Abstract
Cutaneous fistulas, commonly found in association with skin lesions and gangrene, are a severe complication of SSc patients characterized by long-lasting vascular involvement. Local treatment of fistulas is challenging for nurses due to their clinical presentation and the early involvement of deep structures (bones, muscles, and tendons). Fistulas are often associated with infective complications and an increased risk of amputation.
Two cases of SSc patients with cutaneous fistulas have been successfully treated with the association of negative topical pressure (NTP) and split-thickness skin grafting. The placement of a silk thread (seton stitch) for fistulas in skin lesions associated with lymphedema of the legs facilitates the drainage of cavities and promotes healing.
Close monitoring of the ulcer and of its local and systemic symptoms is crucial in order to prevent the evolution of this severe complication. A drainage and a swab should always be obtained when the ulcer is deep, when the deep cutaneous tissue is involved, and when purulent material is abundant across the wound bed. Antiseptic and absorbent dressings are recommended for SSc ulcers complicated with fistulas.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
In patients with systemic sclerosis (SSc), the presence of fistulas, skin lesions, and gangrene is a complication associated with vascular involvement which requires prolonged treatment (over 1 year), sometimes evolving to amputation of the phalanx, finger, or limbs [1].
The common definition of “fistulas” is the “abnormal communication most commonly seen between two internal organs or between an internal organ and the surface of the body” [2]. In the skin, fistula is defined a fistulous tract communicating between an ulcer and an adjacent area or between an injury and the deeper layers of the skin. In these cases, the risk of an increase of the length and depth of the lesion is amplified due to the difficulty to assess the extent and to place a local antiseptic device. This may lead to complications such as the progressive infections of tissue that can affect the tendons, joints, and bones.
Two SSc patients with fistulas have been successfully treated with the association of negative topical pressure (NTP) and split-thickness skin grafting [1]. In both cases, the combination of the two therapies represented the last attempt before proceeding to amputation, while they were treated for a month of intravenous prostacyclins, oral antibiotics, and povidone-iodine ointment [1]. Table 9.1 shows the different uses of NTP .
The placement of a silk thread (seton stitch) for fistulas in skin lesions associated with lymphedema of the legs and complicated by comorbidity and associated with compression bandaging was proposed. This procedure facilitates the drainage of cavities and promotes healing, avoiding the surgical incision that has little benefit [3].
Prevention
A correct approach to prevent this complication should include close monitoring of the wound and planning a follow-up of the patient at least twice weekly by experienced staff. The main purpose is to promptly identify wound signs and symptoms that indicate a potential evolution to a fistula. The main changes of the characteristics of the lesion can be specific and nonspecific.
Specific Signs
-
1.
Appearance of satellite lesions and/or detachment of the surrounding tissue (Fig. 9.1)
-
2.
Depression and/or endowment of the wound edges (Fig. 9.2)
-
3.
Undermining margins assessed by the placement of a cannula or a surgical tool as an ideal environment for microbial growth (Figs. 9.3 and 9.4)
The lesion indicated by the letter “U” is the lesion appeared as first; the lesion indicated by the letter “u” appeared after, and it is correlated to the first. The presence of a darker area (circled in red) above the lesion “U” constitutes a potential signal of expansion of the infectious process (a). Systemic antibiotic therapy targeted, silver dressings, and close monitoring of the patient have averted this possibility (b)
Nonspecific Signs
-
1.
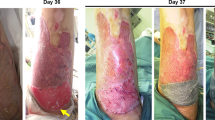
Spread in the local and/or spread in the surrounding tissue (Fig. 9.5)
-
2.
Marked redness around the wound (Fig. 9.5)
-
3.
Increase of necrotic tissue and/or occurrence of slough (Fig. 9.5)
-
4.
Increase in the size of the wound
-
5.
Purulent material
-
6.
Bad smell
One or more than one of these signs may be present but not yet determine the presence of a fistula and thus be only prognostic signs. However it is essential to monitor the evolution in association or not to the appearance of other symptoms reported by the patient:
-
Increase in pain that can become pulsating
-
Feeling of tension around the lesion
-
Impaired quality of life
Local Treatment
In the presence of a fistula, the presence of purulent material is always needed to verify, and drainage must be performed to collect a sample for analysis. Abscesses originating from deep tissue are frequent in the course of immunosuppressive therapies and comorbidity such as diabetes. In this case a broad-spectrum antibiotic therapy is mandatory to prevent deeper skin layer infection, and continue it as a preventive measure even if antibiogram is negative.
Local treatment can be summarized in seven steps:
-
1.
Wash the wound with saline solution using a 10 ml syringe for digital ulcers and a 20/30 ml syringe for the injuries to the lower limbs. Use a cannula 14Fr to ensure cleansing within the fistula. Be careful not to touch the bottom of the wound to avoid pain. The evaluation of the depth of the fistula may be performed later only after the application of local anesthetic.
-
2.
Disinfect the wound with non-cytotoxic products.
-
3.
Repeat the cleansing.
-
4.
Aspirate the abscess material and provide the laboratory a sample for analysis to start a specific antibiotic therapy [4].
-
5.
Proceed with the application of a local anesthetic.
-
6.
Evaluation of the fistula and of the edges of the wound with a cannula or by a surgical tool (Fig. 9.6). In case of undermining dead end, sterile saline can be injected within the fistula by measuring the amount in ml injected and removing it again immediately after. This allows, even if in a very empirical mode, to obtain a comparison parameter for the subsequent follow-up. Sometimes the fistula is extremely low, in the order of a few millimeters, so it is more suitable to assess the fistula through a cannula, with a marker to indicate the depth along the lumen and subsequently measuring with a ruler. In the presence of two adjacent lesions, inject the liquid into a wound using a syringe and cannula allows to confirm the presence of a communication between the two.
-
7.
Apply of a hydrofiber device with antiseptic properties. Medications containing silver ensure a slow and prolonged antiseptic action. These kinds of products are required when containment of exudate and protection of the perilesional skin is needed, thanks to its vertical absorption capacity [5]. In the present case, it is essential to employ devices able to absorb exudate and/or purulent materials and fill the fistula. Care should be taken not to overfill the fistula with the device to avoid pressure on the walls of the cavity and interactions between the dressing and the purulent material with transformation of the medication that acquires occluding characteristics. The placement of the dressing into the wound should be performed to ensure an easy removal, thus preventing residue deposit of dressings on the bottom of the lesion. For this reason, the products that have a structure that prevents it from flaking and loss within the fistula are largely preferred.
It is necessary to evaluate with a Doppler ultrasonography of the vessels of the lower limbs and an x-ray examination to document any possible involvement of the bone. When silver devices are used, x-ray should not be performed because they may interfere with the radiographic imaging.
Lesions due to calcinosis, according to the classification and staging of Amanzi [6], represent a threatening condition that predisposes the patient to fistula formation as through between the deposits of calcium formed in the deeper layers of skin surface. Alternatively they may determine the formation of skin lesions very close and often adjoining or potentially likely to become (Fig. 9.7). These kinds of ulcers require very long treatment times that can establish phenomena of self-maintenance with consequent chronicity of the lesion.
An x-ray examination can be a great help to know size, placement, and depth of the calcium deposits in the soft tissue in order to identify the areas most at risk of infectious processes with onset of abscesses and fistulas (Fig. 9.8).
Conclusions
Fistulas are complications that must be avoided, because it exposes the patient to a higher risk of bacterial infection. It can result in sepsis and interventions that may require amputation of the affected district. In SSc patients, ischemia and immunosuppressive therapies may contribute to facilitate the formation of fistulas.
References
Kajihara I, Jinnin M, Yamada S, Ichihara A, Makino T, Igata T, Masuguchi S, Fukushima S, Ihn H. Successful treatment of skin fistulas in systemic sclerosis patients with the combination of topical negative pressure therapy and split-thickness skin grafting. Mod Rheumatol. 2014;24(2):374–6. https://doi.org/10.3109/14397495.2013.854065.
European Wound Management Association (EWMA). Position document Topical negative pressure in wound management. London: MEP Ltd; 2007.
Lane TA, Shalhoub J, Franklin OJ. Seton sutures for leg ulcers associated fistulous tracts. Ann R Coll Surg Engl. 2010;92(6):533.
Dutronc H, Gobet A, Daucgy FA, Klotz R, Cazave C, Garcia C, Lafarie-Castet S, Fabre T, Dupon M. Stump infection after major lower-limb amputation: a 10-years retrospective. Med Mal Infect. 2013;43(12–12):456–60. study. https://doi.org/10.1016/j.medmal.2013.09.00.
Walker M, Metcalf D, Parsons D, Bowler P. A real-life clinical evaluation of a next-generation antimicrobial dressing on acute and chronic wounds. J Wound Care. 2015;24(1):11–22. https://doi.org/10.12968/jowc.2015.24.1.11.
Amanzi L, Fiori G, Galluccio F, Miniati I, Guiducci S, Conforti ML, Kaloudi O, Nacci F, Sacu O, Candelieri A, Moggi Pignone A, Rasero L, Conforti D, Matucci-Cerinic M. Digital ulcers in scleroderma: staging, characteristics and subsetting through observation of 1614 digital lesions. Rheumatology (Oxford). 2010;49(7):1374–82.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Piemonte, G., Braschi, F., Rasero, L. (2019). Fistulas. In: Matucci-Cerinic, M., Denton, C. (eds) Atlas of Ulcers in Systemic Sclerosis. Springer, Cham. https://doi.org/10.1007/978-3-319-98477-3_9
Download citation
DOI: https://doi.org/10.1007/978-3-319-98477-3_9
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98475-9
Online ISBN: 978-3-319-98477-3
eBook Packages: MedicineMedicine (R0)