Abstract
Abuse of anabolic androgenic steroids (AAS) has been linked to a variety of different cardiovascular side effects. In case reports, acute myocardial infarction is the most common event presented, but other adverse cardiovascular effects such as left ventricular hypertrophy, reduced left ventricular function, arterial thrombosis, pulmonary embolism and several cases of sudden cardiac death have also been reported. However, to date there are no prospective, randomized, interventional studies on the long-term cardiovascular effects of abuse of AAS. In this review we have studied the relevant literature regarding several risk factors for cardiovascular disease where the effects of AAS have been scrutinized:
(1) Echocardiographic studies show that supraphysiologic doses of AAS lead to both morphologic and functional changes of the heart. These include a tendency to produce myocardial hypertrophy (Fig. 3), a possible increase of heart chamber diameters, unequivocal alterations of diastolic function and ventricular relaxation, and most likely a subclinically compromised left ventricular contractile function. (2) AAS induce a mild, but transient increase of blood pressure. However, the clinical significance of this effect remains modest. (3) Furthermore, AAS confer an enhanced pro-thrombotic state, most prominently through an activation of platelet aggregability. The concomitant effects on the humoral coagulation cascade are more complex and include activation of both pro-coagulatory and fibrinolytic pathways. (4) Users of AAS often demonstrate unfavorable measurements of vascular reactivity involving endothelial-dependent or endothelial-independent vasodilatation. A degree of reversibility seems to be consistent, though. (5) There is a comprehensive body of evidence documenting that AAS induce various alterations of lipid metabolism. The most prominent changes are concomitant elevations of LDL and decreases of HDL, effects that increase the risk of coronary artery disease. And finally, (6) the use of AAS appears to confer an increased risk of life-threatening arrhythmia leading to sudden death, although the underlying mechanisms are still far from being elucidated. Taken together, various lines of evidence involving a variety of pathophysiologic mechanisms suggest an increased risk for cardiovascular disease in users of anabolic androgenic steroids.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Anabolic androgenic steroids
- Cardiovascular side-effects
- Left ventricle hypertrophy
- Hypertension
- Relaxation abnormalities
- Vascular reactivity
- Coronary calcification
- Blood platelet function
- Lipid alterations
- Myocardial infarction
- Arrhythmia
- Sudden death
1 Introduction
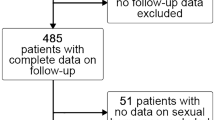
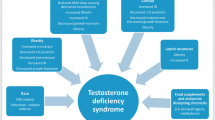
Over the last two decades there has been increased public focus on possible detrimental cardiac effects of the abuse of anabolic androgenic steroids (AAS). This awareness has, at least in part, been fuelled by an increasing number of case reports in the literature, many of them describing the occurrence of serious cardiovascular events more or less obviously linked to AAS abuse, some of them even with deadly outcome. The majority of described events have happened to bodybuilding AAS abusers, though not confined to competing athletes in this sport. Abuse of AAS has been associated with a range of different cardiovascular side effects (Fig. 1), starting with a case report of left ventricular hypertrophy in 1986 (McKillop et al. 1986) and one of a myocardial infarction in 1988 (McNutt et al. 1988), affecting a bodybuilder and a weightlifter, respectively, both of them very young. In 1988 there was also a report of a young bodybuilder with an ischemic cerebrovascular event and signs of cardiomyopathy (Mochizuki and Richter 1988). Several reports followed, and by 2008 there were around 40 altogether. Acute myocardial infarction is the most common event presented (Appleby et al. 1994; Capezzuto et al. 1989; Ferenchick and Adelman 1992; Fisher et al. 1996, Güneş et al. 2004; Halvorsen et al. 2004; Hourigan et al. 1998; Huie 1994; Kennedy 1993; Lyngberg 1991; Tischer et al. 2003; Wysoczanski et al. 2008), but there are also several reports of left ventricular hypertrophy (Figs. 2 and 3) (Campbell et al. 1993; Dickerman et al. 1995, 1997a, c; Hausmann et al. 1998; Kennedy and Lawrence 1993; Mark et al. 2005; McKillop et al. 1986; Stevens et al. 2002; Tischer et al. 2003), reduced left ventricle function (Clark and Schofield 2005; Ferrera et al. 1997; Mark et al. 2005; McCarthy et al. 2000), cerebrovascular incidents (Frankle et al. 1988; Laroche 1990; Mochizuki and Richter 1988; Santamarina et al. 2008), atrial fibrillation (Lau et al. 2007; Sullivan et al. 1999), arterial thrombosis (Alvarado et al. 2001; Falkenberg et al. 1997; Laroche 1990; McCarthy et al. 2000), pulmonary embolism (Gaede and Montine 1992; Liljeqvist et al. 2008), valve disease (Medras et al. 2005; Stevens et al. 2002), even one of a cardiac transplant (Menkis et al. 1991), and, sadly, several ones of sudden cardiac death (Di Paolo et al. 2007; Dickerman et al. 1995; Fineschi et al. 2001, 2007; Hausmann et al. 1998, Kennedy and Lawrence 1993; Luke et al. 1990). Interestingly, a repeated finding has been myocardial infarct without significant atherosclerotic coronary artery disease (Ferenchick and Adelman 1992; Fineschi et al. 2001; McNutt et al. 1988). On the other hand, severe premature coronary artery disease has also been observed (Fisher et al. 1996; Güneş et al. 2004; Huie 1994; Lyngberg 1991; Menkis et al. 1991; Ment and Ludman 2002; Mewis et al. 1996; Nieminen et al. 1996).
A lot of attention has been generated by a Swedish autopsy study (Thiblin et al. 2000) where 34 male users of AAS were medico-legally investigated. Twenty of them were either victims of homicide or had committed suicide, while the other deaths were classified as accidental or indeterminate. Chronic cardiac pathological changes were observed in 12 cases, specifically left ventricular hypertrophy (Fig. 2), cardiac fibrosis and coronary artery disease.
Concomitantly, a number of animal studies have been conducted over the years to shed light on the mechanisms possibly involved in the link between AAS abuse and cardiovascular pathology and/or mortality. The studies that looked at cardiovascular consequences of testosterone or their synthetic derivatives invariably show unfavourable effects. Myocardial hypertrophy (Kinson et al. 1991; Koenig et al. 1982; Marsh et al. 1998; Moore et al. 1978; Morano et al. 1990; Pesola 1988; Tagarakis et al. 2000; Takala et al. 1992), reduced ejection fraction (Rämö et al. 1987), increased myocardial stiffness (Trifunovic et al. 1995), left ventricular remodeling (Woodiwiss et al. 2000), depressed cardiac contractile function (Liang et al. 1993), impaired exercise-induced microvascular adaption (Tagarakis et al. 2000), reduced endothelial function (Cunha et al. 2005), destruction of mitochondria and myofibrils (Appell et al. 1983; Behrendt and Boffin 1977), disruption of morphological integrity of myocardial cells (Melchert et al. 1992) and apoptotic cell death in ventricular myocytes (Zaugg et al. 2001) are among the findings.
Despite this heightened awareness and an increasing knowledge base, to date there are no prospective, interventional studies on the long-term cardiovascular effects of abuse of AAS. In fact, due to ethical considerations, such a study will never be performed, and our present knowledge is largely based on case reports and observational studies. A small number of prospective studies have been published, but they are all done over a short period of time, and the doses of AAS used were relatively low, and do not reflect the real-life practices in the bodybuilding discipline.
As to the almost overwhelmingly high number of case reports and the severity of events described in them, one must – on the other hand – take into consideration the large population (Yesalis et al. 1993) using these drugs, and accept the fact that it still remains to be proven that the associations described are more than chance observations. Hence, from a solely scientific point of view, one must acknowledge the fact that there is only indirect evidence pointing towards harmful effects and possibly life-threatening consequences of AAS abuse, including higher cardiovascular morbidity or mortality in bodybuilders using AAS.
In this article we will review the relevant literature regarding several risk factors for cardiovascular disease where the effects of AAS have been scrutinized. In many aspects, the use of supraphysiologic doses of AAS has shown a probable or certain impact on those risk factors. In addition, and of particular interest, we will review those studies that utilized the investigational modality of echocardiography, in order to find abnormalities in the hearts of the individuals using AAS. In this respect a substantial amount of data has been collected, where both cardiac structure as well as function have been investigated.
Reviewing the entire scientific literature covering such a broad topic as the one described here, the authors cannot refrain from applying a certain selection process to the studies that will be highlighted. This should, however, not restrict our conclusions drawn at the end of each section, which we believe reflect the current state of knowledge in the field.
2 Echocardiographic Studies
Cardiac size, i.e. chamber dimensions and wall thickness, as well as cardiac function and hemodynamics, have been amenable to noninvasive assessment since the introduction of echocardiographic techniques in the 1960s. Applying these diagnostic modalities to the study of the effects of AAS on cardiovascular structure and function has been a cornerstone of the growing knowledge base on cardiovascular (CV) side effects of AAS. Hence a substantial part of the chapter on CV effects of AAS will focus on those findings derived from diagnostic ultrasound applications. The first studies on the effects of AAS on the parameters mentioned above were done in the latter half of the 1980s. As technology has developed in a rapid fashion, particularly in the last decade, the echocardiographic methods have increased considerably in sensitivity and specificity. This has given researchers the opportunity to evaluate the heart’s changes in different pathologic conditions and at various settings with a greatly improved precision compared to the early echocardiographic studies. While this statement is true for most if not all clinical and investigational applications of echocardiography, this is of course also the case regarding the appraisal of effects of AAS on cardiac structure and function.
Nonetheless, and perhaps somewhat surprisingly, the number of these studies (Table 1) is still rather few, given the long period of time since the first investigation was published in 1985 (Salke et al. 1985). The controversy concerning the side effects of AAS, especially within the bodybuilding milieu, has no doubt been partially fuelled by the conflicting results found in echocardiographic studies in the 1980s and 1990s. As is the case in evaluating all kinds of effects of AAS, the unavoidable study limitations pertinent to research in this particular population always make interpretation of findings debatable. Ethical concerns clearly make prospective, placebo-controlled double-blind studies with “real-life” dosages of steroids impossible to design and execute. In the studies that nonetheless have been carried out, the participants often use different types of steroids and different dosages, and the cycles of drug-use vary considerably. In addition, periods of abstinence are not alike, training routines differ, and there is also widespread use of so-called recreational drugs among users of AAS, which can influence the results. Another weakness of the studies is of course the limited number of study participants. Almost all of the studies are conducted on 15 or less AAS users. As previously mentioned, in the few truly randomized studies the drug dosages were low, and the study lengths short.
Nevertheless, and despite all these drawbacks, the echocardiographic studies viewed as a whole have given us an important and comprehensive body of evidence, and a solid basis for further investigations and discussion.
In general, most studies on the impact of AAS on echocardiographic parameters have been done in comparison to strength athletes without AAS use or to sedentary controls, or both. Interpretation of the studies has been made difficult by the everlasting controversy in the literature regarding whether resistance training in itself leads to structural changes in the myocardium, exceeding the degree of increase in body dimensions. Several studies have reported a slight concentric hypertrophy in strength athletes (Colan et al. 1985; D’Andrea et al. 2002; Dickerman et al. 1998; Pearson et al. 1986) not considered to use AAS. In most cases in these studies this was based on information provided by the subjects themselves, and could thus not be objectified or controlled. In contrast, other studies with careful control for AAS intake could not demonstrate increases in left ventricular mass above and beyond the proportions of the increases in body dimensions (De Piccoli et al. 1991; Urhausen and Kindermann 1999; Urhausen et al. 1989). In a study (Pelliccia et al. 1991) of 947 elite, highly trained subjects, only 1.7% had hypertrophy of the myocardium (wall thickness greater than or equal to 13 mm). These individuals were either rowers or canoeists, and one cyclist. In a follow-up study (Pelliccia et al. 1993), 100 highly trained athletes participating in weight and power lifting, wrestling, bobsledding and weight-throwing competitions were studied with echocardiography. None of them had wall thickness of the left ventricle which exceeded the generally accepted limits of normal (8–12 mm). On the other hand, the calculated left ventricle mass index was slightly, but significantly greater than in a control group of 26 sedentary healthy subjects. Taken together, much of the evidence is difficult to reconcile, and further scrutiny of the key studies is therefore mandatory in order to reach an understanding of the major issues in AAS research. The following studies have been chosen for their important contribution to the knowledge base.
In an observational, cross-sectional study, published in 1985, 15 bodybuilders abusing AAS were compared to 15 drug-free bodybuilders and the same number of inactive individuals who had never used AAS (Salke et al. 1985). The main finding of this study was a significant increase in the thickness of the left posterior wall and the interventricular septum of the left ventricle in both weight-training groups as compared to controls. There were no differences between the weight-training athletes with and without AAS when comparing the echocardiographic parameters of wall thickness and chamber size. There was, however, a larger degree of disproportionate septal hypertrophy in the AAS group, compared to the drug-free athletes, though not statistically significant. Cardiac dilatation was not observed, and there were no differences in fractional shortening, indicating no difference in ventricular contractility. Finally, there were no electrocardiographic differences between the three groups. The authors concluded that their study revealed no echocardiographic evidence that anabolic steroids potentiate the myocardial response to weight training.
Later, some studies have come to similar conclusions. On the other hand, the majority of these studies actually pinpointed differences between AAS-using and drug-free strength athletes quite clearly, yet never overwhelmingly.
One of those other negative studies (Zuliani et al. 1989) was a prospective study that also aimed to look at blood lipids. The authors could not find any echocardiographic differences between two groups of bodybuilders, a total of 15 persons, one using both AAS and growth hormone (GH), and the other being drug-free. The drug-using group had been free of steroids and GH for at least 8 weeks before entering the study. They self-administered GH and anabolic steroids of different kinds, apart from one individual who restricted himself to GH use only. After six weeks of medication, there were no significant changes in chamber dimensions, wall thickness, or fractional shortening between the two groups. Apart from the effect of six weeks of AAS use, this study does of course not tell us anything about long-term functional or structural myocardial effects, which, alas, is typical of all prospective studies performed in populations using anabolic steroids.
In a cross-sectional study from 1992, 12 weightlifters on AAS were compared to 11 who claimed never to have used these drugs (Thompson et al. 1992). To be admitted to the study, the drug users were required to have used the drugs for at least three cycles of 6–10 weeks within the past year. Long-term use was not a requirement. All subjects had urine testing done. Interestingly, the detection of steroids in urine did not always match the drug intake as reported by the subjects. Only 66% of 29 declared drugs were actually detected, whereas 58% of the 12 users provided urine samples containing an unreported drug. One of the subjects denied steroid use, but drug testing still revealed traces of nandrolone. This illustrates one of many methodological problems in doing studies on this kind of population. As to the echocardiographic findings, no differences between the two groups were found regarding chamber size, wall thickness or myocardial mass, neither were there any differences in systolic and diastolic function, assessed by ejection fraction, rate of wall thickening and transmitral flow, respectively.
In another mainly negative study (Palatini et al. 1996), the authors did not find any significant echocardiographic differences between ten bodybuilders on AAS and 14 who had not taken drugs. The study on the drug users was done both at the end of a period of AAS intake, and at the end of a period of withdrawal. Only interventricular septal thickness was slightly greater in AAS users than nonusers, but the difference did not attain the level of statistical significance. Left ventricular mass indexed for height or body surface area was only marginally increased in AAS users. No differences were found between the AAS users at the end of a drug cycle (mean 8.4 weeks) and at the end of a withdrawal phase (mean 11 weeks). The E/A ratio (ratio of passive to active filling of the left ventricle, from the left atrium) assessed by Doppler measurement of left ventricle filling rate was a little higher in nonusers than in users, but did not reach statistical significance.
In a small study (Dickerman et al. 1998) published in 1998, four elite resistance-trained athletes using steroids were found to have significant left ventricular hypertrophy; one of them had a left ventricular wall thickness of 16 mm, which at that time was the largest wall thickness ever reported in a resistance-trained athlete. The investigators went on to look retrospectively at the echocardiographic data from their previous study of 16 bodybuilders (Dickerman et al. 1997 c), eight of them on AAS, and eight drug-free. In the latter group, 43% had left ventricle wall thickness beyond the normal range (here defined as 11 mm), whereas all eight AAS users had increased wall thickness. In addition, one of the drug-free subjects and three in the AAS group were beyond the critical value of 13 mm, as defined in Pelliccia’s large survey from 1991. None of the subjects demonstrated diastolic dysfunction, detected by mitral inflow velocity patterns. Based on these findings, the authors dispute previous publications stating that left ventricular wall thickness does not occur in resistance-trained athletes without AAS use, and that the short bursts of arterial hypertension that occur with weightlifting cannot stimulate left ventricular wall thickening. They conclude that wall thickness equal to or above 13 mm can be found in athletes both with and without AAS use. They believe the drugs may increase left ventricular wall thicknesses indirectly through their ability to increase strength, thus allowing a greater overall pressure response with weightlifting.
In a thorough and often cited study from 2003, 25 strength athletes using AAS were compared to 23 drug-free strength athletes (Hartgens et al. 2003). The majority were bodybuilders, a few were power lifters. The investigation was designed and carried out as two separate studies. In Study 1, 17 drug users, who intended to start self-administration, were compared to 15 nonusers. The users had all taken AAS previously, with an average of 4.6 years use before entering the study. They were expected to be free of AAS use for at least 3 months. The subjects were examined at the start of the study, and after eight weeks of self-administration of AAS. A few (seven) were also examined after 12–16 weeks of AAS intake. In Study 2, 16 well-trained recreational bodybuilders were recruited. They were randomized to i.m. injections of either nandrolone decanoate 200 mg/week or placebo. In both groups two subjects had previous experience with AAS, while the remainders had never used AAS. The injections were given in a double-blind fashion. Echocardiographic measurements were performed at baseline and after an eight-week study period. In Study 1, no significant alterations could be detected in the echocardiographic assessment of heart morphology and function after eight weeks. In addition, there were no differences between short-term (eight weeks) and long-term use (12–16 weeks). In Study 2, eight weeks of nandrolone decanoate did not induce significant alterations in echocardiographic measurements of heart morphology nor in parameters reflecting systolic and diastolic function. There were, however, enlargements of the left ventricle and left ventricular wall thickness in a minority of the users in both groups, but considered to be within the limits of physical adaptation to vigorous and demanding training regimens. The authors concluded that steroid regimens of a single- and polydrug regimen as described in this study, as a short-term AAS administration, did not lead to detectable echocardiographic alterations. However, since detrimental cardiac effects of short-term AAS treatment with supraphysiologic doses have been described in animal studies, the authors of this study believed that echocardiographic evaluation may provide incomplete assessment of the actual cardiac condition in AAS users since the method is not sensitive enough to detect alterations at the cellular level. Therefore they stated that no conclusions could be drawn regarding the cardiotoxic effects of long-term AAS abuse.
Later studies have to a certain extent proved the authors right. The introduction of tissue Doppler velocity imaging has given researchers an echocardiographic modality which is more sensitive than traditional echocardiography and standard Doppler measurement of blood flow. The most recent studies have utilized this method and have been able to detect pathological changes not identifiable with conventional echocardiography. We will look closer into these studies later on in this chapter.
As previously mentioned, there are very few prospective, randomized studies looking at cardiac structure and function. Recently, Chung et al. conducted a double-blind, placebo-controlled study on 30 healthy young men, randomized into three groups of ten subjects (Chung et al. 2007). They received four weekly intramuscular injections of 200 mg testosterone esters (Sustanon), 200 mg nandrolone decanoate (Deca-Durabolin), or placebo. None of the participants were athletes. In this study the subjects went through a complete echocardiographic assessment, including the more sensitive method of myocardial tissue velocity measurement with the derived methods of peak systolic strain and strain rates. Bioimpedance measurements of cardiac output and systemic vascular resistance were also performed. Only four weeks of treatment and follow-up was probably the main reason why the study came out completely negative regarding cardiac function, though minor changes within the normal range were observed solely within the testosterone group, among the most interesting being a minor reduction of left ventricle diastolic septal velocity and a slight increase in left ventricle filling pressure.
As previously indicated, several studies, even the older ones, have demonstrated significant increases in left ventricular wall thickness and slight impairment of diastolic function among strength athletes using AAS. In a study by Pearson et al. (1986), 16 weightlifters were examined and compared to ten age-matched control subjects. There was no difference in wall thickness, when corrected for body surface area. Weightlifters had significantly higher LV mass and LV mass index than controls, but there was no difference in Doppler indexes of diastolic filling, indicating that the concentric hypertrophy observed was consistent with a physiologic response. However, five of the weightlifters were AAS users, and in this subset of the group, the Doppler indexes of diastolic filling were significantly reduced. Pathological changes in diastolic filling were also demonstrated in a study by Urhausen et al. (1989). In this cross-sectional study, 14 bodybuilders using AAS were compared to seven who did not use these drugs. The isovolumic relaxation time (the time from aortic valve closure to mitral valve opening) was prolonged in the AAS group, indicating a minor impairment of diastolic function. In addition, the AAS users had lower left ventricle diameter, in spite of having almost identical total heart volume and left ventricle mass as the nonusers. The ratio of left ventricle mass to diameter was increased in the user group.
In another study, by De Piccoli et al. (1991), quite similar changes were demonstrated. In this prospective study, echocardiographic parameters were measured in 14 bodybuilders after eight weeks of self-administration of AAS. The findings were compared to 14 bodybuilders who had never taken steroids, and to a group of 14 sedentary individuals. In addition, the AAS users were examined following nine weeks of drug suspension. Once again, a study of very modest size revealed structural myocardial changes in the user group, although not impressive. Increased wall thickness (ventricular septum) and an increase in left ventricular mass were apparent in the steroid-user group. In the same group there was also a significant increase in the left ventricle end systolic diameter and end diastolic volume. There were, as in previous studies, no changes in systolic function (as judged by ejection fraction). In accordance with Pearson’s and Urhausen’s findings, there were signs of diastolic impairment in the AAS group, shown as significantly longer isovolumic relaxation time. There were no significant differences in blood pressures in the three groups, which indicate that mechanisms other than hypertension lie behind the aforementioned changes, for example a direct effect of the steroids. Interestingly, at the nine-week post-steroid examination, the changes were still there, which urged the investigators to presume that such a period is not enough to restore the morphologic and functional characteristics of the heart.
Looking at 11 weight-training males eight weeks after a period of self-administration of AAS, and again at the top of their next cycle, and comparing them to 13 weight-training males who had never used AAS, Sachtleben et al. (1993) found significant morphological changes, but no signs of systolic impairment in either group. In this longitudinal study the users on cycle had larger ventricular mass and increased interventricular septal thickness as compared to measurements off cycle. These findings were also significant compared to the control group, in addition to the left posterior wall thickness being increased. Another interesting finding was a significantly lower maximum oxygen consumption (VO2 max) in the two user groups compared to the control group. VO2 max was assessed using a Quinton treadmill, where the subjects walked until a defined maximum speed was reached, depending upon heart rate response. Then the grade was increased by 2% every minute until exhaustion. Expired air was collected and gas analyzes conducted, enabling calculation of VO2 max. The finding of lower VO2 max was in spite of the users having reported more frequent aerobic training sessions, though they were shorter in duration. The results in this study indicate that the myocardium, during resistance training, is thickened by approximately six weeks of AAS use (peak cycles occurring at 5–9 weeks).
In another cross-sectional study (Yeater et al. 1996) comparing 24 highly trained resistance athletes, among them a group of eight AAS users, to a group of recreational lifters and a group of eight cross-country runners, the VO2 max did not differ between the groups of resistance athletes, as was the case in the study by Sachtleben et al. The cross-country runners had, as would be expected, significantly higher VO2 max than the other groups. As for the echocardiographic assessments, the AAS users had significantly greater left ventricular mass index than the recreational lifters, but not compared to the highly trained lifters without steroids or the runners. Wall thickness was larger in the steroid group, but did not reach statistical significance. Diastolic functions, assessed by transmitral filling indices, were not compromised.
The finding of increased left ventricular mass and increased wall thicknesses in AAS users has been confirmed in other studies as well, among them studies by Di Bello et al. and Karila et al. In the former (Di Bello et al. 1999), ten male weightlifters using AAS were compared to ten without, and to ten healthy sedentary controls. In addition to conventional echocardiography, the participants were examined with ultrasonic videodensitometry, a method able to detect alterations in ultrasonic textural myocardial parameters. The steroid users had a significantly lower cyclic variation index for the septum and posterior wall compared to both nonusers and healthy subjects. The authors’ interpretation of this finding was that the changes could probably represent the onset of a specific cardiomyopathy. Despite an increase in left ventricular mass among the nonusers, they showed normal cyclic variation, indicating a normal ultrasonic myocardial texture. In Karila et al. (2003)’s cross-sectional study of 20 AAS users, there was a significant association between left ventricular mass and the mean daily AAS dose. There was no correlation with body dimensions, except in the control group of 15 sedentary men. Of the 20 users, four were also injecting growth hormone, and it appeared that the combination treatment resulted in a larger degree of hypertrophy than in the AAS-only group. There was no difference in diastolic filling indices.
As to the reversibility of adverse cardiovascular effects after chronic abuse of AAS, not many studies have addressed this question. In Palatini’s study the subjects were examined 11 weeks (mean) after withdrawal without finding any changes (Palatini et al. 1996). But the slight changes in myocardial structure noted after a cycle of steroids of eight weeks did not reach significance anyway. In Urhausen’s study from 2004 reversibility was addressed specifically (Urhausen et al. 2004). Thirty-two bodybuilders or powerlifters were examined, among them 17 currently on AAS and 15 who had not been taking the drugs for at least a year (mean 43 months). They were compared to 15 AAS-free weightlifters from the national team. Both users and ex-users had higher left ventricular mass related to fat-free body mass than the AAS-free weightlifters. Wall thicknesses were also smaller in the group of weightlifters, but there was no difference between the users and ex-users. Left ventricular wall thickness was correlated with a point score estimating AAS abuse in users. As almost all other studies have concluded, no significant changes in systolic function were noted. However, the maximum late transmitral Doppler flow velocity was higher in users and ex-users than in weightlifters, indicating a slight alteration of diastolic function. The authors concluded that several years after the discontinuation of AAS abuse, strength athletes still show a slight concentric left ventricular hypertrophy in comparison with AAS-free strength athletes.
Urhausen and Kindermans group later published another study (Krieg et al. 2007) where the objective was to clarify whether AAS abuse also induced alterations in left ventricle function, as opposed to mere anatomical changes. Fourteen male bodybuilders with a substantial intake of AAS were examined with echocardiography and cardiac tissue Doppler imaging. They were compared to 11 steroid-free strength athletes and to 15 sedentary control subjects. As in their previous study, there was an increase of left ventricular muscle mass index in the user group. There were no differences in transmitral filling indices using Doppler measurements of blood flow. However, using tissue Doppler imaging in the mitral annulus, there were significantly reduced values in the user group compared to the other groups. These findings are considered to be a clear sign of compromised diastolic function in the AAS group. There were no differences in systolic parameters. Tissue Doppler imaging, as alluded to above, is known to be more sensitive to changes in diastolic function than the traditional transmitral flow measurements, most probably explaining why several previous studies have come out negative in this respect.
In a study from 2006, Nottin et al. (2006) sought to evaluate the effects of regular AAS administration in bodybuilders using pulsed tissue Doppler imaging (TDI) to evaluate left ventricular relaxation properties. They examined 15 bodybuilders, six of whom were currently on AAS, and nine of whom had never taken the drugs. The steroid users were required to have used AAS for the past two years. All the strength-trained athletes had been training for 5–12 h weekly for 10 or more years. Sixteen age-matched sedentary males served as controls. Although there were no differences in wall thicknesses between the groups, the drug-using bodybuilders exhibited larger end-diastolic diameters, volumes and masses than their drug-free counterparts. Most strikingly, though, were the changes noted in pulsed TDI measurements. The AAS users had smaller peak Em (peak passive tissue velocity at the level of the mitral annulus) and smaller peak Em/Am (Am being the active contribution of filling) than both of the other groups. This indicates that the AAS users exhibited depressed left ventricular diastolic function, characterized by a decrease in the contribution of left ventricle passive filling to left ventricle filling. There were also alterations of transmitral flow velocity properties, indicating reduced diastolic function. This has also been noted in several previous studies, although not uniformly. Apart from being a more sensitive method than flow velocity measurements, pulsed TDI also has the advantage of being relatively preload-independent, and is generally accepted as being a good index of left ventricular filling properties. In accordance with previous studies, no changes of systolic function were noted in this study either. Using pulsed TDI, there were no differences in the peak E/Em, which indicates normal left ventricular filling pressures as well. As no significant hypertrophy was detected among the AAS users, these findings indicate that an alteration of intrinsic left ventricle relaxation per se is responsible for the depressed diastolic function. This study was also the first to assess diastolic function with TDI in this population.
The only study so far which has utilized TDI and the derived method of strain rate imaging to evaluate cardiac function in strength athletes with chronic AAS abuse was published by D’Andrea et al. (2007). In this study the authors included 20 bodybuilders who had taken AAS for at least five years, 25 steroid-free bodybuilders and the same number of age-matched healthy sedentary controls (D’Andrea et al. 2007). Both users and nonusers showed increased wall thickness and stroke volume as compared to controls, whereas left ventricular ejection fraction, end-diastolic diameter and transmitral Doppler indexes were comparable between the three groups. TDI showed significantly lower Em/Am ratios in users at the level of both the basal interventricular septum and the left ventricular lateral wall, which is in accordance with the findings of Nottin et al. In addition, and perhaps most notably, the users had a significant reduction in peak systolic strain and strain rate in the middle interventricular septal wall as well as in the left ventricular lateral free wall. The strain rate imaging technique, assessing longitudinal deformation within the myocardium, gives quantitative information of local myocardial function, and it is not influenced by global cardiac displacement and any tethering effects. As such, it is superior to other techniques assessing regional velocity profiles. The findings in this study point to an early impairment of left ventricular myocardial contractile function in AAS users, and hence constitute a watershed point with regard to picking up such subtle systolic impairments, although Di Bello and co-workers (Di Bello et al. 1999) actually also had claimed to find the same functional changes by a completely different technique, the ultrasonic myocardial backscatter/videodensitometric measurement. The study by D’Andrea et al. further revealed that the number of weeks of AAS use per year and the weekly dosage of AAS were independent determinants of impaired strain rate. Adding to the negative cardiac effects of AAS was the fact that impaired left ventricular strain in AAS users was associated with a reduced performance during physical effort, as measured by bicycle ergometric testing.
And finally, adding yet another piece to the somewhat blurred, yet comprehensive and nonetheless increasingly recognizable, puzzle of AAS and the heart, Kasikcioglu et al. very recently published another study addressing diastolic function. Twelve bodybuilders on AAS were compared to 14 nonusers, using conventional echocardiography and TDI. Again the latter method revealed impaired relaxation properties, and in this study not only in the left ventricle, but also in the right, which had not been investigated by TDI before (Kasikcioglu et al. 2008).
2.1 Summary
In conclusion, the echocardiographic studies on AAS using subjects viewed as a whole have produced conflicting results over time, partly due to changes in – and improvement of – investigational modalities, partly due to insufficient and in some cases frankly debatable study designs.
Yet it is safe to state that AAS use does lead to both morphologic and functional changes in the heart. These changes encompass (a) a tendency to produce a myocardial, predominantly septal hypertrophy, partly as a consequence of resistance training and AAS, (b) a possible increase of heart chamber diameters, although not as manifest as seen in endurance athletes, (c) unequivocal alterations of diastolic function and ventricular relaxation, particularly as assessed by modern tools, and (d) a subclinically compromised left ventricular contractile function, detectable only by the most sensitive modern investigational modalities.
As far as prognosis is concerned, the clinical significance of these AAS-induced changes remains to be established, even though many of the phenomenological changes (such as impaired relaxation of the left ventricle) are indicators of diseased hearts prone to deterioration over time.
3 Hypertension
The frequently reported findings of severe myocardial hypertrophy in case reports of abusers of anabolic androgenic steroids (AAS), have led to the suspicion that the drugs may induce arterial hypertension, which could explain these structural changes in the heart. In population studies, arterial hypertension is the most prevalent reason for myocardial hypertrophy (Mancia et al. 2007). Studies of rats and mice have with some frequency reported hypertensive effects of AAS, the first one as early as in 1940 (Grollman et al. 1940). Several possible mechanisms have been suggested, one of them being through an elevation of 11-deoxycorticosterone (DOC), which is caused by testosterone reducing 11β-hydroxylase activity, thus reducing the conversion of DOC to cortisol (Brownie et al. 1978; Gallant et al. 1992). Another contributing mechanism could be by enhanced reactivity of vessels to norepinephrine, which in animal studies has been shown following the administration of testosterone (Ammar et al. 2004; Baker et al. 1978; Bhargava et al. 1967; Greenberg et al. 1974). It has also been reported that testosterone raises plasma renin activity, and that expression of renin mRNA in the adrenal gland, kidney and brain is androgen-dependent (Katz and Roper 1977; Wagner et al. 1990). Aldosterone production is stimulated by testosterone hemisuccinate, according to a study performed in bovine adrenal tissue, which could be another possible contributing mechanism leading to hypertension (Carroll and Goodfriend 1984). In a recent study on rats, the administration of stanozolol for eight weeks caused a significant increase in arterial blood pressure, possibly through increases in cardiac output and peripheral resistance (Beutel et al. 2005).
References to hypertensive effects during self-administration of AAS are common, and indeed Volume II of The Underground Steroid Handbook notes hypertension to be a transient effect of AAS that resolves with completion of the cycle and leaves no residual effects (Duchaine 1989). On the other hand, the clinical studies addressing possible hypertensive effects among strength athletes using AAS have not been able to convincingly confirm these in humans. A few studies have, however, registered a slight elevation of blood pressure compared to strength athletes without AAS or healthy controls, but the main body of evidence tends to lean in the other direction. Amongst the human studies addressing this question, almost all have done so as part of a more comprehensive, broader study looking at other aspects of AAS abuse, for instance the effects on lipids, or as part of an echocardiographic study.
Two human studies performed in the seventies looked at several physiologic and hemodynamic effects of methandienone, among them blood pressure response. In the study by Freed et al. (1975), 13 male weightlifters took either 10 or 25 mg daily, or placebo, for six weeks in a double-blind crossover trial. In the steroid group the systolic blood pressure increased slightly, but significantly, while the diastolic blood pressure remained unchanged. This was of course a small study and there were also withdrawals. In Holma’s study 16 well trained athletes participated (Holma 1977). They were tested before and after two months of a daily oral dose of 15 mg methandienone. Several hemodynamic parameters were measured. Even though the total blood volume increased by 15%, there were no significant changes in resting values of cardiac index, peripheral resistance or mean arterial pressure during methandienone treatment.
In a later cross-sectional study (Lenders et al. 1988), 45 amateur bodybuilders had their serum lipoproteins, blood pressure and liver function examined, following self-administration of different types of AAS over a mean period of 1.7 years (range 0.2–13.0). Twenty of them were studied at the end of a course, 42 after discontinuation of AAS for a mean of five months and 16 after a discontinuation for at least two months and at the end of a nine-week course of AAS. A group of 13 AAS-free bodybuilders served as a control group. All steroid groups showed a slight, but significant, increase of systolic blood pressure, in the range of 3–7 mmHg. This was also the case in the discontinuation group. There were no changes in diastolic blood pressure. In another study of 18 competitive bodybuilders self-administrating AAS, though mainly focusing on the lipid effects, there were no differences in systolic or diastolic blood pressure before and after a 16-week course of AAS, or when compared to a group of non-AAS-using bodybuilders (Kleiner et al. 1989).
There is very little data on blood pressure response to exercise in AAS users. This question was addressed in a study by Riebe et al. (1992) where both rest and exercise blood pressure were measured in nine weightlifters using AAS, and compared to ten individuals not using the drugs, and to ten sedentary controls. The subjects performed a treadmill test until exhaustion as well as a submaximal weightlifting exercise. The AAS users had significantly higher resting blood pressure, though not hypertensive values. They also had higher exercise maximal systolic pressure, exercise diastolic pressure and mean arterial pressure. But there was no significant difference between the groups for the change in systolic, diastolic or mean arterial pressure from rest to maximal exercise. When adjusted for body weight, there were no differences between the groups for either rest or exercise blood pressure values. However, statistical limitations in the study urge the authors to doubt that this alone can explain the differences. When adjusted for biceps size, the higher diastolic blood pressure during exercise in the AAS group still remained significant, which the authors believe implies a possible signal of subsequent hypertension in this group.
An often cited study in this context is the one by Kuipers and Hartgens’ group, from Maastricht. In this study 26 male bodybuilders participated (Kuipers et al. 1991). They all had at least three years experience of strength training. They were divided into three groups; one group (SAD) self-administered anabolic steroids for 8–10 weeks, the second group received i.m. injections of 100 mg nandrolone decanoate weekly or placebo over a period of eight weeks, in a double-blind fashion. The third group received the same treatment, but as a double-blind cross-over study, with weekly injections for two periods of eight weeks, separated by a 12-week washout period. Body composition, lipid profile, liver function and blood pressure were studied, the latter noninvasively. In the SAD group the systolic blood pressure increased from 122.3 to 134.0 mmHg (all mean), but this was not a significant difference. However, the diastolic values increased significantly, from 73.6 to 86.0 mmHg. Six weeks after discontinuation, the diastolic blood pressures had returned to pre-treatment values. In the other two groups there were no differences found in either systolic or diastolic blood pressures. As could be expected, the steroid dosages in the SAD group were considerably higher than in the other two groups, and it is therefore suggested that the effect on blood pressure is dose-dependent. The authors believe that a possible explanation for the increase in blood pressure is through an increase in blood volume, a mechanism which has been suspected by other investigators as well (Riebe et al. 1992; Wilson 1988).
In another study (Hartgens et al. 1996) a few years later, the same group investigated several of the same parameters after at least three months of drug withdrawal in 16 long-term AAS users compared to 12 nonusers, all male bodybuilders. The drug users had taken i.m. and oral steroids for an average of 3.2 (0.7–6.0) years prior to the withdrawal period. The average systolic and diastolic blood pressures were normal and there was no difference between the two groups. Based on these findings, the authors suggested that blood pressure is within the normal range after an AAS-free period of three months, independent of the number of AAS courses used.
The echocardiographic studies on AAS abuse have been discussed previously. However, most investigators also registered blood pressure in all participants and these results need further mention. Beginning with De Piccoli’s study, in which 14 bodybuilders on steroids were compared to the same number of drug-free bodybuilders and sedentary controls, there was no difference in systolic or diastolic blood pressure (De Piccoli et al. 1991). The drug users were also examined after a period of drug withdrawal (mean nine weeks) without any changes in blood pressure being noted. Even though the blood pressures were normal, the investigators interestingly still found signs of impaired diastolic function and an increase in left ventricular mass, and one could therefore assume that these changes were not secondary to hypertensive blood pressures, but rather a direct effect of the drugs taken. In another echocardiographic study by Thompson et al. (1992), 12 weightlifters using AAS were compared to 11 who had not used these drugs. For admission to the study, the users were required to have taken the drugs for at least three cycles within the past year, and the mean length of drug use was 3.3 years. Again, there were no differences in systolic or diastolic blood pressure between the groups.
In the study by Yeater et al. (1996), weightlifters with or without AAS were compared to runners; echocardiographic and other cardiorespiratory variables as well as lipids and body composition were measured. There was no difference in resting blood pressure or blood pressure at the end of a treadmill test between the weightlifter groups. The runners had lower diastolic pressure during recovery from exercise, though all groups had normal values. It should be noted that the subjects were young, with an average age of 21 (all groups), and the steroid users had taken the drugs for a minimum of six months.
There are almost no data on 24-h blood pressure monitoring in the AAS population. However, in one study by Palatini et al. (1996) the participants underwent a 24-h noninvasive blood pressure measurement, though this study primarily was another small echocardiographic study. Ten bodybuilders with an average age of 28 years, who had self-administerered AAS for an average length of five years (range 2–10 years) were compared to 14 nonusing bodybuilders. The steroid users were examined at the end of a treatment period and after a withdrawal period of 8–16 weeks (mean 11 weeks). There was no difference in resting blood pressure between the groups, and systolic and diastolic blood pressures were within normal limits. Average 24-h, daytime and night-time systolic and diastolic blood pressures did not differ in the three groups of AAS users during treatment, users after withdrawal or control subjects. However, the difference between daytime and night-time blood pressure was greater in control subjects than in AAS users, both at the end of the treatment cycle and after the period of withdrawal. Another interesting finding in this study was that the extent of the blood pressure decrease at night was inversely related to the interventricular septal thickness and the concentric remodeling of the left ventricle in the steroid group. This study suggests that weightlifting per se does not alter the 24-h blood pressure rhythm, but the addition of AAS does. An abnormal 24-h rhythm of blood pressure has been observed in many subjects with secondary hypertension and in some patients with essential hypertension, and target organ damage appears to be more common in nondippers (Persons in whom there is an absence of the normal nocturnal fall in blood pressure) (Boggia et al. 2007; O’Brien et al. 1988; Palatini et al. 1992; Verdecchia 2000). The data from this study must nonetheless be treated with caution, as this was a small study, and to our knowledge altered 24-h blood pressure rhythm in AAS users has not been confirmed in any later studies. Another reservation is that the main reason for the difference mentioned seems to be that the nonusers had a slightly higher systolic pressure in daytime, and therefore a higher daytime pulse pressure.
In the echocardiographic study by Karila et al. (2003), there were no differences in blood pressure values between the control group and a group of 20 strength athletes, mainly bodybuilders, who were long-term users of AAS. Four of the steroid users had also taken growth hormone (GH) and notably their average diastolic blood pressure was higher (89 mmHg vs. 77 mmHg in the control group and 76 mmHg in the AAS group without GH) than the two other groups, but statistic significance was not reached, possibly due to the low subject numbers.
In the prospective echocardiographic study by Hartgens et al. (2003), where two groups of AAS users were compared to nonusing strength athletes, there were no changes in systolic or diastolic blood pressure. One AAS group self-administered the drugs for 8–16 weeks, and the other received 200 mg of nandrolone decanoate once a week for eight weeks in a double-blind fashion. The authors concluded that one of the main findings in their study was that short-term administration of AAS did not affect blood pressure.
In a cross-sectional study addressing reversibility of cardiac effects of AAS abuse, Urhausen et al. (2004) examined their subjects with echocardiography and cycle ergometry including measurements of blood pressure at rest and during exercise. Fifteen former AAS users (at least 12 months withdrawal, mean 43 months) were compared to 17 current users and 15 AAS free weightlifters. Systolic blood pressure was higher in users, measuring an average of 140 mmHg at rest vs. 130 mmHg for ex-users and 125 mmHg for the nonusers. This difference persisted as a trend for exercising blood pressure. There was no difference in diastolic blood pressure. The authors suggested that the increases in blood pressure with AAS are rather small and transient.
In a double-blind, randomized, placebo-controlled study by Chung et al. (2007) the effects of weekly injections of testosterone, nandrolone or placebo on cardiovascular parameters were investigated, using state-of-the-art echocardiographic methods. There were ten individuals in each group, all of them healthy young men, but none were involved in strength athletics. They received the treatment for four weeks only. There was no effect on systolic, diastolic or mean blood pressure, or on systemic vascular resistance, assessed by thoracic electrical bioimpedance.
Blood pressure as well as rate pressure product (RPP) response to AAS was investigated by Grace et al. (2003) in 16 users compared to 16 nonusers, all subjects being amateur bodybuilders in their mid-twenties. They all had a minimum of three years of weight-training experience. The drug users had taken various AAS for a mean length of 4.3 years in rather large dosages. The subjects’ blood pressures were measured noninvasively and the rate pressure product was calculated as (HR × SBP/100). The recordings were obtained before a steroid cycle, at the end of the cycle and 6–8 weeks post-cycle. The control group was assessed within the same time intervals. Significant increases were found for both diastolic (79–87 mmHg) and mean arterial blood pressure in the AAS group, but not for systolic blood pressure. Even when adjusted for biceps size, diastolic blood pressure was still significantly greater in this group. There was also a significant increase in resting heart rate in the AAS group, with a subsequent increase in RPP. All mentioned parameters returned to pre-cycle baseline levels within 6–8 weeks following drug cessation. The data from this study indicate that AAS acutely influences blood pressure, especially diastolic blood pressure, though it does not seem that the drugs cause hypertension, and the rise in blood pressure appears to be transient. However, the authors suggest that these findings provide a contra-indication to AAS use, especially in borderline hypertensives.
3.1 Summary
Hypertension as a risk factor for cardiovascular disease is well established (Lewington et al. 2002). Although hypertensive effects of supraphysiologic doses of AAS are often referred to in the bodybuilding community and among self-administering AAS users, the scientific support for this view is scarce. Animal studies have to some extent shown hypertensive effects of AAS, and have given rise to a variety of theories as to the underlying mechanisms. The human data, however, are less convincing, and the overall evidence base leans to the opposite. One must keep in mind that the studies are small and most of them are cross-sectional in design. Some of the studies show a slight increase in systolic blood pressure, some show a slight increase in diastolic blood pressure and many do not show any significant pressure changes at all. The studies assessing reversibility demonstrate that when a pressure increase has been found, it is transient and that full normalization is achieved only a few months after cessation of the drugs.
Hence, taken together, it is likely that the administration of supraphysiologic doses of AAS induces a mild, but transient increase of blood pressure; however the clinical significance of this effect remains modest.
4 Vascular Reactivity and Vascular Function
The frequently reported observations of adverse cardiovascular events among abusers of anabolic androgenic steroids (AAS) have stimulated an interest in possible underlying mechanisms beyond those attributed to established atherosclerosis. It remains a notable fact that coronary angiography and/or autopsies of deceased users of AAS have often shown patent coronary arteries, in spite of the subjects having suffered a myocardial infarction or sudden death. One proposed explanation is steroid-induced vasospasm, perhaps superimposed on or triggered by pro-atherogenic state. It has been shown that androgens can promote monocyte adhesion to endothelial cells (McCrohon et al. 1999) and macrophage lipid loading (McCrohon et al. 2000). Androgens have also been associated with impaired arterial reactivity in females taking high-dose androgenic steroids (McCredie et al. 1998), and, conversely, endothelial function is enhanced in androgen-deprived older men (Herman et al. 1997, Sader et al. 2003; Zitzmann et al. 2002). Endothelial dysfunction has been demonstrated to be an early finding in both experimental and clinical studies of atherogenesis, preceding plaque formation and the occurrence of clinical events (Celermajer et al. 1992; Ross 1993).
There are only a few studies addressing vasoreactivity in the population of AAS abusers. Sader et al. (2001) examined 20 male bodybuilders, ten of them using AAS and ten who denied ever having used the drugs, and compared them to a group of ten age-matched non-bodybuilding controls. The drug users’ mean age was 37 years and the mean duration of steroid abuse was 6.6 years. The investigators measured carotid intima-media thickness (IMT) and arterial reactivity using high-resolution ultrasound. For the latter they studied the right brachial and radial artery, measuring the artery diameter at rest, during reactive hyperemia (leading to flow-mediated dilatation, FMD) and after administration of sublingual nitroglycerine (GTN), the two measurements enabling assessment of endothelial-dependent and endothelial-independent vasodilatation. The AAS users had slightly, but not significantly larger vessels than the bodybuilder controls. Despite this, FMD responses were similar in both groups of bodybuilders. The responses tended to be lower than in the non-bodybuilding controls, but not significantly so. The GTN responses, assessing endothelial-independent vasodilatation, were also not significantly different between the bodybuilder groups, but significantly lower compared to the control group of non-bodybuilders. Carotid IMT measurements were similar in both bodybuilding groups, but significantly higher than in the control group. The authors suggest that their findings might be explained by a defect in smooth muscle capacity, secondary to increased water retention and/or increased vascular muscle mass impairing smooth muscle dilator responses. But a main point still seems to be that AAS does not further impair these responses compared to the bodybuilder group not using the drugs.
In another study of flow-mediated dilatation, Ebenbichler et al. (2001 b) examined 20 male bodybuilders in different phases of their training and AAS cycle. FMD was determined in the same way as in the previously mentioned study. The subjects were examined in an eight-week training phase without steroids, then in a “build-up” phase, where AAS was taken for 8–12 weeks, and then after up to eight weeks following cessation of the drugs, in the “competition phase”. Six athletes not using AAS served as control group. The percent change in brachial artery diameter after reactive hyperemia was diminished in bodybuilders in all phases and the reduction was most pronounced in the competition phase, the differences compared to the control group being significant. Nonendothelial vasodilatation, measured as response to sublingual GTN, was also reduced, though not significantly. Two mechanisms are proposed as explanation of these findings. One could be by endothelial dysfunction through the low HDL-cholesterol found in the steroid user group, the other by a direct effect of AAS on vascular function, which the authors speculate is the most likely mechanism.
In a recent study by Lane et al. (2006), vascular reactivity was assessed by using pulse wave analysis with GTN and salbutamol, to determine endothelial-independent and endothelial-dependent vasodilatation, respectively. The pulse wave analysis noninvasively assessed arterial stiffness and central aortic pressure. Twenty-eight bodybuilders took part in the study; ten who were current users of AAS were compared to eight regular users who had abstained from using substances for the previous three-month period, and to ten who had denied any current or previous use of AAS. Ten healthy sedentary individuals served as control group. Subjects in all four groups had comparable brachial artery blood pressures and resting pulse rates. The administration of salbutamol altered the central arterial waveform and reduced the augmentation index (AIx) in the four groups, reflecting endothelial-dependent dilatation, but there were no significant differences in the degree of change between the groups. Likewise, the GTN administration reduced the AIx in all four groups, but here the percentage reduction of AIx was significantly less in the current AAS users compared to the other three groups. The study therefore suggests that there is no difference in endothelial function between the four groups, but that there is reduced endothelial-independent vasodilatation in the group of current AAS users. There were no differences in AIx alterations between the other three groups, suggesting recovery of vasomotor function following the cessation of AAS.
It has been shown that alteration in elastic properties of the aorta can predict cardiovascular risk (Gosling and Budge 2003). Kasikcioglu et al. (2007) therefore examined 14 male bodybuilders using AAS and compared them to 27 male wrestlers, using a standard Doppler echocardiography unit, and measuring the ascending aorta with two-dimensional guided M-mode tracings. Using the systolic and diastolic aortic diameter, pulse pressure and diastolic blood pressure, the investigators calculated aortic strain, aortic distensibility and aortic stiffness index. Their main finding was that the aortic distensibility in athletes using AAS was significantly lower than in nonusers. This is in contrast to what has been found in endurance athletes (Kasikcioglu et al. 2005), where aortic distensibility was increased.
In summary, there is conflicting evidence regarding vasoreactivity in users of AAS. Nevertheless, based on the studies mentioned before, the steroid-using groups most often tend to demonstrate unfavorable measurements, whether it is involving endothelial-dependent or endothelial-independent vasodilatation. A degree of reversibility seems to be consistent, though. The inconsistent results are likely to arise from the obvious study limitations which are unavoidable in such populations of abusers of AAS. There is a diversity of compounds abused, and a variety of duration and route of administration. Adding to the difficulties of interpreting the results are the highly prevalent simultaneous abuse of other drugs, such as e.g. ephedrine, growth hormone and insulin. Despite these drawbacks, the accumulated evidence base supports the notion of a deleterious effect of AAS abuse on vascular function.
5 Coronary Calcification
Coronary artery calcium content (expressed as a so-called “calcium score”) has been shown to correlate with the total plaque burden in the coronary arteries and hence to be a more direct indicator of endothelial damage than other risk factors, such as low HDL-cholesterol (Brown et al. 2001; Kondos et al. 2003; Rumberger et al. 1995). This applies to all populations hitherto studied.
As regards the population of abusers of anabolic androgenic steroids (AAS), a study published in 2006 by Santora and colleagues measured the coronary artery calcium score of 14 professional bodybuilders with electron beam tomography (Santora et al. 2006). The age of the participants in the study ranged from 28 to 55 years and the mean number of years of AAS use in the group was 12.6 years. None of them had a history of cardiovascular disease. Seven of the 14 men had coronary artery calcium accumulation, i.e. an increased score. According to previous large population studies (Hoff et al. 2001; Mitchell et al. 2001), where percentile tables could be established that provide expected coronary calcium scores for different age groups, the likely number to have such a finding in this age group would have been three (as opposed to seven). As anticipated, all participants had significantly lower HDL-cholesterol than the typical population. None of them had any clinical signs of coronary artery disease. Ejection fraction, measured with echocardiography, was within the normal range for this age group.
The authors concluded that this study for the first time indicates that the abuse of AAS contributes directly to the early development of coronary atherosclerosis (Fig. 4), as determined by noninvasive measures of coronary artery calcium. Whether the pathogenesis is indirectly due to the unfavorable effect upon lipid profile, or a direct toxic or inflammatory effect of the steroids on the endothelium, remains unknown.
With the rapid technological development of multi-detector computed tomography equipment, one might expect further and larger studies in the future, addressing the likely association of long-term AAS abuse and coronary atherosclerosis.
6 Blood Platelet Function and Haemostasis
Case reports of anabolic androgenic steroid (AAS) abusers presenting with manifestations of thromboembolic disease are not rare, at least not when arterial in nature. Of the venous types, both deep venous thrombosis and pulmonary embolism have been described (Gaede and Montine 1992; Liljeqvist et al. 2008). Four cases of superior sagittal sinus thrombosis were reported during androgen treatment for hypoplastic anemia (Chu et al. 2001; Shiozawa et al. 1982). At least two additional cases have been reported, affecting a 22-year-old man (Sahraian et al. 2004), and a 31-year-old man (Jaillard et al. 1994), both bodybuilders using AAS. As for the arterial bed, there is an abundance of reports of cerebrovascular events, myocardial infarctions and peripheral arterial thromboses in this population, and even one of a ventricular thrombosis (McCarthy et al. 2000). However, to date there is no direct scientific evidence that AAS are thrombogenic in humans. Blood platelets together with the fibrinolytic system have a pivotal role in the pathogenesis of arterial thrombosis (Fuster et al. 1985). In support of this notion is the strong evidence from large-scale randomized trials that platelet inhibition significantly decreases the death and infarction rate in patients with coronary artery disease and cerebrovascular disease (Budaj et al. 2002, Cairns et al. 1985; Collins et al. 1994; Diener et al. 2008; Lewis et al. 1983). Reports of venous thromboembolic manifestations in AAS abusers are not as common as the ones of arterial thrombosis. A possible prothrombotic effect through the aromatization of testosterone to estradiol has been suggested (Liljeqvist et al. 2008), as estrogen-based therapies have been shown to increase the risk of venous thromboembolism (Lowe 2002). There are also experimental reports showing alterations at different stages of the hemostatic and fibrinolytic system by AAS administration, as well as effects on platelet function, which might explain what seems to be an increased risk of thromboembolic disease in this population (Ferenchick 1991). Some of these findings have been confirmed in human studies.
Androgen-mediated enhancement of platelet aggregability and augmenting of thrombosis have been shown in experimental animal models of thrombosis, in studies done in the 1970s and 1980s (Emms and Lewis 1985; Johnson et al. 1975; Johnson et al. 1977; Uzunova et al. 1976; Uzunova et al. 1977). Platelet aggregability is largely dependent on arachidonic acid metabolism (Fig. 5), and it has been shown that large doses of androgens affect both the platelet (Pilo et al. 1981) and the vascular cyclooxygenase activity (Greenberg et al. 1974). A decrease in the production of prostacyclin PgI2, a potent inhibitor of platelet aggregation, has been found in rat smooth muscle cells in culture after administration of testosterone (Nakao et al. 1981; Rosenblum et al. 1987). Furthermore, potentiation of platelet aggregation in vitro was demonstrated when incubating human platelets with testosterone, causing intensified response to several different aggregating agents (Pilo et al. 1981). Interestingly, significant bleeding in hypogonadal men has been linked to hypoactive platelets (Pawlowitzki et al. 1986).
In a report from 1992, Ferenchick et al. (1992) studied blood platelet stimulation thresholds in 28 male weightlifters, 24 of them using different kinds of AAS. Non-significant trends toward increased platelet counts and increased platelet aggregation to adenosine diphosphate in the AAS group were noted. Unfortunately the study did not have the power to detect potential between-group differences, as the control group ended up with only four subjects, as ironically eight of the 12 declared nonusers had unexpected findings of positive urine androgen assays. In the same study, subgroup analysis by age showed that AAS users older than 22 years had significantly lower aggregometric collagen threshold levels than their younger counterparts, but, referring to additional studies by the same group, the authors believe that age alone cannot explain this finding.
Ajayi et al. (1995) investigated testosterone as a regulator of the expression of human platelet thromboxane A2 receptors (TXA2 is a metabolite of arachidonic acid, and a potent vasoconstrictor and platelet aggregator). The authors recruited 16 healthy men who in a double-blind, placebo-controlled study were given testosterone cypionate 200 mg i.m. twice, two weeks apart, or saline placebo. As a result, in the treatment group there was a significant increase in platelet TXA2 receptor density and an increase in the maximum platelet aggregation response, though the latter did not increase in proportion with the receptor density increase. The researchers concluded that testosterone confers prothrombotic effects on the platelets.
As for the hemostatic and fibrinolytic system, the picture is less clear. Studies of AAS indicate an effect on these systems, but the results have in some respects been contradictory. The literature gives support to the view that AAS has some hypercoagulable effects, but the extent of it is unclear, and to what degree concomitant apparent AAS-induced fibrinolytic, i.e. protective, mechanism is operational is uncertain. Early studies of stanozolol (Barbosa et al. 1971; Small et al. 1982; Verheijen et al. 1984) gave rise to expectations that the drug had therapeutic potential as an activator of the fibrinolytic system, as elevated levels of both plasminogen activator and plasminogen were found following i.m. injections of the drug. Several 17α-alkylated androgens have been shown to increase plasminogen activator activity and serum levels of plasminogen, protein C and antithrombin III (Kluft et al. 1984; Small et al. 1984). Stanozolol also increased the levels of antithrombin III and protein C in male and female patients suffering from congenital insufficiency syndrome, but the clinical effects were disappointing (Broekmans et al. 1987; Winter et al. 1984). Neither did stanozolol have any preventive effect against postoperative deep vein thrombosis following abdominal surgery (Blamey et al. 1984). However, stanozolol has been shown to increase fibrinolytic activity by reducing the plasma levels and activity of PAI-1 (plasminogen activator inhibitor), yet clinical utilization has hitherto not been justified. In a male contraception study, the hemostatic effects of i.m. injections of testosterone enanthate were investigated. The subjects, 32 healthy men, received the treatment weekly for 52 weeks (Anderson et al. 1995). A slight increase in antithrombin III and prothrombin fragments F1 + 2 was noted, as well as a decrease in protein C levels, free protein S and plasminogen activator inhibitor. The authors summarized that these changes indicate an increase in coagulatory activity, but that the decrease of PAI-1 might outweigh the prothrombotic effects.
Studies of hemostasis in AAS abusers are almost nonexistent. Ansell et al. (1993) found indications of an activated fibrinolytic state, but no signs of a hypercoagulable state when investigating 16 bodybuilders, 11 of them during the influence of a variety of AAS. Those with paired samples (n = 6) showed a significant increase in protein C antigen and free protein S antigen during steroid use. An increase in euglobulin lysis time indicated an activation of the fibrinolytic mechanism in the steroid-using group. All other parameters apart from elevated platelet count (in the steroid group) turned out negative, among them fibrinogen, antithrombin III activity, protein C activity, plasminogen activity, D-dimer and factor VII and VIII activity. However, this study has been criticized because the subjects’ self-reporting of AAS was not confirmed by urine assays, as other studies have demonstrated a remarkable discrepancy between self-reported use of AAS and documented use by urine analyses.
In a larger study of AAS and hemostasis, Ferenchick et al. (1995) investigated 32 weightlifters, 23 users of AAS and 17 nonusers. This was the first, and to our knowledge the only study to describe the effects of AAS on humoral coagulation utilizing steroid-free weightlifters as controls and confirming self-reports with urine assays. Markers of clotting and fibrinolytic activity, namely thrombin/antithrombin III (TAT) complexes, prothrombin fragments1 + 2 and D-dimer were all increased in the user group, while endothelial-based fibrinolytic components, tissue plasminogen activator antigen (t-Pa Ag) and plasminogen activator inhibitor (PAI-1) interestingly were more likely to be higher in the nonuser group. Inhibitors of the clotting system, antithrombin III activity, protein C and S activity were significantly higher in users vs. nonusers. The authors concluded that some AAS-using weightlifters have an accelerated activation of their hemostatic systems evidenced by increased generation of both thrombin and plasmin, and that these changes could reflect a thrombotic diathesis that may contribute to vascular occlusion in AAS-using athletes. They also pointed out that the predictive value of these coagulation abnormalities, in terms of risk of thrombosis to individual athletes or the population as a whole, remains to be studied. Ironically, this statement still is applicable, more than 10 years later, which underscores the difficulties of elucidating clear evidence as to thrombosis and hemostasis in these cohorts.
In a more recent study, Kahn et al. (2006) evaluated the short-term effects of oxandrolone, taken 10 mg twice daily for 14 days, on both platelet function and the hemostatic/fibrinolytic system. The platelet part of the study turned out negative, as the effect on ADP-induced platelet aggregation was not significant. However, the authors believe this was because of a concomitant increase in factor V and X, causing inhibition of thromboxane A2 synthesis in platelets. Oxandrolone induced a highly significant increase in plasminogen and a significant decrease in PAI-1, indicating activation of the fibrinolytic system. The levels of coagulation factors II and V increased significantly, while fibrinogen and factors VII, VIII and X did not change or only did so nonsignificantly. The authors summarize the findings to be evidence of a simultaneous stimulation of both pro-coagulatory and fibrinolytic activity, resulting in a balanced effect on the hemostatic system by oxandrolone.
Another mechanism possibly contributing to thrombogenesis is the AAS-induced increase in the level of erythropoietin causing elevated levels of hemoglobin, a very common finding in AAS users (Shahidi 1973; Teruel et al. 1995). According to the Framingham data, increased hematocrit values are correlated with an increase in the cardiovascular risk and total mortality (Gagnon et al. 1994). Combined with an increase in platelet aggregability, it is likely that the elevated hematocrit in AAS users will contribute to the increased risk of thrombosis.
Taken together, the abuse of AAS does confer an enhanced pro-thrombotic state, most prominently through an activation of platelet aggregability (Fig. 6). The concomitant effects on the humoral coagulation cascade are more complex and include both pro-coagulatory and fibrinolytic pathways of activation.
The illustration shows different pathways of blood platelet activation, adhesion and aggregation. AAS appear to increase the platelet aggregation response. Experimental and human studies have indicated that AAS increase platelet production of TXA2 and increase both platelet and vascular TXA2 receptor density. The drugs may also decrease the production of PGI2. ADP = Adenosine diphosphate; COX = Cyclooxygenase; NO = Nitric oxide; AA = Arachidonic acid; PDGF = Platelet derived growth factor; PGI2 = Prostacyclin; TXA2 = Thromboxane A2; vWF = von Willebrand factor; GP = Glycoprotein
7 Lipids
The most studied cardiovascular effects of anabolic androgenic steroids (AAS) are probably the effects on lipoproteins. The last 25 years have yielded numerous reports from human studies on the subject, and for once the results to a large extent concur, at least concerning readily measurable parameters. The long-term consequences of the alterations of lipid metabolism that these drugs cause are unfortunately still largely unknown.
In the general population, epidemiological studies demonstrate a strong relationship between levels of low-density lipoprotein (LDL) cholesterol and the incidence of atherosclerotic cardiovascular disease (Stamler et al. 1986). Furthermore, there is a large body of evidence which supports a central role for lowering levels of LDL in the prevention of cardiovascular events (Downs et al. 1998, HPS Collaborative Group 2002; Pedersen et al. 1994; Shepherd et al. 1995). Epidemiological studies also show a strong relationship between low levels of high-density lipoprotein (HDL) cholesterol and risk for cardiovascular events (Castelli and Anderson 1986; Gordon et al. 1977). Multivariate analyzes have shown that changes in HDL levels are an independent predictor of atheroma burden (Jacobs et al. 1990). The combined evidence derived from placebo-controlled trials have revealed that the greatest benefit of statin therapy in terms of absolute risk reduction was observed in patients with the lowest baseline levels of HDL (Downs et al. 1998; HPS Collaborative Group 2002; Pedersen et al. 1994). In a recent post-hoc analysis, Nicholls et al. (2007) provide evidence that increases in HDL levels are correlated with beneficial effects of statins on the progression of coronary artery disease.
Atherothrombosis is a complex disease in which cholesterol deposition, inflammation and thrombus formation play a major role. LDL exerts its pathological effects by infiltrating the arterial endothelium into the intima, where matrix proteins including proteoglycans, collagen and fibronectin are attracted. Another important feature of lipoprotein transport is related to the effect of HDL, which promotes reverse cholesterol transport from the arterial wall, specifically from lipid-laden macrophages. The HDL subfractions may play a role in this beneficial effect, with HDL2 being the most important for reverse lipid transport (Fuster et al. 2005). Interestingly, despite its protective effects, patients with high HDL plasma levels still can present an acute coronary syndrome, probably related to elevations in HDL3 rather than in HDL2.
AAS clearly induce an extreme atherogenic alteration on lipid levels. A solid body of evidence has been published on the subject. The drugs cause a marked depression in HDL, especially on subfraction HDL2. The levels of LDL are also negatively affected, though not as pronounced as the effects on HDL are. Though it is far from proven that these alterations transform into coronary artery disease in the population at debate, the association cannot be denied.
The first report of the effect of AAS on plasma lipid values came in 1980, when it was shown that oxandrolone reduced HDL and apolipoproteins AII and AII1 in hyperlipidemic subjects (Cheung et al. 1980). The findings were confirmed in normolipidemic subjects two years later (Taggart et al. 1982). Numerous reports (Bonetti et al. 2008; Frölich et al. 1989; Glazer 1991; Hartgens et al. 1996; Hurley et al. 1984; Kuipers et al. 1991; Palatini et al. 1996; Sachtleben et al. 1997; Thompson et al. 1989; Urhausen et al. 2003; Yeater et al. 1996) with similar findings surfaced over the next two decades, several of them specifically addressing strength athletes abusing AAS. A frequent finding in these studies is also the increase of LDL levels. Most of the studies were prospective cohort studies or cross-sectional studies and the steroids were self-administered, in supraphysiologic doses and as combinations of orally and injected preparations. Many of the studies did not control for diet, exercise, or the type, purity, and dose of AAS used. Of course this precludes the findings from delivering the desired scientific attainments in a purist sense, but the comprehensiveness of the available data nevertheless allows for conclusions. Some of the studies were done with therapeutic doses and were placebo-controlled. A head-to-head comparison of oral AAS vs. injected testosterone has also been done (Thompson et al. 1989).
Although slightly dated, the comprehensive review by Glazer (1991) gives a fine overview of the impact of AAS on HDL and LDL, the underlying mechanisms behind the changes and their possible clinical significance. Only a modest amount of new knowledge has surfaced in subsequent years. Fifteen studies are referred to by Glazer, and the average HDL reduction was 52% (range, 39–63%) for the prospective cohort studies and 51% (range, 41–70%) for the cross-sectional studies. Reductions of this magnitude are far greater than those produced by other pharmacologic or nonpharmacologic agents including smoking and obesity. As for the subfractions of HDL, the most pronounced effect is on HDL2, which has been shown to be reduced by 78% (range, 71–89%), while the average reduction of HDL3 was 35%.
AAS are believed to exert their influence on lipoproteins by the induction of hepatic triglyceride lipase (HTGL) synthesis in the liver. Localized to the luminal surface of hepatic endothelium, HTGL is thought to catabolize HDL via its phospholipase activity and remove HDL from plasma (Applebaum-Bowden et al. 1987; Ehnholm et al. 1975; Haffner et al. 1983; Kantor et al. 1985; Lenders et al. 1988; Taggart et al. 1982). Studies of AAS and HTGL activity have shown increases of HTGL in the range of 143–232% during AAS use (Glazer 1991).
The orally taken 17α-alkylated substances (such as stanozolol, oxymetholone and methandienone) exert much stronger effects than other AAS (Friedl et al. 1990; Thompson et al. 1989). Generally, nonaromatizable androgens have more pronounced effects on HTGL induction and plasma HDL (Friedl et al. 1990; Melchert and Welder 1995; Zmuda et al. 1993). In the prospective crossover study by Thompson et al., 11 weightlifters were given either oral stanozolol (6 mg/day) or intramuscular testosterone enanthate (200 mg/week) for six weeks. Stanozolol reduced HDL and the HDL2 subfraction by 33 and 71% respectively. In contrast, testosterone decreased HDL by only 9%. Moreover, stanozolol increased the HTGL activity by 123% while the effect of testosterone (on the enzyme) was not significant. A similar effect on HDL has also been demonstrated with other 17α-alkylated steroids (Cheung et al. 1980; Friedl et al. 1990).
There appears to be minimal or no dose relationship in oral AAS-induced HDL depression (Glazer 1991) and maximal or near maximal HDL level decrement results from even therapeutic dosages of oral AAS. The injectable testosterones on the other hand seem to affect HDL in a more dose-related manner. In a study on healthy young men, Bhasin et al. (2001) demonstrated that testosterone enanthate dosages (and testosterone concentrations) were negatively correlated to plasma levels of HDL. In another study by Kouri et al. using i.m. injections of escalating dosages of testosterone cypionate, maximum HDL depression was reached at 300 mg/week and this depression remained unchanged with 600 mg/week for two more weeks. Singh et al. demonstrated that i.m. testosterone enanthate 600 mg/week reduced HDL levels, whereas lower doses did not exert any effect on lipoprotein profiles (Singh et al. 2002). The use of therapeutic or supraphysiologic doses of nandrolone decanoate does not seem to affect lipoproteins in a detrimental way (Friedl et al. 1990; Glazer and Suchman 1994; Kuipers et al. 1991).
The AAS-induced HDL depression can be observed within a few days of starting with the drugs and studies suggest that the HDL level reaches its nadir within a few weeks (Glazer 1991; Thompson et al. 1989). In a study by Hartgens et al. (2004), 19 strength athletes self-administering supraphysiologic doses of AAS had no further decline of HDL, HDL2 and HDL3 after eight weeks. After cessation of AAS, the lipoprotein levels seem to recover completely after one to three months (Alén et al. 1985; Hartgens et al. 2004; Kuipers et al. 1991). Notably, in the recent study by Hartgens et al., the authors demonstrated that recovery strongly depended on the duration of the AAS course. In their study, one group self-administered supraphysiologic dosages of AAS for an average of 14 weeks. Their serum concentrations of HDL, apolipoprotein-A1 (Apo-A1) and lipoprotein(a) (Lp(a)) were not normalized six weeks after cessation, while in another group of so-called short-term users (AAS use for eight weeks) the same parameters had returned to baseline levels. Urhausen et al. (2003) investigated the reversibility of AAS effects in 15 long-term (average 26 weeks per year for nine years) users of supraphysiologic doses 12–43 months after cessation. Seventeen current users served as control group. In all of the ex-users HDL concentrations had returned to normal values, with the exception of one, which was believed to be genetically caused.
As for LDL, AAS will generally induce an elevation of serum values, in much the same pattern as they do on HDL, though not to such an extreme level (Applebaum-Bowden et al. 1987; Haffner et al. 1983; Hurley et al. 1984; Kantor et al. 1985; Kleiner et al. 1989; Lenders et al. 1988; Thompson et al. 1989; Webb et al. 1984). In Glazer’s review the degree of increase was estimated at 36%. Injections of testosterone up to a dosage of 600 mg/week do not seem to alter LDL levels (Kouri et al. 1996; Singh et al. 2002; Zmuda et al. 1993). Total cholesterol and triglycerides were generally not significantly changed in the studies previously referred to.
The nonfasting Apo-B/Apo-A1 ratio has recently been assessed as superior to any of the cholesterol ratios for estimation of the risk of acute myocardial infarction in all ethnic groups (McQueen et al. 2008). While Apo-A1 is the major HDL apolipoprotein, it is not surprising that AAS severely decreases its level, in Glazer’s review by 33–41%, calculated from five studies. At the same time an increase in Apo-B levels of the same magnitude was also found. In the recent study by Hartgens et al., the group of self-administering AAS abusers was found to have a large and highly significant decrease of Apo-A1 and a concomitant increase of Apo-B. These changes were apparent after eight weeks’ treatment, but did not increase further at 14 weeks. As for HDL, the 17α-alkylated drugs rather than testosterone esters are responsible for inducing more profound effects on the apolipoproteins (Friedl et al. 1990; Singh et al. 2002; Thompson et al. 1989).
Lipoprotein (a) (Lp(a)) is a risk factor for both atherothrombotic and purely thrombotic events, and it increases global cardiovascular risk, especially when LDL cholesterol is concomitantly elevated (Koschinsky 2005; Kostner et al. 1981; Kronenberg et al. 1999; White et al. 1996). Several reports (Cohen et al. 1996; Crook et al. 1992; Zmunda et al. 1996) have suggested that AAS may favorably lower Lp(a) concentrations, most recently by Hartgens et al. In this study (Hartgens et al. 2004), the investigators found Lp(a) to be highly significantly reduced after 8 and 14 weeks of supraphysiologic dosages of AAS. However, if or to what degree this apparent reduction translates into cardiovascular protection remains unknown.
Finally, another marker of atherosclerotic disease is homocysteine, a byproduct of methionine metabolism (Nygård et al. 1997; Tonstad et al. 1996). Homocysteine has also been shown to impair vascular endothelial function through impairment of nitric oxide production (van Guldener and Stehouwer 2000). Two studies have identified hyperhomocysteinemia in bodybuilders using supraphysiologic doses of various types of AAS (Ebenbichler et al. 2001a; Graham et al. 2006). In a previous study (Zmuda et al. 1997), short-term administration of testosterone enanthate did not affect fasting homocysteine levels in weight lifters. In the study by Graham et al., consisting of ten current users of AAS and control groups, three of the participants died during the study. Interestingly they all had cardiovascular disease as cause of death and their homocysteine levels were – ironically – markedly elevated, and above the mean average of the user group as a whole.
Based on current knowledge of the lipid effects of AAS, how large is the increased risk of developing coronary heart disease (CHD)? Obviously, there are no studies that can answer this most pivotal question. The Framingham data showed that patients with HDL levels less than 1.0 mmol L−1 had a fourfold increase in risk of CHD compared to those with levels of 1.03–1.27 mmol L−1, when total cholesterol levels were normal. Based on the described changes in HDL in the AAS-abusing population and the Framingham data, Glazer in his review puts forward an estimate of risk of CHD to be increased three- to six-fold. However, as he comments, this estimate is complicated by several factors, among them the fact that the studied steroid abusers are younger than the patients who have delivered the data on lipid levels and risk evaluation. Another important feature is that most AAS users take the drugs intermittently, in cycles of 6–16 weeks, with abstinence periods in between, often long enough to reverse the detrimental lipid effects.
To summarize, there is a comprehensive body of evidence documenting the various alterations of lipid metabolism induced by AAS. The most prominent changes are concomitant elevations of LDL and decreases of HDL, the combined effects of which are deleterious. This should be taken into account when counseling abusers, advising health authorities, health care providers and prevention stakeholders, and informing the general public.
8 Arrhythmias and Sudden Death
It is a tragic fact that sudden death is not an unknown end stage after long-term abuse of AAS. The incidence is of course impossible to estimate, but there are several published case reports describing devastatingly fatal events (Di Paolo et al. 2007; Dickerman et al. 1995; Fineschi et al. 2001, 2007; Hausmann et al. 1998; Kennedy and Lawrence 1993; Luke et al. 1990). Indeed, most abusers of AAS are familiar with the risk of sudden death, at least in the sense that they have knowledge of someone in their close or distant milieu who abruptly and tragically lost his life. The etiology behind sudden death in this population is unknown, and will unfortunately most likely continue to be so. It would be impossible to conduct a study to shed light on incidence and underlying mechanisms. It is however not a controversial assumption that a malignant arrhythmia is the underlying cause of death. Whether these arrhythmias are directly triggered by AAS or whether they occur as indirect or secondary consequences of AAS, as for instance through left ventricular hypertrophy or cardiomyopathy, is unclear. To further complicate the issue, there is the widespread use of other drugs among abusers of AAS, both recreational substances as stimulants, marijuana, cocaine and alcohol, the concomitant use of masking agents such as diuretics, and the use of anti-estrogens, thyroid hormones and growth hormone (Furlanello et al. 2003). Insulin injections carry the risk of death due to hypoglycemia. Among stimulants known to have potential arrhythmic properties are ephedrine, caffeine and unequivocally amphetamine, all of which are highly prevalent substances among bodybuilders using AAS. Another important consideration to bear in mind is that inherited arrhythmogenic diseases, such as long QT syndrome and other ion channel diseases and arrhythmogenic right ventricular cardiomyopathy (a genetic disease characterized by fatty infiltration in the right ventricle, causing increased risk of arrhythmia and sudden death) do also exist in the growing population of abusers of AAS. Hard physical exercise combined with illicit drugs of various kinds can very well trigger a malignant arrhythmia in these particularly predisposed individuals.
There are very few scientific reports on arrhythmias and AAS. A handful of case reports have been published, but hardly any work has been done in the field of the pathophysiology of arrhythmias in this particular population, at least not human electrophysiologic studies.
A case report by Sullivan et al. (1999) presents a 22-year-old male bodybuilder who was admitted to hospital with symptomatic rapid atrial fibrillation. He had consumed large doses of AAS, in the form of intramuscular injections. He had no past cardiac medical history or any other condition known to cause atrial fibrillation and did not use tobacco, alcohol or any drugs other than AAS. Echocardiography showed an area of septal hypokinesis, posterior and septal wall thickness at the upper limit of normal, and preserved left ventricular function. The patient was discharged from hospital after two days, after having spontaneously converted to sinus rhythm. Twenty-four hours Holter monitoring three weeks later showed normal sinus rhythm, and the patient had at that time lost 9 kg following steroid cessation. Afterwards he was lost to follow-up, which regrettably is often the case with AAS abusers.
A similar story was quite recently presented in a case report by Lau et al. A 36-year-old bodybuilder was referred to hospital with persistent atrial fibrillation (Lau et al. 2007). He had no medical history, was a nonsmoker and had no cardiovascular risk factors apart from taking intramuscular injections of testosterone enanthate and stanozolol in supraphysiologic doses. Echocardiography showed normal left ventricular size and function and a normal left atrial diameter. The patient was treated with DC cardioversion, but reverted back to atrial fibrillation after 15 days. He was then treated with flecainide 100 mg twice daily and metoprolol 150 mg twice daily. A second cardioversion was successful, though two attempts were needed, finally with 360 J. His left atrium had by this time increased considerably, but the left ventricle parameters had remained unaltered. In the mean time, the patient had lost 16 kg following his own decision to cease the administration of AAS. A year later, he was still in sinus rhythm and without exogenous steroids or antiarrhythmic medication. Despite any other known condition predisposing this patient to arrhythmia, and though his symptomatic onset of atrial fibrillation correlated with the initiation of AAS abuse, the association between AAS and atrial fibrillation must be reviewed as an association only, and there is no evidence of causal relationship.
In a report of four weightlifters abusing AAS, Nieminen et al. (1996) describe serious cardiac side effects of the drugs, one of them being ventricular tachycardia (VT). The weightlifter who experienced this arrhythmia was 29 years old and had taken AAS during several periods over the past eight years. At a routine exercise test at 250 W workload, a monomorphic VT with a frequency of 230/min was recorded and exercise was stopped. After one minute of rest, the rhythm degenerated into a polymorphic VT and then to ventricular fibrillation causing unconsciousness. Cardioversion was performed and the patient regained sinus rhythm and consciousness. There was no sign of myocardial infarction. Echocardiography showed a dilated left ventricle with marked wall thickening. Angiography revealed no stenoses in the coronary arteries, but ventriculography showed a dilated left ventricle with Am ejection fraction of 40%. Programmed electrophysiologic stimulation could not induce VT. Endomyocardial biopsy revealed focal fibrosis of the left ventricle and fat degeneration, and there was no sign of granulocyte infiltration. Five months later, after cessation of AAS, the left ventricular dimension was normalized and the hypertrophy had decreased slightly. There were no further episodes of VT during follow-up. Although the association between AAS and this patient’s symptoms and findings seems rather convincing, his drug regimen also included clenbuterol, growth hormone and human chorionic gonadotropin. As so often in this setting, this contributes to clouding the picture.
Two other case reports describe the occurrence of ventricular tachycardia in AAS-abusing bodybuilders (Appleby et al. 1994; Mewis et al. 1996). However, in both cases the subjects also had coronary artery disease, believed to be the underlying cause of the arrhythmia. The subject described in Mewis’ report had reduced function of left ventricle, assessed by echocardiography. Intriguingly, other than long-term use of stanozolol, this individual had no classic coronary risk factors.
In an electrophysiologic study by Stolt et al. 1999, 15 male powerlifters using large doses of AAS were compared to 30 male orienteering runners from the Finnish national training program and to 15 sedentary young men. The investigators measured QT interval and QT dispersion (the difference between the longest and the shortest QT interval) in a 12-lead resting electrocardiogram. Echocardiographic assessment of the left ventricle (LV) mass, wall thickness and chamber dimension was also performed. The dispersion of the QT intervals between the electrocardiographic leads is an indirect measure of the heterogeneity of ventricular depolarization, and several studies suggest that an increase in QT dispersion is associated with increased risk of arrhythmic events (Higham and Campbell 1994; Mänttäri et al. 1997; Pye et al. 1994). Left ventricular hypertrophy is associated with increased QT dispersion and increased mortality in hypertensive patients (Mayet et al. 1996; Perkiömäki et al. 1996). The athlete group was considered to be a model of physiologic adaptive left ventricular hypertrophy, while the AAS group were expected to have features of pathologic hypertrophy as well. As for the echocardiographic findings, the LV mass was largest in the AAS group, but when related to body surface area, the endurance athletes had 9% greater LV mass than the AAS group. The septum diameter was identical in these two groups, but the posterior wall was thicker in the AAS group than in the endurance athlete group. Both groups had significantly higher values than the sedentary control group, for LV mass as well as LV mass index and wall thicknesses. The main finding, however, was that the endurance athletes had the longest QT intervals and the AAS group of power athletes had the shortest, and the latter group also had the greatest amount of QT dispersion, while the endurance athletes had the least. Even when adjusted for heart rate, the QT interval differences were highly significant. The QT interval did not correlate with LV mass, but it did so significantly with E/A ratio, a Doppler index of altered diastolic function. The AAS group had significantly lower E/A ratio than the endurance athletes. The authors believe the prolonged QT interval seen in the endurance athlete group mainly is a result of enhanced vagal activity. It did not seem that increased LV mass played any role in prolonging the QT interval. In fact, the AAS group, despite their increased LV mass, had shorter QT interval and increased QT dispersion. The authors believe this to be caused by LV hypertrophy with altered myocardial structure. Their findings would suggest that the use of AAS together with resistance training leads to an increased risk of malignant arrhythmias.
In the absence of further human studies on the topic, it appears appropriate to refer to some suggested mechanisms of arrhythmia from studies of rats exposed to AAS. In a study by Pereira-Junior et al. (2006), treatment of rats with supraphysiologic doses of nandrolone decanoate for eight weeks showed impaired tonic cardiac autonomic regulation, which the authors suggest may provide a key mechanism for anabolic steroid-induced arrhythmia and sudden cardiac death. Another nandrolone study, done in vivo on male rats by Phillis et al. (2007), administered a high dose of the drug acutely, and potentiated ischemia-induced arrhythmia and thereby decreased the proportion of rats surviving the ischemia. Though the study does not identify the mechanism behind this finding, the authors speculate that nandrolone may cause the release of intracellular calcium in a similar way to that shown in skeletal muscle, and thereby explain the observed proarrhythmic effects. They also refer to previous studies where other anabolic steroids have been shown to inhibit the reuptake of catecholamines into extraneuronal tissues, thereby increasing catecholamine concentrations at receptor sites. In a recent experimental study by Rocha et al. (2007), in which rats were treated with supraphysiologic doses of nandrolone decanoate, the investigators for the first time show that the combination of exercise and AAS causes an increase in the heart collagen concentration associated with the activation of the cardiac renin–angiotensin system. These pathophysiologic changes undoubtedly provide a patho-anatomic substrate that may explain the increased propensity to the generation and continuation of malignant cardiac arrhythmias.
Taken together, the use of AAS appears to confer an increased risk of life-threatening arrhythmia leading to sudden death, albeit the underlying mechanisms are still far from being elucidated.
References
Ajayi AA, Mathur R, Halushka PV. Testosterone increases human platelet thromboxane A2 receptor density and aggregation responses. Circulation. 1995;91:2742–2747.
Alén M, Rahkila P, Marniemi J. Serum lipids in power athletes self-administering testosterone and anabolic steroids. Int J Sports Med. 1985;6:139–144.
Alvarado RG, Liu JY, Zwolak RM. Danazol and limb-threatening arterial thrombosis: Two case reports. J Vasc Surg. 2001;34:1123–6.
Ammar EM, Said SA, Hassan MS. Enhanced vasoconstriction and reduced vasorelaxation induced by testosterone and nandrolone in hypercholesterolemic rabbits. Pharmacol Res. 2004;50:253–255.
Anderson RA, Ludlam CA, Wu FC. Haemostatic effects of supraphysiological levels of testosterone in normal men. Thromb Haemost. 1995;74:693–697.
Ansell JE, Tiarks C, Fairchild VK. Coagulation abnormalities associated with the use of anabolic steroids. Am Heart J. 1993;125:367–371.
Appell H-J, Heller-Umpfenbach B, Feraudi M, et al. Ultrastructural and morphometric investigations on the effects of training and administration of anabolic steroids on the myocardium of guinea pigs. Int J Sports Med. 1983;4:268–274.
Applebaum-Bowden D, Haffner SM, Hazzard WR. The dyslipoproteinemia of anabolic steroid therapy: increase in hepatic triglyceride lipase precedes the decrease in high density lipoprotein2 cholesterol. Metabolism. 1987;36:949–952.
Appleby M, Fisher M, Martin M. Myocardial infarction, hyperkalaemia and ventricular tachycardia in a young male body-builder. Int J Cardiol. 1994;44:171–174.
Baker PJ, Ramey ER, Ramwell PW. Androgen-mediated sex differences of cardiovascular responses in rats. Am J Physiol. 1978;235(2):H242–H246.
Barbosa J, Seal US, Doe RP. Effects of anabolic steroids on haptoglobin, orosomucoid, plasminogen, fibrinogen, transferrin, ceruloplasmin, alpha-1-antitrypsin, beta-glucuronidase and total serum proteins. J Clin Endocrinol Metab. 1971;33:388–398.
Behrendt H, Boffin H. Myocardial cell lesions caused by an anabolic hormone. Cell Tiss Res. 1977;181:423–426.
Beutel A, Bergamaschi CT, Campos RR. Effects of chronic anabolic steroid treatment on tonic and reflex cardiovascular control in male rats. J Steroid Biochem Mol Biol. 2005;93:43–48.
Bhargava KP, Dhawan KN, Saxena RC. Enhancement of noradrenaline pressor responses in testosterone-treated cats. Br J Pharmacol Chemother. 1967;31:26–31.
Bhasin S, Woodhouse L, Casaburi R, et al. Testosterone dose–response relationships in healthy young men. Am J Physiol Endocrinol Metab. 2001;281:E1172–E1181.
Blamey SL, McArdle BM, Burns P, et al. A double-blind trial of intramuscular stanozolol in the prevention of postoperative deep vein thrombosis following elective abdominal surgery. Thromb Haemost. 1984;51:71–74.
Boggia J, Li Y, Thijs L, et al. Prognostic accuracy of day versus night ambulatory blood pressure: a cohort study. Lancet. 2007;370(9594):1219–1229.
Bonetti A, Tirelli F, Catapano A, et al. Side effects of anabolic androgenic steroid abuse. Int J Sports Med. 2008;29(8):679–687.
Broekmans AW, Conard J, van Weyenberg RG, et al. Treatment of hereditary protein C deficiency with stanozolol. Thromb Haemost. 1987;57:20–24.
Brown BG, Morse J, Zhao XQ et al (2001) Electron-beam tomography coronary calcium scores are superior to Framingham risk variables for predicting the measured proximal stenosis burden. Am J Cardiol 88(2A):23E–26E
Brownie AC, Gallant S, Nickerson PA, et al. The occurrence of 11-deoxycorticosterone (DOC)-induced hypertension in the Long-Evans rat. Endocr Res Commun. 1978;5:71–80.
Budaj A, Yusuf S, Metha SR, et al. Benefit of clopidogrel in patients with acute coronary syndromes without ST-segment elevation in various risk groups. Circulation. 2002;106:1622–1626.
Cairns JA, Gent M, Singer J, et al. Aspirin, sulfinpyrazone, or both in unstable angina. Results of a Canadian multicenter trial. N Engl J Med. 1985;313:1369–1375.
Campbell SE, Farb A, Weber KT. Pathologic remodeling of the myocardium in a weightlifter taking anabolic steroids. Blood Press. 1993;2:213–216.
Capezzuto A, Achilli A, Serra N. Myocardial infarction in a 21-year-old body builder. Am J Cardiol. 1989;63:1539.
Carroll JE, Goodfriend TL. Androgen modulation of adrenal angiotensin receptors. Science. 1984;224:1009–1011.
Castelli WP, Anderson K (1986) A population at risk. Prevalence of high cholesterol levels in hypertensive patients in the Framingham Study. Am J Med 80(2A):23–32
Celermajer DS, Sorensen KE, Gooch VM, et al. Non-invasive detection of endothelial dysfunction in children and adults at risk of atherosclerosis. Lancet. 1992;340:1111–1115.
Cheung MC, Albers JJ, Wahl PW, et al. High density lipoproteins during hypolipidemic therapy. A comparative study of four drugs. Atherosclerosis. 1980;35:215–228.
Chu K, Kang DW, Kim DE, et al. Cerebral venous thrombosis associated with tentorial subdural hematoma during oxymetholone therapy. J Neurol Sci. 2001;185:27–30.
Chung T, Kellehert S, Liu PY, et al. Effects of testosterone and nandrolone on cardiac function: a randomized, placebo-controlled study. Clin Endocrinol. 2007;66:235–245.
Clark BM, Schofield RS. Dilated cardiomyopathy and acute liver injury associated with combined use of ephedra, gamma-hydroxybutyrate, and anabolic steroids. Pharmacotherapy. 2005;25:756–761.
Cohen LI, Hartford CG, Rogers GG. Lipoprotein (a) and cholesterol in body builders using anabolic androgenic steroids. Med Sci Sports Exerc. 1996;28:176–179.
Colan SD, Sanders SP, MacPherson D, et al. Left ventricular diastolic function in elite athletes with physiologic cardiac hypertrophy. J Am Coll Cardiol. 1985;6:545–549.
Collins R, Baigent C, Sandercock P, et al. Antiplatelet therapy for thromboprophylaxis: the need for careful consideration of the evidence from randomised trials. Antiplatelet trialists′ collaboration. Br Med J. 1994;309:1215–1217.
Crook D, Sidhu M, Seed M, et al. Lipoprotein Lp(a) levels are reduced by danazol, an anabolic steroid. Atherosclerosis. 1992;92:41–47.
Cunha TS, Moura MJ, Bernardes CF, et al. Vascular sensitivity to phenylephrine in rats submitted to anaerobic training and nandrolone treatment. Hypertension. 2005;46:1010–1015.
D’Andrea A, Limongelli G, Caso P, et al. Association between left ventricular structure and cardiac performance during effort in two morphological forms of athlete’s heart. Int J Cardiol. 2002;86(2–3):177–184.
D’Andrea A, Caso P, Salerno G, et al. Left ventricular early myocardial dysfunction after chronic misuse of anabolic androgenic steroids: a Doppler myocardial and strain imaging analysis. Br J Sports Med. 2007;41:149–155.
De Piccoli B, Giada F, Benettin A, et al. Anabolic steroid use in body builders: an echocardiographic study of left ventricle morphology and function. Int J Sports Med. 1991;12:408–412.
Di Bello V, Davide G, Massimiliano B, et al. Effects of anabolic-androgenic steroids on weight-lifters′ myocardium: an ultrasonic videodensitometric study. Med Sci Sports Exerc. 1999;31:514–521.
Di Paolo M, Agozzino M, Toni C, et al. Sudden anabolic steroid abuse-related death in athletes. Int J Cardiol. 2007;114:114–117.
Dickerman RD, Schaller F, Prather I, et al. Sudden cardiac death in a 20-year-old bodybuilder using anabolic steroids. Cardiology. 1995;86:172–173.
Dickerman RD, McConathy WJ, Schaller F, et al. Echocardiography in fraternal twin bodybuilders with one abusing anabolic steroids. Cardiology. 1997a;88:50–51.
Dickerman RD, McConathy WJ, Zachariah NY. Testosterone, sex hormone-binding globulin, lipoproteins, and vascular disease risk. J Cardiovasc Risk. 1997b;4:363–366.
Dickerman RD, Schaller F, Zachariah NY, et al. Left ventricular size and function in elite bodybuilders using anabolic steroids. Clin J Sports Med. 1997c;7:90–93.
Dickerman RD, Schaller F, McConathy WJ. Left ventricular wall thickening does occur in elite power athletes with or without anabolic steroid use. Cardiology. 1998;90:145–148.
Diener HC, Sacco RL, Yusuf S et al (2008) Effects of aspirin plus extended-release dipyridamole versus clopidogrel and telmisartan on disability and cognitive function after recurrent stroke in patients with ischaemic stroke in the Prevention Regimen for Effectively Avoiding Second Strokes (PRoFESS) trial: a double-blind, active and placebo-controlled study. Lancet Neurol 7(10):875–884
Downs JR, Clearfield M, Weis S, et al. Primary prevention of acute coronary events with lovastatin in men and women with average cholesterol levels: results of AFCAPS/TexCAPS. Air Force/Texas Coronary Atherosclerosis Prevention Study. JAMA. 1998;279:1615–1622.
Duchaine D. Underground steroid handbook II. Venice, CA: HLR Tech Books; 1989.
Ebenbichler CF, Kaser S, Bodner J, et al. Hyperhomocysteinemia in bodybuilders taking anabolic steroids. Eur J Int Med. 2001a;12:43–47.
Ebenbichler CF, Sturm W, Gänzer H, et al. Flow-mediated, endothelium-dependent vasodilatation is impaired in male body builders taking anabolic-androgenic steroids. Atherosclerosis. 2001b;158:483–490.
Ehnholm C, Huttunen JK, Kinnunen PJ, et al. Effect of oxandrolone treatment on the activity of lipoprotein lipase, hepatic lipase and phospholipase A1 of human postheparin plasma. N Engl J Med. 1975;292:1314–1317.
Emms H, Lewis GP. Sex and hormonal influences on platelet sensitivity and coagulation in the rat. Br J Pharmacol. 1985;86:557–563.
Falkenberg M, Karlsson J, Örtenwall P. Peripheral arterial thrombosis in two young men using anabolic steroids. Eur J Vasc Endovasc Surg. 1997;13:223–226.
Ferenchick GS. Anabolic/androgenic steroid abuse and thrombosis: is there a connection? Med Hypotheses. 1991;35:27–31.
Ferenchick GS, Adelman S. Myocardial infarction associated with anabolic steroid use in a previously healthy 37-year-old weight lifter. Am Heart J. 1992;124:507–508.
Ferenchick G, Schwartz D, Ball M, et al. Androgenic-anabolic steroid abuse and platelet aggregation: a pilot study in weight lifters. Am J Med Sci. 1992;303:78–82.
Ferenchick GS, Hirokawa S, Mammen EF, et al. Anabolic-androgenic steroid abuse in weight lifters: evidence for activation of the hemostatic system. Am J Hematol. 1995;49:282–288.
Ferrera PC, Putnam DL, Verdile VP. Anabolic steroid use as the possible precipitant of dilated cardiomyopathy. Cardiology. 1997;88:218–220.
Fineschi V, Baroldi G, Monciotti F, et al. Anabolic steroid abuse and cardiac sudden death. A pathologic study. Arch Pathol Lab Med. 2001;125:253–255.
Fineschi V, Riezzo I, Centini F, et al. Sudden cardiac death during anabolic steroid abuse: morphologic and toxicologic findings in two fatal cases of bodybuilders. Int J Legal Med. 2007;121:48–53.
Fisher M, Appleby M, Rittoo D, et al. Myocardial infarction with extensive intracoronary thrombus induced by anabolic steroids. Br J Clin Pract. 1996;50(4):222–223.
Frankle MA, Eichberg R, Zachariah SB. Anabolic androgenic steroids and a stroke in an athlete: case report. Arch Phys Med Rehabil. 1988;69:632–633.
Freed DL, Banks AJ, Longson D, et al. Anabolic steroids in athletics: crossover double-blind trial on weightlifters. Br Med J. 1975;2:471–473.
Friedl KE, Hannan CJ Jr, Jones RE, et al. High-density lipoprotein cholesterol is not decreased if an aromatizable androgen is administered. Metabolism. 1990;39:69–74.
Frölich J, Kullmer T, Urhausen A, et al. Lipid profile of body builders with and without self-administration of anabolic steroids. Eur J Appl Physiol. 1989;59:98–103.
Furlanello F, Bentivegna S, Cappato R, et al. Arrhythmogenic effects of illicit drugs in athletes. Ital Heart J. 2003;4:829–837.
Fuster V, Steele PM, Chesebro JH (1985) Role of platelets and thrombosis in coronary atherosclerotic disease and sudden death. J Am Coll Cardiol 5(6 Suppl):175B–184B
Fuster V, Moreno PR, Fayad ZA, et al. Atherothrombosis and high-risk plaque: part I: evolving concepts. J Am Coll Cardiol. 2005;46:937–954.
Gaede JT, Montine TJ. Massive pulmonary embolus and anabolic steroid abuse. JAMA. 1992;267:2328–2329.
Gagnon DR, Zhang TJ, Brand FN, et al. Hematocrit and the risk of cardiovascular disease – the Framingham study: a 34-year follow-up. Am Heart J. 1994;127:674–682.
Gallant S, Alfano J, Chargpin M, et al. The inhibition of rat adrenal cytochrome P-45011 beta gene expression by androgens. Endocr Res. 1992;18:145–161.
Glazer G. Atherogenic effects of anabolic steroids on serum lipid levels. A literature review. Arch Int Med. 1991;151:1925–1933.
Glazer G, Suchman AL. Lack of demonstrated effect of nandrolone in serum lipids. Metabolism. 1994;43:204–210.
Gordon T, Castelli WP, Hjortland MC, et al. High density lipoprotein as a protective factor against coronary heart disease. The Framingham Study. Am J Med. 1977;62:707–714.
Gosling RG, Budge MM. Terminology for describing the elastic behavior of arteries. Hypertension. 2003;41:1180–1182.
Grace F, Sculthorpe N, Baker J, et al. Blood pressure and rate pressure product response in males using high-dose anabolic androgenic steroids (AAS). J Sci Med Sport. 2003;6:307–312.
Graham MR, Grace FM, Boobier W, et al. Homocysteine induced cardiovascular events: a consequence of long term anabolic-androgenic steroid (AAS) abuse. Br J Sports Med. 2006;40:644–648.
Greenberg S, George WR, Kadowitz PJ, et al. Androgen-induced enhancement of vascular reactivity. Can J Physiol Pharmacol. 1974;52:14–22.
Grollman A, Harrison TR, Williams JR Jr. The effect of various sterol derivatives on the blood pressure of the rat. J Pharmacol Exp Ther. 1940;69:149–155.
Güneş Y, Erbaş C, Okuyan E, et al. Myocardial infarction with intracoronary thrombus induced by anabolic steroids. Anatolian J Cardiol. 2004;4:357–358.
Haffner SM, Kushwaha RS, Foster DM, et al. Studies on the metabolic mechanism of reduced high density lipoproteins during anabolic steroid therapy. Metabolism. 1983;32:413–420.
Halvorsen S, Thorsby PM, Haug E (2004) Acute myocardial infarction in a young man who had been using androgenic anabolic steroids. Tidsskr Nor Lægeforen 124:170–172. Norwegian
Hartgens F, Kuipers H, Wijnen JAG, et al. Body composition, cardiovascular risk factors and liver function in long term androgenic-anabolic steroids using bodybuilders three months after drug withdrawal. Int J Sports Med. 1996;17:429–433.
Hartgens F, Cheriex EC, Kuipers H. Prospective echocardiographic assessment of androgenic-anabolic steroids effects on cardiac structure and function in strength athletes. Int J Sports Med. 2003;24:344–351.
Hartgens F, Rietjens G, Keizer HA, et al. Effects of androgenic-anabolic steroids on apolipoproteins and lipoprotein (a). Br J Sports Med. 2004;38:253–259.
Hausmann R, Hammer S, Betz P. Performance enhancing drugs (doping agents) and sudden death–a case report and review of the literature. Int J Legal Med. 1998;111:261–264.
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20, 536 high-risk individuals: a randomised placebo-controlled trial. Lancet. 2002;360:7–22.
Herman SM, Robinson JT, McCredie RJ, et al. Androgen deprivation is associated with enhanced endothelium-dependent dilatation in adult men. Arterioscler Thromb Vasc Biol. 1997;17:2004–2009.
Higham PD, Campbell RW. QT dispersion. Br Heart J. 1994;71:508–510.
Hoff JA, Chomka EV, Krainik AJ, et al. Age and gender distributions of coronary artery calcium detected by electron beam tomography in 35, 246 adults. Am J Cardiol. 2001;87:1335–1339.
Holma P. Effect of an anabolic steroid (metandienone) on central and peripheral blood flow in well-trained male athletes. Ann Clin Res. 1977;9:215–221.
Hourigan LA, Rainbird AJ, Dooris M (1998) Intracoronary stenting for acute myocardial infarction (AMI) in a 24-year-old man using anabolic androgenic steroids. Aust N Z Med 28:838–839
Huie MJ. An acute myocardial infarction occurring in an anabolic steroid user. Med Sci Sports Exerc. 1994;26:408–413.
Hurley BF, Seals DR, Hagberg JM, et al. High-density-lipoprotein cholesterol in bodybuilders v powerlifters. Negative effects of androgen use. JAMA. 1984;252:507–513.
Jacobs DR Jr, Mebane IL, Bangdiwala SI, et al. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the Lipid Research Clinics Prevalence Study. Am J Epidemiol. 1990;131:32–47.
Jaillard AS, Hommel M, Mallaret M. Venous sinus thrombosis associated with androgens in a healthy young man. Stroke. 1994;25(1):212–213.
Johnson M, Ramey E, Ramwell PW. Sex and age differences in human platelet aggregation. Nature. 1975;253:355–357.
Johnson M, Ramey E, Ramwell PW. Androgen-mediated sensitivity in platelet aggregation. Am J Physiol. 1977;232:H381–H385.
Kahn NN, Sinha AK, Spungen AM, et al. Effects of oxandrolone, an anabolic steroid, on hemostasis. Am J Hematol. 2006;81:95–100.
Kantor MA, Bianchini A, Bernier D, et al. Androgens reduce HDL2-cholesterol and increase hepatic triglyceride lipase activity. Med Sci Sports Exerc. 1985;17:462–465.
Karila TAM, Karjalainen JE, Mäntysaari MJ, et al. Anabolic androgenic steroids produce dose-dependent increase in left ventricular mass in power athletes, and this effect is potentiated by concomitant use of growth hormone. Int J Sports Med. 2003;24:337–343.
Kasikcioglu E, Kayserilioglu A, Oflaz H, et al. Aortic distensibility and left ventricular diastolic functions in endurance athletes. Int J Sports Med. 2005;26:165–170.
Kasikcioglu E, Oflaz H, Arslan A, et al. Aortic elastic properties in athletes using anabolic-androgenic steroids. Int J Cardiol. 2007;114:132–134.
Kasikcioglu E, Oflaz H, Umman B et al (2008) Androgenic anabolic steroids also impair right ventriculer function. Int J Cardiol 134(1):123–125
Katz FH, Roper EF. Testosterone effect on renin system in rats. Proc Soc Exp Biol Med. 1977;155:330–333.
Kennedy C. Myocardial infarction in association with misuse of anabolic steroids. Ulster Med J. 1993;63:174–176.
Kennedy MC, Lawrence C. Anabolic steroid abuse and cardiac death. Med J Aust. 1993;158:346–348.
Kinson GA, Layberry RA, Hébert B. Influences of anabolic androgens on cardiac growth and metabolism in the rat. Can J Physiol Pharmcol. 1991;69:1698–1704.
Kleiner SM, Calabrese LH, Fiedler KM, et al. Dietary influences on cardiovascular disease risk in anabolic steroid-using and nonusing bodybuilders. Am Coll Nutr. 1989;8:109–119.
Kluft C, Preston FE, Malia RG, et al. Stanozolol-induced changes in fibrinolysis and coagulation in healthy adults. Thromb Haemost. 1984;51:157–164.
Koenig H, Goldstone A, Lu CY (1982) Testosterone-mediated sexual dimorphism of the rodent heart. Ventricular lysosomes, mitochondria, and cell growth are modulated by androgens. Circ Res 50(6):782–787
Kondos GT, Hoff JA, Sevrukov A, et al. Electron-beam tomography coronary artery calcium and cardiac events: a 37-month follow-up of 5635 initially asymptomatic low- to intermediate-risk adults. Circulation. 2003;107:2571–2576.
Koschinsky ML. Lipoprotein(a) and atherosclerosis: new perspectives on the mechanism of action of an enigmatic lipoprotein. Curr Atheroscler Rep. 2005;7:389–395.
Kostner GM, Avogaro P, Cazzolato G, et al. Lipoprotein Lp(a) and the risk for myocardial infarction. Atherosclerosis. 1981;38:51–61.
Kouri EM, Pope HG Jr, Oliva PS. Changes in lipoprotein-lipid levels in normal men following administration of increasing doses of testosterone cypionate. Clin J Sport Med. 1996;6:152–157.
Krieg A, Scharhag J, Albers T, et al. Cardiac tissue doppler in steroid users. Int J Sports Med. 2007;28:638–643.
Kronenberg F, Kronenberg MF, Kiechl S, et al. Role of lipoprotein(a) and apolipoprotein(a) phenotype in atherogenesis: prospective results from the Bruneck study. Circulation. 1999;100:1154–1160.
Kuipers H, Wijnen JA, Hartgens F, et al. Influence of anabolic steroids on body composition, blood pressure, lipid profile and liver functions in body builders. Int J Sports Med. 1991;12:413–418.
Lane HA, Grace F, Smith JC, et al. Impaired vasoreactivity in bodybuilders using androgenic anabolic steroids. Eur J Clin Invest. 2006;36:483–488.
Laroche GP. Steroid anabolic drugs and arterial complications in an athlete–a case history. Angiology. 1990;41:964–969.
Lau DH, Stiles MK, John B, et al. Atrial fibrillation and anabolic steroid abuse. Int J Cardiol. 2007;117:e86–e87.
Lenders JW, Demacker PN, Vos JA, et al. Deleterious effects of anabolic steroids on serum lipoproteins, blood pressure, and liver function in amateur body builders. Int J Sports Med. 1988;9:19–23.
Lewington S, Clarke R, Qizibash N et al (2002) Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet 360:1903–1913. Erratum in: Lancet. 2003 Mar 22;361(9362):1060
Lewis HD Jr, Davis JW, Archibald DG, et al. Protective effects of aspirin against acute myocardial infarction and death in men with unstable angina. Results of a Veterans Administration Cooperative Study. N Engl J Med. 1983;309:396–403.
Liang MTC, Paulson DJ, Kopp SJ, et al. Effects of anabolic steroids and endurance exercise on cardiac performance. Int J Sports Med. 1993;14:324–329.
Liljeqvist S, Helldén A, Bergman U, et al. Pulmonary embolism associated with the use of anabolic steroids. Eur J Int Med. 2008;19:214–215.
Lowe GD. Hormone replacement therapy: prothrombotic vs. protective effects. Pathophysiol Haemost Thromb. 2002;32:329–332.
Luke JL, Farb A, Virmani R, et al. Sudden cardiac death during exercise in a weight lifter using anabolic androgenic steroids: pathological and toxicological findings. J Forensic Sci. 1990;35:1441–1447.
Lyngberg KK (1991) Myocardial infarction and death of a body builder after using anabolic steroids. Ugeskr Laeger 153:587–588. Danish
Mancia G, De Backer G, Dominiczak A, et al. 2007 Guidelines for the management of arterial hypertension: the task force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007;25:1105–1187.
Mänttäri M, Oikarinen L, Manninen V, et al. QT dispersion as a risk factor for sudden cardiac death and fatal myocardial infarction in a coronary risk population. Heart. 1997;78:268–272.
Mark PB, Watkins S, Dargie HJ. Cardiomyopathy induced by performance enhancing drugs in a competitive bodybuilder. Heart. 2005;91:888.
Marsh JD, Lehmann MH, Ritchie RH, et al. Androgen receptors mediate hypertrophy in cardiac myocytes. Circulation. 1998;98:256–261.
Mayet J, Shahi M, McGrath K, et al. Left ventricular hypertrophy and QT dispersion in hypertension. Hypertension. 1996;28:791–796.
McCarthy K, Tang ATM, Dalrymple-Hay MJR, et al. Ventricular thrombosis and systemic embolism in bodybuilders: etiology and management. Ann Thorac Surg. 2000;70:658–660.
McCredie RJ, McCrohon JA, Turner L, et al. Vascular reactivity is impaired in genetic females taking high-dose androgens. J Am Coll Cardiol. 1998;32:1331–1335.
McCrohon JA, Jessup W, Handelsman DJ, et al. Androgen exposure increases human monocyte adhesion to vascular endothelium and endothelial cell expression of vascular cell adhesion molecule-1. Circulation. 1999;99:2317–2322.
McCrohon JA, Death AK, Nakhla S, et al. Androgen receptor expression is greater in macrophages from male than from female donors. A sex difference with implications for atherogenesis. Circulation. 2000;101:224–226.
McKillop G, Todd IC, Ballantyne D. Increased left ventricular mass in a bodybuilder using anabolic steroids. Brit J Sports Med. 1986;20:151–152.
McNutt RA, Ferenchick GS, Kirlin PC, et al. Acute myocardial infarction in a 22-year old world class weight lifter using anabolic steroids. Am J Cardiol. 1988;62:164.
McQueen MJ, Hawken S, Wang X, et al. Lipids, lipoproteins, and apolipoproteins as risk markers of myocardial infarction in 52 countries (the INTERHEART study): a case-control study. Lancet. 2008;372:224–233.
Medras M, Tworowska U, Jozkow P, et al. Postoperative course and anabolic-androgenic steroid abuse–a case report. Anaesthesia. 2005;60:81–84.
Melchert RB, Welder AA. Cardiovascular effects of androgenic-anabolic steroids. Med Sci Sports Exerc. 1995;27:1252–1262.
Melchert RB, Harron TJ, Welder AA. The effect of anabolic-androgenic steroids on primary myocardial cell cultures. Med Sci Sports Exerc. 1992;24:206–212.
Menkis AH, Daniel JK, McKenzie FN, et al. Cardiac transplantation after myocardial infarction in a 24-year-old bodybuilder using anabolic steroids. Clin J Sport Med. 1991;1(2):138–140.
Ment J, Ludman PF. Coronary thrombus in a 23 year old anabolic steroid user. Heart. 2002;88(4):342.
Mewis C, Spyridopoulos I, Kühlkamp V, et al. Manifestation of severe coronary heart disease after anabolic drug abuse. Clin Cardiol. 1996;19:153–155.
Mitchell TL, Pippin JJ, Devers SM, et al. Age- and sex-based nomograms from coronary artery calcium scores as determined by electron beam computed tomography. Am J Cardiol. 2001;87(453–6):A6.
Mochizuki RM, Richter KJ. Cardiomyopathy and cerebrovascular accident associated with anabolic-androgenic steroid use. Physician Sports Med. 1988;16:109–114.
Moore LG, McMurtry IF, Reeves JT. Effects of sex hormones on cardiovascular and hematologic responses to chronic hypoxia in rats (40268). Proc Soc Exp Biol Med. 1978;158:658–662.
Morano I, Gerstner J, Rüegg JC, et al. Regulation of myosin heavy chain expression in the hearts of hypertensive rats by testosterone. Circ Res. 1990;66:1585–1590.
Nakao J, Change WC, Murota SI, et al. Testosterone inhibits prostacyclin production by rat aortic smooth muscle cells in culture. Atherosclerosis. 1981;39:203–209.
Nicholls SJ, Tuzcu EM, Sipahi I, et al. Statins, high-density lipoprotein cholesterol, and regression of coronary atherosclerosis. JAMA. 2007;297:499–508.
Nieminen MS, Rämö MP, Viitasalo M, et al. Serious cardiovascular side effects of large doses of anabolic steroids in weight lifters. Eur Heart J. 1996;17:1576–1583.
Nottin S, Nguyen L-D, Terbah M, et al. Cardiovascular effects of androgenic anabolic steroids in male bodybuilders determined by tissue doppler imaging. Am J Cardiol. 2006;97:912–915.
Nygård O, Nordrehaug JE, Refsum H, et al. Plasma homocysteine levels and mortality in patients with coronary artery disease. N Engl J Med. 1997;337:230–236.
O’Brien E, Sheridan J, O’Malley K. Dippers and non-dippers. Lancet. 1988;2(8607):397.
Palatini P, Penzo M, Racioppa A, et al. Clinical relevance of nighttime blood pressure and of daytime blood pressure variability. Arch Int Med. 1992;152:1855–1860.
Palatini P, Giada F, Garavelli G, et al. Cardiovascular effects of anabolic steroids in weight-trained subjects. J Clin Pharmacol. 1996;36:1132–1140.
Pawlowitzki IH, Diekstall P, Miny P, et al. Abnormal platelet function in Kallmann syndrome. Lancet. 1986;2(8499):166.
Pearson AC, Schiff M, Mrosek D, et al. Left ventricular diastolic function in weight lifters. Am J Cardiol. 1986;58:1254–1259.
Pedersen et al (1994) Randomised trial of cholesterol lowering in 4444 patients with coronary heart disease: the Scandinavian Simvastatin Survival Study (4S). Lancet 344:1383–1389
Pelliccia A, Maron BJ, Spataro A, et al. The upper limit of physiologic cardiac hypertrophy in highly trained elite athletes. N Engl J Med. 1991;324:295–301.
Pelliccia A, Spataro A, Caselli G, et al. Absence of left ventricular wall thickening in athletes engaged in intense power training. Am J Cardiol. 1993;72:1048–1054.
Pereira-Junior PP, Chaves EA, Costa-E-Sousa RH, et al. Cardiac autonomic dysfunction in rats chronically treated with anabolic steroid. Eur J Appl Physiol. 2006;96:487–494.
Perkiömäki JS, Ikäheimo MJ, Pikkujämsä SM, et al. Dispersion of the QT interval and autonomic modulation of heart rate in hypertensive men with and without left ventricular hypertrophy. Hypertension. 1996;28:16–21.
Pesola MK. Reversibility of the haemodynamic effects of anabolic steroids in rats. Eur J Appl Physiol. 1988;58:125–131.
Phillis BD, Abeywardena MY, Adams MJ, et al. Nandrolone potentiates arrhythmogenic effects of cardiac ischemia in the rat. Toxicol Sci. 2007;99:605–611.
Pilo R, Aharony D, Raz A. Testosterone potentiation of ionophore and ADP induced platelet aggregation: relationship to arachidonic acid metabolism. Thromb Haemost. 1981;46:538–542.
Pye M, Quinn AC, Cobbe SM. QT interval dispersion: a non-invasive marker of susceptibility to arrhythmia in patients with sustained ventricular arrhythmias? Br Heart J. 1994;71:511–514.
Rämö P, Kettunen R, Timisjärvi J, et al. Anabolic steroids alter the haemodynamic effects of endurance training on the canine left ventricle. Pflügers Arch. 1987;410:272–278.
Riebe D, Fernhall B, Thompson PD. The blood pressure response to exercise in anabolic steroid users. Med Sci Sports Exerc. 1992;24:633–637.
Rocha FL, Carmo EC, Roque FR, et al. Anabolic steroids induce cardiac renin-angiotensin system and impair the beneficial effects of aerobic training in rats. Am J Physiol Heart Circ Physiol. 2007;293:H3575–H3583.
Rosenblum WI, el-Sabban F, Nelson GH et al (1987) Effects in mice of testosterone and dihydrotestosterone on platelet aggregation in injured arterioles and ex vivo. Thromb Res 45:719–728
Ross R. The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature. 1993; 362:801–809.
Rumberger JA, Simons DB, Fitzpatrick LA, et al. Coronary artery calcium area by electron-beam computed tomography and coronary atherosclerotic plaque area. A histopathologic correlative study. Circulation. 1995;92:2157–2162.
Sachtleben TR, Berg KE, Elias BA. The effects of anabolic steroids on myocardial structure and cardiovascular fitness. Med Sci Sports Excers. 1993;25:1240–1245.
Sachtleben TR, Berg KE, Cheatham JP. Serum lipoprotein patterns in long-term anabolic steroid users. Res Q Exerc Sport. 1997;68:110–115.
Sader MA, Griffiths KA, McCredie RJ, et al. Androgenic anabolic steroids and arterial structure and function in male bodybuilders. J Am Coll Cardiol. 2001;37:224–230.
Sader MA, Griffiths KA, Skilton MR, et al. Physiological testosterone replacement and arterial endothelial function in men. Clin Endocrinol (Oxf). 2003;59:62–67.
Sahraian MA, Mottamedi M, Azimi AR, et al. Androgen-induced cerebral venous sinus thrombosis in a young body builder: case report. BMC Neurol. 2004;4:22.
Salke RC, Rowland TW, Burke EJ. Left ventricular size and function in body builders using anabolic steroids. Med Sci Sports Exerc. 1985;17:701–704.
Santamarina RD, Besocke AG, Romano LM, et al. Ischemic stroke related to anabolic abuse. Clin Neuropharmacol. 2008;31:80–85.
Santora LJ, Marin J, Vangrow J, et al. Coronary calcification in body builders using anabolic steroids. Prev Cardiol. 2006;9:198–201.
Shahidi NT. Androgens and erythropoiesis. N Engl J Med. 1973;289:72–80.
Shepherd J, Cobbe SM, Ford I, et al. Prevention of coronary heart disease with pravastatin in men with hypercholesterolemia. West of Scotland Coronary Prevention Study Group. N Engl J Med. 1995;333:1301–1307.
Shiozawa Z, Yamada H, Mabuchi C, et al. Superior sagittal sinus thrombosis associated with androgen therapy for hypoplastic anemia. Ann Neurol. 1982;12:578–580.
Singh AB, Hsia S, Alaupovic P, et al. The effects of varying doses of T on insulin sensitivity, plasma lipids, apolipoproteins, and C-reactive protein in healthy young men. J Clin Endocrinol Metab. 2002;87:136–143.
Small M, McArdle BM, Lowe GD, et al. The effect of intramuscular stanozolol on fibrinolysis and blood lipids. Thromb Res. 1982;28:27–36.
Small M, MacLean JA, McArdle BM, et al. Haemostatic effects of stanozolol in elderly medical patients. Thromb Res. 1984;35:353–358.
Stamler J, Wentworth D, Neaton JD. Is relationship between serum cholesterol and risk of premature death from coronary heart disease continuous and graded? Findings in 356, 222 primary screenees of the Multiple Risk Factor Intervention Trial (MRFIT). JAMA. 1986;256:2823–2828.
Stevens QEJ, Dickerman RD, McConathy WJ, et al. Aortic and mitral valve thickening with concentric left ventricular hypertrophy in an elite bodybuilder: a biochemical and/or physiological adaptation? Cardiology. 2002;98:159–161.
Stolt A, Karila T, Viitasalo M. QT interval and QT dispersion in endurance athletes and in power athletes using large doses of anabolic steroids. Am J Cardiol. 1999;84:364–366.
Sullivan ML, Martinez CM, Gallagher EJ. Atrial fibrillation and anabolic steroids. J Emerg Med. 1999;17:851–857.
Tagarakis CV, Bloch W, Hartmann G, et al. Anabolic steroids impair the exercise-induced growth of the cardiac capillary bed. Int J Sports Med. 2000;21:412–418.
Taggart HM, Applebaum-Bowden D, Haffner S, et al. Reduction in high density lipoproteins by anabolic steroid (stanozolol) therapy for postmenopausal osteoporosis. Metabolism. 1982;31:1147–1152.
Takala TES, Kiviluoma K, Kihlström M, et al. Effects of physical training, methandione and their combination on the lysosomal hydrolytic activities in dog heart. Int J Sports Med. 1992;13:52–55.
Teruel JL, Marcén R, Navarro JF, et al. Evolution of serum erythropoietin after androgen administration to hemodialysis patients: a prospective study. Nephron. 1995;70:282–286.
Thiblin I, Lindquist O, Rajs J. Cause and manner of death among users of anabolic androgenic steroids. J Forensic Sci. 2000;45:16–23.
Thompson PD, Cullinane EM, Sady SP, et al. Contrasting effects of testosterone and stanozolol on serum lipoprotein levels. JAMA. 1989;261:1165–1168.
Thompson PD, Sadaniantz A, Cullinane EM, et al. Left ventricular function is not impaired in weight-lifters who use anabolic steroids. J Am Coll Cardiol. 1992;19:278–282.
Tischer KH, Heyny-von Haussen R, Mall G, et al. Koronarthrombosen und -ektasien nach langjäriger Einname von anabolen Steroiden. Z Kardiol. 2003;92:326–331.
Tonstad S, Joakimsen O, Stensland-Bugge E, et al. Risk factors related to carotid intima-media thickness and plaque in children with familial hypercholesterolemia and control subjects. Arterioscler Thromb Vasc Biol. 1996;16:984–991.
Trifunovic B, Norton GR, Duffield MJ, et al. An androgenic steroid decreases left ventricular compliance in rats. Am J Physiol. 1995;268:H1096–H1105.
Urhausen A, Kindermann W. Sports-specific adaptations and differentiation of the athlete’s heart. Sports Med. 1999;28:237–244.
Urhausen A, Hölpes R, Kindermann W. One- and two-dimensional echocardiography in bodybuilders using anabolic steroids. Eur J Appl Physiol. 1989;58:633–640.
Urhausen A, Torsten A, Kindermann W. Reversibility of the effects on blood cells, lipids, liver function and hormones in former anabolic-androgenic steroid abusers. J Steroid Biochem Mol Biol. 2003;84(2–3):369–375.
Urhausen A, Albers T, Kindermann W. Are the cardiac effects of anabolic steroid abuse in strength athletes reversible? Heart. 2004;90:496–501.
Uzunova A, Ramey E, Ramwell PW. Effect of testosterone, sex and age on experimentally induced arterial thrombosis. Nature. 1976;261:712–713.
Uzunova AD, Ramey ER, Ramwell PW. Arachidonate-induced thrombosis in mice: effects of gender or testosterone and estradiol administration. Prostaglandins. 1977;13:995–1002.
van Guldener C, Stehouwer CD. Hyperhomocysteinemia, vascular pathology, and endothelial dysfunction. Semin Thromb Hemost. 2000;26:281–289.
Verdecchia P. Prognostic value of ambulatory blood pressure: current evidence and clinical implications. Hypertension. 2000;35(3):844–851.
Verheijen JH, Rijken DC, Chang GT. Modulation of rapid plasminogen activator inhibitor in plasma by stanozolol. Thromb Haemost. 1984;51:396–397.
Wagner D, Metzger R, Paul M, et al. Androgen dependence and tissue specificity of renin messenger RNA expression in mice. J Hypertens. 1990;8:45–52.
Webb OL, Laskarzewski PM, Glueck CJ. Severe depression of high-density lipoprotein cholesterol levels in weight lifters and body builders by self-administered exogenous testosterone and anabolic-androgenic steroids. Metabolism. 1984;33:971–975.
White AD, Folsom AR, Chambless LE, et al. Community surveillance of coronary heart disease in the Atherosclerosis Risk in Communities (ARIC) Study: methods and initial two years′ experience. J Clin Epidemiol. 1996;49:223–233.
Wilson JD. Androgen abuse by athletes. Endocr Rev. 1988;9:181–199.
Winter JH, Fenech A, Bennett B, et al. Prophylactic antithrombotic therapy with stanozolol in patients with familial antithrombin III deficiency. Br J Haematol. 1984;57:527–537.
Woodiwiss AJ, Trifunovic B, Philippides M, et al. Effects of an androgenic steroid on exercise-induced cardiac remodeling in rats. J Appl Physiol. 2000;2000(88):409–415.
Wysoczanski M, Rachko M, Bergmann SR. Acute myocardial infarction in a young man using anabolic steroids. Angiology. 2008;59(3):376–378.
Yeater R, Reed C, Ullrich I, et al. Resistance trained athletes using or not using anabolic steroids compared to runners: effects on cardiorespiratory variables, body composition, and plasma lipids. Br J Sports Med. 1996;30:11–14.
Yesalis CE, Kennedy NJ, Kopstein AN, et al. Anabolic-androgenic steroid use in the United States. JAMA. 1993;270(10):1217–1221.
Zaugg M, Jamali NZ, Lucchinetti E. Anabolic-androgenic steroids induce apoptotic cell death in adult rat ventricular myocytes. J Cell Physiol. 2001;187:90–95.
Zitzmann M, Brune M, Nieschlag E. Vascular reactivity in hypogonadal men is reduced by androgen substitution. J Clin Endocrinol Metab. 2002;87:5030–5037.
Zmuda JM, Fahrenbach MC, Younkin BT, et al. The effect of testosterone aromatization on high-density lipoprotein cholesterol level and postheparin lipolytic activity. Metabolism. 1993;42:446–450.
Zmuda JM, Bausserman LL, Maceroni D, et al. The effect of supraphysiologic doses of testosterone on fasting total homocysteine levels in normal men. Atherosclerosis. 1997;130:199–202.
Zmunda JM, Thompson PD, Dickenson R, et al. Testosterone decreases lipoprotein(a) in men. Am J Cardiol. 1996;77:1244–1247.
Zuliani U, Bernardini B, Catapano A. Effects of anabolic steroids, testosterone, and hgh on blood lipids and echocardiographic parameters in body builders. Int J Sports Med. 1989;10:62–66.
Acknowledgements
The editorial assistance of Signe T. Nøsterud is highly appreciated. We are indebted to Ms Birgit Skjervik for excellent assistance with graphics and artwork, and we warmly thank Professor Egil Haug for critical review of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Vanberg, P., Atar, D. (2010). Androgenic Anabolic Steroid Abuse and the Cardiovascular System. In: Thieme, D., Hemmersbach, P. (eds) Doping in Sports: Biochemical Principles, Effects and Analysis. Handbook of Experimental Pharmacology, vol 195. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-79088-4_18
Download citation
DOI: https://doi.org/10.1007/978-3-540-79088-4_18
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-79087-7
Online ISBN: 978-3-540-79088-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)