Abstract
Computerized algorithms and solutions in processing and diagnosis mammography X-ray, cardiovascular CT/MRI scans, and microscopy image play an important role in disease detection and computer-aided decision-making. Machine learning techniques have powered many aspects in medical investigations and clinical practice. Recently, deep learning is emerging a leading machine learning tool in computer vision and begins attracting considerable attentions in medical imaging. In this chapter, we provide a snapshot of this fast growing field specifically for mammography, cardiovascular, and microscopy image analysis . We briefly explain the popular deep neural networks and summarize current deep learning achievements in various tasks such as detection, segmentation, and classification in these heterogeneous imaging modalities. In addition, we discuss the challenges and the potential future trends for ongoing work.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
1 Introduction on Deep Learning Methods in Mammography
Breast cancer is one of the most common types of cancer affecting the lives of women worldwide. Recent statistical data published by the World Health Organisation (WHO) estimates that \(23\%\) of cancer-related cases and \(14\%\) of cancer-related deaths among women are due to breast cancer [1]. The most effective tool to reduce the burden associated with breast cancer consists of early detection in asymptomatic women via breast cancer screening programs [2], which commonly use mammography for breast imaging. Breast screening using mammography comprises several steps, which include the detection and analysis of lesions, such as masses and calcifications, that are used in order to estimate the risk that the patient is developing breast cancer. In clinical settings, this analysis is for the most part a manual process, which is susceptible to the subjective assessment of a radiologist, resulting in a potentially large variability in the final estimation. The effectiveness of this manual process can be assessed by recent studies that show that this manual analysis has a sensitivity of 84% and a specificity of 91% [3]. Other studies show evidence that a second reading of the same mammogram either from radiologists or from computer-aided diagnosis (CAD) systems can improve this performance [3]. Therefore, given the potential impact that second reading CAD systems can have in breast screening programs, there is a great deal of interest in the development of such systems.
2 Deep Learning Methods in Mammography
A CAD system that can analyze breast lesions from mammograms usually comprises three steps [3]: (1) lesion detection, (2) lesion segmentation, and (3) lesion classification. The main challenges involved in these steps are related to the low signal-to-noise ratio present in the imaging of the lesion, and the lack of a consistent location, shape, and appearance of lesions [4, 5]. Current methodologies for lesion detection involve the identification of a large number of candidate regions, usually based on the use of traditional filters, such as morphological operators or difference of Gaussians [6,7,8,9,10,11,12,13]. These candidates are then processed by a second stage that aims at removing false positives using machine learning approaches (e.g., region classifier) [6,7,8,9,10,11,12,13]. The main challenges faced by lesion detection methods are that they may generate a large number of false positives, while missing a good proportion of true positives [4]; in addition, another issue is the poor alignment of the detected lesion in terms of translation and scale within the candidate regions—this issue has negative consequences for the subsequent lesion segmentation that depends on a relatively precise alignment. Lesion segmentation is then addressed with global/local energy minimisation models on a continuous or discrete space [14,15,16]. The major roadblock faced by these methods is the limited availability of annotated datasets that can be used in the training of the segmentation models. This is a particularly important problem because, differently from the detection and classification of lesions, the segmentation of lesions is not a common task performed by radiologists, which imposes strong limitations in the annotation process and, as a consequence, in the availability of annotated datasets. In fact, the main reason behind the need for a lesion segmentation is the assumption that the lesion shape is an important feature in the final stage of the analysis: lesion classification. This final stage usually involves the extraction of manually or automatically designed features from the lesion image and shape and the use of those features with traditional machine learning classifiers [17,18,19]. In this last stage, the main limitation is with respect to the features being extracted for the classification because these features are usually hand-crafted, which cannot guarantee optimality for this classification stage.
The successful use and development of deep learning methods in computer vision problems (i.e., classification and segmentation) [20,21,22,23,24] have motivated the medical image analysis community to investigate the applicability of such methods in medical imaging segmentation and classification problems. Compared to the more traditional methods presented above (for the problem of mammogram analysis), deep learning methods offer the following clear advantages: automated learning of features estimated based on specific detection/segmentation/classification objective functions; opportunity to build complete “end-to-end” systems that take an image, detect, segment, and classify visual objects (e.g., breast lesion) using a single model and a unified training process. However, the main challenge faced by deep learning methods is the need for large annotated training sets given the scale of the parameter space, usually in the order of \(10^6\) parameters. This problem is particularly important in medical image analysis applications, where annotated training sets rarely have more than a few thousand samples. Therefore, a great deal of research is focused on the adaptation of deep learning methods to medical image analysis applications that contain relatively small annotated training sets.
There has been an increasing interest in the development of mammogram analysis methodologies based on deep learning . For instance, the problem of breast mass segmentation has been addressed with the use of a structured output model, where several potential functions are based on deep learning models [25,26,27]. The assumption here is that deep learning models alone cannot produce results that are accurate enough due to the small training set size problem mentioned above, but if these models are combined with a structured output model that makes assumptions about the appearance and shape of masses, then it is possible to have a breast mass segmentation that produces accurate results—in fact this method holds the best results in the field in two publicly available datasets [19, 28]. Segmentation of breast tissue using deep learning alone has been successfully implemented [29], but it is possible that a similar structured output model could improve even more the accuracy obtained. Dhungel et al. [30] also worked on a breast mass detection methodology that consists of a cascade of classifiers based on the Region Convolutional Neural Network (R-CNN) [23] approach. The interesting part is that the candidate regions produced by the R-CNN contain too many false positives, so the authors had to include an additional stage based on a classifier to eliminate those false positives. Alternatively, Ertosun and Rubin [31] propose a deep learning -based mass detection method consisting of a cascade of deep learning models trained with DDSM [28]—the main reason that explains the succesful use of deep learning models here is the size of DDSM, which contains thousands of annotated mammograms.
The classification of lesions using deep learning [32,33,34] has also been successfully implemented in its simplest form: as a simple lesion classifier. Carneiro et al. [35] have proposed a system that can classify the unregistered two views of a mammography exam (cranial–caudal and mediolateral–oblique) and their respective segmented lesions and produce a classification of the whole exam. The importance of this work lies in its ability to process multi-modal inputs (images and segmentation maps) that are not registered, in its way of performing transfer learning from computer vision datasets to medical image analysis datasets, and also in its capability of producing high-level classification directly from mammograms. A similar high-level classification using deep learning estimates the risk of developing breast cancer by scoring breast density and texture [36, 37]. Another type of high-level classification is the method proposed by Qiu et al. [38] that assesses the short-term risk of developing breast cancer from a normal mammogram.
3 Summary on Deep Learning Methods in Mammography
Based on the recent results presented above, it is clear that the use of deep learning is allowing accuracy improvements in terms of mass detection, segmentation, and classification. All the studies above have been able to mitigate the training set size issue with the use of regularization techniques or the combination of different approaches that can compensate the relatively poor generalization of deep learning methods trained with small annotated training sets. More importantly, deep learning is also allowing the implementation of new applications that are more focused on high-level classifications that do not depend on lesion segmentation. The annotation for this higher level tasks is readily available from clinical datasets, which generally contain millions of cases that can be used to train deep learning models in a more robust manner. These new applications are introducing a paradigm shift in how the field analyzes mammograms: from the classical three-stage process (detection, segmentation, and classification of lesions) trained with small annotated datasets to a one-stage process consisting of lesion detection and classification trained with large annotated datasets.
4 Introduction on Deep Learning for Cardiological Image Analysis
Cardiovascular disease is the number one cause of death in the developed countries and it claims more lives each year than the next seven leading causes of death combined [39]. The costs for addressing cardiovascular disease in the USA will triple by 2030, from 273 billion to 818 billion (in 2008 dollars) [40]. With the capability of generating images of a patient’s inside body non-invasively, medical imaging is ubiquitously present in the current clinical practice. Various imaging modalities, such as computed tomography (CT), magnetic resonance imaging (MRI), ultrasound, and nuclear imaging, are widely available in clinical practice to generate images of the heart, and different imaging modalities meet different clinical requirements. For example, ultrasound is most widely used for cardiac function analysis (i.e., the pumping of a cardiac chamber) due to its low cost and free of radiation dose; nuclear imaging and MRI are used for myocardial perfusion imaging to measure viability of the myocardium; CT reveals the most detailed cardiac anatomical structures and is routinely used for coronary artery imaging; while fluoroscopy/angiography is the workhorse imaging modality for cardiac interventions.
Physicians review these images to determine the health of the heart and to diagnose disease. Due to the large amount of information captured by the images, it is time consuming for physicians to identify the target anatomy and to perform measurements and quantification. For example, many 3D measurements (such as the volume of a heart chamber, the heart ejection fraction, the thickness and the thickening of the myocardium, or the strain and torsion of the myocardium) are very tedious to calculate without help from an intelligent post-processing software system. Various automatic or semi-automatic cardiac image analysis systems have been developed and demonstrated to reduce the exam time (thereby increase the patient throughput), increase consistency and reproducibility of the exam, and boost diagnosis accuracy of physicians.
Cardiovascular structures are composed of the heart (e.g., cardiac chambers and valves) and vessels (e.g., arteries and veins). A typical cardiac image analysis pipeline is composed of the following tasks: detection, segmentation, motion tracking, quantification, and disease diagnosis. For an anatomical structure, detection means determining the center, orientation, and size of the anatomy; while, for a vessel, it often means extraction of the centerline since a vessel has a tubular shape [41]. Early work on cardiac image analysis usually used non-learning-based data-driven approaches, for example, from simple thresholding and region growing to more advanced methods (like active contours, level sets, graph cuts, and random walker) for image segmentation. In the past decade, machine learning has penetrated into almost all steps of the cardiac image analysis pipeline [42, 43]. The success of a machine learning-based approach is often determined by the effectiveness and efficiency of the image features.
The recent advance of deep learning demonstrates that a deep neural network can automatically learn hierarchical image representations, which often outperform the most effective hand-crafted features developed after years of feature engineering. Encouraged by the great success of deep learning on computer vision, researchers in the medical imaging community quickly started to adapt deep learning for their own tasks. The current applications of deep learning on cardiac image segmentation are mainly focused on two topics: left/right ventricle segmentation [44,45,46,47,48,49,50,51,52] and retinal vessel segmentation [53,54,55,56,57,58,59,60]. Most of them are working on 2D images as input; while 3D deep learning is still a challenging task. First, evaluating a deep network on a large volume may be too computationally expensive for a real clinical application. Second, a network with a 3D patch as input requires more training data since a 3D patch generates a much bigger input vector than a 2D patch. However, the medical imaging community is often struggling with limited training samples (often in hundreds or thousands) due to the difficulty to generate and share patients’ images. Nevertheless, we started to see a few promising attempts [61,62,63] to attack the challenging 3D deep learning tasks.
5 Deep Learning-Based Methods for Heart Segmentation
Carneiro et al. [44] presented a method using a deep belief network (DBN) to detect an oriented bounding box of the left ventricle (LV) on 2D ultrasound images of the LV long-axis views. One advantage of the DBN is that it can be pre-trained layer by layer using unlabeled data; therefore, good generalization capability can be achieved with a small number of labeled training images. A 2D-oriented bounding box has five pose parameters (two for translation, one for rotation, and two for anisotropic scaling). Since an exhaustive searching in this five-dimensional pose parameter space is time consuming, they proposed an efficient search strategy based on the first- or second-order derivatives of the detection score, which accelerated the detection speed by ten times. Furthermore, the DBN has also been applied to train a boundary detector for segmentation refinement using an active shape model (ASM). The LV detection/segmentation module can also be integrated in a particle filtering framework to track the motion of the LV [44]. This work was later extended to segment the right ventricle (RV) too [46]. In follow-up work [47], the DBN was applied to segment the LV on short-axis cardiac MR images. Similarly, the LV bounding box is detected with a DBN. Furthermore, another DBN was trained to generate a pixel-wise probability map of the LV. Instead of using the ASM as [44], the level set method is applied on the probability map to generate the final segmentation.
Avendi et al. [50] proposed a convolutional network (CNN)-based method to detect an LV bounding box on a short-axis cardiac MR image. Stacked autoencoder was then applied to generate an initial segmentation of the LV, which was used to initialize the level set function. Their level set function combines a length-based energy term, a region-based term, and the prior shape. Instead of running level set on the probability map as [44], it was applied on the initial image.
Different to [44, 50], Chen et al. proposed to use a fully convolutional network (FCN) to segment the LV on 2D long-axis ultrasound images [52]. In [44, 50], deep learning was applied in one or two steps of the whole image analysis pipeline. Differently, the FCN can be trained end-to-end without any preprocessing or post-processing. It can generate a segmentation label for each pixel efficiently since the convolution operation is applied once on the whole image. Due to the limited training samples, a deep network often suffers from the over-fitting issue. There are multiple canonical LV long-axis views, namely apical two-chamber (A2C), three-chamber (A3C), four-chamber (A4C), and five-chamber (A5C) views. Instead of training an LV segmentation network for each task, the problem was formulated as a multi-task learning, where all tasks shared the low-level image representations. At the high level, each task had its own classification layers. The segmentation was refined iteratively by focusing on the LV region detected by the previous iteration. Experiments showed that the iterative cross-domain deep learning approach outperformed alternative single-domain deep learning, especially for tasks with limited training samples.
Zhen et al. [49] presented an interesting method for direct estimation of a ventricular volume from images without performing segmentation at all. They proposed a new convolutional deep belief network. A DBN is composed of stacked restricted Boltzman machine (RBM), where each layer is fully connected to the previous layer. Due to the full connectivity, the network has more parameters than a CNN; therefore it is more prone to over-fit. In [49], the first RBM layer was replaced with a multi-scale convolutional layer. The convolutional DBN was trained without supervision on unlabeled data and the trained network was used as an image feature extractor. A random forest regressor was then trained on the DBN image features to directly output an estimate of the LV area on each MR slice. Summing LV areas from all images results in the final volume estimate.
Due to the difficulty of 3D deep learning , all the above-reviewed methods work on 2D images, even though the input may be 3D. A 3D volume contains much richer information than a 2D image. Therefore, an algorithm leveraging 3D image information may be more robust. For heart segmentation, we only found one example using 3D deep learning , namely marginal space deep learning (MSDL) [62]. MSDL is an extension of marginal space learning (MSL), which uses hand-crafted features (i.e., Haar-like features and steerable features) and a boosting classifier. Here, the hand-crafted features are replaced with automatically learned sparse features and a deep network is exploited as the classifier. In [62], Ghesu et al. demonstrated the efficiency and robustness of MSDL on aortic valve detection and segmentation in 3D ultrasound volumes. Without using GPU, the aortic valve can be successfully segmented in less than one second with higher accuracy than the original MSL. MSDL is a generic approach and it can be easily re-trained to detect/segment other anatomies in a 3D volume.
6 Deep Learning-Based Methods for Vessel Segmentation
Early work on vessel segmentation used various hand-crafted vesselness measurements to distinguish the tubular structure from background [64]. Recently, we saw more and more work to automatically learn the most effective application-specific vesselness measurement from an expert-annotated dataset [65, 66]. Deep learning has potential to replace those classifiers to achieve better segmentation accuracy. However, the current applications of deep learning on vessel segmentation are mainly focused on retinal vessels in fundus images [53,54,55,56,57,58,59,60]. We only found limited work on other vessels, e.g., the coronary artery [62, 63] and carotid artery [61]. We suspect that the main reason is that a fundus image is 2D; therefore, it is much easier to apply an off-the-shelf deep learning package on this application. Other vessels in a 3D volume (e.g., CT or MR) are tortuous and we have to take the 3D context for a reliable segmentation. With the recent development of 3D deep learning, we expect to see more applications of deep learning on other vessels too.
In most work, pixel-wise classification is performed by a trained deep network to directly output the segmentation mask. For example, Wang et al. [53] applied a CNN to retinal vessel segmentation. To further improve the accuracy, they also used the CNN as a trainable feature extractor: activations of the network at different layers are taken as features to train random forests (RF). State-of-the-art performance has been achieved by an ensemble of RF classifiers on the public DRIVE and STARE datasets. Li et al. [54] presented another method based on an FCN with three layers. They formulated the task as cross-modality data transformation from the input image to vessel map. The first hidden layer was pre-trained using denoising autoencoder, while the other two hidden layers were randomly initialized. Different to [53] (which generates a label of the central pixel of an input patch), Li et al. approach outputs labels for all pixels in the patch. Since overlapping patches are extracted during classification, a pixel appears on multiple patches. The final label of the pixel is determined by majority voting to improve the classification accuracy. Fu et al. [60] adapted a holistically nested edge detection (HED) method for retinal vessel segmentation. HED is motivated by the FCN and deeply supervised network, where the outputs of intermediate layers are also directly connected to the final classification layer. After getting the the vessel probability map using HED, a conditional random field is applied to further improve the segmentation accuracy.
Since pixel-wise classification is time consuming, Wu et al. [58] proposed to combine pixel classification and vessel tracking to accelerate the segmentation speed. Starting from a seed point, a vessel is traced in the generalized particle filtering framework (which is a popular vessel tracing approach), while the weight of each particle is set by the CNN classification score at the corresponding position. Since CNN classification is invoked only on a suspected vessel region during tracing, the segmentation speed was accelerated by a fact of two. Besides retinal vessel segmentation, deep learning has also been exploited to detect retinal vessel microaneurysms [56] and diabetic retinopathy [57] from a fundus image.
Coronary artery analysis is the killer application of cardiac CT. Due to the tiny size of a coronary artery, CT is currently the most widely used noninvasive imaging modality for coronary artery disease diagnosis due to its superior image resolution (around 0.2–0.3 mm for a state-of-the-art CT scanner). Even with a quite amount of published work on coronary artery segmentation in the literature [64], we only found one work using deep learning [62] for coronary artery centerline extraction. Coronary centerline extraction is still challenging task. To achieve a high detection sensitivity, false positives are unavoidable. The false positives mainly happen on coronary veins or other tubular structures; therefore, traditional methods cannot reliably distinguish false positives from true coronary arteries. In [41], a CNN is exploited to train a classifier which can distinguish leakages from good centerlines. Since the initial centerline is given, the image information can be serialized as a 1D signal along the centerline. Here, the input channels consist of various profiles sampled along the vessel such as vessel scale, image intensity, centerline curvature, tubularity, intensity, and gradient statistics (mean, standard deviation) along and inside a cross-sectional circular boundary, and distance to the most proximal point in the branch. Deep learning -based branch pruning increases the specificity from 50 to 90% with negligible degradation of sensitivity.
Similar to heart segmentation reviewed in Sect. 2.5, almost all previous work on deep learning for vessel segmentation was focused on 2D. Recently, Zheng et al. [61] proposed an efficient 3D deep learning method for vascular landmark detection. A two-step approach is exploited for efficient detection. A shallow network (with one hidden layer) is used for the initial testing of all voxels to obtain a small number of promising candidates, followed by more accurate classification with a deep network. In addition, they proposed several techniques, i.e., separable filter decomposition and network sparsification, to speed up the evaluation of a network. To mitigate the over-fitting issue, thereby increasing detection robustness, small 3D patches from a multi-resolution image pyramid are extracted as network input. The deeply learned image features are further combined with Haar-like features to increase the detection accuracy. The proposed method has been quantitatively evaluated for carotid artery bifurcation detection on a head–neck CT dataset. Compared to the state-of-the-art, the mean error is reduced by more than half, from 5.97 to 2.64 mm, with a detection speed of less than 1 s/volume without using GPU.
Wolterink et al. [63] presented an interesting method using a 2.5D or 3D CNN for coronary calcium scoring in CT angiography. Normally, a standard cardiac CT protocol includes a non-contrasted CT scan for coronary calcium scoring [67] and a contracted scan (called CT angiography) for coronary artery analysis. If calcium scoring can be performed on a contrasted scan, the dedicated non-contrasted scan can be removed from the protocol to save radiation dose to a patient. However, calcium scoring on CT angiography is more challenging due to the reduced intensity gap between contrasted coronary lumen and calcium. In this work voxel-wise classification is performed to identify calcified coronary plaques. For each voxel, three orthogonal 2D patches (the 2.5D approach) or a full 3D patch are used as input. A CNN is trained to distinguish coronary calcium from other tissues.
7 Introduction to Microscopy Image Analysis
Microscopy image analysis can provide support for improved characterization of various diseases such as breast cancer, lung cancer, brain tumor, etc. Therefore, it plays a critical role in computer-aided diagnosis in clinical practice and pathology research. Due to the large amount of image data, which continue to increase nowadays, it is inefficient or even impossible to manually evaluate the data. Computerized methods can significantly improve the efficiency and the objectiveness, thereby attracting a great deal of attention. In particular, machine learning techniques have been widely and successfully applied to medical imaging and biology research [68, 69]. Compared with non-learning or knowledge based methods that might not precisely translate knowledge into rules, machine learning acquires their own knowledge from data representations. However, conventional machine learning techniques usually do not directly deal with raw data but heavily rely on the data representations, which require considerable domain expertise and sophisticated engineering [70].
Deep learning is one type of representation learning methods that directly process raw data (e.g., RGB images) and automatically learns the representations, which can be applied to detection, segmentation, or classification tasks. Compared with hand-crafted features, learned representations require less human intervention and provide much better performance [71]. Nowadays, deep learning techniques have made great advantages in artificial intelligence, and successfully applied to computer vision, natural language processing, image understanding, medical imaging, computational biology, etc. [70, 72]. By automatically discovering hidden data structures, it has beaten records in several computer vision tasks such as image classification [73] and speech recognition [74], and won multiple competitions in medical image analysis such as brain image segmentation [75] and mitosis detection [76]. Meanwhile, it has provided very promising performance in other medical applications [77, 78].
Recently, deep learning is emerging as a powerful tool and will continue to attract considerable interests in microscopy image analysis including nucleus detection, cell segmentation, extraction of regions of interest (ROIs), image classification, etc. A very popular deep architecture is convolutional neural networks (CNNs) [70, 79], which have obtained great success in various tasks in both computer vision [73, 80,81,82] and medical image analysis [83]. Given images and corresponding annotations (or labels), a CNN model is learned to generate hierarchical data representations, which can be used for robust target classification [84]. On the other hand, unsupervised learning can also be applied to neural networks for representation learning [85,86,87]. Autoencoder is an unsupervised neural network commonly used in microscopy image analysis, which has provided encouraging performance. One of significant benefits of unsupervised feature learning is that it does not require expensive human annotations, which are not easy to achieve in medical computing.
There exist a number of books and reviews explaining deep learning principles, historical survey, and applications in various research areas. Schmidhuber [88] presents a historical overview of deep artificial neural networks by summarizing relevant work and tracing back the origins of deep learning ideas. LeCun et al. [70] mainly review supervised learning in deep neural networks, especially CNNs and recurrent neural networks, and their successful applications in object detection, recognition, and nature language processing. The book [71] explains several established deep learning algorithms and provides speculative ideas for future research, the monograph [87] surveys general deep learning techniques and their applications (mainly) in speech processing and computer vision, and the paper [83] reviews several recent deep learning applications in medical image computing (very few in microscopy imaging). Due to the emergence of deep learning and its impacts in a wide range of disciplines, there exist many other documents introducing deep learning or relevant concepts [74, 89,90,91,92].
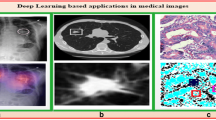
Sample images of breast cancer, muscle, and pancreatic neuroendocrine tumor using different tissues and stain preparations. Hematoxylin and eosin (H&E) staining is used for the first two, while immunohistochemical staining is for the last. These image exhibit significant challenges such as background clutter, touching nuclei, and weak nucleus boundaries, for automated nucleus/cell detection and segmentation
In this chapter, we focus on deep learning in microscopy image analysis, which covers various topics such as nucleus/cell/neuron detection, segmentation, and classification. Compared with other imaging modalities (e.g., magnetic resonance imaging, computed tomography, and ultrasound), microscopy images exhibit unique complex characteristics. In digital histopathology, image data are usually generated with a certain chemistry staining and presents significant challenges including background clutter, inhomogeneous intensity, touching or overlapping nuclei/cells, etc. [72, 93,94,95,96], as shown in Fig. 2.1. We will not review all deep learning techniques in this chapter, but instead introduce and interpret those deep learning-based methods specifically designed for microscopy image analysis. We will explain the principles of those approaches and discuss their advantages and disadvantages, and finally conclude with some potential directions for future research at deep learning in microscopy image analysis.
8 Deep Learning Methods
Deep learning is a kind of machine learning methods involving multi-level representation learning, which starts from raw data input and gradually moves to more abstract levels via nonlinear transformations. With enough training data and sufficiently deep architectures, neural networks can learn very complex functions and discover intricate structures in the data [70]. One significant advantage is that deep learning does not require much engineering work, which is not easy to achieve in some specific domains. Deep learning has been successfully applied to pattern recognition and prediction, and outperforms traditional machine learning methods in many domains including medical image computing [83]. More specifically, deep learning exhibits its great power in microscopy image analysis. To our knowledge, up to now there are mainly four commonly used deep networks in microscopy image analysis: CNNs, fully convolutional networks (FCNs), recurrent neural networks (RNNs), and stacked autoencoders (SAEs). More details related to optimization and algorithms can be found in [71, 89].
9 Microscopy Image Analysis Applications
In microscopy image analysis, deep neural networks are often used as classifiers or feature extractors to resolve various tasks in microscopy image analysis, such as target detection, segmentation, and classification. For the usage of a classifier, a deep neural network assigns a hard or soft label to each pixel of the input image in pixel-wise classification or a single label to the entire input image in image-level classification. CNNs are the most popular networks in this type of applications and their last layers are usually chosen as a multi-way softmax function corresponding to the number of target classes. For the usage of a feature extractor, a network generates a transformed representation of each input image, which can be applied to subsequent data analysis, such as feature selection or target classification. In supervised learning, usually the representation before the last layer of a CNN is extracted, but those from middle layers or even lower layers are also helpful to object recognition [111, 112]. To deal with limited data in medical imaging, it might be necessary to apply pretrain and fine-tune to the neural network. Tables 2.1 and 2.2 summarize the current deep learning achievements in microscopy image analysis.
10 Discussions and Conclusion on Deep Learning for Microscopy Image Analysis
Deep learning is a rapidly growing field and is emerging as a leading machine learning tool in computer vision and image analysis. It has exhibited great power in medical image computing with producing improved accuracy of detection, segmentation, or recognition tasks [83]. Most of works presented in this paper use CNNs or one type of the variants, FCNs, to solve problems in microscopy image analysis. Our conjecture is that CNNs provide consistent improved performance across a large variety of computer vision tasks and thus it might be straightforward to apply convolutional networks to microscopy image computing. More recently, FCNs have attracted a great deal of interest due to the end-to-end training design and efficient fully convolutional inference for image semantic segmentation. FCNs begin to enter in microscopy imaging and are expected to become more popular in the future.
Model training in deep learning is usually computationally expensive and often needs programming with graphics processing units (GPUs) to reduce running time. There are several publicly available frameworks supporting deep learning. Caffe [127] is mainly written with C++ programming languages and supports command line, Python, and MATLAB interfaces. It uses Google protocol buffers to serialize data and has powered many aspects of the communities of computer vision and medical imaging. Theano [128] is a Python library that allows efficient definition, optimization, and evaluation of mathematical expressions. It is very flexible and has supported many scientific investigations. TensorFlow [129] uses data flow graphs for numerical computation and allows automatic differentiation, while Torch [130] is developed with Lua language and it is flexible as well. Another commonly used deep learning library in medical imaging is MatConvnet [131], which is a Matlab toolbox for CNNs and FCNs. It is simple and easy to use. There exist some other libraries supporting deep learning , and more information can be found in [132, 133].
Although unsupervised deep learning is applied to microscopy image analysis, the majority of the works are using supervised learning. However, deep learning with supervision usually require a large set of annotated training data, which might be prohibitively expensive in the medical domain [83]. One way to address this problem is to view a pre-trained model that is learned with other datasets, either natural or medical images, as a fixed feature extractor, and use generated features to train a target classifier for pixel-wise or image-level prediction. If the target data size is sufficiently large, it might be beneficial to initialize the network with a pre-trained model and then fine-tune it toward the target task. The initialization can be conducted in the first several or all layers depending on the data size and properties. On the other hand, semi-supervised or unsupervised learning might be a potential alternative if annotated training data are not sufficient or unavailable.
Another potential challenge of applying deep learning to microscopy image computing is to improve the network scalability, thereby adapting to high resolution images. In pathology imaging informatics, usually it is necessary to conduct quantitative analysis on whole-slide images (WSI) [134] instead of manually selected regions, since it can reduce biases of observers and provide complete information that is helpful to decision-making in diagnosis. The resolution of a WSI image is often over \(50000\times 50000\), and has tens of thousands or millions of object of interest (e.g., nuclei or cells). Currently, pixel-wise prediction with CNNs is mainly conducted in a sliding-window manner, and clearly this will be extremely computationally expensive when dealing with WSI images. FCNs are designed for efficient inference and might be a good choice for computation improvement.
This paper provides a survey of deep learning in microscopy image analysis, which is a fast evolving field. Specifically, it briefly introduces the popular deep neural networks in the domain, summarizes current research efforts, and explains the challenges as well as the potential future trends. Deep learning has benefitted the microscopy imaging domain and we expect that it will play a more important role in the future. New learning algorithms in artificial intelligence can accelerate the process of transferring deep learning techniques from natural toward medical images and enhance its achievements.
References
Jemal A, Siegel R, Ward E, Hao Y, Xu J, Murray T, Thun MJ (2008) Cancer statistics, 2008. CA Cancer J Clin 58(2):71–96
Lauby-Secretan B, Scoccianti C, Loomis D, Benbrahim-Tallaa L, Bouvard V, Bianchini F, Straif K (2015) Breast-cancer screening–viewpoint of the IARC working group. New Engl J Med 372(24):2353–2358
Giger ML, Pritzker A (2014) Medical imaging and computers in the diagnosis of breast cancer. In: SPIE optical engineering + applications. International Society for Optics and Photonics, p 918908
Oliver A, Freixenet J, Marti J, Perez E, Pont J, Denton ER, Zwiggelaar R (2010) A review of automatic mass detection and segmentation in mammographic images. Med Image Anal 14(2):87–110
Tang J, Rangayyan RM, Xu J, El Naqa I, Yang Y (2009) Computer-aided detection and diagnosis of breast cancer with mammography: recent advances. IEEE Trans Inf Technol Biomed 13(2):236–251
Kozegar E, Soryani M, Minaei B, Domingues I et al (2013) Assessment of a novel mass detection algorithm in mammograms. J Cancer Res Ther 9(4):592
Beller M, Stotzka R, Müller TO, Gemmeke H (2005) An example-based system to support the segmentation of stellate lesions. In: Bildverarbeitung für die Medizin 2005. Springer, pp 475–479
te Brake GM, Karssemeijer N, Hendriks JH (2000) An automatic method to discriminate malignant masses from normal tissue in digital mammograms. Phys Med Biol 45(10):2843
Campanini R, Dongiovanni D, Iampieri E, Lanconelli N, Masotti M, Palermo G, Riccardi A, Roffilli M (2004) A novel featureless approach to mass detection in digital mammograms based on support vector machines. Phys Med Biol 49(6):961
Eltonsy NH, Tourassi GD, Elmaghraby AS (2007) A concentric morphology model for the detection of masses in mammography. IEEE Trans Med Imaging 26(6):880–889
Sampat MP, Bovik AC, Whitman GJ, Markey MK (2008) A model-based framework for the detection of spiculated masses on mammographya. Med Phys 35(5):2110–2123
Bellotti R, De Carlo F, Tangaro S, Gargano G, Maggipinto G, Castellano M, Massafra R, Cascio D, Fauci F, Magro R et al (2006) A completely automated cad system for mass detection in a large mammographic database. Med Phys 33(8):3066–3075
Wei J, Sahiner B, Hadjiiski LM, Chan H-P, Petrick N, Helvie MA, Roubidoux MA, Ge J, Zhou C (2005) Computer-aided detection of breast masses on full field digital mammograms. Med Phys 32(9):2827–2838
Ball JE, Bruce LM (2007) Digital mammographic computer aided diagnosis (cad) using adaptive level set segmentation. In: 29th annual international conference of the IEEE engineering in medicine and biology society, 2007. EMBS 2007. IEEE, pp 4973–4978
Rahmati P, Adler A, Hamarneh G (2012) Mammography segmentation with maximum likelihood active contours. Med Image Anal 16(6):1167–1186
Cardoso JS, Domingues I, Oliveira HP (2014) Closed shortest path in the original coordinates with an application to breast cancer. Int J Pattern Recognit Artif Intell 29:1555002
Varela C, Timp S, Karssemeijer N (2006) Use of border information in the classification of mammographic masses. Phys Med Biol 51(2):425
Shi J, Sahiner B, Chan H-P, Ge J, Hadjiiski L, Helvie MA, Nees A, Wu Y-T, Wei J, Zhou C et al (2008) Characterization of mammographic masses based on level set segmentation with new image features and patient information. Med Phys 35(1):280–290
Domingues I, Sales E, Cardoso J, Pereira W (2012) Inbreast-database masses characterization. In: XXIII CBEB
LeCun Y, Bengio Y (1995) Convolutional networks for images, speech, and time series. In: The handbook of brain theory and neural networks, vol 3361
Krizhevsky A, Sutskever I, Hinton GE (2012) Imagenet classification with deep convolutional neural networks. In: NIPS, vol 1, p 4
Farabet C, Couprie C, Najman L, LeCun Y (2013) Learning hierarchical features for scene labeling. IEEE Trans Pattern Anal Machi Intell 35(8):1915–1929
Girshick R, Donahue J, Darrell T, Malik J (2014) Rich feature hierarchies for accurate object detection and semantic segmentation. In: 2014 IEEE conference on computer vision and pattern recognition (CVPR). IEEE, pp 580–587
Zhang Y, Sohn K, Villegas R, Pan G, Lee H (2015) Improving object detection with deep convolutional networks via bayesian optimization and structured prediction. In: IEEE conference on computer vision and pattern recognition (CVPR), pp 249–258
Dhungel N, Carneiro G, Bradley AP (2015) Deep learning and structured prediction for the segmentation of mass in mammograms. In: Medical image computing and computer-assisted intervention–MICCAI 2015. Springer, pp 605–612
Dhungel N, Carneiro G, Bradley AP (2015) Tree re-weighted belief propagation using deep learning potentials for mass segmentation from mammograms. In: 2015 IEEE 12th international symposium on biomedical imaging (ISBI), pp 760–763
Dhungel N, Carneiro G, Bradley AP (2015) Deep structured learning for mass segmentation from mammograms. In: 2015 IEEE international conference on image processing (ICIP), pp 2950–2954
Heath M, Bowyer K, Kopans D, Moore R, Kegelmeyer P (2000) The digital database for screening mammography. In: Proceedings of the 5th international workshop on digital mammography, pp 212–218
Dubrovina A, Kisilev P, Ginsburg B, Hashoul S, Kimmel R (2016) Computational mammography using deep neural networks. In: Workshop on deep learning in medical image analysis (DLMIA)
Dhungel N, Carneiro G, Bradley A (2015) Automated mass detection in mammograms using cascaded deep learning and random forests. In: 2015 international conference on digital image computing: techniques and applications (DICTA), pp 1–8
Ertosun MG, Rubin DL (2015) Probabilistic visual search for masses within mammography images using deep learning. In: 2015 IEEE international conference on bioinformatics and biomedicine (BIBM). IEEE, pp 1310–1315
Arevalo J, González FA, Ramos-Pollán R, Oliveira JL, Lopez MAG (2016) Representation learning for mammography mass lesion classification with convolutional neural networks. Comput Methods Programs Biomed
Qiu Y, Yan S, Tan M, Cheng S, Liu H, Zheng B (2016) Computer-aided classification of mammographic masses using the deep learning technology: a preliminary study. In: SPIE medical imaging. International Society for Optics and Photonics, p 978520
Jiao Z, Gao X, Wang Y, Li J (2016) A deep feature based framework for breast masses classification. Neurocomputing 197:221–231
Carneiro G, Nascimento J, Bradley AP (2015) Unregistered multiview mammogram analysis with pre-trained deep learning models. In: Medical image computing and computer-assisted intervention – MICCAI 2015. Springer, Berlin, pp. 652–660
Kallenberg M, Petersen K, Nielsen M, Ng A, Diao P, Igel C, Vachon C, Holland K, Karssemeijer N, Lillholm M (2016) Unsupervised deep learning applied to breast density segmentation and mammographic risk scoring
Petersen K, Nielsen M, Diao P, Karssemeijer N, Lillholm M (2014) Breast tissue segmentation and mammographic risk scoring using deep learning. In: Breast imaging. Springer, Berlin, pp 88–94
Qiu Y, Wang Y, Yan S, Tan M, Cheng S, Liu H, Zheng B (2016) An initial investigation on developing a new method to predict short-term breast cancer risk based on deep learning technology. In: SPIE medical imaging. International Society for Optics and Photonics, p 978521
Lloyd-Jones D, Adams R, Carnethon M et al (2009) Heart disease and stroke statistics – 2009 update. Circulation 119(3):21–181
Heidenreich PA, Trogdon JG, Khavjou OA et al (2011) Forecasting the future of cardiovascular disease in the United States: a policy statement from the American Heart Association. Circulation 123:933–944
Gulsun MA, Funka-Lea G, Sharma P, Rapaka S, Zheng Y (2016) Coronary centerline extraction via optimal flow paths and CNN path pruning. In: Proceedings of international conference on medical image computing and computer assisted intervention
Zheng Y, Barbu A, Georgescu B, Scheuering M, Comaniciu D (2008) Four-chamber heart modeling and automatic segmentation for 3D cardiac CT volumes using marginal space learning and steerable features. IEEE Trans Med Imaging 27(11):1668–1681
Zheng Y (2015) Model based 3D cardiac image segmentation with marginal space learning. In: Medical image recognition, segmentation and parsing: methods, theories and applications. Elsevier, Amsterdam, pp 383–404
Carneiro G, Nascimento JC, Freitas A (2012) The segmentation of the left ventricle of the heart from ultrasound data using deep learning architectures and derivative-based search methods. IEEE Trans Image Process 21(3):968–982
Carneiro G, Nascimento JC (2013) Combining multiple dynamic models and deep learning architectures for tracking the left ventricle endocardium in ultrasound data. IEEE Trans Pattern Anal Mach Intell 35(11):2592–2607
Ngo TA, Lu Z, Carneiro G (2016) Combining deep learning and level set for the automated segmentation of the left ventricle of the heart from cardiac cine magnetic resonance. Med Image Anal 35:159–171
Ngo TA, Carneiro G (2014) Fully automated non-rigid segmentation with distance regularized level set evolution initialization and constrained by deep-structured inference. In: Proceedings of IEEE conference computer vision and pattern recognition, pp 1–8
Emad O, Yassine IA, Fahmy AS (2015) Automatic localization of the left ventricle in cardiac MRI images using deep learning. In: Proceedings of annual international conference of the IEEE engineering in medicine and biology society, pp 683–686
Zhen X, Wang Z, Islam A, Bhaduri M, Chan I, Li S (2016) Multi-scale deep networks and regression forests for direct bi-ventricular volume estimation. Med Image Anal 30:120–129
Avendi MR, Kheirkhah A, Jafarkhani H (2016) A combined deep-learning and deformable-model approach to fully automatic segmentation of the left ventricle in cardiac MRI. Med Image Anal 30:108–119
Avendi MR, Kheradvar A, Jafarkhani H (2016) Fully automatic segmentation of heart chambers in cardiac MRI using deep learning. J Cardiovasc Magn Reson 18:351–353
Chen H, Zheng Y, Park J-H, Heng PA, Zhou SK (2016) Iterative multi-domain regularized deep learning for anatomical structure detection and segmentation from ultrasound images. In: Proceedings of international conference medical image computing and computer assisted intervention
Wang S, Yin Y, Cao G, Wei B, Zheng Y, Yang G (2015) Hierarchical retinal blood vessel segmentation based on feature and ensemble learning. Neruocomputing 149:708–717
Li Q, Feng B, Xie L, Liang P, Zhang H, Wang T (2016) A cross-modality learning approach for vessel segmentation in retinal images. IEEE Trans Med Imaging 35(1):109–118
Maji D, Santara A, Mitra P, Sheet D (2016) Ensemble of deep convolutional neural networks for learning to detect retinal vessels in fundus images. arXiv:1603.04833
Haloi M (2015) Improved microaneurysm detection using deep neural networks. arXiv:1505.04424
Chandrakumar T, Kathirvel R (2016) Classifying diabetic retinopathy using deep learning architecture. Int J Eng Res Technol 5(6):19–24
Wu A, Xu Z, Gao M, Buty M, Mollura DJ (2016) Deep vessel tracking: a generalized probabilistic approach via deep learning. In: Proceedings of IEEE international symposium on biomedical, imaging, pp 1363–1367
Melinscak M, Prentasic P, Loncaric S (2015) Retinal vessel segmentation using deep neural networks. In: Proceedings of international conference computer vision theory and application, pp 577–582
Fu H, Xu Y, Wong DWK, Liu J (2016) Retinal vessel segmentation via deep learning network and fully-connected conditional random fields. In: Proceedings of IEEE international symposium on biomedical, imaging, pp 698–701
Zheng Y, Liu D, Georgescu B, Nguyen H, Comaniciu D (2015) 3D deep learning for efficient and robust landmark detection in volumetric data. In: Proceedings of international conference on medical image computing and computer assisted intervention, pp 565–572
Ghesu FC, Krubasik E, Georgescu B, Singh V, Zheng Y, Hornegger J, Comaniciu D (2016) Marginal space deep learning: efficient architecture for volumetric image parsing. IEEE Trans Med Imaging 35(5):1217–1228
Wolterink JM, Leiner T, de Vos BD, van Hamersvelt RW, Viergever MA, Isgum I (2016) Automatic coronary artery calcium scoring in cardiac CT angiography using paired convolutional neural networks. Med Image Anal 34:123–136
Lesage D, Angelini ED, Bloch I, Funka-Lea G (2009) A review of 3D vessel lumen segmentation techniques: models, features and extraction schemes. Med Image Anal 13(6):819–845
Zheng Y, Loziczonek M, Georgescu B, Zhou SK, Vega-Higuera F, Comaniciu D (2011) Machine learning based vesselness measurement for coronary artery segmentation in cardiac CT volumes. In: Proceedings of SPIE medical imaging, vol 7962, pp 1–12
Zheng Y, Tek H, Funka-Lea G (2013) Robust and accurate coronary artery centerline extraction in CTA by combining model-driven and data-driven approaches. In: Proceedings of international conference medical image computing and computer assisted intervention, pp 74–81
Wolterink JM, Leiner T, Coatrieux J-L, Kelm BM, Kondo S, Salgado RA, Shahzad R, Shu H, Snoeren M, Takx RA, van Vliet L, de Vos BD, van Walsum T, Willems TP, Yang G, Zheng Y, Viergever MA, Ium I (2016) An evaluation of automatic coronary artery calcium scoring with cardiac CT: the orCaScore challenge. Med Phys 43(5):2361–2373
Sommer C, Gerlich DW (2013) Machine learning in cell biology teaching computers to recognize phenotypes. J Cell Sci 126(24):5529–5539
Wernick MN, Yang Y, Brankov JG, Yourganov G, Strother SC (2010) Machine learning in medical imaging. IEEE Signal Process Mag 27(4):25–38
LeCun Y, Bengio Y, Hinton G (2015) Deep learning. Nature 521:436–444
Goodfellow I, Bengio Y, Courville A (2016) Deep learning. Book in preparation for MIT Press
Xing F, Yang L (2016) Robust nucleus/cell detection and segmentation in digital pathology and microscopy images: a comprehensive review. IEEE Rev Biomed Eng 99
Krizhevsky A, Sutskever I, Hinton GE (2012) Imagenet classification with deep convolutional neural networks. In: Advances neural information processing systems, pp 1097–1105
Hinton G, Deng L, Yu D, Dahl GE, Mohamed Ar, Jaitly N, Senior A, Vanhoucke V, Nguyen P, Sainath TN, Kingsbury B (2012) Deep neural networks for acoustic modeling in speech recognition: The shared views of four research groups. IEEE Signal Process Mag 29(6):82–97
Arganda-Carreras I et al (2015) Crowdsourcing the creation of image segmentation algorithms for connectomics. Front Neuroanat 9(142)
Veta M et al (2015) Assessment of algorithms for mitosis detection in breast cancer histopathology images. Med Image Anal 20(1):237–248
Ma J, Sheridan RP, Liaw A, Dahl GE, Svetnik V (2015) Deep neural nets as a method for quantitative structure-activity relationships. J Chem Inf Model 55:263274
Xiong HY et al (2015) The human splicing code reveals new insights into the genetic determinants of disease. Science 347(6218)
LeCun Y, Bottou L, Bengio Y, Haffner P (1998) Gradient-based learning applied to document recognition. Proc IEEE 86:2278–2324
Girshick R, Donahue J, Darrell T, Malik J (2014) Rich feature hierarchies for accurate object detection and semantic segmentation. In: 2014 IEEE conference on computer vision and pattern recognition, pp 580–587
Girshick R (2015) Fast r-cnn. In: 2015 IEEE international conference on computer vision, pp 1440–1448
Long J, Shelhamer E, Darrell T (2015) Fully convolutional networks for semantic segmentation. In: 2015 IEEE conference on computer vision and pattern recognition, pp 3431–3440
Greenspan H, van Ginneken B, Summers RM (2016) Guest editorial deep learning in medical imaging: overview and future promise of an exciting new technique. IEEE Trans Med Imaging 35(5):1153–1159
LeCun Y, Kavukcuoglu K, Farabet C (2010) Convolutional networks and applications in vision. In: IEEE international symposium on ciruits and systems (ISCAS), pp 253–256
Lee H, Grosse R, Ranganath R, Ng AY (2009) Convolutional deep belief networks for scalable unsupervised learning of hierarchical representations. In: Proceedings of the 26th international conference on machine learning, pp 609–616
Lee H, Grosse R, Ranganath R, Ng AY (2011) Unsupervised learning of hierarchical representations with convolutional deep belief networks. Commun ACM 54(10):95–103
Deng L, Yu D (2014) Deep learning: methods and applications. Found Trends Signal Process 3(3–4):197–387
Schmidhuber J (2015) Deep learning in neural networks: an overview. Neural Networks 61:85–117. Published online 2014; based on TR arXiv:1404.7828 [cs.NE]
Nielsen MA (2015) Neural networks and deep learning. Determination Press
Arel I, Rose DC, Karnowski TP (2010) Deep machine learning - a new frontier in artificial intelligence research [research frontier]. IEEE Comput Intell Mag 5(4):13–18
Bengio Y (2009) Learning deep architectures for ai. Found Trends Mach Learn 2:1–127
Bengio Y, Courville A, Vincent P (2013) Representation learning: a review and new perspectives. IEEE Trans Pattern Anal Mach Intell 35(8):1798–1828
Gurcan MN, Boucheron LE, Can A, Madabushi A, Rajpoot NM, Yener B (2009) Histopatological image analysis: a review. IEEE Rev Biomed Eng 2:147–171
McCann MT, Ozolek JA, Castro CA, Parvin B, Kovacevic J (2015) Automated histology analysis: opportunities for signal processing. IEEE Signal Process Mag 32:78–87
Veta M, Pluim J, van Diest P, Viergever M (2014) Breast cancer histopathology image analysis: a review. IEEE Trans Biomed Eng 61:1400–1411
Irshad H, Veillard A, Roux L, Racoceanu D (2014) Methods for nuclei detection, segmentation, and classification in digital histopathology: a review – current status and fture potential. IEEE Rev Biomed Eng 7:97–114
Ciresan DC, Giusti A, Gambardella LM, Schmidhuber J (2013) Mitosis detection in breast cancer histology images with deep neural networks. In: International conference medical image computing and computer-assisted intervention (MICCAI), vol 8150, pp 411–418
Xing F, Xie Y, Yang L (2015) An automatic learning-based framework for robust nucleus segmentation. IEEE Trans Med Imaging PP(99):1
Mao Y, Yin Z, Schober JM (2015) Iteratively training classifiers for circulating tumor cell detection. In: IEEE international symposium on biomedical imaging, pp 190–194
Wang J, MacKenzie JD, Ramachandran R, Chen DZ (2015) Neutrophils identification by deep learning and voronoi diagram of clusters. In: medical image computing and computer-assisted intervention – MICCAI 2015: 18th international conference, Munich, Germany, 5–9 October 2015, Proceedings, Part III, pp 226–233
Dong B, Shao L, Costa MD, Bandmann O, Frangi AF (2015) Deep learning for automatic cell detection in wide-field microscopy zebrafish images. In: IEEE international symposium on biomedical imaging, pp 772–776
Shkolyar A, Gefen A, Benayahu D, Greenspan H (2015) Automatic detection of cell divisions (mitosis) in live-imaging microscopy images using convolutional neural networks. In: 2015 37th annual international conference of the IEEE engineering in medicine and biology society (EMBC), pp 743–746
Liu F, Yang L (2015) A novel cell detection method using deep convolutional neural network and maximum-weight independent set. In: International conference on medical image computing and computer-assisted intervention (MICCAI), vol 9351, pp 349–357
Xie Y, Xing F, Kong X, Yang L (2015) Beyond classification: structured regression for robust cell detection using convolutional neural network. In: International conference medical image computing and computer-assisted intervention (MICCAI), vol 9351, pp 358–365
Sirinukunwattana K, Raza SEA, Tsang YW, Snead DRJ, Cree IA, Rajpoot NM (2016) Locality sensitive deep learning for detection and classification of nuclei in routine colon cancer histology images. IEEE Trans Med Imaging 35(5):1196–1206
Xie W, Noble JA, Zisserman A (2015) Microscopy cell counting with fully convolutional regression networks. In: MICCAI 1st workshop on deep learning in medical image analysis
Xie Y, Kong X, Xing F, Liu F, Su H, Yang L (2015) Deep voting: a robust approach toward nucleus localization in microscopy images. In: International conference on medical image computing and computer-assisted intervention (MICCAI), vol 9351, pp 374–382
Albarqouni S, Baur C, Achilles F, Belagiannis V, Demirci S, Navab N (2016) Aggnet: deep learning from crowds for mitosis detection in breast cancer histology images. IEEE Trans Med Imaging 35(5):1313–1321
van Grinsven MJJP, van Ginneken B, Hoyng CB, Theelen T, Snchez CI (2016) Fast convolutional neural network training using selective data sampling: application to hemorrhage detection in color fundus images. IEEE Trans Med Imaging 35(5):1273–1284
Xu J, Xiang L, Liu Q, Gilmore H, Wu J, Tang J, Madabhushi A (2015) Stacked sparse autoencoder (ssae) for nuclei detection on breast cancer histopathology images
Razavian AS, Azizpour H, Sullivan J, Carlsson S (2014) CNN features off-the-shelf: an astounding baseline for recognition. In: Proceedings of the 2014 IEEE conference on computer vision and pattern recognition workshops, CVPRW’14, pp 512–519
Tajbakhsh N, Shin JY, Gurudu SR, Hurst RT, Kendall CB, Gotway MB, Liang J (2016) Convolutional neural networks for medical image analysis: full training or fine tuning? IEEE Trans Med Imaging 35(5):1299–1312
Ciresan D, Giusti A, Gambardella LM, Schmidhuber J (2012) Deep neural networks segment neuronal membranes in electron microscopy images. In: Advances in neural information processing systems, pp 2843–2851
Fakhry A, Peng H, Ji S (2016) Deep models for brain EM image segmentation novel insights and improved performance. Bioinformatics 32:2352–2358
Ning F, Delhomme D, LeCun Y, Piano F, Bottou L, Barbano PE (2005) Toward automatic phenotyping of developing embryos from videos. IEEE Trans Image Process 14(9):1360–1371
Song Y, Zhang L, Chen S, Ni D, Lei B, Wang T (2015) Accurate segmentation of cervical cytoplasm and nuclei based on multi-scale convolutional network and graph partitioning. IEEE Trans Biomed Eng 62:2421–2433
Ronneberger O, Fischer P, Brox T (2015) U-Net: convolutional networks for biomedical image segmentation. In: Medical image computing and computer-assisted intervention – MICCAI 2015: 18th international conference, Munich, Germany, 5–9 October 2015, Proceedings, Part III, pp 234–241
Chen H, Qi X, Cheng J, Heng PA (2016) Deep contextual networks for neuronal structure segmentation. In: AAAI, pp1167–1173
Stollenga MF, Byeon W, Liwicki M, Schmidhuber J (2015) Parallel multi-dimensional lstm, with application to fast biomedical volumetric image segmentation. In: Advances in neural information processing systems, vol 28, pp 2980–2988
Su H, Xing F, Kong X, Xie Y, Zhang S, Yang L (2015) Robust cell detection and segmentation in histopathological images using sparse reconstruction and stacked denoising autoencoders. In: International conference on medical image computing and computer assisted intervention (MICCAI), vol 9351, pp 383–390
Gao Z, Wang L, Zhou L, Zhang J (2016) Hep-2 cell image classification with deep convolutional neural networks. IEEE J Biomed Health Inf PP(99):1
Chen CL, Mahjoubfar A, Tai L, Blaby IK, Huang A, Niazi KR, Jalali B (2016) Deep learning in label-free cell classification. Sci Rep 6(21471)
Xu Y, Jia Z, Ai Y, Zhang F, Lai M, Chang EIC (2015) Deep convolutional activation features for large scale brain tumor histopathology image classification and segmentation. In: 2015 IEEE international conference on acoustics, speech and signal processing (ICASSP), pp 947–951
Xu Y, Mo T, Feng Q, Zhong P, Lai M, Chang EIC (2014) Deep learning of feature representation with multiple instance learning for medical image analysis. In: 2014 IEEE international conference on acoustics, speech and signal processing (ICASSP), pp 1626–1630
Cruz-Roa AA, Ovalle JEA, Madabhushi A, Osorio FAG (2013) A deep learning architecture for image representation, visual interpretability and automated basal-cell carcinoma cancer detection. In: Medical image computing and computer-assisted intervention-MICCAI 2013, pp 403–410
Chang H, Zhou Y, Spellman P, Parvin B (2013) Stacked predictive sparse coding for classification of distinct regions in tumor histopathology. In: Proceedings of the IEEE international conference on computer vision, pp 169–176
Jia Y, Shelhamer E, Donahue J, Karayev S, Long J, Girshick R, Guadarrama S, Darrell T (2014) Caffe: convolutional architecture for fast feature embedding. arXiv:1408.5093
Theano Development Team (2016), Theano: a Python framework for fast computation of mathematical expressions. arXiv:abs/1605.02688
Abadi M et al (2015) TensorFlow: large-scale machine learning on heterogeneous systems. Software available from tensorflow.org
Collobert R, Kavukcuoglu K, Farabet C (2011) Torch7: a matlab-like environment for machine learning. In: BigLearn, NIPS workshop
Vedaldi A, Lenc K (2015) Matconvnet – convolutional neural networks for matlab
Mamoshina P, Vieira A, Putin E, Zhavoronkov A (2016) Applications of deep learning in biomedicine. Mol Pharmaceutics 13(5):1445–1454
Wang W, Zhang M, Chen G, Jagadish HV, Ooi BC, Tan KL (2016) Database meets deep learning: challenges and opportunities
Kothari S, Phan JH, Stokes TH, Wang MD (2013) Pathology imaging informatics for quantitative analysis of whole-slide images. J Am Med Inform Assoc 20(6):1099–1108
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Carneiro, G., Zheng, Y., Xing, F., Yang, L. (2017). Review of Deep Learning Methods in Mammography, Cardiovascular, and Microscopy Image Analysis. In: Lu, L., Zheng, Y., Carneiro, G., Yang, L. (eds) Deep Learning and Convolutional Neural Networks for Medical Image Computing. Advances in Computer Vision and Pattern Recognition. Springer, Cham. https://doi.org/10.1007/978-3-319-42999-1_2
Download citation
DOI: https://doi.org/10.1007/978-3-319-42999-1_2
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-42998-4
Online ISBN: 978-3-319-42999-1
eBook Packages: Computer ScienceComputer Science (R0)