: an experimental study in the rat. Neuroscience 1993 Feb; 52(4):1057–1067
Sharma HS, Olsson Y, Cervós-Navarro J. Early perifocal cell changes and edema in traumatic injury of the spinal cord are reduced by indomethacin, an inhibitor of prostaglandin synthesis. Experimental study in the rat. Acta Neuropathol 1993; 85(2):145–153
Sharma HS, Westman J. Prostaglandins modulate constitutive isoform of heat shock protein (72 kD) response following trauma to the rat spinal cord. Acta Neurochir Suppl 1997; 70:134–137
Ray SK, Banik NL. Calpain and its involvement in the pathophysiology of CNS injuries and diseases: therapeutic potential of calpain inhibitors for prevention of neurodegeneration. Curr Drug Targets CNS Neurol Disord 2003 Jun; 2(3):173–189. Review
Sharma HS, Drieu K, Alm P, Westman J. Role of nitric oxide in blood-brain barrier permeability, brain edema and cell damage following hyperthermic brain injury. An experimental study using EGB-761 and Gingkolide B pretreatment in the rat. Acta Neurochir Suppl 2000; 76:81–86
Sharma HS, Drieu K, Westman J. Antioxidant compounds EGB-761 and BN-52021 attenuate brain edema formation and hemeoxygenase expression following hyperthermic brain injury in the rat. Acta Neurochir Suppl 2003; 86:313–319
Olesen SP. An electrophysiological study of microvascular permeability and its modulation by chemical mediators. Acta Physiol Scand Suppl 1989; 579:1–28
Kiyatkin EA, Sharma HS. Permeability of the blood-brain barrier depends on brain temperature. Neuroscience 2009 Jul 7; 161(3):926–939. Epub 2009 Apr 9
Sharma HS, Kiyatkin EA. Rapid morphological brain abnormalities during acute methamphetamine intoxication in the rat: an experimental study using light and electron microscopy. J Chem Neuroanat 2009 Jan; 37(1):18–32. Epub 2008 Aug 19
Kiyatkin EA, Brown PL, Sharma HS. Brain edema and breakdown of the blood-brain barrier during methamphetamine intoxication: critical role of brain hyperthermia. Eur J Neurosci 2007 Sep; 26(5):1242–1253
Sharma HS, Ali SF. Alterations in blood-brain barrier function by morphine and methamphetamine. Ann NY Acad Sci 2006 Aug; 1074:198–224
Acknowledgments
Author’s research described here is supported by Grants from Swedish Medical Research Council (2710), Stockholm Sweden, Göran Gustafsson Foundation, Stockholm, Sweden; Alexander von Humboldt Foundation, Bonn, Germany, European Office of Aerospace Research and Development (EOARD), London Office, UK. Technical assistant of Mari-Anne Carlsson, Kerstin Flink, Ingmarie Olsson and Kerstin Rystedt are highly appreciated.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media B.V.
About this chapter
Cite this chapter
Sharma, H.S., Sharma, A. (2010). Breakdown of the Blood-Brain Barrier in Stress Alters Cognitive Dysfunction and Induces Brain Pathology: New Perspectives for Neuroprotective Strategies. In: Ritsner, M. (eds) Brain Protection in Schizophrenia, Mood and Cognitive Disorders. Springer, Dordrecht. https://doi.org/10.1007/978-90-481-8553-5_9
Download citation
DOI: https://doi.org/10.1007/978-90-481-8553-5_9
Published:
Publisher Name: Springer, Dordrecht
Print ISBN: 978-90-481-8552-8
Online ISBN: 978-90-481-8553-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)