Abstract
Different neurophysiological methods such as evoked potentials (EP), testing of the autonomic nervous system (ANS) or polysomnography have the potential to detect clinically silent lesions or to confirm the existence of an association between a clinical symptom and multiple sclerosis (MS); previously undetected by MRI. Therefore, in the most recent MRI criteria for the diagnosis of MS (MAGNIMS consensus guidelines), neurophysiological confirmation of optic nerve dysfunction (slowed conduction on visual EP), support dissemination in space and, in patients without concurrent visual symptoms, dissemination in time. In this chapter we will review the existing evidence regarding the role of different neurophysiological tests (specifically the role of EPs, autonomic nervous system testing and sleep testing in MS) in the diagnosis and management of MS.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
8.1 Introduction
Multiple sclerosis (MS ) is a chronic idiopathic demyelinating illness of the central nervous system and it is the leading cause of disability in young adults. In the diagnosis of MS , three main principles are applied: demonstration of dissemination in space (DIS), demonstration of dissemination in time (DIT), and reasonable exclusion of alternative explanations for the clinical presentation. The demonstration of DIS and DIT is heavily influenced with MRI, and since its introduction, this method has become the cornerstone in the diagnosis of MS with various MRI criteria applied over time (Poser et al. 1983; Polman et al. 2011). The last version of the McDonald criteria allows making a diagnosis of MS in patients with typical clinically isolated syndrome (CIS).
Despite these advancements, there is still a poor correlation between clinical symptoms and MRI findings in a substantial proportion of MS patients (Habek 2013). Different neurophysiological methods such as evoked potentials (EP ), testing of the autonomic nervous system (ANS ) or polysomnography have the potential to detect clinically silent lesions or to confirm the existence of an association between a clinical symptom and MS ; previously undetected by MRI. A nice example of the latter are EP , which have been widely used in MS , although their clinical use has been reduced after the introduction of MRI. This is not always justifiable since the information provided by evoked potentials is more related to function, unlike the information provided by MRI which is more related to anatomy. (Comi et al. 1998) Therefore in the most recent MRI criteria for the diagnosis of MS (MAGNIMS consensus guidelines), neurophysiological confirmation of optic nerve dysfunction (slowed conduction on visual EP ), support dissemination in space and, in patients without concurrent visual symptoms, dissemination in time. (Filippi et al. 2016).
In this chapter we will review the existing evidence regarding the role of different neurophysiological tests (specifically the role of EPs, autonomic nervous system testing and sleep testing in MS ) in the diagnosis and management of MS .
8.2 Evoked Potentials in Multiple Sclerosis
The role of EPs in the evaluation of MS has changed over time primarily due to advances in neuroimaging technology, dominantly the MRI. In contrast with MRI, EPs provide information about functionality and pathophysiological involvement of a certain neuroanatomic pathway (Chiappa 1997) and their clinical utility is based on their ability to reveal subclinical involvement of a sensory system in the presence of signs/symptoms suggestive for demyelinating disease (Walsh et al. 2005). In routine clinical practice, most frequently used EPs are: pattern reversal visual EPs (VEPs), brainstem auditory EP (BAEP), short latency somatosensory EP (SSEP), and motor evoked potentials (MEPs) (Chiappa 1997).
VEPs are widely used in assessment of patients with clinical signs of optic neuritis (ON) as well as in evaluation of asymptomatic involvement of visual pathways in patients with MS . The most common finding in acute ON is delayed latency of wave P100 together with amplitude reduction (Chirapapaisan et al. 2015). With recovery from ON, the amplitude improves but latency usually remains increased. The sensitivity of VEPs in patients with MS and a history of optic neuritis is about 77–100 % while the frequency of abnormal VEPs in overall patients with MS varies between studies; from 42 to 100 % (Movassat et al. 2009; Palace 2001). According to new MAGNIMS criteria, VEP is reintroduced as part of diagnostic MS criteria (Filippi et al. 2016).
BAEPs are used to detect and approximately localize symptomatic, as well as asymptomatic, dysfunctions of the auditory pathways within the auditory nerve and brainstem. The most common BAEP pathological findings in patients with MS reflect dysfunction of the upper or lower brainstem, including increased wave I-III (lower brainstem) or III-V (upper brainstem) interlatencies (La Mantia et al. 1982). According to published literature, overall sensitivity in evaluation of brainstem involvement is low (Walsh et al. 2005; Ivanković et al. 2013; Comi et al. 1993) and it is inferior to MRI and vestibular evoked myogenic potentials (VEMP) (Ivanković et al. 2013).
SSEP, elicited from the upper and lower limbs, evaluate dorsal columns and the thalamo-cortical sensory system. The diagnostic value of SSEP is most pronounced in diagnostic evaluation of patients with no evidence of demyelinating lesions on the spinal MRI. Tibial SSEP is considered to be among the most valuable EPs (Djuric et al. 2010), giving pathological findings in up to 80 % of patients with MS who do not have sensory symptoms and signs (Kraft et al. 1998). Pathological findings commonly found in tibial SSEP are increased latencies of upper thoracic and cortical response. SSEPs of the median nerve add additional value because through the P14 wave they provide information about the degree to which the lower brainstem is affected. Abnormalities of P14 were found to be a significant contributor to the functional brainstem assessment battery.
MEPs are evaluating the corticospinal tract and together with SSEPs represent a valuable neurophysiological method for evaluation of the spinal cord. Beside its diagnostic value, MEP studies in MS serve as an indication of corticospinal pathway dysfunction (Magnano et al. 2014). The pathological finding in MS is an increased central motor conduction time (CMCT), which is found to be related with EDSS values (Fuhr et al. 2001) and can predict long term disability (Schlaeger et al. 2014a).
Vestibular evoked myogenic potentials (VEMPs) have been proven to be useful in the assessment of brainstem involvement in MS (Habek 2013). VEMP presents a myogenic response to a loud acoustic stimulus and is divided into two parts, depending where the myogenic response is measured: cervical VEMP (ipsilateral sternocleidomastoid muscle, waves P13 and N23), which provides information about vestibulospinal pathways; and ocular VEMP (contralateral ocular muscle, waves N10 and P13), which provides information about the functionality of vestibuloocular reflex. The sensitivity for MS patients varies from 30 to 100% and results are characterized with an absent response, prolonged latencies and reduced amplitudes of major waves (Murofushi et al. 2001; Versino et al. 2002). According to some studies, VEMP is superior to clinical examination, MRI and BAEP in detection of brainstem lesions (Skorić et al. 2014).
8.2.1 The EP Score
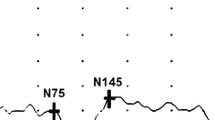
Different modalities of evoked potentials show correlation with disability and disease progression in MS patients, so it could be assumed that a combination of different evoked potential could provide even more useful information. VEP, BAEP, SSEP and MEP could be combined into a multimodal EP score, a specific scale calculated according to normative values for each of the EPs. A different degree of the significance is assigned to each of the types of abnormalities (prolonged latencies, reduced amplitude, absent response), and the level of significance is specific for every study. If the EP score consists of VEP, SSEP of upper and lower extremities where a normal response is scored with 0, prolonged latency with 1, reduced amplitude with 2 and an absent response with 3; then a patient with prolonged VEP latencies on the left side, a reduced amplitude of P40-N50 complex on the left side for tibial nerve SSEP and an absent response on the right side for the medial nerve SSEP has an EP score of 6 (1+2+3), as presented on Fig. 8.1. The EP score could be defined with ordinal values calculated according to normative values or with different transformations of raw EP data (z transformation).
Example of EP score (VEP, SSEP of upper and lower extremities) where normal response is scored with 0, prolonged latency with 1, reduced amplitude with 2, and absent response with 3: presented EP score has value of 6 (1+2+3), (a) VEP: Prolonged latency of P100 wave = 1; (b)Tibial nerve SSEP: Reduced amplitude of P40-N50 complex on the left side = 2 and (c) Medial nerve SSEP: Absent response on the right side = 3
Multimodal evoked potentials (mEPs measure and moderately predict clinically relevant disease activity in patients with early relapsing remitting MS (Jung et al. 2008). The mEPS at baseline has shown correlation with EDSS after 24 months and changes in mEPS correlated with changes in EDSS, where patients with EDSS progression showed stronger mEPD deterioration than clinically stable patients (Jung et al. 2008). A combination of VEP, BAEP, SSEP and MEP results gathered in an EP score has demonstrated a significant correlation between the EP score and EDSS score at the time of neurophysiological study and at 1, 3 and 5 years of follow-up, particularly for MEP and SEP; thus, giving rise to the evidence that EPs, particularly MEP and SEP, have significant value in predicting neurological disability (Invernizzi et al. 2011). Patients with an EP score at a baseline higher than the median value had an 72.5 % increased risk of disability progression at follow-up; meanwhile, patients with a lower EP score had a risk of only 36.3 % (Leocani et al. 2006), suggesting a predictive role of the multimodal EP score. This was confirmed by the fact that patients with worsening at follow-up had a significantly worse global EP score at baseline in comparison with patients without worsening (Leocani et al. 2006).
Different EPs (VEP, BAEP, SSEP and MEP) associated with the EP score have shown moderate and useful correlation with clinical status in patients with primary progressive MS – PPMS (Canham et al. 2015). The numerical score based on VEP, SSEP and MEP results correlates well with disability in PPMS and allows some prediction of the disease course over 3 years (Schlaeger et al. 2014b). Combination of VEP, BAEP and SSEP could be used as an outcome variable for determining the efficiency of a particular treatment (Margaritella et al. 2015). Treatment effects did not show any significance for EDSS, but there was improvement in EP score (mainly because of the significant decrease in VEP score) between different treatment groups (Margaritella et al. 2015). Finally, brainstem involvement in MS patients is very important in the prediction of disease progression. In an EP score that includes BAEP (Leocani et al. 2006), it has not been shown to have any statistically significant correlation between BAEP and EDSS, neither on baseline or follow-up suggesting that BAEP is insufficient in the neurophysiological evaluation of the brainstem in MS and it is necessary to include another measure of brainstem dysfunction.
It is known that VEMP is superior to BAEP in detection of brainstem involvement and because of that, the VEMP score was designed. The VEMP score presents interpretation of VEMP results quantified according to cut-off values (0 = normal response, 1 = prolonged latency, 2 = reduced amplitude, 3 = absent response) calculated separately for every recording position and combined in a unique score, with a minimal value of 0 and maximal of 12. The VEMP score is higher for MS patients with clinical signs of brainstem involvement, correlates with EDSS and disease duration and, according to multiple regression analyses, the VEMP score is a statistically significant predictor for EDSS (Gabelić et al. 2015). These results indicate that the VEMP score is sensitive to brainstem involvement and it could replace BAEP in the EP score and improve its sensitivity to brainstem involvement.
8.3 Autonomic Dysfunction in Multiple Sclerosis
The importance of the autonomic nervous system (ANS ) is well appreciated, as it is paramount for regulating function of each and every organ in the body. However, our capacity to test its activity somewhat lags behind its significance. The reason is that the ANS is unavailable for direct assessment. As we are unable to test it directly, we must rely on testing its reflexes. This kind of testing is mainly related to cardiovascular and sudomotor autonomic reflexes. The cardiovascular autonomic system is tested by the following methods: blood pressure and heart rate response to Valsalva maneuver, heart rate variability during deep breathing and blood pressure and heart rate changes during tilt table testing (Freeman 2006). Sudomotor function is most precisely assessed by the Quantitative Sudomotor Axon Reflex testing (Low et al. 1983). Combining all of these tests we can quantify the severity of ANS dysfunction using the Composite Autonomic Scoring Scale and render the impairment more precisely using the adrenergic, cardiovagal and sudomotor indexes (Low 1993). Another method of ANS assessment, nowadays gaining popularity, is the analysis of heart rate variability (HRV). In this method differences in sympathetic and parasympathetic effects on cardiac activity, reflected in the variability of beat-to-beat R-R intervals on ECG, are exploited to estimate the level of activity of each ANS branch (Shaffer et al. 2014).
Cardiovascular ANS dysfunction is commonly present in multiple sclerosis (MS ) (Adamec and Habek 2013). Furthermore, it is recognized in the early stages of the disease as the clinically isolated syndrome (Crnošija et al. 2016). Altogether, it affects up to two thirds of patients during the course of the disease (Acevedo et al. 2000). It is mainly caused by demyelinating lesions located in the periventricular region of the fourth ventricle that affect the autonomic nuclei, as well as due to the descending and ascending autonomic pathways in the medulla also being affected (Vita et al. 1993; De Seze et al. 2001). Half of MS patients experience orthostatic intolerance with presenting symptoms that can be insidious and nonspecific such as dizziness, lightheadedness and general malaise (Adamec et al. 2013a). The failure of blood pressure to remain stable in an upright position in MS patients is due to impaired sympathetic vasocostrictory reflex that is responsible for maintaining adequate blood pressure during postural change (Flachenecker et al. 1999). This, in turn, results in orthostatic hypotension (OH), a significant and sustained decrease of blood pressure upon standing (Freeman et al. 2011) (Fig. 8.2). The symptoms are caused by cerebral hypoperfusion and are typically induced by standing and quickly resolve when lying flat. If the fall of blood pressure is sufficiently pronounced it can lead to falls and even loss of consciousness with the hazard of traumatic injuries. Patients with OH are commonly fatigued and, using the HRV analysis, it has been found that reduced sympathetic activity during standing correlates with the Modified Fatigue Impact Scale in MS patients (Flachenecker et al. 2003). Another variety of orthostatic intolerance is the postural orthostatic tachycardia syndrome (PoTS). It is characterized by sustained heart rate increase on orthostatic challenge without concomitant OH (Freeman et al. 2011). PoTS is recognized to be present in MS more frequently than in healthy controls and its presence is explained by demyelinating brainstem and hemispheral lesions disrupting the physiological heart rate variability modulation (Adamec et al. 2013b; Kanjwal et al. 2010). Although the true significance of PoTS in MS is not completely elucidated, it is known that PoTS patients have a restricted ability to exercise and an increased sensation of fatigue, which may aggravate preexisting symptoms in MS . Another factor adding to the problem of fatigue in MS is reduced vagal activity that is seen to occur at a younger age in MS (Keselbrener et al. 2000).
MS patients can also present with more severe cardiovascular symptoms, which can actually be secondary to disease activity. Acute central nervous system lesions, including demyelinating lesions, can induce an increased release of catecholamines causing necrotic changes in cardiac myocytes and disrupt the endocardial conduction system leading to arrhythmias such as sinus bradycardia or paroxysmal atrial fibrillation (Sörös and Hachinski 2012; Juric et al. 2012; Chagnac et al. 1986). There have even been reports of cardiogenic shock and pulmonary edema as a presenting symptom of MS due to active lesions in the brainstem affecting the solitary tract nucleus (Midaglia et al. 2016). Furthermore, studies have shown that HRV is reduced in MS patients compared to healthy subjects (Mahovic and Lakusic 2007a; Brezinova et al. 2004) and this reduction seems to be related to disease duration (Mahovic and Lakusic 2007b). This is important since it has been found that reduced HRV is associated with an increased risk of cardiac events (Tsuji et al. 1996). Therefore, the occurrence of cardiac symptoms in an MS patient with no known cardiac disease should prompt consideration of MS relapse as a possible etiology. An interesting finding is that HRV analysis may also be useful in predicting the known cardiac side effects of fingolimod, an immunomodulatory treatment, in an individual MS patient. (Rossi et al. 2015) Reduced sweating ability has also been documented in MS patients. Quantitative assessment has shown a lower sweating response compared to healthy controls without a disease specific pattern (Saari et al. 2009). The MRI lesion load as well as neurologic disability is associated with development of thermoregulatory hypohydrosis. However, sweating impairment can already be seen in the early stage of multiple sclerosis, the clinically isolated syndrome (Crnošija et al. 2016). These abnormalities of sweating to heat exposure seem to result from the disruption of central sudomotor pathways connecting the anterior hypothalamus with the intermediolateral columns of the spine (Davis et al. 2010). It is important to stress that heat intolerance in MS patients can lead to pseudorelapses, the so called Uhthoff phenomenon, which underlines the importance of adequate thermoregulation in MS .
Although autonomic dysfunction is usually considered as a consequence of MS activity, the interaction is more complex and not completely one-sided. Namely, the ANS participates in the regulation of the immunological system via adrenergic and cholinergic receptors on the immune cells (Kohm and Sanders 2001). Its anti-inflammatory effect is mainly based on sympathetic activity that inhibits production of Th1-derived proinflammatory cytokines while stimulating production of Th2-dervied antiinflammatory cytokines (Sternberg 2016). Thus, sympathetic dysfunction, which is more pronounced in the relapsing remitting phase, increases inflammation and further potentiates MS activity. Therefore, research of ANS dysfunction in MS is not only important for the assessment of disease manifestation but also contributes to unfolding the complex mechanisms of interaction between MS and the immune system.
8.4 Sleep Disorders in Multiple Sclerosis
Sleep disorders in multiple sclerosis (MS ) are more common than in the general population and, depending on the study, they account from 25 to 54 % of cases (Barun 2013). The immunological background of disease development in both multiple sclerosis and sleep disorders has been proposed as a possible common pathophysiological mechanism and recent findings of disrupted melatonin pathways in MS patients suggest a multi-level causative mechanism of the development of sleep disorders in MS . Importantly, sleep disorders are considered to be one of the crucial etiological factors in development of fatigue, a common and debilitating symptom of MS . More precisely, decreased sleep efficiency detected by overnight polysomnography significantly correlated with fatigue and lack of energy in MS patients compared to controls (Braley et al. 2012a). Furthermore, a recent study showed that obstructive sleep apnea and sleep disturbance in MS patients were significantly associated with multiple-domain cognitive impairment such as visual memory, verbal memory, executive function, attention, processing speed, and working memory (Braley et al. 2016). However, sleep disorders are commonly undiagnosed and untreated in the MS population (Brass et al. 2014).
Although almost all of the major subgroups of sleep disorders such as insomnia, sleep disordered breathing, REM sleep behavior disorder, narcolepsy and restless legs syndrome have been described in MS patients, a higher prevalence in the MS population than in healthy controls was well established for insomnia, obstructive sleep apnea, and restless legs syndrome (RLS) (Merlino et al. 2009; Braley et al. 2014; Italian REMS Study Group et al. 2008a). Insomnia is more frequent in patients with multiple sclerosis (40 %) than in the general population (10–15 %) and it has been proposed that insomnia in MS occurs due to a multifactorial etiology associated with MS per se like nocturia, spasticity, pain and depression (Ferini-Strambi et al. 1994).
Sleep-disordered breathing are disorders characterized by respiratory abnormalities during sleep. The most common among them is obstructive sleep apnea (OSA) which is characterized by repeated collapse of the upper airway during sleep with consecutive sleep fragmentation and intermittent hypoxia resulting in increased daytime sleepiness and higher risk for development of atherosclerosis. Multiple sclerosis brainstem lesions could be additional risk factors for development of OSA (Braley et al. 2012b). One study included 62 MS patients and 32 healthy controls who where evaluated by overnight polisomnography, showed the prevalence of obstructive sleep apnea was 58 and 47 %, respectively (Kaminska and Kimoff 2012).
A high prevalence of restless leg syndrome (RLS) in MS patients has been confirmed in several studies (Auger et al. 2005; Deriu et al. 2009; Italian REMS Study Group et al. 2008b; Manconi et al. 2008) and they have been correlated with disease duration, older age and cervical cord lesions. Distinguishing RLS from other motor and sensory symptoms in MS can be difficult. Unlike leg discomfort encountered in RLS which is worse in evening, leg spasms, often seen in MS patients, are worse on awakening and can occur at any time of the day.
The prevalence of REM sleep behavior disorder (RBD) in the general population ranges from 0.38 to 0.5 % (Frenette 2010). RBD is a parasomnia characterized by loss of muscle atonia during REM sleep and consecutive abnormal motor or verbal behaviors associated with unpleasant dreams (American Academy of Sleep Medicine et al. 2005). A study that investigated prevalence of RBD in 135 MS patients and 118 healthy individuals using RBD questionnaires found four (2.9 %) MS patients and none of the healthy controls having RBD (Gómez-Choco et al. 2007). There are also case reports of RBD in MS patients which suggest that a MS lesion in the proximity of the penduculopontine nucleus causes this disorder of REM sleep (Tippman-Peikert et al. 2006; Plazzi and Montagna 2002).
In addition to the case series describing narcolepsy features in MS patients (Poirier et al. 1987), a study on the secondary causes of narcolepsy has revealed that MS is the fourth most common cause after inherited disorders, CNS tumors and brain injury; in this study, 12 % of the cases of secondary narcolepsy were due to MS (Nishino and Kanbayashi 2005). The fact that both of these diseases are related to human leukocyte antigen DQB1*0602 might suggest that similar autoimmune process may be important in development of narcolepsy and MS . Finally, hypothalamic MS lesions resulting in low CSF hypocretin levels have been described to cause hypersomnia in affected patients (Oka et al. 2004).
Several humoral immunologic factors, such as IL-1 and TNF alpha, have been implicated in development of sleep disorders and sleepiness. Since MS is proven to be characterized by immune abnormalities, the notion that MS and sleep disorders share a similar background seems plausible. However, sleep disorder should be viewed separately due its differing etiopatological grounds. Considering the fact that sleep disorders largely contribute to development of fatigue, the most common and debilitating symptom of MS , assessment of sleep disorders in multiple sclerosis is important.
8.5 Conclusion
In conclusion, EPs are reliable procedures to predict disability in MS patients. The index of global EP alteration (EP score), which combines alterations in VEP, BAEP, motor and somatosensory EP , shows significant correlation with the EDSS score at the time of neurophysiological study and at 1, 3 and 5 years of follow-up. Furthermore, autonomic nervous system dysfunction can lead to an array of clinical symptoms often observed in MS patients. There is a connection between dysfunction of autonomic cardiovascular reflexes and development of cardiac side effects of several drugs that are used in MS treatment; and cardiovascular and thermoregulatory autonomic dysfunctions in MS have considerable potential to adversely affect exercise. Finally, sleep disorders largely contribute to fatigue in MS , making formal assessment of sleep important.
Abbreviations
- ANS:
-
autonomic nervous system
- BAEP:
-
brainstem auditory EP
- CIS:
-
clinically isolated syndrome
- CMCT:
-
central motor conduction time
- DIS:
-
dissemination in space
- DIT:
-
dissemination in time
- EP:
-
evoked potentials
- HRV:
-
heart rate variability
- mEPs:
-
Multimodal evoked potentials
- MEPs:
-
motor evoked potentials
- MS:
-
multiple sclerosis
- OH:
-
orthostatic hypotension
- ON:
-
optic neuritis
- OSA:
-
obstructive sleep apnea
- PoTS:
-
orthostatic tachycardia syndrome
- RBD:
-
REM sleep behavior disorder
- RLS:
-
restless legs syndrome
- SSEP:
-
short latency somatosensory EP
- VEMP:
-
vestibular evoked myogenic potentials
- VEPs:
-
pattern reversal visual Eps
References
Acevedo AR, Nava C, Arriada N, Violante A, Corona T (2000) Cardiovascular dysfunction in multiple sclerosis. Acta Neurol Scand 101:85–88
Adamec I, Habek M (2013) Autonomic dysfunction in multiple sclerosis. Clin Neurol Neurosurg 115(Suppl 1):S73–S78
Adamec I, Bach I, Barušić AK, Mišmaš A, Habek M (2013a) Assessment of prevalence and pathological response to orthostatic provocation in patients with multiple sclerosis. J Neurol Sci 324:80–83
Adamec I, Lovrić M, Zaper D, Barušić AK, Bach I, Junaković A, Mišmaš A, Habek M (2013b) Postural orthostatic tachycardia syndrome associated with multiple sclerosis. Auton Neurosci 173:65–68
American Academy of Sleep Medicine (2005) In: Winkleman J, Kotagal S, Olson E, Scammel T, Schenk C (eds) International classification of sleep disorders: diagnostic and coding manual, 2nd edn. American Academy of Sleep Medicine, Westchester
Auger C, Montplaisir J, Duquette P (2005) Increased frequency of restless legs syndrome in a French–Canadian population with multiple sclerosis. Neurology 65:1652–1653
Barun B (2013) Pathophysiological background and clinical characteristics of sleep disorders in multiple sclerosis. Clin Neurol Neurosurg 115(Suppl 1):S82–S85
Braley TJ, Chervin RD, Segal BM (2012a) Fatigue, tiredness, lack of energy, and sleepiness in multiple sclerosis patients referred for clinical polysomnography. Mult Scler Int 2012:67393
Braley TJ, Segal BM, Chervin RD (2012b) Sleep-disordered breathing in multiple sclerosis. Neurology 79:929–936
Braley TJ, Segal BM, Chervin RD (2014) Obstructive sleep apnea and fatigue in patients with multiple sclerosis. J Clin Sleep Med 10:155–162
Braley TJ, Kratz AL, Kaplish N, Chervin RD (2016) Sleep and cognitive function in multiple sclerosis. Sleep 3:pii: sp-00688-15
Brass SD, Li CS, Auerbach S (2014) The underdiagnosis of sleep disor- ders in patients with multiple sclerosis. J Clin Sleep Med 10:1025–1031
Brezinova M, Goldenberg Z, Kucera P (2004) Autonomic nervous system dysfunction in multiple sclerosis patients. Bratisl Lek Listy 105:404–407
Canham LJ, Kane N, Oware A, Walsh P, Blake K, Inglis K, Homewood J, Witherick J, Faulkner H, White P, Lewis A, Furse-Roberts C, Cottrell DA (2015) Multimodal neurophysiological evaluation of primary progressive multiple sclerosis - An increasingly valid biomarker, with limits. Mult Scler Relat Disord 4:607–613
Chagnac Y, Martinovits G, Tadmor R, Goldhammer Y (1986) Paroxysmal atrial fibrillation associated with an attack of multiple sclerosis. Postgrad Med J 62:385–387
Chiappa K (1997) Evoked potentials in clinical medicine, 3rd edn. Raven press, Philadelphia
Chirapapaisan N, Laotaweerungsawat S, Chuenkongkaew W, Samsen P, Ruangvaravate N, Thuangtong A, Chanvarapha N (2015) Diagnostic value of visual evoked potentials for clinical diagnosis of multiple sclerosis. Doc Ophthalmol 130:25–30
Comi G, Filippi M, Martinelli V, Scotti G, Locatelli T, Medaglini S, Triulzi F, Rovaris M, Canal N (1993) Brain stem magnetic resonance imaging and evoked potential studies of symptomatic multiple sclerosis patients. Eur Neurol 33:232–237
Comi G, Martinelli V, Locatelli T, Leocani L, Medaglini S (1998) Neurophysiological and cognitive markers of disease evolution in multiple sclerosis. Mult Scler 4:260–265
Crnošija L, Adamec I, Lovrić M, Junaković A, Krbot Skorić M, Lušić I, Habek M (2016) Autonomic dysfunction in clinically isolated syndrome suggestive of multiple sclerosis. Clin Neurophysiol 127:864–869
Davis SL, Wilson TE, White AT, Frohman EM (2010) Thermoregulation in multiple sclerosis. J Appl Physiol (1985) 109:1531–1537
De Seze J, Stojkovic T, Gauvrit JY, Devos D, Ayachi M, Cassim F et al (2001) Autonomic dysfunction in multiple sclerosis: cervical spinal cord atrophy correlates. J Neurol 248:297–303
Deriu M, Cossu G, Molari A, Murgia D, Mereu A, Ferrigno P et al (2009) Restless legssyndrome in multiple sclerosis: a case–control study. Mov Disord 24:697–701
Djuric S, Djuric V, Zivkovic M, Milosevic V, Jolic M, Stamenovic J, Djordjevic G, Calixto M (2010) Are somatosensory evoked potentials of the tibial nerve the most sensitive test in diagnosing multiple sclerosis? Neurol India 58:537–541
Ferini-Strambi L, Filippi M, Martinelli V et al (1994) Nocturnal sleep study in multiple sclerosis: correlations with clinical and brain magneticresonance imaging findings. J Neurol Sci 125:194–197
Filippi M, Rocca MA, Ciccarelli O, MAGNIMS Study Group et al (2016) MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guidelines. Lancet Neurol 15:292–303
Flachenecker P, Rufer A, Bihler I, Hippel C, Reiners K, Toyka KV, Kesselring J (2003) Fatigue in MS is related to sympathetic vasomotor dysfunction. Neurology 61:851–853
Flachenecker P, Wolf A, Krauser M, Hartung HP, Reiners K (1999) Cardiovascular autonomic dysfunction in multiple sclerosis: correlation with orthostatic intolerance. J Neurol 246:578–586
Freeman R (2006) Assessment of cardiovascular autonomic function. Clin Neurophysiol 117:716–730
Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I (2011) Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Clin Auton Res 21:69–72
Frenette E (2010) REM sleep behavior disorder. Med Clin N Am 94:593–614
Fuhr P, Borggrefe-Chappuis A, Schindler C, Kappos L (2001) Visual and motor evoked potentials in the course of multiple sclerosis. Brain 124:2162–2168
Gabelić T, Krbot Skorić M, Adamec I, Barun B, Zadro I, Habek M (2015) The vestibular evoked myogenic potentials (VEMP) score: a promising tool for evaluation of brainstem involvement in multiple sclerosis. Eur J Neurol 22:261–269 e21
Gómez-Choco MJ, Iranzo A, Blanco Y, Graus F, Santamaría J, Saiz A (2007) Prevalence ofrestless legs syndrome and REM sleep behavior disorder in multiple sclerosis. Mult Scler 13:805–808
Habek M (2013) Evaluation of brainstem involvement in multiple sclerosis. Expert Rev Neurother 13:299–311
Invernizzi P, Bertolasi L, Bianchi MR, Turatti M, Gajofatto A, Benedetti MD (2011) Prognostic value of multimodal evoked potentials in multiple sclerosis: the EP score. J Neurol 258:1933–1939
Italian REMS Study Group, Manconi M, Ferini-Strambi L, Filippi M, Bonanni E, Iudice A et al (2008a) Multicenter case–control study on restless legs syndrome in multiple sclerosis: the REMS study. Sleep 31:944–952
Italian REMS Study Group, Manconi M, Ferini-Strambi L et al (2008b) Multicenter case–control study on restless legs syndrome in multiple sclerosis: the REMS study. Sleep 31:944–952
Ivanković A, Nesek Mađarić V, Starčević K, Krbot Skorić M, Gabelić T, Adamec I, Habek M (2013) Auditory evoked potentials and vestibular evoked myogenic potentials in evaluation of brainstem lesions in multiple sclerosis. J Neurol Sci 328:24–27
Jung P, Beyerle A, Ziemann U (2008) Multimodal evoked potentials measure and predict disability progression in early relapsing-remitting multiple sclerosis. Mult Scler 14:553–556
Juric S, Mismas A, Mihic N, Barac AM, Habek M (2012) Newly onset sinus bradycardia in context of multiple sclerosis relapse. Intern Med 51:1121–1124
Kaminska M, Kimoff R, Benedetti A et al (2012) Obstructive sleep apnea is associated with fatigue in multiple sclerosis. Mult Scler 18:1159–1169
Kanjwal K, Karabin B, Kanjwal Y, Grubb BP (2010) Autonomic dysfunction presenting as postural orthostatic tachycardia syndrome in patients with multiple sclerosis. Int J Med Sci 7:62–67
Keselbrener L, Akselrod S, Ahiron A, Eldar M, Barak Y, Rotstein Z (2000) Is fatigue in patients with multiple sclerosis related to autonomic dysfunction? Clin Auton Res 10:169–175
Kohm AP, Sanders VM (2001) Norepinephrine and beta 2-adrenergic receptor stimulation regulate CD4+ T and B lymphocyte function in vitro and in vivo. Pharmacol Rev 53:487–525
Kraft GH, Aminoff MJ, Baran EM, Litchy WJ, Stolov WC (1998) Somatosensory evoked potentials: clinical uses. AAEM somatosensory evoked potentials subcommittee. American association of electrodiagnostic medicine. Muscle Nerve 21:252–258
La Mantia L, Milanese C, Corridori F, Brusa M, Formenti A, Cocchini F, Richichi M (1982) Brainstem auditory evoked potentials in the diagnosis of multiple sclerosis. Ital J Neurol Sci 3:289–293
Leocani L, Rovaris M, Boneschi FM, Medaglini S, Rossi P, Martinelli V et al (2006) Multimodal evoked potentials to assess the evolution of multiple sclerosis: a longitudinal study. J Neurol Neurosurg Psychiatry 77:1030–1035
Low PA (1993) Composite autonomic scoring scale for laboratory quantification of generalized autonomic failure. Mayo Clin Proc 68:748–752
Low PA, Caskey PE, Tuck RR, Fealey RD, Dyck PJ (1983) Quantitative sudomotor axon reflex test in normal and neuropathic subjects. Ann Neurol 14:573–580
Magnano I, Pes GM, Pilurzi G, Cabboi MP, Ginatempo F, Giaconi E, Tolu E, Achene A, Salis A, Rothwell JC, Conti M, Deriu F (2014) Exploring brainstem function in multiple sclerosis by combining brainstem reflexes, evoked potentials, clinical and MRI investigations. Clin Neurophysiol 125:2286–2296
Mahovic D, Lakusic N (2007a) Progressive impairment of autonomic control of heart rate in patients with multiple sclerosis. Arch Med Res 38:322–325
Mahovic D, Lakusic N (2007b) Progressive impairment of autonomic control of heart rate in patients with multiple sclerosis. Arch Med Res 38:322–325
Manconi M, Rocca MA, Ferini-Strambi L et al (2008) Restless legs syndrome is a common finding in multiple sclerosis and correlates with cervical cord damage. Mult Scler 14:86–93
Margaritella N, Mendozzi L, Garegnani M, Nemni R, Gilardi E, Pugnetti L (2015) The EP-score to assess treatment efficacy in RRMS patients: a preliminary study. Int J Neurosci 125:38–42
Merlino G, Fratticci L, Lenchig C, Valente M, Cargnelutti D, Picello M et al (2009) Prevalence of ‘poor sleep’ among patients with multiple sclerosis: an independent predictor of mental and physical status. Sleep Med 10:26–34
Midaglia L, Juega Mariño JM, Sastre-Garriga J, Rovira A, Vidal-Jordana A, López-Pérez MA, Marzo-Sola ME, Librada Escribano F, Montalban X (2016) An uncommon first manifestation of multiple sclerosis: Tako-Tsubo cardiomyopathy. Mult Scler 22:842–846
Movassat M, Piri N, AhmadAbadi MN (2009) Visual evoked potential study in multiple sclerosis disease. Iran J Ophthalmol 21:37–44
Murofushi T, Shimizu K, Takegoshi H, Cheng PW (2001) Diagnostic value of prolonged latencies in the vestibular evoked myogenic potential. Arch Otolaryngol Head Neck Surg 127:1069–1072
Nishino S, Kanbayashi T (2005) Symptomatic narcolepsy, cataplexy and hypersomnia,and their implications in the hypothalamic hypocretin/orexin system. Sleep Med Rev 9:269–310
Oka Y, Kanbayashi T, Mezaki T et al (2004) Low CSFhypocretin-1/orexin-A associated with hypersomnia secondary to hypothalamic lesion in a case of multiple sclerosis. J Neurol 251:885–886
Palace J (2001) Making the diagnosis of multiple sclerosis. J Neurol Neurosurg Psychiatry 71:ii3–ii8
Plazzi G, Montagna P (2002) Remitting REM sleep behavior disorder as the initial sign of multiple sclerosis. Sleep Med 3:437–439
Poirier G, Montplaisir J, Dumont M et al (1987) Clinical and sleep laboratory study of narcoleptic symptoms in multiple sclerosis. Neurology 37:693–695
Polman CH, Reingold SC, Banwell B et al (2011) Diagnostic criteria for multiple sclerosis: 2010 revisions to the McDonald criteria. Ann Neurol 69:292–302
Poser CM, Paty DW, Scheinberg L et al (1983) New diagnostic criteria for multiple sclerosis: guidelines for research protocols. Ann Neurol 13:227–231
Rossi S, Rocchi C, Studer V, Motta C, Lauretti B, Germani G, Macchiarulo G, Marfia GA, Centonze D (2015) The autonomic balance predicts cardiac responses after the first dose of fingolimod. Mult Scler 21:206–216
Saari A, Tolonen U, Pääkkö E et al (2009) Sweating impairment in patients with multiple sclerosis. Acta Neurol Scand 120:358–363
Schlaeger R, Schindler C, Grize L, Dellas S, Radue EW, Kappos L, Fuhr P (2014a) Combined visual and motor evoked potentials predict multiple sclerosis disability after 20 years. Mult Scler 20:1348–1354
Schlaeger R, D’Souza M, Schindler C, Grize L, Kappos L, Fuhr P (2014b) Electrophysiological markers and predictors of the disease course in primary progressive multiple sclerosis. Mult Scler 20:51–56
Shaffer F, McCraty R, Zerr CL (2014) A healthy heart is not a metronome: an integrative review of the heart’s anatomy and heart rate variability. Front Psychol 5:1040
Skorić MK, Adamec I, Mađarić VN, Habek M (2014) Evaluation of brainstem involvement in multiple sclerosis. Can J Neurol Sci 41:346–349
Sörös P, Hachinski V (2012) Cardiovascular and neurological causes of sudden death after ischaemic stroke. Lancet Neurol 11:179–188
Sternberg Z (2016) Impaired neurovisceral integration of cardiovascular modulation contributes to multiple sclerosis morbidities. Mol Neurobiol 7:1–13 . [Epub ahead of print]
Tippman-Peikert M, Boeve BF, Keegan BM (2006) REM sleep behavior disorder initiated by acute brainstem multiple sclerosis. Neurology 66:1277–1279
Tsuji H, Larson MG, Venditti FJ Jr, Manders ES, Evans JC, Feldman CL, Levy D (1996) Impact of reduced heart rate variability on risk for cardiac events. The framingham heart study. Circulation 94:2850–2855
Versino M, Colnaghi S, Callieco R, Bergamaschi R, Romani A, Cosi V (2002) Vestibular evoked myogenic potentials in multiple sclerosis patients. Clin Neurophysiol 113:1464–1469
Vita G, Fazio MC, Milone S, Blandino A, Salvi L, Messina C (1993) Cardiovascular autonomic dysfunction in multiple sclerosis is likely related to brainstem lesions. J Neurol Sci 120:82–86
Walsh P, Kane N, Butler S (2005) The clinical role of evoked potentials. J Neurol Neurosurg Psychiatry 76(Suppl 2):ii16–ii22
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Habek, M., Adamec, I., Barun, B., Crnošija, L., Gabelić, T., Krbot Skorić, M. (2017). Clinical Neurophysiology of Multiple Sclerosis. In: Asea, A., Geraci, F., Kaur, P. (eds) Multiple Sclerosis: Bench to Bedside. Advances in Experimental Medicine and Biology, vol 958. Springer, Cham. https://doi.org/10.1007/978-3-319-47861-6_8
Download citation
DOI: https://doi.org/10.1007/978-3-319-47861-6_8
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-47860-9
Online ISBN: 978-3-319-47861-6
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)