Abstract
Intracranial aneurysms can be induced by a single stereotaxic injection of elastase into the cerebrospinal fluid at the right basal cistern in hypertensive mice. This mouse model produces large aneurysm formations with an incidence of 60–80% within 3–4 weeks. Intracranial aneurysms in this model recapitulate key pathological features of human intracranial aneurysms. Several technical factors are critical for the successful induction of intracranial aneurysms in this model. Precise stereotaxic placement of the needle tip into the cerebrospinal fluid space is especially important. Aneurysm formations in this model can serve as a simple and easily interpretable outcome for future studies that utilize various inhibitors, knockout mice, or transgenic mice to test roles of specific molecules and pathways in the pathophysiology of intracranial aneurysms.
Authors Yoshiteru Tada and Yasuhisa Kanematsu contributed equally to this study
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Intracranial aneurysm ·
- Animal model ·
- Macrophage ·
- Matrix metalloproteinase ·
- Hypertension ·
- Inflammation ·
- Mouse
Introduction
Despite recent advances in diagnosis and treatment, the mechanisms for formation, growth, and subsequent rupture of intracranial aneurysms are not well understood [1]. In order to understand the pathophysiology of intracranial aneurysms and identify therapeutic targets for the prevention of aneurysmal rupture, an animal model of intracranial aneurysm would be useful. Recently, we have developed a new mouse model of intracranial aneurysm that recapitulates key pathological features of human intracranial aneurysms [2]. This model produces large intracranial aneurysms within a short incubation time of 2–3 weeks. In this article, we will discuss technical considerations that are critical for the successful application of this model for future studies.
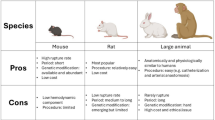
Overview of Elastase-Induced Intracranial Aneurysm in Hypertensive Mice
In this model, two well-known clinical factors associated with human intracranial aneurysms – hypertension and the degeneration of elastic lamina – are combined to induce intracranial aneurysm formation in mice [2]. Hypertension is associated with the formation and rupture of intracranial aneurysms. Degeneration of the elastic lamina is a key pathological change of intracranial aneurysms. Fragmentation of the elastic lamina alone is considered a pre-aneurysmal change that can eventually mature into an aneurysm. In this model, hypertension is induced by continuous infusion of angiotensin II; degradation of the elastic lamina is induced by a single injection of elastase into the cerebrospinal fluid using a stereotaxic method. This model produces large intracranial aneurysms at an incidence of 60–80% within 3–4 weeks. Aneurysms are formed in the circle of Willis and its major branches. Figure 1 shows a control brain (a) and representative aneurysms (b, c) from this model.
Representative aneurysms. (a) Control brain. (b) Aneurysms were found at the bifurcation at the right middle cerebral artery and the internal carotid artery and at the proximal part of right middle cerebral artery. (c) Aneurysm at the right anterior cerebral artery. (RACA right anterior cerebral artery, LACA left anterior cerebral artery, RMCA right middle cerebral artery). Arrows in Figure 1b and 1c indicate aneurysms
There are dose-dependent effects of angiotensin II and elastase on the incidence of aneurysms in this model. Neither angiotensin II nor elastase alone could induce aneurysms, indicating that synergistic effects of elastase and hypertension are needed for the aneurysm formation in our model. When hypertension-induced vascular remodeling is coupled with elastase-induced inflammation, abnormal vascular remodeling may occur. Intracranial aneurysm formation may represent maladaptive vascular remodeling that is mediated by hemodynamic changes and inflammation [3].
Histologically, intracranial aneurysms formed in this model closely resemble human intracranial aneurysms. Part of the aneurysmal wall in this model is often thickened. Although endothelial and smooth muscle cell layers are sometimes fragmented, they are generally present throughout the aneurysmal wall, showing that the intracranial aneurysms formed in this model are true aneurysms, not pseudo-aneurysms.
Aneurysms formed in this model are generally large and easily distinguishable from the normal arteries without using histological assessment. Aneurysm formations in this model can serve as a simple and easily interpretable outcome for future studies that utilize various inhibitors, knockout mice, or transgenic mice to test roles of specific molecules and pathways in the pathophysiology of intracranial aneurysms. For example, using this model, we have shown critical roles of matrix metalloproteinases (MMPs) in the formation of intracranial aneurysms [2].
Angiotensin II-Induced Hypertension
Angiotensin II infusion through an implanted osmotic pump is a well-established, well-characterized model of hypertension in mice [4–6]. A horizontal skin incision approximately 1 cm long should be made on one side of the back at 1 cm cephalad from the base of the tail. The small pocket between the skin and muscle layers that will contain the osmotic pump can be made using a pair of forceps. The osmotic pump can be implanted into this pocket, and the skin should be closed with sutures. This procedure takes only 5–10 min with a minimum amount of training. Proper suturing of the incision is very important since the wound dehiscence can result in unexpected explantation of the osmotic pump. Frequent monitoring of the wound site is needed, and the additional sutures can be added as needed.
Using angiotensin II infusion, a rise in systolic blood pressure can be detected at as early as 1 week, and hypertension can be maintained for up to 6 weeks. Norepinephrine infusion or deoxycorticosterone acetate (DOCA)-salt treatment can also be used to induce hypertension in mice [5, 6]. DOCA-salt hypertension may be useful when non-hemodynamic effects of angiotensin II need to be avoided. Angiotensin II can exert various effects on the vasculature in addition to its hypertensive effect, including induction of reactive oxygen species and promotion of inflammation [5]. It should be noted that in our experience, the rise in blood pressure in these two methods was milder than that in angiotesin II-induced hypertension; hypertension became less significant after 3 weeks using norepinephrine infusion or deoxycorticosterone acetate (DOCA)-salt treatment. Angiotensin II-induced hypertension may be more consistent and sustained.
Blood Pressure Measurement
To monitor successful induction and maintenance of systemic hypertension, blood pressure measurement is critical. Since repeated measurements of blood pressure are needed, the tail cuff method is used in our laboratory (ML125M, ADinstruments). In our experience, this method provides accurate estimates for systolic blood pressure. Our preliminary data showed a highly significant correlation between the systolic blood pressure values using the tail cuff method and the mean blood pressure values obtained from the direct measurement using a femoral artery catheter.
Blood pressure measurement of conscious mice requires a series of training of mice. Some strains of mice, such as C57BL/6 J mice, appear to have high locomotor activity and resistance to restraint, even after training for blood pressure measurements [4]. Alternatively, blood pressure measurement can be performed on anesthetized mice. Systolic blood pressure can be reliably measured when mice are under a steady state of isoflurane anesthesia [2, 5]. This would require a continuous monitoring of isoflurane concentration in the anesthesia chamber or mask. We have conducted an experiment comparing systolic blood pressure values between conscious state and anesthetized state.
In three groups of mice, blood pressure was measured in both conscious and anesthetized states. Mice received either phosphate-buffered saline, angiotensin II at 500 ng/kg/min, or angiotensin II at 1,000 ng/kg/min through osmotic pumps (n = 3 in each group). After two consecutive days of acclimation training, mice underwent “conscious” blood pressure measurement. Immediately after the blood pressure measurements were taken in the conscious state, mice were anesthetized with isoflurane, and blood pressure was measured at the steady state of isoflurane anesthesia (after 15 min of equilibration with isoflurane concentration at 1.5%). As shown in Fig. 2, there was a close correlation between systolic blood pressure measured under conscious state and that under anesthetized state (R 2 = 0.96, P < 0.05). As we have expected, systolic blood pressure measured under anesthetized state was slightly lower than that under conscious state (y = 1.05 x −17), reflecting the blood pressure lowering effect of isoflurane. We have previously shown that isoflurane anesthesia does not mask effects of antihypertensive agents [5]. These data showed that systolic blood pressure measurement under a steady isoflurane anesthesia can be reliably used to monitor changes in blood pressure in mice.
Stereotaxic Injection of Elastase
The detailed method for the single stereotaxic injection of elastase into the cerebrospinal fluid at the right basal cistern has been described previously [2]. Briefly, the tip of a 26-gauge needle (10 μl syringe, Model 701, with 26 g 2 inches, Hamilton Replacement needle Point style 3, Fisher Scientific) was stereotaxically placed in the right basal cistern using the coordinates obtained from Mouse Brain Atlas (2.4–2.8 mm posterior to the bregma, 0.9–1.1 mm lateral to the midline, and 4.9–5.1 mm ventral to the skull surface). Elastase (E7885, porcine pancreatic elastase, lyophilized powder, 20 mg, Sigma Aldrich) was dissolved in PBS, and 2.5 μl of the elastase solution (0–35 milli-units) was injected at 0.2 μl/min. This part of the procedure will take approximately 30–40 min. Significant variations may exist in the potency of elastase activity in different lots or different preparations of commercially available elastase [7, 8]. It may be prudent to use elastase from the same lot in each set of experiments.
In our experience, we found that the stereotaxic coordinates need to be adjusted depending on the operator and the age of mice. Therefore, a series of test injections using dye (bromophenol blue) was extremely important to ensure the correct placement of the needle tip at the right basal cistern. The coordinates we described in the original paper [2] should be regarded as a guideline. Each researcher should perform a series of test injections to adjust for the appropriated coordinates before starting the actual experiments. Figure 3a shows a result of typical successful test injections. The mouse was sacrificed immediately after injection; bromophenol blue dye was observed along the right half of the circle of Willis. It appears that at least ten test injections are needed before each operator establishes the appropriate coordinates that yield stable aneurysm induction. We routinely perform a test injection once every ten mice to ensure the correct needle placement.
Inspection of brain tissues 1 day after injection of dye or elastase. (a) Test injection of dye. Immediately after a stereotaxic injection of bromophenol blue (2.5 μl) into the cerebrospinal fluid at the right basal cistern, the mouse brain was extracted. The dye was observed along the right half of the circle of Willis. Arrows indicate the dye. (b) Intracerebral hemorrhage due to elastase injection into the brain parenchyma. If the needle depth is too shallow, an injection of elastase results in intracerebral hemorrhage. (c) Diffuse bleeding from the brain surface. If the needle tip is too close to the surface of the brain, the injection of elastase into the cerebrospinal fluid can result in diffuse hemorrhage from the surface of the brain, even when the needle tip is inside the subarachnoid space. (d) Successful injection of elastase. When the brain was inspected 1 day after elastase injection, there was no diffuse bleeding from the surface of the brain or intracerebral hemorrhage, indicating a successful placement of the needle
The depth of the needle is another critical factor for the successful induction of aneurysm in this model. If the needle depth is too shallow, the injection of elastase into the brain parenchyma results in intracerebral hemorrhage similar to the collagenase-induced intracerebral hemorrhage (Fig. 3b) [9–11]. If the needle tip is too close to the surface of the brain, the injection of elastase into the cerebrospinal fluid can result in diffuse hemorrhage from the surface of the brain, even when the needle tip is inside the subarachnoid space (Fig. 3c). This might be due to compartmentalization of the subarachnoid space.
We recommend that the operator should find the depth at which the needle tip touches the surface of the dura matter or skull base. Then, the operator can use the depth that is approximately 0.3–0.4 mm shallower than the dura or skull base for subsequent test injections using dye. The spread of dye along the right half of the circle of Willis should be confirmed (Fig. 3a). If the dura matter is intensely stained with the dye, subdural injection should be suspected. After establishing the needle depth for successful injections, the operator should perform test injections of elastase and sacrifice the animals 1 day after injection. Lack of diffuse bleeding from the surface of the brain or intracerebral hemorrhage would indicate the successful placement of the needle (Fig. 3d).
The surgical procedures for the aneurysm induction seem to cause significant perioperative stress to mice. Water intake of some of the postoperative mice seemed to have decreased during the first 2 postoperative days. Therefore, we inject 500 μl of saline subcutaneously once a day for the first 2 postoperative days in all mice.
Conclusion
Elastase-induced intracranial aneurysms in hypertensive mice represents an easily reproducible animal model that yields a high incidence of large intracranial aneurysms within a practical incubation time. There are several technical issues that are critical for the successful use of this model. This model can be used to study molecular pathways that are potentially involved in the pathophysiology of intracranial aneurysms.
Sources of Funding This study was funded by NIH R01NS055876 (TH) and NIH P01NS044155 (TH).
References
Shi C, Awad IA, Jafari N, Lin S, Du P, Hage ZA, Shenkar R, Getch CC, Bredel M, Batjer HH, Bendok BR (2009) Genomics of human intracranial aneurysm wall. Stroke 40:1252–1261
Nuki Y, Tsou TL, Kurihara C, Kanematsu M, Kanematsu Y, Hashimoto T (2009) Elastase-induced intracranial aneurysms in hypertensive mice. Hypertension 54:1337–1344
Hashimoto T, Meng H, Young WL (2006) Intracranial aneurysms: links between inflammation, hemodynamics and vascular remodeling. Neurol Res 28:372–380
Daugherty A, Manning MW, Cassis LA (2000) Angiotensin II promotes atherosclerotic lesions and aneurysms in apolipoprotein E-deficient mice. J Clin Invest 105:1605–1612
Kanematsu Y, Kanematsu M, Kurihara C, Tsou TL, Nuki Y, Liang EI, Makino H, Hashimoto T (2010) Pharmacologically induced thoracic and abdominal aortic aneurysms in mice. Hypertension 55:1267–1274
Weiss D, Kools JJ, Taylor WR (2001) Angiotensin II-induced hypertension accelerates the development of atherosclerosis in apoE-deficient mice. Circulation 103:448–454
Carsten CG III, Calton WC, Johanning JM, Armstrong PJ, Franklin DP, Carey DJ, Elmore JR (2001) Elastase is not sufficient to induce experimental abdominal aortic aneurysms. J Vasc Surg 33:1255–1262
Ding YH, Danielson MA, Kadirvel R, Dai D, Lewis DA, Cloft HJ, Kallmes DF (2006) Modified technique to create morphologically reproducible elastase-induced aneurysms in rabbits. Neuroradiology 48:528–532
Kitaoka T, Hua Y, Xi G, Hoff JT, Keep RF (2002) Delayed argatroban treatment reduces edema in a rat model of intracerebral hemorrhage. Stroke 33:3012–3018
Rosenberg GA, Mun-Bryce S, Wesley M, Kornfeld M (1990) Collagenase-induced intracerebral hemorrhage in rats. Stroke 21:801–807
Tang J, Liu J, Zhou C, Alexander JS, Nanda A, Granger DN, Zhang JH (2004) Mmp-9 deficiency enhances collagenase-induced intracerebral hemorrhage and brain injury in mutant mice. J Cereb Blood Flow Metab 24:1133–1145
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag/Wien
About this chapter
Cite this chapter
Tada, Y. et al. (2011). A Mouse Model of Intracranial Aneurysm: Technical Considerations. In: Zhang, J., Colohan, A. (eds) Intracerebral Hemorrhage Research. Acta Neurochirurgica Supplementum, vol 111. Springer, Vienna. https://doi.org/10.1007/978-3-7091-0693-8_6
Download citation
DOI: https://doi.org/10.1007/978-3-7091-0693-8_6
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-7091-0692-1
Online ISBN: 978-3-7091-0693-8
eBook Packages: MedicineMedicine (R0)