Abstract
Rare lung diseases encompass a broad spectrum of conditions and affect an estimated 1.2–2.5 million people in North America and 1.5–3 million people in Europe. While individual rare lung diseases affect less than 1 in 2000 individuals, collectively they have a significant impact upon the population at large. Hence it is vital to understand firstly the epidemiology and subsequently the pathogenesis and clinical course of these disorders. Through a greater understanding of these aspects of disease, progress can be made in reducing symptoms, containing healthcare costs and utilizing resources efficiently. Furthermore, a greater understanding of the pathobiology of rare lung diseases can inform both the pathogenesis and management of more common pulmonary disorders.
In this chapter we review how epidemiological approaches and the utilization of patient registries has improved the knowledge and management of rare lung diseases. We further focus on the epidemiology of several of the more widely known rare pulmonary disorders, including idiopathic pulmonary fibrosis (IPF), cystic fibrosis (CF) and alpha-1 antitrypsin deficiency (AATD). To conclude we describe how patient advocacy groups and foundations have driven advances in research and management of ultra-rare lung diseases, namely, the major strides made in the management and understanding of lymphangioleiomyomatosis (LAM) and pulmonary alveolar proteinosis (PAP).
We conclude that the models used to study some of the rarest of diseases may be successfully adopted by other rare and common disease communities, leading to improved care and the possibility of novel therapeutic options.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Rare Lung Disease
- Cystic Fibrosis
- Alpha-1 Antitrypsin
- Lymphangioleiomyomatosis
- Pulmonary Alveolar Proteinosis
- Idiopathic Pulmonary Fibrosis
1 Introduction
Rare lung diseases are a group of conditions that individually affect fewer than 1 in 2000 persons [127]; or for the ultra-rare disorders, fewer than 1 in 2 million individuals [45]. Collectively, however, these disorders affect quite a large number of patients; estimated at 1.2–2.5 million individuals in North America [43] and 1.5–3 million people in Europe [78, 127]. It is therefore important to understand pathogeneses and epidemiology [72] of these disorders, in order to reduce human suffering, contain healthcare costs and maximize efficiency of resource utilization. In addition, research into rare diseases often provides valuable insights into the pathogenesis of more common disorders [90]. As an example, azithromycin was recently adopted as a prophylactic agent to prevent exacerbations in chronic obstructive pulmonary disease (COPD) [3], almost a decade after studies of this anti-inflammatory antibiotic were shown to be beneficial in cystic fibrosis (CF) [116].
In this chapter we will discuss the epidemiology of rare lung diseases, with a focus on some of the more common and widely known members, including idiopathic pulmonary fibrosis (IPF), CF and alpha-1 antitrypsin deficiency (AATD). We will review how epidemiological approaches and patient registries have improved the knowledge of these conditions, and how these methods may benefit rarer lung diseases. Finally we will describe how the efforts of patient advocacy groups and foundations have led to advances in two rare lung diseases, lymphangioleiomyomatosis (LAM) and pulmonary alveolar proteinosis (PAP).
2 Rare Lung Disease: Diagnostic and Classification Challenges
Classifying all rare lung disease together under one heading is problematic, as some conditions are relatively more common, such as CF or AATD, while other diseases are quite rare, such as PAP, LAM or Hermansky-Pudlak syndrome (HPS). In addition, there is substantial variation among diseases in clinical features and manifestations, including age of onset, patterns of extra-pulmonary involvement, mode of inheritance and prognosis. Some conditions are caused by monogenic mutations (AATD, CF) which are amenable to screening [14, 71, 126], facilitating earlier diagnosis and intervention. Other conditions are multifactorial and have an unknown genetic basis (e.g. lymphangiomatosis), which can result in diagnostic delays and difficulties with classification [32]. Symptoms of rare lung diseases may be mistaken for those of more common conditions [66] as often happens with AATD; a disorder which can present clinically as one of the most common chronic respiratory conditions (COPD) and, despite its high penetrance, can vary considerably depending on the exposure to external factors such as tobacco smoke [122].
The principle of parsimony does not necessarily apply to rare diseases, and applying Occam’s razor can be hazardous. For instance, the failure to realize that recurrent pneumothoraces may be due to LAM rather than primary spontaneous pneumothorax [54], may delay pleurodesis and place patients at risk of future morbidity. In cases where intervention has a clear impact on outcome, such as sirolimus treatment to slow progression in LAM, timely diagnosis is especially important to preserve lung function, limit unnecessary and invasive investigations and contain costs. Early referral to specialist centres for rare lung diseases can be helpful in this regard [42]. Correct coding and use of proper nomenclature impacts upon the ability to classify the epidemiology of these conditions [127], design appropriate clinical trials and optimise management.
3 Rare Disease Networks and Databases: Establishing Prevalence and Enabling Research
Estimates of the prevalence and incidence of rare disorders are made possible by the existence of networks, consortia and patient organisation alliances such as the National Institutes of Health Rare Diseases Clinical Research Network (NIH-RDCRN), European Organisation for Rare Diseases (EURODIS) and Orphanet. The prevalence of rare lung disease in Europe varies greatly, from 20 per 100,000 people for AATD to 0.15 per 100,000 people for HPS. The prevalence data of several rare lung diseases is listed in Table 24.1, gleaned from data obtained from Orphanet’s 2016 report, which is compiled through a systematic survey of published and online sources [98]. These data help establish a clear picture of the natural history of rare lung diseases, and facilitate clinical trials and standardised care, aimed at improving patient satisfaction and outcomes [127].
The RDCRN is made up of 22 research consortia and maintains an online registry that supports international multicentre studies [92]. The Rare Lung Diseases Consortium (RLDC) is part of this network, which itself consists of 29 US and 18 international clinics that contribute to both data collection and study recruitment, accelerate clinical research and improve medical care access for persons with rare lung diseases. The RLDC collaborates closely with several patient organisations including the LAM Foundation, PAP Foundation, Alpha-1 Foundation, HPS Network and Histiocytosis Association and others to provide educational resources and recruit for clinical trials. In rare lung disease research, the major obstacle to conducting a clinical trial is the small number of participants available for inclusion. The use of internet based communications by patient organisations is a novel and exciting method which has proven to be a useful strategy for trial recruitment [123]. Networks and patient registries increase the pool of patients available for research studies, and often include repositories for sample collection and distribution. (Tables 24.2 and 24.3).
Patient foundations and registries often engage in collection of self-reported data, which can be useful for demographic studies but is not generally sufficiently validated for rigorous studies involving prevalence, incidence, mortality and outcome data. Hospital coding data and insurance claims databases have proven to be useful in determining the prevalence of several rare diseases, including IPF [68, 96, 110]. Other methods have included surveying death certificates [22], supplemented with data from patient registries to improve accuracy [26]. The latter approach is based on the premise that combined approaches to epidemiological data collection are particularly well suited to the rare diseases.
Clinical trials are difficult to perform in rare diseases. Validation of optimal outcome measures of rare lung disease is vital, as is the identification of surrogate markers that accurately predict meaningful endpoints. Randomised control trials are not always feasible in rare conditions, and alternative study designs such as ‘n-of-1’ single patient, crossover and sequential approaches may be considered [11, 75]. In diseases where prognosis is poor, survival is the most important outcome to ascertain the efficacy of a new drug, but this is not always practical or feasible when conditions are extremely rare or survival is prolonged; in those cases use of clinical parameters which are predictive of survival are necessary surrogates. Examples of rare disease communities that have successfully conducted large epidemiological studies to discover powerful surrogates for survival include IPF [27] and CF [61]. In these diseases, pulmonary function and frequency of acute exacerbations [76] correlate with risk of death and are now used as outcome measures in pivotal trials, speeding the discovery of new treatments. Studies are desperately needed in other rare diseases, including those of much lower prevalence, to determine appropriate surrogates for each particular condition.
The study of the more common rare lung diseases including IPF, AATD and CF can inform the approach to ultra-rare conditions and drug development. For example, in AATD, a well-designed National Heart Lung and Blood Institute (NHLBI) Registry facilitated accurate description of key demographic and physiologic characteristics of AATD individuals [86], including patterns of lung function decline that are critical for the design of trials. One recent benefit of the Registry was the discovery of a promising surrogate for the efficacy of therapeutics, including augmentation therapy [16]. Furthermore, in AATD the information recorded in national registries has been useful in identifying differences in cohorts of patients in disease severity, smoking exposure, access to treatment and frequency of phenotypes including very rare mutations [33, 100].
To understand the challenges of describing the epidemiology of individual rare lung diseases, we will focus on how IPF, CF and AATD may inform future work in other conditions. Following this we will briefly describe the challenges in extremely rare conditions and detail some of the exceptional progress in LAM and PAP.
4 Idiopathic Pulmonary Fibrosis: Epidemiological Challenges
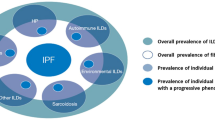
Although idiopathic pulmonary fibrosis (IPF) is perhaps more widely known to the broader medical and lay communities than most rare lung diseases, many aspects of the approach to this disease require refinement. IPF is a complex disease that requires a multidisciplinary approach to ensure timely and accurate diagnosis [108]. When the correct diagnosis is delayed or missed, lags in specialist care are associated with increased risk of death [69]. The discovery and approval of novel treatments has sparked renewed interest in IPF clinical care and translational research. Prior to the year 2000, very few clinical trials had been performed in IPF, encompassing a total of only about 100 patients enrolled in small, low quality studies. Since that time, thousands of patients have been enrolled in randomized, controlled clinical studies [21, 127], leading to significant improvements in therapeutic options and a large body of data that is being used to inform trial design. The emergence of pirfenidone [21, 59, 62] and nintedanib [59, 114] as medications that have shown benefit in reducing pulmonary function decline in IPF has led to a greater focus on the epidemiology and clinical course of IPF, including identification of the subsets of patients who may uniquely benefit from such novel treatments.
The epidemiology of IPF had been poorly described in the literature until recently. It was not until 1998 [60] that a clear definition of the disease was proposed and incorporated into the 2000 consensus diagnostic criteria, which were then subsequently updated [63, 108]. This confusion in accurately defining IPF compromised accurate epidemiologic data collection, as many patients were coded under alternative and often erroneous diagnoses. The reported prevalence range of IPF using these methods was therefore implausibly broad, spanning almost three logs from 0.7 per 100,000 to 63 per 100,000, and incidence figures ranging from 0.6 per 100,000 to 17.4 per 100,000 [106, 107]. The methods used to acquire epidemiological data in IPF have included accessing healthcare insurance claims and benefits databases [68, 96, 110], medical record linkage systems [99], primary care databases [41], surveys of pulmonary clinics [47, 58, 89], and death certificates and pathology reports [22]. These varied approaches led to conflicting reports of mortality rates and incidence, with the effect of increased age poorly accounted for [91]. Under recognition and misclassification [56] have plagued data collection based on extraction from death certificates and national registries [73]. Although the use of insurance claims databases may be more accurate for demographic and outcome data collection, this method is heavily dependent on correct initial coding, incompletely validated [29] and subject to overestimation of prevalence and various outcomes.
5 Evolving Management of IPF: Improving Epidemiological Data
While the epidemiology of IPF is still not well understood, it continually improving. Evidence for epidemiologic progress includes new, approved therapeutic options and better diagnostic and management strategies. Rapid and accurate methods of diagnosing IPF are now possible in the form of high resolution computed tomography (HRCT) imaging, which is considered diagnostic if the classic pattern of usual interstitial pneumonia characterised by subpleural, basilar-predominant reticular abnormality with honeycombing is identified [79, 108]. The recognition that the diagnosis can be made based on clinical criteria has reduced the need for lung biopsy [109]. Developments in bronchoscopic techniques such as transbronchial cryobiopsy have further improved the ability to accurately diagnose IPF by less invasive, non-surgical methods [5, 35, 67, 102]. More accurate diagnosis of IPF will also allow better data acquisition, that together with the growing portfolio of novel candidate therapies and biomarkers will be used to assess disease progression and prognosis [37] and design and accelerate trials. Accurate identification of IPF will, in turn, lead to better understanding the natural history of the disease, as well as its societal impact on health care use and costs [74]. The use of well-designed registries have dramatically improved clinical trial recruitment in IPF. The NHLBI sponsored IPF Clinical Research Network (IPFnet) has screened over 1000 patients [23] for inclusion in clinical trials for a range of treatments including prednisolone, azathioprine, and N-acetylcysteine [6, 81], sildenafil [48] and warfarin [93], to name a few. While none of these medications showed any clinically significant benefit in trials, the use of IPFnet as a source for patient recruitment has provided a platform for future accurate epidemiological classification of IPF, and a template for other rare lung disease communities to emulate.
6 Cystic Fibrosis: A Model for Epidemiological Studies in Rare Disease
Cystic fibrosis is a rare disease caused by mutations in the Cystic Fibrosis Transmembrane Conductance Regulator gene (CFTR), and it is the most common life shortening autosomal recessive disorder in Caucasians. It is a multisystem disease, in which the major cause of mortality is due to pulmonary complications [111]. The genetic inheritance pattern in CF lends itself to screening at birth [31], which has led to a better understanding of the natural course of disease progression and facilitated collection of powerful epidemiological data. Although rapid and inexpensive genotyping for CFTR mutations is increasingly accessible and has greatly improved the diagnostic yields of newborn screening [126], on a world-wide basis the workhorse for diagnosis remains sweat chloride testing. Together these methods have the potential to identify almost all cases of CF in early infancy. This combination of early and accurate diagnosis, well understood molecular pathophysiology and powerful patient advocacy place CF at the vanguard of all models to study rare lung disease.
The incidence of CF ranges from approximately 1 in 350,000 in Japan [49, 139] to 1 in 3,500 live births in the USA [65] to approximately 1 in 1,353 in Ireland [30], which has the highest incidence and prevalence worldwide. Registry data has been essential for facilitating between-country comparisons of incidence, prevalence, survival and other outcomes [12, 52]. For instance, it is now clear that children and young adults born in the USA have better pulmonary function than those in the UK [38]. Observations such as these, which have been a direct result of development of informative registries, spur investigation into the underlying reasons for differences, facilitate interventions and provide opportunities for quality improvement.
6.1 Improved CF Care: The Benefits of Registries and Patient Foundations
Registries in CF are excellent sources of demographic data and have been used to great effect in outcome studies, for clinical trial recruitment and as prognostic markers. More so than in perhaps any other rare lung disease, CF patient registries have informed the natural history of disease progression and facilitated breakthrough discoveries.
The use of data from CF registries has helped to identify the association between particular genotypes and mortality risk [87], as well as the prediction of prognosis based on clinical parameters including FEV1, body mass index (BMI) and bacterial colonisation of sputum [76]. The impact of external factors such air pollutants [40], second-hand smoke exposure [18] and socioeconomic status [94, 121] on lung function decline, mortality and other outcome measures has also been gathered from registry studies. As CF is a multisystem disorder, the accurate collection of data is essential for predicting prognosis and measuring response to intervention, and registries are useful for capturing data on comorbidities, including osteoporosis, diabetes, pancreatic insufficiency and gastrointestinal complications, all of which impact upon disease progression [83].
While registries ideally should collect similar data in a standardized manner, major differences can occur internationally which may affect their use as validated sources of information regarding outcomes and prognosis. The European CF Demographics Registry Project compared data collected from 35 European countries’ registries, including demographic data for 29,000 patients [85], and demonstrated significant variation between the age at death and proportion of patients diagnosed with CF in non-EU countries compared to EU countries, perhaps due to either under-diagnosis, premature mortality or differences in patient registration in the former. To tackle this difference in reporting the European CF Society (ECFS) has launched an initiative to develop standardised care programmes [19]. Improvements in care have been well demonstrated through collaboration between caregivers, patient foundations, registries and patients in several countries. In the USA, for instance, the CF Foundation developed extensive quality improvement programmes, setting key performance indicators for CF centres, and using registry data to create a transparent forum for quality improvement [119, 120]. The efforts have resulted in greater compliance with diabetes screening [104, 105], and improvement in BMI [128] and in overall care provision [130]. Furthermore, the use of clinical prediction tools in CF identifies patients for lung transplantation earlier [77] and predicts overall prognosis [82]. Registries have been essential for validating scoring systems, which in some cases have developed as candidates for surrogate outcome measures. They are also useful in cost analysis and assessing referral patterns [80]. Finally, CF registries are ideal sources of information to examine the long term effects and impact novel therapies have on outcomes, including survival, exacerbations and quality of life measures [131].
6.2 Cystic Fibrosis Registries and Novel Treatment Development
CF registry studies have shown survival benefits associated with long term use of nebulised dornase alfa (DNase) [137] and tobramycin [118]; cases in which short-term randomised control trials [36, 113] failed to reveal an effect. These examples highlight the utility of registry studies in assessing therapies in rare diseases with small study populations. Furthermore, collaborative studies employing CF registries have played a pivotal role in the development of novel drugs, in particular the CFTR potentiator ivacaftor [112].
The Cystic Fibrosis Foundation Therapeutics Development Network (TDN) has successfully conducted numerous clinical trials since its inception [39] and was instrumental in developing high-throughput screening to identify candidate drugs, and enrolling patients in phase I, II and III trials around the world. Apart from establishing a significant pool of over 20,000 patients from the USA and links to international sites, this network improved the integrity and efficiency of trial conduct and data collection and management. The subsequent development of ivacaftor has been revolutionary in CF care, demonstrating a significant improvement in inflammation, pulmonary function, exacerbation frequency and quality of life in a subset of patients with CF [101, 117]. These exciting results are transforming care in CF and are setting expectations for future novel and personalized medicine at a very high level for CF, and other genetic lung diseases. Network development and intelligent use of registry data in CF are exemplars for all rare lung diseases.
7 Alpha-1 Antitrypsin Deficiency: Epidemiological Findings of a Complex Genetic Condition
Alpha-1 antitrypsin (AAT) is a serine protease inhibitor produced in the liver, which is abundant in the blood stream and acts mainly in the lung to counteract neutrophil elastase. In AAT deficiency (AATD) there is an imbalance in the protease/antiprotease balance leading to parenchymal lung damage and emphysema. AATD is a multisystem disorder where polymerisation of mutated AAT can accumulate in hepatocytes leading to chronic liver disease and the rare occurrence of AATD associated panniculitis [34]. AAT is inherited in an autosomal codominant pattern with more than 50 known deficient alleles, the most common being those encoding the S and Z mutations, with prevalence varying markedly across continents and within countries.
Despite commendable attempts to characterize the genetic landscape of AAT worldwide, small studies have often fallen short and detailed genetic epidemiological studies are lacking in about half of all countries across the globe [25]. However, innovative tools used in other scientific areas of knowledge have been used to compensate this circumstance; Blanco et al used an informatics approach namely the ArcMap (ArcGGIS Geographical Information System, for Microsoft Windows) based on the inverse distance weighting (IDW) multivariate interpolation method to develop detailed maps of the prevalence of S and Z alleles worldwide. This approach identified an unsuspected significance of S and Z allele frequencies in areas where AAT deficient allele prevalence had not been previously studied, highlighting these areas as priority targets for further screening and future trials [8].
Interestingly, these epidemiological studies supported the hypothesis that the Z mutation appeared in the Scandinavian Peninsula approximately 2000-6500 years ago and that Viking raids may have spread the Z allele. In contrast, the S allele may have originated in the Iberian Peninsula more than 9000 years ago and it shows the opposite distribution with a gradient south-north and west-east in Europe [9]. The approach to National registries in AATD have served as a platform to share knowledge about the condition, promote screening amongst at risk individuals and produce local guidelines regarding diagnoses and treatment, and serves as an exemplar for all rare diseases [14, 15, 24, 70].
8 Lymphangioleiomyomatosis: Excellence in Foundation Driven Developments in Care
Lymphangioleiomyomatosis (LAM) is a rare, progressive, cystic lung disease found almost exclusively in women [57, 115]. Similar to other rare lung diseases, the limited available epidemiological data about the disease has been acquired from federal and international registries and advocacy group sources, as well as case report series.
Data from the NHLBI LAM registry [115] and the Japanese LAM Registry [44] together with several large cases series from Europe [55, 136], Korea [95] and Japan [64] have been used to compile a demographic and epidemiologic picture for LAM. With such a rare disease, accurate prognostic information and survival data has been difficult to acquire due to the small, geographically disperse populations and variable study methodology. Mortality was initially reported to be very high, with early retrospective cohorts reporting 10-year survival rates of only approximately 20% [20, 125], but more recent studies have estimated the 10-year survival to be approximately 76-91% after symptom onset [44, 55, 88, 136]. Although the mean age at diagnosis is approximately 40-41 years [97, 115] cases in prepubertal individuals and octogenarians have also been reported [46]. Until recently it had been difficult to elucidate the factors that determine survival or predict prognosis in LAM, and there have been some associations made that are not intuitively obvious; for instance, pneumothorax as the initial presentation has been associated with favourable outcome [44, 129] while airflow obstruction which is responsive to bronchodilators is associated with pulmonary function decline [132].
The LAM Foundation, a disease specific patient advocacy organisation established in 1995, has been instrumental in accelerating advances in LAM. A population-based study conducted on 410 patients with LAM registered with the LAM Foundation has been influential in defining the prognostic indicators in this previously poorly classified condition [97]. A study by Oprescu et al using the LAM Foundation registry and the National Death Index at the Centers for Disease Control (CDC) validated the prolonged survival reported in a few recent studies, with 86% of patients surviving at least 10 years [97], and was the first to specifically report federally-compiled causes of death. Respiratory failure accounted for 4.12% of deaths, while pulmonary infection and pneumothorax accounted for 11.76% and 2.94%, respectively [97]. While the 10-year survival was 86%, similar to previous Japanese and UK studies (76% and 91% respectively), the median survival was much better than previously estimated, with a median transplant-free survival of 29 years from symptom onset and 23 years from diagnosis [97]. Analysis of a population based cohort rather than a hospital and clinic based cohort is the likely explanation for differences.
The importance of defining prognosis in LAM is vital in determining treatment options, especially as novel therapeutics have become available in the last decade [84]. The LAM Foundation assisted in the recruitment and operations of the Multicenter International LAM Efficacy of Sirolimus (MILES) Trial [84], a landmark study for LAM and for the greater rare disease community in terms of conducting trials for orphan drug development. Sirolimus, which inhibits the mammalian target of rapamycin (mTOR) signalling pathway, was shown to significantly improve pulmonary function compared to placebo [84], as well as reduce blood levels of vascular endothelial growth factor D (VEGF-D), a lymphangiogenic growth factor [140], and improve quality of life in LAM patients. This trial raised additional questions about criteria for future patient selection, and the importance of identifying accurate prognostic factors and biomarkers to guide therapeutic decisions. Sirolimus has been demonstrated to improve CT measurements of gas trapping in LAM [4], and in a small study of 25 mild LAM patients with a history of chylothorax and/or lymphangioleiomyoma, to favorably impact the lymphatic manifestations of the disease [134]. VEGF-D has been demonstrated to perform well as a diagnostic, prognostic and predictive biomarker [84, 140]. This trial was conducted by the Rare Lung Diseases Consortium as an international, multicenter investigator initiated study without pharmaceutical company involvement in the conduct of the trial, and although not designed with a label change in mind, served as the sole basis for FDA approval.
The LAM Foundation has been cited as an ‘model to emulate’ by the New England Journal of Medicine [50] an exemplar among patient organisations that aspire to organize, support and educate those affected; to promote collaboration between the patient community, the NIH and medical researchers; and to fund the research that forms the basis for clinic trials. A decade of building and supporting a network of researchers and patients provided the platform for recruitment of patients for a pivotal, randomised control trial. Additionally, the LAM Foundation has identified specialty clinics around the world, which serve to focus care, nurture expertise and facilitate clinical trials.
9 Pulmonary Alveolar Proteinosis: Epidemiological Challenges and Opportunities to be Gained from Claims Databases
Another very rare lung disease that is instructive with respect to epidemiologic approaches is pulmonary alveolar proteinosis (PAP), a disease in which there have been great strides in our understanding of the natural history and molecular pathogenesis over recent years. PAP is characterised by the accumulation of surfactant within alveolar macrophages and alveoli, resulting in restrictive lung disease, varying degrees of hypoxemia and respiratory insufficiency, and an increased risk of pulmonary infection [124, 135]. PAP can be categorized as primary, secondary or congenital [114, 116]. The prevalence of primary or autoimmune PAP, which accounts for 90% of all cases, had been historically estimated at approximately 0.5 per 100,000 individuals [98, 135]. However, more recent data based on insurance sources suggest that the disorder may be tenfold more common than originally thought. The evolution in approaches to gathering epidemiologic data has been instructive.
The primary source of data regarding the clinical course and natural history of PAP has been large case series, including a meta-analysis by Seymour et al of 410 cases from published literature [124]. Other sources have included multicentre series from Japan (n=248) [51], China (n=241) [138] and single centre reports from the US (n=34) [103], Germany (n=70) [10], Israel (n=15) [7] and Italy (n=81) [13]. While these studies have been crucial in defining the progression and response to treatment in PAP, they have likely underestimated the prevalence of this rare condition. While prevalence has been previously reported as 3.7–6.2 per million patients [7, 51, 124] this is likely an underestimate. Through the use of de-identified claims data acquired from the OptumInsight database, (Table 24.4) which include outpatient, inpatient, emergency department and pharmacy dispensing data, we estimate that the prevalence of PAP at 6.87 per million. By identifying 164 newly diagnosed PAP patients who were continually enrolled with Optum for full medical and pharmacy benefits and a control group of age/gender matched individuals followed for 12 months, it was possible to define some features of the epidemiology of the disease. The prevalence was noted to increase with age, and the disease occurred equally in males and females with a bimodal peak at 45-54 years of age. Similar methods utilising the OptumInsight database have been employed to assess the long-term healthcare costs in IPF [28] .
Other sources of claims data are available and have been employed in a variety of diseases, both rare and common, to determine outcome and prevalence data. The National (Nationwide) Inpatient Sample (NIS) is a large inpatient care database in the US, containing data on more than seven million hospital stays, covering all payment sources. The large population size is ideal for determining prevalence estimates, enabling analysis of rare diseases, and aiding in calculations of economic burden, mortality and other outcome measures for individual conditions [17, 133]. MarketScan is a collection of databases, containing healthcare claims information from large employers, managed care organisations, and Medicare and Medicaid programmes [1] which may also be useful in identifying rare disease prevalence and patterns. The Medicare database has been employed successfully to determine the prevalence of nontuberculous mycobacteria (NTM), a rare pulmonary infection, where an increasing prevalence rate was identified in a sample comprising 5% of Medicare beneficiaries over a 10 year period from 1997-2007, increasing from 20 to 47 cases per 100,000 individuals [2]. These databases are ideal sources to study rare disease, and are especially powerful in combination with registry and patient foundation data. Linking of society and registry data with claims databases has been useful in the facilitation of long term study in other fields [53], and hence similar links could be beneficial to rare lung disease research. (Table 24.4)
10 The Future of Rare Lung Disease: Registries and Foundations to Facilitate Research
The significant growth in the knowledge of rare diseases in general and the astounding progress in select conditions, including IPF, CF and LAM in particular, bodes well for future advances in rare lung diseases. The collaboration of researchers, expert clinicians, patient organisations and registries has made possible the huge leaps in understanding and therapeutic options; highlighting the value of collaborative approaches in rare diseases. Lessons learned from trial design and quality improvement in smaller populations, are often instructive for other disease communities. The excellent results of the CF Foundation, Alpha 1 Foundation and the LAM Foundation in educating, supporting and organizing patients, facilitating clinical trials through recruitment and direct participation in study operations, and funding research has proven to be a pivotal component of improving outcomes of patients with these conditions [39, 84, 112]. Through advocacy, optimization of resources, networking, coordination and development of registries, the conduct of clinical studies that have impact are uniquely possible in rare diseases. Similar cohesive strategies are required in other rare conditions including the ultra-rare disorders; but will require collaborative approaches to develop multicentre networks and expert-led clinics. The LAM Foundation and the Rare Lung Diseases Consortium, a network supported by the National Center for Accelerating Translational Research, are attempting to do just that using the platform of special centers for the care of LAM patients. The LAM Foundation and the RLDC have invited over a dozen rare lung disease communities to refer their patients to the LAM Clinics, now dubbed RLDC clinics. Recently, the third annual RLDC Conference was hosted by the RLDC and the LAM Foundation in Cincinnati, with 472 attendees from 35 states and 20 countries represented, from over a dozen rare lung disease communities and advocacy organizations. This collaborative approach to clinical care and conferences focuses rare lung disease patients to a limited number of academic health centers within major cities, nurtures expertise, improves quality and consistency of care, and facilitates clinical trials. In this way, rare lung diseases are pooling resources and enabling breakthroughs in even the rarest of members.
In summary, studying the epidemiology of rare lung disease has historically been difficult and has produced mixed results, but the dawn of the information era is revolutionizing our approaches and expanding our opportunities. Models of successful registries and clinical studies by some of the rarest of diseases are available for adoption by other disease communities, including the common disorders, and promise to improve care and lead to new therapeutic options.
Reference
Adamson DM, Chang S, Hansen LG (2008) Health research data for the real world: the MarketScan databases. Thompson Healthcare, New York, p b28
Adjemian J, Olivier KN, Seitz AE et al (2012) Prevalence of nontuberculous mycobacterial lung disease in US Medicare beneficiaries. Am J Respir Crit Care Med 185(8):881–886
Albert RK, Connett J, Bailey WC et al (2011) Azithromycin for prevention of exacerbations of COPD. N Engl J Med 365(8):689–698
Argula RG, Kokosi M, Lo P et al (2016) A novel quantitative computed tomographic analysis suggests how sirolimus stabilizes progressive air trapping in Lymphangioleiomyomatosis. Ann Am Thorac Soc 13(3):342–349
Babiak A, Hetzel J, Krishna G et al (2009) Transbronchial cryobiopsy: a new tool for lung biopsies. Respiration 78(2):203–208
Behr J (2012) Prednisone, azathioprine, and N-acetylcysteine for pulmonary fibrosis. N Engl J Med 367(869):870–871
Ben-Dov I, Kishinevski Y, Roznman J et al (1999) Pulmonary alveolar proteinosis in Israel: ethnic clustering. Isr Med Assoc J: IMAJ 1(2):75–78
Blanco I, de Serres FJ, Carcaba V et al (2012) Alpha-1 antitrypsin deficiency PI*Z and PI*S gene frequency distribution using on maps of the world by an inverse distance weighting (IDW) multivariate interpolation method. Hepat Mon 12(10 HCC):e7434
Blanco I, de Serres FJ, Fernandez-Bustillo E et al (2006) Estimated numbers and prevalence of PI*S and PI*Z alleles of alpha1-antitrypsin deficiency in European countries. Eur Respir J 27(1):77–84
Bonella F, Bauer PC, Griese M et al (2011) Pulmonary alveolar proteinosis: new insights from a single-center cohort of 70 patients. Respir Med 105(12):1908–1916
Buckley BM (2008) Clinical trials of orphan medicines. Lancet 371(9629):2051–2055
Buzzetti R, Salvatore D, Baldo E et al (2009) An overview of international literature from cystic fibrosis registries: 1. Mortality and survival studies in cystic fibrosis. J Cyst Fibros 8(4):229–237
Campo I, Mariani F, Rodi G et al (2013) Assessment and management of pulmonary alveolar proteinosis in a reference center. Orphanet J Rare Dis 8(1):1
Carroll TP, O’Connor CA, Floyd O et al (2011) The prevalence of alpha-1 antitrypsin deficiency in Ireland. Respir Res 12(1):91
Casas F, Blanco I, Martinez MT et al (2015) Indications for active case searches and intravenous alpha-1 antitrypsin treatment for patients with alpha-1 antitrypsin deficiency chronic pulmonary obstructive disease: an update. Arch Bronconeumol 51(4):185–192
Chapman KR, Burdon JG, Piitulainen E et al (2015) Intravenous augmentation treatment and lung density in severe alpha1 antitrypsin deficiency (RAPID): a randomised, double-blind, placebo-controlled trial. Lancet 386(9991):360–368
Chung L, Krishnan E, Chakravarty EF (2007) Hospitalizations and mortality in systemic sclerosis: results from the Nationwide Inpatient Sample. Rheumatology 46(12):1808–1813
Collaco JM, Vanscoy L, Bremer L et al (2008) Interactions between secondhand smoke and genes that affect cystic fibrosis lung disease. JAMA 299(4):417–424
Colombo C, Littlewood J (2011) The implementation of standards of care in Europe: state of the art. J Cyst Fibros 10:S7–S15
Corrin B, Liebow AA, Friedman PJ (1975) Pulmonary lymphangiomyomatosis. A review. Am J Pathol 79(2):348
Cottin V (2012) Changing the idiopathic pulmonary fibrosis treatment approach and improving patient outcomes. Eur Respir Rev 21(124):161–167
Coultas DB, Zumwalt RE, Black WC et al (1994) The epidemiology of interstitial lung diseases. Am J Respir Crit Care Med 150(4):967–972
de Andrade J, Schwarz M, Collard HR et al (2015) The idiopathic pulmonary fibrosis clinical research network (ipfnet): diagnostic and adjudication processes. Chest 148(4):1034–1042
de la Roza C, Rodriguez-Frias F, Lara B et al (2005) Results of a case-detection programme for alpha1-antitrypsin deficiency in COPD patients. Eur Respir J 26(4):616–622
de Serres FJ (2002) Worldwide racial and ethnic distribution of alpha1-antitrypsin deficiency: summary of an analysis of published genetic epidemiologic surveys. Chest 122(5):1818–1829
Dodge JA, Morison S, Lewist PA et al (1993) Cystic fibrosis in the United Kingdom, 1968–1988: incidence, population and survival. Paediatr Perinat Epidemiol 7(2):157–166
du Bois RM, Weycker D, Albera C et al (2011) Forced vital capacity in patients with idiopathic pulmonary fibrosis: test properties and minimal clinically important difference. Am J Respir Crit Care Med 184(12):1382–1389
Eliot O-T, Yanxin W, Bonni H et al (2012) The economic burden of idiopathic pulmonary fibrosis from diagnosis to lung transplant. In: A40. The economic burden of respiratory disease and cost-effectiveness of treatments. American Thoracic Society. pp A1497–A1497
Esposito DB, Lanes S, Donneyong M et al (2015) Idiopathic pulmonary fibrosis in United States automated claims. Incidence, prevalence, and algorithm validation. Am J Respir Crit Care Med 192(10):1200–1207
Farrell P, Joffe S, Foley L et al (2007) Diagnosis of cystic fibrosis in the Republic of Ireland: epidemiology and costs. Ir Med J 100(8):557
Farrell PM, Rosenstein BJ, White TB et al (2008) Guidelines for diagnosis of cystic fibrosis in newborns through older adults: Cystic Fibrosis Foundation consensus report. J Pediatr 153(2):S4–S14
Faurisson F, (2011) Survey of the delay in diagnosis for 8 rare diseases in Europe: EurordisCare2. European Organisation for Rare Diseases Web site. 2004
Ferrarotti I, Baccheschi J, Zorzetto M et al (2005) Prevalence and phenotype of subjects carrying rare variants in the Italian registry for alpha1-antitrypsin deficiency. J Med Genet 42(3):282–287
Franciosi AN, McCarthy C, Carroll TP et al (2015) Unusual acute sequelae of alpha1-antitrypsin deficiency: a myriad of symptoms with one common cure. Chest 148(5):e136–e138
Fruchter O, Fridel L, El Raouf BA et al (2014) Histological diagnosis of interstitial lung diseases by cryo-transbronchial biopsy. Respirology 19(5):683–688
Fuchs HJ, Borowitz DS, Christiansen DH et al (1994) Effect of aerosolized recombinant human DNase on exacerbations of respiratory symptoms and on pulmonary function in patients with cystic fibrosis. N Engl J Med 331(10):637–642
Fujimoto K, Taniguchi H, Johkoh T et al (2012) Acute exacerbation of idiopathic pulmonary fibrosis: high-resolution CT scores predict mortality. Eur Radiol 22(1):83–92
Goss CH, MacNeill SJ, Quinton HB et al (2015) Children and young adults with CF in the USA have better lung function compared with the UK. Thorax 70(3):229–236
Goss CH, Mayer-Hamblett N, Kronmal RA et al (2002) The cystic fibrosis therapeutics development network (CF TDN): a paradigm of a clinical trials network for genetic and orphan diseases. Adv Drug Deliv Rev 54(11):1505–1528
Goss CH, Newsom SA, Schildcrout JS et al (2004) Effect of ambient air pollution on pulmonary exacerbations and lung function in cystic fibrosis. Am J Respir Crit Care Med 169(7):816–821
Gribbin J, Hubbard RB, Le Jeune I et al (2006) Incidence and mortality of idiopathic pulmonary fibrosis and sarcoidosis in the UK. Thorax 61(11):980–985
Gupta S, Bayoumi AM, Faughnan ME (2011) Rare lung disease research: strategies for improving identification and recruitment of research participants. Chest 140(5):1123–1129
Haffner ME, Whitley J, Moses M (2002) Two decades of orphan product development. Nat Rev Drug Discov 1(10):821–825
Hayashida M, Seyama K, Inoue Y et al (2007) The epidemiology of lymphangioleiomyomatosis in Japan: a nationwide cross-sectional study of presenting features and prognostic factors. Respirology 12(4):523–530
Hennekam RC (2011) Care for patients with ultra-rare disorders. Eur J Med Genet 54(3):220–224
Ho TBL, Hull JH, Hughes NC (2006) An 86-yr-old female with lymphangioleiomyomatosis. Eur Respir J 28(5):1065
Hodgson U, Laitinen T, Tukiainen P (2002) Nationwide prevalence of sporadic and familial idiopathic pulmonary fibrosis: evidence of founder effect among multiplex families in Finland. Thorax 57(4):338–342
Idiopathic Pulmonary Fibrosis Clinical Research, Network (2010) A controlled trial of sildenafil in advanced idiopathic pulmonary fibrosis. N Engl J Med 363(7):620
Imaizumi Y (1995) Incidence and mortality rates of cystic fibrosis in Japan, 1969-1992. Am J Med Genet 58(2):161–168
Ingelfinger JR, Drazen JM (2011) Patient organizations and research on rare diseases. N Engl J Med 364(17):1670–1671
Inoue Y, Trapnell BC, Tazawa R et al (2008) Characteristics of a large cohort of patients with autoimmune pulmonary alveolar proteinosis in Japan. Am J Respir Crit Care Med 177(7):752–762
Jackson AD, Daly L, Jackson AL et al (2011) Validation and use of a parametric model for projecting cystic fibrosis survivorship beyond observed data: a birth cohort analysis. Thorax 66:674–679
Jacobs JP, Edwards FH, Shahian DM et al (2010) Successful linking of the society of thoracic surgeons adult cardiac surgery database to centers for medicare and medicaid services medicare data. Ann Thorac Surg 90(4):1150–1157
Johnson SR, Cordier JF, Lazor R et al (2010) European Respiratory Society guidelines for the diagnosis and management of lymphangioleiomyomatosis. Eur Respir J 35(1):14–26
Johnson SR, Whale CI, Hubbard RB et al (2004) Survival and disease progression in UK patients with lymphangioleiomyomatosis. Thorax 59(9):800–803
Johnston I, Britton J, Kinnear W et al (1990) Rising mortality from cryptogenic fibrosing alveolitis. BMJ 301(6759):1017–1021
Juvet SC, McCormack FX, Kwiatkowski DJ et al (2007) Molecular pathogenesis of lymphangioleiomyomatosis: lessons learned from orphans. Am J Respir Cell Mol Biol 36(4):398–408
Karakatsani A, Papakosta D, Rapti A et al (2009) Epidemiology of interstitial lung diseases in Greece. Respir Med 103(8):1122–1129
Karimi-Shah BA, Chowdhury BA (2015) Forced vital capacity in idiopathic pulmonary fibrosis — FDA review of pirfenidone and nintedanib. N Engl J Med 372(13):1189–1191
Katzenstein A-LA, Myers JL (1998) Idiopathic pulmonary fibrosis: clinical relevance of pathologic classification. Am J Respir Crit Care Med 157(4):1301–1315
Kerem E, Reisman J, Corey M et al (1992) Prediction of mortality in patients with cystic fibrosis. N Engl J Med 326(18):1187–1191
King TE, Bradford WZ, Castro-Bernardini S et al (2014) A phase 3 trial of pirfenidone in patients with idiopathic pulmonary fibrosis. N Engl J Med 370(22):2083–2092
King TE, Costabel U, Cordier JF (2000) American Thoracic Society. Idiopathic pulmonary fibrosis: diagnosis and treatment. Am J Respir Crit Care Med 161:646–664
Kitaichi M, Nishimura K, Itoh H et al (1995) Pulmonary lymphangioleiomyomatosis: a report of 46 patients including a clinicopathologic study of prognostic factors. Am J Respir Crit Care Med 151(2):527–533
Knapp EA, Fink AK, Goss CH et al (2016) The cystic fibrosis foundation patient registry: design and methods of a national observational disease registry. Ann Am Thorac Soc 13:1173–1179
Knight AW, Senior TP (2006) The common problem of rare disease in general practice. Med J Aust 185(2):82–83
Kropski JA, Pritchett JM, Mason WR et al (2013) Bronchoscopic cryobiopsy for the diagnosis of diffuse parenchymal lung disease. PloS one 8(11):e78674
Lai C-C, Wang C-Y, Lu H-M et al (2012) Idiopathic pulmonary fibrosis in Taiwan–a population-based study. Respir Med 106(11):1566–1574
Lamas DJ, Kawut SM, Bagiella E et al (2011) Delayed access and survival in idiopathic pulmonary fibrosis: a cohort study. Am J Respir Crit Care Med 184(7):842–847
Lara B, Miravitlles M (2015) Spanish registry of patients with alpha-1 antitrypsin deficiency; comparison of the characteristics of PISZ and PIZZ individuals. COPD 12(Suppl 1):27–31
Laurell CB, Sveger T (1975) Mass screening of newborn Swedish infants for alpha antitrypsin deficiency. Am J Hum Genet 27(2):213–217
Lavandeira A (2002) Orphan drugs: legal aspects, current situation. Haemophilia 8(3):194–198
Ley B, Collard HR (2013) Epidemiology of idiopathic pulmonary fibrosis. Clin Epidemiol 5:483
Ley B, Collard HR (2015) House of cards? Testing fundamental assumptions in idiopathic pulmonary fibrosis epidemiology. Am J Respir Crit Care Med 192(10):1147–1148
Lillie EO, Patay B, Diamant J et al (2011) The n-of-1 clinical trial: the ultimate strategy for individualizing medicine? Pers Med 8(2):161–173
Liou TG, Adler FR, Fitzsimmons SC et al (2001) Predictive 5-year survivorship model of cystic fibrosis. Am J Epidemiol 153(4):345–352
Liou TG, Adler FR, Huang D (2005) Use of lung transplantation survival models to refine patient selection in cystic fibrosis. Am J Respir Crit Care Med 171(9):1053–1059
Luisetti M, Balfour-Lynn IM, Johnson SR et al (2012) Perspectives for improving the evaluation and access of therapies for rare lung diseases in Europe. Respir Med 106(6):759–768
Lynch DA, Godwin JD, Safrin S et al (2005) High-resolution computed tomography in idiopathic pulmonary fibrosis: diagnosis and prognosis. Am J Respir Crit Care Med 172(4):488–493
Martin C, Hamard C, Kanaan R et al (2015) Causes of death in French cystic fibrosis patients: the need for improvement in transplantation referral strategies! J Cyst Fibros 15:204–212
Martinez FJ, De Andrade JA, Anstrom KJ et al (2014) Randomized trial of N-acetylcysteine in idiopathic pulmonary fibrosis. N Engl J Med 370(22):2093
McCarthy C, Dimitrov BD, Meurling IJ et al (2013) The CF-ABLE score: a novel clinical prediction rule for prognosis in patients with cystic fibrosis. Chest 143(5):1358–1364
McCarthy C, O’Carroll O, Franciosi AN et al (2015) Factors affecting prognosis and prediction of outcome in cystic fibrosis lung disease. Cystic Fibrosis in the Light of New Research. InTech, DOI: 10.5772/60899
McCormack FX, Inoue Y, Moss J et al (2011) Efficacy and safety of sirolimus in lymphangioleiomyomatosis. N Engl J Med 364(17):1595–1606
McCormick J, Mehta G, Olesen HV et al (2010) Comparative demographics of the European cystic fibrosis population: a cross-sectional database analysis. Lancet 375(9719):1007–1013
McElvaney NG, Stoller JK, Buist AS et al (1997) Baseline characteristics of enrollees in the National Heart, Lung and Blood Institute Registry of alpha 1-antitrypsin deficiency. Alpha 1-Antitrypsin Deficiency Registry Study Group. Chest 111(2):394–403
McKone EF, Goss CH, Aitken ML (2006) CFTR genotype as a predictor of prognosis in cystic fibrosis. Chest 130(5):1441–1447
Moses MA, Harper J, Folkman J (2006) Doxycycline treatment for lymphangioleiomyomatosis with urinary monitoring for MMPs. N Engl J Med 354(24):2621–2622
Musellim B, Okumus G, Uzaslan E et al (2014) Epidemiology and distribution of interstitial lung diseases in Turkey. Clin Respir J 8(1):55–62
Nakao K (2009) Strategy for translational research and breakthroughs for common human diseases using excellent animal models and rare human diseases. Endocr J 56(5):637–638
Navaratnam V, Fleming KM, West J et al (2011) The rising incidence of idiopathic pulmonary fibrosis in the UK. Thorax 66(6):462–467
Network, R.D.C.R. Rare Diseases Clinical Research Network RDCRN: Rare Disease Clincal Research Studies. 20th June 2016. Available from: http://www.rarediseasesnetwork.org/studies/index.htm
Noth I, Anstrom KJ, Calvert SB et al (2012) A placebo-controlled randomized trial of warfarin in idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 186(1):88–95
O’Connor GT, Quinton HB, Kneeland T et al (2003) Median household income and mortality rate in cystic fibrosis. Pediatrics 111(4):e333–e339
Oh Y-M, Mo EK, Jang SH et al (1999) Pulmonary lymphangioleiomyomatosis in Korea. Thorax 54(7):618–621
Ohno S, Nakaya T, Bando M et al (2008) Idiopathic pulmonary fibrosis—results from a Japanese nationwide epidemiological survey using individual clinical records. Respirology 13(6):926–928
Oprescu N, McCormack F, Byrnes S et al (2013) Clinical predictors of mortality and cause of death in lymphangioleiomyomatosis: a population-based registry. Lung 191(1):35–42
Orphanet (2016) Prevalence and incidence of rare diseases: Bibilographic data. Orphanet: http://www.orpha.net/orphacom/cahiers/docs/GB/Prevalence_of_rare_diseases_by_alphabetical_list.pdf
Pérez ERF, Daniels CE, Schroeder DR et al (2010) Incidence, prevalence, and clinical course of idiopathic pulmonary fibrosis: a population-based study. CHEST J 137(1):129–137
Piras B, Ferrarotti I, Lara B et al (2013) Clinical phenotypes of Italian and Spanish patients with alpha1-antitrypsin deficiency. Eur Respir J 42(1):54–64
Pohl K, Hayes E, Keenan J et al (2014) A neutrophil intrinsic impairment affecting Rab27a and degranulation in cystic fibrosis is corrected by CFTR potentiator therapy. Blood 124(7):999–1009
Poletti V, Casoni GL, Gurioli C et al (2014) Lung cryobiopsies: a paradigm shift in diagnostic bronchoscopy? Respirology 19(5):645–654
Prakash UB, Barham SS, Carpenter HA et al (1987) Pulmonary alveolar phospholipoproteinosis: experience with 34 cases and a review. Mayo Clinic Proceedings 62:499–518. Elsevier
Quinton HB, O'Connor GT, Northern New England, C.V.C.F.C (2007) Current issues in quality improvement in cystic fibrosis. Clin Chest Med 28(2):459–472
Quon BS, Goss CH (2011) A story of success: continuous quality improvement in cystic fibrosis care in the USA. Thorax 66(12):1106–1108
Raghu G, Chen S-Y, Hou Q et al (2016) Incidence and prevalence of idiopathic pulmonary fibrosis in US adults 18–64 years old. Eur Respir J 48:179–186. ERJ-01653
Raghu G, Chen S-Y, Yeh W-S et al (2014) Idiopathic pulmonary fibrosis in US Medicare beneficiaries aged 65 years and older: incidence, prevalence, and survival, 2001–11. Lancet Respir Med 2(7):566–572
Raghu G, Collard HR, Egan JJ et al (2011) An official ATS/ERS/JRS/ALAT statement: idiopathic pulmonary fibrosis: evidence-based guidelines for diagnosis and management. Am J Respir Crit Care Med 183(6):788–824
Raghu G, Lynch D, Godwin JD et al (2014) Diagnosis of idiopathic pulmonary fibrosis with high-resolution CT in patients with little or no radiological evidence of honeycombing: secondary analysis of a randomised, controlled trial. Lancet Respir Med 2(4):277–284
Raghu G, Weycker D, Edelsberg J et al (2006) Incidence and prevalence of idiopathic pulmonary fibrosis. Am J Respir Crit Care Med 174(7):810–816
Ramsey BW (1996) Management of pulmonary disease in patients with cystic fibrosis. N Engl J Med 335(3):179–188
Ramsey BW, Davies J, McElvaney NG et al (2011) A CFTR potentiator in patients with cystic fibrosis and the G551D mutation. N Engl J Med 365(18):1663–1672
Ramsey BW, Pepe MS, Quan JM et al (1999) Intermittent administration of inhaled tobramycin in patients with cystic fibrosis. N Engl J Med 340(1):23–30
Richeldi L, du Bois RM, Raghu G et al (2014) Efficacy and safety of nintedanib in idiopathic pulmonary fibrosis. N Engl J Med 370(22):2071–2082
Ryu JH, Moss J, Beck GJ et al (2006) The NHLBI lymphangioleiomyomatosis registry: characteristics of 230 patients at enrollment. Am J Respir Crit Care Med 173(1):105–111
Saiman L, Marshall BC, Mayer-Hamblett N et al (2003) Azithromycin in patients with cystic fibrosis chronically infected with Pseudomonas aeruginosa: a randomized controlled trial. JAMA 290(13):1749–1756
Sawicki GS, McKone EF, Pasta DJ et al (2015) Sustained benefit from ivacaftor demonstrated by combining clinical trial and cystic fibrosis patient registry data. Am J Respir Crit Care Med 192(7):836–842
Sawicki GS, Signorovitch JE, Zhang J et al (2012) Reduced mortality in cystic fibrosis patients treated with tobramycin inhalation solution. Pediatr Pulmonol 47(1):44–52
Schechter MS (2012) Benchmarking to improve the quality of cystic fibrosis care. Curr Opin Pulm Med 18(6):596–601
Schechter MS, Gutierrez HH (2010) Improving the quality of care for patients with cystic fibrosis. Curr Opin Pediatr 22(3):296–301
Schechter MS, Shelton BJ, Margolis PA et al (2001) The association of socioeconomic status with outcomes in cystic fibrosis patients in the United States. Am J Respir Crit Care Med 163(6):1331–1337
Seersholm N, Kok-Jensen A, Dirksen A (1994) Survival of patients with severe alpha 1-antitrypsin deficiency with special reference to non-index cases. Thorax 49(7):695–698
Serrano-Aguilar P, Linertová R, Posada-de-la-Paz M et al (2015) Recruitment procedures for descriptive socio-economic studies in rare diseases. The BURQOL-RD project. Expert Opin Orphan Drugs 3(7):759–765
Seymour JF, Presneill JJ (2002) Pulmonary alveolar proteinosis: progress in the first 44 years. Am J Respir Crit Care Med 166(2):215–235
Silverstein EF, Ellis K, Wolff M et al (1974) Pulmonary lymphangiomyomatosis. Am J Roentgenol 120(4):832–850
Southern KW, Munck A, Pollitt R et al (2007) A survey of newborn screening for cystic fibrosis in Europe. J Cyst Fibros 6(1):57–65
Spagnolo P, du Bois RM, Cottin V (2013) Rare lung disease and orphan drug development. Lancet Respir Med 1(6):479–487
Stark LJ, Opipari-Arrigan L, Quittner AL et al (2011) The effects of an intensive behavior and nutrition intervention compared to standard of care on weight outcomes in CF. Pediatr Pulmonol 46(1):31–35
Steagall WK, Glasgow CG, Hathaway OM et al (2007) Genetic and morphologic determinants of pneumothorax in lymphangioleiomyomatosis. Am J Phys Lung Cell Mol Phys 293(3):L800–L808
Stern M, Wiedemann B, Wenzlaff P (2008) From registry to quality management: the German Cystic Fibrosis Quality Assessment project 1995–2006. Eur Respir J 31(1):29–35
Strobl J, Enzer I, Bagust A et al (2003) Using disease registries for pharmacoepidemiological research: a case study of data from a cystic fibrosis registry. Pharmacoepidemiol Drug Saf 12(6):467–473
Taveira-DaSilva AM, Steagall WK, Rabel A et al (2009) Reversible airflow obstruction in lymphangioleiomyomatosis. CHEST J 136(6):1596–1603
Torio CM, Andrews RM (2013) National inpatient hospital costs: the most expensive conditions by payer, 2011
Toshinori T, Kuniaki S, Yoshikazu I et al (2016) Early intervention with sirolimus benefits mild Lymphangioleiomyomatosis-related lung disease. In: C104. Rare interstitial lung disease: lam, cystic lung disease, and more. American Thoracic Society. p. A6255–A6255
Trapnell BC, Whitsett JA, Nakata K (2003) Pulmonary alveolar proteinosis. N Engl J Med 349(26):2527–2539
Urban T, Lazor R, Lacronique J et al (1999) Pulmonary lymphangioleiomyomatosis: a study of 69 patients. Medicine 78(5):321–337
Wagener JS, Kupfer O (2012) Dornase alfa (Pulmozyme). Curr Opin Pulm Med 18(6):609–614
Xu Z, Jing J, Wang H et al (2009) Pulmonary alveolar proteinosis in China: a systematic review of 241 cases. Respirology 14(5):761–766
Yamashiro Y, Shimizu T, Oguchi S et al (1997) The estimated incidence of cystic fibrosis in Japan. J Pediatr Gastroenterol Nutr 24(5):544–547
Young LR, Inoue Y, McCormack FX (2008) Diagnostic potential of serum VEGF-D for lymphangioleiomyomatosis. N Engl J Med 358(2):199–200
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
McCarthy, C., Lara Gallego, B., Trapnell, B.C., McCormack, F.X. (2017). Epidemiology of Rare Lung Diseases: The Challenges and Opportunities to Improve Research and Knowledge. In: Posada de la Paz, M., Taruscio, D., Groft, S. (eds) Rare Diseases Epidemiology: Update and Overview. Advances in Experimental Medicine and Biology, vol 1031. Springer, Cham. https://doi.org/10.1007/978-3-319-67144-4_24
Download citation
DOI: https://doi.org/10.1007/978-3-319-67144-4_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-67142-0
Online ISBN: 978-3-319-67144-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)