Abstract
Digital ulcers (DU) have a major clinical impact in systemic sclerosis, and treatment and prevention are two logical and effective approaches to reduce the risk of complications and DU-related morbidity. Patient education, Raynaud’s phenomenon attacks control and identifications and treatment of potential risk factors for DU development are primary features of the above-mentioned approach. When this is not sufficient, different drug with shown evidences of efficacy in preventing or healing DU can be used, such as phosphodiesterase -5 inhibitors, endothelin-1 receptors antagonists and prostacyclin analogues, usually in combination with local topical treatment. Moreover, new approaches are also available, ranging from regenerative medicine to surgical procedures.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Digital ulcers
- Prevention
- Healing
- Drugs
- Treatment
- Endothelin receptor antagonists
- Phosphodiesterase 5 inhibitors
- Prostacyclin analogues
- Local topical treatment
- Regenerative medicine
Digital ulcers (DU) are common in systemic sclerosis (SSc) and have a major clinical impact. Whilst treating established ulcers is important, the most logical and effective approach to DU is to prevent their formation, as this will immediately remove the risk of severe complications and avoid the morbidity that is otherwise inevitable and substantial. Thus, the best therapeutic strategy for DU is prevention of their occurrence or recurrence, which is strategically linked to the frequency and severity of Raynaud’s phenomenon (RP) episodes . For this reason, it is necessary to achieve RP control and to educate patients regarding its non-pharmacological management [1]. Patients should be taught to avoid cold temperatures by means of proper garments and gloves, hats and heavy socks, whenever there is exposure to different external temperature (e.g., cold temperature in hot seasons due to sudden weather changes, conditionated air, refrigerators in a supermarket, etc.). Stress is also an impacting trigger for vasospasm in RP [2], requiring careful examination of the psychologic conditions of SSc patients and, if necessary, counseling or prescription for antidepressants or anxiolytics. Patients should also be taught to treat dry skin with simple topical lubricating products and emulsifying ointments, in order to prevent dry skin from cracking or fissuring. Patients should be suggested to avoid nicotine [3] and any substances that cause vasoconstriction (caffeine, cephalosporins, b-blockers), and whenever possible, also to avoid trauma to the digits, such as those related to repetitive hand actions (e.g. typing or manual work) [1].
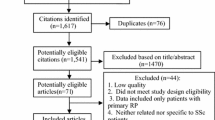
Given the impossibility to primarily prevent SSc and DU onset, DU secondary prevention begins with the identification and detection of risk factors. A recent systematic literature review identified male gender, early diffuse cutaneous SSc, in particular associated with anti-topoisomerase I antibody positivity and previous history of DU, as the predominant SSc-related features increasing the risk for DU appearance [4]. Moreover, circulating biomarkers studies identified high placental growth factor levels and low endothelial progenitor cells levels were associated with increased risk for future DU appearance, in particular for patients with history of previous digital ulcers [5]. Another study also identified Interleukin-6 levels as a predictor for future DU development, representing systemic inflammation [6]. Nail fold video capillaroscopy has an additional value in identifying patients at risk for vascular worsening: this was demonstrated for both qualitative evaluation with the late scleroderma pattern or evolution in the microvascular signs of vasculopathy [7] and for a composite videocapillaroscopic parameters score, named CSURI, derived from the combination of capillary number, maximum loop diameter and the number of giant capillaries, with a 2.9 score cut-off predicting high risk for DU development at 3 months [8].
Given these early high-impact disease-related features, the prompt initiation of background treatment could prevent new DU onset, which is strongly based on immunosuppression [9] and vasoactive-vasodilating treatments [10].
It is pivotal to understand how the concepts of healing and prevention are strongly linked and imbricated when taking care of SSc-DU patients. In fact, tertiary prevention starts once DU are manifested, in order to promote and determine their healing, avoid recurrency and positively influence patient reintroduction in daily social, working and family life. Therefore, a drug that helps DU healing can still also be practically considered as a preventive drug (see overview in Table 20.1).
Among vasoactive drugs, Bosentan, a dual endothelin-1 receptor antagonist, was approved for DU prevention after two randomized clinical trials (RCT). Its use determined a 30–48% reduction in new DU appearance at 16–24 weeks, more effectively in patients entering the trial with ≥3 DU, although no effect was shown in healing rates of already present DU [29, 30]. The positive short-term RCT results were also confirmed in various real-life studies: in particular, drug effects were evident also when the drug was primarily prescribed for pulmonary arterial hypertension treatment [18], and these effects maintained for at least 12 months [17] up to 3 years for both safety [15] and efficacy [14]. Moreover, Fanauchi et al. hypothesized possible extravascular effects on the drug, in particular antifibrotic properties [16].
The DU-preventing properties of anti-ET1 bosentan could be at least partially explained by its effect on microvasculature: in particular, it was shown to determine deremodeling effects of nailfold videocapillaroscopy changes, both alone [31] and when used in combination with prostanoids [32].
These results have not been reproduced for other members of this pharmacological class, such as macitentan [33] and ambrisentan. Conversely, ambrisentan has shown efficacy in DU healing, both in combination with iloprost [11] and alone: although a definite placebo-controlled study has not been fully performed, Chung et al. showed a complete healing of all baseline DUs in 14/20 patients [12].
Healing of DUs is possible and easier if early detected . Treatment should be started promptly, and, although pharmacologic systemic treatment is pivotal, it is not the only possible approach. DU treatment is mostly based on vasodilating agents, which take into account various pharmacological entities, characterized by different mechanisms of action, routes of administration and direct/indirect costs. Calcium-channel blockers are commonly used for the treatment of both primary and secondary RP and have been anecdotally used for treating DUs [34]. Intravenous prostaglandin analogue alprostadil has shown effect in treating SSc-DU [35] and is still commonly used, in particular, when other treatments are not easily available [36]. Prostacyclin analogues are frequently prescribed for treating pulmonary arterial hypertension, and, given the pathogenetic link with DU, their use has been exported to DU treatment. Intravenous iloprost, infused continuously for 6 h 0.5–2.0 ng/kg/min on 5 consecutive days, has been extensively used for RP and DU treatment: it was shown to determine DU healing in both open-label [21] and double-blinded [19] studies. Iloprost has shown to be comparably effective for both low and high dosages (0.5 and 2.0 ng/kg/min) [20] also characterized by long-term efficacy in preventing new DU appearance [37]. Recent data have also shown the possibility of avoiding hospitalization using a portable siring pump [38]. Among other prostacyclin analogues, treprostenil showed initial significant impact on DU healing in a small open-label pilot study [39] and the worsening of the DU status after its withdrawal [40]. A recent double-blind RCT did not show any significant effect in reducing DU net burden and impacting healing and prevention [41]. Similarly, oral beraprost and intravenous epoprostenol showed only a trend to improvement of DU prevention and healing, although data seem to be less supportive compared to iloprost [42, 43].
Phosphodiesterase 5 inhibitors are also commonly prescribed vasodilators in SSc-related RP and DU, in particular sildenafil, supporting initial promising results in case series [24, 25]. The SEDUCE study showed a trend for higher DU healing rate and a significantly lower DU number after 8 and 12 weeks of treatment with sildenafil vs placebo [26]. In this RCT, 28 patients received bosentan concomitantly with sildenafil: in this subgroup time to healing was shorter in the sildenafil group than in the placebo group [26]. From the same class, Tadalafil also proved some beneficial effect on RP and DU in two small double-blinded placebo-controlled studies [27, 28].
Among other IV treatments, intravenous administration of N-acetyl cysteine has shown beneficial effects on both SSc-related RP and DU, both in short-term [22] and long-term [23] treatment duration.
Combined with above-mentioned systemic treatments, local topical treatment is also crucial: in fact, a careful management is important to prevent further complications, i.e. infection, osteomyelitis and/or gangrene needing amputation. Among wound healing procedures, the use of different advanced dressings is supported and needs to be adapted to the changing DU status [44]. Vitamin E gel application, in combination with local wound healing procedures and dressings, was shown to significantly reduce time to DU healing [45].
The association of local and systemic treatment is of pivotal importance, and the combination of vasoactive and vasodilating drugs is frequently used to have higher impact on DU healing [46].
Case reports and case series also show promising positive effect of other medical or surgical treatments. Botulin A toxin injection, for example, is a minimally invasive and relatively safe local vasodilating treatment: it has shown beneficial effects in improving blood flow and RP and promoting DU healing in both a case series [47] and a single-blinded placebo-controlled study [48]. Beneficial effects were also demonstrated in a placebo-controlled double-blind trial of atorvastatin for 4 months, determining significant reduction in overall DU number and new DU development [13].
Regenerative medicine is also a possible approach for treating patients who are resistant to medical treatment. Autologous platelet-rich gel is a hemo-component containing numerous growth factors, which has been shown to determine improvement to healing in few case reports and an Italian case series [49]. Bone-marrow mononuclear cells have also been administered into the DU affected limb, improving pain and reducing risk of amputation/ischaemia recurrence [50, 51]. Autologous adipose-derived stromal vascular fraction and autologous adipose tissue-derived cells fractions are other source of regenerative factors: fat can be derived from patient body and then reinjected after an extraction procedure. Their use has been tested in some case series with interesting reports regarding DU number decrease [52] and reduced time to healing, also associated with pain reduction and increase in capillary number on nailfold videocapillaroscopy [53]. RCTs are currently ongoing to definitively support fat grafting use in clinical practice.
Among other medical options, tocilizumab [54], rituximab [55], recombinant human erythropoietin [56], hyperbaric oxygen therapy [57], vacuum-assisted closure therapy [58] and extracorporeal shock wave therapy [59] can be listed. Regarding surgical approaches, digital sympathectomy [60] and skin grafting [61] could be also considered but further studies are needed before being routinely performed. They can however be used for refractory DU cases or when conventional treatments are contraindicated.
Whatever the treatment choice, chronic wounds management requires full patient participation. It is therefore crucial to provide therapeutic educational interventions to increase and ensure treatment adherence and compliance. This starts from either DU-related [62] and procedures-related [63] pain control, as among the most patient perceived DU features. Patient collaboration is indeed a key aspect for achieving maximum results.
References
Herrick AL. Recent advances in the pathogenesis and management of Raynaud's phenomenon and digital ulcers. Curr Opin Rheumatol. 2016;28(6):577–85.
Raynaud's Treatment Study Investigators. Comparison of sustained-release nifedipine and temperature biofeedback for treatment of primary Raynaud phenomenon. Results from a randomized clinical trial with 1-year follow-up. Arch Intern Med. 2000;160(8):1101–8.
Caramaschi P, Martinelli N, Volpe A, et al. A score of risk factors associated with ischemic digital ulcers in patients affected by systemic sclerosis treated with iloprost. Clin Rheumatol. 2009;28(7):807–13.
Silva I, Almeida J, Vasconcelos C. A PRISMA-driven systematic review for predictive risk factors of digital ulcers in systemic sclerosis patients. Autoimmun Rev. 2015;14(2):140–52.
Avouac J, Meune C, Ruiz B, et al. Angiogenic biomarkers predict the occurrence of digital ulcers in systemic sclerosis. Ann Rheum Dis. 2012;71(3):394–9.
Alivernini S, De Santis M, Tolusso B, et al. Skin ulcers in systemic sclerosis: determinants of presence and predictive factors of healing. J Am Acad Dermatol. 2009;60(3):426–35.
Smith V, Riccieri V, Pizzorni C, et al. Nail fold capillaroscopy for prediction of novel future severe organ involvement in systemic sclerosis. J Rheumatol. 2013;40(12):2023–8.
Sebastiani M, Manfredi A, Vukatana G, et al. Predictive role of capillaroscopic skin ulcer risk index in systemic sclerosis: a multicentre validation study. Ann Rheum Dis. 2012;71(1):67–70.
Cappelli S, Bellando-Randone S, Guiducci S, et al. Is immunosuppressive therapy the anchor treatment to achieve remission in systemic sclerosis? Rheumatology (Oxford). 2014;53(6):975–87. Review
Guiducci S, Bellando Randone S, Bruni C, et al. Bosentan fosters microvascular de-remodelling in systemic sclerosis. Clin Rheumatol. 2012;31(12):1723–5.
Parisi S, Peroni CL, Laganà A, et al. Efficacy of ambrisentan in the treatment of digital ulcers in patients with systemic sclerosis: a preliminary study. Rheumatology (Oxford). 2013;52(6):1142–4.
Chung L, Ball K, Yaqub A, et al. Effect of the endothelin type A-selective endothelin receptor antagonist ambrisentan on digital ulcers in patients with systemic sclerosis: results of a prospective pilot study. J Am Acad Dermatol. 2014;71(2):400–1.
Abou-Raya A, Abou-Raya S, Helmii M. Statins: potentially useful in therapy of systemic sclerosis-related Raynaud's phenomenon and digital ulcers. J Rheumatol. 2008;35(9):1801–8.
Tsifetaki N, Botzoris V, Alamanos Y, et al. Bosentan for digital ulcers in patients with systemic sclerosis: a prospective 3-year followup study. J Rheumatol. 2009;36(7):1550–2.
García de la Peña-Lefebvre P, Rodríguez Rubio S, Valero Expósito M, et al. Long-term experience of bosentan for treating ulcers and healed ulcers in systemic sclerosis patients. Rheumatology (Oxford). 2008;47(4):464–6.
Funauchi M, Kishimoto K, Shimazu H, et al. Effects of bosentan on the skin lesions: an observational study from a single center in Japan. Rheumatol Int. 2009;29(7):769–75.
Roman Ivorra JA, Simeon CP, Alegre Sancho JJ, et al. Bosentan in clinical practice for treating digital and other ischemic ulcers in Spanish patients with systemic sclerosis: IBER-DU cohort study. J Rheumatol. 2011;38(8):1631–5.
Cozzi F, Pigatto E, Rizzo M, et al. Low occurrence of digital ulcers in scleroderma patients treated with bosentan for pulmonary arterial hypertension: a retrospective case-control study. Clin Rheumatol. 2013;32(5):679–83.
Wigley FM, Seibold JR, Wise RA, et al. Intravenous iloprost treatment of Raynaud's phenomenon and ischemic ulcers secondary to systemic sclerosis. J Rheumatol. 1992;19(9):1407–14.
Kawald A, Burmester GR, Huscher D, et al. Low versus high-dose iloprost therapy over 21 days in patients with secondary Raynaud's phenomenon and systemic sclerosis: a randomized, open, single-center study. J Rheumatol. 2008;35(9):1830–7.
Zachariae H, Halkier-Sørensen L, Bjerring P, et al. Treatment of ischaemic digital ulcers and prevention of gangrene with intravenous iloprost in systemic sclerosis. Acta Derm Venereol. 1996;76(3):236–8.
Sambo P, Amico D, Giacomelli R, et al. Intravenous N-acetylcysteine for treatment of Raynaud's phenomenon secondary to systemic sclerosis: a pilot study. J Rheumatol. 2001;28(10):2257–62.
Rosato E, Borghese F, Pisarri S, et al. The treatment with N-acetylcysteine of Raynaud's phenomenon and ischemic ulcers therapy in sclerodermic patients: a prospective observational study of 50 patients. Clin Rheumatol. 2009;28(12):1379–84.
Brueckner CS, Becker MO, Kroencke T, et al. Effect of sildenafil on digital ulcers in systemic sclerosis: analysis from a single centre pilot study. Ann Rheum Dis. 2010;69(8):1475–8.
Kumar U, Sankalp G, Sreenivas V, et al. Prospective, open-label, uncontrolled pilot study to study safety and efficacy of sildenafil in systemic sclerosis-related pulmonary artery hypertension and cutaneous vascular complications. Rheumatol Int. 2013;33(4):1047–52.
Hachulla E, Hatron PY, Carpentier P, et al. Efficacy of sildenafil on ischaemic digital ulcer healing in systemic sclerosis: the placebo-controlled SEDUCE study. Ann Rheum Dis. 2016;75(6):1009–15.
Agarwal V, Parasar G, Aman S, et al. Efficacy of Tadalafil in Raynaud’s Phenomenon Secondary to Systemic Sclerosis: A Double Blind Randomized Placebo Controlled Parallel Group Multicentric Study. Arthritis&Rheumatism. 2010;62(10):Supplement.
Shenoy PD, Kumar S, Jha LK, et al. Efficacy of tadalafil in secondary Raynaud's phenomenon resistant to vasodilator therapy: a double-blind randomized cross-over trial. Rheumatology (Oxford). 2010;49(12):2420–8.
Korn JH, Mayes M, Matucci Cerinic M, et al. Digital ulcers in systemic sclerosis: prevention by treatment with bosentan, an oral endothelin receptor antagonist. Arthritis Rheum. 2004;50(12):3985–93.
Matucci-Cerinic M, Denton CP, Furst DE, et al. Bosentan treatment of digital ulcers related to systemic sclerosis: results from the RAPIDS-2 randomised, double-blind, placebo-controlled trial. Ann Rheum Dis. 2011;70(1):32–8.
Guiducci S, Bellando Randone S, Bruni C, et al. Bosentan fosters microvascular de-remodelling in systemic sclerosis. Clin Rheumatol. 2012;31(12):1723–5.
Cutolo M, Zampogna G, Vremis L, et al. Long term effects of endothelin receptor antagonism on microvascular damage evaluated by nail fold capillaroscopic analysis in systemic sclerosis. J Rheumatol. 2013;40(1):40–5.
Khanna D, Denton CP, Merkel PA, et al. Effect of macitentan on the development of new ischemic digital ulcers in patients with systemic sclerosis: DUAL-1 and DUAL-2 randomized clinical trials. JAMA. 2016;315(18):1975–88.
Woo TY, Wong RC, Campbell JP, et al. Nifedipine in scleroderma ulcerations. Int J Dermatol. 1984 Dec;23(10):678–80.
Baron M, Skrinskas G, Urowitz MB, et al. Prostaglandin E1 therapy for digital ulcers in scleroderma. Can Med Assoc J. 1982;126(1):42–5.
Abuowda Y, Almeida RS, Oliveira AA, et al. Treatment of digital ulcers in systemic sclerosis: Case series study of thirteen patients and discussion on outcome. Rev Assoc Med Bras (1992). 2017;63(5):422–6.
Colaci M, Lumetti F, Giuggioli D, et al. Long-term treatment of scleroderma-related digital ulcers with iloprost: a cohort study. Clin Exp Rheumatol. 2017;35 Suppl 106(4):179–83.
Fraticelli P, Martino GP, Murri M, et al. A novel iloprost administration method with portable syringe pump for the treatment of acral ulcers and Raynaud's phenomenon in systemic sclerosis patients. A pilot study (ILOPORTA). Clin Exp Rheumatol. 2017;35 Suppl 106(4):173–8.
Chung L, Fiorentino D. A pilot trial of treprostinil for the treatment and prevention of digital ulcers in patients with systemic sclerosis. J Am Acad Dermatol. 2006;54(5):880–2.
Shah AA, Schiopu E, Chatterjee S, et al. The recurrence of digital ulcers in patients with systemic sclerosis after discontinuation of oral Treprostinil. J Rheumatol. 2016;43(9):1665–71.
Seibold R, Wigley FM, Schiopu E, et al. Digital ulcers in SSc treated with oral treprostinil: a randomized, double-blind, placebo-controlled study with open-label follow-up. J Scleroderma Relat Disord. 2017;2(1):42–9.
Cruz JE, Ward A, Anthony S, et al. Evidence for the use of epoprostenol to treat Raynaud's phenomenon with or without digital ulcers. Ann Pharmacother. 2016;50(12):1060–7.
Vayssairat M. Preventive effect of an oral prostacyclin analog, beraprost sodium, on digital necrosis in systemic sclerosis. French Microcirculation Society Multicenter Group for the Study of Vascular Acrosyndromes. J Rheumatol. 1999;26(10):2173–8.
Fujimoto M, Asano Y, Ishii T, et al. The wound/burn guidelines - 4: guidelines for the management of skin ulcers associated with connective tissue disease/vasculitis. J Dermatol. 2016;43(7):729–57.
Fiori G, Galluccio F, Braschi F, et al. Vitamin E gel reduces time of healing of digital ulcers in systemic sclerosis. Clin Exp Rheumatol. 2009;27(3 Suppl 54):51–4.
Kowal-Bielecka O, Fransen J, Avouac J, et al. Update of EULAR recommendations for the treatment of systemic sclerosis. Ann Rheum Dis. 2017;76(8):1327–39.
Motegi S, Yamada K, Toki S, et al. Beneficial effect of botulinum toxin A on Raynaud's phenomenon in Japanese patients with systemic sclerosis: a prospective, case series study. J Dermatol. 2016;43(1):56–62.
Motegi SI, Uehara A, Yamada K, et al. Efficacy of Botulinum Toxin B injection for Raynaud's Phenomenon and Digital Ulcers in Patients with Systemic Sclerosis. Acta Derm Venereol. 2017;97(7):843–50.
Giuggioli D, Colaci M, Manfredi A, et al. Platelet gel in the treatment of severe scleroderma skin ulcers. Rheumatol Int. 2012;32(9):2929–32.
Ishigatsubo Y, Ihata A, Kobayashi H, et al. Therapeutic angiogenesis in patients with systemic sclerosis by autologous transplantation of bone-marrow-derived cells. Mod Rheumatol. 2010;20(3):263–72.
Takagi G, Miyamoto M, Tara S, et al. Therapeutic vascular angiogenesis for intractable macroangiopathy-related digital ulcer in patients with systemic sclerosis: a pilot study. Rheumatology (Oxford). 2014;53(5):854–9.
Daumas A, Magalon J, Jouve E, et al. Long-term follow-up after autologous adipose-derived stromal vascular fraction injection into fingers in systemic sclerosis patients. Curr Res Transl Med. 2017;65(1):40–3.
Del Papa N, Di Luca G, Sambataro D, et al. Regional implantation of autologous adipose tissue-derived cells induces a prompt healing of long-lasting indolent digital ulcers in patients with systemic sclerosis. Cell Transplant. 2015;24(11):2297–305.
Fernandes das Neves M, Oliveira S, Amaral MC, et al. Treatment of systemic sclerosis with tocilizumab. Rheumatology (Oxford). 2015;54(2):371–2.
Khor CG, Chen XL, Lin TS, et al. Rituximab for refractory digital infarcts and ulcers in systemic sclerosis. Clin Rheumatol. 2014;33(7):1019–20.
Ferri C, Giuggioli D, Sebastiani M, Colaci M. Treatment of severe scleroderma skin ulcers with recombinant human erythropoietin. Clin Exp Dermatol. 2007;32(3):287–90.
Mirasoglu B, Bagli BS, Aktas S. Hyperbaric oxygen therapy for chronic ulcers in systemic sclerosis - case series. Int J Dermatol. 2017;56(6):636–40.
Pauling JD, Brown SJ, James J, et al. Vacuum-assisted closure therapy: a novel treatment for wound healing in systemic sclerosis. Rheumatology (Oxford). 2011;50(2):420–2.
Saito S, Tomonori I, Kenta I, et al. Extracorporeal shock wave therapy for digital ulcers associated with systemic sclerosis. J Scleroderma Relat Disord. 2016;1(2):181–5.
Chiou G, Crowe C, Suarez P, et al. Digital Sympathectomy in patients with scleroderma: an overview of the practice and referral patterns and perceptions of rheumatologists. Ann Plast Surg. 2015;75(6):637–43.
Barsotti S, Mattaliano V, d'Ascanio A, et al. Systemic sclerosis chronic ulcers: preliminary results of treatment with allogenic skin grafting in a cohort of Italian patients. Int Wound J. 2016;13(5):1050–1.
Giuggioli D, Manfredi A, Colaci M, et al. Oxycodone in the long-term treatment of chronic pain related to scleroderma skin ulcers. Pain Med. 2010;11(10):1500–3.
Braschi F, Bartoli F, Bruni C, et al. Lidocaine controls pain and allows safe wound bed preparation and debridement of digital ulcers in systemic sclerosis: a retrospective study. Clin Rheumatol. 2017;36(1):209–12.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Bruni, C., Bellando-Randone, S., Denton, C.P., Matucci-Cerinic, M. (2019). Ulcer Healing and Prevention in Systemic Sclerosis. In: Matucci-Cerinic, M., Denton, C. (eds) Atlas of Ulcers in Systemic Sclerosis. Springer, Cham. https://doi.org/10.1007/978-3-319-98477-3_20
Download citation
DOI: https://doi.org/10.1007/978-3-319-98477-3_20
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-98475-9
Online ISBN: 978-3-319-98477-3
eBook Packages: MedicineMedicine (R0)