Abstract
Polynitroxylated pegylated hemoglobin (PNPH, VitalHeme™, SynZyme Technologies LLC, Irvine, CA) is a pegylated hemoglobin covalently labeled with catalytic nitroxides, aka caged nitric oxide (cNO). PNPH serves as a hyperoncotic biopolymer coated and redox transformed hemoglobin acting in the plasma phase as a neurovascular protective multifunctional nanomedicine. This drug is for the correction or prevention of inadequate regional and/or global blood flow without oxidative stress under normal or hypovolemic states in critical care and transfusion medicine. Specific clinical indications for which PNPH has shown efficacy are traumatic brain injury complicated by hemorrhagic shock, stroke, and sickle cell disease. PNPH may also be an ideal alternative to aged red blood cells and a bridge to transfusion.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Nitric Oxide
- Traumatic Brain Injury
- Sickle Cell Disease
- Middle Cerebral Artery Occlusion
- Hemorrhagic Shock
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Evolving beyond the current generation of hemoglobin based oxygen carriers (HBOCs), a multifunctional hemoglobin nanomedicine (MHN) has been developed. PNPH is an example of a MHN, which contains one hemoglobin molecule per nanoparticle and functions from the intravascular plasma phase as a drug for small volume transfusion for the prevention or correction of interrupted or inadequate blood flow without oxidative stress in critical care and transfusion medicine (Hsia and Ma 2012, 2013).
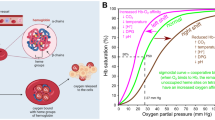
Similar to HBOCs, PNPH retains the binding and transport capacity for oxygen, nitric oxide and carbon monoxide to function as a gas carrier in the plasma phase. However, in sharp contrast to current generation HBOCs, PNPH has the added functions of: (1) superoxide dismutase (SOD) mimetic activity, (2) catalase (CAT) mimetic activity, (3) unusual peroxidase activity, (4) nitric oxide protective activity by virtue of reduced superoxide through SOD activity, (5) hyperoncotic activity and (6) neuron protective activity. Thus PNPH has the added advantages of providing (1) improved hemodynamic stability, (2) superior volume expansion, (3) prevention of ischemia, (4) protection against reperfusion and inflammatory injuries and (5) hemoglobin detoxification capacity. In this chapter, data supporting the added functions are presented and PNPH is discussed as a drug for un-met medical needs such as traumatic brain injury complicated with hemorrhagic shock (TBI + HS), hemorrhagic and ischemic stroke, and sickle cell disease (SCD) as well as an alternative to red blood cell (RBC) transfusion to meet a worldwide unmet medical need.
2 PNPH
Through evolution, Hb as an oxygen carrier has diverged into two forms: a cellular Hb in vertebrates and an acellular Hb in invertebrates. Attempts to convert vertebrate cellular Hb into acellular Hb during the past two to three decades have failed to attenuate the intrinsic Hb toxicity or to counter the pro-oxidant activities of the vertebrate Hb. The significant challenges that had been encountered in HBOC development were highlighted at the FDA/NIH/HHS workshop in 2008 (FDA 2008). Following that workshop, the combination of challenges, negative perceptions, and difficulties in obtaining adequate funding for continued research and product evaluation led the NIH/FDA/DOD to convene a working group of experts in Boston in July 2011 to examine the future of oxygen therapeutics (NIH 2011). This later group re-affirmed the medical needs for oxygen therapeutics and outlined the basic and applied research needed to continue drug development for clinical applications including (1) a bridge to transfusion, (2) an alternative to blood transfusion, and (3) a therapeutic in indications where blood transfusion is not normally used.
Below we describe PNPH, a new generation product of hemoglobin based oxygen carrier (HBOC) that has evolved beyond the single function oxygen carriers to a MHN (Hsia and Ma 2012). We applied catalytic free-radical caged nitric oxide (cNO) technology to pegylated Hb to produce PNPH, a multifunctional, anti-oxidative nanomedicine that may also function as a life saving drug in massive volume transfusion.
2.1 HBOC Development
Since the NIH/FDA/HHS 2008 Workshop, clinical trials of the current generation HBOCs have been terminated in the United States and continued clinical trials and commercialization have moved off shore. In countries where the AIDS epidemic and limited testing of banked blood makes the blood transfusion unsafe, the development and commercialization of current generation HBOCs may be justified. Additionally, use of an HBOC for delivery of carbon monoxide to treat SCD as an orphan indication is being pursued off shore. While these new approaches to current generation HBOCs seems to be making incremental improvements, they have not addressed the original limitations because these HBOCs still have the inherent toxicity of cell free Hb making them low therapeutic index oxygen carriers. However, if these off shore commercial uses and clinical trials are successful, it may aid in the approval and wide spread use of these HBOCs in the United States and European markets as alternatives for transfusion of stored RBCs. The next generation HBOC may be dependent on development of invertebrate extracelluar hemoglobins, which lack the inherent toxicity of vertebrate cell free Hb making them higher therapeutic HBOCs (Elmer and Palmer 2012; Tsai et al. 2012).
2.2 MHN Development
Our main focus has been development of drugs for the treatment of life threatening disruption of blood flow. Catalytic caged nitric oxide (cNO, aka nitroxide) platform technology has enabled the development of drugs that enhance blood flow in critical organs and treat the toxicity of acute Hb release, excessive superoxide production and nitric oxide depletion. Based on decades of research, we have developed a drug pipeline of cNO modified macromolecules, in particular albumin and Hb, as multifunctional neurovascular protective, hemodynamic stabilizing, antioxidative drugs for unmet medical needs in critical care medicine. From this pipeline, PNPH is being developed mainly to meet clinical indications where blood transfusion is not normally used. With PNPH, we are targeting major diseases like hemorrhagic and ischemic stroke, TBI + HS, and SCD. Herein we describe PNPH and how it may meet the challenges posted by the NIH/FDA/DOD Working Group of 2011.
2.3 PNPH - Science and Technology
Focusing solely on the oxygen carrying and transport capacities of the HBOCs appears to have been a major flaw in the design of HBOCs. The conventional wisdom concerning the causes of the adverse effects of experimental HBOCs is that the primary mechanism of toxicity is nitric oxide (NO) scavenging at the endothelium, causing vasoconstriction and, paradoxically for a product intended to deliver oxygen, compromised tissue perfusion and oxygenation (Alayash 1999). Cell-free Hb derivatives tested to date may also bring another set of toxicities in addition to NO scavenging. These toxicities are related to pro-oxidant activity. While current generation HBOCs have attempted to deal with NO scavenging, they have not addressed the toxicities related to pro-oxidant Hb, which result from the combination of oxygen and heme iron in the absence of the controlling influence of the antioxidant enzymes of the red cell. The result can be the generation of toxic molecules such as superoxide, hydrogen peroxide, hydroxyl radical, oxoferryl porphyrin, etc. (Alayash 1999; Sloan 2003). Thus the reduction in oxygen delivery resulting from Hb’s NO scavenging and vasoconstriction is further exacerbated by oxidative stress through a burst of superoxide generation from heme iron auto oxidation in the transfused HBOCs (Alayash 2004). In this view, cell-free Hb without appropriate regulation would actually add to the inflammatory insult of ischemia and reperfusion, adding to the underlying pathology in the very clinical situations where a blood substitute would be most useful. Polynitroxylation may well provide the controlling influence to tame the pro-oxidant activity of Hb (Ma and Hsia 2005).
Polynitroxylation covalently links multiple nitroxides to various macromolecules. Nitroxides have been shown to act as mimics of SOD (Samuni et al. 1990; Krishna et al. 1992) and CAT (Krishna et al. 1996), inhibit peroxidation of lipids and lipoproteins (Damiani et al. 1994; Nilsson et al. 1989), and inhibit peroxynitrite-mediated nitration (Carroll et al. 2000). They are effective agents in the protection of cells against reactive oxygen species mediated damage caused by inflammation (Tsuhako et al. 2010; Cuzzocrea et al. 2004). More recently, their antihypertensive effects (Wilcox and Pearlman 2008), their vasodilatation effects (Simonsen et al. 2009), their neuroprotective effects in animal models of TBI (Deng-Bryant et al. 2008), and their protection of spinal cord mitochondria from oxidative stress (Xiong et al. 2009) have been reported. The therapeutic efficacy and mechanism of physiological effects of nitroxides has been comprehensively reviewed (Wilcox 2010). Unfortunately, the problem with low molecular weight nitroxides is that they show poor pharmacokinetics because they are isotropically distributed in vivo and rapidly bio-inactivated to their reduced hydroxylamine form with half-life on the order of minutes. The nitroxides on a macromolecule have distinct therapeutic advantage over low molecular weight nitroxides, such as 4-hydroxy-2,2,6,6-tetramethylpiperidin-1-oxyl (Tempol) (Rozantsev 1970) since linking multiple nitroxides to macromolecules has been shown to prolong the half-life of the nitroxide in vivo (Kuppusamy et al. 1996, 1998). Thus, polynitroxylation is a novel technology for improving the therapeutic index of nitroxides by linking multiple nitroxides to macromolecules for delivery to the vasculature.
Polynitroxylation maintains the oxygen carrying and delivery capabilities of Hb while adding multiple therapeutic activities such as vascular and multiple-organ protective activities against oxidative stress and reperfusion and inflammation injuries. The nitroxide and heme iron act in concert to perform antioxidant activities that mimic the behavior of the two physiologically important anti-oxidant enzymes that are found in red blood cells, SOD and CAT. Thus polynitroxylation technology restores the missing red cell enzymatic controls to the HBOC, thereby reducing superoxide concentration, H2O2 concentration, and NO depletion. The unusual peroxidase activity is also accomplished through further redox coupling of the nitroxide/heme iron complex with endogenous plasma anti-oxidants (Stoyanovsky et al. 2010).
PNPH derives its high therapeutic index from the synergy of the triple chemical modifications of carboxylation, pegylation, and polynitroxylation of 64Kd Hb. The 3D structure of PNPH is shown in Fig. 16.1 as a dissected view with a core Hb and its hydrated polyethylene glycol (Peg) shell, shown in light gray, formed by covalently attaching approximately 10 Peg molecules and an extra inner SOD mimetic nitroxide shell, shown in dark gray, formed by covalently attaching approximately 12 nitroxides (white balls). Figure 16.2 shows the electron paramagnetic resonance (EPR) spectrum of the free nitroxide compared to PNPH. The spectrum of PNPH is characteristic of a covalent attachment of the nitroxides to the protein in which the nitroxides have a high spinning mobility independent of the protein and thus are freely moving around to form a nitroxide shell with SOD mimetic activity. This SOD shell prevents the release of superoxide from the core Hb into the vascular space, which is the key to the success of PNPH as a multifunctional therapeutic drug that is completely free of Hb toxicities. Furthermore, this SOD shell is also able to break down excess superoxide in the vascular space. This prevention of superoxide release from the core Hb of PNPH and dismutation of vascular superoxide together lead to the correction of inadequate blood flow through conservation of vascular NO.
Structure of PNPH is shown in a dissected view with a core Hb and its outer hydrated Peg shell, shown in light gray, formed by covalently attaching approximately 10 Peg molecules and an extra inner SOD mimetic nitroxide shell, shown in dark gray, formed by covalently attaching approximately 12 nitroxides (white balls)
Electron Paramagnetic Spectroscopy (EPR) EPR spectra of BrAcTPO (gray) in alcohol at 0.1 μM and PNPH (black) at 1 μM. EPR conditions: microwave power, 0.5 mW; modulation amplitude, 0.5 G for BrACTPO and 2 G for PNPH; receiver gain, 36 dB; sweep width, 100 G for BrAcTPO and 150 G for PNPH; temperature, room temp
PNPH is a hyperoncotic colloid wherein nitroxides, with intrinsic SOD mimetic activity as described above, are covalently attached to pegylated carboxy Hb and are thereby also redox coupled with the heme iron to function as a CAT mimetic. Enclosed in a hydrated pegylation shell to reduce immunogenicity, these enzyme mimetic activities keep the Hb in an environment resembling that of the red blood cell to attenuate the toxicities observed with cell free Hb. PNPH has five structural and functional components contributing to its unique therapeutic activities: (1) Hb as the protein center provides oxygen carrier capability but is caboxylated to provide thermo stability and added anti-inflammatory activity, (2) the hydrated polyethylene glycol moieties of PNPH make it a hyperoncotic colloid (iso-oncotic at only 4 g/dl) which is important to stabilizing hemodynamics during hypotension and hypovolemia, (3) the nitroxide moieties of PNPH not only improve the safety of cell-free Hb but also provide anti-oxidant/anti-inflammatory, neuroprotective, and NO protective activities, (4) the desirable redox coupling of heme iron with the nitroxide is promoted in the stoichiometry, and (5) further redox coupling of the nitroxide/heme iron complex with endogenous free plasma anti-oxidants such as ascorbate, which provides additional anti-oxidant activities.
These added intra-vascular and extra-vascular coupled redox reactions that attenuate vasoconstriction and the vascular inflammatory effects of ischemia and reperfusion are the new anti-oxidative stress therapeutic activities of this unique PNPH. Thus this approach represents a paradigm shift in blood substitute development, away from the traditional focus on oxygen delivery and NO supplementation and toward a new focus on safely correcting inadequate blood flow and oxidative stress.
2.4 PNPH Therapeutic Properties
2.4.1 Enzyme Mimetic Activities
SOD and CAT mimetic activities: D’Agnillo and Chang (1998) reported that the complex formed by co-polymerization of Hb with endogenous red cell SOD and CAT released less free iron in the presence of H2O2 than Hb alone. Using the same assay method, free iron release was measured. The absorption measured at 562 nm was used for free iron release against standard calibration curve. The data shown in Fig. 16.3 demonstrates that PNPH released less free iron than pegylated bovine hemoglobin (PegHb) at different H2O2 concentrations.
Comparison of free iron release from PNPH and PegHb under challenge by H2O2 Free iron was measured by the Ferrozine method (D’Agnillo and Chang 1998). A 2-ml reaction mixture of 10 μM hemoglobin tetramer of PEGHb (a) or PNPH (b) with various concentrations of H2O2 was mixed with 100 μL of 100 % trichloroacetic (TCA) acid and then titrated with ascorbic acid to final concentration of 0.01 %. Finally, 1 ml of ammonium acetate (10 %) and 0.3 ml of Ferrozine solution was added to complete the reaction. The absorption measured at 562 nm was used for free iron release (n = 3)
SOD mimetic activity: Levels of superoxide formation measured by luminol activity assays in the lung samples from WT littermate (WT control), and sickle cell mice (SS) exposed to saline (SS + NaCl), stroma free hemoglobin (SS + SFH), and PNPH (SS + PNPH) are shown in Fig. 16.4. Lung samples from SS mice exposed to saline had a significantly higher amount of superoxide formation when compared to WT control (* P < 0.05). Furthermore, stroma free hemoglobin resulted in a marked increase in superoxide formation as compared to SS + NaCl mice (# P < 0.05). In contrast, exposure to an equal amount of hemoglobin in the form of PNPH actually attenuated the increase in superoxide formation found in SS + NaCl mice (# P < 0.05) and had no significant difference compared with WT control mice. These in vivo findings suggested that PNPH reversed the elevation of superoxide formation and normalized the ROS signaling in the lung of the SS mice. (# P < 0.05) (Hsia and Ma 2009).
PNPH attenuation of superoxide formation in sickle cell (HbSS) mice. Luminol-enhanced chemiluminescence (CalBiochem, CA) was measured in relative light units (RLU) in lung samples of WT littermate (WT control), and sickle cell mice (SS) exposed to saline (SS + NaCl), stroma free hemoglobin (SS + SFH), and PNPH (SS + PNPH) (n = 4–7).* p < 0.05 and ** p < 0.01 compared with WT Control group # p < 0.05 omcpared with SS + NaCl group
CAT mimetic activity: Inside the red cell, CAT converts H2O2 to O2 and H2O. Using the rate of oxygen evolution as a measure of CAT mimetic activity as previously described (Krishna 1994), the CAT mimetic activity of PNPH and PegHb were determined after adding various concentrations of H2O2. Data showed PNPH has a higher rate of oxygen release than that of PegHb at each H2O2 concentration (Fig. 16.5). PNPH also reduces the oxo-ferrylformation with exposure to H2O2. Data showed that, over time, Fe4+ formation, measured by absorption at 545 nm, is much smaller in PNPH than in PegHb (Fig. 16.6).
Comparison of the rate of oxygen evolution by PNPH and PegHb under challenge by hydrogen peroxide. Catalase mimetic activity of PegHb (a) or PNPH (b) was determined by their rate of oxygen evolution measured by oxygen electrode under challenge by hydrogen peroxide (Krishna et al. 1996). The reaction mixture contained 100 μM hemoglobin tetramer with various concentrations of H2O2 in 50 mM phosphate buffer, pH 7.4 at room temperature. The electrode was calibrated by air saturated phosphate buffer (n = 3)
Comparison of oxo-ferryl formation by PNPH and PegHb with exposure to hydrogen peroxide. Oxo-ferryl formation of PegHb (a) and PNPH (b) with exposure to H2O2 was determined by their OD reading at 545 nm and is time dependent. The reaction mixtures contained 50 mM sodium phosphate buffer, pH 7.4, 25 μM H2O2, and 50 μM of either PegHb or PNPH
2.4.2 Neuroprotective Effect Against Hb Toxicity
Using primary cortical neuron cultures, data shows that PNPH is not only safe but also neuroprotective in three models; (a) a cytotoxicity study by incubating neurons with SFH or PNPH for 24 h, (b) study of PNPH protection against excitotoxicity in a glutamate/glycine-induced neuronal death model, and (c) study of PNPH protection against TBI-like stretch injury. Unlike SFH, which was neurotoxic, there was a lack of neurotoxicity of PNPH across a wide range of concentrations as measured by lactate dehydrogenase release and MTT viability tests. Also, dose dependent neuroprotection by PNPH in both glutamate/glycine induced neurotoxicity and neuronal stretch injury was demonstrated: when compared to saline treatment neuronal death was reduced between 40 and 85 % with PNPH treatment at concentrations of 0.2 and 2 μM in both tests. (Shellington DK et al. 2011).
2.4.3 Vascular Protective Effect
By virtue of its SOD, CAT and peroxidase mimetic activities, PNPH is likely to stabilize the vasculature during ischemia and reduce hemorrhagic transformation arising from delayed reperfusion. Polynitroxylated albumin (PNA; VACNO®) has been shown to be protective of the vasculature by inhibiting hemorrhagic transformation in studies of delayed tissue type plasminogen activator (tPA) treatment (Hsia 2012). Similar studies are ongoing for PNPH.
2.4.4 Physical Properties
The physical properties of PNPH are shown in Table 16.1.
2.5 PNPH Clinical Indications
2.5.1 Traumatic Brain Injury (TBI) Complicated by Hemorrhagic Shock (HS)
TBI is responsible for the greatest number of potential years of life lost from any cause and carries the highest burden on loss of quality-adjusted life-years among survivors (Gross et al. 1999). The primary injury to the brain occurs at the time of impact; however, subsequent compromise of cerebral perfusion can lead to an ischemic insult that extends the primary injury, creating a secondary brain injury (Stahel et al. 2008). The combination of TBI plus secondary insults such as HS can be devastating and new therapies are badly needed.
PNPH has been shown to be an efficacious, anti-oxidative hyper-colloid neuroprotective small volume resuscitative fluid for TBI + HS when compared to standard therapies in a model simulating the pre-hospital setting (Shellington et al. 2011). The data demonstrate that the pathophysiology from TBI + HS can be minimized with PNPH as a pre-hospital treatment and the exacerbation of edema caused by the large volume resuscitation with current standard care can be avoided (Brockman et al. 2012). PNPH requires the least volume to restore and maintain mean arterial blood pressure when compared to Lactated Ringer’s (LR), standard civilian therapy, or Hextend (HEX), standard military therapy, and confers neuroprotection in a relevant mouse model of TBI + HS. Mice resuscitated with PNPH had fewer Fluoro-Jade C + identified dying neurons in region 1 of the hippocampus proper vs. HEX and LR. PNPH also reduced the exacerbation of edema caused by the large volume resuscitation of current standard care while maintaining cerebral oxygenation better than LR as measured by implanted direct oxygen electrodes. In addition, recent data suggest a substantive attenuation of the development of intracranial hypertension during resuscitation compared to conventional therapy in TBI plus severe HS in mice (Brockman et al. 2012). In a separate publication studying TBI + HS, in vivo measurement of hemodynamic response, cerebral perfusion and intracranial pressure (ICP) demonstrated a beneficial synergistic effect of breathing 100 % oxygen and PNPH resuscitation, which included reduced ICP (Blasiole et al. 2010). Thus, multifunctional PNPH is an exciting therapy for TBI resuscitation in the setting of hemorrhagic hypotension as it confers multiple benefits including functioning as a small volume resuscitation solution, more promptly restoring MAP and CPP, reducing ICP, brain edema, and neuronal death when compared to standard resuscitation with LR. In on-going studies in the laboratories of Patrick Kochanek and his collaborators at the Safar Center for Resuscitation Research, PNPH also appears to have potential to confer benefit on some aspects of long-term cognitive function vs. resuscitation with LR, and certainly does not have deleterious effects on this very important clinical parameter.
2.5.2 Stroke
“Time is brain” is the mantra for stroke treatment, and a drug safe for immediate (pre-hospital) and universal use in all stroke victims without the need for neuroimaging would be a major breakthrough and a paradigm change in stroke therapy. The efficacy and safety requirements of such an early treatment drug is that it can enhance or maintain cerebral blood flow for oxygen delivery to the ischemic region without reperfusion damage and inflammation injuries and can also reduce the cerebral injuries from ongoing hemolysis in hemorrhagic stroke and hemorrhagic transformation in ischemic stroke. PNPH has shown such properties and, as discussed above, it has also been shown to protect neurons from Hb toxicity.
Transfusion of PNPH has been shown to be protective in a rat filament model of 2 h of middle cerebral artery occlusion (MCAO). Transfusion of 10 ml/kg of PNPH at 20 min of MCAO reduced the median infarct volume in the cerebral cortex from 40 % (37–47 % interquartile range; n = 10) in controls to 3 % (0–7 %; n = 10; P < 0.001) and in striatum from 78 % (66–88 %) to 34 % (0–37 %; P < 0.001). To determine whether delaying PNPH transfusion until 90 min of MCAO would improve penumbral perfusion, laser-Doppler flow (LDF) was measured in the ischemic border region where the reduction in LDF was less severe than in the core. LDF significantly increased from 48 ± 18 % of the pre-ischemic baseline to 67 ± 21 % (P < 0.005). Thus, PNPH transfusion has a significant therapeutic window for protection from transient MCAO and may act, in part, by stabilizing vascular function and improving collateral blood flow (Zhang 2013). The efficacy of PNPH to enhance blood flow in the ischemic penumbra while protecting the vasculature and reducing hemorrhagic transformation could expand the number of ischemic stroke patients treatable with lytic therapy well beyond the current 2–3 % per 2011 STAIR report (Albers 2011).
2.5.3 Sickle Cell Disease
Daily administration of oral hydroxyurea is the first pharmacological intervention documented to provide clinically significant prevention of complications in sickle cell disease. Hydroxyurea treatment has recently been shown to reduce pain events, hospital admissions and the need for blood transfusions by 50 % and mortality by 40 %. However, there are side effects and patient’s CBCs must be monitored every two weeks for evidence of bone marrow suppression. Once a stable or maximally tolerated dose is obtained, the patient can be monitored monthly. The long-term benefits and toxicities of hydroxyurea are unknown.
Transfusion of PNPH has recently been shown to significantly reduce the global insufficiency of vascular NO in transgenic SCD mice as measured by pulmonary hypertension and aortic stiffness. PNPH acts via the elevation of vascular NO through the suppression of the superoxide induced by cell free hemoglobin from the chronic hemolysis of SCD (Hsia and Ma 2009). Thus PNPH may represent an alternative to hydroxyurea SCD therapy or increase efficacy of hydroxyurea treatment with conjunctive use.
2.5.4 Alternative to Stored Red Blood Cells
Massive transfusion of blood can lead to clinical complications, including multi-organ dysfunction and death. These severe clinical outcomes have been associated with the use of RBCs stored for longer periods of time in a recent meta-analysis on available data including 409,966 patients and 21 studies (Wang et al. 2012). In a guinea pig transfusion model with blood stored under standard blood banking conditions for 2 (new), 21 (intermediate), or 28 days (old blood), transfusion with old but not new blood led to intravascular hemolysis, acute hypertension, vascular injury, and kidney dysfunction associated with the pathophysiology driven by hemolysis of old blood (Baek et al. 2012).
The most effective and safest way to avoid the problem of RBC aging with storage is simply to decrease the storage time, for example from 42 to 21 days or even less. But such a decrease in the allowed storage time for RBCs will cause a dramatic decrease in the blood supply all over the world, especially in the developed countries like US that have a much higher stable number of blood donors than the developing countries, which are already struggling with blood supply shortage. When this happens, it will be crucial that safe alternatives to RBC transfusion are available.
Additional adverse effects of blood transfusion relate to the antigenicity of donor blood and its ability to transmit infections. In addition to being a potentially high therapeutic index drug, PNPH has pegylation to reduce antigenicity and eliminates, or at least substantially reduces, the incidents of disease transmission. Hence, PNPH may be an ideal alternative to RBC transfusion and could play a major role in the setting of trauma care and some elective surgeries and could also benefit patients with medical conditions who are in need of long-term blood transfusions and experience immunological sensitization.
2.6 PNPH- Summary of Pre-clinical, Current Status, and Future Clinical Strategy
In additional to the efficacy testing in the various indications discussed above, a preliminary toxicology study in rats has been completed. The study concluded that there was no mortality or clinical observations that were associated with systemic toxicity in the rats. Weight gain and food consumption was indicative of good overall health of the rats.
Based on this preliminary toxicology study and the results of the multiple pre-clinical efficacy studies, the FDA concurred with SynZyme on November 1, 2012, at a PIND meeting that the development of PNPH as a therapeutic for critical care and transfusion medicine was justified. NINDS funding is expected to continue to IND submission in 2016 through NINDS grant #U44 NS07032. Private funding through corporate partnering could shorten the timeline. Looking several years into the future, the clinical development strategy is expected to be to establish the safety of PNPH as a small volume resuscitative fluid in Phase I and then expand to multiple exploratory Phase II clinical trials in the indications discussed above where efficacy has been established. Proposed endpoints for these exploratory Phase II clinical trials could be:
-
TBI + HS: Superior 6 month neurological outcome or survival with PNPH over standard care to benefit the more than 1.4 million TBI patients per year in America.
-
Stroke: Extension of the tPA treatment window with early PNPH treatment. There are over 700,000 ischemic stroke patients annually, yet only 2–3 % are treated with tPA after 16 years of continuous clinical use in America.
-
SCD: Reduction of pain events, hospital admissions and the need for blood transfusions by >50 % and mortality by >40 % when alone or in conjunctive treatments with Hydrea to benefit the ~100,000 American SCD patients.
-
Alternative to stored RBCs: Compare blood flow response and biomarkers between fresh RBCs, aged RBCs, and PNPH to reduce the over 15 million units of stored RBCs being transfused in the U.S. annually.
References
Alayash AI (1999) Hemoglobin-based blood substitutes: oxygen carriers, pressor agents, or oxidants? Nat Biotechnol 17:545–549
Alayash AI (2004) Oxygen therapeutics: can we tame haemoglobin? Nat Rev Drug Discovery 3:152–159
Albers GW, Goldstein LB, Hess DC, Wechsler LR, Furie KL, Gorelick PB, Hurn P, Liebeskind DS, Nogueira RG, Saver JL (2011) STAIR VII consortium. Stroke treatment academic industry roundtable (STAIR) recommendations for maximizing the use of intravenous thrombolytics and expanding treatment options with intra-arterial and neuroprotective therapies. Stroke 42:2645–2650
Baek JH, D’Agnillo F, Vallelian F, Pereira CP, Williams MC, Jia Y, Schaer DJ, Buehler PW (2012) Hemoglobin-driven pathophysiology is an in vivo consequence of the red blood cell storage lesion that can be attenuated in guinea pigs by haptoglobin therapy. J Clin Invest 122:1444–1458
Blasiole B, Bayir H, Vagni V, Feldman K, Ma L, Hsia C, Kochanek P (2010) Resuscitation of experimental traumatic brain injury and hemorrhagic shock in mice: acute effects of polynitroxylated pegylated hemoglobin and 100% oxygen. Crit Care Med 38:S411–S420, No. 12 (Suppl) Abstract 145
Brockman EC, Dixon CE, Bayir H, Blasiole B, Clark RSB, Vagni V, Ma L, Hsia C, Kochanek PM (2012) Polynitroxylated pegylated hemoglobin attenuates fluid requirements and brain edema in combined traumatic brain injury plus hemorrhagic shock in mice. J Neurotrauma 29:A205–A206
Carroll RT, Galatsis P, Borosky S, Kopec KK, Kumar V, Althaus JS, Hall ED (2000) 4-Hydroxy-2,2,6,6-tetramethylpiperidine-1-oxyl (Tempol) inhibits peroxynitrite-mediated phenol nitration. Chem Res Toxicol 13:294–300
Cuzzocrea S, Pisano B, Dugo L, Ianaro A, Patel NS, Caputi AP, Thiemermann C (2004) Tempol reduces the activation of nuclear factor-kappaB in acute inflammation. Free Radic Res 38:813–819
D’Agnillo F, Chang TM (1998) Polyhemoglobin-superoxide dismutase-catalase as a blood substitute with antioxidant properties. Nat Biotechnol 16:667–671
Damiani E, Paganga G, Greci L, Rice-Evans C (1994) Inhibition of copper-mediated low density lipoprotein peroxidation by quinoline and indolinone nitroxide radicals. Biochem Pharmacol 48:1155–1161
Deng-Bryant Y, Singh IN, Carrico KM, Hall ED (2008) Neuroprotective effects of tempol, a catalytic scavenger of peroxynitrite-derived free radicals, in a mouse traumatic brain injury model. J Cereb Blood Flow Metab 28:1114–1126
Elmer J, Palmer AF (2012) Biophysical properties of lumbricus terrestris erythrocruorin and its potential use as a red blood cell substitute. J Funct Biomater 3:49–60. doi:10.3390/jfb3010049
FDA/NIH/HHS Workshop (2008) Hemoglobin based oxygen carriers: current status and future directions. http://www.fda.gov/downloads/BiologicsBloodVaccines/NewsEvents/WorkshopsMeetingsConferences/TranscriptsMinutes/UCM051545
Gross CP, Anderson GF, Powe NR (1999) The relation between funding by the national institutes of health and the burden of disease. N Engl J Med 340:1881–1887
Hsia CJC (2012) VACNO®: a universal multifunctional drug for treating all stroke victims, ottawa 2012 international symposium on biochemistry and biophysics. Ottawa, Canada
Hsia CJC, Ma L (2009) PNPH - a therapeutic for inadequate blood flow and superoxide-, nitric oxide- dependent vascular dysfunctions. In: XIIth international symposium on blood substitutes, Parma, Italy
Hsia CJC, Ma L (2012) Hemoglobin-based multifunctional therapeutic: PNPH. Artif Organs 36:215–220
Krishna MC, Samuni A (1994) Nitroxides as antioxidants. Methods Enzymol 234:580–589
Krishna MC, Grahame DA, Samuni A, Mitchell JB, Russo A (1992) Oxoammonium cation intermediate in the nitroxide-catalyzed dismutation of superoxide. Proc Natl Acad Sci USA 89:5537–5541
Krishna MC, Samuni A, Taira J, Goldstein S, Mitchell JB, Russo A (1996) Stimulation by nitroxides of catalase-like activity of hemeproteins. Kinetics and mechanism. J Biol Chem 271:26018–26025
Kuppusamy P, Wang P, Zweier JL, Krishna MC, Mitchell JB, Ma L, Trimble CE, Hsia CJ (1996) Electron paramagnetic resonance imaging of rat heart with nitroxide and polynitroxyl-albumin. Biochemistry 35:7051–7057
Kuppusamy P, Wang P, Shankar RA, Ma L, Trimble CE, Hsia CJ, Zweier JL (1998) In vivo topical EPR spectroscopy and imaging of nitroxide free radicals and polynitroxyl-albumin. Magn Reson Med 40:806–811
Ma L, Hsia CJC (2005) Taming the hemoglobin: therapeutic and imaging applications of redox coupled nitroxide and hemoglobin. In: Xth international symposium on blood substitutes
Ma L, Hsia CJC (2013) Polynitroxylated hemoglobin as a multifunctional therapeutic for critical care and transfusion medicine. In: Chang TMS (ed) Selected topics in nanomedicine. World Science Publisher and Imperial College Press, Singapore
NIH/FDA/DOD Interagency Working Group on Oxygen Therapeutics (2011) http://www.nhlbi.nih.gov/meetings/workshops/therapeutics.htm
Nilsson UA, Olsson LI, Carlin G, Bylund-Fellenius AC (1989) Inhibition of lipid peroxidation by spin labels. Relationships between structure and function. J Biol Chem 264:11131–11135
Rozantsev EG (1970) Free nitroxyl radicals. Plenum Press, New York
Samuni A, Krishna CM, Mitchell JB, Collins CR, Russo A (1990) Superoxide reaction with nitroxides. Free Radic Res Commun 9:241–249
Shellington DK, Du L, Wu X, Exo J, Vagni V, Ma L, Janesko-Feldman K, Clark RSB, Bayır H, Dixon CE, Jenkins LW, Hsia CJC, Kochanek PM (2011) Polynitroxylated pegylated hemoglobin: a novel neuroprotective hemoglobin for acute volume-limited fluid resuscitation after combined traumatic brain injury and hemorrhagic hypotension in mice. Crit Care Med 39:494–505
Simonsen U, Christensen FH, Buus NH (2009) The effect of tempol on endothelium-dependent vasodilatation and blood pressure. Pharmacol Ther 122:109–124
Sloan EP (2003) The clinical trials of diaspirin cross-linked hemoglobin (DCLHb) in severe traumatic hemorrhagic shock: the tale of two continents. Intensive Care Med 29:347–349
Stahel PF, Smith WR, Moore EE (2008) Hypoxia and hypotension, the “lethal duo” in traumatic brain injury: implications for prehospital care. Intensive Care Med 34:402–404. doi:10.1007/s00134-007-0889-3
Stoyanovsky DA, Kapralov A, Huang Z, Maeda A, Osipov A, Hsia CJC, Ma L, Kochanek PM, Bayr H, Kagan VE (2010) Unusual peroxidase activity of polynitroxylated pegylated hemoglobin: elimination of H2O2 coupled with intramolecular oxidation of nitroxides. Biochem and Biophys Res Com 399:139–143
Tsai AG, Intaglietta M, Sakai H, Delpy E, La Rochelle CD, Rousselot M, Zal F (2012) Microcirculation and NO-CO studies of a natural extracellular hemoglobin developed for an oxygen therapeutic carrier. Curr Drug Discov Technol 9:166–172
Tsuhako MH, Augusto O, Linares E, Chadi G, Giorgio S, Pereira CA (2010) Tempol ameliorates murine viral encephalomyelitis by preserving the blood-brain barrier, reducing viral load, and lessening inflammation. Free Radic Biol Med 48:704–712
Wang D, Sun J, Solomon SB, Klein HG, Natanson C (2012) Transfusion of older stored blood and risk of death: a meta-analysis. Transfusion 52:1184–1195
Wilcox CS (2010) Effects of tempol and redox-cycling nitroxides in models of oxidative stress. Pharmacol Ther 126:119–145
Wilcox CS, Pearlman A (2008) Chemistry and antihypertensive effects of tempol and other nitroxides. Pharmacol Rev 60:418–469
Xiong Y, Singh IN, Hall ED (2009) Tempol protection of spinal cord mitochondria from peroxynitrite-induced oxidative damage. Free Radic Res 43:604–612
Zhang J, Cao S, Ma L, Hsia CJC, Koehler RC (2013) Protection from Transient Focal Cerebral Ischemia by Transfusion of Polynitroxylated Pegylated Hemoglobin, Stroke in press, Honolulu
Acknowledgments
We thank Dr. C.T. Robinson at University of South Carolina for the artwork of Fig. 16.1; Dr. P.M. Kochanek at Safar Center, University of Pittsburgh, for PNPH neuron protection and TBI studies; Dr. R.C. Koehler at Johns Hopkins University for PNPH ischemic stroke studies; and Dr. H·C. Champion formerly at Johns Hopkins University for PNPH studies in SCD mice. Most study results presented this chapter were supported by NIH and DOD (grant numbers, W81XWH-06-1-0247, NS38684, and U44-NS07032.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Ma, L., Thompson, F.M., Wang, D., Hsia, C.J.C. (2013). Polynitroxylated Pegylated Hemoglobin (PNPH): A Nanomedicine for Critical Care and Transfusion. In: Kim, H., Greenburg, A. (eds) Hemoglobin-Based Oxygen Carriers as Red Cell Substitutes and Oxygen Therapeutics. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-40717-8_16
Download citation
DOI: https://doi.org/10.1007/978-3-642-40717-8_16
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-40716-1
Online ISBN: 978-3-642-40717-8
eBook Packages: Chemistry and Materials ScienceChemistry and Material Science (R0)