Abstract
For recovery-oriented care to be implemented, clinicians who are typically indoctrinated into traditional models of mental health care will need to be effectively taught the key principles, processes, and practices of recovery-oriented care. This chapter addresses this challenge by first examining reports of efforts to teach recovery-oriented care and then presenting a conceptual model based on the theoretical and empirical literature pertaining to effective methods of teaching and implementing changes in patient care practices. In consideration of this recovery teaching-learning model, the following components are examined: (1) the content that needs to be taught; (2) the characteristics of the targeted learners that would influence the teaching-learning process; (3) the characteristics of the training providers that would best facilitate desired outcomes; and (4) general teaching strategies designed to promote adoption of recovery-oriented care. This chapter concludes with a review of some of the significant challenges to the teaching and implementation of a recovery orientation to mental health care. These challenges include an insufficient workforce to provide the mental health care that is needed for our society today, a drift toward primarily psychopharmacological management with little time available to address recovery-oriented matters, and a mental health system that has become focused on crisis stabilization rather than the longer term goals that are the focus of recovery. It is proposed that overcoming these challenges to the teaching and implementation of recovery-oriented care will require administrative leadership and support as well as ample exposure to recovery stories that can inspire genuine change in clinicians’ attitudes and practice behaviors.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Recovery-oriented care
- Personal recovery
- Teaching-learning model
- Adult learners
- Instructors
- Teaching strategies
Introduction
Since the 1990s, the advocacy of recovery-oriented practices in mental health care has been gaining considerable traction worldwide. In contrast to the traditional model of mental health care that focuses on reduction of symptoms and restoration of individuals to premorbid levels of functioning, this emerging model of care places the emphasis on recovery as a restoration of individuals to meaningful lives regardless of the ongoing presence of mental illness (Davidson et al. 2009; Davidson and Roe 2007). This new recovery model, often referred to as personal recovery, acknowledges and attends to the suffering related to mental illness, but contextualizes clinical symptoms within the larger picture of what it means to be human. That is, it emphasizes the wholeness, strengths, cultural identity, and striving for meaning that individuals with mental illness share in common with their peers in the population as a whole. Within the past 10 years, virtually every mental health professional and advocacy organization in the United States has endorsed the recovery model of mental health care.
The adoption of this new model of mental health care has been a primary mission of the Substance Abuse and Mental Health Services Administration (SAMHSA). In 2009, the Center for Mental Health Services (CMHS), Office of the Associate Director for Consumer Affairs within SAMHSA, contracted with Developmental Services Group, Inc. (DSG) to launch a 5-year Recovery to Practice (RTP) initiative to translate the vision of recovery into the practice of mental health professionals of all disciplines (Davidson and Dain 2010). In 2004, the Department of Veterans Affairs initiated a 5-year action plan for the transformation of the Veterans Administration mental health services into recovery-oriented services (Greenberg and Rosenheck 2009). The enthusiasm that has been driving the ascendance of the recovery movement appears to focus its emphasis on: (1) broader treatment goals and measures of success that extend beyond symptom reduction (e.g., hope, empowerment, and life satisfaction); (2) a truly collaborative relationship between the clinician and the consumer of services; and (3) the inclusion of individuals with mental illness, their family members, and advocacy groups as members of the treatment team (Peebles et al. 2007).
Supported by national policies, professional organization endorsements, and mental health advocacy groups the push to explicitly train the mental health workforce in recovery-oriented approaches has certainly been gaining momentum. As a consequence, several training initiatives have been developed to bring about mental health care system transformation. Most of these initiatives, however, have focused on broad organizational and procedural changes as well as hospital and clinic staff development. Unfortunately, in the promotion of recovery-oriented care relatively little attention has been focused on the training of clinicians. Consequently, it is not surprising that surveys of the key providers of mental health services including psychiatrists, psychologists, and social workers suggest that they have little familiarity with the recovery literature and hold mixed beliefs regarding the feasibility and utility of recovery-oriented practice (e.g., Hardiman and Hodges 2008). It is proposed that if recovery-oriented care is to be effectively implemented, as proposed by recent national policies and endorsements, the clinicians engaged in such work need to be taught the key principles, processes, and practices of recovery-oriented care.
This chapter addresses the formidable challenge by first examining recent reports of efforts to teach recovery-oriented care and then presenting a conceptual model based on the theoretical and empirical literature pertaining to effective methods of teaching and implementing changes in patient care practices. It should be noted that the conceptual model for teaching recovery-oriented care was borne out of the efforts of Project Georgia Recovery-based Educational Approach to Treatment (GREAT) that represents a 7-year programmatic initiative to transform the Department of Psychiatry and Health Behavior at the Augusta University (formerly the Medical College of Georgia) into a department that fully embraces the recovery orientation to mental health care. Similar to the initiatives of the Recovery Education in the Academy Program (REAP) at the University of Illinois, Chicago (Razzano et al. 2010), Project GREAT aspired to influence the education and practice of a diverse array of trainees and practitioners including clinical staff and faculty, medical students, nursing students, psychiatry residents, psychology predoctoral interns, and postdoctoral fellows. The primary focus of Project GREAT as well as the focus of this chapter, however, has been to develop strategies to shape the recovery knowledge, attitudes, and practices of clinicians in the fields of psychiatry and psychology.
While there is no overarching blueprint for recovery-oriented care, there appears to be an emerging consensus regarding the fundamental nature of personal recovery and the processes that clinicians can facilitate to support recovery in both outpatient and inpatient settings. Thus, it is believed that the processes and methods that are proposed to teach recovery-oriented care to clinicians have a broad applicability to the various clinical contexts in which psychiatric care is provided.
Outcome Studies of Recovery Training for Clinicians
Published reports regarding the impact of recovery training for clinicians have been extremely limited and have primarily entailed survey studies and prepost quasi-experimental design studies. Survey studies regarding the impact of any recovery training experiences on mental health staff have generally reported positive outcomes of recovery training that have included: (1) improved optimism regarding patient outcomes (Tsai et al. 2010, 2011); (2) higher overall personal optimism (Tsai et al. 2011); (3) greater sense of agency recovery attitudes (Tsai et al. 2010, 2011); and (4) higher levels of recovery-oriented competencies when more in-depth training was provided (Stuber et al. 2014a). Though details regarding the types of trainings examined in these survey studies were lacking, Tsai et al. (2010) reported in their survey of staff in two-state psychiatric hospitals that those who received specific, practical training as opposed to more general, inspirational training had a greater increase in agency recovery attitudes.
A limited number of examinations of recovery-oriented workshops have been reported that have ranged from 2–4 days of recovery-oriented care training. The content of these recovery workshops has been remarkably similar in their inclusion of teaching the participants recovery principles, promoting attitudes that support recovery-oriented care (e.g., eliminating stigmatizing views of individuals with mental illness, viewing patients as equal partners in their care), and introducing recovery-oriented practices such as self-directed goal-setting, identifying patients’ strengths, and methods for instilling hope. The format and techniques utilized were also found to cut across several of the training programs examined and included group discussion and problem solving, demonstrations, role play/skill building exercises, and the sharing of recovery narratives. Most of the workshops included participation by individuals with a lived experience of mental illness as trainers; a strategy bolstered by the core message of empowerment advocated in recovery-oriented care and research findings that have indicated the benefits of using consumer trainers (e.g., Cook et al. 1995).
Overall, the outcome findings for recovery workshops have consistently demonstrated that improved knowledge of recovery principles and practices are quite achievable (Crowe et al. 2006; Gilburt et al. 2013; Meehan and Glover 2009; Peebles et al. 2009; Salgado et al. 2010; Wilrycx et al. 2012). In addition, findings support the position that beliefs and attitudes supportive of recovery-oriented care can be measurably enhanced through workshop trainings. These include attitudes of general hopefulness and optimism regarding recovery (Salgado et al. 2010), the belief that individuals with mental illness have skills and competence and are capable of participating in their own care (Peebles et al. 2009), and beliefs that individuals with mental illness are capable of setting and achieving goals even if symptoms are present (Crowe et al. 2006). It is noteworthy, however, that in their examination of a two-day recovery workshop, Peebles et al. (2009) indicated that while attitudes of hopefulness regarding recovery and beliefs about individuals’ ability to participate actively in their own care did increase, more stigmatizing attitudes such as beliefs that patients should be feared, pitied, and/or avoided, were not impacted by the workshop. This suggests that further work needs to be done to explore techniques or approaches that impact both positive and negative recovery attitudes.
In their examination of a four-day recovery workshop and an in-team half-day session on supporting recovery, Gilburt et al. (2013) found that providers’ knowledge, attitudes, and preliminary clinical practices were all positively impacted. Specifically, this workshop included the topic of assessment and care planning from service users’ perspective, and in an audit of the care plans of 700 patients, it was reported that the clinicians who participated in the workshop made significantly more changes to their plans consistent with service users’ perspectives than clinicians who did not participate in the workshop. Gilburt et al. (2013) further described qualitative findings pertaining to the impact of recovery workshops on the participants. They conducted 16 team leader interviews following their four-day workshops and an in-team session on supporting recovery. In these interviews, the training was highly rated with over half of the interviewees favoring mandated recovery training. Most viewed the training as leading to staff consideration of areas of care that emphasized improvement more so than just maintaining the patients’ current mental status. Also in a positive direction were attitudes that hope was a universally positive value that was integral to mental health care. There were, however, problematic reactions to the training experience. For example, following the training there continued to be confusion about what recovery meant, and many members of the staff believed that they “already did recovery.” Furthermore, following the training, many framed recovery as something primarily driven by staff, failing to appreciate the role of service users. While multidisciplinary services were considered a valuable aspect of recovery-oriented care, a prevailing attitude was that when physicians were not on-board, they could be barriers to recovery-oriented care. Many interviewees noted that recovery-oriented care was often seen as conflicting with, rather than complementing, the overarching roles of the service agency (e.g., “moving people on”). Finally, interviewees expressed doubts concerning the availability of resources to actually implement recovery-oriented care.
Efforts to successfully transfer or incorporate training into practice have been a longtime aspiration of those who seek to bring about the sustained implementation and application of new knowledge, skills, and attitudes in clinicians. Yet, trainers have often been left feeling disappointed about the degree of integration of the principles and practices in various settings. In regard to recovery-oriented care training, Uppal et al. (2010) examined the transfer of training impact of an initial two-day recovery training workshop, followed by one-day booster sessions between 6 and 12 months later. A core aspect of the recovery training was the use of collaborative goal-setting and collaborative homework assignments. In chart audits conducted six months after the individual training, approximately 37 % of the trained clinicians participating in the study were found to be implementing collaborative goal-setting and collaborative homework assignments in clinical practice. Moreover, the average time taken to implement these recovery practices was 5.6 months following training. Thus, it was concluded that transfer of recovery training in the form of recovery workshops followed by booster sessions may be difficult to achieve in clinical practice.
Deanne et al. (2014) examined the benefits of adding individual coaching for a 12-month period following the initial workshop trainings. The study compared the results of monthly coaching consisting of either an emphasis on skills acquisition training or transformational coaching that focused on clinicians’ personal values versus promotion of personal growth and/or professional development. Chart audits examining the use of collaborative goal-setting indicated that coaching in general, even though the study implementation only achieved coaching sessions approximately every two months, was able to improve transfer of training over workshops alone. There was some trend that the transformational coaching was somewhat superior in achieving clinicians’ use of care planning than the skills acquisition coaching.
The empirical study of recovery training is clearly in its infancy. Of the few published reports, the content and teaching techniques used to teach recovery-oriented care have been quite similar, but often lacked detail in regard to rationale and theory. The studies that do report outcomes of efforts to train clinicians in recovery-oriented care have generally reported positive results in terms of gains in recovery knowledge and attitudes, and initial steps toward recovery-oriented practice. It should be pointed out that this initially positive view of recovery-oriented training needs to be tempered by the relative absence of strong methodological designs used to study recovery training outcomes and initial findings that effective transfer of training to practice should not be assumed.
These initial studies also suggest that barriers to the adoption of recovery-oriented practice are evident and include clinician confusion about the principles and practice of recovery-oriented care as well as institutional issues, such as lack of resources, and an agenda that may not be compatible with recovery-oriented care (e.g., “moving people on”). In this early phase of “research and design” of recovery training, the unavoidable conclusion is that there is, as yet, no empirically based implementation strategy specific to training clinicians in effective applications of the recovery model. Nevertheless, there is valuable research and conceptual literature pertaining to effective methods of teaching and implementing changes in patient care practices that can be readily applied to the development of recovery-oriented care training.
Designing a Recovery-Oriented Care Training Model
As suggested by Stuart et al. (2004), education and training in health care is best viewed as a teaching-learning process, and in our consideration of this process we will now examine: (1) the content that need to be taught; (2) the characteristics of the targeted learners that would influence the teaching-learning process; (3) the characteristics of the training providers that would best facilitate desired outcomes; and (4) general teaching strategies designed to promote adoption of recovery-oriented care.
The Content that Needs to be Taught
Knowledge of Recovery. It is uncontroversial to suggest that any recovery-oriented training ought to teach the foundational principles of recovery. More controversial, however, is just what those foundational principles are. Since the inception of recovery-oriented care, there have been numerous disparate attempts to conceptualize, categorize, and define what is meant by recovery. Historically, the concept of recovery emanated from two distinct forces (Davidson and Roe 2007). One argument for rethinking traditional views of mental health care has been based on the accumulating evidence that the course of even serious mental illness is not inevitably negative. In fact, many people with serious mental illness can and do recover to levels that allow them to resume productive and meaningful lives even in the presence of enduring symptoms (Davidson et al. 2009). Moreover, these recoveries are not always brought about by traditional forms of mental health care, but often entail efforts independent of standard forms of treatment such as medications or psychotherapy (Davidson et al. 2009). From this clinical focus on people’s illness and dysfunction, there has been an emphasis on recovery being related to traditional clinical outcomes of amelioration or remission of symptoms.
A second argument pertains to the fundamental dissatisfaction with what consumers of mental health care characterize as paternalistic and stigmatizing care. Beginning in the late 1980s, a consumer movement arose in opposition to traditional mental health care and proposed that the emphasis on illness and dysfunction generated feelings of helplessness and hopelessness (Bellack 2006). In addition, it was argued that traditional care often placed patients in highly dependent roles in which personal choice and strengths were often overlooked. In response to these assertions against traditional mental health care, the concept of recovery became associated with processes that emphasized an empowerment approach to care that acknowledges the right to individual choice, equal partnership in care, and the pursuit of meaningful lives even in the context of illness. Slade (2009) differentiated between these two perspectives of recovery, with the former representing clinical recovery and the latter representing personal recovery. The teaching of recovery may benefit from the adoption of both of these ostensibly contrasting views of recovery. From an educational perspective, two arguments can be made for the use of both clinical and personal recovery concepts. First, adult learners come to learner situations with pre-existing knowledge and experiences that frame their expectations and influence their facility in learning new information. When there is an interaction between existing knowledge and new knowledge or skills, training success tends to be more likely (Lyon et al. 2011). In the context of training clinicians, it can be anticipated that teaching the concept of clinical recovery as a component of recovery-oriented care would validate their prior knowledge and skill, and make them more comfortable in expanding their view of recovery. Second, learners are more likely to be motivated to learn new knowledge or skills when it becomes clear that existing practices are inadequate (Lyon et al. 2011). By presenting both clinical and personal recovery concepts, the learner begins with the familiar understanding of recovery, but then can begin to see the insufficiency of clinical recovery in contrast to personal recovery that promotes a focus on the process of recovery (e.g., a way of living a satisfying, hopeful and meaningful life even with the limitations imposed by illness). Davidson et al. (2009) described this complementary approach to the concept of recovery and noted that the addition of recovery in a personal sense highlights that people do recover from mental illness and many more find meaning in the face of enduring illness.
A commonly used definition of recovery comes from SAMHSA (2006), initially defining mental health recovery as “a journey of healing and transformation enabling a person with a mental health problem to live a meaningful life in a community of his or her choice while striving to achieve his or her full potential.” Along with this definition, SAMHSA listed ten fundamental components of recovery: self-direction, individualized and person-centered, empowerment, holistic, nonlinear, strengths based, peer support, respect, responsibility, and hope. In 2012, SAMHSA offered a new working definition of recovery from mental disorders and/or substance use disorders, emphasizing that recovery is “[a] process of change through which individuals improve their health and wellness, live a self-directed life, and strive to reach their full potential (Paragraph 5).” In this updated definition of recovery, SAMHSA further delineated four dimensions that support recovery: health, home, purpose, and community. Though efforts to comprehensively define and elucidate the multiple pathways, processes, outcomes, and characteristics of a life in recovery are both necessary and laudable, it is the very breadth and heterogeneity of this construct that pose significant challenges to those who seek to educate about the principles and resulting practices associated with recovery. Specifically, critical reviews of the educational research that informs the teaching of clinicians have indicated that in terms of content, “Less is more” (Stuart et al. 2004; Van der Vleuten et al. 2000). That is, the less complex and more concise the material being taught, the more that will be attained and applied to clinical practice. For example, even a basic change, such as attempting to get health care providers to practice proper standards of hand washing, has proven to be quite difficult (Grol and Grimshaw 2003). Therefore, effective teaching of recovery-oriented practice must incorporate this “less is more” educational principle.
Leamy et al. (2011) provided a systematic review of 366 papers that explicitly described or developed a conceptualization of personal recovery. In so doing, they arrived at a narrative synthesis that sought to define the overarching processes of personal recovery, the acronym of which is CHIME: Connectedness (e.g., being a part of a community, having relationships, receiving support from others); Hope and optimism about the future; Identity (e.g., rebuilding/redefining positive sense of identity, overcoming stigma); Meaning in life (e.g., meaningful life goals and social roles, quality of life); and Empowerment (e.g., personal responsibility, control over life, and focusing on strengths).
We believe that these recovery processes are sufficiently representative of the domain of personal recovery while also being succinct thus making them a teachable model of recovery that can readily inform clinical practice.
Attitudes. Attitudes generally reflect a mental disposition and readiness that, for clinicians, can significantly influence reactions to and actions with individual with mental illness. Many leaders in the field contend that the concept of recovery fundamentally reflects an attitude about people with mental illness (e.g., Davidson et al. 2009; Resnick et al. 2005). Clinicians who hold positive attitudes toward recovery are more likely to promote empowerment and encourage an optimistic approach to the treatment of mental illness (Corrigan 2002). Thus, implementing recovery-oriented care requires clinician attitudes that support patient rights and empowerment. Through our examination of conceptual writing in the extant literature on recovery, as well as commonly used measures of recovery-oriented attitudes, the following attitudes emerge as key targets for recovery teaching efforts:
-
1.
Recovery is a civil right of the individual to access and join in those elements of community life that the person chooses and to be in control of his or her own life, including making choices about one’s own health care.
-
2.
Stigma toward individuals with mental illness is a significant part of the illness experience and thus should be addressed by clinicians as it exists in the community and within the system of mental health care.
-
3.
Individuals with mental illness are capable of being full partners in their own mental health care and they should be empowered to achieve their own recovery.
-
4.
Recovery can be difficult and its course will vary among people.
-
5.
Risk taking is an inevitable part of recovery processes and willingness to take risks is an essential aspect of empowering people to take control of their lives.
-
6.
Recovery is possible. It should be emphasized that a general sense of hopefulness about recovery being possible is an essential attitude to be held by clinicians and to be fostered in individuals collaborating in their care.
Clinician Competencies. While knowledge of recovery principles and processes along with attitudes supportive of recovery are foundational, recovery-oriented care will not take root unless clinicians change their practice in some fashion. In the absence of evidence-based recovery practices, the current state of the field is represented by various attempts to define clinician competencies that are necessary for recovery-oriented care. Lakeman (2010) conducted an online Delphi survey of experts in mental health recovery and identified 18 top-ranked recovery competencies of which the top five were (p. 62):
-
1.
A competent mental health worker recognizes and supports the personal resourcefulness of people with mental illness.
-
2.
To work in a recovery-focused way, mental health workers need to reflect a belief that recovery is possible.
-
3.
To work in a recovery-focused way, mental health workers need to be able to listen to what service users are actually saying and respect their views.
-
4.
To work in a recovery-focused way, mental health workers need to reflect respect for the expertise and unique knowledge gained as a result of having experienced mental health problems.
-
5.
A competent mental health worker helps persons in recovery to develop belief in themselves, thereby promoting their ability to help themselves.
Le Boutillier et al. (2011) conducted a qualitative analysis of international recovery-oriented practice guidelines and found 16 dominant themes within the following four practice domains (p. 1474):
-
1.
Promote citizenship—support individuals with mental illness to reintegrate into society and live as equal citizens.
-
2.
Organizational commitment—organizational commitment to ensure that there is a work environment and service structure that promotes recovery-oriented practice.
-
3.
Support personally defined recovery—there is a focus on supporting personally defined recovery and viewing recovery as the heart of clinical practice.
-
4.
Working relationship—clinician interactions demonstrate a genuine desire to support individuals and their families to fulfill their potential and shape their own future.
We view both of these aggregating efforts to establish practice competencies as meaningful at the broad policy and organizational level, though generally lacking in the specificity needed for the clinician in the field who is attempting to translate knowledge of recovery processes into competencies that they can learn to support recovery. Also, these proposed general competencies do not meet the educational principle of “less is more” and thus will likely be viewed by clinicians as too complex and time-consuming to be adopted in any meaningful way. In order to effectively teach recovery-oriented practice to clinicians, the competencies to be taught should meet the following criteria: (1) the competency conceptually links to one of the five core processes described in the CHIME model of personal recovery (see Leamy et al. 2011); (2) the competency can be readily integrated with the tasks generally focused on in clinical as opposed to personal recovery; and (3) the competency can be practiced within the usual time constraints of patient encounters.
As outlined in Table 4.1, we provide the competencies chosen by Project GREAT to be taught as an illustration of how these criteria may be applied. The competencies provided are not intended to be comprehensive or necessarily reflective of an optimal list of competencies for all mental health care settings. We contend, however, that the list of competencies suggested is sufficiently parsimonious, teachable, and adaptable to a variety of clinical contexts, from inpatient psychiatric settings to outpatient community clinics. Through our iterative efforts to disseminate and enhance recovery knowledge, attitudes, and practices via Project GREAT, we have discovered that even our own competency recommendations pose instructional challenges that require significant time, effort, feedback, and consistently honed teaching skills to execute training effectively. It is our hope that the proposals that we advance in this chapter will be of benefit to those seeking to impact learners in a personally meaningful manner that brings about sustained change in their recovery-oriented practices.
Characteristics of the Targeted Learners
Recovery-oriented care requires a fundamental shift in how clinicians address mental health care. Analysis of the targeted learners suggests three core features of clinicians that would need to be addressed to effectively teach them recovery-oriented care.
Indoctrinated in Traditional Views of Illness and Mental Health Care. Most clinicians hold core beliefs about mental illness and its treatment that are likely to be hindrances to the adoption of the transformative model of recovery. In traditional conceptualizations of mental illness, it is the clinician that is “the expert” and thus has primary responsibility for defining and “curing” illness. The focus on intervention begins with an accurate diagnosis formed by an assessment of symptoms and concludes with interventions designed to cure or ameliorate symptoms associated with the underlying illness.
From a recovery orientation, however, such a myopic view of mental illness neglects to consider that healing can entail more than the elimination or reduction of symptoms, and can touch on such profound issues as finding purpose and meaning in life even while experiencing the demands and stresses of mental illness. Traditional models of care maintain that the “nature of healing” lies in scientifically derived interventions designed and implemented by the expert to address the underlying etiology of mental illness. Though collaboration may be emphasized as an important component of the clinical strategy, the clinical recovery lens leans heavily on adherence to the prescribed treatment devised by the expert. Inevitably, this view of mental health care makes it difficult for clinicians to connect with other realties such as the importance of patients’ sense of ownership about their own recovery, their strengths, their resources, and healing actions that they might take that lie outside those prescribed by the clinician.
As is readily apparent, the teaching of clinicians in recovery-oriented care must necessarily encourage an expansion beyond traditional views of illness and associated treatments to fully embrace the possibility that satisfying and meaningful lives entail more than just the reduction or elimination of symptoms. Moreover, the practice of mental health care must acknowledge that there truly are two experts in the room that can and should share the responsibility for defining problems and devising pathways to recovery.
Finally, it is important to note that the traditional model of mental health care has been founded on the clinicians’ sense of duty to reduce risks for their patients. For example, the Hippocratic oath compels doctors to avoid doing harm to their patients, and medical risk management strategists advise against any practice that might risk an increase in symptoms or risk for relapse. Playing safe and avoiding risks are routinely taught and practiced in traditional models of care. Initial introductions to recovery-oriented care are often met with concerns by clinicians that the risks are too great to allow patients to make decisions about their own care when their judgment is impaired. They express fears associated with the possible risks to their patients’ wellbeing and their own professional liability should “bad” decisions be made. In contrast, recovery-oriented care must encourage clinicians to view self-determination and choice as patient rights that are an integral pathway to recovery. Moreover, individuals should be encouraged to take risks in the service of seeking opportunities for a life with greater purpose and meaning, even though making such efforts might result in an increase in stress and symptoms (see Davidson et al. 2006).
Stigmatizing Attitudes. Attitudinal surveys have suggested that clinicians have greater support for the civil rights of their patients and generally more positive attitudes toward individuals with mental illness than the general public. Yet, many clinicians also hold stigmatizing attitudes such as beliefs that individuals with mental illness are more dangerous and less capable than those without mental illness (Schulze 2007; Stuber et al. 2014b; Wahl and Aroesty‐Cohen 2010). Moreover, clinicians commonly appear to be quite similar to the general public in regard to a “them versus us” attitude in which they view individuals with mental illness as socially undesirable and people to be avoided (Schulze 2007; Stuber et al. 2014b; Wahl and Aroesty‐Cohen 2010). Unfortunately, such negative beliefs are likely to make it quite difficult for clinicians to fully engage with their patients as equal partners and have hopeful attitudes of achieving clinical or personal recovery.
The implications for the educator attempting to instill recovery-oriented principles and practices in clinicians are that stigmatizing attitudes must be identified and targeted for intervention. Based on research findings (e.g., Corrigan 2004; Corrigan et al. 2012; Rüsch et al. 2005; Wood and Wahl 2006), we propose the following efforts to diminish problems of stigma among clinicians: (1) education that identifies stigmatizing attitudes and provides information that counters misunderstandings regarding individuals with mental illness; (2) self-reflection and perspective taking that increase understanding for and empathy with individuals with mental illness; and (3) contacts with individuals with mental illness in contexts in which their competencies and general social desirability are manifest. At the very least, consumers should play active roles in recovery instruction of clinicians.
Adult Learners. Educational theory and research has pointed out that methods in teaching adults need to take into account their unique characteristics that distinguish them from children or adolescent learners. Based on representative theory and research in the field of health professional training (Bowen 2006; Bussema and Nemec 2006; Davies 2000; Stuart et al. 2004; Zisook et al. 2005), the following instructional strategies are advised in teaching clinicians recovery-oriented care:
-
1.
Adults have a foundation of life experiences and knowledge, and by drawing out connections of this existing data bank to the new knowledge, attitudes, and skills to be learned, adoption of the new material is facilitated. For example, the skills developed by clinicians in the context of developing treatment goals would be quite relevant for learning the skills required in developing life goals. More specifically, assessment of life goals and treatment goals require steps to turn general ideas into actions and behaviors, and both require specification of goals that can be addressed in the short-term as well as the long-term.
-
2.
Adults are relevancy oriented and thus they will need to see the reason for learning something. For example, the teaching of the nonlinear nature of recovery is more likely to be perceived as relevant by clinicians when the presentation of this concept includes clinical vignettes that illustrate problems of symptom relapse that may lead to premature termination of treatment by their patients.
-
3.
Adults are goal-directed, and thus instruction must show participants how the learning experience will help them attain their goals. For the clinician who is trained with a focus on clinical recovery, the complementary nature of clinical recovery and personal recovery could be emphasized. Considering relapse problems, clinicians will be more inclined to embrace the teaching of the nonlinear when it is emphasized that patients that are better informed about the ups and downs of recovery are more likely to sustain treatment efforts and bounce back from relapses of symptoms.
-
4.
Adults tend to be autonomous and self-directed in their learning style, and thus respond better to active learning. Consequently, clinicians are more likely to be engaged in learning recovery-oriented practices when there is a sense of challenge and active learning through Socratic questions, clinical vignettes are presented that pose problems to be solved, and skill practice are components of instruction.
The Characteristics of the Instructors
Learning recovery-oriented care entails more than merely transferring knowledge about recovery principles and practices. Integral to the practice of recovery-oriented care are the emotions and attitudes that have been compelling forces in the recovery movement. Therefore, the effectiveness of teaching recovery-oriented practice requires careful attention to the characteristics of the messenger and not just the message.
Provider - Driven Training. Educational research has consistently demonstrated that effective teachers are knowledgeable, establish clear goals of the instruction, and are able to present key information in an organized fashion using familiar and understandable language (Sutkin et al. 2008; Towler and Dipboye 2001). Moreover, effective teachers are generally approachable, open-minded, show patience and respect for students, care about students’ success and are fair, show enthusiasm and humor, and intentionally engage with their students to establish rapport (Benson et al. 2005; Sutkin et al. 2008).
In clinical contexts, the experience and expertise of the instructor play important roles in eliciting the attention of learners and helping them learn and retain knowledge and skills obtained during instruction (Burke and Hutchins 2008; Sutkin et al. 2008). Research has yet to be conducted on those characteristics of instructors that may effectively teach recovery-oriented care. On conceptual grounds, and based on Project GREAT’s experience in disseminating recovery-oriented care training over the past seven years, we propose the following additional characteristics of effective instructors:
-
1.
It is important to have instructors with similar educational and clinical experiences as those of the learners in order to maximize the relevance of the instruction being provided. Instructors with doctoral training in the mental health field and practical experience in the provision of mental health care have the advantage of familiarity with the existing knowledge, beliefs, attitudes, and practices of the learners targeted. With this knowledge of the learners, the content can be presented in an effective manner.
-
2.
Clinical teaching in general is demanding, and those who do it well have passion for their work as well as a high level of technical skill (Bussema and Nemec 2006; Irby and Papadakis 2001; Stuart et al. 2004). Likewise, the effective teaching of recovery-oriented care requires passion to convey the emotions and attitudes that are the compelling force behind the recovery movement. Therefore, to train others in recovery-oriented care, the instructor must possess a strong conviction of its worth and have the ability to stimulate serious contemplation of the fallibilities of traditional models of mental health care, while inspiring a heartfelt desire to do more for those facing the challenges of mental illness. The outcome of the recovery instruction will rely heavily on the ability of the instructor to passionately convey the message and to share inspiring stories that move clinicians toward recovery-oriented care.
-
3.
Finally, instructors who have personally experienced the process of transformation from a traditional model of mental health care to a recovery-based one are more likely to be more persuasive models of and advocates for recovery-oriented care. With this personal experience of professional practice change, the instructor would have the advantage of having a greater appreciation for the challenges involved in systems and practice change, and thus could better direct the learner in addressing these challenges. Moreover, a coping model of a clinician/instructor who has actively engaged in and succeeded in transforming his or her practice into a recovery model can be a valuable change agent.
Consumer - Driven Training. Recovery-oriented care champions the individuality of the lived experience and the ownership of the recovery process (Oades et al. 2005). Individuals with a lived experience of mental illness have valuable insights that can contribute to the development of curriculum and influence presentation of the recovery process (Young et al. 2005). Research has suggested that by involving consumers in mental health education both positive knowledge and attitude change can be enhanced (Happell et al. 2014; Wood and Wahl 2006). In addressing diverse problems with stigma/prejudice/discrimination, there is accumulating evidence that exposure to the stigmatized group can reduce adverse attitudinal and social responding problems (Wood and Wahl 2006).
Individuals with a lived experience of mental illness are not only helpful in teaching clinicians principles and practices of recovery, but also absolutely essential in addressing matters of attitude (e.g., perceptions of consumer competence and social desirability). By presenting competent consumers articulately telling their recovery stories, clinicians will begin to form more positive impressions of consumers and their ability to collaborate in their care. Moreover, by encouraging consumer educators to contrast their traditional psychiatric care experiences with recovery care experiences, clinicians would have “real” examples of the potential value of the recovery-oriented care. Consumer involvement in the education of clinicians can also better ensure that the curriculum content is responsive to the needs and goals of those individuals who use mental health services.
The use of consumer-driven education is not without some potential problems. For example, if consumers have limited teaching roles then they may experience a sense of tokenism in the educational enterprise and likewise clinician participants may devalue the consumer’s potential contributions while maintaining a “them versus us” attitude. Moreover, if presentations by individuals with mental illness are adversarial toward mental health professionals and/or reflect poor communication skills, then attitudes toward recovery-oriented care with its emphasis on collaborative care would be adversely affected. Therefore, we would propose the following qualifications and preparations to maximize the contribution of consumer-driven training:
-
1.
Consumer educators must have meaningful lived experiences with mental illness so that insights regarding the impact of mental illness and associated interventions can be shared with clinicians in an effective manner. Communication regarding these experiences may include negative experiences with clinicians, but these negative experiences should not be the sole message. In other words, consumer educators should be encouraged to convey a positive message of hope regarding recovery-oriented care as opposed to merely taking the opportunity to be critical of past encounters with clinicians.
-
2.
Consumer educators must also have meaningful recovery stories that they can effectively articulate in a manner that demonstrates how embracing recovery processes can lead to positive life outcomes. They certainly do not emphasize stories of clinical recovery and, in fact, consumer educators may be even more effective in their message when they present not as “expert models” but as “coping models” who continue to be challenged by mental illness, but demonstrate the courage and competence to achieve personal recovery.
-
3.
Consumer educators and professional instructors need to model a collaborative approach to the teaching of recovery-oriented care such that the learners can appreciate the reality that there are “two experts in the room,” and both appreciate and use the expertise of the other.
-
4.
As is the case with instructors, the effectiveness of consumer educators will rely heavily on their skills in gaining rapport with the learner, technical competence in teaching, and passion for recovery-oriented care. However, merely being an individual with a compelling recovery story is insufficient for the broader enterprise of teaching recovery-oriented care. Consumer educators also need to learn to appreciate the challenges that clinicians face, to recognize how clinicians think, to develop patience and diplomacy with those clinicians who have difficulty understanding and adopting recovery principles and practices, and to learn effective strategies for influencing clinicians’ attitudes and behaviors.
General Teaching Strategies
Attempting to achieve the transformative changes in clinicians’ knowledge, attitudes, and clinical practice behavior as advocated by the recovery approach to mental health care is a daunting enterprise. As Bussema and Nemec (2006, p. 315) stated, “… making lasting changes in the behavior of mental health practitioners is astoundingly difficult, and implementing new practices in mental health systems is painfully slow.” Moreover, there is no empirically based general teaching strategy specific to recovery-oriented care training. There is, however, valuable research literature pertaining to effective methods of teaching and implementing changes in patient care practices that can be applied to the teaching of recovery-oriented care. In examining original studies and systematic reviews regarding interventions to change medical practices across disciplines, the most robust and consistent finding has been that single teaching strategies are ineffective in changing practice behaviors (Grol and Grimshaw 2003; Lyon et al. 2011). Instead, changes in medical practice are more likely when multiple strategies are implemented (Chow et al. 2009; Grol and Grimshaw 2003). On the basis of a narrative review of the effectiveness of various teaching strategies in changing clinical practice as well as consideration of the resource and time feasibility of implementing teaching strategies within traditional mental health settings, we propose the following five general strategies for teaching recovery-oriented care.
Workshops and Courses. Despite evidence of its modest effectiveness, direct instruction of recovery-oriented practice through workshops or courses likely represents a necessary though insufficient strategy for teaching recovery. Effective recovery workshops and courses should have the following characteristics:
Content that needs to be taught. The content of instruction should adhere to the “less is more” principle in which complexity is reduced as much as possible. The concepts of clinical recovery (i.e., “recovery from”) and personal recovery (i.e., “recovery in”) should be taught as legitimate components of clinical practice, although the insufficiency of sole attention to clinical recovery should be highlighted. In addition to recovery principles and processes, instruction should also explicitly address clinician attitudes and competencies that are needed to support recovery-oriented care.
Characteristics of the targeted learners. Indoctrinated in traditional views of mental illness and care, clinicians should be instructed in a more expanded view of care that recognizes the possibility of a satisfying and meaningful life even when patients are experiencing ongoing psychiatric symptoms. Furthermore, the value of and civil right to receive a collaborative model of mental health care should be emphasized. Clinicians should be challenged to recognize and directly address their own stigmatizing views of the individuals that they serve. In the endeavor to teach adult learners, recovery instruction should acknowledge and use clinicians’ existing knowledge and experiences, make the case for the clinical relevance of recovery processes and practices, link recovery instruction with clearly articulate clinician goals, and employ active learning strategies such as discussion questions, problem solving around case vignettes, and skill practice.
Characteristics of the instructors. Both clinicians and individuals with lived experience with mental illness and its treatment best deliver instruction in recovery. In addition to having skills in engaging with and teaching adult learners, both professional instructors and consumer educators need to be knowledgeable, experienced, and passionate regarding recovery-oriented care. Furthermore, the professional instructors and consumer educators need to be able to effectively model respect for one another and a collaborative partnership in the teaching endeavor.
Coaching. As previously noted, one of the few empirical findings regarding efforts to train clinicians in recovery-oriented care demonstrated that the addition of individual coaching enhanced the transfer of recovery knowledge into practice (Deane et al. 2014). In this strategy, the instructor meets with the individual clinician in the work setting and offers feedback and instruction directly related to the clinician’s attitudes and behavior. Thus, coaching not only provides more specific and direct feedback to the learner, but also it extends the time of instruction and provides instruction within the highly relevant context of actual clinical practice (Lyon et al. 2011). In addition, coaching provides an opportunity for the instructor to address the clinician’s questions and ambivalence about adopting new clinical practices and supporting the clinician’s morale and engagement in the adoption of recovery-oriented practice (Lyon et al. 2011).
Reminders/Prompts. Research has indicated that prompts to engage in recommended practice habits can be effective in implementing clinical care changes (Grol and Grimshaw 2003; Lyon et al. 2011; Stuart et al. 2004). Point-of-care reminders or prompts are provided in the context of routine practice and can be issued in the form of written or electronic communications. For example, Project GREAT has used worksheets provided to patients that inquire about their life goals and strengths that are to be shared with their clinicians. Thus, clinicians are reminded by their patients of the importance of obtaining and using such information that is vital to recovery-oriented care. Project GREAT also embedded prompts for recovery-oriented care in the electronic health care record so that all documentation of care templates includes recovery-relevant information. Of course, the most effective reminders or prompts require a response from the clinician (e.g., acknowledging a receipt of information or documenting that a certain practice was performed) and, with the increasing use electronic records, the technology is available to insure that clinicians are at least responding to recovery-oriented care reminders/prompts.
Audit and Feedback. This strategy entails periodic audits of clinician’s professional practice along with feedback offered to the clinician with accompanying benchmarks or peer comparisons. The feedback may or may not include practice recommendations to guide the clinician’s future behavior. Research has suggested that audit and feedback may be most effective when there is significant room for improvement, the person responsible for the audit and feedback is a supervisor or colleague, the process is repeatedly provided, feedback is provided in both verbal and written forms, and feedback includes clear targets for action (Ivers et al. 2012). As an example of how this might be applied to the teaching of recovery-oriented care, Project GREAT took advantage of the audit and feedback system within the institution which consisted of a routinely administered patient satisfaction survey. Specifically, we have been able to revise the departmental patient satisfaction measure to better assess recovery-oriented care by including the five-item Empowerment subscale of the Recovery-Promoting Relationship Scale (Russinova et al. 2006). Patient satisfaction information can be used as a training tool for individual clinicians as well as used as a metric for monitoring overall progress in the implementation of recovery-oriented care in the department.
Mass Media Communications in the Form of Newsletters/Pamphlets. Mass media campaigns have been used to modify health knowledge, attitudes, and behaviors in the general population using a variety of social marketing strategies. These efforts have realized promising outcomes in changing clinician behaviors as well (Grol and Grimshaw 2003). For example, mass media campaigns have had positive impact in reducing excessive antibiotic dispensing (Butler et al. 2012). From the perspective of training clinicians, the premise is that broad efforts to change patients’ behavior can result in changes in clinicians’ behavior. In the context of recovery-oriented care, transformation of knowledge, attitudes, and behaviors in clinicians can be greatly enhanced by changes in individuals that they serve. That is, by teaching the consumer about the processes of personal recovery, the manner in which they relate to their clinicians and their positive engagement in their own care could be quite influential on the practice of clinicians.
SAMHSA’s Recovery to Practice initiative provides an excellent example of a program that broadly disseminates recovery-oriented information through an online centralized information center that has the potential to impact how clinician’s use recovery processes and practices in their care as well as how consumers of mental health services participate in their care. Project GREAT has employed two teaching strategies along this line. First, a newsletter entitled “Taking Flight” is broadly distributed to patients and clinicians providing a recovery story as well as instruction on recovery processes and practices. Second, a patient pamphlet is distributed at the time of the initial appointment entitled, “Making the Most of Your Care.” This pamphlet provides basic information about the clinic and the services available, and also instructs patients on an active and collaborative approach to their own care.
Conclusion
Despite the broad advocacy for recovery-oriented care, there are significant challenges to the teaching and implementation of a recovery orientation to mental health care. In addition to the challenges imposed by the complexities of defining recovery-oriented care, the traditional views of mental illness and treatment as well as ongoing stigmatizing attitudes of clinicians, there are practice stresses that will likely limit the efforts of teaching recovery-oriented care. For example, time with the doctor is limited and has been steadily decreasing over the past 20 years across all of medicine and specifically in psychiatric care (Olfson et al. 1999). For the most part, there is an insufficient workforce to provide the mental health care that is needed for our society today, and thus caseloads of existing mental health workers are quite high, limiting the time needed for training in recovery-oriented care.
Moreover, it is not surprising that psychiatric practice appears to be drifting toward primarily psychopharmacological management with precious little time available to address such recovery matters as identifying life goals relevant for treatment or identification and utilization of consumer strengths and supports to achieve life goals. That “health care comes at a price,” has also been increasing over the past 20 years (Rowan et al. 2013). Though mental health care is more than just a commodity that responds predictably to market pressures, the reality is that the financial price tag for recovery-oriented care must be addressed.
Systems adopting the recovery model of care have to consider how to pay for the training and how to get reimbursement for what, at present, does not fall into the traditional forms of psychiatric care (e.g., peer specialist services and psychoeducational training in wellness activities versus traditional services that are reimbursed—diagnostic assessments, medication management, and psychotherapy). In addition, the mental health care system has been persistently “underfunded and undermanned” (Appelbaum 2002) and, as a result, the mental health system has by and large become focused on crisis stabilization and does not aspire to longer term goals that are the focus of recovery. Unfortunately, this crisis stabilization focus likely perpetuates and at times exacerbates the deteriorating patterns of more frequent and more severe relapses, further driving the focus of care toward symptom reduction rather than the development of sustained efforts to develop and build upon the broader goals of developing a life of meaning and purpose.
Overcoming these challenges to the teaching and implementation of recovery-oriented care will require administrative leadership and support. Written policies that promote recovery-oriented practice and even the hiring of peer specialists can represent only token measures that ultimately fail to achieve the cultural changes needed. Instead, there will need to be administrative leadership that promotes an organizational mission and vision that truly embraces recovery and commits the necessary capital to recovery-oriented training and practice. Administrative leadership will also be needed to build a consensus among the clinicians in a system of care that values recovery and believes that the goals of recovery can be achieved. Essential will be administrative steps to integrate consumers as full partners in the education of clinicians including roles of designing recovery-oriented curricula and providing teaching to clinicians. Finally, administrative leadership is needed to balance the organization’s need to reduce risk and contain cost with the higher calling of giving individuals, facing the challenges of mental illness the hope that a recovery journey can be achieved that offers worth and meaningful connections with others.
We have learned through Project GREAT that exposure to recovery stories can be a powerful tool in overcoming the challenges facing recovery-oriented care. While we embrace the value of using empirical evidence to support the design and implementation of teaching strategies to support the adoption of recovery-oriented care, we have learned that personal recovery stories can inspire genuine change in clinicians’ attitudes and practice behaviors. Inherent in these recovery stories are a deeper understanding of the lived experiences of those facing the challenges of mental illness. Inherent in their telling is an authenticity that recovery is “real” and not just an aspiration drawn from the more abstract principles of recovery. Moreover, recovery stories convey struggles and emotions that stir up affect in the learner that can more effectively influence beliefs, attitudes, and behaviors than mere presentation of recovery principles. And, for clinicians and patients alike, recovery stories provide vivid pictures of coping models that did not easily provide recovery-oriented care or overcome the challenges of mental illness. And yet in those stories can be found partners in care who had the courage and determination to endure hardships and setbacks in order to achieve lives of purpose and meaning.
References
Appelbaum, P. S. (2002). Starving in the midst of plenty: The mental health care crisis in America. Psychiatric Services, 53(10), 1247–1248.
Bellack, A. S. (2006). Scientific and consumer models of recovery in schizophrenia: Concordance, contrasts, and implications. Schizophrenia Bulletin, 32(3), 432–442.
Benson, T. A., Cohen, A. L., Buskist, W., Gurung, R. A., Cann, A., Marek, P., et al. (2005). Faculty forum. Teaching of Psychology, 32(4), 237–270.
Bowen, J. L. (2006). Educational strategies to promote clinical diagnostic reasoning. New England Journal of Medicine, 355(21), 2217–2225.
Burke, L. A., & Hutchins, H. M. (2008). A study of best practices in training transfer and proposed model of transfer. Human Resource Development Quarterly, 19(2), 107–128.
Bussema, E., & Nemec, P. (2006). Effective teaching. Psychiatric Rehabilitation Journal, 29(4), 315–317.
Butler, C. C., Simpson, S. A., Dunstan, F., Rollnick, S., Cohen, D., Gillespie, D., & Evans, M. R. (2012). Effectiveness of multifaceted educational programme to reduce antibiotic dispensing in primary care: Practice based randomised controlled trial. British Medical Journal, 344, d8173.
Chow, C., Cichocki, B., & Leff, H. S. (2009). The support for evidence-based training strategies. Psychiatric Rehabilitation Journal, 33(2), 156–159.
Cook, J. A., Jonikas, M. J. A., & Razzano, L. (1995). A randomized evaluation of consumer versus nonconsumer training of state mental health service providers. Community Mental Health Journal, 31(3), 229–238.
Corrigan, P. (2004). How stigma interferes with mental health care. The American Psychologist, 59(7), 614–625.
Corrigan, P. W. (2002). Empowerment and serious mental illness: Treatment partnerships and community opportunities. Psychiatric Quarterly, 73(3), 217–228.
Corrigan, P. W., Morris, S. B., Michaels, P. J., Rafacz, J. D., & Rüsch, N. (2012). Challenging the public stigma of mental illness: A meta-analysis of outcome studies. Psychiatric Services, 63(10), 963–973.
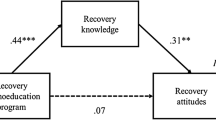
Crowe, T., Deane, F., Oades, L., Caputi, P., & Morland, K. (2006). Effectiveness of a collaborative recovery training program in Australia in promoting positive views about recovery. Psychiatric Services, 57(10), 1497–1500.
Davidson, L., & Dain, D. (2010). Recovery to practice—Project overview. Retrieved November 16, 2011, from http://www2.dsgonline.com/rtp/webinar_materials/Handout%201.6.8.10.pdf
Davidson, L., Drake, R. E., Schmutte, T., Dinzeo, T., & Andres-Hyman, R. (2009). Oil and water or oil and vinegar? Evidence-based medicine meets recovery. Community Mental Health Journal, 45(5), 323–332.
Davidson, L., O’Connell, M., Tondora, J., Styron, T., & Kangas, K. (2006). The top ten concerns about recovery encountered in mental health system transformation. Psychiatric Services, 57(5), 640–645.
Davidson, L., & Roe, D. (2007). Recovery from versus recovery in serious mental illness: One strategy for lessening confusion plaguing recovery. Journal of Mental Health, 16(4), 459–470.
Davies, P. (2000). Approaches to evidence-based teaching. Medical Teacher, 22(1), 14–21.
Deane, F. P., Andresen, R., Crowe, T. P., Oades, L. G., Ciarrochi, J., & Williams, V. (2014). A comparison of two coaching approaches to enhance implementation of a recovery-oriented service model. Administration and Policy in Mental Health and Mental Health Services Research, 41, 660–667.
Gilburt, H., Slade, M., Bird, V., Oduola, S., & Craig, T. K. (2013). Promoting recovery-oriented practice in mental health services: A quasi-experimental mixed-methods study. BMC Psychiatry, 13, 167–178.
Greenberg, G. A., & Rosenheck, R. A. (2009). An evaluation of an initiative to improve Veterans Health Administration Mental Health Services: Broad impacts of the VHAs mental health strategic plan. Military Medicine, 174(12), 1263–1269.
Grol, R., & Grimshaw, J. (2003). From best evidence to best practice: Effective implementation of change in patients’ care. The Lancet, 362(9391), 1225–1230.
Happell, B., Byrne, L., McAllister, M., Lampshire, D., Roper, C., Gaskin, C. J., & Lakeman, R. (2014). Consumer involvement in the tertiary-level education of mental health professionals: A systematic review. International Journal of Mental Health Nursing, 23(1), 3–16.
Hardiman, E., & Hodges, J. (2008). Professional differences in attitudes toward and utilization of psychiatric recovery. Families in Society, 89(2), 220–227.
Irby, D. M., & Papadakis, M. (2001). Does good clinical teaching really make a difference? The American Journal of Medicine, 110(3), 231–232.
Ivers, N., Jamtvedt, G., Flottorp, S., Young, J. M., Odgaard-Jensen, J., French, S. D., et al. (2012). Audit and feedback: Effects on professional practice and healthcare outcomes. Cochrane Database Systematic Review, 6.
Lakeman, R. (2010). Mental health recovery competencies for mental health workers: A delphi study. Journal of Mental Health, 19(1), 62–74.
Le Boutillier, C., Leamy, M., Bird, V. J., Davidson, L., Williams, J., & Slade, M. (2011). What does recovery mean in practice? A qualitative analysis of international recovery-oriented practice guidance. Psychiatric Services, 62(12), 1470–1476.
Leamy, M., Bird, V., Le Boutillier, C., Williams, J., & Slade, M. (2011). Conceptual framework for personal recovery in mental health: Systematic review and narrative synthesis. The British Journal of Psychiatry, 199(6), 445–452.
Lyon, A. R., Stirman, S. W., Kerns, S. E., & Bruns, E. J. (2011). Developing the mental health workforce: Review and application of training approaches from multiple disciplines. Administration and Policy in Mental Health and Mental Health Services Research, 38(4), 238–253.
Meehan, T., & Glover, H. (2009). Using the Recovery Knowledge Inventory (RKI) to assess the effectiveness of a consumer-led recovery training program for service providers. Psychiatric Rehabilitation Journal, 32(3), 223–226.
Oades, L., Deane, F., Crowe, T., Lambert, W. G., Kavanagh, D., & Lloyd, C. (2005). Collaborative recovery: an integrative model for working with individuals who experience chronic and recurring mental illness. Australasian Psychiatry, 13(3), 279–284.
Olfson, M., Marcus, S. C., & Pincus, H. A. (1999). Trends in office-based psychiatric practice. American Journal of Psychiatry, 156(3), 451–457.
Peebles, S. A., Mabe, P. A., Davidson, L., Fricks, L., Buckley, P. F., & Fenley, G. (2007). Recovery and systems transformation for schizophrenia. The Psychiatric Clinics of North America, 30(3), 567–583.
Peebles, S. A., Mabe, P. A., Fenley, G., Buckley, P. F., Bruce, T. O., Narasimhan, M., & Williams, E. (2009). Immersing practitioners in the recovery model: An educational program evaluation. Community Mental Health Journal, 45(4), 239–245.
Razzano, L. A., Jonikas, J. A., Goelitz, M. A., Hamilton, M. M., Marvin, R., Jones-Martinez, N., & Cook, J. A. (2010). The recovery education in the academy program: Transforming academic curricula with the principles of recovery and self-determination. Psychiatric Rehabilitation Journal, 34(2), 130–136.
Resnick, S. G., Fontana, A., Lehman, A. F., & Rosenheck, R. A. (2005). An empirical conceptualization of the recovery orientation. Schizophrenia Research, 75(1), 119–128.
Rowan, K., McAlpine, D. D., & Blewett, L. A. (2013). Access and cost barriers to mental health care, by insurance status, 1999–2010. Health Affairs, 32(10), 1723–1730.
Rüsch, N., Angermeyer, M. C., & Corrigan, P. W. (2005). Mental illness stigma: Concepts, consequences, and initiatives to reduce stigma. European Psychiatry, 20(8), 529–539.
Russinova, Z., Rogers, E. S., & Ellison, M. L. (2006). RPRS manual: Recovery promoting relationships scale. Bostob, MA: Boston University, Center for Psychiatric Rehabilitation.
Salgado, J. D., Deane, F. P., Crowe, T. P., & Oades, L. G. (2010). Hope and improvements in mental health service providers’ recovery attitudes following training. Journal of Mental Health, 19(3), 243–248.
Schulze, B. (2007). Stigma and mental health professionals: a review of the evidence on an intricate relationship. International Review of Psychiatry (Abingdon, England), 19(2), 137–155.
Slade, M. (2009). The contribution of mental health services to recovery. Journal of Mental Health, 18(5), 367–371.
Snyder, C. R., Ilardi, S. S., Cheavens, J., Michael, S. T., Yamhure, L., & Sympson, S. (2000). The role of hope in cognitive-behavior therapies. Cognitive Therapy and Research, 24(6), 747–762.
Stuart, G., Tondora, J., & Hoge, M. (2004). Evidence-based teaching practice: Implications for behavioral health. Administration and Policy in Mental Health and Mental Health Services Research, 32(2), 107–130.
Stuber, J., Rocha, A., Christian, A., & Johnson, D. (2014a). Predictors of recovery-oriented competencies among mental health professionals in one community mental health system. Community Mental Health Journal, 50, 909–914.
Stuber, J. P., Rocha, A., Christian, A., & Link, B. G. (2014b). Conceptions of mental illness: Attitudes of mental health professionals and the general public. Psychiatric Services, 65(4), 490–497.
Substance Abuse and Mental Health Services Administration. (2006). National consensus statement on mental health recovery. Rockville, MD: U.S. Department of Health and Human Services. Retrieved from http://mentalhealth.samhsa.gov/publications/allpubs/SMA05-4129/
Substance Abuse and Mental Health Services Administration. (2012). SAMHSA’s working definition of recovery. Rockville, MD: U.S. Department of Health and Human Services, U.S.
Sutkin, G., Wagner, E., Harris, I., & Schiffer, R. (2008). What makes a good clinical teacher in medicine? A review of the literature. Academic Medicine, 83(5), 452–466.
Towler, A. J., & Dipboye, R. L. (2001). Effects of trainer expressiveness, organization, and trainee goal orientation on training outcomes. Journal of Applied Psychology, 86(4), 664–673.
Tsai, J., Salyers, M. P., & Lobb, A. L. (2010). Recovery-oriented training and staff attitudes over time in two state hospitals. Psychiatric Quarterly, 81(4), 335–347.
Tsai, J., Salyers, M. P., & McGuire, A. B. (2011). A cross-sectional study of recovery training and staff attitudes in four community mental health centers. Psychiatric Rehabilitation Journal, 34(3), 186–193.
Uppal, S., Oades, L. G., Crowe, T. P., & Deane, F. P. (2010). Barriers to transfer of collaborative recovery training into Australian mental health services: Implications for the development of evidence-based services. Journal of Evaluation in Clinical Practice, 16(3), 451–455.
Van der Vleuten, C. P. M. V. D., Dolmans, D. H. J. M., & Scherpbier, A. J. J. A. (2000). The need for evidence in education. Medical Teacher, 22(3), 246–250.
Wahl, O., & Aroesty-Cohen, E. (2010). Attitudes of mental health professionals about mental illness: A review of the recent literature. Journal of Community Psychology, 38(1), 49–62.
Wilrycx, G., Croon, M., van den Broek, A., & Van Nieuwenhuizen, C. (2012). Mental health recovery: Evaluation of a recovery-oriented training program. The Scientific World Journal. doi:10.1100/2012/820846. (ID: 820846).
Wood, A. L., & Wahl, O. F. (2006). Evaluating the effectiveness of a consumer-provided mental health recovery education presentation. Psychiatric Rehabilitation Journal, 30(1), 46–53.
Young, A. S., Chinman, M., Forquer, S. L., Knight, E. L., Vogel, H., Miller, A., & Mintz, J. (2005). Use of a consumer-led intervention to improve provider competencies. Psychiatric Services, 56(8), 967–975.
Zisook, S., Benjamin, S., Balon, R., Glick, I., Louie, A., Moutier, C., & Servis, M. (2005). Alternate methods of teaching psychopharmacology. Academic Psychiatry, 29(2), 141–154.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Alex Mabe, P., Rollock, M., Duncan, G.N. (2016). Teaching Clinicians the Practice of Recovery-Oriented Care. In: Singh, N., Barber, J., Van Sant, S. (eds) Handbook of Recovery in Inpatient Psychiatry . Evidence-Based Practices in Behavioral Health. Springer, Cham. https://doi.org/10.1007/978-3-319-40537-7_4
Download citation
DOI: https://doi.org/10.1007/978-3-319-40537-7_4
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-40535-3
Online ISBN: 978-3-319-40537-7
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)