Abstract
Tetraspanins are small integral membrane proteins that are known to control a variety of cellular processes, including signaling, migration and cell–cell fusion. Research over the past few years established that they are also regulators of various steps in the HIV-1 replication cycle, but the mechanisms through which these proteins either enhance or repress virus spread remain largely unknown.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Feline Immunodeficiency Virus
- Immunological Synapse
- Myotube Formation
- Virological Synapse
- Tetraspanin Family
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Virus proteomics, i.e., the mapping of interactions that take place between cellular and viral proteins on a global, whole cell scale, or based on analyses of cellular components incorporated into virions, has led to the identification of cellular proteins, and indeed entire cellular pathways, that are critical for the propagation of HIV-1 and other retroviruses (for recent overviews, e.g., Goff 2007, 2008). The most straightforward approach leading to the identification of such proteins/pathways is the analysis of virion content. Fifteen years ago such an analysis hinted at the possibility that tetraspanins play a role in the replication of this virus by revealing that a member of the tetraspanin family is specifically incorporated into HIV-1 particles (Orentas and Hildreth 1993). Over the past 5 years, various investigators have followed up on this early study, primarily by further characterizing the presence of tetraspanins at the viral budding site. However, of the two dozen reports that now link tetraspanins with HIV-1 replication steps (see Table 1), so far only a few document functional roles in virus propagation. Therefore, and as I will discuss in this review, while we now know that tetraspanins have regulatory roles during HIV-1 replication, we are only at the very beginning of understanding exactly how these proteins function during transmission, and thus ultimately propagation and pathogenesis, of HIV-1.
In the following, I will first briefly summarize what we know about cellular tetraspanin functions. Subsequently, I will review the existing literature on the interaction between tetraspanins and HIV-1. Finally, I will discuss potential mechanisms through which tetraspanins exert their functions and, though only very briefly, I will also touch upon the role of tetraspanins in the replication cycles of other viruses.
2 Tetraspanins: Organizers of Membrane-Based Processes
Tetraspanins form a diverse family of small (20–30 kDa, not including mass contributed by glycosylation) membrane proteins that compromises 33 members in mammals (Hemler 2005). Consistent with their involvement in controlling membrane-based processes such as signaling, adhesion and cell–cell fusion, tetraspanins have emerged at the transition from unicellular to multicellular organisms and have since undergone intense evolution (Huang et al. 2005).
2.1 Structure and Subcellular Distribution of Tetraspanins
Tetraspanins contain short cytoplasmic N- and C-termini and one short inner loop that separates a small (SEL) from a large (LEL) extracellular loop. A recent cryoelectron microscopic analysis together with molecular modeling studies revealed that tetraspanins, due to close juxtapositioning of the four transmembrane segments, span the lipid bilayer as compact, rod-shaped structures. Plasma membrane-based tetraspanins are relatively “invisible” from the outside, as they protrude only approximately 5 nms. This probably explains why only very few of them do serve as receptors. However, as described elegantly by others, “with the lower half of the bundle embedded in the lipid bilayer, the tetraspanins may serve as pilings in the lipid sea, ideal for docking other transmembrane proteins” (Min et al. 2006). Indeed, the consensus reached by researchers analyzing these proteins is that tetraspanins function primarily as scaffold proteins that laterally organize various membrane-based cellular functions (e.g., Stipp et al. 2003; Hemler 2005; Levy and Shoham 2005a, b). Biochemical analyses over the past 15 years have demonstrated that they form homodimers and that they also tightly associate with other transmembrane proteins, including specific integrins and members of the immunoglobulin superfamily. These associations link molecular events taking place within membranes with membrane-peripheral signaling complexes and the cytoskeleton. Recent high resolution ultrastructural (electron microscopy) and/or fluorescence microscopy studies performed in our lab as well as by others (Nydegger et al. 2006; Unternaehrer et al. 2007), for the first time visualized these up to few hundred nanometer-wide, tetraspanin-mediated assemblages of proteins (TEMs: tetraspanin-enriched microdomains). Importantly, while these initial studies were performed in fixed cells, using bivalent antibody-based detection (which can exaggerate the discreteness of microdomains due to antibody-induced microclustering), two very recent analyses of tetraspanin distribution at the single molecule level in live cells clearly confirmed that these proteins are locally concentrated, thus forming submicron-sized “interaction platforms” (Barreiro et al. 2008; Espenel et al. 2008). One of these latter studies (Espenel et al. 2008) also confirmed what was previously reported by others (e.g., Yang et al. 2004), i.e., that TEMs are clearly distinct from lipid rafts (now also called membrane rafts).
2.2 Cellular Functions of Tetraspanins
Based on analyses of amino acid sequences of the LEL, the segment known to be the primary binding site for tetraspanin-associated proteins, the 33 members of this family can be subdivided into four subgroups (Seigneuret et al. 2001). Members of the same subgroup apparently can partially fulfill each other’s role, in case a specific tetraspanin is ablated (e.g., in mouse knockout systems), suggesting a certain degree of redundancy. While such redundancy provides obvious benefits to organisms, it complicates genetic analyses of functions for individual members of a protein family, and thus not surprisingly, only in a few cases has the deletion of a tetraspanin gene resulted in dramatic phenotypes, such as the loss of fertility in CD9 knock-out mice, or retinal degeneration in peripherin (tetraspanin 22) knockout mice (reviewed, e.g., in Hemler 2005; see also Fradkin et al. 2002). Nevertheless, genetic studies clearly revealed that tetraspanins play regulatory roles in numerous membrane-based processes and several recent reviews provide an overview of the various functions (Boucheix et al. 2001; Wright et al. 2004; Levy and Shoham 2005a, b; Hemler 2008). Here, I will merely summarize what we know so far about the involvement of two members of subgroup 1 (Seigneuret et al. 2001) of the tetraspanin family, CD9 and CD81, in the regulation of membrane fusion, because, as will be discussed later, these two members of the tetraspanin family, and also CD63 (subgroup 2b), are co-regulators of HIV-1-induced virus–cell or cell–cell fusion.
Importantly, like other scaffold proteins, tetraspanins can both enhance or repress the activities of other cellular proteins. For example, the expression of specific cell surface tetraspanins has been shown to either enhance or slow down cell migration, depending on the conditions. Similarly, signaling cascades can either be augmented or dampened by these proteins, and, as will be described in the following, the same tetraspanins can also act as either positive or negative regulators of cellular fusion processes. CD9 and CD81 were documented to promote myotube formation through their enhancement of muscle cell fusion (Tachibana and Hemler 1999). As was already apparent at that time, these two members of the tetraspanin family do not achieve this through binding to partner proteins on adjacent cells and they do not themselves function as fusion proteins. Rather, they regulate myotube formation through the organization in cis of associated, so far still unidentified, cellular fusogens. Interestingly, 4 years after having been recognized to be fusion promoters, the same two tetraspanins (CD9 and CD81) were found to negatively regulate the fusion of another type of somatic cell: Mekada and colleagues showed that the formation of multinuclear phagocytes which ingest infectious microbes, cell fragments etc, is enhanced in CD9- and CD81-null mice (Takeda et al. 2003). This was surprising because, by then, these tetraspanins had also been implicated, besides enhancing myotube formation, in promoting the fusion of germ line cells: CD9 knockout mice oocytes are unable to fuse with sperm (Le Naour et al. 2000; Miyado et al. 2000), and overexpression of CD81 in CD9 knockout mice can partially compensate for CD9’s fusion promoting function (Kaji et al. 2002). Importantly, comparable to the situation in muscle cells, the expression of CD9 in oocytes is required not because tetraspanin acts as cellular fusogen, but because this protein laterally organizes (a) cellular fusion protein(s) (Ziyyat et al. 2006) that interacts in trans with sperm-based proteins, such as Izumo (Inoue et al. 2005), possibly through interactions mediated by its LEL (e.g., Zhu et al. 2002; Higginbottom et al. 2003). Finally, and most intriguingly (at least for virologists), a very recent report demonstrates that CD9 fulfills its fusion control function not through its presence at the oocyte surface but rather upon incorporation into (exosome-like) vesicles that are shed from the oocytes (Miyado et al. 2008).
3 Tetraspanins are Regulators of HIV-1 Replication
3.1 Tetraspanins are present at viral exit sites
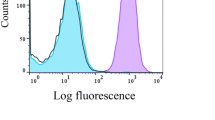
The analysis of virus lipid content (Aloia et al. 1993) guided subsequent studies revealing that HIV-1 buds through membrane domains enriched in distinct lipids (reviewed, e.g., in Ono and Freed 2005; see also Brugger et al. 2006). Similarly, three early analyses of cellular proteins incorporated into HIV-1 which revealed the incorporation of a tetraspanin, CD63, into viral particles (Meerloo et al. 1992, 1993; Orentas and Hildreth 1993), foreshadowed what is now well established: HIV-1 exits at segments of cellular membrane that are enriched in tetraspanins. Importantly, one of these early studies, using a solid phase virus capture assay to identify cellular proteins incorporated into HIV-1 particles, combined with flow cytometric analysis of the host cell membrane, already documented that CD63 incorporation into virions is a non-random process. As also shown for the major histocompatibility antigen HLA-DR, this tetraspanin is specifically incorporated into HIV-1 particles released from T lymphocytes. However, except for another study of host cell protein incorporation into HIV-1 virions, which confirmed that CD63 is enriched in infectious particles (Gluschankof et al. 1997), to the best of my knowledge, nobody followed up on these early findings until about 5 years ago.
Tetraspanins were “re-identified” as potential players in HIV-1 replication when different investigators started scrutinizing (primarily using fluorescence and electron microscopy) where exactly HIV-1 buds from cells and how this virus recruits the cellular ESCRT machinery that mediates its release from cells (for reviews, e.g., Freed 2004; Morita and Sundquist 2004; Bieniasz 2006). Initially, it was shown that HIV-1 (and also SIV) components, particularly the viral envelope glycoprotein, Env, at least under certain physiological conditions and in certain cell types, can traffic through sections of the cellular endocytic system (Hunter and Swanstrom 1990; Rowell et al. 1995; Sauter et al. 1996; Ohno et al. 1997; Boge et al. 1998; reviewed in Marsh and Pelchen-Matthews 2000), where the tetraspanin CD63 was known to primarily reside. Further support for the idea that HIV-1 exit sites may share certain characteristics, may perhaps even be somehow related to endosomal membranes, came from the finding that TSG101, a component of the ESCRT I complex which is required for the formation of intralumenal vesicles of late endosomes/multivesicular bodies (LEs/MVBs), is critical for HIV–1 release. Further, an electron microscopy study by Raposo and colleagues suggested that in macrophages HIV-1 buds into LEs/MVBs (Raposo et al. 2002). Promptly, two studies published in 2003 documented that this virus acquires CD63 (and also CD81 and CD82 if produced in macrophages), when it buds through either what appeared at that time to be LE/MVB membranes of macrophages (Pelchen-Matthews et al. 2003) or when it buds through the plasma membrane in HeLa cells (Nydegger et al. 2003). The latter finding was puzzling because in HeLa cells CD63 has extremely low abundance at the plasma membrane. Nevertheless, based on those data, we hypothesized that this tetraspanin, perhaps together with other members of this family, accumulates at relatively discrete plasma membrane microdomains, and in a subsequent study we indeed provided a first visualization of TEMs, as mentioned above (Nydegger et al. 2006). This analysis, together with biochemical, fluorescence microscopy and again electron microscopy analyses by several other groups, unequivocally confirmed and extended the earlier studies by showing that HIV-1 exits through membrane microdomains enriched in the tetraspanins CD9, CD63, CD81 and CD82 in epithelial cells, T lymphocytes, macrophages and dendritic cells (Booth et al. 2006; Grigorov et al. 2006; Nydegger et al. 2006; Deneka et al. 2007; Jolly and Sattentau 2007; Welsch et al. 2007; Garcia et al. 2008; Turville et al. 2008). Last, but certainly not least, a virion proteomics study of cellular proteins incorporated into HIV-1 released from macrophages not only again revealed the presence of these four tetraspanins, it also reported the incorporation of two additional members of the family (CD53 and tetraspanin 14) (Chertova et al. 2006). How TEMs form and exactly when and how HIV-1 components start interacting with tetraspanins remains to be elucidated. We originally speculated that CD63-containing TEMs at the plasma membrane derive from TEMs that originate in LEs/MVBs and that the viral components perhaps even associate with these domains while they are still part of these organelles (Nydegger et al. 2003). Such a scenario would appear plausible, as it has been documented that the limiting membrane of LE/MVB, upon movement of these organelles to the cell surface, can be inserted as patches into the plasma membrane (Jaiswal et al. 2004). This idea received support from the findings that Rab9 and AP3, cellular proteins implicated in trafficking to and from LEs/MVBs, are necessary for efficient HIV-1 release (Dong et al. 2005; Murray et al. 2005). However, the fact that a very considerable fraction of CD63 traffics to the cell surface before reaching its final destination (LEs/MVBs) (Janvier and Bonifacino 2005), together with other evidence, also makes it likely that the HIV-1 components start associating with tetraspanins only at the plasma membrane, and not while these membrane proteins are carried along vesicles. Indeed, data presented in a recent high resolution (TIRF) microscopy analysis (Jouvenet et al. 2008) also support this idea. The investigators of that study reported that, surprisingly, they did not detect any CD63 association with budding virions at the plasma membrane, while they observed large amounts of this tetraspanin in intracellular vesicles (sometimes containing Gag) moving near the sites of viral morphogenesis and release, but never fusing with the plasma membrane. However, as previously documented (Nydegger et al. 2006), surface CD63 cannot be detected in settings when total cellular CD63 is visualized (either by GFP-tagging or by overall staining). Thus, the failure by Jouvenet et al. to detect CD63 in viral budding structures (Jouvenet et al. 2008) can presumably be explained technically: the strong fluorescence signal for CD63 that emanated from membrane-proximal vesicles densely packed with this tetraspanin probably prevented the detection of much fainter signals that emanate from the relatively low amounts of CD63 associated with HIV-1 budding structures.
Given their presence at HIV-1 exit sites, are tetraspanins gatekeepers, do they facilitate or even promote particle release? Two recently published studies (Sato et al. 2007; Ruiz-Mateos et al. 2008) in which one tetraspanin (CD63) was either ablated or overexpressed, negatively answers this question for HIV-1 release from macrophages and 293 T cells, and our own investigations of release from HeLa cells and T lymphocytes lead to the same conclusion (Krementsov et al., Retrovirology, in press), though one recent study reports that decreased CD63 expression in macrophages results in reduced HIV-1 particle output (Chen et al. 2008), and an even more recent study correlates reduced levels of CD81 with decreased virus release from Molt T cells (Grigorov et al. 2009). Again arguing against the idea that tetraspanins act as general release factors, recent data from our laboratory demonstrate that CD9 expression can be abrogated without consequences for the rate with which HIV-1 is released from these cells (Krementsov et al., Retrovirology, in press). Initially, this came as a surprise to us, because an incubation of cells producing another lentivirus (feline immunodeficiency virus, FIV, see below) with an anti-feline CD9 antibody (de Parseval et al. 1997), as well as the incubation of HIV-1-producing HeLa cells with an anti-human CD9 antibody (K41) can significantly reduce the rate with which HIV-1 is released from these cells (Khurana et al. 2007). However, as we documented in that latter study, the treatment with K41 resulted in the aggregation of CD9 and other members of the tetraspanin family at cell–cell junctions, thus possibly simply sterically blocking virus release. Altogether, currently available evidence suggests that tetraspanins do not generally act as budding co-factors for HIV-1, though further studies will need to address the question if some of them play a supportive role in certain cell types.
3.2 Tetraspanins in HIV-1 Virions Inhibit Env-Induced Membrane Fusion
If tetraspanins do not act as budding co-factors, why did HIV-1 evolve to exit at membrane segments enriched in these proteins? Given what we now know about the crucial role that CD9 plays in the sperm–egg fusion process, it would have appeared reasonable to hypothesize that tetraspanins, upon incorporation into viral particles, enhance their fusogenicity, e.g., by laterally organizing viral Env. Indeed, to virologists the recent finding that CD9-bearing exosomes mediate fusion of adjacent cells (sperm and egg, see above) is reminiscent of the phenomenon called “fusion from without” (Bratt and Gallaher 1969); documented for HIV-1 in (Clavel and Charneau 1994): virions that are added to cells in large numbers will act as fusion-bridges, thus promoting the formation of syncytia. However, data recently published by the Koyanagi laboratory (Sato et al. 2007) together with our unpublished observations demonstrate that tetraspanins, if acquired by HIV-1 particles, reduce the fusogenicity of the virions. Indeed, the incorporation of tetraspanins CD9, CD63, CD81, CD82, and CD231 considerably diminishes the infectivity of HIV-1 particles, and these tetraspanins thus act as negative regulators of Env-induced membrane fusion, comparable to how CD9 and CD81 negatively regulate the fusion of monocyte-macrophages. Based on these data, it has been speculated (Sato et al. 2007) that such a fusion-suppressing activity of, e.g., CD63 explains why this tetraspanin is specifically downregulated upon reactivation of chronically infected T lymphocytes, once they increase their virus output (Sato et al. 2007). However, the finding that tetraspanins, despite an overall downregulation from the surface of infected cells (Krementsov et al. Retrovirology, in press), still accumulate at virus release sites (e.g., Jolly and Sattentau 2007) and are still incorporated into virions, as described above, suggests that tetraspanins do not merely act as restriction factors for HIV-1. Rather, combined with the observation that some anti-tetraspanin antibodies appear to negatively affect the alignment of HIV-1 producer and target cells (Jolly and Sattentau 2007), this suggests that they can act as both promoters and inhibitors of HIV-1 transmission. Indeed, as I will lay out below, the role played by tetraspanins expressed at the surface of uninfected or of newly infected cells further supports the idea that these proteins have pleiotropic effects on HIV-1 replication and that these effects can be positive or negative.
3.3 Tetraspanins Regulate HIV-1 Entry and the Transcription of the Viral Genome in Newly Infected Cells
While most of the papers on HIV-1 replication and tetraspanins suggest or describe roles of these proteins during the assembly/release phase of the viral replication cycle, recent reports clearly document that tetraspanins also affect virus replication at the entry phase and upon integration of the viral genome into host chromosomes. Data presented in two studies showed that the treatment of macrophages with either an anti-CD63 antibody (von Lindern et al. 2003) or with recombinant LELs of the tetraspanins CD9, CD63, CD81, and CD151 (Ho et al. 2006) can inhibit HIV-1 entry, probably by blocking a post-binding step. While this suggests positive roles for these tetraspanins in the infection process, CD63, but none of the other tetraspanins analyzed (CD9, CD81, and CD151) was also recently shown to divert the co-receptor CXCR4 from its trafficking to the cell surface, thus reducing its presence there and consequently reducing the susceptibility of cells to HIV-1 (Yoshida et al. 2008). This later report, which suggested that tetraspanins, specifically CD63, negatively regulate HIV-1 replication, is counterbalanced by another report, which documented a potential role for CD81 as a co-stimulatory molecule that enhances the transcription of the newly integrated HIV-1 genome (Tardif and Tremblay 2005). Finally, the authors of a fourth paper remain ambiguous about whether the observed result of CD9 and CD81 downregulation from the surface of potential target cells overall has positive or negative consequences for HIV-1 replication: Sanchez-Madrid and colleagues (Gordon-Alonso et al. 2006) demonstrated that either siRNA-mediated reduction of tetraspanin levels, or antibody-induced interference with normal tetraspanin function in T cells and in CD4-positive target cells, leads to increased fusion of infected and uninfected cells. As will be discussed below, such increased fusion could restrict virus spread, and the presence of tetraspanins at the surface of potential target cells could thus be beneficial for the virus. However, it is also possible that tetraspanins prevent HIV-1 infection because, as was also shown in that paper (Gordon-Alonso et al. 2006), the elimination of tetraspanins from the surface of potential target cells makes these cells more susceptible for HIV-1 infection.
3.4 Tetraspanins Regulate Cell-to-Cell Transmission of HIV-1
As reviewed elsewhere (e.g., Johnson and Huber 2002; Sattentau 2008), and indeed as already proposed 15 years ago (Phillips 1994), HIV-1 apparently is most efficiently transmitted from cell-to-cell, if it is released at cell-cell junctions, into the cleft of what is now called the virological synapse (VS) (Igakura et al. 2003; Jolly et al. 2004; for a review see Piguet and Sattentau 2004; see also Hope 2007). Transmission via the VS may be particularly important in secondary lymphoid organs, which are the major sites of virus replication and where cells can be densely packed, (e.g., in the order of 109 cells/ml in lymph nodes, as compared to 105–106 cells in blood) (see also Sourisseau et al. 2007, for further citations). Evidence that such synaptic transmission takes place in vivo comes from data that document clusters of patient-derived spleen cells that have been infected by HIV-1 derived from the same progeny virus (Cheynier et al. 1994; Hosmalin et al. 2001).
The VS shares certain characteristics with the so-called immunological synapse (IS), which forms between antigen presenting cells and T cells (e.g., Friedl et al. 2005; see also Fackler et al. 2007). Like the IS, the VS represents a transient but nevertheless well-organized functional entity. Comparable to the IS, (and also to the neural synapse), the producer/effector cell, i.e., the presynaptic cell, does not fuse with the target cell (the postsynaptic cell) upon synapse formation. While this lack of fusion may seem normal in the case of the IS and the neural synapse, it certainly comes as a surprise in the case of the VS: why do producer cells, which express Env at their surface, typically not fuse with target cells which express CD4 and chemokine receptors? Why do they not form a syncytium, a multinucleated cell? Adherence without fusion may be explained at least partially by the fact that unprocessed HIV-1 Gag represses Env fusion activity through an interaction with the cytoplasmic tail of Env (EnvCT) (Murakami et al. 2004; Wyma et al. 2004; Davis et al. 2006; Jiang and Aiken 2006, 2007; for a recent review, see Murakami 2008). Hence, if expressed as part of the virus, most Env becomes fusogenic only when it leaves the producer cell as part of the budding virion, but it can already bind to CD4 before that. One could thus envision a scenario in which a fraction of Env located at the presynapse and still associated with precursor Gag, and thus not fusogenic, triggers adherence of the producer to the target cell, thus allowing for the formation of the synaptic cleft into which virions (with fusion-active Env) can be shed. However, Env-mediated cell–cell fusion is also known to be regulated by cellular proteins, e.g., integrins, present at the surface of producer and target cells (e.g., Ohta et al. 1994; Fais et al. 1996) and it thus seems most likely that viral and cellular proteins, including tetraspanins, act in concert to promote efficient particle transfer by regulating Env-induced membrane fusion. As already mentioned above, CD9 and CD81 prevent syncytium formation through their presence at the virological postsynapse, but they also act at the other side of the VS: our own data demonstrate that the same tetraspanins (CD9 and CD81, and also CD63) prevent HIV-1 Env-induced cell–cell fusion through their presence at the virological presynapse (Weng et al. 2009). Quite likely, such repression of Env-induced fusion by tetraspanins, unlike their fusion inhibitory function in virions (see above), is beneficial for the virus but not for the host, because syncytia, while being able to still produce HIV-1 particles (indeed lots of them; see, e.g., Sylwester et al. 1997), have limited life span and thus cannot continue spreading the virus.
If fusion prevention by tetraspanins is positive for the virus, how can this be reconciled with the finding that tetraspanin incorporation into budding HIV-1 particles reduces their infectivity and is thus detrimental to virus replication and spread? It seems reasonable to assume that fusion regulation at the VS, as well as other transmission related processes that take place at that site, depends on proper spatio-temporal organization of the synapse. Spatial organization of the synapse is now well documented for the IS (e.g., Kaizuka et al. 2007) which, at least in its more stable form (Friedl et al. 2005), has a central zone known as the cSMAC (central supramolecular activation complex) that contains the T cell receptor (TCR), co-stimulatory molecules and signaling components, and an outer ring of proteins known as the pSMAC (peripheral SMAC), comprised of adhesion molecules such as the ICAM-1-LFA-1 pair. Interestingly, a similar localization of ICAM-1 was reported for a VS-like structure that formed when CD4-positive T cells adhered to coverslips coated with gp120 and ICAM-1, with ICAM-1 forming a ring around gp120 that accumulated in the center (Vasiliver-Shamis et al. 2008). A scenario that would reconcile the opposing effects of fusion repression by tetraspanins (negative for the virus because it reduces its infectivity – positive because it prevents syncytium formation) would see tetraspanins, like the adhesion molecules, accumulating preferentially at the VS periphery, where their presence would prevent Env molecules from initiating the fusion of pre- and postsynaptic cells, while the center of the VS, where HIV-1 may bud preferentially, would be relatively deserted by these proteins, thus allowing for the formation of particles with (relatively) few tetraspanins (see Fig. 1 for a scheme of the VS). Examinations of the spatial organization of the VS will allow testing this hypothetical distribution. An alternative, simpler explanation would envision that the virus downregulates tetraspanins to an optimal level that enhances the infectivity of the virions but which still prevents syncytia formation.
Tetraspanin functions before, during and after transmission of HIV-1 particles. (A) Formation of viral exit gateways. (B) Incorporation into virions and reduction of infectivity. (C) Repression of Env-mediated virus-cell and cell-cell fusion through interactions with the receptor/coreceptor complex. (D) Reduction of susceptibility to HIV-1 infection through interference with CXCR4 transport to the cell surface. (E) Costimulation of HIV-1 gene expression. (F) Prevention of syncytia formation through interactions with Env in producer cells (see text for details)
3.5 How do Tetraspanins Regulate HIV-1 Entry, Viral Protein Expression, and Env/Receptor-Mediated Fusion Processes?
3.5.1 Tetraspanin Functions in Potential Target Cells and in Newly Infected Cells
While CD63 has been shown to divert CXCR4 from reaching the cell surface, thus preventing infection of cells by HIV-1, it remains to be analyzed if CD63 fulfills this chaperoning function through direct interaction with CXCR4, and if so, where it starts to interact with the coreceptor for HIV-1. Even less is known about the mechanisms with which tetraspanins at the surface of target cells repress fusion of the target cell membrane with the membrane of bound virions and/or bound producer cells. While CD81 is known to associate with CD4 (Imai et al. 1995), downregulation of this HIV-1 receptor apparently is not responsible for the observed fusion repressor function of CD9 and CD81 (Gordon-Alonso et al. 2006). Comparably, receptor/co-receptors in potential target cells are not downregulated upon incubation of these cells with LEL, which inhibits virus entry into macrophages. It seems plausible, however, that tetraspanin knockdowns in T lymphocytes or incubation of these cells with anti-tetraspanin antibodies, as well as LEL treatment of macrophages, either prevent conformational changes that need to take place for fusion to ensue, or that they alter the microenvironment of the receptors/coreceptors. Such lateral reorganizations may also be at play when CD81 acts as co-stimulator of HIV-1 gene transcription. Since CD81 is known to associate with CD4, one could speculate that an engagement of CD4 by its counter receptor (Env, either on virions or on producer cells) triggers local protein translocations or conformational changes in target cell signaling complexes.
3.5.2 Repression of Fusion Triggered by Virion-Associated or Producer Cell-Associated Env
As described above, we know very little about how tetraspanins regulate infection and post-infection events in lymphocytes. We are even more ignorant about tetraspanin functions in HIV-1 producer cells and in virions. And while these cellular membrane proteins have been established as important players in the replication cycle of other viruses, e.g., in hepatitis C virus (HCV) entry, apparently we cannot extrapolate to HIV-1 from that knowledge. CD81 serves as coreceptor for HCV (e.g., Kapadia et al. 2007; Brazzoli et al. 2008), but the interaction of HCV’s envelope glycoprotein E2 with CD81 so far is one of only two cases where a tetraspanin directly interacts with a protein situated in trans, i.e., on the plasma membrane of an adjacent cell (or on the viral membrane). Even the role that the tetraspanin CD82 plays in the replication cycle of another retrovirus (HTLV-1) may be distinct from how tetraspanins regulate HIV-1-induced fusion processes (both virus- or cell-associated fusion processes): while a (probably direct) interaction between HTLV-1 Gag and CD82 was reported to take place (Mazurov et al. 2007), HTLV-1 Env-induced fusion repression by this tetraspanin, unlike what we see in the case of HIV-1 (Weng et al. 2009), does not require coexpression of Gag (Pique et al. 2000). At this point in time, while we do not know the mechanism of fusion regulation by tetraspanins in producer cells, it would appear plausible that these proteins do so by laterally interacting with HIV-1 Env, similar to how they are thought to organize the viral receptors in the target cell.
4 Conclusions – Perspectives
As should be obvious from my remarks above, we are only at the very beginning of understanding the mechanisms that allow tetraspanins to act at various HIV-1 replication steps. Further genetic, biochemical and cell biological analyses are clearly warranted at this point in time. Analyses of how tetraspanins regulate HIV-1 Env-triggered membrane fusion processes at the VS may also benefit from emerging knowledge about the biochemistry and the physics of cellular fusion processes. Clearly, two flat membranes opposed to each other will not spontaneously fuse. A curved membrane however, as it exists in vesicles or at the tip of a microvillus, can get into closer contact with an opposed flat membrane (because there will be less repulsive force between the two membranes) and this will lower the energy barrier that needs to be overcome in order for membrane fusion to take place. Interestingly, expression of the tetraspanin CD9 has recently been documented to be a key requirement for the formation of proper microvilli (Runge et al. 2007). Considering also the previously mentioned finding that extracellular vesicles enriched in CD9 can trigger sperm-oocyte fusion process (Miyado et al. 2008), one is then tempted to speculate that tetraspanins act as organizers of fusion platforms not only by allowing (or not allowing) access of cellular and viral fusogens to these membrane microsegments (e.g., Singethan et al. 2008), but also by recruiting cellular proteins and lipids that promote curvature of the lipid bilayer.
In conclusion, because of their regulatory functions in fusion platforms that are situated at both sides of the VS, as well as within virions, it will not be easy to dissect exactly how tetraspanins regulate the HIV-1 transmission process. It should also be pointed out that while virus transmission in lymph nodes takes place primarily within a static setting of cells, we know very little about cell-to-cell transmission process in other organs, e.g., in the gut-associate lymphoid system. Quite likely, motile HIV-1-infected cells serve as source for the distribution of the virus at some of those other sites. It will thus eventually become imperative to study tetraspanin functions under conditions that reflect these physiological circumstances, all the more so given that tetraspanins such as CD63 (Mantegazza et al. 2004) or CD9 and CD81 (Takeda et al. 2008) also regulate cell motility, which in turn will probably influence HIV-1 transmission to target cells and thus overall virus dissemination in situ.
References
Aloia RC, Tian H et al (1993) Lipid composition and fluidity of the human immunodeficiency virus envelope and host cell plasma membranes. Proc Natl Acad Sci USA 90(11):5181–5185
Barreiro O, Zamai M et al (2008) Endothelial adhesion receptors are recruited to adherent leukocytes by inclusion in preformed tetraspanin nanoplatforms. J Cell Biol 183(3):527–542
Bieniasz PD (2006) Late budding domains and host proteins in enveloped virus release. Virology 344(1):55–63
Boge M, Wyss S et al (1998) A membrane-proximal tyrosine-based signal mediates internalization of the HIV-1 envelope glycoprotein via interaction with the AP-2 clathrin adaptor. J Biol Chem 273(25):15773–15778
Booth AM, Fang Y et al (2006) Exosomes and HIV Gag bud from endosome-like domains of the T cell plasma membrane. J Cell Biol 172(6):923–935
Boucheix C, Duc GH et al (2001) Tetraspanins and malignancy. Expert Rev Mol Med 2001:1–17
Bratt MA, Gallaher WR (1969) Preliminary analysis of the requirements for fusion from within and fusion from without by Newcastle disease virus. Proc Natl Acad Sci USA 64(2):536–543
Brazzoli M, Bianchi A et al (2008) CD81 is a central regulator of cellular events required for hepatitis C virus infection of human hepatocytes. J Virol 82(17):8316–8329
Brugger B, Glass B et al (2006) The HIV lipidome: a raft with an unusual composition. Proc Natl Acad Sci USA 103(8):2641–2646
Chen H, Dziuba N et al (2008) A critical role for CD63 in HIV replication and infection of macrophages and cell lines. Virology 379(2):191–196
Chertova E, Chertov O et al (2006) Proteomic and biochemical analysis of purified human immunodeficiency virus type 1 produced from infected monocyte-derived macrophages. J Virol 80(18):9039–9052
Cheynier R, Henrichwark S et al (1994) HIV and T cell expansion in splenic white pulps is accompanied by infiltration of HIV-specific cytotoxic T lymphocytes. Cell 78(3):373–387
Clavel F, Charneau P (1994) Fusion from without directed by human immunodeficiency virus particles. J Virol 68(2):1179–1185
Davis MR, Jiang J et al (2006) A mutation in the human immunodeficiency virus type 1 Gag protein destabilizes the interaction of the envelope protein subunits gp120 and gp41. J Virol 80(5):2405–2417
de Parseval A, Lerner DL et al (1997) Blocking of feline immunodeficiency virus infection by a monoclonal antibody to CD9 is via inhibition of virus release rather than interference with receptor binding. J Virol 71(8):5742–5749
Deneka M, Pelchen-Matthews A et al (2007) In macrophages, HIV-1 assembles into an intracellular plasma membrane domain containing the tetraspanins CD81, CD9, and CD53. J Cell Biol 177(2):329–341
Dong X, Li H et al (2005) AP-3 directs the intracellular trafficking of HIV-1 Gag and plays a key role in particle assembly. Cell 120(5):663–674
Espenel C, Margeat E et al (2008) Single-molecule analysis of CD9 dynamics and partitioning reveals multiple modes of interaction in the tetraspanin web. J Cell Biol 182(4):765–776
Fackler OT, Alcover A et al (2007) Modulation of the immunological synapse: a key to HIV-1 pathogenesis? Nat Rev Immunol 7(4):310–317
Fais S, Borghi P et al (1996) Human immunodeficiency virus type 1 induces cellular polarization, intercellular adhesion molecule-1 redistribution, and multinucleated giant cell generation in human primary monocytes but not in monocyte-derived macrophages. Lab Invest 75(6):783–790
Fradkin LG, Kamphorst JT et al (2002) Genomewide analysis of the Drosophila tetraspanins reveals a subset with similar function in the formation of the embryonic synapse. Proc Natl Acad Sci USA 99(21):13663–13668
Freed EO (2004) HIV-1 and the host cell: an intimate association. Trends Microbiol 12(4):170–177
Friedl P, den Boer AT et al (2005) Tuning immune responses: diversity and adaptation of the immunological synapse. Nat Rev Immunol 5(7):532–545
Garcia E, Nikolic DS et al (2008) HIV-1 replication in dendritic cells occurs through a tetraspanin-containing compartment enriched in AP-3. Traffic 9(2):200–214
Gluschankof P, Mondor I et al (1997) Cell membrane vesicles are a major contaminant of gradient-enriched human immunodeficiency virus type-1 preparations. Virology 230(1):125–133
Goff SP (2007) Host factors exploited by retroviruses. Nat Rev Microbiol 5(4):253–263
Goff SP (2008) Knockdown screens to knockout HIV-1. Cell 135(3):417–420
Gordon-Alonso M, Yanez-Mo M et al (2006) Tetraspanins CD9 and CD81 modulate HIV-1-induced membrane fusion. J Immunol 177(8):5129–5137
Grigorov B, Arcanger F et al (2006) Assembly of infectious HIV-1 in human epithelial and T-lymphoblastic cell lines. J Mol Biol 359(4):848–862
Grigorov BV, Attuil-Audenis V et al (2009) A role for CD81 on the late steps of HIV-1 replication in a chronically infected T cell line. Retrovirolgy 6:28
Hemler ME (2005) Tetraspanin functions and associated microdomains. Nat Rev Mol Cell Biol 6(10):801–811
Hemler ME (2008) Targeting of tetraspanin proteins - potential benefits and strategies. Nat Rev Drug Discov 7(9):747–758
Higginbottom A, Takahashi Y et al (2003) Structural requirements for the inhibitory action of the CD9 large extracellular domain in sperm/oocyte binding and fusion. Biochem Biophys Res Commun 311(1):208–214
Ho SH, Martin F et al (2006) Recombinant extracellular domains of tetraspanin proteins are potent inhibitors of the infection of macrophages by human immunodeficiency virus type 1. J Virol 80(13):6487–6496
Hope TJ (2007) Bridging efficient viral infection. Nat Cell Biol 9(3):243–244
Hosmalin A, Samri A et al (2001) HIV-specific effector cytotoxic T lymphocytes and HIV-producing cells colocalize in white pulps and germinal centers from infected patients. Blood 97(9):2695–2701
Huang S, Yuan S et al (2005) The phylogenetic analysis of tetraspanins projects the evolution of cell-cell interactions from unicellular to multicellular organisms. Genomics 86(6):674–684
Hunter E, Swanstrom R (1990) Retrovirus envelope glycoproteins. Curr Top Microbiol Immunol 157:187–253
Igakura T, Stinchcombe JC et al (2003) Spread of HTLV-I between lymphocytes by virus-induced polarization of the cytoskeleton. Science 299(5613):1713–1716
Imai T, Kakizaki M et al (1995) Molecular analyses of the association of CD4 with two members of the transmembrane 4 superfamily, CD81 and CD82. J Immunol 155(3):1229–1239
Inoue N, Ikawa M et al (2005) The immunoglobulin superfamily protein Izumo is required for sperm to fuse with eggs. Nature 434(7030):234–238
Jaiswal JK, Chakrabarti S et al (2004) Synaptotagmin VII restricts fusion pore expansion during lysosomal exocytosis. PLoS Biol 2(8):E233
Janvier K, Bonifacino JS (2005) Role of the Endocytic Machinery in the Sorting of Lysosome-associated Membrane Proteins. Mol Biol Cell 16(9):4231–4242
Jiang J, Aiken C (2006) Maturation of the viral core enhances the fusion of HIV-1 particles with primary human T cells and monocyte-derived macrophages. Virology 346(2):460–468
Jiang J, Aiken C (2007) Maturation-dependent human immunodeficiency virus type 1 particle fusion requires a carboxyl-terminal region of the gp41 cytoplasmic tail. J Virol 81(18):9999–10008
Johnson DC, Huber MT (2002) Directed egress of animal viruses promotes cell-to-cell spread. J Virol 76(1):1–8
Jolly C, Kashefi K et al (2004) HIV-1 cell to cell transfer across an Env-induced, actin-dependent synapse. J Exp Med 199(2):283–293
Jolly C, Sattentau QJ (2007) Human immunodeficiency virus type 1 assembly, budding, and cell-cell spread in T cells take place in tetraspanin-enriched plasma membrane domains. J Virol 81(15):7873–7884
Jouvenet N, Bieniasz PD et al (2008) Imaging the biogenesis of individual HIV-1 virions in live cells. Nature 454(7201):236–240
Kaizuka Y, Douglass AD et al (2007) Mechanisms for segregating T cell receptor and adhesion molecules during immunological synapse formation in Jurkat T cells. Proc Natl Acad Sci USA 104(51):20296–20301
Kaji K, Oda S et al (2002) Infertility of CD9-deficient mouse eggs is reversed by mouse CD9, human CD9, or mouse CD81; polyadenylated mRNA injection developed for molecular analysis of sperm-egg fusion. Dev Biol 247(2):327–334
Kapadia SB, Barth H et al (2007) Initiation of hepatitis C virus infection is dependent on cholesterol and cooperativity between CD81 and scavenger receptor B type I. J Virol 81(1):374–383
Khurana S, Krementsov DN et al (2007) Human immunodeficiency virus type 1 and influenza virus exit via different membrane microdomains. J Virol 81(22):12630–12640
Krementsov DN, Weng J et al (2009) Tetraspanins regulate cell-to-cell transmission of HIV-1. Retrovirology 6:64
Le Naour F, Rubinstein E et al (2000) Severely reduced female fertility in CD9-deficient mice. Science 287(5451):319–321
Levy S, Shoham T (2005a) Protein-protein interactions in the tetraspanin web. Physiology (Bethesda) 20:218–224
Levy S, Shoham T (2005b) The tetraspanin web modulates immune-signalling complexes. Nat Rev Immunol 5(2):136–148
Mantegazza AR, Barrio MM et al (2004) CD63 tetraspanin slows down cell migration and translocates to the endosomal-lysosomal-MIICs route after extracellular stimuli in human immature dendritic cells. Blood 104(4):1183–1190
Marsh M, Pelchen-Matthews A (2000) Endocytosis in viral replication. Traffic 1(7):525–532
Mazurov D, Heidecker G et al (2007) The inner loop of tetraspanins CD82 and CD81 mediates interactions with human T cell lymphotrophic virus type 1 Gag protein. J Biol Chem 282(6):3896–3903
Meerloo T, Parmentier HK et al (1992) Modulation of cell surface molecules during HIV-1 infection of H9 cells. An immunoelectron microscopic study. Aids 6(10):1105–1116
Meerloo T, Sheikh MA et al (1993) Host cell membrane proteins on human immunodeficiency virus type 1 after in vitro infection of H9 cells and blood mononuclear cells. An immuno-electron microscopic study. J Gen Virol 74(Pt 1):129–135
Min G, Wang H et al (2006) Structural basis for tetraspanin functions as revealed by the cryo-EM structure of uroplakin complexes at 6-A resolution. J Cell Biol 173(6):975–983
Miyado K, Yamada G et al (2000) Requirement of CD9 on the egg plasma membrane for fertilization. Science 287(5451):321–324
Miyado K, Yoshida K et al (2008) The fusing ability of sperm is bestowed by CD9-containing vesicles released from eggs in mice. Proc Natl Acad Sci USA 105(35):12921–12926
Morita E, Sundquist WI (2004) Retrovirus budding. Annu Rev Cell Dev Biol 20:395–425
Murakami T (2008) Roles of the interactions between Env and Gag proteins in the HIV-1 replication cycle. Microbiol Immunol 52(5):287–295
Murakami T, Ablan S et al (2004) Regulation of human immunodeficiency virus type 1 Env-mediated membrane fusion by viral protease activity. J Virol 78(2):1026–1031
Murray JL, Mavrakis M et al (2005) Rab9 GTPase is required for replication of human immunodeficiency virus type 1, filoviruses, and measles virus. J Virol 79(18):11742–11751
Nydegger S, Foti M et al (2003) HIV-1 egress is gated through late endosomal membranes. Traffic 4(12):902–910
Nydegger S, Khurana S et al (2006) Mapping of tetraspanin-enriched microdomains that can function as gateways for HIV-1. J Cell Biol 173(5):795–807
Ohno H, Aguilar RC et al (1997) Interaction of endocytic signals from the HIV-1 envelope glycoprotein complex with members of the adaptor medium chain family. Virology 238(2):305–315
Ohta H, Tsurudome M et al (1994) Molecular and biological characterization of fusion regulatory proteins (FRPs): anti-FRP mAbs induced HIV-mediated cell fusion via an integrin system. Embo J 13(9):2044–2055
Ono A, Freed EO (2005) Role of lipid rafts in virus replication. Adv Virus Res 64:311–358
Orentas RJ, Hildreth JE (1993) Association of host cell surface adhesion receptors and other membrane proteins with HIV and SIV. AIDS Res Hum Retroviruses 9(11):1157–1165
Pelchen-Matthews A, Kramer B et al (2003) Infectious HIV-1 assembles in late endosomes in primary macrophages. J Cell Biol 162(3):443–455
Phillips DM (1994) The role of cell-to-cell transmission in HIV infection. Aids 8(6):719–731
Piguet V, Sattentau Q (2004) Dangerous liaisons at the virological synapse. J Clin Invest 114(5):605–610
Pique C, Lagaudriere-Gesbert C et al (2000) Interaction of CD82 tetraspanin proteins with HTLV-1 envelope glycoproteins inhibits cell-to-cell fusion and virus transmission. Virology 276(2):455–465
Raposo G, Moore M et al (2002) Human macrophages accumulate HIV-1 particles in MHC II compartments. Traffic 3(10):718–729
Rowell JF, Stanhope PE et al (1995) Endocytosis of endogenously synthesized HIV-1 envelope protein Mechanism and role in processing for association with class II MHC. J Immunol 155(1):473–488
Ruiz-Mateos E, Pelchen-Matthews A et al (2008) CD63 is not required for production of infectious human immunodeficiency virus type 1 in human macrophages. J Virol 82(10):4751–4761
Runge KE, Evans JE et al (2007) Oocyte CD9 is enriched on the microvillar membrane and required for normal microvillar shape and distribution. Dev Biol 304(1):317–325
Sato K, Aoki J et al (2007) Modulation of Human Immunodeficiency Virus Type 1 Infectivity through Incorporation of Tetraspanin Proteins. J Virol 82(2):1021–1033
Sattentau Q (2008) Avoiding the void: cell-to-cell spread of human viruses. Nat Rev Microbiol 6(11):815–826
Sauter MM, Pelchen-Matthews A et al (1996) An internalization signal in the simian immunodeficiency virus transmembrane protein cytoplasmic domain modulates expression of envelope glycoproteins on the cell surface. J Cell Biol 132(5):795–811
Seigneuret M, Delaguillaumie A et al (2001) Structure of the tetraspanin main extracellular domain. A partially conserved fold with a structurally variable domain insertion. J Biol Chem 276(43):40055–40064
Singethan K, Muller N et al (2008) CD9 clustering and formation of microvilli zippers between contacting cells regulates virus-induced cell fusion. Traffic 9(6):924–935
Sourisseau M, Sol-Foulon N et al (2007) Inefficient human immunodeficiency virus replication in mobile lymphocytes. J Virol 81(2):1000–1012
Stipp CS, Kolesnikova TV et al (2003) Functional domains in tetraspanin proteins. Trends Biochem Sci 28(2):106–112
Sylwester A, Murphy S et al (1997) HIV-induced T cell syncytia are self-perpetuating and the primary cause of T cell death in culture. J Immunol 158(8):3996–4007
Tachibana I, Hemler ME (1999) Role of transmembrane 4 superfamily (TM4SF) proteins CD9 and CD81 in muscle cell fusion and myotube maintenance. J Cell Biol 146(4):893–904
Takeda Y, He P et al (2008) Double deficiency of tetraspanins CD9 and CD81 alters cell motility and protease production of macrophages and causes chronic obstructive pulmonary disease-like phenotype in mice. J Biol Chem 283(38):26089–26097
Takeda Y, Tachibana I et al (2003) Tetraspanins CD9 and CD81 function to prevent the fusion of mononuclear phagocytes. J Cell Biol 161(5):945–956
Tardif MR, Tremblay MJ (2005) Tetraspanin CD81 provides a costimulatory signal resulting in increased human immunodeficiency virus type 1 gene expression in primary CD4+ T lymphocytes through NF-kappaB, NFAT, and AP-1 transduction pathways. J Virol 79(7):4316–4328
Turville SG, Aravantinou M et al (2008) Resolution of de novo HIV production and trafficking in immature dendritic cells. Nat Methods 5(1):75–85
Unternaehrer JJ, Chow A et al (2007) The tetraspanin CD9 mediates lateral association of MHC class II molecules on the dendritic cell surface. Proc Natl Acad Sci USA 104(1):234–239
Vasiliver-Shamis G, Tuen M et al (2008) Human immunodeficiency virus type 1 envelope gp120 induces a stop signal and virological synapse formation in noninfected CD4+ T cells. J Virol 82(19):9445–9457
von Lindern JJ, Rojo D et al (2003) Potential role for CD63 in CCR5-mediated human immunodeficiency virus type 1 infection of macrophages. J Virol 77(6):3624–3633
Welsch S, Keppler OT et al (2007) HIV-1 Buds Predominantly at the Plasma Membrane of Primary Human Macrophages. PLoS Pathog 3(3):e36
Weng J, Krementsov DN et al (2009) Formation of syncytia is repressed by tetraspanins in HIV-1 producing cells. J Virol 83(15):7467–7474
Wright MD, Moseley GW et al (2004) Tetraspanin microdomains in immune cell signalling and malignant disease. Tissue Antigens 64(5):533–542
Wyma DJ, Jiang J et al (2004) Coupling of human immunodeficiency virus type 1 fusion to virion maturation: a novel role of the gp41 cytoplasmic tail. J Virol 78(7):3429–3435
Yang X, Kovalenko OV et al (2004) Palmitoylation supports assembly and function of integrin-tetraspanin complexes. J Cell Biol 167(6):1231–1240
Yoshida T, Kawano Y et al (2008) A CD63 mutant inhibits T-cell tropic human immunodeficiency virus type 1 entry by disrupting CXCR4 trafficking to the plasma membrane. Traffic 9(4):540–558
Zhu GZ, Miller BJ et al (2002) Residues SFQ (173–175) in the large extracellular loop of CD9 are required for gamete fusion. Development 129(8):1995–2002
Ziyyat A, Rubinstein E et al (2006) CD9 controls the formation of clusters that contain tetraspanins and the integrin alpha 6 beta 1, which are involved in human and mouse gamete fusion. J Cell Sci 119(Pt 3):416–424
Acknowledgements
I thank the current members of my group, Dimitry Krementsov, Marie Lambelé, Nate Roy and Jia Weng, for critical reading of the manuscript. Work in our laboratory is supported by the NIH and by UVM’s College of Medicine.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Thali, M. (2009). The Roles of Tetraspanins in HIV-1 Replication. In: Spearman, P., Freed, E. (eds) HIV Interactions with Host Cell Proteins. Current Topics in Microbiology and Immunology, vol 339. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-642-02175-6_5
Download citation
DOI: https://doi.org/10.1007/978-3-642-02175-6_5
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-02174-9
Online ISBN: 978-3-642-02175-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)