Abstract
Botulinum neurotoxins (BoNTs) are the most potent human toxins known and the causative agent of botulism, and are widely used as valuable pharmaceuticals. The BoNTs are modular proteins consisting of a heavy chain and a light chain linked by a disulfide bond. Intoxication of neuronal cells by BoNTs is a multi-step process including specific cell binding, endocytosis, conformational change in the endosome, translocation of the enzymatic light chain into the cells cytosol, and SNARE target cleavage. The quantitative and reliable potency determination of fully functional BoNTs produced as active pharmaceutical ingredient (API) requires an assay that considers all steps in the intoxication pathway. The in vivo mouse bioassay has for years been the ‘gold standard’ assay used for this purpose, but it requires the use of large numbers of mice and thus causes associated costs and ethical concerns. Cell-based assays are currently the only in vitro alternative that detect fully functional BoNTs in a single assay and have been utilized for years for research purposes. Within the last 5 years, several cell-based BoNT detection assays have been developed that are able to quantitatively determine BoNT potency with similar or greater sensitivity than the mouse bioassay. These assays now offer an alternative method for BoNT potency determination. Such quantitative and reliable BoNT potency determination is a crucial step in basic research, in the development of pharmaceutical BoNTs, and in the quantitative detection of neutralizing antibodies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Botulinum neurotoxins (BoNTs) are the most potent, naturally occurring toxins known to humankind. BoNTs are produced primarily by the gram-positive bacteria Clostridium botulinum, as well as by some strains of Clostridium argentinense, and rare strains of Clostridium baratii and Clostridium butyricum (Peck 2009) (Hill and Smith 2012). BoNTs are the causative agent of botulism, which is a serious and potentially deadly neuro-paralytic human and animal disease. The toxins exert their toxic effect primarily by binding and entering peripheral cholinergic neurons and blocking acetylcholine release at neuromuscular junctions, leading to long-lasting descending paralysis (Johnson and Montecucco 2008; Schiavo et al. 2000). BoNTs are extraordinarily potent with the parenteral human lethal dose estimated to be 0.1–1 ng/kg and the oral lethal dose estimated at 1 μg/kg (Schantz and Johnson 1992; Arnon et al. 2001). This high potency, combined with the high affinity of the toxin for motor neurons and longevity of its action (up to several months), has raised serious concerns to their use as potential bioterrorism agents (Arnon et al. 2001). Remarkably, the same features have also facilitated the use of BoNTs (A and B) as extremely valuable drugs for treatment of a variety of neurological diseases as well as for cosmetic treatments. To date, BoNT/A is the most prominent serotype used in medical treatments (Truong et al. 2009; Evidente and Adler 2010) with over 1 million treatments carried out each year in the USA. Future developments of BoNTs as pharmaceuticals will no doubt utilize the specific characteristics of other BoNT sero- or subtypes in endogenous as well as recombinant BoNTs (Pickett and Perrow 2011; Cartee and Monheit 2011).
In order to establish a precise and reliable BoNT potency assay to ensure safe and consistent preparations for pharmaceutical utility, it is essential to understand the cellular biology of BoNTs and to ensure that assay considers all aspects of the BoNT intoxication process. In addition, fast, sensitive, and reliable BoNT detection platforms are desirable for research and for BoNT detection in contaminated foods, in food safety studies, and for use in the field in the case of suspected use of BoNTs for bioterrorism. Many sensitive assay platforms for BoNT detection have been developed and are applied today, with the in vivo mouse bioassay having long been regarded as the ‘gold standard’ (Solomon and Lilly 2001). Recent advances in cell-based assays now enable complementation or even replacement of the mouse bioassay for several applications. This chapter will first review the most important characteristics of BoNTs pertinent to assay systems, followed by a short overview of different BoNT detection methods, and an in-depth description of the current status of cell-based assays.
2 Botulinum Neurotoxins
2.1 Botulinum Neurotoxin Structure
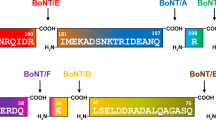
BoNTs are classified into seven serotypes (A-G) based on immunological differences (Gimenez and Gimenez 1995), and most of the serotypes are subdivided into subtypes denoted by numbers after letters (i.e. BoNT/A1-5). At least 32 subtypes have been described based on differences in their amino acid sequences and structural models. Differences range from 35 to 70 % among BoNT serotypes and from 2.6 to 32 % among subtypes within one serotype (Smith et al. 2005; Kalb et al. 2011; Raphael et al. 2010; Macdonald et al. 2011; Hill and Smith 2012).
BoNTs are modular proteins, the structure and function of which are reviewed in detail elsewhere (Montal 2010) and in this book (Bercsenyi et el. 2012; Fischer 2012; Binz 2012). In short, all BoNTs consist of a heavy chain (HC) (~100 kDa) and a light chain (LC) (~50 kDa) linked by a disulfide bond. The first solved crystal structure was that of BoNT/A (Lacy et al. 1998). Since then the structures of BoNT/B and E, and of subdomains of those and several other serotypes and subtypes have also been reported (Swaminathan 2011). These studies indicate remarkable similarity in the individual functional domains of the BoNT serotypes, but significant differences in the organization of these domains. Unique structural features in the receptor and ganglioside binding domains as well as the catalytic domains define serotype specific binding and substrate selectivity. These structural characteristics also determine BoNT species specificity and immunological and cell trafficking properties, thus lending unique characteristics to each BoNT serotype (Swaminathan 2011). This is supported by studies showing that different BoNT serotypes bind to different protein and ganglioside receptors on neuronal cell surfaces and have different cell entry kinetics. For example, BoNT/A, D, E, and F bind to SV2 receptors with different affinities (Dong et al. 2006, 2008; Rummel et al. 2009; Peng et al. 2011), whereas BoNT/B and G bind to synaptotagmin I and II (Rummel et al. 2004; Dong et al. 2003; Nishiki et al. 1994). In addition, BoNT/B, and C bind to gangliosides with greater affinity than BoNT/A (Rummel et al. 2011). BoNT/E and BoNT/A2 have been shown to enter cells faster than BoNT/A1 (Pier et al. 2011; Keller et al. 2004).
2.2 Neuronal Cell Entry and Catalysis by BoNTs
Neuronal cell entry by BoNTs is a multi-step process, which has been reviewed in detail elsewhere (Montal 2010) and in (Rummel 2012; Bercsenyi et el. 2012; Fischer 2012). The process requires fully functional BoNT holotoxins, including both the intact heavy and light chains (HC and LC). The C-terminal domain of the HC functions in specific protein and ganglioside receptor binding at the neuronal cell surface, leading to internalization of the BoNTs into endosomes by receptor mediated endocytosis. After endocytosis, protonation in the endosome contributes to membrane insertion of HC (s) coupled to LC unfolding. This is followed by HC-chaperoned LC conduction into the cell’s cytosol and subsequent release by disulfide bond reduction and its refolding in the cytoplasm of the cell (Fischer and Montal 2007a, b, Schiavo et al. 2000).
LCs of BoNTs are zinc endopeptidases that target and cleave SNARE proteins, which are core proteins involved in trafficking and release of synaptic vesicles containing neurotransmitters. The BoNT serotypes each have their own specific SNARE target and cleavage site. BoNT/A and E cleave SNAP-25 at distinct sites (Binz et al. 1994; Blasi et al. 1993a), whereas BoNT/B, D, G, and F cleave synaptobrevin 2 (VAMP-2) at distinct sites (Schiavo et al. 1992, 1993; Yamasaki et al. 1994; Schiavo et al. 1994). BoNT/C cleaves both SNAP-25 and syntaxin at unique cleavage sites (Schiavo et al. 1995; Williamson et al. 1996; Blasi et al. 1993b). In all cases, the cleavage of the SNARE protein results in a disruption of the exocytosis mechanism, and consequently a block in stimulatory neurotransmitter release, resulting in the flaccid paralysis characteristic of botulism.
2.3 Overview of the Detection of BoNTs
The field of botulinum toxins encompasses many areas including pharmaceutical use, biodefense, botulism diagnosis and treatment, as well as basic and applied research. The reliable detection of BoNTs is essential for all of these areas. The type and methodology of the detection assay or model used can influence the study outcome and conclusions, and it is important to understand the potential and limitations of the many different detection methods available. The first quantitative assay developed was the in vivo mouse bioassay (LD50 assay, MBA), in which mice are injected intraperitoneally or intravenously with dilutions of toxin and observed for signs of toxicity and death (Hatheway 1988; Schantz and Kautter 1978), and this assay has been considered the ‘gold standard’ for detection of BoNTs. BoNT activity is generally described in mouse LD50 Units [U], which is defined as the quantity of toxin required to kill 50 % of the population of injected mice. The assay is quantitative, well established, and is the only BoNT assay widely accepted by regulatory agencies of the United States for all types of samples. However, this assay has a large error (20–40 % depending on the method used and the laboratory), involves a large number of mice, incurs high costs associated with the use and housing of animals, and requires specially trained staff. Furthermore, the nature of the assay (observing mice until death) exposes the animals to pain and distress. The inclusion of a toxin standard and careful method standardization has been shown to significantly decrease the error of the mouse bioassay to approximately 15 % (Sesardic et al. 2003). However, the overall attributes of this assay still have led to a strong motivation by researchers and regulatory agencies to replace, reduce, or refine the use of animals in BoNT testing. (Adler et al. 2010). Several in vivo simulation assays, such as the hemidiaphragm assay and local injection assays (Wilder-Kofie et al. 2011; Rasetti-Escargueil et al. 2011b; Jones et al. 2006), have been developed to reduce the number of animals used (hemidiaphragm assay) and/or the suffering of animals (local injection assays). These assays are excellent research tools, but they still require the use of large numbers of animals and technical skills that make them unsuitable for medium-throughput applications such as potency determination of BoNTs or antibody screening.
Several in vitro assays for BoNT detection have also been developed, and a comprehensive review of these is presented in the preceding (Dorner et al. 2012) by Dr. Brigitte Dorner. The in vitro BoNT detection assays can be split into two groups: (1) Immunological detection methods and (2) Endopeptidase assays. While some of these assays are as or more sensitive than the MBA, they also have important restrictions. In general, immunological detection assays such as ELISA detect active as well as inactive BoNTs, and do not differentiate between holotoxin and reduced toxin in which the HC and LC are separated. Endopeptidase assays detect proteolytic activity of LCs (in reduced or nonreduced toxin), but do not require fully functional holotoxin. The buffer components or contaminating proteases have the potential to lead to falsely positive results or erroneous quantification of toxin. This problem is exemplified in the recent finding that human serum albumin itself, a commonly used excipient in pharmaceutical preparations of BoNTs, has an enzymatic activity similar to BoNT/A and C (Jones et al. 2011). A combination of specific immunological detection of the receptor-binding domain and an endopeptidase assay were recently suggested as an alternative to surmount these issues and appears to correlate with the in vivo MBA for BoNT/A (Liu et al. 2012). However, this assay is still restricted in the testing parameters of BoNT function, and extensive testing is required to ensure that potential damage to other functional regions of the toxin such as the ganglioside binding pocket, the translocation domain, or toxin aggregation do not lead to errors in potency determination.
An alternative BoNT detection method that requires the integrity of all steps of BoNT intoxication and thereby only detects fully functional holotoxin is cell-based assays, which are discussed in detail below.
3 Neuronal Cell-Based Assays
Neuronal cell-based assays (NCB assays) provide a model for BoNT detection that requires all steps of the cellular intoxication including cell surface binding, endocytosis, translocation of the LC into the cellular cytosol, and enzymatic activity of the LC on SNARE substrates. Within the past 5–7 years, cell assays have been developed that exceed the sensitivity of the mouse bioassay (Pellett et al. 2010, 2011; Whitemarsh et al. 2012; McNutt et al. 2011; Nuss et al. 2010; Kiris et al. 2011). Such cell-based assays now offer a sensitive model for the testing of fully functional BoNTs, as is necessary in the potency testing of pharmaceutical and research preparations of BoNTs. This opens the possibility of using cell-based assays as an alternative detection method to the MBA. In fact in fall of 2011, Allergan Inc., the distributor of the pharmaceutical BoNT preparation onabotulinumtoxin A (Botox®), announced that the Food and Drug Administration (FDA) for the first time had approved a cell-based assay for potency testing of its product. However, details about this assay have not been released.
In addition to BoNT detection, NCB assays provide an alternative assay to the MBA for the sensitive and specific detection of neutralizing antibodies to BoNTs (Whitemarsh et al. 2012; Pellett et al. 2007). NCB assays also have utility as a research model to study many characteristics of BoNTs, including binding to the neuronal cell surface, cell entry, intracellular catalytic activity of the LC, and inhibition of neurotransmitter release by the cells, as well as other factors.
3.1 NCB Assay Methods
Irrespective of the source of cells, all NCB assays require incubation of the cells with BoNTs for a defined time period, followed by removal of the toxin and a quantitative endpoint for determining toxin activity. Among the most specific endpoints for BoNT activity is SNARE cleavage, and this endpoint can be used in any neuronal cell type. SNARE cleavage can be determined in cell lysates by Western blot (Pellett et al. 2010; Whitemarsh et al. 2012; McNutt et al. 2011) or by ELISA (Nuss et al. 2010), or in live cells by quantitative immunofluorescence methods using cleavage-specific antibodies (Kiris et al. 2011). An alternative proposed endpoint is the introduction of a sensor into neurons such as a SNARE-FRET construct, which undergoes a change in fluorescence emission after specific BoNT cleavage inside the cells (Dong et al. 2004). While this approach has been shown to work in cells transiently transfected with FRET constructs (Dong et al. 2004), only one cell line stably expressing such a sensor has been constructed so far, and this cell line is about 2–3 orders of magnitude less sensitive than the MBA (Biosentinal Inc). The sensitivity of this endpoint compared to SNARE cleavage or neurotransmitter release remains unknown.
Another important, but less specific endpoint, is inhibition of neurotransmitter release, which can be measured in primary neuronal cell cultures and stem cell-derived neurons, as well as in some continuous cell lines. Most commonly, the cells are pre-loaded with radioactively labeled neurotransmitter, followed by measurement of the released radioactivity (Benatar et al. 1997; Bigalke et al. 1978; Keller and Neale 2001; McInnes and Dolly 1990; Sheridan et al. 2005). Other methods that determine endogenous neurotransmitter release include direct measurement by HPLC or immunoassay (McNutt et al. 2011; Yaguchi and Nishizaki 2010; Welch et al. 2000), or indirect measurement detecting enzymatic breakdown products (McMahon and Nicholls 1991) or the postsynaptic currents by voltage clamping (Akaike et al. 2010). The use of a fluorescent dye as a marker of neurotransmitter release has also been suggested (Rasetti-Escargueil et al. 2011a; Tegenge et al. 2012). Another potential but not yet developed endpoint is the measurement of electrical conductance of an entire population of cultured neurons.
The incubation time of the cells with BoNT is an important factor impacting sensitivity and is cell type specific; most cells require 24–72 h incubations for maximal sensitivity. Short incubation times of only a few hours require significantly increased toxin doses to reach the desired sensitivity. Chemically, stimulating neuronal activity in cells by modifying the toxin exposure medium or buffer to contain 56–80 mM KCl and 1–2 mM CaCl2 can dramatically increase the BoNT uptake speed in some cells to 2 to several minutes (Pier et al. 2011; Keller et al. 2004; Whitemarsh et al. 2012). After removal of extracellular toxin, several hours of incubation is then required to achieve efficient SNARE cleavage, which continues to increase for 24–48 h. While useful in research applications, this approach does not reach the same sensitivity as a 24 or 48 h toxin exposure and requires at least 100-times more toxin. This indicates that both toxin binding/cell entry and SNARE proteolysis are rate limiting factors.
When exposing cultured cells to BoNTs, it is important to not only control the toxin concentration, which sometimes is the only reported parameter, but also the total volume of medium added to the cells and the specific activity of the toxin. All of these factors determine sensitivity. For example, 200 μl of a 1 pM solution of BoNT/A provides four times more toxin to the same number of cells as 50 μl of the same solution, and research in our laboratory has indicated that this affects SNAP-25 cleavage (Pellett et al., unpublished data). In addition, the specific activity of the toxin is an extremely important factor that needs to be considered when using cells (unless the NCB assay is used in a standardized and controlled format to determine specific activity), as only fully functional BoNT is able to enter the cells. Thus, the same molar quantity of a toxin preparation containing 95 % of fully functional holotoxin will have a much greater activity than a toxin preparation in which 50 % of the toxin is inactive through mishandling or degradation. Additional components included in the reaction mix such as proteins, excipients salts, metals, sugars, detergents, and many other factors may also affect the outcome of a cell-based assay. Thus, experiments using cell-based assays should always describe the toxin source and characteristics, specific activity, exposure volume, and toxin concentration in molar amounts, mass, and U/well, and the complete reaction composition.
3.2 Types of Cell-Based BoNT Detection Assays
While cell-based assays allow for a dramatic reduction in animal testing and enable BoNT potency determination, it is important to understand the characteristics and limitations of the various cell-based assays. All cell-based assays present a ‘closed system’. Furthermore, they do not determine effects of pharmacokinetic properties that might play important roles in different in vivo assay (e.g., MBA) such as distribution, clearance, diffusion, transport, and other parameters. Therefore, BoNT studies conducted in cell-based assays need to be interpreted with these restrictions in mind, and some studies may require additional research using specific in vivo models. Another important consideration is the cell type and its source. Continuous cell lines are relatively easy to maintain and inexpensive compared to primary and stem cell-derived neurons, but most are derived from cancerous cells and may have altered gene expression profiles that affect their BoNT sensitivity and cellular biology. Primary neurons require the sacrifice of some animals and skilled personnel for preparation, but are relatively inexpensive. These cells can be obtained from different sources (e.g., spinal cord, dorsal root ganglion, hippocampal, or cortical neurons) and different species, which may affect the outcome of the studies. In addition, primary cells do not constitute a pure neuronal population, but rather are mixed cultures of neurons and supportive cells such as glial cells. Stem cells can be differentiated to different types of neuronal subpopulations, although the current state of stem cell technology limits the neuronal subpopulations and purity that can be achieved. As BoNT research advances to analyze different BoNT sero- and subtypes and recombinant BoNTs, cell models offer a powerful research model and assay platform if the characteristics of the model are carefully considered. Differences among cell models are discussed in the following sections.
3.2.1 Continuous Cell Lines for BoNT Detection
Several continuous neuronal cell lines derived from cancer cells have been used to detect BoNTs. The most commonly used cell lines are neuro-2a (mouse neuroblastoma) and PC12 (rat pheochromocytoma) cells (Schiavo et al. 1993; Yowler et al. 2002; Benatar et al. 1997). Both cell types are relatively insensitive to BoNTs, requiring a long incubation time for 2–3 days and large quantities of BoNTs (in the nM range) to achieve adequate SNARE cleavage. The sensitivity of neuro-2a cells was first reported to be in the range of 0.67–6 nM (Yowler et al. 2002), while other studies have reported 50 % SNAP-25 cleavage with approx. 30 nM BoNT/A (or about 30,000 U) (Dong et al. 2006; Pier et al. 2011; Fischer and Montal 2007a; Conway et al. 2010). Sensitivity can be increased to about 2 nM (~2,000 U) by over-night pre-incubation of the cells with 25–50 μg/ml of the ganglioside GT1b (Pier et al. 2011; Yowler et al. 2002).
For PC12 cells, inhibition of acetylcholine release by BoNT/A was reported with approximate EC50s of ~0.02 nM in cells differentiated with nerve growth factor (NGF) (Ray 1993), while noradrenaline release at 120 nM was reported in undifferentiated cells (Shone and Melling 1992). In our laboratory, 50 % cleavage of SNAP-25 was achieved in undifferentiated PC12 cells at ~2,000 Units (~2.5 nM) after 48 h BoNT/A exposure (unpublished data). Plating of the cells onto collagen coated plates and pre-loading with 25 μg/ml of GT1b in serum-free medium increased the sensitivity to an EC50 of 400 U (~500 pM). Sensitivity was increased even further to ~100–200 U (EC50) when the cells were exposed to toxin in a modified neurobasal medium (cell stimulation medium) containing 56 mM KCl and 2.2 mM CaCl2 (Invitrogen custom medium) for 24 h, independent of GT1b pre-incubation (Pellett et al., unpublished data). Preloading PC12 cells with the ganglioside GT1b sensitized the cells to BoNT/B, allowing detection of VAMP2 cleavage with 50 nM BoNT/B (Dong et al. 2003).
There are other important characteristics of the PC12 and neuro2A cell lines with regard to BoNT testing. Besides the obvious morphological differences, PC12 cells are from rat origin and express only the SV2A isoform as receptor, whereas neuro-2a mouse cells express only the SV2C isoform (Dong et al. 2006). Both cell lines have unique ganglioside profiles. Neurite sprouting can be induced in PC12 cells by addition of NGF or pituitary adenylate cyclase-activating polypeptide (PACAP) (Ravni et al. 2006), while neuro-2a cells are neuronal growth factor insensitive. While BoNT/A analysis in neuro-2a cells used SNAP-25 cleavage as an endpoint, PC12 cells can release neurotransmitter, and thus inhibition of neurotransmitter release can serve as an additional endpoint in these cells.
Other cell lines used in BoNT research include the human neuroblastoma cell line SH-SY5Y (Purkiss et al. 2001). This cell line detected SNARE cleavage by several BoNT serotypes with significantly different potencies, and the EC50s ranged from 0.54 nM for BoNT/C to 300 nM for BoNT/F. Further research on pre-differentiating the SH-SY5Y cell line by addition of retinoic acid for 5 days followed by culture in medium containing BDNF markedly increased the BoNT/A sensitivity to 100 pM as determined by a neurotransmitter release assay. Pre-incubation of the cells with GT1b further increased sensitivity to 35 pM for BoNT/A (Rasetti-Escargueil et al. 2011a; Sesardic and Das 2007). BoNT/C and D/C can also sensitively be detected in neurons differentiated from the mouse embryonal carcinoma cell line P19. Differentiation of these cells in the presence of 0.5 μM RA for 4 days followed by a 4 day maturation period in serum-free medium results in a population of neurons with cholinergic characteristics (Parnas and Linial 1995), and a sensitivity to BoNT/C and C/D similar to that in primary hippocampal cells (EC50 of 217 pM (syntaxin cleavage) and 310 pM (SNAP-25-cleavage), and 58 pM VAMP2 cleavage, respectively) (Tsukamoto et al. 2012).
The human neuroblastoma derived BE(2) M17 cell line shows SNAP-25 cleavage by BoNT/A with an EC50 of about 1 nM, which was slightly improved by pre-incubation of the cells with the ganglioside GT1b. Norepinephrine release was inhibited by 10 nM BoNT/A (Lee et al. 2008). In addition, BoNT/C inhibited norepinephrine release with an approximate EC50 of ~1 nM, but BoNT/B, D, E, F, and G did not significantly inhibit norepinephrine release at 10 nM concentrations (Lee et al. 2008). The human neuronally committed teratocarcinoma cell line NT2, which can be differentiated to fully functioning postmitotic neurons, was recently tested as a model for BoNT/A intoxication (Tegenge et al. 2012). After a 1–3 h exposure of cells to 1 nM BoNT/A, transmitter release was significantly inhibited. However, results showing long-term exposure of these cells and effects of other factors have not been published.
While no definitive data have been released or published yet, patent descriptions indicate that Allergan has developed a cell-based assay for the onabotulinumtoxin A (Botox®) product using a clonal cell line derived from the human neuroblastoma SiMa cell line (Zhu et al. 2010). This cell line appears to have an EC50 of about 1 pM for BoNT/A if pre-differentiated in serum-free medium containing GT1b, which is of comparable sensitivity to the mouse bioassay.
Other cell lines that have been tested for BoNT detection include the human neuroblastoma cell line SK-N-SH, which requires addition of 50 μg/ml of GT1b for the detection of low nM amounts of BoNT/A (Yowler et al. 2002). Rat neuroblastoma B35 cells and the mouse hypothalamus N-44 cells do not express sufficient levels of SNAP-25 to be useful in a BoNT/A assay using SNAP-25 cleavage as an endpoint. The level of SNAP-25 did not change in B35 cells upon differentiation by serum deprivation. Whereas differentiation of N-44 cells by NGF treatment induced SNAP-25 expression, the cells were resistant to BoNT/A treatment at low nM amounts (Pellett et al., unpublished data). The human cortical neuronal cell line HCN1 was disregarded for BoNT assay since this cell line grows extremely slow and is difficult to propagate. The mouse motor neuron like cell line NSC-34 expresses high levels of SNAP-25 and was differentiated to motor neuron like morphology by serum deprivation, but was insensitive to BoNT/A at low nM amounts (Kiris et al. 2011) and Johnson lab, unpublished data). The known sensitivities of different neuronal cell lines to BoNT serotypes (subtypes 1, respectively) are summarized in (Table 1).
3.2.2 Primary Cells for BoNT Detection
Primary cells have been used as model systems for BoNT detection for 35 years or longer. Research on primary cells has helped immensely in our understanding of the biology and characteristics of BoNTs, including SNARE protein cleavage, inhibition of neurotransmitter release, duration of action, and cell entry mechanisms. A variety of primary cells derived from rat, mouse, or chicken embryos have been used (Keller et al. 2004; Pellett et al. 2007, 2010; Sheridan et al. 2005; Stahl et al. 2007; Bigalke et al. 1985). Among these are cortical neurons (Pier et al. 2011; Stahl et al. 2007; Saadi et al. 2012), spinal cord neurons (Keller et al. 2004; Pellett et al. 2007, 2010; Bigalke et al. 1985), hippocampal neurons (Verderio et al. 2007; Dong et al. 2007), and dorsal root ganglion cells (Welch et al. 2000; Stahl et al. 2007; Duggan et al. 2002). Early experiments in primary neurons indicated much greater sensitivity than in continuous cell lines; however, these assays did not have sensitivity comparable to the mouse bioassay. In the past few years, improvements in cell culture materials and methods have enabled primary neuronal cell assays to reach sensitivity similar to or even exceeding that of the mouse bioassay, with EC50 values as low as 0.3 mouse LD50 Units of BoNT/A in a 96-well format (Pellett et al. 2010, 2011; Whitemarsh et al. 2012).
One of the major advances is the culture of primary neurons in serum-free medium optimized for neurons (e.g., Neurobasal medium supplemented with B27 and glutamax, all from Invitrogen) (Pellett et al. 2007; Xie et al. 2000; Kivell et al. 2001; Brewer 1995; Brewer et al. 1993). This medium avoids the necessity of adding cytostatic compounds to prevent overgrowth of nonneuronal cells and results in robust and stable primary neuron cultures that can be maintained for weeks to months. In addition, plating matrices such as collagen, laminin, and matrigel are now widely available, facilitating the surface attachment of primary cells and likely also contributing to the maturation process of the cells after plating (Kohno et al. 2005; Uemura et al. 2010). Preparation of primary cells generally requires some skills and practice but can be cost-effective (e.g., one pregnant rat can yield 5–6 96-well plates of spinal cord cells), and in our experience primary cells yield very reproducible results in quantitative BoNT detection. Figure 1 outlines the steps involved in preparing and using primary rat/mouse spinal cord cells for BoNT detection. In addition, several companies now offer tissue pieces such as isolated rat or mouse embryonic spinal cords, hippocampi, or cortical pieces. While significantly more expensive, these sources allow for rapid and simple culture of primary neurons by scientists with minimal experience in primary cell preparation.
Steps involved in preparing and using primary rat/mouse spinal cord cells for BoNT detection by Western bot. The uterus containing the pups of an E15 pregnant Sprague–Dawley rat or an E13 pregnant mouse (e.g., NIH Swiss) are removed and placed in dissection medium (Hanks balanced salt solution, 10 mM HEPES, 20 mM glucose. The pups are dissected out, and spinal cords removed and cleaned of all membranes and ganglia. The spinal cords are minced, and cells dissociated by trypsinization using 10 % TrypLE express (Invitrogen) in dissection medium, followed by trituration in 1 ml of culture medium (Neurobasal with B27 and glutamax) pre-warmed to 37 °C. Live cells are counted by trypan exclusion assay, and 75,000 cells/well are plated into 96-well TPP plates (MidSci) that have been coated with type I rat tail collagen (BD Biosciences), or matrigel (BD Biosciences) according to manufacturer’s instructions. The cells are allowed to mature at 37 °C in a humidified 5 % CO2 atmosphere for at least 18 days with bi-weekly changes of culture medium before they are used in the toxin assay. For the toxin assay, toxin dilutions are prepared in culture medium and added to the cells. After a specified incubation time, the toxin is aspirated, and the cells lysed in 75 μl of 1× LDS lysis buffer (Invitrogen). The samples are separated using 12 % Bis–Tris gels and MES running buffer (Invitrogen), and analyzed by Western blot using a monoclonal anti-SNAP-25 antibody (Synaptic Systems, Germany) and densitometry. The details of this method are described in (Pellett et al. 2007, 2010). The methods for preparation and use of other primary cells are similar
Unlike continuous cell lines, which differ in their sensitivity to BoNT serotypes based on unique expression of surface receptors, ganglioside profiles, and other often not well-defined characteristics, primary cells present normal neurons which can be used to study all BoNT serotypes and subtypes. In fact, primary cells are ideal models to study differences between BoNT sero- and subtypes in the respective neuronal subpopulations. Spinal cord cells or motor-neuron-enriched spinal cord cells would be expected to be the most relevant and sensitive BoNT cell model based on the neuromuscular symptomatology of botulism. However, other primary cells such as cortical neurons, hippocampal cells, and dorsal root ganglion cells also seem to be exquisitely sensitive to BoNTs and have been used as study models (Pier et al. 2011; Welch et al. 2000; Stahl et al. 2007; Saadi et al. 2012; Verderio et al. 2007; Dong et al. 2007; Duggan et al. 2002).
While most primary neuronal cell models are very sensitive to BoNT/A, some cell models, such as primary rat spinal cord cells, differ in their sensitivity to other BoNT serotypes. This can be explained by species-specific differences in BoNT receptors and/or SNARE proteins, as well as by other species- or cell type-specific characteristics. It is important to remember that the specific activity of all BoNT serotypes is currently determined in the mouse bioassay, and thus do not necessarily reflect the activity in other species including humans. This is exemplified by the differential potency of pharmaceutical BoNT/A and B in humans (Dressler and Benecke 2007; Flynn 2004), which is likely due to a variation in the amino acid sequence between mouse and human synaptotagmin II (the BoNT/B receptor) (Strotmeier et al. 2012; Peng et al. 2012). Thus, when using primary neurons, both the animal source and the neuronal subpopulation should be taken into careful consideration.
3.2.3 Stem Cell-Derived Neurons for BoNT Detection
Embryonic stem (ES) cells are pluripotent cells derived from the inner part of a blastocyst. ES cells can be propagated and frozen similar to continuous cell lines and can be differentiated into any cell type, including neurons. Mouse ES (mES) cells can be differentiated into neurons by addition of retinoic acid. Addition of purmorphamine or sonic hedgehog further directs this differentiation to motor neurons (Zhang 2006; Wichterle and Peljto 2008). This differentiation takes about 2 weeks, and the resulting cells are nearly as sensitive as primary neurons to all BoNT serotypes, and have equal sensitivity to the MBA (Pellett et al. 2011; McNutt et al. 2011; Kiris et al. 2011). However, differentiation of mES cells to neurons, and especially to motor neurons, requires significant experience and practice working with stem cells. Figure 2a outlines the major steps involved in mES cells differentiation to neurons, including propagation of undifferentiated mES cells, differentiating the cells into embryoid bodies (EBs), inducing neuronal differentiation of the EBs, and dissociation and plating of the differentiated neurons, followed by maturation (Fig. 2). Many variables can affect the outcome of neuronal differentiation, and thus sensitivity to BoNTs, including the quality of the materials, concentration of retinoic acid, time of retinoic acid addition and incubation, the dissociation of EBs, the plating matrix, medium composition, and so on. Even with standardization of the protocol, factors such as the source, storage and age of medium components, and cell handling practice can influence the differentiation success. This makes implementation of a BoNT detection assay using mES cells derived neurons challenging in a (nonstem cell focused) research lab and probably also in a commercial setting.
Steps involved in preparing and using mouse embryonic stem cell (mES) derived neurons a or purchased human induced pluripotent stem (hiPS) cell-derived neurons b for BoNT detection by Western blot. a: The mES cells are maintained in a basic maintenance medium containing human leukemia inhibitory factor (LIF) to avoid cell differentiation, such as DMEM/F12, 15 % fetal bovine serum, 1× nonessential amino acids, sodium pyruvate (1 mM), glutamax, 2-mercaptoethanol (0.1 mM) and LIF, (1,000 units/ml) on 6-well plates that have been coated for 1 h at 37 °C with 0.1 % gelatin. Medium is replaced every 2 days, and cells are split by trypsin–EDTA digestion. The cells can be propagated and cryopreserved at this stage. For differentiation to neurons, ~2–4 × 106 cells are transferred to a 100 mm Petri dish in differentiation medium such as MES/SR (same as MES, but with 15 % Knockout serum replacement instead of FBS and no LIF) in order to induce embryoid body (EB) formation. After 2 days 0.5–5 μM retinoic acid is added, and for motorneurons 1 μM purmorphamine is also added. After 4 days, the EBs are digested with accutase or TrypLE, and 75,000 cells/well are seeded into 96-well plates coated with 1 μg/well of laminin in culture medium (such as Neurobasal supplemented with B27, 1 μM cAMP, and 20 ng/ml GDNF) to maintain neurons. The neurons are allowed to mature in culture for 9 days before use in toxin assays. For details of this method see (Pellett et al. 2011; McNutt et al. 2011; Kiris et al. 2011). b: The hiPS cells derived neurons are purchased as already differentiated and cryopreserved cells. The cells are thawed and seeded into 96-well plates at a density of 30–40,000 cells/well (Whitemarsh et al. 2012). For the toxin assay, toxin dilutions are prepared in culture medium and added to the cells. After a specified incubation time, the toxin is aspirated, and the cells lysed in 50 μl of 1× LDS lysis buffer. The samples are separated using 12 % Bis–Tris gels and MES running buffer, and analyzed by Western blot using a monoclonal anti-SNAP-25 antibody and densitometry
Differentiation of human embryonic stem (hES) cells to neurons is even more involved and requires at least 6 weeks. In addition, the differentiation rate of hES cells is significantly lower than that of mES cells (50 vs. 90 %) (Zhang 2006; Hu and Zhang 2010). Furthermore, there is considerable ethical controversy in the use of hES cells for various purposes. Probably for this reason, a BoNT detection assay using hES cell-derived neurons has not been developed.
Major advances in stem cell research during the past decade have enabled the conversion of normal adult somatic cells (e.g., skin or blood cells) to stem cells by inducing expression of a small set of genes that is otherwise silenced in these cells (Takahashi et al. 2007; Yu et al. 2007). The resulting cells are pluripotent-like ES cells and can be propagated and frozen in the undifferentiated state. These human-induced pluripotent stem (hiPS) cells can be differentiated into mature human neurons much like ES cells. In addition, methods have now been developed for cryopreservation of differentiated neurons or partially differentiated neurons from hiPS cells for commercial purposes. Thus, such neurons are now commercially available, enabling the use of high quality human neurons for BoNT detection assays in most lab settings as well as in the pharmaceutical industry while requiring only basic knowledge about tissue culture techniques (e.g., seeding of the neurons into tissue culture plates and medium changes for every 2–3 days, Fig. 2b). Importantly, commercially well-prepared cells undergo quality control tests, ensuring consistency among different cell lots within the defined parameters used for quality control standards of the company.
Human iPS cells derived neurons have been recently shown to be a highly sensitive cell model for BoNT detection with an EC50 around 0.3 mouse LD50 Unit (U) for BoNT/A (Whitemarsh et al. 2012). The hiPS cells derived neurons have also shown utility in detection of neutralizing antibodies to BoNTs (Whitemarsh et al. 2012). These cells have much potential and relevance for research and commercial detection of BoNTs and antibodies, including their human origin, and the fact that these cells resemble normal somatic neurons (unlike cancerous cells in continuous cell lines). Interestingly, the EC50s in these neurons differed for different serotypes of BoNTs (BoNT/A: ~0.3 U, BoNT/C: ~0.4 U, BoNT/E: ~1.8, BoNT/B: ~16 U). Limited human studies confirm serotype specific differences in humans with a 40-fold decreased activity of BoNT/B compared to BoNT/A (Johnson and Montecucco 2008; Eleopra et al. 2004; Eleopra et al. 1998). This highlights the importance of considering species specificity when assaying different BoNT serotypes, which are currently all assayed in mice. The steps involved in the use of cryopreserved hiPS cells derived neurons for BoNT detection is shown in (Fig. 2b).
3.3 Applications of NCB Assays
The high sensitivity, specificity, reproducibility, and low error of NCB assays using primary or stem cell-derived neurons enable the introduction and further development of standardized cell-based assays to complement and to eventually replace the mouse bioassay for many uses. The most important applications requiring an assay that measures all steps of the intoxication process include potency determination of research and pharmaceutical BoNTs, quantitative detection of neutralizing antibodies, and use as research models. Other applications may include the sensitive detection of BoNTs in foodstuffs or in field samples, although these applications would require a combination of the cell-based assay with a BoNT isolation and purification step. The following paragraphs discuss considerations for using cell-based assays for potency determination of pharmaceutical BoNTs, neutralizing antibody detection, and as a research model.
3.3.1 Potency Determination of Pharmaceutical BoNTs
BoNTs are extremely valuable drugs for treatment of a variety of neurological diseases as well as for cosmetic treatments. To date, BoNT/A and to a lesser extent BoNT/B are being employed as pharmaceuticals (Cartee and Monheit 2011; Dressler and Benecke 2007). The number of treatments is steadily increasing with currently over 1 million treatments carried out each year in the United States alone. A reliable and well-established assay for BoNT potency testing is required to ensure safe and consistent preparations for pharmaceutical utility. This assay should test for fully functional holotoxins in a quantitative and reproducible manner, taking into consideration all steps of cellular intoxication (e.g., cell binding, endocytosis, translocation, and intracellular enzymatic activity) (Adler et al. 2010; Sesardic and Das 2007). Until recently, the MBA was the only assay approved and used for this purpose. However, the drawbacks of the MBA have led to a strong impetus by researchers and regulatory agencies to find alternatives for the potency determination of pharmaceutical preparations of BoNTs (Adler et al. 2010). Cell-based assays are especially well suited for this application, because they test for fully functional BoNTs that undergo all steps of cell intoxication are specific, and exceed the sensitivity of the mouse bioassay. Since Allergan’s announcement in fall of 2011 that the FDA for the first time had approved a cell-based assay for the potency testing of its product (Botox®), the interest surrounding cell-based assays has increased markedly among commercial producers of pharmaceutical BoNTs. Research has shown that both primary cells and stem cell-derived neurons have the required sensitivity. However, the need for repeated new preparations of primary cells and the quality control issues involved makes it unlikely that this cell model will be established in a commercial setting. On the other hand, stem cell-derived neurons appear to be an ideal cell system for a potency assay, as they provide normal neurons (as opposed to cancerous cell lines), and neurons derived from hiPS cells are species specific. In order to introduce these cell assays for potency determination of pharmaceutical BoNTs, they will need to be optimized and standardized for each product, and cross-validated against the MBA. It cannot be assumed that a pharmaceutical preparation of BoNT in excipient and possibly containing complex proteins will yield the same EC50 values as a purified 150 kDa BoNT/A product that is stored as a concentrated stock and diluted in cell culture medium. The excipient composition as well as the potential presence of complex (or other) proteins may affect the sensitivity of a NCB assay. Thus, assay conditions need to be optimized for each specific use (product) to ensure required sensitivity and accuracy. For example, commonly used stabilizers such as human serum albumin likely increase sensitivity, and saline commonly used to re-suspend lyophilized BoNT in vials will need to be sufficiently diluted in order to avoid salt effects on the cells. After such optimization studies are completed and a toxin standard has been validated, the cell assay has the potential to fully replace the MBA for BoNT potency determination of pharmaceutical BoNTs, although periodic control assays using the MBA may be advisable. Unlike in the MBA, which is highly dependent on proper injection techniques and mice strains, the methods used in a NCB assay can readily be standardized among different laboratories. Thus, replacement of the MBA with a carefully optimized and standardized NCB assay has the potential to significantly reduce the intra-laboratory error currently observed during BoNT potency evaluations (Sesardic et al. 2003). In addition, using a human specific cell model will allow for species-appropriate potency evaluation of different BoNT sero-or subtypes. It is well known that significantly more BoNT/B mouse LD50 Units are required to achieve the same therapeutic effect as with BoNT/A in humans (Dressler and Benecke 2007; Flynn 2004). Recent evidence suggests that the predominant mechanism underlying this is species-specific differences in the BoNT/B and G cell surface receptor synaptotagmin II between humans and chimpanzees versus rats and mice (Strotmeier et al. 2012; Peng et al. 2012). Determining pharmaceutical BoNT Units derived from human neurons EC50 values (e.g., human neuron EC50 Unit) will likely aid physicians in converting from one BoNT product to another without the confusion of having to use a different number of Units among products.
3.3.2 Detection of Neutralizing Antibodies to BoNTs
Despite their effective use of BoNT/A and BoNT/B in clinical applications, a major adverse effect has been the formation of neutralizing antibodies that make patients refractory to treatment (Dressler et al. 2010; Borodic 2007; Muller et al. 2009; Dressler 2004). The estimates for the percentage of patients developing neutralizing antibodies vary and are dependent on the toxin dose, indication, number of repeat injections, and the commercial product. In some estimates, as many as 5–12 % of patients who received repeated BoNT/A treatments for spasticity developed resistance to treatments due to the presence of circulating neutralizing serum antibodies (Muller et al. 2009; Cordivari et al. 2006; Kessler and Benecke 1997). Currently, patients are not routinely monitored for antibody formation during their treatment regime (Sesardic et al. 2004). In vitro methods, such as ELISA, are sensitive and specific but do not currently differentiate between neutralizing and nonneutralizing antibodies. The MBA can specifically detect neutralizing antibodies, but requires a large number of mice and is not sufficiently sensitive to detect low levels of antibodies in some treatment-resistant patients. A currently used alternative test system is the mouse phrenic nerve hemidiaphragm assay (Dressler et al. 2002, 2005; Rasetti-Escargueil et al. 2009, 2011b), which quantitatively detects neutralizing antibodies without performing live-animal experiments and is also commercially available for patients. In addition, local injection assays, such as remote point injection in the forehead (Borodic et al. 1995) or the EDB (extensor digitorum brevis) assay, in which BoNT/A is ‘test’ injected into the EDB muscle of the patient and electrophysiological measurements, are taken before and after the injection (Cordivari et al. 2006; Kessler and Benecke 1997). While the latter assays are inexpensive, do not require the use of animals, and correlate with clinical observations of BoNT/A effectiveness, they require the injection of BoNTs into a patient for testing purposes only and are not practical.
NCB assays offer a sensitive alternative that is specific for neutralizing antibodies, provided a qualified cell model as described above is used. As proof in point, a cell-based assay using primary rat spinal cord cells was shown in a pilot study to be about 10 times more sensitive than the mouse bioassay in detection of neutralizing antibodies and correlated 100 % with patient outcome (Pellett et al. 2007). Similarly, neurons derived from hiPS cells have been shown to be about 10 times more sensitive than the MBA for neutralizing antibody detection (Whitemarsh et al. 2012). Future studies are needed to optimize and standardize a cell-based assay for this purpose and to confirm correlation of patient nonresponse to BoNT treatments and detection of neutralizing antibodies. Factors that may affect a cell assay for antibodies include the quality and sterility of the serum, which are critical to avoid cell damage, the concentration of serum and toxin used in the assay, and the incubation time and temperature of toxin with antibody or serum prior to cell exposure. When choosing a cell model, it is also important to consider that the BoNT sensitivity of the cells will also determine the neutralizing antibody detection sensitivity as more antibodies will be needed to neutralize greater amounts of toxin. Additionally, consideration must be given to the serum source and the endpoint used. In clinical trials using animals, the serum should be collected in a sterile manner and drugs that potentially may cause cytotoxicity or affect the serum quality by inducing red cell lysis (e.g., pentobarbital) should be avoided as a means of euthanasia before serum collection. If a nonspecific endpoint such as inhibition of neurotransmitter release is used instead of a SNARE cleavage endpoint, potential direct effects of the serum on this endpoint must also be evaluated.
3.3.3 Research Applications
Research on BoNTs requires the determination of BoNT specific activity. At present, this is generally determined using the MBA, but as discussed above specific toxicity determination can now be performed in cell-based assays. In addition, many research projects often address important biological properties of BoNTs such as cell binding and trafficking mechanisms. Different cell models may provide advantages and disadvantages to each specific research application. Continuous cell lines lack sensitivity but might provide characteristics desirable for a specific purpose, such as the expression of a particular surface marker. Cell lines can be manipulated to transiently or stably express a desired protein or marker, or to increase, decrease, or abolish expression levels of a particular gene. Studies demonstrating use of such techniques have, for example, led to the identification of the receptor SV2, with SV2C being the favored isoform, and polysialiogangsliosides as the receptors for BoNT/A (Dong et al. 2006; Yowler et al. 2002), strengthening the ‘dual receptor’ model that necessitates BoNT binding of both, a protein and a ganglioside receptor for cell entry (Montecucco 1986). While such techniques are now also possible in stem cells or stem cell-derived neurons, the methods used in those cells are much more difficult or cost-prohibitive for many studies.
Other research applications such as cellular entry and trafficking studies benefit most from using a research model that most closely mimics the behavior of BoNT in normal human cells. Since the symptoms of botulism indicate that BoNTs primarily affect cholinergic neurons, primary cell models such as mouse or rat primary spinal cord cells could present good models. In fact, many important discoveries about botulinum toxin activity have been made in primary cell models, such as for example, the much longer duration of the BoNT/A LC activity in neurons compared to the BoNT/E LC (Keller et al. 1999). However, these models are not human specific, and potential species-specific differences of the cells have to be considered when interpreting these studies. For example, the differences in human/primate and mouse/rat synaptotagmin II (Strotmeier et al. 2012; Peng et al. 2012) likely result in BoNT/B entering human neurons via the weaker synaptotagmin I receptor. Besides explaining the difference in BoNT/A and B potency in humans, this also has important implications with regard to neuron specificity of BoNT/B, considering the differential expression of synaptotagmin I and II in the central nervous system (Ullrich et al. 1994).
Neurons derived from hiPS cells offer a human specific alternative; however, the currently available neurons resemble forebrain neurons rather than neurons from the peripheral nervous system. Neurons derived from mES cells can be differentiated to mixed central nervous system neurons or motor-neuron enriched cultures, and both neuronal populations appear to be equally sensitive to BoNTs (Pellett et al. 2011; McNutt et al. 2011; Kiris et al. 2011). While all of these cell models have limitations that need to be considered, they are sensitive to BoNTs, and therefore are good models for research applications such as the screening of new BoNT antitoxins or inhibitors. The neurons derived from hiPS cells are about 10 times more sensitive for fast (5 min) BoNT cell entry during chemical cell stimulation compared to primary neurons (Whitemarsh et al. 2012), and thus are especially well suited for experiments such as screening and analyses of intracellular BoNT inhibitors. In these experiments, cells are exposed to BoNT prior to addition of potential inhibitors, which avoids potential secondary effects of inhibitors on BoNT cell entry (Fischer et al. 2009).
While cell models may not entirely replace in vivo studies, they provide an excellent research model to study the biological properties of BoNTs and inhibitors in a ‘closed’ neuronal model. Thus, in a hypothetical situation, a specific BoNT inhibitor may not be stable in vivo and be cleared out of the system, but may effectively enter neuronal cells and inhibit LC activity inside the cells. Such an inhibitor would be missed if only screened in animals, but identification in cell assays and modifications to improve the stability in vivo might yield a new and important drug for treatment of botulism. Equally important, cell assays allow the screening of a moderately large number of inhibitors or antitoxins before testing in animals and thereby significantly reduces the number of animals used.
4 Future Perspectives and Conclusion
Throughout the years, cell-based assays have found many applications in the field of botulinum toxins, aiding in the biologic and molecular understanding of these important toxins. The recent introduction of highly sensitive and human specific cell models enables novel areas of basic study, as well as the use of cell-based assays for commercial uses in BoNT potency determination and neutralizing antibody screening. Future developments of pharmaceutical BoNTs include the use of other BoNT sero-or subtypes and recombinantly altered BoNTs, as well as novel indications (Pickett and Perrow 2011; Cartee and Monheit 2011; Rummel et al. 2011). In addition, improved vaccines and antitoxins are being developed, and the search for an effective cure or treatment of botulism beyond antitoxin, which has to be administered within the first 24–48 h after toxin exposure, continues. Research efforts continue to identify new information on the biologic and molecular function of BoNT sero-and subtypes. NCB assays offer a unique study model that can be used to examine cell binding, entry, translocation, and intracellular trafficking and catalytic activity, and are an essential tool in these developments. The most promising NCB assays for replacement of the MBA use neurons derived from stem cells, in particular hiPS cells. Such neurons are difficult to prepare and either require collaboration with one of the several laboratories around the world that are routinely preparing them, or need to be purchased. While currently very expensive, future research in the stem cell area and competition in the market will likely lead to lowered prizes of such neurons. So far, hiPS cell-derived neurons have been tested as a model for BoNT research and potency detection from only one source (Cellular Dynamics International, WI) (Whitemarsh et al. 2012), but other companies are starting to offer similar products (Globalstem, MD, ReproCELL, CA). In addition, neurons representing neuronal subpopulations other than the currently available forebrain neurons will likely become available in the future and will enable comparative studies of different BoNT sero- and subtypes in different neuronal subpopulations. This is exemplified by companies that are developing neurons containing a large percentage of cholinergic neurons derived from hiPS cells, as well as neuronal stem cells that can be differentiated into mature neurons of different phenotypes within 2 weeks. Eventually, more affordable cell models for research purposes are primary cells or mES cells derived neurons. Table 2 provides a summary of different cell models and their important features.
One important aspect of NCB assays is the endpoint used. The Western blot method is an excellent method for research purposes as it is easy to set up in any laboratory, does not require special equipment, provides visual results, and is applicable to any cell type. In a commercial high-throughput setting, however, this method is laborious, and using Western blots for quantitative purposes in general can introduce error. This problem is reduced by comparing cleaved versus uncleaved SNAP-25 bands for BoNT/A and E, and in fact data indicate that the error of this method is still smaller than that of the MBA (Pellett et al. 2010). Nevertheless, the error rate for other serotypes that are assayed by the disappearance of the VAMP2 band compared to a loading standard such as syntaxin is much greater (Whitemarsh et al. 2012). Other detection methods, such as ELISA of cleaved and unlceaved SNARE proteins in cell lysates, are being developed and are more suitable for commercial applications (Nuss et al. 2010; Zhu et al. 2010). These methods will likely improve accuracy, speed, and costs of NCB assays and are also applicable to any cell type. Neurotransmitter release is cell type specific, and while it is an important endpoint to explore in research especially in mES and hiPS cells derived neurons, is not useful by itself for commercial purposes because it is relatively nonspecific. The stable introduction of a sensor into a cell line that enables an easy and fast read out, such as a fluorescent or FRET sensor (Dong et al. 2004) would be of tremendous value for both research and commercial applications. Creating such a cell line can be easiest achieved in continuous cell lines (see BoCell assay, Biosentinal Inc.,), but is also possible (although much more difficult and expensive) in mES and hiPS cells cell lines that can then be differentiated to neurons. Sensitivity and species specificity of the cells should be considered before construction of such a cell model.
The mouse bioassay has been the ‘gold standard’ for BoNT detection since the beginnings of BoNT research. The recent and ongoing development of NCB assays including systems using normal human neurons opens the possibility to largely replace the mouse bioassay for BoNT potency determination and neutralizing antibody detection, and to study BoNTs in species-specific neuronal cell models. This has the potential to lead to important new insights on the behavior and effect of BoNT sero-and subtypes on specific human neurons, which will aid in the design of novel and improved BoNT-based pharmaceuticals as well as botulism countermeasures.
Abbreviations
- NCB assay:
-
Neuronal cell-based assay
- BoNT:
-
Botulinum neurotoxins
- HC:
-
Heavy chain
- LC:
-
Light chain
- SNAP-25:
-
Synaptosomal-associated protein 25
- VAMP:
-
Vesicle-associated membrane protein
- SNARE:
-
Soluble N-ethylmaleimide-sensitive factor attachment protein receptor
- FRET:
-
Fluorescence resonance energy transfer
- FDA:
-
Food and Drug Administration
- SV2:
-
Synaptic vesicle protein 2
- MBA:
-
Mouse bioassay
- NGF:
-
Nerve growth factor
- EB:
-
Embryoid body
- mES cells:
-
Mouse embryonic stem cells
- hiPS cells:
-
Human induced pluripotent stem cells
- ELISA:
-
Enzyme-linked immunosorbent assay
- EDB:
-
Extensor digitorum brevis
- LD50 :
-
Lethal dose at which 50 % of animals die
- U:
-
Mouse LD50 Unit
- EC50 :
-
Half maximal effective concentration
- GT1b:
-
Trisialoganglioside GT1b
References
Adler S, Bicker G, Bigalke H et al (2010) The current scientific and legal status of alternative methods to the LD50 test for botulinum neurotoxin potency testing. The report and recommendations of a ZEBET expert meeting. Altern Lab Anim 38:315–330
Akaike N, Ito Y, Shin MC, Nonaka K, Torii Y, Harakawa T, Ginnaga A, Kozaki S, Kaji R (2010) Effects of A2 type botulinum toxin on spontaneous miniature and evoked transmitter release from the rat spinal excitatory and inhibitory synapses. Toxicon 56:1315–1326
Arnon SS, Schechter R, Inglesby TV et al (2001) Botulinum toxin as a biological weapon: medical and public health management. JAMA 285:1059–1070
Benatar MG, Willison HJ, Vincent A (1997) Lack of effect of Miller Fisher sera/plasmas on transmitter release from PC12 cells. J Neuroimmunol 80:1–5
Bercsenyi K, Giribaldi F, Schiavo G (2012) The elusive compass of clostridial neurotoxins: deciding when and where to go? doi:10.1007/978-3-642-33570-9_5
Bigalke H, Dimpfel W, Habermann E (1978) Suppression of 3H-acetylcholine release from primary nerve cell cultures by tetanus and botulinum-A toxin. Naunyn Schmiedebergs Arch Pharmacol 303:133–138
Bigalke H, Dreyer F, Bergey G (1985) Botulinum A neurotoxin inhibits non-cholinergic synaptic transmission in mouse spinal cord neurons in culture. Brain Res 360:318–324
Binz T (2012) Clostridial neurotoxin light chains: devices for SNARE cleavage mediated blockade of neurotransmission. doi:10.1007/978-3-642-33570-9_7
Binz T, Blasi J, Yamasaki S et al (1994) Proteolysis of SNAP-25 by types E and A botulinal neurotoxins. J Biol Chem 269:1617–1620
Blasi J, Chapman ER, Link E et al (1993a) Botulinum neurotoxin A selectively cleaves the synaptic protein SNAP-25. Nature 365:160–163
Blasi J, Chapman ER, Yamasaki S et al (1993b) Botulinum neurotoxin C1 blocks neurotransmitter release by means of cleaving HPC-1/syntaxin. EMBO J 12:4821–4828
Borodic G (2007) Botulinum toxin, immunologic considerations with long-term repeated use, with emphasis on cosmetic applications. Facial Plast Surg Clin North Am 15:11–16
Borodic GE, Duane D, Pearce B et al (1995) Antibodies to botulinum toxin. Neurology 45:204
Brewer GJ (1995) Serum-free B27/neurobasal medium supports differentiated growth of neurons from the striatum, substantia nigra, septum, cerebral cortex, cerebellum, and dentate gyrus. J Neurosci Res 42:674–683
Brewer GJ, Torricelli JR, Evege EK et al (1993) Optimized survival of hippocampal neurons in B27-supplemented neurobasal, a new serum-free medium combination. J Neurosci Res 35:567–576
Cartee TV, Monheit GD (2011) An overview of botulinum toxins: past, present, and future. Clin Plast Surg 38:409–426
Conway JO, Sherwood LJ, Collazo MT et al (2010) Llama single domain antibodies specific for the 7 botulinum neurotoxin serotypes as heptaplex immunoreagents. PLoS ONE 5:e8818
Cordivari C, Misra VP, Vincent A et al (2006) Secondary nonresponsiveness to botulinum toxin A in cervical dystonia: the role of electromyogram-guided injections, botulinum toxin A antibody assay, and the extensor digitorum brevis test. Mov Disord 21:1737–1741
Dong M, Liu H, Tepp WH et al (2008) Glycosylated SV2A and SV2B mediate the entry of botulinum neurotoxin E into neurons. Mol Biol Cell 19:5226–5237
Dong M, Richards DA, Goodnough MC et al (2003) Synaptotagmins I and II mediate entry of botulinum neurotoxin B into cells. J Cell Biol 162:1293–1303
Dong M, Tepp WH, Johnson EA et al (2004) Using fluorescent sensors to detect botulinum neurotoxin activity in vitro and in living cells. Proc Natl Acad Sci U S A 101:14701–14706
Dong M, Tepp WH, Liu H et al (2007) Mechanism of botulinum neurotoxin B and G entry into hippocampal neurons. J Cell Biol 179:1511–1522
Dong M, Yeh F, Tepp WH et al (2006) SV2 is the protein receptor for botulinum neurotoxin A. Science 312:592–596
Dorner MB, Schulz KM, Kull S (2012) Complexity of botulinum neurotoxins: challenges for detection technology. doi:10.1007/978-3-642-33570-9_11
Dressler D (2004) Clinical presentation and management of antibody-induced failure of botulinum toxin therapy. Mov Disord 19(Suppl 8):S92–S100
Dressler D, Benecke R (2007) Pharmacology of therapeutic botulinum toxin preparations. Disabil Rehabil 29:1761–1768
Dressler D, Bigalke H (2002) Botulinum toxin antibody type A titres after cessation of botulinum toxin therapy. Mov Disord 17:170–173
Dressler D, Lange M, Bigalke H (2005) Mouse diaphragm assay for detection of antibodies against botulinum toxin type B. Mov Disord 20:1617–1619
Dressler D, Wohlfahrt K, Meyer-Rogge E et al (2010) Antibody-induced failure of botulinum toxin a therapy in cosmetic indications. Dermatol Surg 36(Suppl 4):2182–2187
Duggan MJ, Quinn CP, Chaddock JA et al (2002) Inhibition of release of neurotransmitters from rat dorsal root ganglia by a novel conjugate of a Clostridium botulinum toxin A endopeptidase fragment and Erythrina cristagalli lectin. J Biol Chem 277:34846–34852
Eleopra R, Tugnoli V, Quatrale R et al (2004) Different types of botulinum toxin in humans. Mov Disord 19(Suppl 8):S53–S59
Eleopra R, Tugnoli V, Rossetto O et al (1998) Different time courses of recovery after poisoning with botulinum neurotoxin serotypes A and E in humans. Neurosci Lett 256:135–138
Evidente VG, Adler CH (2010) An update on the neurologic applications of botulinum toxins. Curr Neurol Neurosci Rep 10:338–344
Fischer A (2012) Synchronized chaperone function of botulinum neurotoxin domains mediates light chain translocation into neurons. doi:10.1007/978-3-642-33570-9_6
Fischer A, Montal M (2007a) Crucial role of the disulfide bridge between botulinum neurotoxin light and heavy chains in protease translocation across membranes. J Biol Chem 282:29604–29611
Fischer A, Montal M (2007b) Single molecule detection of intermediates during botulinum neurotoxin translocation across membranes. Proc Natl Acad Sci U S A 104:10447–10452
Fischer A, Nakai Y, Eubanks LM et al (2009) Bimodal modulation of the botulinum neurotoxin protein-conducting channel. Proc Natl Acad Sci U S A 106:1330–1335
Flynn TC (2004) Myobloc. Dermatol Clin 22:207–211 vii
Gimenez DF, Gimenez JA (1995) The typing of botulinal neurotoxins. Int J Food Microbiol 27:1–9
Hatheway CL (1988) Botulism. In: Balows A, Hausler WH, Ohashi M, Turano MA (eds) Laboratory diagnosis of infectious diseases: principles and practice, vol 1. Springer, New York, pp 111–133
Hill KK, Smith TJ (2012) Genetic diversity within Clostridium botulinum serotypes, botulinum neurotoxin gene clusters and toxin subtypes. doi:10.1007/978-3-642-33570-9_1
Hu BY, Zhang SC (2010) Directed differentiation of neural-stem cells and subtype-specific neurons from hESCs. Methods Mol Biol 636:123–137
Johnson EA, Montecucco C (2008) Chapter 11 Botulism. In: Engel Andrew G (ed) Handbook of clinical neurology, vol 91. Elsevier, pp 333–368
Jones RG, Alsop TA, Hull R et al (2006) Botulinum type A toxin neutralisation by specific IgG and its fragments: a comparison of mouse systemic toxicity and local flaccid paralysis assays. Toxicon 48:246–254
Jones RG, Liu Y, Halls C et al (2011) Release of proteolytic activity following reduction in therapeutic human serum albumin containing products: detection with a new neoepitope endopeptidase immunoassay. J Pharm Biomed Anal 54:74–80
Kalb SR, Baudys J, Egan C et al (2011) Different substrate recognition requirements for cleavage of synaptobrevin-2 by Clostridium baratii and Clostridium botulinum type F neurotoxins. Appl Environ Microbiol 77:1301–1308
Keller JE, Cai F, Neale EA (2004) Uptake of botulinum neurotoxin into cultured neurons. Biochemistry 43:526–532
Keller JE, Neale EA (2001) The role of the synaptic protein snap-25 in the potency of botulinum neurotoxin type A. J Biol Chem 276:13476–13482
Keller JE, Neale EA, Oyler G et al (1999) Persistence of botulinum neurotoxin action in cultured spinal cord cells. FEBS Lett 456:137–142
Kessler KR, Benecke R (1997) The EBD test–a clinical test for the detection of antibodies to botulinum toxin type A. Mov Disord 12:95–99
Kiris E, Nuss JE, Burnett JC et al (2011) Embryonic stem cell-derived motoneurons provide a highly sensitive cell culture model for botulinum neurotoxin studies, with implications for high-throughput drug discovery. Stem Cell Res 6:195–205
Kivell BM, McDonald FJ, Miller JH (2001) Method for serum-free culture of late fetal and early postnatal rat brainstem neurons. Brain Res Brain Res Protoc 6:91–99
Kohno K, Kawakami T, Hiruma H (2005) Effects of soluble laminin on organelle transport and neurite growth in cultured mouse dorsal root ganglion neurons: difference between primary neurites and branches. J Cell Physiol 205:253–261
Lacy DB, Tepp W, Cohen AC et al (1998) Crystal structure of botulinum neurotoxin type A and implications for toxicity. Nat Struct Biol 5:898–902
Lee JO, Rosenfield J, Tzipori S et al (2008) M17 human neuroblastoma cell as a cell model for investigation of botulinum neurotoxin A activity and evaluation of BoNT/A specific antibody. The Botulinum J 1:135–152
Liu YY, Rigsby P, Sesardic D et al (2012) A functional dual-coated (FDC) microtitre plate method to replace the botulinum toxin LD (50) test. Anal Biochem 425:28–35
Macdonald TE, Helma CH, Shou Y et al (2011) Analysis of Clostridium botulinum serotype E strains by using multilocus sequence typing, amplified fragment length polymorphism, variable-number tandem-repeat analysis, and botulinum neurotoxin gene sequencing. Appl Environ Microbiol 77:8625–8634
McInnes C, Dolly JO (1990) Ca2(+)-dependent noradrenaline release from permeabilised PC12 cells is blocked by botulinum neurotoxin A or its light chain. FEBS Lett 261:323–326
McMahon HT, Nicholls DG (1991) Transmitter glutamate release from isolated nerve terminals: evidence for biphasic release and triggering by localized Ca2+. J Neurochem 56:86–94
McNutt P, Celver J, Hamilton T et al (2011) Embryonic stem cell-derived neurons are a novel, highly sensitive tissue culture platform for botulinum research. Biochem Biophys Res Commun 405:85–90
Montal M (2010) Botulinum neurotoxin: a marvel of protein design. Annu Rev Biochem 79:591–617
Montecucco C (1986) How do tetanus and botulinum toxins bind to neuronal membranes? Trends Biochem Sci 11:314–317
Muller K, Mix E, Adib Saberi F et al (2009) Prevalence of neutralising antibodies in patients treated with botulinum toxin type A for spasticity. J Neural Transm 116:579–585
Nishiki T, Kamata Y, Nemoto Y et al (1994) Identification of protein receptor for Clostridium botulinum type B neurotoxin in rat brain synaptosomes. J Biol Chem 269:10498–10503
Nuss JE, Ruthel G, Tressler LE et al (2010) Development of cell-based assays to measure botulinum neurotoxin serotype A activity using cleavage-sensitive antibodies. J Biomol Screen 15:42–51
Parnas D, Linial M (1995) Cholinergic properties of neurons differentiated from an embryonal carcinoma cell-line (P19). Int J Dev Neurosci 13:767–781
Peck MW (2009) Biology and genomic analysis of Clostridium botulinum. Adv Microb Physiol 55(183–265):320
Pellett S, Du ZW, Pier CL et al (2011) Sensitive and quantitative detection of botulinum neurotoxin in neurons derived from mouse embryonic stem cells. Biochem Biophys Res Commun 404:388–392
Pellett S, Tepp WH, Clancy CM et al (2007) A neuronal cell-based botulinum neurotoxin assay for highly sensitive and specific detection of neutralizing serum antibodies. FEBS Lett 581:4803–4808
Pellett S, Tepp WH, Toth SI et al (2010) Comparison of the primary rat spinal cord cell (RSC) assay and the mouse bioassay for botulinum neurotoxin type A potency determination. J Pharmacol Toxicol Methods 61:304–310
Peng L, Berntsson RP, Tepp WH et al. (2012) Botulinum neurotoxin D-C uses synaptotagmin I/II as receptors and human synaptotagmin II is not an effective receptor for type B, D-C, and G toxins. J Cell Sci. March 2012 epub ahead of print
Peng L, Tepp WH, Johnson EA et al (2011) Botulinum neurotoxin D uses synaptic vesicle protein SV2 and gangliosides as receptors. PLoS Pathog 7:e1002008
Pickett A, Perrow K (2011) Towards new uses of botulinum toxin as a novel therapeutic tool. Toxins (Basel) 3:63–81
Pier CL, Chen C, Tepp WH et al (2011) Botulinum neurotoxin subtype A2 enters neuronal cells faster than subtype A1. FEBS Lett 585:199–206
Purkiss JR, Friis LM, Doward S et al (2001) Clostridium botulinum neurotoxins act with a wide range of potencies on SH-SY5Y human neuroblastoma cells. Neurotoxicology 22:447–453
Raphael BH, Choudoir MJ, Luquez C et al (2010) Sequence diversity of genes encoding botulinum neurotoxin type F. Appl Environ Microbiol 76:4805–4812
Rasetti-Escargueil C, Jones RG, Liu Y, Sesardic D (2009) Measurement of botulinum types A, B and E neurotoxicity using the phrenic nerve-hemidiaphragm: improved precision with in-bred mice. Toxicon 53:503–511
Rasetti-Escargueil C, Machado CB, Preneta-Blanc R et al (2011a) Enhanced sensitivity to botulinum type A neurotoxin of human neuroblastoma SH-SY5Y cells after differentiation into mature neuronal cells. The Botulinum J 2:30–48
Rasetti-Escargueil C, Liu Y, Rigsby P et al (2011b) Phrenic nerve-hemidiaphragm as a highly sensitive replacement assay for determination of functional botulinum toxin antibodies. Toxicon 57:1008–1016
Ravni A, Bourgault S, Lebon A et al (2006) The neurotrophic effects of PACAP in PC12 cells: control by multiple transduction pathways. J Neurochem 98:321–329
Ray P (1993) Botulinum toxin A inhibits acetylcholine release from cultured neurons in vitro. In Vitro Cell Dev Biol Anim 29A:456–460
Rummel A (2012) Double receptor anchorage of botulinum neurotoxins accounts for their exquisite neurospecificity. doi:10.1007/978-3-642-33570-9_4
Rummel A, Hafner K, Mahrhold S et al (2009) Botulinum neurotoxins C, E and F bind gangliosides via a conserved binding site prior to stimulation-dependent uptake with botulinum neurotoxin F utilising the three isoforms of SV2 as second receptor. J Neurochem 110:1942–1954
Rummel A, Karnath T, Henke T et al (2004) Synaptotagmins I and II act as nerve cell receptors for botulinum neurotoxin G. J Biol Chem 279:30865–30870
Rummel A, Mahrhold S, Bigalke H et al (2011) Exchange of the H (CC) domain mediating double receptor recognition improves the pharmacodynamic properties of botulinum neurotoxin. FEBS J 278:4506–4515
Saadi RA, He K, Hartnett KA et al (2012) SNARE-dependent upregulation of potassium chloride co-transporter 2 activity after metabotropic zinc receptor activation in rat cortical neurons in vitro. Neuroscience 210:38–46
Schantz EJ, Kautter DA (1978) Standardized assay for Clostridium botulinum toxins. J Assoc Official Anal Chem 61:96–99
Schantz EJ, Johnson EA (1992) Properties and use of botulinum toxin and other microbial neurotoxins in medicine. Microbiol Rev 56:80–99
Schiavo G, Benfenati F, Poulain B et al (1992) Tetanus and botulinum-B neurotoxins block neurotransmitter release by proteolytic cleavage of synaptobrevin. Nature 359:832–835
Schiavo G, Malizio C, Trimble WS et al (1994) Botulinum G neurotoxin cleaves VAMP/synaptobrevin at a single Ala–Ala peptide bond. J Biol Chem 269:20213–20216
Schiavo G, Matteoli M, Montecucco C (2000) Neurotoxins affecting neuroexocytosis. Physiol Rev 80:717–766
Schiavo G, Shone CC, Bennett MK et al (1995) Botulinum neurotoxin type C cleaves a single Lys-Ala bond within the carboxyl-terminal region of syntaxins. J Biol Chem 270:10566–10570
Schiavo G, Shone CC, Rossetto O et al (1993) Botulinum neurotoxin serotype F is a zinc endopeptidase specific for VAMP/synaptobrevin. J Biol Chem 268:11516–11519
Sesardic D, Jones RG, Leung T et al (2004) Detection of antibodies against botulinum toxins. Mov Disord 19(Suppl 8):S85–S91
Sesardic D, Das RG (2007) Alternatives to the LD50 assay for botulinum toxin potency testing: strategies and progress towards refinement, reduction and replacement. Special Issue 14:581–585
Sesardic D, Leung T, Gaines Das R (2003) Role for standards in assays of botulinum toxins: international collaborative study of three preparations of botulinum type A toxin. Biologicals 31:265–276
Sheridan RE, Smith TJ, Adler M (2005) Primary cell culture for evaluation of botulinum neurotoxin antagonists. Toxicon 45:377–382
Shone CC, Melling J (1992) Inhibition of calcium-dependent release of noradrenaline from PC12 cells by botulinum type-A neurotoxin. Long-term effects of the neurotoxin on intact cells. Eur J Biochem 207:1009–1016
Smith TJ, Lou J, Geren IN et al (2005) Sequence variation within botulinum neurotoxin serotypes impacts antibody binding and neutralization. Infect Immun 73:5450–5457
Solomon HM, Lilly T (2001) Clostridium botulinum. In: BAM bacteriological analytical manual U.S. Food and Drug Administration, Chapter 17, 8th edn. Revision A
Stahl AM, Ruthel G, Torres-Melendez E et al (2007) Primary cultures of embryonic chicken neurons for sensitive cell-based assay of botulinum neurotoxin: implications for therapeutic discovery. J Biomol Screen 12:370–377
Strotmeier J, Willjes G, Binz T et al (2012) Human synaptotagmin-II is not a high affinity receptor for botulinum neurotoxin B and G: increased therapeutic dosage and immunogenicity. FEBS Lett 586:310–313
Swaminathan S (2011) Molecular structures and functional relationships in clostridial neurotoxins. FEBS J 278:4467–4485
Takahashi K, Tanabe K, Ohnuki M et al (2007) Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131:861–872
Tegenge MA, Bohnel H, Gessler F et al (2012) Neurotransmitter vesicle release from human model neurons (NT2) is sensitive to botulinum toxin A. Cell Mol Neurobiol 32:1021–1029
Truong DD, Stenner A, Reichel G (2009) Current clinical applications of botulinum toxin. Curr Pharm Des 15:3671–3680
Tsukamoto K, Arimitsu H, Ochi S et al. (2012) P19 embryonal carcinoma cells exhibit high sensitivity to botulinum type C and D/C mosaic neurotoxins. Microbiol Immunol July 2012 epub ahead of print
Uemura M, Refaat MM, Shinoyama M et al (2010) Matrigel supports survival and neuronal differentiation of grafted embryonic stem cell-derived neural precursor cells. J Neurosci Res 88:542–551
Ullrich B, Li C, Zhang JZ, McMahon H et al (1994) Functional properties of multiple synaptotagmins in brain. Neuron 13:1281–1291
Verderio C, Grumelli C, Raiteri L et al (2007) Traffic of botulinum toxins A and E in excitatory and inhibitory neurons. Traffic 8:142–153
Welch MJ, Purkiss JR, Foster KA (2000) Sensitivity of embryonic rat dorsal root ganglia neurons to Clostridium botulinum neurotoxins. Toxicon 38:245–258
Whitemarsh RC, Strathman MJ, Chase LG et al (2012) Novel application of human neurons derived from induced pluripotent stem cells for highly sensitive botulinum neurotoxin detection. Toxicol Sci 126:426–435
Wichterle H, Peljto M (2008) Differentiation of mouse embryonic stem cells to spinal motor neurons. Curr Protoc Stem Cell Biol Chapter 1: Unit 1H.1.1–1H.1.9
Wilder-Kofie TD, Luquez C, Adler M et al (2011) An alternative in vivo method to refine the mouse bioassay for botulinum toxin detection. Comp Med 61:235–242
Williamson LC, Halpern JL, Montecucco C et al (1996) Clostridial neurotoxins and substrate proteolysis in intact neurons: botulinum neurotoxin C acts on synaptosomal-associated protein of 25 kDa. J Biol Chem 271:7694–7699
Xie C, Markesbery WR, Lovell MA (2000) Survival of hippocampal and cortical neurons in a mixture of MEM+ and B27-supplemented neurobasal medium. Free Radic Biol Med 28:665–672
Yaguchi T, Nishizaki T (2010) Extracellular high K+ stimulates vesicular glutamate release from astrocytes by activating voltage-dependent calcium channels. J Cell Physiol 225:512–518
Yamasaki S, Baumeister A, Binz T et al (1994) Cleavage of members of the synaptobrevin/VAMP family by types D and F botulinal neurotoxins and tetanus toxin. J Biol Chem 269:12764–12772
Yowler BC, Kensinger RD, Schengrund CL (2002) Botulinum neurotoxin A activity is dependent upon the presence of specific gangliosides in neuroblastoma cells expressing synaptotagmin I. J Biol Chem 277:32815–32819
Yu J, Vodyanik MA, Smuga-Otto K et al (2007) Induced pluripotent stem cell lines derived from human somatic cells. Science 318:1917–1920
Zhang SC (2006) Neural subtype specification from embryonic stem cells. Brain Pathol 16:132–142
Zhu H, Wang J, Jacky BPS et al (2010) Cells useful for immuno-based botulinum toxin serotype A activity assays. US-Patent 12/722801 (Allergan Inc) CA, USA
Acknowledgments
I thank Dr. Eric A Johnson and Regina Whitemarsh for critical review of the manuscript. This work was supported by the National Institutes of Health (contract numbers 1R01AI095274-01A1 and 1R21AI082826-01A2).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Pellett, S. (2012). Progress in Cell Based Assays for Botulinum Neurotoxin Detection. In: Rummel, A., Binz, T. (eds) Botulinum Neurotoxins. Current Topics in Microbiology and Immunology, vol 364. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-33570-9_12
Download citation
DOI: https://doi.org/10.1007/978-3-642-33570-9_12
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-33569-3
Online ISBN: 978-3-642-33570-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)