Abstract
In multiple myeloma, imaging is required to determine the stage of disease and to anticipate impending bone fractures. Whereas the traditionally used Durie and Salmon staging system includes lytic bone lesions in plain films as criteria, modern systems include MRI findings. MRI is most sensitive to both diffuse bone marrow involvement as well as solid plasma cell tumors. Whole-body low-dose CT (WBCT) may replace plain films in the near future, since it is quicker, more sensitive, and is better tolerated by patients. Intramedullary lesions are well seen as long as they are located in long bones where they are surrounded by fat. Diffuse bone marrow infiltration as well as intravertebral lesions, however, are difficult to detect with WBCT in the absence of frank destruction of cancellous bone. PET or PET-CT with 18-fluoro-deoxyglucose (FDG) are insensitive to diffuse bone marrow infiltration, but may help to assess treatment response in solitary or multiple solid plasma cell tumors which have a high FDG uptake before treatment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Positron Emission Tomography
- Multiple Myeloma
- Apparent Diffusion Coefficient
- Malignant Plasma Cell
- Diffuse Bone Marrow
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Multiple myeloma is a low-grade non-Hodgkin’s B-cell lymphoma which is characterized by a proliferation of monoclonal, malignant plasma cells. It is a disease which usually originates in the bone marrow, and eventually extends into soft tissue or spreads into the peripheral blood (plasma cell leukemia). The main effects and causes of pain and disability are replacement of hematopoietic bone marrow (leading to anemia, leucopenia, and thrombocytopenia, and their sequelae), osteoporosis and bone destruction (leading to fractures and pain), renal damage by paraproteins, and systemic amyloidosis. The treatment consists of chemotherapy (often high-dose with stem cell rescue), thalidomide and its derivates, proteasome inhibitors, and bisphosphonates. Radiotherapy is used for local manifestations which are particularly painful, or where complications are imminent. Surgical stabilizations also have an important role for local disease. Vertebroplasty or kyphoplasty are used to prevent progressive vertebral collapse, and to treat pain. To date, however, there is no definite cure.
The term “plasmacytoma” denotes solitary plasma cell tumors without evidence of systemic spread – which has to be excluded by serum and bone marrow samples as well as imaging studies. They may also primarily arise outside the bone and are then termed “extraosseous soft-tissue myeloma.” As a rule, soft-tissue involvement – either primary or secondary (by extension from a bone lesion) – indicates a dismal prognosis.
Monoclonal gammopathy of unclear significance (MGUS) has to be discriminated to overt multiple myeloma. Its criteria are a M-protein in serum <30 g/l, bone marrow plasma cells <10%, no evidence of any other B-cell proliferative disorders and no related organ or tissue impairment, such as renal damage or bone lesions (International myeloma working group 2003).
Multiple myeloma causes a wide variety of symptoms and complications, fractures and destruction of bones being the most painful and disabling ones. In osteoporotic bones, typically in the spine, fractures may occur with minimal trauma – or at least trauma insufficient to cause fracture in a normal bone. Fractures of tubular bones, whose stability relies mainly on cortical, not cancellous bone, are most commonly caused by focal solid myeloma nodules which erode the cortex from inside outward. Therefore, the radiologist is required to anticipate impending fractures and initiate referral for surgical stabilization or vertebroplasty. Furthermore, the presence or absence of focal destructions is an important criterion for initial staging (e.g., using the Durie and Salmon staging system) and for follow-up. Until today, the x-ray skeletal survey is standard for screening the skeleton for osteoporosis and bone destruction. Not surprisingly, whole-body CT is superior to plain x-ray films for finding focal bone destructions (Mahnken et al. 2002), and MRI is even more sensitive (Baur-Melnyk et al. 2008), particularly in the vertebral bone marrow, to show diffuse or focal involvement which has not or not yet caused destruction of mineralized bone.
2 Imaging Methods
2.1 Morphologic Imaging
We term plain x-ray, CT, and MRI “morphological” imaging techniques, as opposed to functional ones which measure microcirculation, diffusion, or metabolic processes. A plain x-ray skeletal survey is standard for staging and follow-up of bone involvement by multiple myeloma, and consists of a frontal and lateral view of the skull, the cervical, thoracic, and lumbar spine, a coned-down frontal image of the dens axis, as well as frontal views of the rib cage, humeri, femora, knees, and pelvis. The hallmark of neoplastic bone involvement is osteoporosis or focal destruction. CT, or whole-body CT (which requires state-of-the-art multidetector scanners) is reasonable alternative to x-ray films, for many reasons. Since the intrinsic contrast is high, the tube current can be lowered significantly (i.e., to 50–100 mAs, depending on the weight of the patient), resulting in an effective equivalent dose in the same range as that of a skeletal survey (4–5 mSv). The entire examination takes around 1 or 2 min, the patient lying comfortably on his or her back. Note that the varied positions required for x-ray films are painful and tiring for patients who are often elderly and disabled due to previous fractures. Iodine-containing contrast agents are contraindicated for patients with Bence-Jones proteinuria because of the risk of cast nephropathy and renal failure, and actually they are not needed for skeletal CT. Focal bone destruction is more easily seen than on plain films, and also easier to discriminate from normal sparing in trabecular bone, which will have fat and not soft-tissue density. Diffuse bone marrow involvement within preserved spongious bone, however, is difficult to detect with CT and better seen with MRI.
MRI of the spine, or whole-body MRI, is to date the most sensitive method for detecting diffuse and focal multiple myeloma in the spine as well as the extra-axial skeleton. Sequences commonly used are unenhanced and contrast-enhanced T1-weighted spin-echo sequences and T2-weighted sequences with fat suppression, either by spectral pre-saturation, or using STIR (short tau inversion recovery) techniques. If scanners with whole-body capabilities are available, the examination should include the entire skeleton, since most patients have axial as well as extra-axial bone lesions. If not, at least the spine should be scanned with MRI, because of the insensitivity of CT and plain x-ray films to intravertebral myeloma.
2.2 Functional Imaging
All of the above methods show the extent of tumor (or more specifically its damage to mineralized bone) but not its activity or viability, and have limitations when assessing treatment response or early progression. Patients with monoclonal gammopathy of unclear significance constitute a particular problem, because they have no measurable lesion at all which could be followed over time to anticipate progression. Functional imaging methods therefore measure microcirculation, diffusion of interstitial water molecules or glucose uptake as surrogates for tumor viability, and aggressiveness.
2.2.1 Dynamic Contrast-Enhanced MRI (DCE MRI)
The term DCE MRI denotes repeat scanning with high temporal resolution before, during, and after intravenous infusion of a Gadolinium-containing contrast agent, using fast T1-weighted sequences. The change in signal intensity (which depends on the concentration of contrast agent) over time in a given region is a function of local perfusion, relative blood volume, capillary surface exchange area, vessel permeability, and systemic elimination. To quantitatively describe such time-concentration curves, pharmacokinetic models are used, but the interpretation of parameters derived in this way with respect to pathophysiological processes has to be made with great caution. The parameter which is easiest to interpret is the maximal relative rise in intensity, since this is chiefly determined by the local, regional blood volume.
2.2.2 Diffusion-Weighted Imaging (DWI)
The freedom of interstitial water molecules to move depends on many factors, but cell density or the presence of organized structures (e.g., fibers) are of high influence. Studies, e.g., in brain tumors have shown that the diffusion is impaired within tumors, and that a decrease of diffusion may herald progression. Effective treatment may cause a transient decrease in diffusion, owing to toxic cell swelling, but thereafter, as the cellular load is reduced, diffusion increases significantly. DWI uses opposing phase gradients switched shortly after each other, which causes rephasing and thereby regain of signal in stationary water, but a signal loss in moving molecules. Within a certain range, such signal loss can be mainly attributed to diffusion rather than blood flow, and using varying gradient strengths and durations, the apparent diffusion coefficient (ADC) can be calculated. The experiences with multiple myeloma are still limited, and due to the presence of trabeculae, the conditions are more difficult than in the brain. However, it can be shown that a low ADC in fractured vertebrae indicates local tumor infiltration as a cause rather than osteoporosis. It is still unclear whether DWI may serve as a tool to monitor treatment or progression. Bone marrow in myeloma patients contains several components which may influence diffusion processes separately, such as hematopoietic cells, fatty marrow, and plasmacellular infiltrates, and it is unclear how changes in its composition will influence diffusion. Solid myeloma nodules will probably be more easily assessed since they lack hematopoietic and fatty components (Mulkern and Schwartz 2003).
2.2.3 Bone Scintigraphy and Positron Emission Tomography (PET)
Bone scintigraphy, using 99 m Tc-labeled bisphosphonates, is insensitive to diffuse or focal myeloma because there is no increased osteoblastic activity – unlike bone metastases from most other solid tumors. PET with 18-F-deoxyglucose (FDG) detects tumors according to their glucose demand, the glucose transport molecules expressed in the cell membrane, the local cell density, and the metabolic activity of the surrounding tissue. As a rule, multiple myeloma has a rather low metabolic activity, and is hardly detected when only a diffuse bone marrow involvement is present – simply because the local cell density is too low. Whenever myeloma is detected on PET scans – this is often the case in solid myeloma nodules – the standardized uptake value is a good parameter to monitor response, since after chemotherapy, the drop in glucose uptake clearly precedes the morphologically measurable response.
3 Radiological–Pathological Correlation
Three patterns of spread of multiple myeloma are relevant for imaging: diffuse bone marrow involvement, focal bone destructions by solid tumor nodules, and extraosseous manifestations. In diffuse bone marrow involvement, generalized or partial, hematopoietic and fatty marrow and plasmacellular infiltrates are found besides each other. In the beginning fat cell content might be even increased and hematopoiesis is still normal. As malignant plasma cells increase in number, they gradually replace normal marrow. Thus, there is a shift with an increase of cellular, and a decrease of fatty components. This process takes place within a preserved cancellous bone, which only gradually becomes eroded. Very typically, osteoporosis triggered by multiple myeloma progresses more rapidly than other forms, particularly senile or postmenopausal ones. Degradation of bone is mediated via osteoclast-activating factors (typically RANK-Ligand, Interleukin-2 and TNF) and amounts to frank focal destructions, where solid tumor nodules are present which contain almost no bony remnants. Such nodules contain malignant plasma cells and some tumor stroma, but neither hematopoietic fatty nor osseous components, and behave like any destructively growing solid tumor. Obviously, the loss of stability is much more severe than with diffuse bone marrow infiltration where the cancellous bone is at least partly preserved. Any destruction of cortical bone is by definition due to solid myeloma nodules.
Diffuse and focal bone involvement are commonly seen besides each other. Focal nodules may eventually extend beyond the confines of the bone and invade adjacent tissue, where they can cause symptoms like any other solid malignant tumor. Although the commonest cause of soft-tissue involvement is the extension of a primary bone lesion into adjacent tissue but primary soft-tissue lesions are also observed. Their pattern of spread does not usually follow the pathways commonly seen in carcinomas, but is often rather “atypical”, like in melanoma or non-epithelial neoplasms (Zechmann et al. 2007).
By their nature, x-ray films only show the effects of myeloma on mineralized bone, namely, osteoporosis (Fig. 7.1a, b) and focal destructions (Fig. 7.2). The criteria of osteoporosis are the same as those used for postmenopausal or idiopathic forms, and it is the axial skeleton which is mainly involved. Rapid progression and an inhomogeneous, coarse and streaky appearance of the vertebral spongiosa are signs which may raise suspicion of a neoplastic cause in patients with osteoporosis, and so will osteoporosis in the young and in males. Otherwise only focal destructions will point more specifically at the true underlying cause. Notably, the presence of osteoporosis in patients with known plasma cell disorders does not prove a causal relationship. Due to its severity and rapid progression, osteoporosis due to myeloma frequently causes vertebral compression fractures, which are most often diagnosed on radiographs, but whose impact on stability should be assessed on CT.
Lateral (a) and frontal (b) lumbar spine x-ray films in a patient with multiple myeloma. Corresponding sagittal reconstruction from whole-body low-dose computed CT (WBCT) (c), sagittal T1-weighted (d) and fat-suppressed T2-weighted (e) MRI slices. Signs of osteoporosis are visible on the plain films as well as the reconstructed WBCT slices. There is a focal destruction in the third lumbar vertebra (arrows) which is visible on WBCT (c), and which corresponds to an area of low signal intensity in T1-weighted (d), and a slightly elevated signal intensity on fat-suppressed T2-weighted images (e). Without fat suppression, this area appears hypointense, due to the relatively high signal intensity of the surrounding. On the plain films, however (a, b), the corresponding region (arrows) appears innocent, and is also difficult to assess due to superimposition of bowel gas. The T1-weighted MRI also shows signs of diffuse bone marrow involvement, with a “salt-and-pepper” appearance in the not fat-suppressed T1- and T2-weighted images (d)
Focal areas of destruction are by definition always due to solid myeloma nodules, which arise in the cancellous bone but then erode the cortical bone from the inside, causing the typical “scalloped” appearance (Fig. 7.2). In the skull, this occurs early, resulting in multiple, sharply delineated osteolytic lesions. As a rule, areas of focal, lytic bone destruction are more easily seen in cortical than in cancellous bone, because of the contrast between the defect and its surrounding. Areas of destruction inside the spongiosa of the vertebral bodies are almost invisible on radiographs (Fig. 7.1a, b), and the superimposition of soft tissue, air, or ribs makes the assessment even more difficult. In one study, half of the cases proven to have vertebral involvement on MRI were negative on x-ray films (Baur et al. 1996). Locations where trabeculae are “physiologically” rarefied, e.g., in the femoral neck, and which are common in the elderly, may be mistaken for lytic lesions. CT showing fatty density and MRI can rule out infiltration by myeloma.
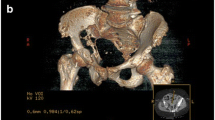
Like x-ray films, computed tomography (CT) mainly shows alterations to mineralized bone, but there are no problems with superimposition. Pure bone marrow infiltrates may also be seen if they lie within fatty marrow, but are hardly visible in vertebral bodies (Fig. 7.3e), unless they are very osteoporotic. Furthermore, osteolytic areas in cancellous bone, which are occult to plain films, are easily detected. CT is the gold standard to assess the stability of bone and should be performed prior to vertebroplasty to ensure that the cortex is intact and the vertebral body will retain the injected material.
Coronal reconstructions in WBCT over the long bones (a, b), frontal (c) and lateral (d) cervical x-ray films, sagittal WBCT reconstruction over the spine (e), and sagittal T2-weighted, fat-suppressed MRI (f) of the cervical spine in a patient with multiple myeloma. The long bones show no focal destructions. Note the low density in the CT of the medullary spaces of the long bones where any solid, intramedullary nodule would be frankly visible. The plain films of the cervical spine appear normal, and the sagittal reconstruction of WBCT shows osteoporosis, a fracture of the ninth thoracic vertebra, but no focal areas of destruction inside the vertebral bodies. The cervical MRI, however shows focal T2 hyperintense areas in the fourth and fifth cervical vertebra, along with disseminated tiny areas of signal elevation in all other vertebral bodies and spinous processes, typical of myeloma infiltration, and invisible with both plain x-rays and CT
In magnetic resonance imaging (MRI), the signal intensity of the spinal bone marrow on both T1- and T2-weighted images depends on the relation of fatty and cellular components, cellular ones being either hematopoietic marrow or plasmacellular infiltrates. In adults in the axial skeleton hematopoietic “red” marrow is present. In the periphery “yellow” fatty marrow is present. With age the fatty components within red marrow (usually 40–50%) increases. Typically, the vertebral bodies are T1-hyperintense (i.e., brighter than the intervertebral disk) and hypointense on fat-suppressed T2-weighted images (darker than normal disks). An increase in the cellular and decrease of the fatty component in the bone marrow will cause a decrease in T1 and an increase in signal on STIR images (Wasser et al. 2005). The best combination of sequences for imaging myeloma is a combination of T1-w SE and fat-suppressed sequences, e.g., STIR (Baur et al. 1998).
On T1- and T2-weighted images without fat suppression, one may also see a “salt-and-pepper” pattern, which is a mixture of small hypointense and hyperintense spots (Fig. 7.1d). This reflects an inhomogeneous composition of bone marrow with fatty islands and low-grade interstitial infiltration by myeloma cells. Those patients are usually stage I disease and do not require any treatment. Beware of pitfalls like young individuals with a high amount of hematopoiesis (thus low signal on T1-w SE images), or patients pre-treated with chemotherapy and possibly growth factors, in whom bone marrow reconversion may cause grossly misleading findings on MRI.
Since multiple myeloma is angiogenic, involved bone marrow shows enhancement on fat-suppressed, contrast-enhanced T1-weighted images. The strength of enhancement has been histologically proven to depend on the degree of infiltration by myeloma cells, and also on vessel density (Baur et al. 2004; Nosas-Garcia 2004; Nosas-Garcia et al. 2005). Therefore, contrast-enhanced MRI may be used whenever unenhanced T1w or STIR images are inconclusive. Again, there is some age-dependence, but as a rule a signal increase by 40% or more is deemed pathological (Baur et al. 2004). Dynamic contrast-enhanced MRI may be used to better assess the kinetics of contrast enhancement (Fig. 7.4).
Parameter maps from dynamic contrast-enhanced MRI (DCE MRI) (a) in a patient with multiple myeloma, showing diffuse and rather homogeneous contrast enhancement. A time-intensity curve obtained from these vertebrae (b) shows an early but nevertheless gradual rise in intensity during the first two minutes, followed by a “wash-out”
Solid myeloma nodules are homogeneously T1-hypointense and hyperintense on fat-suppressed images and show a strong enhancement on post-contrast images (Fig. 7.5). A breech of the cortical bone is easy to see, as the signal-free bone contour is interrupted, and the tumor extends beyond it. The distinction between diffuse and micronodular patterns is not sharp, and thus such discrimination is somewhat academic. In every area of bone destruction caused by myeloma a corresponding myeloma nodule should be found on MRI. A possible exception is the case of collapsed vertebrae in which compressed bone and reactive changes may cause the diagnosis to be difficult.
Parameter maps from dynamic contrast-enhanced MRI (DCE MRI) (a) in a patient with multiple myeloma, showing markedly inhomogeneous enhancement and “hot spots” in the third and fourth vertebra, which on static images corresponded to solid plasma cell tumors. The time-intensity curve obtained from these areas (b) shows a marked and sharp rise with a maximum at one minute after injection, followed by a wash-out. Note the distinct difference between the curves in 7.4b (diffuse pattern) and 7.5b (focal pattern)
In positron emission tomography (PET or PET/CT, respectively), solid myeloma nodules have an increased uptake of 18 F-deoxyglucose (FDG), but their conspicuousness depends on the uptake of the surrounding tissue. The sensitivity of FDG-PET in vertebral bone marrow depends on the infiltration degree: in 30% of cases positive on MRI, PET was false negative, most frequently in diffuse infiltration patterns (Zamagni et al. 2007). It is more sensitive than the x-ray skeletal survey (Zamagni et al. 2007), but less sensitive than multidetector-CT (Hur et al. 2007). However, PET-CT is better, since new MDCT scanners allow for high resolution of bone in addition to FDG uptake as a marker for avid tumor tissue. Thereby PET-CT may play an increasing role for evaluation of success of therapy (Bredella et al. 2005).
Nevertheless, PET for staging and risk assessment is favored over MRI in the Anglo-American world, the rationale being that those myeloma foci which are clinically and prognostically relevant will also be positive on PET (Durie 2006; Durie et al. 2002). In Germany, conversely, PET is hardly used for multiple myeloma, since it has been almost generally excluded from reimbursement by the legal insurers.
4 Differential Diagnosis
Metastases due to solid tumors are far more common than is multiple myeloma, and they may be difficult to discriminate (Ooi et al. 2006). Features in favor of multiple myeloma are:
-
Osteolytic lesions in the convexity of the skull and the diaphysis of long bones
-
Nonreactive, sharply delineated, lytic lesions
-
Scalloping (half-moon shaped erosions of cortical bone from its inward surface)
-
Marked osteoporosis
-
Negative bone scan or “cold lesions”
-
No primary tumor as a possible cause of bone metastases
Osteosclerotic lesions are unlikely to be myeloma, although rare forms of sclerosing myeloma have been described.
Multiple myeloma affects mostly patients aged 50 or more – an age group in which osteoporosis is common and usually not caused by malignant disease. To tell whether osteoporosis in a given patient with known myeloma is independent of or rather caused by the disease can be difficult or impossible in x-rays or CT. However, in MRI diffuse infiltration can be depicted as the underlying cause.
Degenerative changes – particularly osteochondrosis with inflammatory bone reaction – may cause pain and also signal alterations in MRI like T2 hyperintensities and contrast uptake. However, there are some typical features of benign alterations:
-
Hemispheric or triangular shape
-
Abutting the upper or lower end plate
-
Symmetric above and below one intervertebral disk
-
Loss of height and T2 signal of the adjacent disk
-
Osteosclerosis in CT
Fractured vertebrae may cause significant diagnostic problems. The lack of an overt destruction does not argue against a destruction as a cause, because the compression may have obscured it. In MRI, the features of fractures caused by either osteoporosis or myeloma may be also very similar, especially in severe collapse. Low T1 and high T2 signal intensity as well as marked contrast enhancement are signs in favor of malignant involvement as the underlying cause (Cuenod et al. 1996).
Diffusion-weighted MRI of fractured vertebrae may help in differential diagnosis showing a lower apparent diffusion coefficient when malignant involvement was the cause rather than when the fracture was due to trauma or osteoporosis (Raya et al. 2006).
5 Staging
The most widely used staging system – among more than ten systems – is the one proposed by Durie and Salmon in 1975, where the stages, ranging from one to three, rely on blood tests (e.g., hemoglobin, calcium, paraproteins) and the results of the x-ray skeletal survey (Durie and Salmon 1975). The latter are fallible, and their prognostic implications are very insecure because many lesions are missed. Most important is the discrimination between stage 1 and 2 without signs of disease progression, needing no treatment, and stages 2 or 3, both requiring chemotherapy. For current recommendations, see (Dispenzieri et al. 2007). A survival analysis demonstrated that the degree of skeletal involvement shown on MRI was pivotal for the patient’s prognosis. Including MRI findings in a clinical staging system, such as the Durie & Salmon system, significantly improved the discrimination between the three groups concerning survival (Baur et al. 2002). Cross-section imaging with either MRI (or whole-body MRI where available) or CT is progressively replacing the skeletal survey. Durie did suggest a modified staging system (“Durie & Salmon PLUS”) (Durie 2006). From what is known today, one would recommend performing whole-body MRI as a primary staging examination, and using x-ray films or CT for assessing bone stability where MRI is abnormal. If no scanners with whole-body capabilities are accessible, MRI should be performed for the entire spine, and the peripheral skeleton assessed with x-ray films or whole-body low-dose CT. Compared with whole-body MRI, however, CT appears to understage multiple myeloma (Baur-Melnyk et al. 2008). In addition, a baseline bone density measurement is always recommended.
6 Treatment Effects
MRI is without doubt the method of choice to monitor effects of chemotherapy, since it images the tumor directly, and not only its effects on mineralized bone, which may persist despite effective treatment. Chemotherapy will cause a reduction in T2 signal intensity and reduced contrast uptake in both diffusely involved bone marrow and solid nodules (Wasser et al. 2004). Although large studies are lacking, early results show that PET-CT might be a tool to show early effects of chemotherapy (Zamagni et al. 2007). In necrotic tumor a strong reduction of FDG uptake has been found (Bredella et al. 2002; Fonti et al. 2008).
7 Prognostic Factors
There are two events which are hard to predict: the progression into a stage needing treatment in patients with stage 1 multiple myeloma or monoclonal gammopathy of unclear significance (MGUS), and the occurrence of major complications – particularly fractures – in patients who already are in an advanced stage. Of patients with MGUS, e.g., 1% per year progress into myeloma (Kyle et al. 2002). Blood and bone marrow tests (albumin, paraproteins, β2-microglobulin, chromosomal and genetic factors) and the urine excretion of paraproteins are important factors, and so are the initial stage and the presence or absence of skeletal abnormalities (lytic lesions, osteoporosis with compression fractures). According to the criteria of the International Myeloma Working Group, the diagnosis of absence of bone involvement still relies on plain films, and CT or MRI are tools for clarification only (International myeloma working group 2003). However, a considerable proportion of MGUS patients do have abnormal findings at MRI – most frequently diffuse ones (T1 hypointensity, salt-and-pepper appearance), occasionally also focal lesions. Very probably, their classification as having MGUS rather than multiple myeloma is false, owing to the limited sensitivity of plain films, but there is no consensus as yet, when and how they should be “upstaged.” In the new staging system of Durie & Salmon PLUS (Durie 2006), in patients with MGUS, whole-body MRI or PET-CT are required to exclude myeloma involvement (Table 7.1).
In patients, stage I disease according to the old staging system, abnormalities (focal or diffuse) in the skeletal MRI imply a significantly worse prognosis (time to progression, 10–16 months) than if the MRI were normal (32–43 months) (Baur-Melnyk et al. 2005; Moulopoulos et al. 1995; Vande Berg et al. 1996; Walker et al. 2007).
In stage 2 or 3, the relevant parameter is the time until the diseases progresses clinically, particularly until complications like fractures occur. Here also, besides serum markers, a pathological MRI is an independent bad prognostic sign, in particular the intensity of contrast agent uptake (Hillengass et al. 2007).
8 The Radiologist’s Tasks
Diagnosis and treatment monitoring rely on bone marrow histology and serum and urine tests, such as monoclonal immunoglobins, activity markers (e.g., β-microglobulin), enzymes, blood film, electrolytes, etc. Non-secreting myeloma may be difficult to monitor; here imaging plays an even more crucial role. Generally, imaging serves to:
-
Verify the extent of skeletal and extraskeletal involvement
-
Supply the information required by commonly used staging systems (e.g., Durie & Salmon (PLUS))
-
Assess stability of involved bones
-
Assess treatment response
The x-ray skeletal survey, until now standard for staging, will probably not remain for a longer period of time, given the higher sensitivities of both CT and MRI, and the additional information they provide on marrow infiltration, local bone stability, and soft-tissue extension. By using MDCT and/or MRI, 30–40% of patients will be upstaged. Some modified staging systems (Durie and Salmon PLUS) which include whole-body MRI and/or PET-CT have been suggested.
In long bones, x-ray films are usually sufficient to assess their stability, but in vertebrae and the pelvis this is best done with CT, at least in doubtful cases. CT is also best before vertebroplasty to ensure that the posterior cortex is intact.
For treatment monitoring and follow-up, MRI is clearly superior to x-ray films, for good reasons. Areas of destruction to mineralized bone, as seen on films, are simply the tip of the iceberg, the underlying tumor being invisible, and they usually show no reaction or sclerosis though the tumor itself does respond. To some extent, the same limitations also apply to CT, although CT is capable of demonstrating solid nodules (Horger et al. 2007). In vertebrae, however, it is clearly inferior to MRI.
References
Baur A, Stäbler A, Bartl R, Lamerz R, Reiser M (1996) Infiltrationsmuster des Plasmozytoms in der Magnetresonanztomographie. Fortschr Röntgenstr 164:457–463
Baur A, Stäbler A, Steinborn M, Schnarkowski P, Pistitsch C, Lamerz R, Bartl R, Reiser M (1998) Magnetresonanztomographie beim Plasmozytom: Wertigkeit verschiedener Sequenzen bei diffuser und fokaler Infiltrationsform. Fortschr Röntgenstr 168:323–329
Baur A, Stäbler A, Nagel D, Lamerz R, Bartl R, Hiller E, Wendtner C, Bachner F, Reiser M (2002) Magnetic resonance imaging as a supplement for the clinical staging system of Durie and Salmon? Cancer 95:1334–1345
Baur A, Bartl R, Pellengahr C, Baltin V, Reiser M (2004) Neovascularization of bone marrow in patients with diffuse multiple myeloma: a correlative study of magnetic resonance imaging and histopathologic findings. Cancer 101:2599–2604
Baur-Melnyk A, Buhmann S, Durr HR, Reiser M (2005) Role of MRI for the diagnosis and prognosis of multiple myeloma. Eur J Radiol 55:56–63
Baur-Melnyk A, Buhmann S, Becker C, Schoenberg SO, Lang N, Bartl R, Reiser MF (2008) Whole-body MRI versus whole-body MDCT for staging of multiple myeloma. Am J Roentgenol 190:1097–1104
Bredella MA, Caputo GR, Steinbach LS (2002) Value of FDG positron emission tomography in conjunction with MR imaging for evaluating therapy response in patients with musculoskeletal sarcomas. Am J Roentgenol 179:1145–1150
Bredella MA, Steinbach L, Caputo G, Segall G, Hawkins R (2005) Value of FDG PET in the assessment of patients with multiple myeloma. Am J Roentgenol 184:1199–1204
Cuenod CA, Laredo JD, Chevret S, Hamze B, Naouri JF, Chapaux X, Bondeville JM, Tubiana JM (1996) Acute vertebral collapse due to osteoporosis or malignancy: appearance on unenhanced and gadolinium-enhanced MR images. Radiology 199:541–549
Dispenzieri A, Rajkumar SV, Gertz MA, Fonseca R, Lacy MQ, Bergsagel PL, Kyle RA, Greipp PR, Witzig TE, Reeder CB, Lust JA, Russell SJ, Hayman SR, Roy V, Kumar S, Zeldenrust SR, Dalton RJ, Stewart AK (2007) Treatment of newly diagnosed multiple myeloma based on Mayo Stratification of Myeloma and Risk-adapted Therapy (mSMART): consensus statement. Mayo Clin Proc 82:323–341
Durie BG (2006) The role of anatomic and functional staging in myeloma: description of Durie/Salmon plus staging system. Eur J Cancer 42:1539–1543
Durie BG, Salmon SE (1975) A clinical staging system for multiple myeloma. Correlation of measured myeloma cell mass with presenting clinical features, response to treatment, and survival. Cancer 36(3):842–854
Durie BG, Waxman AD, D’Agnolo A, Williams CM (2002) Whole-body (18)F-FDG PET identifies high-risk myeloma. J Nucl Med 43:1457–1463
Fonti R, Salvatore B, Quarantelli M, Sirignano C, Segreto S, Petruzziello F, Catalano L, Liuzzi R, Rotoli B, Del Vecchio S, Pace L, Salvatore M (2008) 18 F-FDG PET/CT, 99mTc-MIBI, and MRI in evaluation of patients with multiple myeloma. J Nucl Med 49:195–200
Hillengass J, Wasser K, Delorme S, Kiessling F, Zechmann C, Benner A, Kauczor HU, Ho AD, Goldschmidt H, Moehler T (2007) Lumbar bone marrow microcirculation measurements from dynamic contrast-enhanced MRI is a predictor of event-free survival in progressive multiple myeloma. Clin Cancer Res 13:475–481
Horger M, Kanz L, Denecke B, Vonthein R, Pereira P, Claussen CD, Driessen C (2007) The benefit of using whole-body, low-dose, nonenhanced, multidetector computed tomography for follow-up and therapy response monitoring in patients with multiple myeloma. Cancer 109:1617–1626
Hur J, Yoon CS, Ryu YH, Yun MJ, Suh JS (2007) Efficacy of multidetector row computed tomography of the spine in patients with multiple myeloma: comparison with magnetic resonance imaging and fluorodeoxyglucose-positron emission tomography. J Comput Assist Tomogr 31:342–347
International myeloma working group (2003) Criteria for the classification of monoclonal gammopathies, multiple myeloma and related disorders: a report of the International Myeloma Working Group. Br J Haematol 121(5):749–757
Kyle RA, Therneau TM, Rajkumar SV, Offord JR, Larson DR, Plevak MF, Melton LJ III (2002) A long-term study of prognosis in monoclonal gammopathy of undetermined significance. N Engl J Med 346:564–569
Mahnken AH, Wildberger JE, Gehbauer G, Schmitz-Rode T, Blaum M, Fabry U, Gunther RW (2002) Multidetector CT of the spine in multiple myeloma: comparison with MR imaging and radiography. Am J Roentgenol 178:1429–1436
Moulopoulos LA, Dimopoulos MA, Smith TL, Weber DM, Delasalle KB, Libshitz HI, Alexanian R (1995) Prognostic significance of magnetic resonance imaging in patients with asymptomatic multiple myeloma. J Clin Oncol 13:251–256
Mulkern RV, Schwartz RB (2003) In re: characterization of benign and metastatic vertebral compression fractures with quantitative diffusion MR imaging. Am J Neuroradiol 24(7):1489–1490; author reply 1490–1491
Nosas-Garcia S (2004) Dynamic contrast-enhanced MRI for assessing the disease activity of multiple myeloma: comparison with histological and clinical markers. Diss Med Fak University, Heidelberg
Nosas-Garcia S, Moehler T, Wasser K, Kiessling F, Bartl R, Zuna I, Hillengass J, Goldschmidt H, Kauczor HU, Delorme S (2005) Dynamic contrast-enhanced MRI for assessing the disease activity of multiple myeloma: a comparative study with histology and biochemical markers. J Magn Reson Imaging 22:154–162
Ooi GC, Chim JC, Au WY, Khong PL (2006) Radiologic manifestations of primary solitary extramedullary and multiple solitary plasmacytomas. Am J Roentgenol 186:821–827
Raya JG, Dietrich O, Reiser MF, Baur-Melnyk A (2006) Methods and applications of diffusion imaging of vertebral bone marrow. J Magn Reson Imaging 24:1207–1220
Vande Berg BC, Lecouvet FE, Michaux L, Labaisse M, Malghem J, Jamart J, Maldague BE, Ferrant A, Michaux JL (1996) Stage I multiple myeloma: value of MR imaging of the bone marrow in the determination of prognosis. Radiology 201:243–246
Walker R, Barlogie B, Haessler J, Tricot G, Anaissie E, Shaughnessy JD Jr, Epstein J, van Hemert R, Erdem E, Hoering A, Crowley J, Ferris E, Hollmig K, van Rhee F, Zangari M, Pineda-Roman M, Mohiuddin A, Yaccoby S, Sawyer J, Angtuaco EJ (2007) Magnetic resonance imaging in multiple myeloma: diagnostic and clinical implications. J Clin Oncol 25:1121–1128
Wasser K, Moehler T, Neben K, Nosas S, Heiss J, Goldschmidt H, Hillengass J, Düber C, Kauczor HU, Delorme S (2004) Dynamische MRT des Knochenmarks zum Monitoring des Multiplen Myeloms unter Thalidomid-Monotherapie oder Kombination mit CED-Chemotherapie. Fortschr Röntgenstr 176:1285–1295
Wasser K, Moehler T, Nosas-Garcia S, Rehm C, Bartl R, Goldschmidt H, Düber C, Kauczor HU, Delorme S (2005) Korrelation zwischen MRT und Histopathologie des Knochenmarks bei Patienten mit Multiplem Myelom. Fortschr Röntgenstr 177:1116–1122
Zamagni E, Nanni C, Patriarca F, Englaro E, Castellucci P, Geatti O, Tosi P, Tacchetti P, Cangini D, Perrone G, Ceccolini M, Brioli A, Buttignol S, Fanin R, Salizzoni E, Baccarani M, Fanti S, Cavo M (2007) A prospective comparison of 18 F-fluorodeoxyglucose positron emission tomography-computed tomography, magnetic resonance imaging and whole-body planar radiographs in the assessment of bone disease in newly diagnosed multiple myeloma. Haematologica 92:50–55
Zechmann C, Giesel FL, Hillengass J, Mehndiratta A, Delorme S, Moehler M (2007) Where is the primary tumor? Lancet 370:1800
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Delorme, S., Baur-Melnyk, A. (2011). Imaging in Multiple Myeloma. In: Moehler, T., Goldschmidt, H. (eds) Multiple Myeloma. Recent Results in Cancer Research, vol 183. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-85772-3_7
Download citation
DOI: https://doi.org/10.1007/978-3-540-85772-3_7
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-85771-6
Online ISBN: 978-3-540-85772-3
eBook Packages: MedicineMedicine (R0)