Abstract
Adenocarcinoma of the distal esophagus, gastric cardia, and upper gastric third are grouped in type I-III by the Siewert classification. This classification is based on the endoscopic localisation of the tumor center, and is the most important diagnostic tool to group these tumors. On a molecular level, there is currently no marker that would allow to differentiate the three different types. Furthermore, the Siewert classification was not uniformly used in the recent literature, making interpretation and generalization of these results difficult. However, several potential targets have been identified that may help to separate these tumors by molecular markers, and are summarized in this chapter.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Vascular Endothelial Growth Factor
- Esophageal Carcinoma
- Intestinal Metaplasia
- Gastric Cardia
- Cardia Cancer
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
5.1 Introduction
The incidence of cancer at the gastroesophageal junction is rising in the US and in Europe (Devesa et al. 1998). The increase of these junction tumors was accompanied by a simultaneous decrease of noncardia tumors of the stomach (Botterweck et al. 2000). A clinical classification of carcinomas of the gastroesophageal junction exists according to Siewert, distinguishing between type I (distal esophagus), type II (true cardia), and type III (subcardial tumors) (Siewert and Stein 1998). This classification is based on endoscopic appearance and defines the cardia as a zone of 2 cm at the proximal end of the longitudinal folds.
The clinical management of type I tumors includes, as for esophageal carcinomas, a transthoracic esophageal resection and a mediastinal and coeliacal lymphadenenectomy. Type II and III tumors are treated by abdominal, transhiatal extended gastrectomy with a D2 lymphadenenctomy (Stein et al. 2000; von Rahden et al. 2006).
Known prognostic factors are a complete (R0) resection and involvement of lymph nodes. Type I tumors metastasize to lymph node compartments in the mediastinum, whereas type II and III tumors spread mainly into the celiac compartment. A study with 145 patients found a significantly increased rate (24% vs. 7%) of micrometastasis in type II and III tumors compared with type I tumors (Mueller et al. 2000). A significant impact on survival for micrometastasis was observed in type I and II tumors in a series of 85 patients (Schurr et al. 2006).
5.2 Microsatelite Instability (MSI) and Loss of Heterozygosity (LOH)
By comparing MSI and LOH by genomic hybridization, a significant difference was found on locus 14q31–32.1. This mutation occured more often in Barrett-related adenocarcinoma than in cardia cancer (van Dekken et al. 1999). This result was not confirmed by a following study and many others did not succeed in demonstrating any significant differences by genomic hybridization (El-Rifai et al. 2001; Marsman et al. 2004; Menke-Pluymers et al. 1996; Weiss et al. 2003; Yanagi et al. 2000). A comparative analysis using microarrays showed some differences between the two types but concrete and reproducible results must follow (Chang et al. 2004).
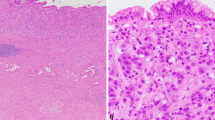
5.3 Difference in Phenotype on Histology and Immunohistochemistry
A prospective analysis of 1,346 patients observed intestinal metaplasia (Barrett’s esophagus) adjacent to the tumor in 76.9% of the specimens and in 97.4% after neoadjuvant chemotherapy. In contrast, only 2% of the type III tumors exhibited this growth pattern. Similarly, 81% of the type I but only 39% of the type III tumors had an intestinal growth pattern (Siewert et al. 2005) (Table 5.1).
Cytokeratin (CK) 7 and 20 are structural proteins of the cytoskeleton. Intestinal cells express CK20, lining the glandular surfaces and crypts. CK7 is a marker of differentiated intestinal cells. A typical CK20/CK7 expression pattern was observed in long-segment Barrett’s esophagus compared to the gastric cardia (Couvelard et al. 2001; Ormsby et al. 1999). This pattern was not seen in intestinal metaplasia in the stomach (Shen et al. 2002). The expression rate of the CK7/CK20 pattern may be lower in patients with a short-segment Barrett’s esophagus (Liu et al. 2005). For the distinction of benign lesions, the value of the CK7/CK20 expression pattern is still under discussion (Nurgalieva et al. 2007).
For the differentiation of junctional carcinomas, the literature is also controversial; a positive predictive value of 87% was found for the CK7/CK20 phenotype in 85 cases. This sharp edged difference is supported by other studies (Mattioli et al. 2007; Taniere et al. 2002). But in several publications, no important difference in CK7/20 staining between esophageal and cardia cancer was observed (Driessen et al. 2004; Flucke et al. 2003; van Lier et al. 2005).
Mucin peptide core antigens were identified as markers for the progression of dysplasia in Barrett’s esophagus (Arul et al. 2000). MUC1 and MUC6 helped to differentiate intestinal metaplasia originating from a Barrett’s esophagus only in some studies (Flucke et al. 2003; Glickman et al. 2003).
5.4 Differences in the Hallmarks of Cancer
Self-sufficiency in growth signals, insensitivity to antigrowth signals, evasion of apoptosis, limitless replicative potential, sustained angiogenesis, and tissue invasion are called the hallmark capabilities of cancer cells (Hanahan and Weinberg 2000). The tumor cell achieves these capabilities in a multistep process by mutation of genes leading to a gain or loss of function of gene products. Candidate genes for progression of Barrett’s esophagus to adenocarcinoma have been described (Fitzgerald 2006; Morales et al. 2002). In the following sections, we will discuss important candidate genes and factors that are involved and may be different between type I, II, and III tumors of the esophagogastric junction (Table 5.2).
5.5 Self-Sufficiency in Growth Signals
In gastric cancer, chronic infection with Helicobacter pylori (Hp) is a known risk factor for the development of gastric carcinoma. Chronic Hp infection induces mitogen-activated protein kinase (MAPK) activity and subsequently activates mitogenic pathways (Kacar et al. 2007). Type II esophagogastric carcinomas showed a significantly higher rate of gastric Hp infection, compared to type I carcinomas (Mattioli et al. 2007). In contrast, chronic gastric Hp infection was associated with a statistically reduced risk for esophageal carcinoma and was not associated with cardia cancer in other studies (Anderson et al. 2008; Kamangar et al. 2006; Ye et al. 2004).
In Barrett’s esophagus, repeated exposure to bile salts induces an increased proliferation (Kaur et al. 2000). Activation of proliferative signals by bile exposure involves inflammation-associated signaling pathways I kappaB kinases beta (IKK beta), tuberous sclerosis complex 1 (TSC1), and mammalian target of rapamycin (mTOR) downstream effector S6 kinase (S6K1) (Yen et al. 2008) or nuclear factor kappa B (Abdel-Latif et al. 2004) and c-myc (Tselepis et al. 2003). Bile reflux is also associated with intestinal metaplasia in the gastric cardia (Dixon et al. 2002). The localization of metaplasia may be related to the severity of reflux and the function of the lower esophageal sphincter (Csendes et al. 2002).
5.6 Insensitivity to Antigrowth Signals
Antigrowth pathways block proliferation or can induce a quiescent stage. Hypermethylation of the p16 gene, controlling the transition of the G2/S phase, is a mechanism of neoplastic progression in esophageal neoplasia (Bian et al. 2002; Klump et al. 1998). Loss of p16 staining on immunohistochemistry was also significantly more frequent in cardia compared to noncardia gastric cancer (Kim et al. 2005). Hypermethylation of the APC locus may also contribute to esophageal cancer progression (Eads et al. 2000). APC mutations were observed to be significantly more in cardia than in distal gastric carcinomas (Tajima et al. 2007). Studies comparing the differences among all three types of junctinal tumors are lacking.
5.7 Evasion of Apoptosis
An important cell cycle control mechanism and potential switch to apoptosis is mediated by p53 (Levine 1997). Mutation-positive status for p53 has been shown to be a marker of progression to malignancy and an independent prognostic factor for patients after complete resection of a Barrett’s carcinoma (Schneider et al. 1996, 2000). Mutations of p53 seem to occur in a similar frequency in distal esophageal and cardia carcinomas (Ireland et al. 2000). In more distal gastric carcinomas, this mutation is much less common (Flejou et al. 1999).
Increased expression of cyclooxygenase Type 2 (COX-2) is an important prognostic factor in Barrett’s carcinoma (Buskens et al. 2002; Wilson et al. 1998). This expression was significantly weaker in cardia carcinoma than in the distal esophagus (Buskens et al. 2003; Marsman et al. 2004).
The enzyme 15-Lipoxygnase (15-LOX-1) showed a decreased expression in esophageal carcinoma. An upregulation of the enzyme and induction of apoptosis by NSAIDs could be demonstrated in vitro (Shureiqi et al. 2001). In gastric carcinoma cells, inhibition of 15-LOX-1 also induced apoptosis by upregulation of the enzyme (Wu et al. 2003).
5.8 Limitless Replicative Potential
Normal cells lack telomerase, the enzyme required to replicate the last 50–200 basepairs of the genome. Thus, every replication cycle shortens this region, finally inducing a growth-arrested G0 stage. Most human cancer cells reactivate telomerase; this was also observed in esophageal adenocarcinoma (Morales et al. 1998) and in gastric carcinomas (Gulmann et al. 2005). No difference was observed for the expression in both types of cancers and a diagnostic value seems improbable as this mutation occurs early in carcinogenesis (Barclay et al. 2005).
5.9 Sustained Angiogenesis
Expression of vascular endothelial growth factor (VEGF) is an essential and early step in the carcinogenesis of Barrett’s adenocarcinoma (Auvinen et al. 2002; Couvelard et al. 2000). This was also shown for early gastric cancer (Cabuk et al. 2007). Expression of VEGF was a marker of progression and had a prognostic impact on disease free survival and overall survival in patients with gastric cancer (Kolev et al. 2007). There is a correlation of COX-2 expression and VEGF. Inhibition of COX-2 resulted in a decreased lymphangiogenesis in an experimental model (Iwata et al. 2007).
5.10 Tissue Invasion
The glycoprotein e-cadherin on the cell surface mediates the anchoring of cells via intracellular catenins and the actin cytoskeleton. Significant reduction of e-cadherin expression is a step in the dysplasia-adenocarcinoma sequence of Barrett’s esophagus (Bailey et al. 1998). Beta-catenin plays a structural role by binding to cadherins at the intracellular cell surface. It also has a role in downstream signaling by the wnt pathway and mediates transcriptional activation in a complex with lymphoid enhancer factor/T cell factor (Lef/Tcf) (Novak and Dedhar 1999). One study showed a significantly increased nuclear accumulation of beta-catenin in patients with esophageal adenocarcinoma, compared to patients with gastric cardia cancer (Marsman et al. 2004).
5.11 Conclusion
The anatomical classification by Siewert is safe and easily applicable and translates in a different surgical strategy for type I compared to type II and III carcinomas. The classification is nowadays widely, but not uniformly used. This makes interpretation of some results difficult.
Two major risk factors are identified for the development of adenocarcinoma in the gastroesophageal region: Gastroesophageal reflux and Hp infection. Gastroesophageal reflux has clear association with Barrett’s carcinoma, the association with cardia carcinoma is only suspected. For gastric adenocarcinoma – and type III tumors are considered as such – there is a clear association with chronic Hp infection. This association seems less probable for type II carcinomas.
At the moment, the literature fails to show a clearcut molecular differentiation between the three types. Differences between distal esophageal (type I) and gastric (type III) carcinomas are partially established. These genes include p16 and p53. Cardia carcinomas (type II) differ from type I tumors in the expression of COX-2 and from type III tumors in APC mutational status.
Immunohistochemical discrimination by cytokeratin (CK7 and CK20) or mucin phenotype is considered to be controversial, although some studies showed promising results.
Further molecular differentiation of the three tumor types is mandatory and should follow a uniform classification.
References
Abdel-Latif MM, O’Riordan J, Windle HJ, Carton E, Ravi N, Kelleher D, Reynolds JV (2004) NF-kappaB activation in esophageal adenocarcinoma: relationship to Barrett’s metaplasia, survival, and response to neoadjuvant chemoradiotherapy. Ann Surg 239:491–500
Anderson LA, Murphy SJ, Johnston BT, Watson RGP, Ferguson HR, Bamford KB, Ghazy A, McCarron P, McGuigan J, Reynolds JV et al (2008) Relationship between Helicobacter pylori infection and gastric atrophy and the stages of the oesophageal inflammation, metaplasia, adenocarcinoma sequence: results from the FINBAR case-control study. Gut 57:734–739
Arul GS, Moorghen M, Myerscough N, Alderson DA, Spicer RD, Corfield AP (2000) Mucin gene expression in Barrett’s oesophagus: an in situ hybridisation and immunohistochemical study. Gut 47:753–761
Auvinen MI, Sihvo EI, Ruohtula T, Salminen JT, Koivistoinen A, Siivola P, Ronnholm R, Ramo JO, Bergman M, Salo JA (2002) Incipient angiogenesis in Barrett’s epithelium and lymphangiogenesis in Barrett’s adenocarcinoma. J Clin Oncol 20:2971–2979
Bailey T, Biddlestone L, Shepherd N, Barr H, Warner P, Jankowski J (1998) Altered cadherin and catenin complexes in the Barrett’s esophagus-dysplasia-adenocarcinoma sequence: correlation with disease progression and dedifferentiation. Am J Pathol 152:135–144
Barclay JY, Morris A, Nwokolo CU (2005) Telomerase, hTERT and splice variants in Barrett’s oesophagus and oesophageal adenocarcinoma. Eur J Gastroenterol Hepatol 17:221–227
Bian YS, Osterheld MC, Fontolliet C, Bosman FT, Benhattar J (2002) p16 inactivation by methylation of the CDKN2A promoter occurs early during neoplastic progression in Barrett’s esophagus. Gastroenterology 122:1113–1121
Botterweck AA, Schouten LJ, Volovics A, Dorant E, van Den Brandt PA (2000) Trends in incidence of adenocarcinoma of the oesophagus and gastric cardia in ten European countries. Int J Epidemiol 29:645–654
Buskens CJ, Sivula A, van Rees BP, Haglund C, Offerhaus GJ, van Lanschot JJ, Ristimaki A (2003) Comparison of cyclooxygenase 2 expression in adenocarcinomas of the gastric cardia and distal oesophagus. Gut 52:1678–1683
Buskens CJ, Van Rees BP, Sivula A, Reitsma JB, Haglund C, Bosma PJ, Offerhaus GJ, Van Lanschot JJ, Ristimaki A (2002) Prognostic significance of elevated cyclooxygenase 2 expression in patients with adenocarcinoma of the esophagus. Gastroenterology 122:1800–1807
Cabuk D, Basaran G, Celikel C, Dane F, Yumuk PF, Iyikesici MS, Ekenel M, Turhal NS (2007) Vascular endothelial growth factor, hypoxia-inducible factor 1 alpha and CD34 expressions in early-stage gastric tumors: relationship with pathological factors and prognostic impact on survival. Oncology 72:111–117
Chang Y, Gong J, Liu B, Zhang J, Dai F (2004) Gene expression profiling in Barrett’s esophagus and cardia intestinal metaplasia: a comparative analysis using cDNA microarray. World J Gastroenterol 10:3194–3196
Couvelard A, Cauvin JM, Goldfain D, Rotenberg A, Robaszkiewicz M, Flejou JF (2001) Cytokeratin immunoreactivity of intestinal metaplasia at normal oesophagogastric junction indicates its aetiology. Gut 49:761–766
Couvelard A, Paraf F, Gratio V, Scoazec JY, Henin D, Degott C, Flejou JF (2000) Angiogenesis in the neoplastic sequence of Barrett’s oesophagus. Correlation with VEGF expression. J Pathol 192:14–18
Csendes A, Smok G, Quiroz J, Burdiles P, Rojas J, Castro C, Henriquez A (2002) Clinical, endoscopic, and functional studies in 408 patients with Barrett’s esophagus, compared to 174 cases of intestinal metaplasia of the cardia. Am J Gastroenterol 97:554–560
Devesa SS, Blot WJ, Fraumeni JF Jr (1998) Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer 83:2049–2053
Dixon MF, Mapstone NP, Neville PM, Moayyedi P, Axon ATR (2002) Bile reflux gastritis and intestinal metaplasia at the cardia. Gut 51:351–355
Driessen A, Nafteux P, Lerut T, Van Raemdonck D, De Leyn P, Filez L, Penninckx F, Geboes K, Ectors N (2004) Identical cytokeratin expression pattern CK7+/CK20- in esophageal and cardiac cancer: etiopathological and clinical implications. Mod Pathol 17:49–55
Eads CA, Lord RV, Kurumboor SK, Wickramasinghe K, Skinner ML, Long TI, Peters JH, DeMeester TR, Danenberg KD, Danenberg PV et al (2000) Fields of aberrant CpG island hypermethylation in Barrett’s esophagus and associated adenocarcinoma. Cancer Res 60:5021–5026
El-Rifai W, Frierson HF Jr, Moskaluk CA, Harper JC, Petroni GR, Bissonette EA, Jones DR, Knuutila S, Powell SM (2001) Genetic differences between adenocarcinomas arising in Barrett’s esophagus and gastric mucosa. Gastroenterology 121:592–598
Fitzgerald RC (2006) Molecular basis of Barrett’s oesophagus and oesophageal adenocarcinoma. Gut 55:1810–1820
Flejou JF, Gratio V, Muzeau F, Hamelin R (1999) p53 abnormalities in adenocarcinoma of the gastric cardia and antrum. Mol Pathol 52:263–268
Flucke U, Steinborn E, Dries V, Monig SP, Schneider PM, Thiele J, Holscher AH, Dienes HP, Baldus SE (2003) Immunoreactivity of cytokeratins (CK7, CK20) and mucin peptide core antigens (MUC1, MUC2, MUC5AC) in adenocarcinomas, normal and metaplastic tissues of the distal oesophagus, oesophago-gastric junction and proximal stomach. Histopathology 43:127–134
Glickman JN, Shahsafaei A, Odze RD (2003) Mucin core peptide expression can help differentiate Barrett’s esophagus from intestinal metaplasia of the stomach. Am J Surg Pathol 27:1357–1365
Gulmann C, Lantuejoul S, Grace A, Leader M, Patchett S, Kay E (2005) Telomerase activity in proximal and distal gastric neoplastic and preneoplastic lesions using immunohistochemical detection of hTERT. Dig Liver Dis 37:439–445
Hanahan D, Weinberg RA (2000) The hallmarks of cancer. Cell 100:57–70
Ireland AP, Shibata DK, Chandrasoma P, Lord RV, Peters JH, DeMeester TR (2000) Clinical significance of p53 mutations in adenocarcinoma of the esophagus and cardia. Ann Surg 231:179–187
Iwata C, Kano MR, Komuro A, Oka M, Kiyono K, Johansson E, Morishita Y, Yashiro M, Hirakawa K, Kaminishi M et al (2007) Inhibition of cyclooxygenase-2 suppresses lymph node metastasis via reduction of lymphangiogenesis. Cancer Res 67:10181–10189
Kacar F, Meteoglu I, Yasa H, Levi E (2007) Helicobacter pylori-induced changes in the gastric mucosa are associated with mitogen-activated protein kinase (MAPK) activation. Appl Immunohistochem Mol Morphol 15:224–228
Kamangar F, Dawsey SM, Blaser MJ, Perez-Perez GI, Pietinen P, Newschaffer CJ, Abnet CC, Albanes D, Virtamo J, Taylor PR (2006) Opposing risks of gastric cardia and noncardia gastric adenocarcinomas associated with Helicobacter pylori seropositivity. J Natl Cancer Inst 98:1445–1452
Kaur BS, Ouatu-Lascar R, Omary MB, Triadafilopoulos G (2000) Bile salts induce or blunt cell proliferation in Barrett’s esophagus in an acid-dependent fashion. Am J Physiol Gastrointest Liver Physiol 278:G1000–G1009
Kim MA, Lee HS, Yang HK, Kim WH (2005) Clinicopathologic and protein expression differences between cardia carcinoma and noncardia carcinoma of the stomach. Cancer 103:1439–1446
Klump B, Hsieh CJ, Holzmann K, Gregor M, Porschen R (1998) Hypermethylation of the CDKN2/p16 promoter during neoplastic progression in Barrett’s esophagus. Gastroenterology 115:1381–1386
Kolev Y, Uetake H, Iida S, Ishikawa T, Kawano T, Sugihara K (2007) Prognostic significance of VEGF expression in correlation with COX-2, microvessel density, and clinicopathological characteristics in human gastric carcinoma. Ann Surg Oncol 14:2738–2747
Levine AJ (1997) p53, the cellular gatekeeper for growth and division. Cell 88:323–331
Liu GS, Gong J, Cheng P, Zhang J, Chang Y, Qiang L (2005) Distinction between short-segment Barrett’s esophageal and cardiac intestinal metaplasia. World J Gastroenterol 11:6360–6365
Marsman WA, Birjmohun RS, van Rees BP, Caspers E, Johan G, Offerhaus A, Bosma PJ, Jan J, van Lanschot B (2004) Loss of heterozygosity and immunohistochemistry of adenocarcinomas of the esophagus and gastric cardia. Clin Cancer Res 10:8479–8485
Mattioli S, Ruffato A, Di Simone MP, Corti B, D’Errico A, Lugaresi ML, Mattioli B, D’Ovidio F (2007) Immunopathological patterns of the stomach in adenocarcinoma of the esophagus, cardia, and gastric antrum: gastric profiles in Siewert type I and II tumors. Ann Thorac Surg 83:1814–1819
Menke-Pluymers MB, van Drunen E, Vissers KJ, Mulder AH, Tilanus HW, Hagemeijer A (1996) Cytogenetic analysis of Barrett’s mucosa and adenocarcinoma of the distal esophagus and cardia. Cancer Genet Cytogenet 90:109–117
Morales CP, Lee EL, Shay JW (1998) In situ hybridization for the detection of telomerase RNA in the progression from Barrett’s esophagus to esophageal adenocarcinoma. Cancer 83:652–659
Morales CP, Souza RF, Spechler SJ (2002) Hallmarks of cancer progression in Barrett’s oesophagus. Lancet 360:1587–1589
Mueller JD, Stein HJ, Oyang T, Natsugoe S, Feith M, Werner M, Rudiger Siewert J (2000) Frequency and clinical impact of lymph node micrometastasis and tumor cell microinvolvement in patients with adenocarcinoma of the esophagogastric junction. Cancer 89:1874–1882
Novak A, Dedhar S (1999) Signaling through beta-catenin and Lef/Tcf. Cell Mol Life Sci 56:523–537
Nurgalieva Z, Lowrey A, El-Serag HB (2007) The use of cytokeratin stain to distinguish Barrett’s esophagus from contiguous tissues: a systematic review. Dig Dis Sci 52:1345–1354
Ormsby AH, Goldblum JR, Rice TW, Richter JE, Falk GW, Vaezi MF, Gramlich TL (1999) Cytokeratin subsets can reliably distinguish Barrett’s esophagus from intestinal metaplasia of the stomach. Hum Pathol 30:288–294
Schneider PM, Casson AG, Levin B, Garewal HS, Hoelscher AH, Becker K, Dittler HJ, Cleary KR, Troster M, Siewert JR et al (1996) Mutations of p53 in Barrett’s esophagus and Barrett’s cancer: a prospective study of ninety-eight cases. J Thorac Cardiovasc Surg 111:323–331; discussion 331–323
Schneider PM, Stoeltzing O, Roth JA, Hoelscher AH, Wegerer S, Mizumoto S, Becker K, Dittler HJ, Fink U, Siewert JR (2000) P53 mutational status improves estimation of prognosis in patients with curatively resected adenocarcinoma in Barrett’s esophagus. Clin Cancer Res 6:3153–3158
Schurr PG, Yekebas EF, Kaifi JT, Lasch S, Strate T, Kutup A, Cataldegirmen G, Bubenheim M, Pantel K, Izbicki JR (2006) Lymphatic spread and microinvolvement in adenocarcinoma of the esophago-gastric junction. J Surg Oncol 94:307–315
Shen B, Ormsby AH, Shen C, Dumot JA, Shao YW, Bevins CL, Gramlich TL (2002) Cytokeratin expression patterns in noncardia, intestinal metaplasia-associated gastric adenocarcinoma: implication for the evaluation of intestinal metaplasia and tumors at the esophagogastric junction. Cancer 94:820–831
Shureiqi I, Xu X, Chen D, Lotan R, Morris JS, Fischer SM, Lippman SM (2001) Nonsteroidal anti-inflammatory drugs induce apoptosis in esophageal cancer cells by restoring 15-lipoxygenase-1 expression. Cancer Res 61:4879–4884
Siewert JR, Feith M, Stein HJ (2005) Biologic and clinical variations of adenocarcinoma at the esophago-gastric junction: relevance of a topographic-anatomic subclassification. J Surg Oncol 90:139–146; discussion 146
Siewert JR, Stein HJ (1998) Classification of adenocarcinoma of the oesophagogastric junction. Br J Surg 85:1457–1459
Stein HJ, Feith M, Siewert JR (2000) Cancer of the esophagogastric junction. Surg Oncol 9:35–41
Tajima Y, Yamazaki K, Makino R, Nishino N, Masuda Y, Aoki S, Kato M, Morohara K, Kusano M (2007) Differences in the histological findings, phenotypic marker expressions and genetic alterations between adenocarcinoma of the gastric cardia and distal stomach. Br J Cancer 96:631–638
Taniere P, Borghi-Scoazec G, Saurin JC, Lombard-Bohas C, Boulez J, Berger F, Hainaut P, Scoazec JY (2002) Cytokeratin expression in adenocarcinomas of the esophagogastric junction: a comparative study of adenocarcinomas of the distal esophagus and of the proximal stomach. Am J Surg Pathol 26:1213–1221
Tselepis C, Morris CD, Wakelin D, Hardy R, Perry I, Luong QT, Harper E, Harrison R, Attwood SE, Jankowski JA (2003) Upregulation of the oncogene c-myc in Barrett’s adenocarcinoma: induction of c-myc by acidified bile acid in vitro. Gut 52:174–180
van Dekken H, Geelen E, Dinjens WN, Wijnhoven BP, Tilanus HW, Tanke HJ, Rosenberg C (1999) Comparative genomic hybridization of cancer of the gastroesophageal junction: deletion of 14Q31-32.1 discriminates between esophageal (Barrett’s) and gastric cardia adenocarcinomas. Cancer Res 59:748–752
van Lier MG, Bomhof FJ, Leendertse I, Flens M, Balk AT, Loffeld RJ (2005) Cytokeratin phenotyping does not help in distinguishing oesophageal adenocarcinoma from cancer of the gastric cardia. J Clin Pathol 58:722–724
von Rahden BH, Stein HJ, Siewert JR (2006) Surgical management of esophagogastric junction tumors. World J Gastroenterol 12:6608–6613
Weiss MM, Kuipers EJ, Hermsen MA, van Grieken NC, Offerhaus J, Baak JP, Meuwissen SG, Meijer GA (2003) Barrett’s adenocarcinomas resemble adenocarcinomas of the gastric cardia in terms of chromosomal copy number changes, but relate to squamous cell carcinomas of the distal oesophagus with respect to the presence of high-level amplifications. J Pathol 199:157–165
Wilson KT, Fu S, Ramanujam KS, Meltzer SJ (1998) Increased expression of inducible nitric oxide synthase and cyclooxygenase-2 in Barrett’s esophagus and associated adenocarcinomas. Cancer Res 58:2929–2934
Wu J, Xia HHX, Tu SP, Fan DM, Lin MCM, Kung HF, Lam SK, Wong BCY (2003) 15-Lipoxygenase-1 mediates cyclooxygenase-2 inhibitor-induced apoptosis in gastric cancer. Carcinogenesis 24:243–247
Yanagi M, Keller G, Mueller J, Walch A, Werner M, Stein HJ, Siewert JR, Hofler H (2000) Comparison of loss of heterozygosity and microsatellite instability in adenocarcinomas of the distal esophagus and proximal stomach. Virchows Arch 437:605–610
Ye W, Held M, Lagergren J, Engstrand L, Blot WJ, McLaughlin JK, Nyren O (2004) Helicobacter pylori infection and gastric atrophy: risk of adenocarcinoma and squamous-cell carcinoma of the esophagus and adenocarcinoma of the gastric cardia. J Natl Cancer Inst 96:388–396
Yen C-J, Izzo JG, Lee D-F, Guha S, Wei Y, Wu T-T, Chen C-T, Kuo H-P, Hsu J-M, Sun H-L et al (2008). bile acid exposure up-regulates tuberous sclerosis complex 1/mammalian target of rapamycin pathway in Barrett’s-associated esophageal adenocarcinoma. Cancer Res 68:2632–2640
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2009 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Lehmann, K., Schneider, P.M. (2009). Differences in the Molecular Biology of Adenocarcinoma of the Esophagus, Gastric Cardia, and Upper Gastric Third. In: Schneider, P. (eds) Adenocarcinoma of the Esophagogastric Junction. Recent Results in Cancer Research, vol 182. Springer, Berlin, Heidelberg. https://doi.org/10.1007/978-3-540-70579-6_5
Download citation
DOI: https://doi.org/10.1007/978-3-540-70579-6_5
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-540-70578-9
Online ISBN: 978-3-540-70579-6
eBook Packages: MedicineMedicine (R0)