Abstract
This review article focuses on studies of Sigma 1 Receptor (Sigma1R) and retina . It provides a brief overview of the earliest pharmacological studies performed in the late 1990s that provided evidence of the presence of Sigma1R in various ocular tissues. It then describes work from a number of labs concerning the location of Sigma1R in several retinal cell types including ganglion, Müller glia , and photoreceptors . The role of Sigma1R ligands in retinal neuroprotection is emphasized. Early studies performed in vitro clearly showed that targeting Sigma1R could attenuate stress-induced retinal cell loss. These studies were followed by in vivo experiments. Data about the usefulness of targeting Sigma1R to prevent ganglion cell loss associated with diabetic retinopathy are reviewed. Mechanisms of Sigma1R-mediated retinal neuroprotection involving Müller cells , especially in modulating oxidative stress are described along with information about the retinal phenotype of mice lacking Sigma1R (Sigma1R −/− mice). The retina develops normally in Sigma1R −/− mice, but after many months there is evidence of apoptosis in the optic nerve head, decreased ganglion cell function and eventual loss of these cells. Additional studies using the Sigma1R −/− mice provide strong evidence that in the retina, Sigma1R plays a key role in modulating cellular stress. Recent work has shown that targeting Sigma1R may extend beyond protection of ganglion cells to include photoreceptor cell degeneration as well.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Retina
- Sigma 1 receptor
- Ganglion cell
- (+)-pentazocine
- ERG
- Electroretinogram
- nSTR
- Negative scotopic threshold response
- Mouse
- Diabetic retinopathy
- Photoreceptor cell
- Müller cell
- Ganglion cell death
- Neuroprotection
- rd10 mouse
18.1 Introduction
There has been substantial interest in the potential role of Sigma 1 Receptor (Sigma1R) as a target in neurodegenerative diseases. Numerous publications have explored this in brain and included in this compendium are chapters from several leaders in the field describing progress in the field. Neurodegenerative diseases affect not only the brain but also the retina , which some authorities consider an extension of the brain because the optic nerve is actually a tract of the brain. There have been a number of studies of this enigmatic protein in the retina and other components of the eye. This chapter will present an overview of some of investigations of Sigma1R in the eye with an emphasis on retina, the primary focus of work in our laboratory.
18.2 Structure and Organization of the Eye and Retina
The eye is situated within the bony orbit of the skull and functions to transmit visual information through the transparent cornea and lens to the retina . A diagram of the eye is shown in Fig. 18.1a. The cornea is the most anteriorly placed structure and is transparent to allow the passage of light. Light then travels through the aqueous humor and followed by the lens and ultimately strikes the photosensitive retina. Within the retina photic stimuli trigger a cis-to-trans isomerization of rhodopsin, the visual pigment, which in turn activates the neurochemical stimulation of retinal neurons for transmission via the optic nerve to the brain. Excessive exposure of the eye to light can damage various ocular structures including cornea, lens and retina. In addition to radiation, oxidative stress associated with ocular diseases such as diabetic retinopathy , glaucoma , macular degeneration, and cataract can trigger debilitating visual loss. The retina comprises the innermost tunic of the eyeball. Microscopically, the mammalian retina is composed of an outer pigmented layer, the retinal pigment epithelium (RPE), and an inner neurosensory layer, the neural retina. The retina is a stratified tissue characterized by cellular layers separated by synaptic layers. As shown in Fig. 18.1b, the outermost layer is the RPE. On its basal surface, which faces the choroid a major blood supply to outer retina, there are basal infoldings; whereas on its apical side, the RPE features microvillous processes, which interdigitate with the outer segments (OS) of photoreceptor cells . The OS are connected by a cilium to the inner segments (IS) of the photoreceptor cells, the first order neuron of the visual system. The photoreceptor nuclei form the outer nuclear layer (ONL). There are two general types of photoreceptor cells, rods and cones. Rods mediate scotopic (dark-adapted) vision, while cones mediate photopic (light-adapted vision). In the outer plexiform layer (OPL), the axons of rods and cones synapse with bipolar cells, the second order neurons of the visual pathway. The bipolar cells occupy the inner nuclear layer (INL). Within the INL are amacrine and horizontal cells, modulatory neurons of the retina. The major glial cell of the retina known as the Müller cell has its cell bodies within the INL, radially oriented processes emanate from these cells towards the inner and outer retina. Other glial cells of the retina include astrocytes and microglia. The inner plexiform layer (IPL) of retina is the synaptic layer in which bipolar cells communicate with ganglion cells (and some displaced amacrine cells). The ganglion cells reside in the ganglion cell layer (GCL) (along with some amacrine cells). The axons of the ganglion cells form the nerve fiber layer (NFL), the fibers of which join together to form cranial nerve II, the optic nerve. The inner most layer of the retina, the inner limiting membrane is actually formed by the inner processes (footplates) of the radially oriented Müller cells and the outer limiting membrane is also formed by footplates of the Müller cells. Comprehensive information about the eye can be found in Adler’s Physiology of the Eye [1] and details about retinal structure in health and disease are provided in an excellent three volume series Retina [2].
Anatomy of the eye and microstructure of the retina . (a) Diagram of the mammalian eye showing the anteriorly placed cornea, behind which is the aqueous humor and the centrally placed lens. The ciliary body projects into the eyeball. It synthesizes aqueous humor and also has suspensory ligaments that hold the lens in place behind the iris. The retina is the innermost tunic of the eye and comprises the posterior five-sixths of this inner tunic. (b) Hematoxylin-eosin stained section of mammalian retina (mouse ). The outermost layer is the retinal pigment epithelium (RPE). The microvillous processes of RPE cells interdigitate with the outer segments (OS) of adjacent photoreceptor cells . The cell bodies of the photoreceptor cells, known as rods and cones, constitute the outer nuclear layer (ONL). Photoreceptor cells synapse in the outer plexiform layer (OPL) with bipolar cells. Bipolar cells, horizontal cells and amacrine cells have their cell bodies in the inner nuclear layer (INL). Axons of the bipolar cells synapse in the inner plexiform layer (IPL) with dendrites of the ganglion cells (gcl). The axons of the ganglion cells form the nerve fiber layer (nfl); then continue on as the optic nerve . (Antioxidants and Redox Signaling, with permission, fig. 12, Ref. [65])
18.3 Establishing the Presence of Sigma1R in Retina
The existence of Sigma1R was proposed in the mid-1970s [3], however it would not be until the mid-1990s that Sigma1R would be investigated in eye. The first studies examined Sigma1R in cells of the lacrimal gland, which produces tears to keep the cornea moist. Schoenwald performed binding studies and demonstrated the presence of Sigma1R in rabbit lacrimocytes [4]. Bucolo and colleagues demonstrated the presence of Sigma1R binding in rabbit iris-ciliary body [5]. Within a few years, Sigma1R binding studies were performed in retina . Senda and colleagues showed that (+)-pentazocine ((+)-PTZ) and (+)-DTG bound bovine retinal membranes with high affinity and established that the densities of Sigma1R were higher in retina than in other tissues, including brain, adrenal medulla and lacrimocytes [6]. While the studies provided evidence that Sigma1R were present in retina, they did not demonstrate in which cell type(s) Sigma1R was present nor did they establish the molecular identify of the receptor. Working with our colleague, Dr. Vadivel Ganapathy , whose laboratory cloned Sig1R in human [7], rat [8] and mouse [9] at the same time as Hanner’s lab did so in guinea pig [10], we addressed these issues in mouse retina. Using reverse transcription–polymerase chain reaction (RT–PCR) analysis we amplified Sigma1R in neural retina, RPE–choroid complex, and lens isolated from mice [11]. We then determined in which retinal layers Sigma1R gene was expressed using in situ hybridization analysis and found abundant expression in the ganglion cell layer, cells of the inner nuclear layer, inner segments of photoreceptor cells and the RPE. We used an antibody developed in the lab of P. Casellas [12] and detected the Sigma1R protein in retinal ganglion, photoreceptor, RPE cells and surrounding the soma of cells in the inner nuclear layer. This study provided information on the cellular location of Sigma1R in retina and established the molecular identity of Sigma1R in retinal cell lines (rMC1, ARPE19 and RGC -5). In this same study, we demonstrated the presence of Sigma1R in lens and corneal epithelial cells and confirmed the presence of Sigma1R in the iris-ciliary body. Other laboratories have investigated the location of Sigma1R in retina. Liu and co-workers used RT-PCR and immunofluorescence to localize Sigma1R in the inner nuclear and ganglion cell layer of the rat retina [13]. They determined that Sigma1R was present in horizontal cells and several types of amacrine cells. Interestingly, they did not observe Sigma1R labeling in rat bipolar cells. Elegant ultrastructural studies from the Guo lab have demonstrated Sigma1R in mouse bipolar, photoreceptor and ganglion cells [14] as described in detailed in this book.
18.4 Studies of Sigma1R Neuroprotective Functions In Vitro
The earliest examination of the neuroprotective role of Sigma1R in retina used minced tissues isolated from embryonic rats [15]. The mixed neuronal-glial culture was exposed to L-glutamate, a known neurotoxin, at a high concentration [500 μM] for 10 min and cell death was determined using the trypan blue exclusion viability assay. The cells were pre-treated 10 min prior to insult with Sigma1R agonists SA4503 or (+)-PTZ and both afforded neuroprotection in a dose-dependent manner. These studies laid the foundation of future work examining the role of various Sigma1R ligands in a variety of retinal in vitro systems.
Some of the earliest in vitro studies of Sigma1R in retina were conducted in a cell line (RGC -5) that was originally described as a mouse retinal ganglion cell line [16], but was later determined to be the 661 W photoreceptor cell line derived from mouse [17]. Nonetheless, the early studies using these cells showed that targeting Sigma1R could prevent death of this transformed neuronal cell line and likely involved regulation of calcium channels [18, 19] and ER stress [20]. Bucolo demonstrated that increased intraocular pressure, which occurs in some forms of glaucoma , could be attenuated when Sigma1R ligands (+)-PTZ and (+)NANM (N-allylnormetazocine) were applied topically [5]. This group continued to study the beneficial effects of targeting Sigma1R in ischemia-reperfusion damage [21, 22], ocular hypotension models [23], and oxidative stress models [24]. In all cases targeting Sigma1R proved useful in attenuating stress-induced retinal cell loss.
18.5 Sigma1R in Retinal Disease : Expression Analysis and In Vitro Studies
The aforementioned studies set the stage to examine whether Sigma1R would continue to be expressed during retinal disease . We were particularly interested in its expression during diabetic retinopathy (DR ) because ganglion cells , which our studies showed express Sigma1R at high levels [11], are lost in DR in human patients [25], rats [25] and mice [26]. DR is a major sight-threatening disease and a leading cause of blindness globally [27]. It is characterized by loss of retinal neurons and disruption of vasculature [28]. Patients with diabetes lose color and contrast sensitivity within 2 years of onset. Focal ERG (electroretinogram ) analysis, which detects electrical responses of ganglion cells, reveals dysfunction of these cells early in diabetes [reviewed in 29]. We carried out studies in retinas of diabetic and age-matched control mice [30]. Mice that had been made diabetic using streptozotocin, a compound that kills pancreatic beta cells, had blood glucose levels that were consistently greater than 300 mg/dl. We did not administer insulin in the study to avoid confounding interpretation of the data. The neural retinas expressed Sigma1R mRNA at levels comparable to age-matched controls as assessed by semi-quantitative RT-PCR. In situ hybridization studies showed that Sigma1R continued to be expressed in ganglion cells of diabetic mice; western blot analysis and immunohistochemistry showed that Sigma1R protein was present in ganglion cells of diabetic mice. These were very encouraging findings because they provided a rationale for using Sigma1R agonists to block ganglion cell death characteristic of diabetic retinopathy .
To begin exploring the neuroprotective effects of Sigma1R ligands in retinal disease we first performed in vitro studies. Using the retinal neuronal cell line (RGC5), we demonstrated that exposure of these cells to high dosages of the excitotoxic amino acid homocysteine, which has been implicated in some forms of glaucoma , induced cell death, could be attenuated by pre- and co-treatment with (+)-PTZ ([3 or 10 μM]) [31]. There were limitations associated with using the RGC -5 cell line. First, millimolar concentrations of excitotoxins (e.g. glutamate, homocysteine) were required to induce cell death in these cells, whereas ganglion cells are sensitive to micromolar concentrations of these in vivo (e.g. [15 μM] glutamate). Second, cell lines replicate in culture, which is not characteristic of neurons in vivo. Third, neuronal cell lines do not form neurite processes characteristic of neurons. For these reasons we optimized culture of primary ganglion cells using the two-step immunopanning procedure developed by Barres [32, 33]. We used micromolar concentrations of glutamate and homocysteine as neurotoxic agents to study effects of (+)-PTZ as a neuroprotectant [34]. Primary ganglion cells pre-treated 1 h with (+)-PTZ followed by 18 h co-treatment with 25 μM Glu and (+)-PTZ showed a marked decrease in cell death: (25 μM Glu alone: 50 %; 25 μM Glu/0.5 μM (+)-PTZ: 38 %; 25 μM Glu/1 μM (+)-PTZ: 20 %; 25 μM Glu/3 μM (+)-PTZ: 18 %). Similar results were obtained when cells were exposed to 50 μM D,L-homocysteine and were pre-/co-treated with 3 μM (+)-PTZ. As with the studies using glutamate as a neurotoxin, the expression of Sigma1R at the gene and protein level was not altered by (+)-PTZ, suggesting that its neuroprotective effects involve activation of Sigma1R rather than altered expression of the receptor [34].
In addition to affording protection to ganglion cells , (+)-PTZ treatment preserved the processes of these neurons. We used differential interference contrast (DIC) microscopy in the cells exposed to homocysteine or glutamate and observed shrunken cell bodies and contracted and disrupted, stubby neuronal processes (Fig. 18.2.). Cells pre-/co-treated with (+)-PTZ showed marked preservation of the neuronal processes. The cell bodies were similar to the control cells and the fibers emanated in complex arrays. Clearly, (+)-PTZ protected the cells against death and preserved their fibers. The stereoselective effect of (+)-PTZ for sigmaR1 was established in experiments in which (−)-PTZ, the levo-isomer form of pentazocine, had no neuroprotective effect on excitotoxin-induced ganglion cell death .
Differential interference contrast microscopic analysis of cells exposed to Glu or homocysteine (Hcy) and (+)-PTZ. 1°GCs were isolated and cultured as described. Control cells (Con) were not exposed to excitotoxins; the row of photographs labeled “Glu” shows cells that were incubated with 25 μM Glu over a period of 18 h; photomicrographs were acquired at 0, 3, 6, 18 h post-incubation. The row of photographs labeled “Hcy” shows cells that were incubated with 50 μM Hcy over an 18 h period and photographed at 0, 3, 6 and 18 h post-incubation. In additional experiments, cells were pretreated with (+)-PTZ for 1 h and then co-incubated with (+)-PTZ and the excitotoxin for 18 h. Cell bodies and processes of cells co-treated with either Glu or Hcy and (+)-PTZ were similar in appearance to control cells. In the top left panel (control, 0 time) the arrow points to a process extending from the cell body. (Magnification bar = 15 μm). All photomicrographs are the same magnification (IOVS, with permission fig. 8, Ref. [34])
Our in vitro studies using primary retinal ganglion cells were complemented by studies in primary retinal Müller cells isolated from mouse retina . Müller cells, the key retinal glial cell, span the retinal thickness, contacting and ensheathing neuronal cell bodies and processes. They are crucial role for neuronal survival providing trophic substances and precursors of neurotransmitters to neurons [35]. Evaluating the role of Sigma1R in glial cells has great relevance to neurodegenerative diseases. Most retinal diseases are associated with reactive Müller cell gliosis, which may contribute to neuronal cell death. We sought to characterize Sigma1R in these cells. We used the rat Müller cell line, rMC-1 and showed that Sigma1R mRNA was expressed in these cells [36]. We then optimized primary mouse Müller cell isolation and culture in our lab, verifying that the cells were not contaminated by neurons or RPE cells [37]. In studies using primary Müller cells we showed that Sigma1R mRNA was expressed in these cells and determined using laser scanning confocal microscopy that Sigma1R was present on the nuclear and endoplasmic reticular membranes of these primary glial cells [36] (Fig. 18.3). It is noteworthy that other investigators interested in determining the subcellular location of Sigma1R in retina have reported its location on the nuclear membrane of photoreceptor cells [14]. This work is described in more detail elsewhere in this book .
Subcellular localization of σR1 in1°MCs. Müller cells were isolated from mouse retina and cultured. They were subjected to double-labeling immunocytochemical analysis using a polyclonal antibody specific for σR1 (which fluoresced red) and monoclonal antibodies (which fluoresced green) that label the nuclear membrane (lamin-A) or the endoplasmic reticulum (PDI), respectively. Optical sectioning by confocal microscopy detected co-localization of σR1 with lamin-A (merged image) and with PDI (merged image). In the merged images, the signal was orange when the red and green fluorescence overlap indicative of co-localization. (IOVS, with permission, fig. 2, Ref. [36])
Unlike primary neurons, primary Müller cells can proliferate in culture (just as they can proliferate in vivo), which allowed us to analyze Sigma1R binding activity in these cells. Previous studies of Sigma1R in retina demonstrated binding activity; however these studies used whole retina from large models (bovine) [6] and did not attempt to study the binding activities of individual retinal cell types. Sigma1R binding in primary Müller cells was characterized using the high-affinity Sigma1R ligand (+)-PTZ [38]. The binding was saturable over a (+)-PTZ concentration range of 1.25–75 nM. The apparent dissociation constant (Kd) for primary Müller cells was 18.9 ± 5.6 nM. Scatchard analysis of the binding data revealed the presence of a single binding site in these cells. The binding constant (Bmax) calculated for primary Müller cells was 1.32 ± 0.13 pmol/mg protein .
We also analyzed Sigma1R binding activity when Müller cells were exposed to either nitric oxide (NO) donors (SNAP, SNOG, SIN-1) or reactive oxygen species (ROS) donors (hydrogen peroxide and xanthine;xanthine oxidase), because NO and oxidative stress are implicated in retinal disease [39, 40]. Treatment of cells with NO and ROS donors resulted in marked increase in [3H]-(+)-PTZ binding activity. Taken collectively, the data show that oxidative stress increases Sigma1R binding activity [38].
18.6 Sigma1R in Retinal Disease : Expression Analysis and In Vivo Studies
Given the promising effects of (+)-PTZ in attenuating death of ganglion cells in vitro and the evidence that oxidative stress increases Sigma1R binding activity, we sought to investigate the effects of Sigma1R activation in murine models of diabetic retinopathy [41]. We used an induced diabetes model initially (streptozotocin injections in WT mice) to establish dosages and then performed a comprehensive analysis using the Ins2 Akita/+ mouse , which has a point mutation of the Insulin2 gene leading to hyperglycemia and hypoinsulinemia in heterozygous mice by ∼4 weeks [26]. In addition to increased retinal vascular permeability and an increase in acellular capillaries, Ins2 Akita/+ mice demonstrate ∼20–25 % reduction in the thickness of the inner plexiform layer (IPL), ∼16 % reduction in the thickness of the INL, and ∼25 % reduction in the number of cell bodies in the retinal GCL. Cells in the GCL are immunoreactive for active caspase-3 after 4 weeks of hyperglycemia, consistent with cell death by apoptosis. In our study, Ins2 Akita/+ mice were injected intraperitoneally beginning at diabetes onset with 0.5 mg kg−1 (+)-PTZ twice weekly for 22 weeks. The progression of changes in Ins2 Akita/+ retinas compared with wild-type over this time period is shown in Fig. 18.4. Wild-type mice had uniform thickness of layers throughout the central and midperipheral retina (Fig. 18.4a). Ins2 Akita/+ mice had modest INL thinning at 7 weeks (Fig. 18.4b) and more dramatic INL cell dropout at 10 weeks (Fig. 18.4c). By 17–25 weeks, there was marked INL and GCL cell loss in Ins2 Akita/+ mice (Figs. 18.4d–f). The IPL, which is composed of synaptic processes of cells in the INL and GCL, was also thinner. The cell loss and misalignment of inner retinal layers resulted in a somewhat wavy appearance in some of the retinas of 17- to 25-week-old Ins2 Akita/+mice. We found that (+)-PTZ treatment of Ins2 Akita/+ mice led to marked preservation of retinal architecture. The data shown (Figs. 18.4g–i) are from retinas of three different (+)-PTZ treated Ins2 Akita/+ mice, representative of the excellent retinal structure observed in the eyes of all diabetic mice treated with (+)-pentazocine (n = 8 mice, 16 eyes). Morphometric analysis indicated a significant decrease in the thickness of Ins2 Akita/+ mouse retinas , whereas (+)-PTZ-treated Ins2 Akita/+ mice were comparable to wild-type mice (Fig. 18.4j). The IPL and INL in Ins2 Akita/+ mice measured 30.3 ± 6.4 and 19.68 ± 2.72 μm, respectively. In (+)-PTZ-treated Ins2 Akita/+ mice, the values for the thicknesses of the IPL and INL (51.2 ± 4.9 and 31.3 ± 1.3 μm, respectively) were comparable to those in wild-type mice (51.1 ± 4.6 and 31.9 ± 2.4 μm , respectively; (Fig. 18.4k, l). There were 30 % fewer cell bodies in the GCL of Ins2 Akita/+ mice compared with wild-type mice (10.4 ± 1.2 vs. 15.4 ± 1.2 cells/100 μm retinal length, respectively) whereas the values for (+)-PTZ-treated Ins2 Akita/+ mice (15.6 ± 1.5 cells/100 μm) were similar to those in wild-type (Fig. 18.4m). The (+)-PTZ-treated Ins2 Akita/+ mice remained hyperglycemic throughout treatment. Blood glucose levels were ∼500 mg/dL (similar to untreated Ins2 Akita/+ mice) and were significantly higher than those in wild-type mice (104–160 mg/dL), suggesting that hyperglycemia per se may not be sufficient to trigger retinal neuronal loss in diabetes.
Preservation of retinal structure in Ins2 Akita/+ mice administered (+)-pentazocine . Representative H&E-stained retinal cryosections of (a) wild-type mice: GCL cells are distributed evenly, nuclear layers are uniformly thick; (b–f) Ins2 Akita/+ mice: INL becomes disrupted with age, GCL density is decreased; (g–i) Ins2 Akita/+mice treated with (+)-pentazocine (0.5 mg/kg, 2X/wk. i.p./22 weeks): marked preservation of retinal layers. PTZ pentazocine, gcl ganglion cell layer, ipl inner plexiform layer, inl inner nuclear layer, onl outer nuclear layer, magnification bar = 50 μm). Retinal sections were subjected to morphometric analysis: (j) total retinal thickness (k) IPL thickness (l) INL thickness (m) number of cell bodies in GCL per 100 μm length of retina . Data are means ± S.E. of measurements from retinas of 6 wildtype (12 eyes), 9 Ins2 Akita/+ (18 eyes) and 8 Ins2 Akita/+ treated with (+)-pentazocine (16 eyes). * Significantly different from wildtype and (+)-pentazocine-treated mice (p < 0.001). (IOVS, with permission, fig. 3, Ref. [41])
Recently, other studies have been conducted to evaluate whether targeting Sigma1R can afford retinal neuroprotection in vivo. Hara’s group used cutamesine dihydrochloride, an agonist of Sigma1R and evaluated the effects of intravitreal administration on light irradiation-induced photoreceptor cell death. Cutamesine suppressed light-induced retinal dysfunction and thinning of the outer nuclear layer in the mouse retina [42]. These were important findings because they suggested that targeting Sigma1R may have potential in neuroprotection of non-ganglion neurons within retina. Very recently, we explored activation of Sigma1R in treatment of a genetic model of photoreceptor cell loss. We utilized Pde6β rd10 (rd10) mice , which harbor a mutation in the rod-specific phosphodiesterase gene Pde6β and lose rod and cone photoreceptors within the first six weeks of life, as a model for severe retinal degeneration. Systemic administration of (+)-PTZ beginning at post-natal day 14 and continuing every other day for several weeks led to significant rescue of cone function in in treated rd10 mice as indicated by photopic electroretinographic recordings using natural noise stimuli and preservation cone cells upon retinal histological examination [43, 44]. The dramatic protective effect appears to be due to activation of Sigma1R because when rd10/Sigma1R −/− mice were administered (+)-PTZ, there was no preservation of cones [44]. (+)-PTZ treatment attenuated reactive gliosis and decreased lipid and protein oxidative stress in the mutant retinas . Additionally, activation of Sigma1R initially increased expression of the key antioxidant transcription factor NRF2 and downstream antioxidant genes, which then returned to WT levels over the course of the disease. The finding that activation of Sigma1R attenuates inherited photoreceptor cell loss may have far reaching therapeutic implications for retinal neurodegenerative diseases .
18.7 Mechanisms of Sigma1R Retinal Neuroprotection
Our in vivo data showing activation of Sigma1R might afford retinal neuroprotection prompted studies to understand the mechanism(s) of this neuroprotection. Pioneering work from Su’s laboratory showed that Sigma1R acts as a ligand-operated molecular chaperone at the mitochondria-associated endoplasmic reticulum (ER) membrane [45–47]. The ER is the entry site for proteins into the secretory pathway. Proteins are translocated into the ER lumen in an unfolded state and require protein chaperones and catalysts of protein folding to attain their final appropriate conformation. A sensitive system termed the unfolded protein response (UPR) prevents misfolded proteins from progressing through the secretory pathway and directs them toward a degradative pathway. Proteins such as BiP (a 78-kDa glucose-regulated protein also known as GRP78) and its downstream effector proteins (e.g., PERK, IRE1, and ATF6) have been studied extensively to determine whether ER stress is involved in pathogenesis of diabetes, atherosclerosis, and neurodegenerative disorders. ER stress is implicated in the pathogenesis of diabetic retinopathy and other retinal diseases [48].
We investigated whether chronic stress in vitro (oxidative stress model) and in vivo stress (diabetes) altered Sigma1R and BiP expression in retinal neurons, how the interaction between these proteins may be altered during oxidative stress, and whether (+)-PTZ alters Sigma1R–BiP binding and expression of ER stress-related genes in these models [20]. We conducted experiments in primary ganglion cells , which showed marked sensitivity to oxidative stress, characterized by neurite process disruption and cellular apoptosis. Oxidative stress increased expression of the proteins that initiate and execute apoptosis (caspase-9 and -3, respectively) and the upstream pro-apoptotic genes FasL andTRAIL. (+)-PTZ treatment reduced caspase-9 and -3 levels and the pro-apoptotic genes. Expression of the anti-apoptotic gene Survivin increased when oxidatively stressed cells were treated with (+)-PTZ. Neurite disruption detected in primary ganglion cells exposed to oxidative stress was not observed in (+)-PTZ-treated cells. We used the RGC5 cell line to analyze the interaction of Sigma1R with BiP under oxidative stress. Exposing these cells to xanthine:xanthine oxidase as an oxidative stressor did not alter Sigma1R protein levels over the 18-hour period examined; however it increased binding of Sigma1R to BiP [20]. When the cells were treated with (+)-PTZ [3 μM], Sigma1R–BiP binding was at baseline level. Our data are similar to those in the glucose-deprivation model [46], wherein Sigma1R–BiP interaction appeared to increase rather than the thapsigargin stress model in which σR1 dissociated from BiP .
Many proteins are regulated by phosphorylation resulting in an increase or decrease of biological activity, movement between subcellular compartments, and interactions with other proteins. We asked whether there are differences in Sigma1R phosphorylation under oxidative stress conditions, specifically phosphorylation of serine and tyrosine residues [20]. While there was no difference in tyrosine phosphorylation under stress, there was a robust increase in phosphorylation of serine (sixfold by 18 h of oxidative stress). Sigma1R serine phosphorylation in oxidatively-stressed cells decreased markedly when the cells were treated with (+)-PTZ. Our studies showed Sigma1R phosphorylation is altered by cellular stress and by ligand treatment. Phosphorylation of Sigma1R may facilitate its binding to BiP, as the increase in Sigma1R–BiP interaction parallels phosphorylation of Sigma1R. Additional studies are needed to demonstrate this potentially interesting and important phenomenon unequivocally. Sigma1R binding to proteins is not limited to BiP; it interacts also with IP3R3 receptors [46]. There have been reports that Sigma1R interacts with L-type calcium channels in ganglion cells [19, 49], although reports from del Pozo’s group in fura-2-loaded synaptosomes harvested from WT and Sigma1R −/− mice suggest that Sigma1R is not involved in calcium influx via calcium channels [50]. Clearly, this is an area that warrants further investigation. It is noteworthy that studies have shown that Sigma1R may be involved in the regulation of output signaling of ganglion cells by preferentially modulating NMDA receptor-mediated light-evoked excitatory postsynaptic currents (eEPSCs) of these retinal neurons [51]. This group showed that suppression of NMDA responses of rat retinal ganglion cells caused by the activation of Sigma1R may be mediated by a distinct intracellular calcium-dependent PLC-PKC pathway [52] .
We investigated ER stress in neural retinas from diabetic Ins2 Akita/+ mice treated with (+)-PTZ over the course of several weeks [20]. Several of the same genes that had increased in our in vitro system (BiP, PERK, IRE1a, and ATF4) were increased in the in vivo diabetic model and expression levels were similar to control values when the mice were treated with (+)-PTZ. It appears that as with the in vitro system, (+)-PTZ attenuates upregulation of ER stress genes in an in vivo model of diabetic retinopathy .
While the role of Sigma1R in ER stress was supported by our data [20], we were interested in other genes (not necessarily directly linked to ER stress) whose expression might be altered by σR1 ligands in vivo. We analyzed the retinal transcriptome in diabetic mice using gene array technology [20]. Interesting data emerged showing alterations in diabetic conditions that were reversed with the 4-week (+)-PTZ treatment. Included among the affected genes were Frzp and slit homolog 1, genes involved in cell differentiation and axon guidance, respectively. Expression of crystallins γ-B and -D was reversed markedly when diabetic mice were treated with (+)-PTZ. These data are noteworthy, given that proteins of the crystallin superfamily increase dramatically in early diabetic retinopathy reviewed in [53]. Another gene with altered expression in the Ins2 Akita/+ mouse , which was reversed by (+)-PTZ treatment, was VEGF receptor 1. VEGF (vascular endothelial growth factor) is a molecule involved in numerous physiological functions, including angiogenesis . VEGF bioactivity is transmitted through the binding of specific receptors (VEGF receptor 1, 2, and 3). Our data show an elevation of VEGFR1 in diabetic mice compared with WT mice, but a decrease in receptor expression when (+)-PTZ was administered to diabetic animals. A number of other genes related to antioxidant function, axon guidance and calcium signaling were also altered in this model following treatment with (+)-PTZ [20] .
18.8 Evaluation of the Eye and Retina of Sigma1R −/− Mice
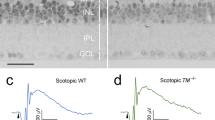
Given its abundant expression in the eye, its role in neuroprotection and cell survival, and its putative molecular chaperone role, we postulated that Sigma1R would be critical for ocular development and/or maintenance of normal ocular structure/function. The consequences of absence of Sigma1R on ocular phenotype had not been investigated, but the availability of genetically manipulated mice lacking Sigma1R (Sigma1R −/− mice) offered a tool to clarify the role of σR1 in ocular development and disease. In collaboration with Dr. E. Zorrilla , Scripps Institute, La Jolla, CA we established a colony of Sigma1R −/− mice. To determine whether Sigma1R was critical for ocular development and/or maintenance of normal ocular structure/function, we used functional, morphologic, and cell biological tools to examine comprehensively the ocular phenotype in Sigma1R −/− versus wildtype (WT, Sigma1R +/+) mice over a 1-year period [54]. The anterior segment of the eye (cornea, lens, and ciliary body-iris) is normal in Sigma1R −/− mice and intraocular pressure (IOP) is within normal limits at least through 1 year. In the retina , however, there are electrophysiological changes in Sigma1R −/− mice including significantly decreased ERG b-wave amplitudes and diminished negative scotopic threshold responses (nSTR ) detected at 12 months, consistent with inner retina dysfunction (Fig. 18.5a). Comprehensive morphometric analyses reveal significantly fewer cells in the ganglion cell layer (GCL) by one year and an increase in cells undergoing apoptosis in this layer (Fig. 18.5b, d). Interestingly, we did not observe dying cells in the GCL in mice that were younger than 6 months; however, we did observe alterations in the optic nerve head (ONH) of the Sigma1R −/− mice. At 18 weeks, TUNEL-positive cells were present in the astrocyte -rich region of the ONH, which forms a mesh-like network of glial cells through which ganglion cell axons pass. The astrocytes are intimately associated with axons of the ONH. Within this glial laminar region of the optic nerve, many TUNEL-positive glial cells were detected. The ultrastructural analysis of the ONH revealed disruption of the axonal processes. The axon fibers in the Sigma1R −/− mice were swollen with accumulation of various organelles, especially mitochondria. It appears that alterations of the ONH presage the retinal dysfunction and death observed in later months in these mice. The data suggest that σR1 is critical in maintaining inner retinal function [54] The alterations of the ONH and subsequent ganglion cell loss were not accompanied by an increase in IOP or a change in retinal vascularization [54].
Late onset retinal dysfunction in Sigma1R −/− mice. Sigma1R is not required for normal retinal development. By 6 months however, dying cells are detected in the optic nerve head; by 1 year there is loss of RGC function (e.g. decreased negative scotopic threshold responses (nSTR ) of the ERG (a). Retinal cryosections were stained to detect neurons in the ganglion cell layer (gcl) (green fluorescence, left panels) or active caspase-3, an apoptosis marker (red fluorescence, right panels). There are fewer cells in the gcl of Sigma1R −/− mice compared to WT (b). Electron microscopy was performed to evaluate health and integrity of ganglion cells in retinas of WT and Sigma1R −/− mice. Electron micrographs show the nerve fiber layer (nfl) is labeled and just below it are plump RGC bodies in WT retinas . In Sigma1R −/− retinas are areas of cell drop out (“*” denotes missing cells) (c). The numbers of cells in the ganglion cell layer was quantified and cell loss was worse in the central retina (d; *p < 0.05). The complete assessment of this late-onset retinal degeneration has been published [54] (IOVS, with permission, portions of figs. 4 and 9, Ref. [54])
Recently, investigations from Guo’s lab analyzed whether Sigma1R had any role in an acute retinal injury model [55]. They performed intraorbital optic nerve crush in Sigma1R −/− mice and determined that the number of surviving cells in the GCL of Sigma1R −/− mice was significantly decreased (18.5 %) compared to WT mice subjected to the same injury. Their data strongly support the notion that lack of Sigma1R increases susceptibility to acute retinal injury and they found that if Sigma1R is present in retina crush-induced degeneration, ganglion cell loss is attenuated. The effects of chronic stress to the retina in the absence of Sigma1R, however, had not been explored. We investigated whether the late-onset RGC death reported for Sigma1R −/− mice [54] would be accelerated under the chronic stress of diabetes. Diabetes was induced in WT mice and Sigma1R −/− mice by injecting streptozotocin at 3 weeks of age [56]. Eyes were evaluated 12 weeks post onset of diabetes when mice were 15 weeks of age. When Sigma1R −/− mice non-DB mice were analyzed at this age, no functional deficits or structural alterations were observed, confirming earlier findings [54]. However, rendering the Sigma1R −/− mice diabetic accelerated retinal dysfunction [56]. Retinas were examined functionally by assessing IOP and nSTRs . Sigma1R −/−-DB mice had IOPs that were significantly elevated at night compared to Sigma1R −/− non-DB mice as well as to WT non-DB and WT-DB mice. The levels detected were ~15 mmHg, which is within the normal range; nevertheless, the elevation in Sigma1R −/−-DB was significantly greater than in the other mouse groups examined. We also performed functional tests on the animals and detected a marked decrease in nSTRs in the Sigma1R −/−-DB mice compared to the other mice in the study. The nSTRs ranged between 9 and 13 μV for WT non-DB, WT-DB, and Sigma1R −/−- non-DB mice compared to ~5 μV in the Sigma1R −/−-DB mice [56]. The nSTR is a highly sensitive test for RGC activity; thus, these data provide strong evidence that σR1 modulates ganglion cell function under chronic stress. As was the case with acute stress [55], chronic stress can accelerate ganglion cell dysfunction in the absence of Sigma1R. Accompanying the decreased ganglion cell function was a decrease in the numbers of Brn3a-positive cells detected in the ganglion cell layer of Sigma1R −/−-DB mice compared with WT mice. Our data clearly show that there is a much earlier loss of ganglion cells and evidence of inner retinal dysfunction in Sigma1R −/−-DB mice compared with WT mice; this supports the role of Sigma1R in forestalling retinal stress. There was a decrease in the number of ganglion cells in Sigma1R −/−-DB compared to Sigma1R −/−-(nondiabetic), although the decrease was similar to the decrease in cell number between WT and WT-DB. It appears that cell loss as an endpoint is not as severe an indicator as the nSTR and IOP changes we observed [56]. The in vivo data comparing diabetic versus nondiabetic Sigma1R −/− mice allowed us to investigate the role of chronic stress on retinal function in the absence of Sigma1R. The acceleration of ganglion cell dysfunction during chronic diabetic stress coupled with the late onset inner retinal dysfunction of nondiabetic Sigma1R −/− mice underscores the role of this protein as a stress modulator.
18.9 Evidence that Sigma1R Is Required for (+)-PTZ Retinal Neuroprotection
In in vitro and in vivo studies, we observed considerable neuroprotection using (+)-PTZ. We took advantage of the observation that the absence of Sigma1R does not hinder normal retinal development [54] and used Sigma1R −/− mice to investigate whether the previously reported neuroprotective effects of (+)-PTZ are mediated via Sigma1R. While (+)-PTZ is considered a highly specific ligand for Sigma1R with an affinity in the nanomolar range (0.0046 μM [Kd]) [57], it had not been demonstrated unequivocally that (+)-PTZ mediates neuroprotection via Sigma1R. Moreover, there have been reports of alternative targets for (+)-PTZ [58]. Thus, we designed an experiment to examine this question specifically in ganglion cells , because of their vulnerability in diabetic retinopathy [29]. By isolating ganglion cells from WT mice and from Sigma1R −/− mice, we had a neuronal population that either did or did not contain Sigma1R. The cells could be manipulated using a known stressor and we had clear endpoints (neurite processes, TUNEL positivity) that could be analyzed in a straightforward manner to inform whether (+)-PTZ afforded protection. RGCs were isolated following a well-established immunopanning procedure from neonatal WT and Sigma1R −/− mice; they were cultured under oxidative stress conditions with or without (+)-PTZ. The data showed that ganglion cells from Sigma1R −/− mice succumbed to oxidative stress in a manner similar to those harvested from WT; however, unlike WT-treated cells, (+)-PTZ did not prevent death in cells isolated from Sigma1R −/− mice. That is, (+)-PTZ did not protect against oxidative stress in cells lacking Sigma1R. These findings provide compelling evidence that neuroprotective effects of (+)-PTZ are obligatorily dependent on Sigma1R. Our recent studies demonstrating cone photoreceptor preservation in rd10 mice revealed no protective effects if (+)-PTZ was administered in rd10/Sigma1R –/– mice [43].
18.10 Additional Mechanisms of Sigma1R Neuroprotection Involving Retinal Müller Glial Cells
Several laboratories have been exploring mechanisms by which Sigma1R mediates retinal neuroprotection and many of these investigators describe their findings in other chapters in this book. Our group has been exploring how Sigma1R may mediate neuronal protection via its actions on glial cells, particularly Müller glial cells. The interactions between glia and neurons contribute to retinal homeostasis as reviewed in detail [59]. It has been proposed that cooperativity exists among retinal cells that arise from a common stem cell to form a columnar array [60]. The idea is that the retina is constituted by many functional units in which local interactions occur between the group of retinal neurons and their supportive Müller glial cell, limiting the sphere of influence of the latter. Thus, each Müller cell may only have to meet the requirements of its immediate neighbors for the extracellular environment to remain stable in the face of intense neural activity.
We had established earlier that Sigma1R is present in Müller cells [36] and we knew that Müller cells isolated from Sigma1R −/− mice showed an increase in ER stress proteins [61]. A common feature of retinal disease is Müller cell reactive gliosis, which includes cytokine release. We investigated whether lipopolysaccharide (LPS) stimulates cytokine release by primary mouse Müller cells and whether (+)-PTZ could alter that release [62]. Using a highly sensitive inflammatory cytokine array we observed significant release of macrophage inflammatory proteins (MIP1γ, MIP2, MIP3α) and interleukin-12 (IL12 (p40/p70)) in LPS-treated cells compared to controls, and a significant decrease in secretion upon (+)-PTZ treatment. Müller cells from Sigma1R −/− mice demonstrated increased MIP1γ, MIP2, MIP3α and IL12 (p40/p70) secretion when exposed to LPS compared to LPS-stimulated WT cells. Cells exposed to LPS demonstrated increased NFκB nuclear location, which was reduced significantly by (+)-PTZ-treatment. NFκB, which is the abbreviation for nuclear factor kappa-light-chain-enhancer of activated B cells, is a protein complex that controls transcription of DNA, cytokine production and cell survival. Media conditioned by LPS-stimulated-Müller cells induced leukocyte-endothelial cell adhesion and endothelial cell migration, which was attenuated by (+)-PTZ treatment [62]. The findings suggest that release of certain inflammatory cytokines by Müller cells can be attenuated by Sigma1R ligands providing insights into the retinal neuroprotective role of this receptor.
Reactive gliosis can also be caused by oxidative stress , which figures prominently in retinal diseases , including diabetic retinopathy , glaucoma , and retinitis pigmentosa. Since Müller cells are essential for homeostatic support of the retina , we investigated whether Sigma1R mediates the oxidative stress response of Müller cells using WT and Sigma1R −/− mice [63]. We observed increased endogenous reactive oxygen species (ROS) levels in Sigma1R −/− mouse Müller cells compared to WT, which was accompanied by decreased expression of the genes encoding antioxidants Sod1, catalase, Nqo1, Hmox1, Gstm6, and Gpx1. The protein levels of SOD1, CAT, NQO1, and GPX1 were also significantly decreased. The genes encoding these antioxidants contain an antioxidant response element (ARE), which under stress is activated by NRF2, a transcription factor that typically resides in the cytoplasm bound by KEAP1. In the Sigma1R −/− Müller cells, Nrf2 expression was decreased significantly at the gene (and protein) level, whereas Keap1 gene (and protein) levels were markedly increased. NRF2-ARE binding affinity was decreased markedly in Sigma1R −/− Müller cells. We investigated system xc(−), the cystine-glutamate exchanger, which is critical for synthesis of glutathione (GSH) [64], and observed decreased function in Sigma1R −/− Müller cells compared to WT as well as decreased GSH and GSH/GSSG ratios [63]. This was accompanied by decreased gene and protein levels of xCT, the unique component of system xc(−). Thus it appears that Müller glial cells lacking Sigma1R manifest elevated ROS, perturbation of antioxidant balance, suppression of NRF2 signaling, and impaired function of system xc(−). The data suggest that the oxidative stress-mediating function of retinal Müller glial cells may be compromised in the absence of Sigma1R. The neuroprotective role of Sigma1R may be linked directly to the oxidative stress-mediating properties of supportive glial cells. Future studies to evaluate the role of Sigma1R in modulating NRF2 and KEAP1 will provide important insights about whether this constitutes a key mechanism by which Sigma1R mediates retinal neuroprotection .
18.11 A Note About Sigma2R
Sigma receptor 2 is much less studied than Sigma1R, and is thought to be a distinct protein that shares the ability to bind some ligands common to both receptors. Whether the two receptors share overlapping biological functions is unknown. Recently, progesterone receptor membrane component 1(PGRMC1) was shown to contain the putative Sigma2R binding site [66], although additional studies suggest otherwise indicating that this issue is controversial [67]. PGRMC1 has not been studied in retina . We hypothesized that biological interactions between Sigma1R and PGRMC1 would be evidenced by compensatory upregulation of PGRMC1 in Sigma1R −/− mice. Immunofluorescence, RT-PCR, and immunoblotting methods were used to analyze expression of PGRMC1 in wild-type mouse retina and tissues from Sigma1R −/− mice were used to investigate whether a biological interaction exists between Sigma1R and PGRMC1 [67]. We found that in the eye, PGRMC1 is expressed in corneal epithelium, lens, ciliary body epithelium, and retina. In retina, PGRMC1 is present in Müller cells and retinal pigment epithelium. This expression pattern is similar, but not identical to Sigma1R. PGRMC1 protein levels in neural retina and eye cup from Sigma1R −/− mice did not differ from WT mice. Nonocular tissues, lung, heart, and kidney showed similar Pgrmc1 gene expression in WT and Sigma1R −/− mice. In contrast, liver, brain, and intestine showed increased Pgrmc1 gene expression in Sigma1R −/− mice. If indeed Sigma2R is PGRMC1 [66], our work showed that deletion of Sigma1R did not result in compensatory change in PGRMC1 [67]. Future studies await the precise clarification of the molecular identity of Sigma2R at which time its role in retina can be investigated comprehensively.
18.12 Conclusions
Sigma receptors were first described 40 years ago and since that time there have been nearly 4000 articles published regarding the function of this enigmatic protein. Many of the studies have focused on its role in brain and in neurodegenerative diseases. Over the past 20 years, there have been increasing reports of the role of Sigma1R in the eye. Within the eye, the light sensitive retina has been the subject of many studies. As noted in this chapter and several others in this book, a number of very important roles have been ascribed to Sigma1R. In this chapter we have attempted to provide a brief overview of the earliest pharmacological studies showing that Sigma1R was present in eye followed by descriptions of studies localizing Sigma1R in various tissues including retina. Increasingly, it has become clear that Sigma1R ligands exert profound neuroprotection in retina including in retinal ganglion cells and now more recently in photoreceptor cells . Studies have utilized cell lines and primary cell culture to determine mechanisms by which Sigma1R effects neuroprotection. The availability of mice lacking Sigma1R (Sigma1R −/− mice) has provided a powerful tool to explore the role of Sigma1R in retina and to evaluate the specificity of Sigma1R ligands. Data suggest that in retina, Sigma1R plays a key role in modulating cellular stress.
References
Levin L, Nilsson FE, Ver Hoeve J, Wu S, Kaufman PL, Alm A (2011) Adler’s physiology of the eye, 11th edn. Saunders/Elsevier, New York
Ryan SJ, Sadda SR, Hinton DR, Schachat AP, Wilkinson CP, Wiedemann P (2013) Retina, 5th edn. Saunders/Elsevier, New York
Martin WR, Eades CG, Thompson JA, Huppler RE, Gilbert PE (1976) The effects of morphine- and nalorphine- like drugs in the nondependent and morphine-dependent chronic spinal dog. J Pharmacol Exp Ther 197:517–532
Schoenwald RD, Barfknecht CF, Xia E, Newton RE (1993) The presence of sigma-receptors in the lacrimal gland. J Ocul Pharmacol 9:125–139
Bucolo C, Campana G, Di Toro R, Cacciaguerra S, Spampinato S (1999) Sigma1 recognition sites in rabbit iris-ciliary body: topical sigma1-site agonists lower intraocular pressure. J Pharmacol Exp Ther 289:1362–1369
Senda T, Matsuno K, Mita S (1997) The presence of sigma receptor subtypes in bovine retinal membranes. Exp Eye Res 64:857–860
Kekuda R, Prasad PD, Fei YJ, Leibach FH, Ganapathy V (1996) Cloning and functional expression of the human type 1 sigma receptor (hSigmaR1). Biochem Biophys Res Commun 229:553–558
Seth P, Fei YJ, Li HW, Huang W, Leibach FH, Ganapathy V (1998) Cloning and functional characterization of a sigma receptor from rat brain. J Neurochem 70:922–931
Seth P, Leibach FH, Ganapathy V (1997) Cloning and structural analysis of the cDNA and the gene encoding the murine type 1 sigma receptor. Biochem Biophys Res Commun 241:535–540
Hanner M, Moebius FF, Flandorfer A, Knaus HG, Striessnig J, Kempner E, Glossmann H (1996) Purification, molecular cloning, and expression of the mammalian sigma1-binding site. Proc Natl Acad Sci U S A 93:8072–8077
Ola MS, Moore P, El-Sherbeny A, Roon P, Agarwal N, Sarthy VP, Casellas P, Ganapathy V, Smith SB (2001) Expression pattern of sigma receptor 1 mRNA and protein in mammalian retina. Brain Res Mol Brain Res 95:86–95
Jbilo O, Vidal H, Paul R, De Nys N, Bensaid M, Silve S, Carayon P, Davi D, Galiègue S, Bourrié B, Guillemot JC, Ferrara P, Loison G, Maffrand JP, Le Fur G, Casellas P (1997) Purification and characterization of the human SR 31747A-binding protein. A nuclear membrane protein related to yeast sterol isomerase. J Biol Chem 272:27107–27115
Liu LL, Wang L, Zhong YM, Yang XL (2010) Expression of sigma receptor 1 mRNA and protein in rat retina. Neuroscience 167:1151–1159
Mavlyutov TA, Epstein M, Guo LW (2015) Subcellular localization of the sigma-1 receptor in retinal neurons – an electron microscopy study. Sci Rep 5:10689
Senda T, Mita S, Kaneda K, Kikuchi M, Akaike A (1998) Effect of SA4503, a novel sigma1 receptor agonist, against glutamate neurotoxicity in cultured rat retinal neurons. Eur J Pharmacol 342:105–111
Krishnamoorthy RR, Agarwal P, Prasanna G, Vopat K, Lambert W, Sheedlo HJ, Pang IH, Shade D, Wordinger RJ, Yorio T, Clark AF, Agarwal N (2001) Characterization of a transformed rat retinal ganglion cell line. Brain Res Mol Brain Res 86:1–12
Krishnamoorthy RR, Clark AF, Daudt D, Vishwanatha JK, Yorio T (2013) A forensic path to RGC-5 cell line identification: lessons learned. Invest Ophthalmol Vis Sci 54:5712–5719
Tchedre KT, Yorio T (2008) Sigma-1 receptors protect RGC-5 cells from apoptosis by regulating intracellular calcium, Bax levels, and caspase-3 activation. Invest Ophthalmol Vis Sci 49:2577–2588
Tchedre KT, Huang RQ, Dibas A, Krishnamoorthy RR, Dillon GH, Yorio T (2008) Sigma-1 receptor regulation of voltage-gated calcium channels involves a direct interaction. Invest Ophthalmol Vis Sci 49:4993–5002
Ha Y, Dun Y, Thangaraju M, Duplantier J, Dong Z, Liu K, Ganapathy V, Smith SB (2011) Sigma receptor 1 modulates endoplasmic reticulum stress in retinal neurons. Invest Ophthalmol Vis Sci 52:527–540
Bucolo C, Marrazzo A, Ronsisvalle S, Ronsisvalle G, Cuzzocrea S, Mazzon E, Caputi A, Drago F (2006) A novel adamantane derivative attenuates retinal ischemia-reperfusion damage in the rat retina through sigma1 receptors. Eur J Pharmacol 536:200–203
Bucolo C, Drago F (2004) Effects of neurosteroids on ischemia-reperfusion injury in the rat retina: role of sigma1 recognition sites. Eur J Pharmacol 498:111–1114
Campana G, Bucolo C, Murari G, Spampinato S (2002) Ocular hypotensive action of topical flunarizine in the rabbit: role of sigma 1 recognition sites. J Pharmacol Exp Ther 303:1086–1094
Bucolo C, Drago F, Lin LR, Reddy VN (2006) Sigma receptor ligands protect human retinal cells against oxidative stress. Neuroreport 17:287–291
Barber AJ, Lieth E, Khin SA, Antonetti DA, Buchanan AG, Gardner TW (1998) Neural apoptosis in the retina during experimental and human diabetes. Early onset and effect of insulin J Clin Invest 102:783–791
Barber AJ, Antonetti DA, Kern TS, Reiter CE, Soans RS, Krady JK, Levison SW, Gardner TW, Bronson SK (2005) The Ins2Akita mouse as a model of early retinal complications in diabetes. Invest Ophthalmol Vis Sci 46:2210–2218
Lee R, Wong TY, Sabanayagam C (2015) Epidemiology of diabetic retinopathy, diabetic macular edema and related vision loss. Eye Vis (Lond) 30(2):17
Antonetti DA, Barber AJ, Bronson SK, Freeman WM, Gardner TW, Jefferson LS, Kester M, Kimball SR, Krady JK, LaNoue KF, Norbury CC, Quinn PG, Sandirasegarane L, Simpson IA, JDRF Diabetic Retinopathy Center Group (2006) Diabetic retinopathy: seeing beyond glucose-induced microvascular disease. Diabetes 55:2401–2411.
Kern TS, Barber AJ (2008) Retinal ganglion cells in diabetes. J Physiol 586:4401–4408
Ola MS, Moore P, Maddox D, El-Sherbeny A, Huang W, Roon P, Agarwal N, Ganapathy V, Smith SB (2002) Analysis of sigma receptor (sigmaR1) expression in retinal ganglion cells cultured under hyperglycemic conditions and in diabetic mice. Brain Res Mol Brain Res 107:97–107
Martin PM, Ola MS, Agarwal N, Ganapathy V, Smith SB (2004) The sigma receptor ligand (+)-pentazocine prevents apoptotic retinal ganglion cell death induced in vitro by homocysteine and glutamate. Brain Res Mol Brain Res 123:66–75
Barres BA, Silverstein BE, Corey DP, Chun LL (1988) Immunological, morphological, and electrophysiological variation among retinal ganglion cells purified by panning. Neuron 1:791–803
Dun Y, Mysona B, Van Ells T, Amarnath L, Ola MS, Ganapathy V, Smith SB (2006) Expression of the cystine-glutamate exchanger (xc-) in retinal ganglion cells and regulation by nitric oxide and oxidative stress. Cell Tissue Res 324:189–202
Dun Y, Thangaraju M, Prasad P, Ganapathy V, Smith SB (2007) Prevention of excitotoxicity in primary retinal ganglion cells by (+)-pentazocine, a sigma receptor-1 specific ligand. Invest Ophthalmol Vis Sci 48:4785–4794
Reichenbach A, Bringmann A (2013) New functions of Müller cells. Glia 61:651–678
Jiang G, Mysona B, Dun Y, Gnana-Prakasam JP, Pabla N, Li W, Dong Z, Ganapathy V, Smith SB (2006) Expression, subcellular localization, and regulation of sigma receptor in retinal Müller cells. Invest Ophthalmol Vis Sci 47:5576–5582
Umapathy NS, Li W, Mysona BA, Smith SB, Ganapathy V (2005) Expression and function of glutamine transporters SN1 (SNAT3) and SN2 (SNAT5) in retinal Müller cells. Invest Ophthalmol Vis Sci 46:3980–3987
Su TP (1982) Evidence for sigma opioid receptor: binding of [3H]SKF-10047 to etorphine-inaccessible sites in guinea-pig brain. J Pharmacol Exp Ther 223:284–290
Goldstein IM, Ostwald P, Roth S (1996) Nitric oxide: a review of its role in retinal function and disease. Vision Res. 36:2979–2994
Schmetterer L, Findl O, Fasching P, Ferber W, Strenn K, Breiteneder H, Adam H, Eichler HG, Wolzt M (1997) Nitric oxide and ocular blood flow in patients with IDDM. Diabetes 46:653–658
Smith SB, Duplantier J, Dun Y, Mysona B, Roon P, Martin PM, Ganapathy V (2008) In vivo protection against retinal neurodegeneration by sigma receptor 1 ligand (+)-pentazocine. Invest Ophthalmol Vis Sci 49:4154–4161
Shimazawa M, Sugitani S, Inoue Y, Tsuruma K, Hara H (2015) Effect of a sigma-1 receptor agonist, cutamesine dihydrochloride (SA4503), on photoreceptor cell death against light-induced damage. Exp Eye Res 132:64–72
Wang J, Saul A, Roon P, Smith SB (2016) Activation of the molecular chaperone, sigma 1 receptor, preserves cone function in a murine model of inherited retinal degeneration. Proc Natl Acad Sci 113:E3664–E3672
Wang J, Saul A, Roon P, Smith SB (2016) Activation of the molecular chaperone, sigma 1 receptor, preserves cone function in a murine model of inherited retinal degeneration. Proc Natl Acad Sci U S A 113(26):E3764–E3772
Hayashi T, Su TP (2007) Sigma-1 receptor chaperones at the ER-mitochondrion interface regulate Ca(2+) signaling and cell survival. Cell 131:596–610
Su TP, Hayashi T, Maurice T, Buch S, Ruoho AE (2010) The sigma-1 receptor chaperone as an inter-organelle signaling modulator. Trends Pharmacol Sci 31:557–566
Tsai SY, Hayashi T, Mori T, Su TP (2009) Sigma-1 receptor chaperones and diseases. Cent Nerv Syst Agents Med Chem 9:184–189
Zhang SX, Ma JH, Bhatta M, Fliesler SJ, Wang JJ (2015) The unfolded protein response in retinal vascular diseases: implications and therapeutic potential beyond protein folding. Prog Retin Eye Res 45:111–131
Mueller BH, Park Y, Daudt DR, Ma HY, Akopova I, Stankowska DL, Clark AF, Yorio T (2013) Sigma-1 receptor stimulation attenuates calcium influx through activated L-type voltage gated calcium channels in purified retinal ganglion cells. Exp Eye Res 107:21–31
González LG, Sánchez-Fernández C, Cobos EJ, Baeyens JM, del Pozo E (2012) Sigma-1 receptors do not regulate calcium influx through voltage-dependent calcium channels in mouse brain synaptosomes. Eur J Pharmacol 677:102–106
Zhang XJ, Liu LL, Wu Y, Jiang SX, Zhong YM, Yang XL (2011) σ receptor 1 is preferentially involved in modulation of N-methyl-D-aspartate receptor-mediated light-evoked excitatory postsynaptic currents in rat retinal ganglion cells. Neurosignals 19:110–116
Zhang XJ, Liu LL, Jiang SX, Zhong YM, Yang XL (2011) Activation of the sigma receptor 1 suppresses NMDA responses in rat retinal ganglion cells. Neuroscience 177:12–22
Kannan R, Sreekumar PG, Hinton DR (2012) Novel roles for α-crystallins in retinal function and disease. Prog Retin Eye Res 31:576–604
Ha Y, Saul A, Tawfik A, Williams C, Bollinger K, Smith R, Tachikawa M, Zorrilla E, Ganapathy V, Smith SB (2011) Late-onset inner retinal dysfunction in mice lacking sigma receptor 1 (σR1). Invest Ophthalmol Vis Sci 52:7749–7760
Mavlyutov TA, Nickells RW, Guo LW (2011) Accelerated retinal ganglion cell death in mice deficient in the Sigma-1 receptor. Mol Vis 17:1034–1043
Ha Y, Saul A, Tawfik A, Zorrilla EP, Ganapathy V, Smith SB (2012) Diabetes accelerates retinal ganglion cell dysfunction in mice lacking sigma receptor 1. Mol Vis 18:2860–2870
McCann DJ, Weissman AD, Su TP (1994) Sigma-1 and sigma-2 sites in rat brain: comparison of regional, ontogenetic, and subcellular patterns. Synapse 17:182–189
Cobos EJ, Entrena JM, Nieto FR, Cendán CM, Del Pozo E (2008) Pharmacology and therapeutic potential of sigma(1) receptor ligands. Curr Neuropharmacol 6:344–366
Vecino E, Rodriguez FD, Ruzafa N, Pereiro X, Sharma SC (2016) Glia-neuron interactions in the mammalian retina. Prog Retin Eye Res 51:1–40
Reichenbach A, Stolzenburg JU, Eberhardt W, Chao TI, Dettmer D, Hertz L (1993) What do retinal müller (glial) cells do for their neuronal 'small siblings'? J Chem Neuroanat 6:201–213
Ha Y, Shanmugam AK, Markand S, Zorrilla E, Ganapathy V, Smith SB (2014) Sigma receptor 1 modulates ER stress and Bcl2 in murine retina. Cell Tissue Res 356:15–27
Shanmugam A, Wang J, Markand S, Perry RL, Tawfik A, Zorrilla E, Ganapathy V, Smith SB (2015) Sigma receptor 1 activation attenuates release of inflammatory cytokines MIP1γ, MIP2, MIP3α, and IL12 (p40/p70) by retinal Müller glial cells. J Neurochem 132:546–558
Wang J, Shanmugam A, Markand S, Zorrilla E, Ganapathy V, Smith SB (2015) Sigma 1 receptor regulates the oxidative stress response in primary retinal Müller glial cells via NRF2 signaling and system xc(−), the Na(+)-independent glutamate-cystine exchanger. Free Radic Biol Med 86:25–36
Lewerenz J, Hewett SJ, Huang Y, Lambros M, Gout PW, Kalivas PW, Massie A, Smolders I, Methner A, Pergande M, Smith SB, Ganapathy V, Maher P (2013) The cystine/glutamate antiporter system xc- in health and disease: from molecular mechanisms to novel therapeutic opportunities. Antioxid Redox Signal 18:522–555
Xu J, Zeng C, Chu W, Pan F, Rothfuss JM, Zhang F, Tu Z, Zhou D, Zeng D, Vangveravong S, Johnston F, Spitzer D, Chang KC, Hotchkiss RS, Hawkins WG, Wheeler KT, Mach RH (2011) Identification of the PGRMC1 protein complex as the putative sigma-2 receptor binding site. Nat Commun 2:380
Chu UB, Mavlyutov TA, Chu ML, Yang H, Schulman A, Mesangeau C, McCurdy CR, Guo LW, Ruoho AE (2015) The Sigma-2 receptor and progesterone receptor membrane component 1 are sifferent binding sites derived from independent genes. EBioMedicine 2(11):1806–1813
Shanmugam AK, Mysona BA, Wang J, Zhao J, Tawfik A, Sanders A, Markand S, Zorrilla E, Ganapathy V, Bollinger KE, Smith SB (2015) Progesterone receptor membrane component 1 (PGRMC1) expression in murine retina. Curr Eye Res 7:1–8
Acknowledgements
We acknowledge the many post-doctoral fellows, students and faculty colleagues who have worked with us in the past on studies of Sigma1R and retina including our longtime collaborator Dr. V. Ganapathy, Dr. E. Zorrilla who so graciously shared Sigma1R -/- mice and helped us establish our mouse colony and Dr. K. Bollinger for the clinical perspective she offers to our project. We thank the many individuals who have performed experiments described in this chapter including Dr. Y. Dun, Dr. Y. Ha, Dr. B. Mysona, Dr. P. Martin, Dr. A. Tawfik, Dr. S. Markand, Dr. L. Perry, Dr. A. Shanmugam, Dr. M.S. Ola, Dr. G. Jiang, Ms. J. Duplantier and Mr. C. Williams. We acknowledge the National Institutes of Health (R01 EY014560 and R21 EY13089) for their generous support of this work. We thank the administration and especially the Provost and the VP for Research of Augusta University for support of the EM/histology Core Facility and the Imaging Core Facility. We acknowledge the support for equipment necessary to test visual function provided by the Office of the Dean, Medical College of Georgia at Augusta University. J Wang, R Cui, A Saul and SB Smith are members of the James and Jean Culver Vision Discovery Institute of Augusta University; we thank the institute for facilitating interactions and fruitful discussions about this work.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG (outside the USA)
About this chapter
Cite this chapter
Wang, J., Cui, X., Roon, P., Saul, A., Smith, S.B. (2017). The Role of Sigma1R in Mammalian Retina. In: Smith, S., Su, TP. (eds) Sigma Receptors: Their Role in Disease and as Therapeutic Targets. Advances in Experimental Medicine and Biology, vol 964. Springer, Cham. https://doi.org/10.1007/978-3-319-50174-1_18
Download citation
DOI: https://doi.org/10.1007/978-3-319-50174-1_18
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-50172-7
Online ISBN: 978-3-319-50174-1
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)